Abstract
Background Despite the high prevalence of unstable distal radius fractures (DRFs), there is no consensus regarding the optimal method and treatment timing, especially for elderly patients with multiple associated injuries.
Purpose This study aimed to compare the grip strength achieved with two different methods for definitive dynamic external fixation of DRFs in elderly patients with polytrauma operated on within the first 24 hours.
Methods In this prospective randomized trial, 35 patients were assigned to undergo definitive external dynamic fixation of DRFs using the nonbridging (group A) or bridging (group B) method. The grip strength, range of motion (ROM), Disabilities of the Arm, Shoulder and Hand (QuickDASH) outcome measure, visual analog scale (VAS) score for pain, and radiographic characteristics were evaluated at 6 and 12 months.
Results At 12 months, no significant between-group difference was observed with respect to grip strength. All patients showed results in the third or fourth quartiles. The mean ROMs were 96.94 and 96.38% and the mean QuickDASH scores were 3.53 and 3.85 in groups A and B, respectively. The VAS scores were 1.60 and 1.85 in groups A and B, respectively. The overall complication rates were 13.3 and 15% in groups A and B, respectively. Initial fracture reduction was maintained in 86.67 and 95% of the patients in groups A and B, respectively.
Conclusions Both bridging and nonbridging external definitive dynamic fixation proved safe and reliable for the treatment of unstable DRFs in elderly patients with polytrauma. The grip strength results in both groups predicted the restoration of ability in elderly patients to perform activities of daily living independently.
Keywords: distal radius fracture, elderly, multiple trauma, closed fracture reduction, external fixators, randomized trial
Despite the high prevalence of unstable distal radius fractures (DRFs), there is still no consensus regarding the preferred method and ideal timing of treatment, especially in elderly patients with multiple injuries 1 2 in whom the treatment timing can have a strong psychological impact. 3 4 The use of dynamic external fixation as a definitive treatment for unstable DRFs in elderly patients with polytrauma within the first 24 hours may be a good strategy under the paradigm of early total care (ETC). This approach is convenient, fast, and safe and employs a minimally invasive and reproducible method that avoids the inflammatory systemic response to trauma, enables early functional recovery, and shortens the hospitalization time of these patients. The primary goal of this study was to compare the postoperative grip strength of elderly patients with polytrauma with unstable DRFs treated with dynamic external fixation using bridging and nonbridging methods. The secondary objective was to compare the clinical outcomes including patient-reported and radiographic outcomes.
Patients and Methods
A single-center, parallel group, prospective, randomized clinical trial was conducted at the Department of Hand Surgery, Faculdade de Medicina do ABC University Hospital, Santo Andre, Brazil. The following two implants used for fixation after the closed reduction of DRFs were compared: the bridging dynamic Galaxy Wrist external fixator (Orthofix, Verona, Italy) and the nonbridging Galaxy Wrist external fixator system (Orthofix). The protocol was approved by the institutional research ethics committee (no. ETIK 805.909). Written informed consent was obtained from all patients prior to their enrolment. The inclusion criterion was elderly patient (aged ≥60) with a diagnosis of unstable DRF (AO type A or C) associated with multiple injuries (polytrauma) who were treated within the first 24 hours. The exclusion criteria were injuries of the ipsilateral limb, ongoing chemotherapy or radiotherapy, and patients with mental illnesses or alcohol abuse. This trial was registered at the ClinicalTrials.gov Web site (ID no. 32925713.9.0000.0082).
Sample Size Calculation
Based on the results of a previous study in which external fixation was compared with closed treatment using a bone substitute, 5 grip strength was chosen as the primary outcome parameter and used to estimate the required sample size. A minimum of 17 patients were required in each group to show a 20% difference in grip strength (20 N; standard deviation: 19), with a statistical power of 85% in a two-sided test at a 5% significance level.
During the study period (from June 2015 to June 2017), a total of 45 patients met the patient selection criteria ( Fig. 1 ; Consolidated Standards of Reporting Trials). 6 Five eligible patients were operated on by orthopedic surgeons who did not participate in the study and were not included. Another five patients were operated on after the first 24 hours. Posthoc analysis showed that 35 of the patients included in the study did not show differences with respect to age, gender, or fracture type compared with the 10 eligible but not randomized patients. Of the patients, 24 were women and 11 were men. The average age of the patients was 65 years (range: 60–73). The fractures were classified according to the AO classification system. 7
Fig. 1.
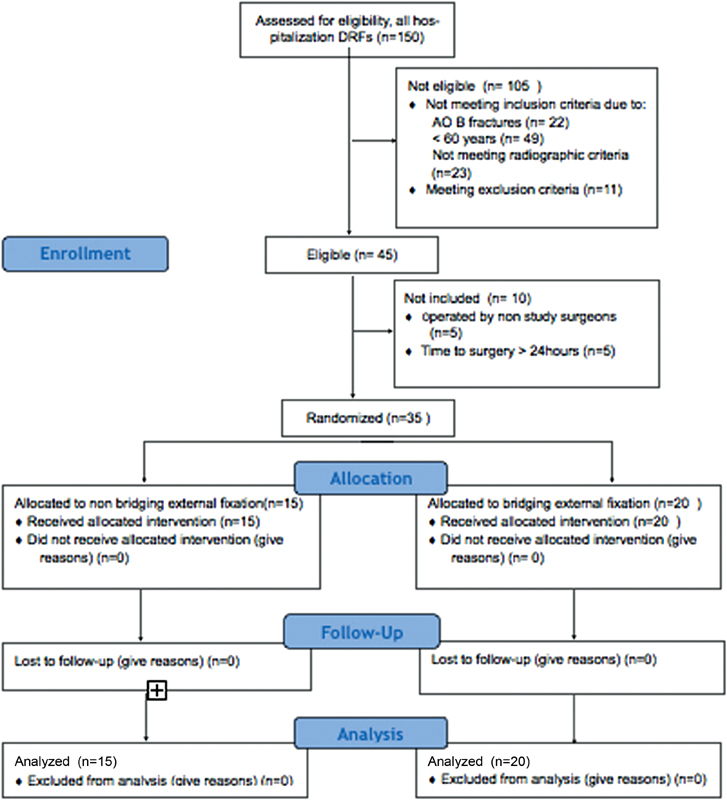
Consolidated Standards of Reporting Trial (CONSORT) flowchart. DRF, distal radius fracture.
The patients were randomized by drawing currency lots (face = group A, treatment with nonbridging fixation; crown = group B, treatment with bridging fixation). The currency lots were placed in 50 sealed envelopes prior to the start of the study. All examiners were blinded to the randomization. Simple randomization was used, and the envelopes were opened in the operating room immediately prior to the surgery. The surgical instruments for both procedures were available in a single box. Twenty patients were randomized to the bridging group and 15 patients to the nonbridging group. The groups were similar. All randomized patients were available for the intention-to-treat analysis at the 6- and 12-month follow-up.
Surgical Technique
All patients underwent surgery under general anesthesia. The surgical method of treatment was closed fracture reduction (achieved with longitudinal traction associated with a volar translation maneuver) and stabilization with two or three Kirschner (K-wires) (Rayhack, Stahl, De Palma methods) followed by augmentation with an external fixator and four pins (Schantz) specific to the hilt. In both groups, the two pins were positioned proximally to the fracture, the dorsal lateral shaft region of the radius bone. The difference was with respect to the positioning of the two pins at the distal segment ( Figs. 2 3 4 5 ).
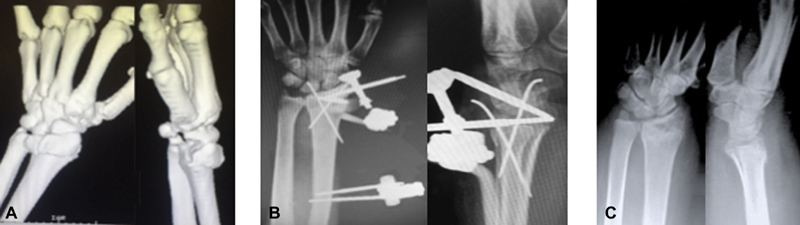
Fig. 2.

Radiographic aspects. ( A ) Preoperative. ( B ) Postoperative. ( C ) After 12 months, bridging group: left side.
Fig. 3.

Clinical aspects. After 12 months, bridging group: left side.
Fig. 4.
Radiographic aspects. ( A ) Computed tomography (CT) preoperative. ( B ) Postoperative. ( C ) After 12 months, nonbridging group: left side.
Fig. 5.
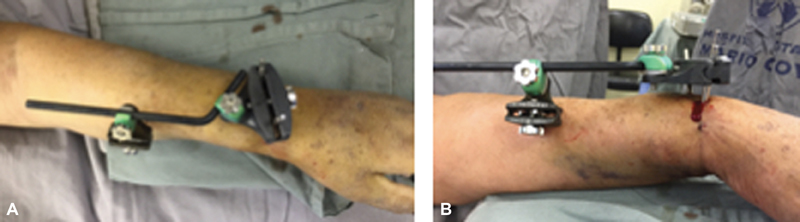
Clinical intraoperative aspects. ( A ) posteroanterior view. ( B ) Lateral view, nonbridging group: left side.
In group A (the nonbridging group), the pins were inserted into the metaepiphyseal dorsolateral part of the radius bone. In group B (the bridging group), the pins were fixed in the proximal and dorsolateral region of the second metacarpal bone. The correct placement of pins stabilizes the fracture together with the external fixator assembly. All patients were assessed radiographically and clinically at 1, 2, and 8 weeks and at 6 and 12 months.
The grip strength was measured at 6 and 12 months with a Jamar Hand Dynamometer (Sammons Preston, Bolingbrook, IL), as recommended by the American Society of Hand Therapists, 8 9 after fracture healing (defined as callus formation in both posteroanterior [PA] and lateral views, and painless at the fracture site). The mean value was calculated from three attempts and expressed as an absolute value and as a percentage of the value at the contralateral uninjured side. 10
The patients were classified into four groups (1, 2, 3, 4) according to the quartiles ( Table 1 ) and according to their inability to perform activities of daily living (ADLs). The wrist's range of motion (ROM) was evaluated using a standard goniometer. The patient-reported outcomes were recorded using the Disabilities of the Arm, Shoulder and Hand (QuickDASH) questionnaire (scale: 0–100, where 0 indicates the best result) 11 12 and the visual analog scale (VAS) score for pain (scale: 0–10, where 0 indicates no pain). Complications were assessed at 6 and 12 months.
Table 1. Hazard ratio analysis predicting 7-year incidence of any ADL limitation form.
| Hand grip strength quartiles | Men, HR 95% CI, N = 979 | Women, HR 95% CI, N = 1,310 |
|---|---|---|
| 1st: Men (<22 kg) women (<14 kg) | 1.90 (1.14–3.17) | 2.28 (1.59–3.27) |
| 2nd: Men (22.01–30 kg) women (14.01–18.20 kg) | 1.83 (1.12–2.98) | 1.72 (1.21–2.45 |
| 3rd: Men (30.01–35 kg) women (18.21–22.50 kg) | 1.25 (0.75–2.11) | 1.41 (1.00–2.02) |
| 4th: Men (>35.01 kg) women (>22.51 kg) | 1.00 | 1.00 |
Abbreviations: ADL, activities of daily living; CI, confidence interval; HR, hazard ratio.
Radiographic parameters were evaluated immediately after surgery and at 2 weeks, 8 weeks, 6 months, and 12 months after surgery. Radial shortening was measured as ulnar variance from the distal radial surface to the distal ulnar surface, as assessed using the PA radiographs of the wrist obtained in a neutral position. Volar tilt was measured on the lateral view and expressed as the angle of joint surface relative to the radial axis. The implants (external fixator, pins, and K-wires) were removed after fracture healing (defined as osseous bridging across the fracture site on both PA and lateral views) with the use of local block anesthesia in an ambulatory setting. The mean of fixation period of the implants was 6.94 weeks, whereas that in the nonbridging and bridging groups was 7 and 6.9, respectively
After surgery, early mobilization for the upper limb was employed: nonbridging group was free movement and bridging group patients placed ex fix as if were dynamic wrist bracing, thus allowing complete wrist flexion–extension or restriction of the last 20 degrees, if necessary. The first dressing change occurred 7 days postoperatively. On the same day, the patient was referred to the rehabilitation sector. Daily sessions of rehabilitation lasted for about 3 months, and then the patient could be allowed to start physical activities.
Statistical Methods
Data are presented as mean or median according to the type of variable and distribution. Between-group differences with respect to parametric variables were assessed using the Mann–Whitney U test, and p < 0.05 was considered indicative of a statistically significant difference. The Statistical Package for the Social Sciences (SPSS) version 23.0 (SPSS Inc.) was used for data analyses.
Results
The baseline demographic characteristics and injury details are presented in Table 2 . At the 12-month follow-up, no significant between-group difference was observed with respect to the mean grip strength. The mean grip strength of the affected wrist of men in the bridging group was 80.78% of the normal side versus 85.33% of the normal side in the nonbridging group distributed in four groups (both corresponding the third quartiles). The corresponding grip strength of women was 90.12 and 89.09% of the normal side, respectively, (both in the third quartiles) ( Table 3 ).
Table 2. Demographic characteristics and injury details.
| Nonbridging ( n = 15) | Bridging ( n = 20) | |
|---|---|---|
| Age (years) a | 65 (60–73) | 64 (60–68) |
| Gender b | ||
| Female | 11 (73) | 13 (65) |
| Male | 4 (27) | 7 (35) |
| Hand dominance | ||
| Right | 13 (87) | 10 (50) |
| Left | 2 (13) | 10 (50) |
| Dominant extremity fractured | 5 (33) | 11 (55) |
| AO classification | ||
| A3 | 6 (40) | 8 (40) |
| C1 | 4 (27) | 5 (25) |
| C2 | 2 (13) | 5 (25) |
| C3 | 3 (20) | 2 (10) |
| Preoperative radiograph displacement | ||
| Volar tilt > 20 degrees | 10 (67) | 13 (65) |
| Ulnar variance > 10 mm | 11 (73) | 15 (75) |
| Associated lesions | ||
| TBI | 6 (40) | 9 (45) |
| Chest injury | 3 (20) | 6 (30) |
| Femur fracture | 2 (13) | 2 (10) |
| Combinated | 4 (27) | 3 (15) |
Abbreviation: TBI, traumatic brain injury.
Data are presented as mean (range).
Data are presented as frequency (percentage).
Table 3. Mean grip strength at 12 months.
| Nonbridging, group A ( n = 15) | Bridging, group B ( n = 20) | Quartile position | p -Value | |
|---|---|---|---|---|
| Male | ( n = 4) | ( n = 7) | ||
| Affected wrist (kg) | 32.00 | 30.00 | 3/3 degrees | 0.527 |
| Normal wrist (kg) | 37.5 | 37.14 | 4/4 degrees | 0,512 |
| % Normal side | 85.33 | 80.78 | – | – |
| Female | ( n = 11) | ( n = 13) | ||
| Affected wrist (kg) | 20.00 | 19.69 | 3/3 degrees | 0.252 |
| Normal wrist (kg) | 22.45 | 21.85 | 3/3 degrees | 0.733 |
| % Normal side | 89.09 | 90.12 | – | – |
The objective and patient-reported outcomes are presented in Table 4 . The mean ROM in the total study population was 342.01 degrees (96.67% of the nonaffected side). The mean ROM was 344.47 degrees (96.94%) in the nonbridging group and 339.7 degrees (96.38%) in the bridging group. The mean QuickDASH score in the total study population was 3.691–18, whereas the scores in the nonbridging and bridging groups were 3.53 and 3.85, respectively. The mean VAS score in the total study population was 1.73, whereas the scores in the nonbridging and bridging groups were 1.60 and 1.85, respectively. On X-ray examination, an initial fracture reduction was observed in 91.43% of the patients, 86.67% and 95% of the patients, respectively. Complications were observed in five (14.28%) patients. These included pin infection (one patient in each group; Fig. 6 ), extensor pollicis longus tendon spontaneous lesion (one patient in group B), stiffness (one patient in group A), and heterotopic ossification (one patient in group B).
Table 4. Objective and patient-reported outcomes at 12-month follow-up.
| Nonbridging ( n = 15) |
Bridging ( n = 20) |
p -Value | |
|---|---|---|---|
| 12 months | |||
| ROM (in degrees) b | 344.47 (96.94%) | 339.7 (96.38%) | 0.482 |
| QuickDASH score (points) b | 3.53 | 3.85 | 0.986 |
| VAS pain (mm/10 mm) b | 1.60 | 1.85 | 0.615 |
| Maintenance initial reduction | 87% | 95% | – |
| Complication rate | 13% | 15% | – |
Abbreviations: DASH, Disabilities of the Arm, Shoulder and Hand; ROM, range of motion; VAS, visual analog scale.
Fig. 6.
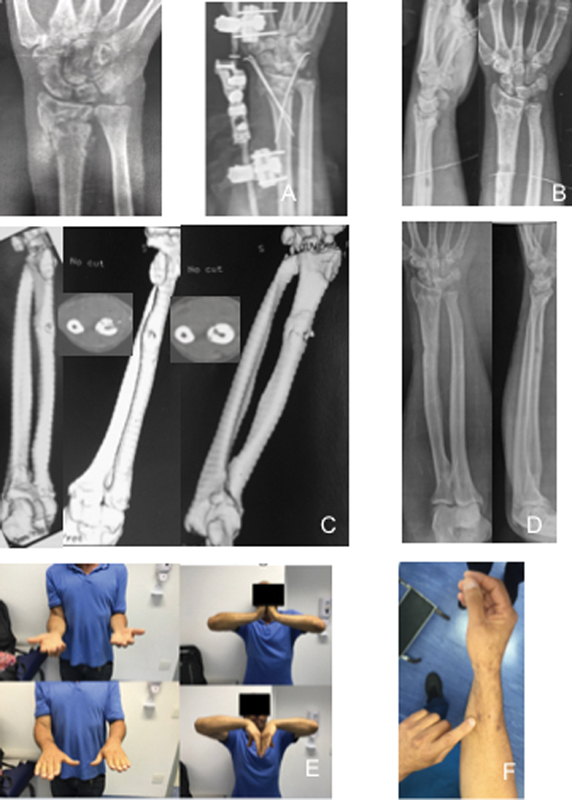
Complications. ( A,B ) X-ray pre/post. ( C ) Computed tomography (CT) scan preoperative. ( D ) functional aspects. ( E ) Clinical aspects: bridging group—right side and pin infection in radius shaft.
Discussion
Studies that have been published over the last few years have shown no significant difference between the outcomes of internal fixation and those of external fixation of distal radial fractures with respect to grip strength. 2 3 Of note, grip strength is commonly used to evaluate the treatment outcomes of DRFs and is an independent predictor of ADL disability among elderly patients. The test is an easy, reliable, valid, inexpensive screening method for the identification of older adults at risk of disability of ADLs in the lowest (first or second) quartile when compared with patients in the highest (third or fourth) hand grip strength quartile. All of our patients were in the third or fourth quartile. 9 In this study, no significant between-group differences were observed with respect to the clinical results and incidence of complications. In a study by McQueen, 13 treatment with a nonbridging external fixator showed better outcomes than those achieved with the bridging method. In our study, five patients developed complications, and the incidence of complications was comparable in the two groups (two patients in group A, three in group B).
In a study, patients who underwent internal fixation of DRFs showed better ROM in the early rehabilitation period as compared with those who received external fixation; however, the outcomes were comparable at the 1-year follow-up. 14 A criticism of the traditional external fixation of DRFs is the inability of longitudinal ligamentotaxis to attain a sagittal plane (volar tilt) reduction at the articular surface. The study by Taylor et al 15 and this study demonstrate that a multiplanar reduction technique using K-wires in association with dynamic external fixation augmentation can achieve an acceptable reduction. Only 8.57% of the patients showed loss of initial reduction.
Currently, the paradigm of ETC envisages early definitive surgery of patients with polytrauma. 16 17 According to this approach, the use of external fixation for the definitive treatment of DRFs is recommended wherever possible. Such an approach improves the quality of life of patients, reduces the hospitalization time, allows the immediate start of a rehabilitation protocol, and reduces the time of restoration of ADLs and work-related activities.
This study was a prospective randomized clinical trial, and all patients were operated on by a single surgeon, who is an upper limb trauma specialist, in a uniform group with complete follow-up. Nonetheless, some limitations need to be acknowledged. The inclusion criterion was AO type A or C fractures, and the sample size was small for QuickDASH and VAS analysis; however, it was sufficient for the statistical evaluation of the grip strength. There is a strong trend toward the use of volar plates for the treatment of DRFs in elderly patients, 18 although the results found were similar. However, further comparative studies are required to determine the method of choice.
Conclusion
Both bridging and nonbridging external dynamic fixations were found to be safe and reliable definitive treatment methods for unstable DRFs in elderly patients with polytrauma. The grip strength results in both groups predict the restoration of the ability of elderly patients to independently perform ADLs.
Acknowledgments
Translation service was provided by Sandra Miaguti. Paper correction was provided by Paulo Roberto Barbosa Lourenço, Marcos Ghizoni, and Matheus Azi.
Funding Statement
Funding None.
Conflict of Interest Authors Fabio Lucas Rodrigues, Karyse Helena Crispim Ribeiro Alves, Ricardo Kaempf de Oliveira, Gustavo Mantovani Ruggiero, and Luciano Miller Reis Rodrigues hereby declare that they have no conflicts of interest to disclose, and this project presents a potential conflict of interest between the principal investigator and the Orthofix. The conflict of interest pertains only to the development of implant external fixator (Galaxy Fixation System wrist).
Informed Consent
An informed consent document was provided to all research participants, who read and signed it according to their will.
Ethical Approval
The research was approved by and was in accordance with the ethical standards of the Faculdade de Medicina do ABC Ethics Committee on human experimentation (no. 805.909).
References
- 1.Safdari M, Koohestani M M. Comparing the effect of volar plate fixators and external fixators on outcome of patients with intra-articular distal radius fractures: a clinical trial. Electron Physician. 2015;7(02):1085–1091. doi: 10.14661/2015.1085-1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Landgren M, Abramo A, Geijer M, Kopylov P, Tägil M. Fragment-specific fixation versus volar locking plates in primarily nonreducible or secondarily redisplaced distal radius fractures: a randomized controlled study. J Hand Surg Am. 2017;42(03):156–1650. doi: 10.1016/j.jhsa.2016.12.001. [DOI] [PubMed] [Google Scholar]
- 3.Xie X, Xie X, Qin H, Shen L, Zhang C. Comparison of internal and external fixation of distal radius fractures. Acta Orthop. 2013;84(03):286–291. doi: 10.3109/17453674.2013.792029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ma C, Deng Q, Pu H et al. External fixation is more suitable for intra-articular fractures of the distal radius in elderly patients. Bone Res. 2016;4:16017. doi: 10.1038/boneres.2016.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kopylov P, Runnqvist K, Jonsson K, Aspenberg P. Norian SRS versus external fixation in redisplaced distal radial fractures. A randomized study in 40 patients. Acta Orthop Scand. 1999;70(01):1–5. doi: 10.3109/17453679909000946. [DOI] [PubMed] [Google Scholar]
- 6.Moher D, Hopewell S, Schulz K F et al. CONSORT 2010 explanation and elaboration: update guidelines for reporting parallel group randomized trials. BMJ. 2010;340:c869. doi: 10.1136/bmj.c869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ruedi T P, Murphy W M. Davos Platz, Switzerland: Thieme; 2000. Distal radius classification. [Google Scholar]
- 8.Fess E E. Chicago, IL: American Society of Hand Therapists; 1992. Grip Strength. 2nd ed. [Google Scholar]
- 9.Al Snih S, Markides K S, Ottenbacher K J, Raji M A. Hand grip strength and incident ADL disability in elderly Mexican Americans over a seven-year period. Aging Clin Exp Res. 2004;16(06):481–486. doi: 10.1007/BF03327406. [DOI] [PubMed] [Google Scholar]
- 10.Petersen P, Petrick M, Connor H, Conklin D. Grip strength and hand dominance: challenging the 10% rule. Am J Occup Ther. 1989;43(07):444–447. doi: 10.5014/ajot.43.7.444. [DOI] [PubMed] [Google Scholar]
- 11.Gummesson C, Ward M M, Atroshi I. The shortened Disabilities of the Arm, Shoulder and Hand questionnaire (QuickDASH): validity and reliability based on responses within the full-length DASH. BMC Musculoskelet Disord. 2006;7:44. doi: 10.1186/1471-2474-7-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Orfale A G, Araújo P MP, Ferraz M B, Natour J. Translation into Brazilian Portuguese, cultural adaptation and evaluation of the reliability of the Disabilities of the Arm, Shoulder and Hand Questionnaire. Braz J Med Biol Res. 2005;38(02):293–302. doi: 10.1590/s0100-879x2005000200018. [DOI] [PubMed] [Google Scholar]
- 13.McQueen M M. Redisplaced unstable fractures of the distal radius. A randomised, prospective study of bridging versus non-bridging external fixation. J Bone Joint Surg Br. 1998;80(04):665–669. doi: 10.1302/0301-620x.80b4.8150. [DOI] [PubMed] [Google Scholar]
- 14.Aita M A, Vieira Ferreira C H, Schneider Ibanez D et al. Randomized clinical trial on percutaneous minimally invasive osteosynthesis of fractures of the distal extremity of the radius. Rev Bras Ortop. 2014;49(03):218–226. doi: 10.1016/j.rboe.2014.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Taylor K F, Gendelberg D, Lustik M B, Drake M L. Restoring volar tilt in AO type C2 Fractures of the distal radius with unilateral external fixation. J Hand Surg Am. 2017;42(07):511–516. doi: 10.1016/j.jhsa.2017.03.020. [DOI] [PubMed] [Google Scholar]
- 16.Bates P, Parker P, McFadyen I, Pallister I. Demystifying damage control in musculoskeletal trauma. Ann R Coll Surg Engl. 2016;98(05):291–294. doi: 10.1308/rcsann.2016.0111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Simons T, Brinck T, Handolin L. Timing of surgical treatment of fractures of multiply injured patients - from science to tactics [in Finnish] Duodecim. 2016;132(09):828–835. [PubMed] [Google Scholar]
- 18.Lee D J, Elfar J C. External fixation versus open reduction with locked volar plating for geriatric distal radius fractures. Geriatr Orthop Surg Rehabil. 2014;5(03):141–143. doi: 10.1177/2151458514542337. [DOI] [PMC free article] [PubMed] [Google Scholar]


