Abstract
The Diagnostic and Statistical Manual of Mental Disorders’ (5th ed.) Social (Pragmatic) Communication Disorder is meant to capture the social elements of communication dysfunction in children who do not meet autism spectrum disorder criteria. It is unclear whether Social (Pragmatic) Communication Disorder captures these elements without overlapping with Autism Spectrum Disorder or the Diagnostic and Statistical Manual of Mental Disorders’ (5th ed.) Language Disorder. Standardized behavioral assessments administered during a family genetics study were used to evaluate the social communication impairment and the restricted interests and repetitive behaviors in persons with autism spectrum disorder, language impairment, or neither. Social communication impairment and restricted interests and repetitive behavior were significantly correlated in all family members regardless of affection status. Rates of social communication impairment and restricted interests and repetitive behavior were highest in individuals with autism spectrum disorder. One-third of family members with language impairment presented with at least mild/ moderate levels of social communication impairment (36.6%) and restricted interests and repetitive behavior (43.3%). A subset of unaffected members also presented with mild/moderate levels of social communication impairment (parents = 10.1%, siblings 11.6%) and restricted interests and repetitive behavior (parents = 14.0%, siblings= 22.1%). The majority of child family members with mild/moderate levels of social communication impairment had similar restricted interest and repetitive behavior levels reflecting criteria representing the Broad Autism Phenotype. These data suggest that social pragmatic communication disorder does not capture the profiles of children who have both social communication impairment and restricted interests and repetitive behavior but are in need of clinical services.
A commentary by Brukner-Wertman et al., (2016) brought to the forefront issues that have been circulating since DSM-5 (American Psychiatric Association, 2013) redefined autism spectrum disorders (ASD) in 2013. Two, instead of three, distinct behavioral categories necessary to meet the diagnosis of ASD were created: social interaction and social communication impairment (SCI) and restricted interests and repetitive behaviors (RRB). In addition, a new diagnostic category was created to address those children who presented with only one of the core ASD criteria (SCI) but showed no clinical-level evidence of the other (RRB). Questions remain for many medical and clinical professionals as to the utility of this new category: Social Pragmatic Communication Disorder (SPCD). Are there tools that clinical professionals can use (besides DSM-5) to make this differential diagnosis of ASD versus SPCD and are the core characteristics of ASD so compartmentalized that one can actually exist without the other? In other words, 1) Can a social impairment as characterized in ASD exist independently from restricted interests and repetitive behaviors, and if so how does this impact the diagnosis of SPCD? 2) Is SPCD similar to the current definition of the Broad Autism Phenotype (BAP), a description of subclinical ASD behaviors? 3) Are there current standardized measures that can aid in the differential diagnosis of SPCD from ASD?
The introduction of SPCD and the uncoupling of SCI and RRB raises questions not only for clinicians but also for scientists, especially behavioral geneticists, who have looked at distinct endophenotypes in family studies of ASD and other psychiatric disorders where social impairment or OCD-like and restricted interests and repetitive behaviors are relevant. While there is still hope that specific behaviors can be valuable tools for targeting genetic variants, specifically in ASD, scientists are more aware than ever that multiple disorders share behaviors and thus, may also share genetic variants (Buxbaum, 2015; Gandal et al., 2018). If SCI and RRB are not separable and co-occur more often than not, then perhaps neither can stand alone as a distinct independent phenotype and attempting to segregate them is not helpful for research nor in the clinical world where access to services may depend upon a specific diagnosis.
Presently, other than DSM-5 criteria, there are no published, standardized measures that specifically address SPCD, a criticism recently addressed by Visser and Tops (2017). The diagnosis is made primarily by those professionals who use the DSM-5 during an observational office assessment and caregiver interview. This type of clinical environment can be hampered by the fact that it is often difficult for a clinician to create an appropriate communication setting to assess social skills during an office visit (Norbury, 2014). Other critics suggest that the category of SPCD was released before any empirical evidence of separable constructs had been developed to support the diagnostic category (Ash et al., 2017) and before consideration such as sex differences could be explored (Halladay et al., 2015).
In this paper, we attempt to address the issues related to SPCD by analyzing data from families who were recruited for a family genetics study of ASD. 1) We examine the rates and independence issues related to SCI and RRB in affected and unaffected family members. 2) We refer to the extensive body of work that exists over the past decade on the Broad Autism Phenotype (BAP) in families of children on the autism spectrum suggesting that SPCD fits comfortably into the definition of the Broad Autism Phenotype, a behavioral pattern where there are already assessments available to reliably assess the characteristics that comprise the SPCD diagnosis.
Social Pragmatic Communication Disorder and the Broad Autism Phenotype
Prior to DSM-5 there were three separate categories of behavior required to meet the diagnosis of ASD: Social interaction, Communication, and Restricted, Repetitive and Stereotyped Behaviors. Social Interaction and Communication have been essentially merged into a single criterion called Social Communication (with structural language as an auxiliary descriptor) while the RRB criteria remain relatively the same except for the addition of sensory issues, behaviors not included in DSM-IV. Social Pragmatic Communication Disorder (SPCD) was introduced to include children who did not meet the new ASD diagnostic criteria but in the past might have met criteria for DSM-IV, PDD-NOS, including evidence of restricted interests and repetitive behaviors (Swineford et al., 2014). By definition, children with SPCD present with social communication issues that do not meet DSM-5 ASD 299.00 (F84.0) or Language Disorder DSM-5 315.39 (F80.9). SPCD is defined as a developmental disorder characterized by difficulties related to social, verbal, and non-verbal communication. To receive this diagnosis, weaknesses in the four following categories of social communication must be present: 1. Using social communication for purposes such as greeting or exchanging information; 2. Changing communication to match context or the needs of the listener; 3. Following rules for conversation or storytelling, such as taking turns in conversation; 4. Difficulty understanding what is not explicitly stated. Exclusionary criteria include the language disorder diagnosis mentioned above. It is unclear what the fate is of children who meet the criteria of SPCD and demonstrate subclinical RRB behaviors. This raises the question, can these two categories of behavior be separated in any individual? This is where the issue of independence of SCI and RRB characteristics emerges and whether even subclinical RRB behaviors can exacerbate social impairment thus, raising the question of co-occurrence and possibly cause and effect. The fact that for a diagnosis of ASD, a child must be affected for all three SC categories and at least two of four RRB categories implies distinct behaviors and a distinct separation between SC and RRB.
Currently, there are several instruments that address pragmatic skills and social language in children. Most widely used is the Children’s Communication Checklist −2 (CCC-2) (Bishop, 2003). The CCC-2 is a revision of the original checklist (Bishop, 1998) developed to assess communication skills in children. It consists of 10 subscales with five items in each. The subscales address measures of structural language, higher order language, pragmatic language, social issues, and interests. The examiner can also derive a Social Interaction Deviance Composite from a subset of the subscales that closely aligns with behaviors identified in autism spectrum disorders. While useful in identifying specific social behaviors, results often identify social communication impairments in children who also present with structural language impairment (Norbury et al., 2004), an exclusionary criterion for SPCD. In a review paper, Norbury (2014) referenced several parent/teacher reports and structural observation assessments that examined pragmatic language and social communication. However, other than the Autism Diagnostic Observation Schedule-2 (Lord et al., 2012), few assessments directly address the other behaviors associated with ASD such as repetitive behaviors and those assessments that do, are lengthy and not practical in a busy clinical setting.
The Broad Autism Phenotype (BAP) is a well-documented behavioral phenotype that was first identified in the 1990s and has been studied by multiple researchers interested in observing and documenting the behavioral characteristics of family members of individuals with ASD (Bailey et al., 1998; Fombonne et al., 1997; Micali et al., 2004; Piven, 1997). It is equally widely recognized in the quantitative genetics literature and has been used to create behavioral endophenotypes for genetic analyses, especially in family studies (Constantino et al., 2004; Losh and Piven, 2007). The BAP includes groups of sub-threshold social skills, communication traits, and unusual personality features that are frequently found in the relatives of people with autism (both children and adults). They are believed to be milder manifestations of trait characteristics for clinically diagnosed autism. Among the characteristics are problems with social behavior including difficulties in communication (both verbal and nonverbal), social cognition, awareness, and rigidity.
There are several available diagnostic questionnaires that assess the BAP in adults. One of the first, The Pragmatic Rating Scale (Landa et al., 1992), is a 30-item observation scale developed to assess pragmatic behaviors in parents of children with ASD. Other popular scales include The Broad Autism Phenotype Questionnaire (BAPQ) (Hurley et al., 2007), a 36 item self- reporting questionnaire originally developed for parents of children on the autism spectrum and the Broader Phenotype Autism Symptom Scale (BPASS) (Dawson et al., 2007), originally developed for genetic studies and is a more involved assessment including an interview that requires training in order to administer. Finally, the Autism-Spectrum Quotient (AQ) (Baron-Cohen et al., 2001) is a 50 item self-assessment for teenagers and adults. The Social Responsiveness Scales (SRS, SRS-2) (Constantino, 2005; Constantino, 2012), has been used in multiple studies of BAP. The SRS was originally developed to measure the severity of autism spectrum symptoms in children with ASD, but it has been used successfully to capture mild phenotypic symptoms in both children and adults, making it a very useful tool for family studies of ASD.
In this paper, we addressed and began to untangle the issues associated with the independence of social impairment and restricted and repetitive behaviors and how current published assessments might or might not be informative for the diagnosis of SPCD. Addressing these issues helped us to determine if separating SC and RRB as clinical characteristics was a reasonable approach for diagnosing SPCD in children. An alternative approach would include acknowledging an overlap of SC and RRB, thus representing a diagnosis more consistent with BAP. In the long run, a more inclusive BAP diagnosis could better serve children who do not meet criteria for ASD or language impairment but require clinical services and guidance.
This present study is based on a larger study that consisted of families with at least one individual on the autism spectrum with or without a structural language impairment, at least one other individual with a structural language impairment, and unaffected family members. Because there was a heavy loading for language impairment and ASD in these families, this type of pedigree was ideal for disambiguating the characteristics of ASD from language and communication impairments, both social and structural. It allows for identifying traits of SPCD in children and traits of BAP in all family members and to explore if the criteria for SPCD actually existed as an independent diagnosis. First, we addressed the question of independence between SCI and RRB characteristics in family members with ASD, family members with structural language impairments and unaffected family members that will support or not support the diagnostic criteria of SPCD. Secondly, we looked at rates of SCI and RRB in unaffected family members, and then looked specifically at child family members (the diagnostic group for SPCD) to determine if SPCD is a necessary category and if BAP might well suffice as a diagnostic category since restricted and repetitive behaviors are included in the BAP profile. Finally, we explored the use of already available diagnostic measures to assess SPCD as its own entity or as part of the BAP.
METHODS
Subjects/Families
Subjects for this study were part of a larger family genetics study of autism and language impairment described above. Data on 535 family members are reported in this paper. Prior to behavioral testing, all subjects gave informed consent conforming to the guidelines for treatment of human subjects at Rutgers University. All subjects were tested with a comprehensive psycho-educational battery administered by an experienced psychometrician, speech language pathologist, or psychologist.
To be identified as the ASD subject in the larger study, the individual was required to meet the cut-off for ASD on at least two of the three following measures:
1) Autism Diagnostic Interview-Revised (ADI-R) (Lord et al., 1994), a structured caregiver interview with a cut-off algorithm for ASD diagnosis, 2) Autism Diagnostic Observation Schedule (ADOS, ADOS-2), a semi-structured assessment, and 3) Diagnostic and Statistical Manual-IV (American Psychiatric Association, 2000) and/or 5 (American Psychiatric Association, 2013).
To meet criteria for structural language impairment (LI), a family member had to receive a Core Score at least one standard deviation below on the age appropriate version of the Comprehensive Evaluation of Language Fundamentals (CELF-4) (Semel et al., 2003) or the Preschool CELF (Semel et al., 2004). For parents and adult siblings who were beyond the CELF-4 scoring range (21–11 years), the 17–0 to 21–11 standard scores were used. To further confirm LI affection status for out-of-age range subjects, a positive clinical history of language-based learning problems was required.
All other family members received the psycho-educational battery and questionnaires related to social behavior. See Bartlett et al. (2014) for a complete description of the diagnostic and psycho-educational batteries. Note that numbers of subjects for each measure varied based on age cut-offs for each measure and are reflected in the associations that follow. See Table 1 and Table 2.
Table 1.
Mean ages, age ranges, and test scores for family members with ASD.
| Male ASD | Female ASD | |
|---|---|---|
| Mean age 9.27 | Mean age 8.77 | |
| range 3–34.11) years | (range 3.02–36.07)years | |
| IQ | 91.12 (20.7) n=64 | 89.53 (19.95) n=15 |
| SCI-T | 75.37 (12.24) n=115 | 76.64 (10.11) n=22 |
| RRB-T | 78.06 (13.46) n=115 | 78.73 (14.97) n=22 |
| ADI-SI | 20.72 (6.88) n=137 | 19.85 (7.10) n=27 |
| ADI-RRB | 5.82 (2.54) n=137 | 5.41 (2.56) n=27 |
ASD: autism spectrum disorder; SCI-T: SRS-Social Communication Index T-score; RRB-T: SRS Restricted Interests and Repetitive Behavior; ADI-SI: Autism Diagnostic Interview Social Interaction; ADI-RRB: Autism Diagnostic Interview Restricted Interests and Repetitive Behaviors.
Table 2.
Mean age, age range, and test scores for unaffected family members and those with language impairment.
| Unaffected Fathers | Unaffected Mothers | Unaffected Brothers | Unaffected Sisters | Male LI | Female LI | |
|---|---|---|---|---|---|---|
| Mean age 44.85 | Mean age 41.62 | Mean age 11.94 | Mean age 13.11 | Mean age 18.76 | Mean age 16.37 | |
| [range 30–65.03] | [range 28–65.05] | [range 3.03–33.08] | [range 3.09–37.08] | [range 4.04–55] | [range 5.11–47.02] | |
| IQ | 113.46 (11.26) n=74 | 109.88 (12.15) n=100 | 107.36 (12.06) n=58 | 108.75 (11.28) n=44 | 94.88 (13.6) n=25 | 88 (10.34) n=15 |
| CELF | 112.21 (8.63) n=75 | 111.26 (8.62) n=104 | 104.82 (11.63) n=61 | 109.44 (10.72) n=43 | 74.43 (10.67) n=28 | 75.12 (9.42) n=16 |
| SCI-T | 46.42 (10.07) n=74 | 47.95 (9.35) n=92 | 47.77 (10.49) n=48 | 48.45 (9.51) n=38 | 56.06 (13.32) n=17 | 57.92 (14.9) n=13 |
| RRB-T | 47.57 (8.92) n=74 | 49.92 (9.13) n=92 | 50.65 (13.04) n=48 | 52.03 (14.1) n=38 | 57.65 (14.58) n=17 | 58.62 (17.56) n=13 |
| CASL NL | 99.57 (12.59) n=67 | 98.31 (11.79) n=100 | 102.81 (14.81) n=42 | 109.54 (12.92) n=35 | 81 (9.94) n=15 | 88.17 (20.41) n=12 |
| CASL PJ | 97.6 (9.18) n=70 | 97.9 (11.31) n=99 | 98.83 (11.84) n=59 | 105.43 (11.71) n=42 | 80.58 (15.93) n=24 | 84.53 (12.26) n=15 |
Variable Key: IQ= WASI Performance IQ or DAS Non-verbal Reasoning, SCI-T=SRS Social Communication Index T-Score, RRB-T= Restricted Interests and Repetitive Behaviors T-Score, CELF= CELF 4 or Preschool CELF, CASL NL= Comprehensive Assessment of Spoken Language Non-Literal Language, CASL PJ= Comprehensive Assessment of Spoken Language Pragmatic Judgment.
Materials
Social Responsiveness Scale (SRS-2)
As part of the psycho-educational battery referenced above, every family member received the Social Responsiveness Scale (SRS/SRS-2) (Constantino, 2005; Constantino, 2012). Parents completed the scale for their children and their spouses. The Social Responsiveness Scale (SRS-2) is a 65-item questionnaire of social impairment that has been rigorously tested in both children and adults. T-scores are available for an overall reciprocal social behavior and subscale behaviors (Social Awareness, Social Cognition, Social communication, Social Motivation, and Restricted and Repetitive Behaviors). T-scores between 60 and 75 denote a mild to moderate social impairment while anything over 75 is indicative of a severe social impairment. In this study, we considered a T-score 60 as performing in the clinical range of impairment.
A Social Communication Index (SCI), reported as a T-score, was also included to better reflect the social impairment characteristics of DSM-5 and includes all sub-scores noted above except restricted and repetitive behaviors. Since the focus of the current study is on the DSM-5 category of Social Pragmatic Communication Disorder, the SCI T-score best mirrors the social behaviors characterized in SPCD while the Restricted Interests and Repetitive Behaviors T- Score (RRB-T) best reflects the characteristics of RRBs. In all further analyses the SCI T-score will be referred to as SCI-T and the RRB-T score will be referred to as RRB-T.
Comprehensive Assessment of Spoken Language- CASL
Given that the communication characteristics of DSM-5 SPCD include higher order language skills including understanding what is not explicitly stated and nonliteral meanings of language, subtests from the Suprasegmental section of the Comprehensive Assessment of Spoken Language CASL (Carrow-Woolfolk, 1999) were administered to all family members who had enough language to receive the assessment. The Suprasegmental score specifically addresses abstract levels of spoken language. For this study we included two of the six suprasegmental subtests to address higher order language. Non-literal Language (CASL NL) measured understanding of spoken passages independent of literal interpretation and Pragmatic Judgement (CASL PJ) measured the use of appropriate language by presenting social situations that require appropriate verbal responses. For parents and adult siblings who were beyond the CASL scoring range (21–11 years), the 20–0 to 21–11 standard scores were used.
ADI-R Variables
For subjects with ASD, the diagnostic algorithm scores of Social Impairment (Section A) and Restricted and Repetitive Behaviors (Section C) were used to explore associations of these behaviors in subjects with ASD and compare them to the same constructs on the SRS. In all analyses the ADI Social Interaction score is referred to as ADI-SI and the ADI Restricted Interests and Repetitive Behaviors score is referred to as ADI-RRB.
The Wechsler Abbreviated Scale of Intelligence- (WASI PIQ) and the Developmental Abilities Scale (DAS IQ)
The Performance IQ scores of the WASI (Wechsler, 1999) and the Non-Verbal Reasoning sub-scales of the DAS (Elliott, 1990) were included, when available, to observe if non-linguistic cognitive abilities had any effect on associations related to social impairment, higher order language impairment, and the presence of restricted interests and repetitive behaviors.
Analysis
To assess the relationships among characteristics associated with ASD and SPCD, Pearson correlations were performed for ASD subjects, first- degree family members who met criteria for LI, and those who were unaffected for both ASD and LI using specific variables associated with social skills, restricted interests and repetitive behaviors, and higher order language skills. Results were focused on whether behaviors associated with social communication and restricted and repetitive behaviors could exist independently or if they were associated in affected and unaffected individuals.
Rates of clinical and subclinical performance on the SRS and the CASL were examined to determine if unaffected family members might meet criteria for BAP and whether, specifically, sibling family members might meet criteria for SPCD. Cognitive ability was co-varied with all measures to determine what role intellectual disability might play in the interaction of SCI and RRB.
RESULTS
Influence of cognitive level on measures of social communication impairment (SCI), restricted interests and repetitive behaviors (RRB), and higher order language abilities
We co-varied for IQ on correlations among measures for all ASDs, all LIs and all unaffected first-degree relatives. Levels of association and significance levels were comparable (almost identical) for all measures with and without co-varying for IQ. Thus, the remaining associations are presented with IQ included as a comparison association rather than as a co-vary.
Influence of sex on all measures
Before reporting associations, we ran t-tests on all measures to determine if there were sex differences on individual measures for ASD subjects, LI subjects, and all unaffected family members. Male and female ASD subjects did not differ on IQ or any ASD measures and thus, their correlations were analyzed as a group. There were no differences for any IQ, SRS or CASL measures for LI subjects based on sex, and thus their correlations were also analyzed as one group. For unaffected parents, there were no differences for any IQ, SRS, or CASL measures based on sex so their correlations were also analyzed together. For unaffected siblings, after accounting for multiple testing, Pragmatic Judgement of the CASL was significantly different between males and females so their subsequent correlational analyses were run separately.
Independence of social communication impairment (SCI) and restricted interests and repetitive behaviors (RRB) in ASD subjects
Bivariate correlations of all variables related to social impairment and restricted interests and repetitive behaviors in ASD revealed significant correlations for all four measures. Social behavior variables were positively and significantly correlated with both restricted and repetitive behavior variables (SCI-T/ RRB-T, r=.77, p<.001, SCI-T/ADI SI r=.47, p<.001, SCI-T/ADI RRB r=.34, p<.001, ADI-SI/ RRB-T r=.39 p<.001, ADI SI/ ADI RRB r=.32 p<.001). IQ was significantly and negatively correlated with both social measures and RRB-T but not ADI RRB (IQ/SCI-T, r=−.26, p<.05, IQ/ RRB-T r=.30, p<.05, IQ/ADI SI r=.40 p<.005). See Table 3.
Table 3.
Correlation tables of all measures used to determine the independence of social communication skills and restricted interests and repetitive behaviors.
| ALL ASD | ||||||
|---|---|---|---|---|---|---|
| IQ | SCI-T | RRB-T | ADI SI | ADI RRB |
||
| Mean (SD) | n=79 | n=137 | n=137 | n=164 | n=164 | |
| IQ | 90.82 (20.44) | 1 | ||||
| SCI-T | 75.58 (11.9) | −.264* | 1 | |||
| RRB-T | 78.17 (13.66) | −.298* | .774** | 1 | ||
| ADI SI | 20.58 (6.9) | −.395** | .472** | .386** | 1 | |
| ADI RRB | 5.76 (2.54) | −0.064 | .337** | .403** | .321** | 1 |
| ALL LI | ||||||
|---|---|---|---|---|---|---|
| IQ | SCI-T | RRB-T | CASL NL |
CASL PJ | ||
| Mean (SD) | n=40 | n=30 | n=30 | n=27 | n=39 | |
| IQ | 92.3 (12.79) | 1 | ||||
| SCI-T | 56.87 (13.80) | −0.085 | 1 | |||
| RRB-T | 58.07(15.66) | 0.059 | 0.828** | 1 | ||
| CASL NL | 84.19 (15.57) | 0.267 | −0.354 | −0.324 | 1 | |
| CASL PJ | 82.1 (14.59) | −0.01 | −0.263 | −0.302 | 0.603** | 1 |
| Unaffected Parents | ||||||
|---|---|---|---|---|---|---|
| IQ | SCI-T | RRB-T | CASL NL |
CASL PJ | ||
| Mean (SD) | n=190 | n=178 | n=178 | n=180 | n=182 | |
| IQ | 111 (11.83) | 1 | ||||
| SCI-T | 47.51 (10.27) | −0.117 | 1 | |||
| RRB-T | 49.22 (9.61) | −.150* | .829** | 1 | ||
| CASL NL | 97.91 (12.68) | .363** | −0.073 | −0.086 | 1 | |
| CASL PJ | 97.08 (10.68) | .293** | −.151* | −.160* | .547** | 1 |
| Unaffected Brothers | ||||||
|---|---|---|---|---|---|---|
| IQ | SCI-T | RRB-T | CASL NL |
CASL PJ | ||
| Mean (SD) | n=58 | n=48 | n=48 | n=42 | n=59 | |
| IQ | 107.36 (12.06) | 1 | ||||
| SCI-T | 47.77 (10.49) | −0.189 | 1 | |||
| RRB-T | 50.65 (13.04) | −0.023 | .826** | 1 | ||
| CASL NL | 102.81 (14.81) | .348* | −0.034 | 0.078 | 1 | |
| CASL PJ | 98.83 (11.84) | .323* | −0.208 | −0.036 | .657** | 1 |
| Unaffected Sisters | ||||||
|---|---|---|---|---|---|---|
| IQ | SCI-T | RRB-T | CASL NL |
CASL PJ | ||
| Mean (SD) | n=44 | n=38 | n=38 | n=35 | n=42 | |
| IQ | 108.75 (11.28) | 1 | ||||
| SCI-T | 48.45 (9.51) | 0.028 | 1 | |||
| RRB-T | 52.03 (14.10) | −0.044 | .851** | 1 | ||
| CASL NL | 109.54 (12.92) | .386* | −.361* | −0.326 | 1 | |
| CASL PJ | 105.43 (11.71) | 0.242 | −0.209 | −0.2 | .588** | 1 |
Correlation is significant at the 0.05 level (2-tailed).
Correlation is significant at the 0.01 level (2-tailed).
Variable Key: IQ= WASI Performance IQ or DAS Non-verbal Reasoning, SCI-T=SRS Social Communication Index T-Score, SRS RRB= Restricted Interests and Repetitive Behaviors T-Score, ADI SI= Autism Diagnostic Interview Social Interaction, ADI RRB Autism Diagnostic Interview Restricted Interests and Repetitive Behaviors, CASL NL= Comprehensive Assessment of Spoken Language Non-literal Language, CASL PJ= Comprehensive Assessment of Spoken Language Pragmatic Judgment.
Independence of social communication Impairment (SCI) and restricted interests and repetitive behaviors (RRB) in nuclear family members meeting criteria for LI
For LI family members, social communication and restricted and repetitive behaviors of the SRS were significantly and positively correlated (SCI-T/RRB-T r=.83, p<.001) but neither was correlated with any other measures of IQ or higher order language/pragmatic skills. Likewise, both CASL scores were significantly and positively correlated (r=.60, p<.01) but not significantly correlated with IQ or any SRS measures. See Table 3.
Independence of social communication impairment (SCI) and restricted interests and repetitive behaviors (RRB) in unaffected nuclear family members
Parents
For unaffected parents of ASD subjects SCI-T and RRB-T were, again, positively and significantly correlated (r=.83, p<.001). RRB-T also had a significant negative correlation with CASL PJ (r=−.16, p < .05) as did SCI-T (r= −.15, p=.05). Higher order language tasks (CASL PJ and CASL NL) had a positive significant correlation (r=.55, p <.001). Finally, IQ was positively and significantly correlated with both CASL higher order tasks (IQ/CASL NL, r=.36 p<.001 and IQ/ CASL PJ, r=.29, p<.001) and had a significant negative correlation with RRB-T (r=−.15, p<.05). See Table 3.
Siblings
For unaffected brothers of ASD subjects SCI-T and RRB-T were positively and significantly correlated (SCI-T/RRB-T r=.83, p<.001), and both higher order language tasks were significantly and positively correlated with each other but not with either SRS measure (CASL IN/CASL PJ, r=.66 p<.001). IQ was significantly and positively correlated with both higher order language tasks but not with either SRS measure (IQ/CASL NL, r=.35, p<.05, IQ/CASL PJ r=.32, p<.05). For unaffected sisters of ASD subjects, SCI-T and RRB-T were positively and significantly correlated (SCI-T/ RRB-T r=.85, p<.001). SCI-T was significantly and negatively correlated with CASL NL (SCI-T/CASL NL, r=−.36, p=.05) but not with CASL PJ. Both CASL measures were significantly correlated with each other (CASL NL/ CASL PJ, r=.59, p<.001) and CASL NL was significantly correlated with IQ (CASL NL/IQ, r=.39, p<.05). See Table 3.
Rates of social communication impairment (SCI) and of restricted interests and repetitive behaviors (RRB) in all family members.
We examined rates of clinically significant SCI-T and RRB-T scores reported in all family members with and without ASD. Participants with T-scores 60 on SRS SCI or SRS RRB were deemed “affected”. There were no sex differences in LI subjects, unaffected parents, or unaffected siblings. Figure 1 demonstrates these rates of impairment based on all ASD, all LI, and all unaffected parents and siblings.
Figure 1.
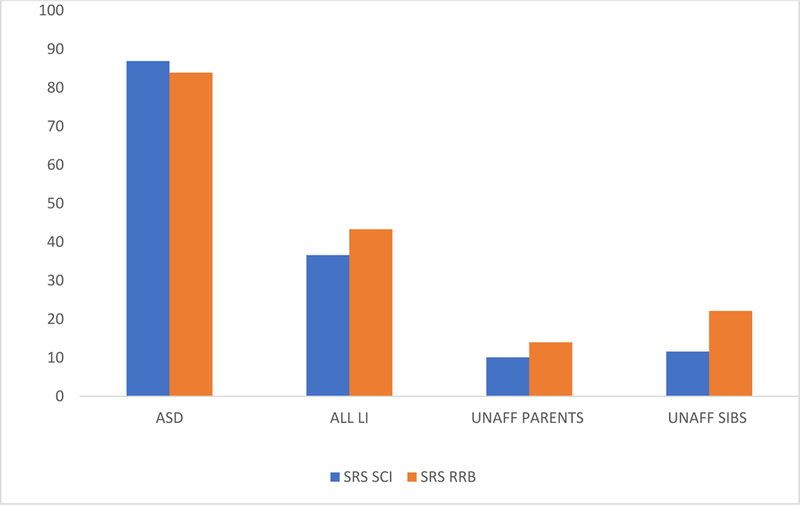
Percentage with Social Communication Impairment and/or Restricted Interests and Repetitive Behaviors Based on SRS T-Scores.
By definition, rates of impairment for ASD subjects using the SCI-T and RRB-T scores were higher than any other family members (SCI-T=86.9% and RRB-T=83.9%). However, the rates of impairment for family members meeting criteria for LI were also high. More than one third of family members who were classified as LI met criteria for at least a social impairment (36.6%) and almost one-half showed some degree of restricted interests and repetitive behaviors (43.3%). There was a small percentage of unaffected parents who also presented with scores 60 on the SRS (SCI-T= 10.1%, RRB-T= 14.0%). Rates for unaffected siblings were higher with SCI-T scores 60 at 11.6% and rates of RRB-T at 22.1%.
Using the SRS and CASL to identify Social Pragmatic Communication Disorder (SPCD)
One of the hypotheses was to examine whether current assessments of social behavior and higher order language were useful in diagnosing SPCD. We looked at affection rates based on SRS and CASL scores to see how many siblings, under the age of 19, who did not have LI or ASD, might meet the DSM-5 SPCD diagnosis-social communication impairment with no clinical evidence of restricted interests and repetitive behaviors (RRB-T60).
Table 4 shows the number of unaffected (for ASD and LI) siblings under the age of 19 and their SRS and CASL affection status based on the cutoffs designed for this study, SCI-T 60 and RRB-T < 60 or CASL subtest 85 and RRB-T<60. Row A shows that 58/78 (74.4%) were unaffected based on the SRS criteria while only one sibling (1.2%) met the SPCD criteria. However, there were nine siblings (11.5%) who met the SCI-T criteria as well as the RRB-T criteria. Yet, these children did not meet traditional ASD criteria. In Row B we looked at a combination of CASL subtest scores (as a proxy for SPCD/social impairment) and the RRB-T scores. Based on these criteria, 56/78 (72%) were unaffected. There were 3/78 (3.8%) who received a score on either CASL subtest 85 (impaired range) with RRB-T scores 60. Row C shows what happened if we accepted an affected status for social impairment using either the SCI-T score or a CASL suprasegmental score. Using this scenario, we captured 13/78 (16.7%) with a social score in the affected range but of the 13, only four (5.1%) had RRB-T scores < 60 while 9 had affected social scores and high RRB-T scores (11.5%).
Table 4.
Affection status based on assessments of social communication and restricted interests and repetitive behaviors of unaffected siblings under the age of 19.
| 78 siblings without ASD or LI |
SRS RRB-T | |||
|---|---|---|---|---|
| SRS | <60 | ≥60 | ||
| A | SCI-T <60 | 68 | 58 | 10 |
| SCI-T ≥60 | 10 | 1 | 9 | |
| CASL | ||||
| Both CASL NL and PJ >85 | 75 | 56 | 19 | |
| B | Either CASL NL or PJ <85 | 3 | 3 | 0 |
| SRS and CASL | ||||
| Neither SCI-T >60 nor a CASL <85 | 65 | 55 | 10 | |
| C | Either SCI-T >60 or a CASL <85 | 13 | 4 | 9 |
| Both SCI-T and a CASL impaired | 0 | 0 | 0 | |
DISCUSSION
Our primary aim was to determine if using the DSM-5 diagnosis of SPCD was practical in a clinical setting and valuable for a research setting. Related to this was the question of whether the current description of the Broad Autism Phenotype (BAP) might work just as well or better in diagnosing children who meet the SPCD criteria. We approached this by examining the independence of the variables involved in the diagnosis: evidence of social communication issues (including higher order language skills) without structural language impairment and no clinical levels of restricted interests and repetitive behaviors. Our family sample was an ideal cohort to study this question since it included subjects on the autism spectrum, subjects with structural language impairment, and unaffected individuals without ASD or language impairment. Results from all three groups did not support the concept of independence of social communication impairment and independence of SCI and RRBs. The SCI-T and RRB-T variables were significantly correlated for all groups as well as the SC and RRB scores of the ADI-R for the ASD group.
There has been considerable discussion related to the question of ASD symptomology being fractionable, meaning that behaviors associated with ASD could be viewed as independent. In a review of their own twin samples and other samples, Happe’ and Roland (2008) suggested that the characteristics of ASD are independent and thus, 1) useful for molecular genetics studies in defining the phenotype/genotype relationship and 2) helpful on the cognitive level for diagnosis in the clinical setting. This conclusion was reached based on DSM-IV criteria when there were three categories for a diagnosis of ASD: social interaction, communication, and restricted interests and repetitive behaviors. However, in a review of current research, Visser and Tops (2017) suggested that the characteristics of ASD fell on a continuum rather than as distinct and separable diagnosed behaviors. Moreover, Murray et al. (2014) studied social and behavioral characteristics of ASD in affected individuals as well as unaffected individuals and suggested that those who have used only clinical samples may have underestimated the extent of how symptoms of social impairment and restricted interests and repetitive behaviors are associated. Our study had the advantage of having unaffected family members receiving the same measures as those diagnosed with ASD and LI.
We examined the rates of SCI-T and RRB-T in the three groups. Not surprisingly, the rates for ASD family members were quite high as they should have been by definition. However, rates for family members who met criteria for LI were especially interesting. Over one-third (36.6%) of family members who met criteria for LI also met the SCI-T criteria of at least mild to moderate impairment in social communication and almost half (43.3%) of those with LI had at least an RRB-T score in the mild to moderate range. These rates demonstrated the difficulties when attempting to separate structural language impairment from social communication impairment. If individuals had difficulties expressing their needs and ideas at the structural language level, it followed that social communication issues could become impacted. Like Ash et al. (2017), we were not able to disambiguate the differences in characteristics associated with structural language impairment and those characteristics associated with SPCD to create an isolated diagnosis such as required with SPCD. When combined with the lack of independence of social impairment and restricted interests and repetitive behaviors, the utility and complexities of the diagnosis of SPCD became questionable.
We examined the profiles of our unaffected subjects under the age of 19 to see if we could identify any as meeting a profile of SPCD, scoring clinically significant impairment in social communication (SCI) yet not having clinically significant RRB. We found that almost all children who scored in the mild to moderate range of impairment on the SRS Social Communication Impairment (SCI-T) also scored in the same range on the restricted interests and repetitive behavior scale (RRB-T), again, supporting the idea that the two constructs were not independent. Only one child in our sample scored in the impaired range for SCI-T and not RRB-T. Since there are no current assessments other than DSM-5 to diagnose SPCD, we explored whether the CASL Supralinguistic subtests (Non-literal Language and/or Pragmatic Judgement) might be another approach to confirm the diagnosis of SPCD when a child presented with abstract language difficulties. When we used either one of the subtest scores as a proxy for a characteristic of a social impairment, there were only three siblings under the age of 19 who scored in the impaired range (standard scores 85) and still received an RRB-T score less than 60 (4%). At the same time, we identified nine siblings (11.5%) who had high levels of SPCD behaviors as well as high levels of RRB and yet, did not have an ASD diagnosis. To this point, Mandy et al., (2017) looked at a large sample of children who were receiving clinical services for social communication issues while considered to have fluent language and an IQ within the normal range, a profile of children who should fit comfortably into the DSM-5 criteria of SPCD. However, of the 1,081children receiving this type of intervention, only 88 (8.1%) met the official SPCD criteria.
One issue we raised in the introduction was the utility of the diagnosis of SPCD, especially since the features of the Broad Autism Phenotype included the behaviors associated with SPCD. Researchers have been examining the “soft” characteristics of ASD in both children and adults without a diagnosis of ASD since the early 2000s. Social behavior, language impairments, restricted interests and repetitive behaviors are all included in its definition and there are assessments specifically designed to pick up irregularities and differences in these behaviors for all ages. Studies such as Ash et al. (2017), Mandy et al. (2017) and Visser and Tops (2017) have reported difficulty in separating the symptoms of SPCD from other communication and social emotional disorders, describing SPCD as lying on the “borderlands” of ASD but not meeting any of the expected thresholds. The BAP could be a reasonable alternative that would help these children receive the services that they need, either for communication or behavior issues. While the BAP has been used extensively in the research world, it is, unfortunately, not a currently recognized diagnostic category in the clinical or educational worlds, and so, as of now, would not be helpful in securing appropriate clinical services and support. We identified 10 children who met the 60 RRB-T cut-off and had only minimally lower scores for SCI-T levels of social impairment. Using SPCD criteria, they did not qualify under the SPCD diagnosis, nor did they meet criteria for ASD. For lack of a legitimate diagnosis these children would not be eligible for intervention services.
As opposed to many other studies, we did not find sex differences in ASD subjects and parents on any measures of social impairment, IQ, or higher order language measures from the CASL. Unaffected siblings were significantly different on only the CASL measures. Given that our sample was relatively small and the male-female ratio was large, we may not have been able to capture the types of sex differences reported by Ash et al., (2017) or Klusek et al., (2014).
Limitations
We understand that these results may not be representative of population studies of SPCD as there was no control group. This cohort was part of a larger genetic family study of ASD and as such was a convenience sample, but it allowed us to look specifically at ASD, LI, and SPCD where all subjects received the same battery of assessments that address the characteristics of SPCD. We acknowledge that the individual rates of SCI and RRB may be higher for LI and the unaffected family group than in a control sample since there is a family history of ASD, but even in this sample there were only four children who met potential SPCD criteria when one would assume that the rate would be higher given the family history component. If we had designed a study specifically to assess the utility of the diagnosis of SPCD, we would have used more detailed child-centered assessment of social communication and behavior such as the Children’s Communicative Checklist (CCC-2). The SRS-2 has normative data on both children and adults making it a reasonable initial attempt at untangling the interactions of social behaviors and restricted interests and repetitive behaviors.
Unlike the many cognitive, processing, and reading assessments that have been normed through late adulthood, there are limited assessments to diagnose language impairments in adults. This has been a recurrent issue for speech and language researchers for the past 20 years (Barry et al., 2007). We confirmed our language impairment diagnosis by using a combination of the highest scoring range on the CELF-4 and a significant developmental history of language and reading problems.
Conclusion
The utility and accuracy of the SPCD diagnosis is still unclear. These questions still remain: how well are we doing in diagnosing SPCD? Are we accommodating children who do not fit neatly into a diagnosis of ASD, language impairment or SPCD? If a child doesn’t meet gold standard criteria for ASD yet shows clear social communication impairment with or without structural language impairment with elements of RRB, are they receiving clinical services? There are at least two areas that require further action: 1) larger scale studies in school systems and clinical facilities allowing us to better understand if children are actually being diagnosed with SPCD and 2) reliable and easy to administer assessments specifically designed to address levels of restricted interest and flexibility in relation to levels of social communication issues in children. Perhaps, adopting a mindset that SPCD is more akin to the BAP rather than a diagnosis completely separate from ASD would help bridge these gaps.
Acknowledgements
Our very sincere thanks to our study families whose interest in ASD research has motivated them to participate in hours of evaluation to support our research. A special thanks to all the many professionals and research aides who administered and checked our testing battery. We are thankful to our funders: NIMH Grants # R01 MH70366 and #RC1 MH088288 and the New Jersey Governor’s Council for Medical Research and Treatment of Autism CAUT12APS006, CAU15APL026.
In addition to NIH funding the manuscript received funding from the New Jersey Governor's Council for Medical Research and Treatment of Autism #CAUT12APS006 and CAU15APL026.
NIH Grants # R01 MH70366 and #RC1 MH088288
Contributor Information
Judy Flax, Department of Genetics, Rutgers University
Christine Gwin, Department of Genetics, Rutgers University
Sherri Wilson, Department of Genetics, Rutgers University
Yuli Fradkin, Rutgers University Behavioral Health Care, Rutgers University
Steve Buyske, Department of Statistics and Biostatistics, Rutgers University
Linda Brzustowicz, Department of Genetics, Rutgers University
References
- American Psychiatric Association; (2000) Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC. [Google Scholar]
- American Psychiatric Association. (2013) Diagnostic and Statistical Manual of Mental Disorders 5th Edition Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Ash AC, Redmond SM, Timler GR, et al. (2017) The influence of scale structure and sex on parental reports of children’s social (pragmatic) communication symptoms. Clinical Linguistics & Phonetics 31: 293–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey A, Palferman S, Heavey L, et al. (1998) Autism: the phenotype in relatives. J Autism Dev Disord 28: 369–392. [DOI] [PubMed] [Google Scholar]
- Baron-Cohen S, Wheelwright S, Skinner R, et al. (2001) The Autism-Spectrum Quotient (AQ): Evidence from Asperger Syndrome/High-Functioning Autism, Malesand Females, Scientists and Mathematicians. Journal of Autism and Developmental Disorders 31: 5–17. [DOI] [PubMed] [Google Scholar]
- Barry JG, Yasin I and Bishop DV. (2007) Heritable risk factors associated with language impairments. Genes Brain Behav 6: 66–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartlett CW, Liping Hou, Flax Judy F., et al. (2014) A Genome Scan for Loci Shared by Autism Spectrum Disorder and Language Impairment. American Journal of Psychiatry 171: 72–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop DVM. (1998) Development of the Children’s Communication Checklist (CCC): A Method for Assessing Qualitative Aspects of Communicative Impairment in Children. The Journal of Child Psychology and Psychiatry and Allied Disciplines 39: 879–891. [PubMed] [Google Scholar]
- Bishop DVM. (2003) Children’s Communication Checklist-2. London: Psychological Corporation. [Google Scholar]
- Brukner-Wertman Y, Laor N and Golan O. (2016) Social (Pragmatic) Communication Disorder and Its Relation to the Autism Spectrum: Dilemmas Arising From the DSM-5 Classification. Journal of Autism and Developmental Disorders 46: 2821–2829. [DOI] [PubMed] [Google Scholar]
- Buxbaum JD. (2015) DSM-5 and Psychiatric Genetics — Round Hole, Meet Square Peg. Biological Psychiatry 77: 766–768. [DOI] [PubMed] [Google Scholar]
- Carrow-Woolfolk E (1999) Comprehensive Assessment of Spoken Language. Bloomington, MN: Pearson Assessments. [Google Scholar]
- Constantino JN. (2005) Social Responsiveness Scale (SRS). In: Gruber CP (ed). Los Angeles, CA: Western Psychological Services. [Google Scholar]
- Constantino JN. (2012) The Social Responsiveness Scale™, Second Edition (SRS™−2). In: CP G (ed). Los Angeles, CA: Western Psychological Services. [Google Scholar]
- Constantino JN, Gruber CP, Davis S, et al. (2004) The factor structure of autistic traits. Journal of Child Psychology and Psychiatry 45: 719–726. [DOI] [PubMed] [Google Scholar]
- Dawson G, Estes A, Munson J, et al. (2007) Quantitative Assessment of Autism Symptom-related Traits in Probands and Parents: Broader Phenotype Autism Symptom Scale. Journal of Autism and Developmental Disorders 37: 523–536. [DOI] [PubMed] [Google Scholar]
- Elliott CD. (1990) Differential Ability Scales. San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Fombonne E, Bolton P, Prior J, et al. (1997) A family study of autism: cognitive patterns and levels in parents and siblings. J Child Psychol Psychiatry 38: 667–683. [DOI] [PubMed] [Google Scholar]
- Gandal MJ, Haney JR, Parikshak NN, et al. (2018) Shared molecular neuropathology across major psychiatric disorders parallels polygenic overlap. Science 359: 693–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halladay AK, Bishop S, Constantino JN, et al. (2015) Sex and gender differences in autism spectrum disorder: summarizing evidence gaps and identifying emerging areas of priority. Molecular Autism 6: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Happé F and Ronald A. (2008) The ‘Fractionable Autism Triad’: A Review of Evidence from Behavioural, Genetic, Cognitive and Neural Research. Neuropsychology Review 18: 287–304. [DOI] [PubMed] [Google Scholar]
- Hurley RSE, Losh M, Parlier M, et al. (2007) The Broad Autism Phenotype Questionnaire. Journal of Autism and Developmental Disorders 37: 1679–1690. [DOI] [PubMed] [Google Scholar]
- Klusek J, Losh M and Martin GE. (2014) Sex differences and within-family associations in the broad autism phenotype. Autism 18: 106–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landa R, Piven J, Wzorek MM, et al. (1992) Social language use in parents of autistic individuals. Psychol Med 22: 245–254. [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore PC, et al. (2012) Autism Diagnostic Observation Schedule, second edition (ADOS-2). Manual. Torrane, CA: Western Psychological Services. [Google Scholar]
- Lord C, Rutter M and Le Couteur A. (1994) Autism Diagnostic Interview-Revised: a revised version of a diagnostic scale for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders 24: 659–685. [DOI] [PubMed] [Google Scholar]
- Losh M and Piven J. (2007) Social-cognition and the broad autism phenotype: identifying genetically meaningful phenotypes. J Child Psychol Psychiatry 48: 105–112. [DOI] [PubMed] [Google Scholar]
- Mandy W, Wang A, Lee I, et al. (2017) Evaluating social (pragmatic) communication disorder. J Child Psychol Psychiatry 58: 1166–1175. [DOI] [PubMed] [Google Scholar]
- Micali N, Chakrabarti S and Fombonne E. (2004) The broad autism phenotype: findings from an epidemiological survey. Autism 8: 21–37. [DOI] [PubMed] [Google Scholar]
- Murray AL, McKenzie K, Kuenssberg R, et al. (2014) Are we under-estimating the association between autism symptoms?: The importance of considering simultaneous selection when using samples of individuals who meet diagnostic criteria for an autism spectrum disorder. J Autism Dev Disord 44: 2921–2930. [DOI] [PubMed] [Google Scholar]
- Norbury CF. (2014) Practitioner Review: Social (pragmatic) communication disorder conceptualization, evidence and clinical implications. Journal of Child Psychology and Psychiatry 55: 204–216. [DOI] [PubMed] [Google Scholar]
- Norbury CF, Nash M, Baird G, et al. (2004) Using a parental checklist to identify diagnostic groups in children with communication impairment: a validation of the Children’s Communication Checklist—2. International Journal of Language & Communication Disorders 39: 345–364. [DOI] [PubMed] [Google Scholar]
- Piven J (1997) Broader autism phenotype: evidence from a family history study of multiple-incidence autism families. American Journal of Psychiatry 154: 185–190. [DOI] [PubMed] [Google Scholar]
- Semel E, Wiig E and Secord W. (2003) Clinical Evaluation of Language Fundamentals, Fourth Edition (CELF-4). Toronto: The Psychological Corporation/A Harcourt Assessment Company. [Google Scholar]
- Semel E, Wiig E and Secord W. (2004) Clinical Evaluation of Language Fundamentals – Preschool – Second Edition (CELF-P 2). [Google Scholar]
- Swineford LB, Thurm A, Baird G, et al. (2014) Social (pragmatic) communication disorder: a research review of this new DSM-5 diagnostic category. Journal of Neurodevelopmental Disorders 6: 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visser S, Tops W (2017) Social Pragmatic Communication Disorder and Autism Spectrum Disorder: Two of a Kind? A Narrative Review Ann Psychiatry Ment Health 5. [Google Scholar]
- Wechsler D (1999) Wechsler Abbreviated Scale of Intelligence WASI: Manual: Pearson/PsychCorpl. [Google Scholar]


