Abstract
This study examines the associations between maternal Traditional dietary pattern adherence and HIV/treatment with neonatal size and adiposity in urban, black South Africans, as well as how specific maternal factors - i.e. BMI and GWG - may influence these associations. Multiple linear regression models were used to examine associations between maternal Traditional diet pattern adherence (pattern score), HIV/treatment status [three groups: HIV negative, HIV positive (antenatal antiretroviral treatment (ART) initiation), HIV positive (pre-pregnancy ART initiation)], BMI and GWG (kg/week) and: newborn (1) weight-to-length ratio (WLR, kg/m) in 393 mother-neonate pairs; (2) Peapod estimated fat mass index (FMI, kg/m3) in a 171-pair subsample. In fully adjusted models, maternal obesity and GWG were associated with 0.25 kg/m (P=0.008) and 0.48 kg/m (P=0.002) higher newborn WLR, while Traditional diet pattern score was associated with lower newborn WLR (-0.04 kg/m per +1 SD; P=0.033). Additionally, Traditional diet pattern score was associated with 0.13 kg/m3 (P=0.027) and 0.32 kg/m3 (P=0.005) lower FMI in the total sample and in newborns of normal weight women, respectively. HIV positive (pre-pregnancy ART) vs. HIV negative (ref) status was associated with 1.11 kg/m3 (P=0.002) higher newborn FMI. Promotion of a Traditional dietary pattern, alongside a healthy maternal pre-conception weight, in South African women may reduce newborn adiposity and metabolic risk profiles. In HIV-positive women, targeted monitoring and management strategies are necessary to limit treatment-associated effects on in utero fat deposition.
Key words/phrases: Pregnancy, Traditional dietary pattern, antiretroviral treatment, neonatal adiposity, South Africa
Introduction
Maternal pre-pregnancy body mass index (BMI) and gestational weight gain (GWG) are established predictors of fetal growth and birth outcomes; with both obesity and excessive weight gain being associated with high birth weight and large-for-gestational age (LGA) deliveries, as well as with obesity and cardiometabolic disease risk in later life (1–5). Although the effects of anthropometrically defined maternal nutritional status on birth weight have been well documented, the influence of dietary patterns on birth size – particularly in increasingly urbanised low-and-middle income countries (LMICs) such as South Africa – is not known. In addition, the predominant use of birth weight as a proxy for fetal growth fails to elucidate the effects of diet on adiposity (i.e. fat vs. fat-free mass) and therefore provides only a weak indication of newborn metabolic risk (6,7). Studies have shown that adiposity in early infancy tends to track through childhood and is associated with long term risk of central adiposity, as well as of elevated triglyceride levels and insulin resistance (8,9). Finally, the extent to which high HIV and antiretroviral treatment (ART) exposure in this setting prior to, and during, pregnancy may impact these associations is yet to be explored.
During a previous study in urban, black South Africans, we used principal component analysis (PCA) to identify three distinct dietary patterns in pregnant women; namely Western, Traditional and Mixed (10). These patterns were consistent with those expected for a transitioning African population experiencing a shift towards increasingly westernised diets high in saturated fat, sugar, salt, processed/convenience foods and edible oils and low in essential micronutrients (11,12). We further showed that adherence to the Traditional dietary pattern – characterised by high intakes of vegetables, beans and legumes, traditional meats and whole grains - was associated with lower rate of gestational weight gain (GWG) and reduced odds of excessive weight gain. These associations remained evident in women of normal weight after stratification, but not in overweight or obese subgroups. This suggests that the relationship between diet and maternal adiposity may be modified by baseline BMI. However, whether Traditional pattern intake is similarly associated with beneficial reductions in neonatal adiposity – either independently or via interactions with maternal nutritional status - is not known.
The maternal high risk profile in this setting – where 66% of women are overweight or obese and 55% experience excessive gestational weight gain - is further complicated by a 33% prevalence of HIV (10). While ART initiation is mandatory in South Africa for all HIV positive pregnant women not yet receiving treatment, and this has had undeniable benefits in the prevention of vertical transmission, the metabolic consequences for both mother and infant are not clear. Both HIV infection and ART exposure have been positively associated with weight and fat distribution changes and altered glucose and lipid metabolism in both adults and children, as well as with adverse birth outcomes (13–17). However, little is known about the possible effects of HIV/treatment on fetal growth and adiposity, as well the risk of non-communicable disease in the long term.
The aim of this study was therefore to examine the associations between maternal Traditional dietary pattern adherence and HIV/treatment with neonatal size and adiposity in urban, black South Africans, as well as how specific maternal factors - i.e. BMI and GWG - may influence these associations.
Methods
Study Setting and Participants
This study was nested within a large pregnancy cohort study (Soweto First 1000-Day Study; S 1000), based at the Chris Hani Baragwanath Hospital in Soweto, Johannesburg, South Africa between 2013 and 2016. Overall, S 1000 aimed to understand the complex associations between multiple maternal factors and fetal and infant outcomes in an urban-poor African context, and to identify the levers that could optimise maternal and child health within the first 1000 days. Inclusion criteria for S 1000 were as follows: resident of Soweto, or the Greater Soweto area, <20 weeks gestational age at recruitment, non-epileptic, non-diabetic, 18 years or older and pregnant with a singleton, naturally conceived pregnancy. Data collection for S 1000 took place at six time points during pregnancy (<14 weeks; 14–18 weeks; 19–23 weeks; 24–28 weeks; 29–33 weeks and 34–38 weeks) and eight time points after delivery (<14 days; 6 weeks; 2 months; 3 months; 6 months; 12 months; 18 months and 24 months). All women provided written informed consent prior to their inclusion in the pregnancy component of the study (Soweto Fetal Growth Study), as well as prior to the inclusion of themselves and their infants in the post-delivery follow-up (Soweto Baby Growth Study). Ethical approval was obtained from the University of the Witwatersrand’s Research Ethics Committee (Medical) for both components of S 1000 (M120524 and M130905). 559 women were recruited into this sub-study and had dietary intake assessed at 14-18 weeks.
Maternal Variables
Demographic, Health and Socio-Economic Variables
Maternal demographic and socio-economic variables were collected by trained members of research staff using interviewer-administered questionnaires at the first pregnancy visit (<14 weeks gestational age). Parity was defined as the number of previous births at a gestational age of 24 weeks or more - regardless of whether the infant was born alive or was stillborn. Smoking and/or chewing tobacco was reported at baseline. HIV-status was self-reported at each pregnancy visit and confirmed using the results recorded in the participant’s antenatal clinic card. According to South Africa’s national Prevention of Mother-to-Child Transmission (PMTCT) guidelines, routine HIV counselling and testing is required during pregnancy; for any HIV-positive woman who is not already receiving treatment, ART is initiated. All HIV-positive participants in this study were therefore receiving ART and were stratified according to whether they had been initiated on ART prior to pregnancy (pre-pregnancy ART) or during the current pregnancy (antenatal ART). Household socio-economic status (SES) was assessed using an asset index which scored each participant according to the number of assets that they possessed out of a possible 9 (electricity, radio, television, refrigerator, mobile phone, personal computer, bicycle, motorcycle/scooter, car). This was based on standard measures used in the Demographic and Health Surveys household questionnaire (available at: www.measuredhs.com) and has been extensively utilised in this setting (18,19). Asset index scores were subsequently grouped into low (<5), medium (5-7) and high (>7) SES categories. Maternal education was defined according to the highest level of completed (primary, secondary or tertiary).
Anthropometry
A wall-mounted Stadiometer (Holtain, UK) was used to measure maternal height to the nearest 1 mm at baseline. Maternal weight was measured to the nearest 0.1 kg at each visit during pregnancy using a digital scale. Weight at recruitment (<14 weeks) was used as a proxy for pre-pregnancy weight and, together with height, was used to calculate maternal BMI (weight (kg)/height (m2)). There were no underweight women in this sample and therefore BMI was classified according to the following categories: normal weight (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2) or obese (≥30.0 kg/m2). GWG (kg/week) was calculated as: [(weight at final pregnancy visit − weight at recruitment)/duration of follow-up]. GWG was classified as inadequate, adequate or excessive according to the BMI-specific Institute of Medicine recommended weight gain ranges (20).
Dietary Intake
Habitual dietary intake was assessed at the second pregnancy visit (14-18 weeks) using an interviewer-administered quantitative food-frequency questionnaire (QFFQ). This nationally utilised QFFQ was developed by the South African Medical Research Council (SAMRC) based on analyses of 11 dietary surveys conducted in rural and urban South Africa and includes all foods consumed by at least 3% of the population (21). Retrospective data was collected on the frequency and quantity of food and beverage intake during the previous week using food flash cards (high quality photographs of food items) and a combination of household measures, two-dimensional life-size drawings of foods and utensils, and three-dimensional food models as described and validated by Steyn et al (22). According to the criteria developed by Dennis et al, this QFFQ is a very high quality tool – scoring a total of 13 points (high quality classified as a score of seven or higher) (23). This QFFQ has been extensively piloted and utilised in this setting and results are published elsewhere (10,24,25). QFFQ data was captured electronically using REDCap electronic data capture tools hosted at The University of the Witwatersrand (26).
Neonatal variables
Neonates were included in this study if they were born at term (≥37 weeks) and had complete delivery outcome data. Additionally, body composition was analysed for a sub-sample who had assessments via either air displacement plethysmography (ADP) using the Peapod (Cosmed, USA) or dual-energy x-ray absorptiometry (DXA; (Hologic DiscoveryA S/N 86254, APEX software version 4.0.2, Hologic Inc., USA) within the first two weeks of life.
Birth outcomes
Gestational age at delivery (weeks) was calculated as: [duration of pregnancy follow-up (date of delivery – date of baseline ultrasound dating scan) + gestational age at baseline (crown-to-rump length measured by ultrasound; days)]. Birth weight and length were measured by trained research nurses within 24 hours of delivery for 82% of neonates. Where assessment within this window was not possible – for example due to the infant being admitted to the hospital for observation – measurements were taken within 48 hours. Weight to length ratio (WLR; kg/m) was calculated to represent the best anthropometric predictor of neonatal body composition (fat-free mass and fat mass) as described by Villar et al (27).
Neonatal body composition
Weight and length were measured and fat mass and fat-free mass estimated for nude neonates within 14 days of birth. According to a previous study in which we demonstrated the level of agreement between ADP and DXA estimated body composition in this population, ADP was utilised where available (28). In cases where a neonate had only DXA measurements, fat mass and fat-free mass were converted to their ADP equivalent estimates using the following linear equations:
Fat mass (ADP equivalent) = 139.8311 + 0.7974718 * DXA fat mass
Fat-free mass (ADP equivalent) = 89.40371 + 0.8728309 * DXA fat-free mass
These equations were generated for the population from the regression of ADP on DXA measurements in the aforementioned ADP/DXA comparison study and provided reliable ADP equivalent estimates (28). Fat mass index (FMI; kg/m3) was calculated from these estimates to describe adiposity in neonates. As described by Villar et al, the applicability of exponents in body composition indices to address the relationship between body composition and size may vary across populations (27). We therefore regressed fat mass on length (data in natural logarithms) to confirm that this index (kg/m3) provided the best description of the relationship between weight and length in the study population. This was indeed confirmed - regression power exponent: 2.8±0.6 (SE) (29).
ADP
Peapod assessments were performed according to standard procedures as previously described (30,31). Participants were placed inside the Peapod chamber wearing only a wig cap if necessary. Body volume was estimated using pressure and volume changes (air displacement) within the chamber and body density calculated using body mass and volume measurements. Fat mass, and fat-free mass were subsequently derived using gender-specific equations developed by Fomon et al (32).
DXA
DXA scanning was performed according to standard procedures as described elsewhere (33). Typically, neonates were fed prior to DXA scanning and were sleeping during the procedure. Neonates were placed supine on the scanning bed wearing only a disposable diaper and swaddled in a cotton blanket. Scans were satisfactory for use if the subject’s body lay within the scanning region and there was minimal movement during assessment. Whole body measurements of fat mass and fat-free mass were extracted for use in analyses.
Statistical Analysis
Data were analysed for 393 mother-neonate pairs with complete data using STATA 13.0 (StataCorp, College Station, TX, USA). The flow of participants through the sub-study to reach the final sample sizes for the primary and secondary outcomes (WLR and FMI respectively) is depicted in Supplementary Figure 1. Mother-neonate pairs included in the final analyses did not differ in any baseline maternal characteristics (demographics, socio-economic status and anthropometry) from those excluded.
The dietary patterns previously identified in this population – namely Western, Traditional and Mixed – were confirmed in this sub-sample using PCA as described elsewhere (10). PCA was conducted using orthogonal (varimax) rotation on the weekly frequency of consumption of the QFFQ food items, classified as 48 food items/groups based on those described by Crozier et al (34,35). The Kaiser-Meyer-Olkin measure of sampling adequacy (0.68) and Bartlett’s test of sphericity (p<0.001) confirmed PCA as an appropriate dimension reduction technique for use in this sample. Eigen values, as well as their visual inflections on a scree plot, and the percentage of total variance explained were used to retain patterns. As described elsewhere, foods or food groups with factor loadings ≥ 0.2 reflected strong associations with principal components and were used to name the dietary patterns (36). Dietary pattern scores for each pattern were generated by multiplying factor loadings by the standardised intake of each food/food group and then summing these. Mean factor scores for the patterns were zero; with positive and negative scores representing high and low adherence respectively of each dietary pattern (37). Due to the associations previously demonstrated between the Traditional diet pattern and GWG in this population, maternal diet was classified according to adherence to the Traditional pattern (Traditional pattern score) in all subsequent study analyses.
Maternal and neonatal characteristics of the sample are presented as median (interquartile range) and percentages (%) for continuous and categorical variables respectively. The Kruskal-Wallis test was used to compare neonatal WLR and FMI according to the following maternal and infant factors: maternal age, parity, HIV/treatment status, smoking status, education, marital status, SES, BMI at recruitment, GWG, Traditional diet pattern adherence, neonate sex and gestational age at birth.
Based on known associations between maternal factors and birth size, as well as previously described associations in this population (10), we proposed a conceptual framework for the associations between maternal Traditional pattern adherence (continuous: diet pattern score), BMI (categorical: normal weight (ref) vs. overweight and obese), GWG (continuous: kg/week), HIV/treatment status (categorical: HIV negative (ref) vs. HIV positive (antenatal ART) and HIV positive (pre-pregnancy ART) and neonatal WLR (continuous: kg/m) and FMI (continuous: kg/m3). The bivariate associations between these maternal factors and each neonatal outcome were tested using linear regression analyses.
In order to identify the independent associations between diet, BMI, GWG, HIV/treatment status and WLR and FMI we performed hierarchical regression analyses per outcome. Covariates included in analyses were maternal or infant variables conclusively associated with infant outcome(s) (namely parity, newborn sex and gestational age at birth). Additionally, for FMI, age at scan (days) was included to adjust for variation across the two week assessment period. Regression coefficients and R2 values are therefore presented across three models for WLR and FMI. Variables included in the models were as follows: Model 1 (M1): neonate sex and Traditional diet pattern score; Model 2 (M2): M1 with HIV/treatment status, BMI and GWG; Model 3 (M3): M2 with parity and gestational age at delivery (and age at scan for FMI). In order to test for an interaction between BMI and dietary pattern adherence, a fourth model per outcome was run as follows: M3 with the interaction term BMI category*Traditional pattern score (data not shown). P-values tailed at 0.05 were considered statistically significant.
Results
Maternal and infant characteristics are presented in Table 1. The median age of pregnant women was 30 years. 35% and 30% of women were overweight and obese at recruitment, respectively, while 58% gained excessive weight according to the IoM BMI-specific guidelines. 34% of women were HIV positive; with 23% in total being initiated on ART during the current pregnancy. 52% of newborns were male. Neonates had a median birth weight of 3100 g and WLR and FMI were 6.4 kg/m and 3.6 kg/m3 respectively.
Table 1. Maternal and neonatal characteristics of urban, black South Africans (n=393).
| Median (IQR) or % | |
|---|---|
| Maternal variables | |
| Demographic and health characteristics | |
| Maternal age, y | 30 (25-35) |
| Parity | |
| Para 0 | 25 |
| Para 1 | 45 |
| Para ≥2 | 30 |
| HIV status | |
| HIV-negative | 66 |
| HIV-positive (antenatal ART) | 23 |
| HIV-positive (pre-pregnancy ART) | 11 |
| Smokes/chews tobacco | |
| No | 87 |
| Yes | 13 |
| Socioeconomic characteristics | |
| Maternal education | |
| Primary | 2 |
| Secondary | 70 |
| Tertiary | 28 |
| Marital status [n=387] | |
| Single | 61 |
| Married/cohabiting | 39 |
| Household SES | |
| Low | 13 |
| Medium | 80 |
| High | 7 |
| Anthropometry | |
| BMI at recruitment, kg/m2 (<14 weeks) | 27.2 (23.8-30.9) |
| Normal weight (18.5-24.9) | 35 |
| Overweight (25-29.9) | 35 |
| Obese (≥30) | 30 |
| GWG, kg/week | 0.41 (0.28-0.56) |
| Inadequate | 22 |
| Adequate | 20 |
| Excessive | 58 |
| Neonatal variables | |
| Sex | |
| Male | 52 |
| Female | 48 |
| Gestational age at delivery, weeks | 39 (38-40) |
| Anthropometry | |
| Birth weight, g | 3100 (2850-3365) |
| Birth length, cm | 48.9 (47.3-50.3) |
| Weight to length ratio (kg/m) | 6.4 (5.9-6.8) |
| Body composition [n=171]a | |
| Age at scanning, d | 8 (4) |
| Fat mass, g | 435 (331-548) |
| Fat-free mass, g | 2774 (2530-2929) |
| Fat mass index, kg/m3 | 3.6 (2.9-4.6) |
Abbreviations: BMI, body mass index; GWG, gestational weight gain; ART, antiretroviral treatment IoM GWG ranges (kg/week): inadequate, normal weight <0.35, overweight <0.23, obese <0.17; adequate, normal weight 0.35-0.50, overweight 0.23-0.33, obese 0.17-0.27; excessive, normal weight >0.50, overweight >0.33, obese >0.27
Measured by air displacement plethysmography (ADP; Peapod) or dual-energy x-ray absorptiometry (DXA) corrected for the measurement differences between techniques
As previously described, for the purpose of this study maternal diet was classified according to Traditional diet pattern adherence (i.e. Traditional diet pattern score). This dietary pattern was characterised by high factor loadings for vegetables, beans and legumes, traditional meats and porridge/pap (Supplementary Table 1).
Of the maternal variables described as potential covariates in this population, only parity was consistently associated with neonatal outcomes; with higher WLR and FMI seen in infants born to mothers who had experienced at least one previous birth (Supplementary Table 2). Female neonates had significantly higher FMI than males and WLR increased with gestational age.
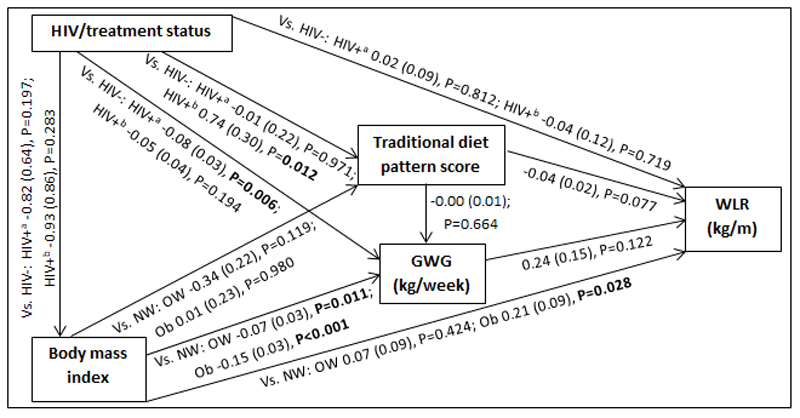
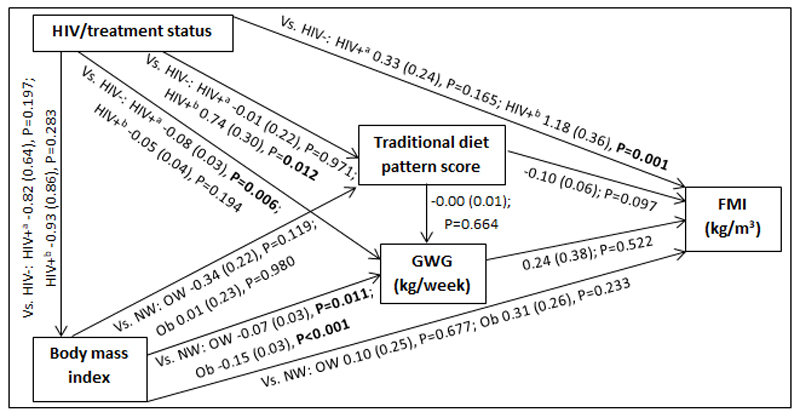
Conceptual models for the bivariate associations between maternal Traditional diet pattern, BMI, GWG and HIV/treatment status and outcomes of interest are presented in Figures 1 (WLR) and 2 (FMI). Compared to those of normal weight at recruitment, overweight and obese women exhibited significantly lower GWG. GWG was also lower in HIV positive (antenatal ART initiation) vs. HIV negative women. Additionally, in HIV positive women, pre-pregnancy ART initiation was associated with higher adherence to the Traditional diet pattern. Maternal obese vs. normal weight BMI was positively associated with WLR during bivariate analyses, while HIV positive (pre-pregnancy ART) status was positively associated with FMI when compared to HIV negative status.
Figure 1.
Conceptual model with bivariate associations between maternal factors and neonatal weight-to-length ratio (kg/m) in urban, black South Africans Values are regression coefficients with standard errors [β(SE)] from linear regression analyses; significant results presented in bold (P<0.05) Abbreviations: GWG, gestational weight gain; HIV-, HIV negative; HIV+a, HIV positive (antenatal ART); HIV+b, HIV positive (pre-pregnancy ART); NW, normal weight; OW, overweight; Ob, obese; Vs, versus (i.e. compared to the following reference category); WLR, newborn weight-to-length ratio
Figure 2.
Conceptual model with bivariate associations between maternal factors and neonatal fat mass index (kg/m3) in urban, black South Africans Values are regression coefficients with standard errors [β(SE)] from linear regression analyses; significant results presented in bold (P<0.05) Abbreviations: FMI, neonatal fat mass index; GWG, gestational weight gain; HIV-, HIV negative; HIV+a, HIV positive (antenatal ART); HIV+b, HIV positive (pre-pregnancy ART); NW, normal weight; OW, overweight; Ob, obese; Vs, versus (i.e. compared to the following reference category)
Table 2 presents the results of hierarchical regression analyses of maternal variables on newborn WLR. In fully adjusted models (M3: adjusted for neonate sex, Traditional diet pattern score, HIV/treatment status, BMI, GWG, parity and gestational age at delivery) a 1 SD increase in Traditional diet pattern score was inversely associated with newborn WLR (-0.04 kg/m; P=0.033). In addition, compared to a normal weight BMI at recruitment, maternal obesity was positively associated with WLR (M3: 0.25 kg/m; P=0.008) and a 1 kg/week increase in GWG was associated with a 0.48 kg/m increase in newborn WLR (M3: P=0.002). M3 explained approximately 14% of the variation in newborn WLR.
Table 2. Hierarchical regression for the associations between maternal factors and neonatal weight to length ratio (n=393).
| WEIGHT TO LENGTH RATIO (kg/m) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Independent Variables | Model 1 | Model 2 | Model 3 | ||||||
| B | 95% CI | P-valueb | β | 95% CI | P-valueb | β | 95% CI | P-valueb | |
| Neonate sex | |||||||||
| Male | Ref | Ref | Ref | ||||||
| Female | -0.02 | -0.17; 0.13 | 0.769 | -0.05 | -0.19; 0.10 | 0.533 | -0.06 | -0.20; 0.08 | 0.396 |
| Maternal dietary pattern | |||||||||
| Traditional pattern score | -0.04 | -0.08; 0.00 | 0.078 | -0.04 | -0.08; 0.00 | 0.081 | -0.04 | -0.08; -0.00 | 0.033 |
| HIV/treatment status | |||||||||
| HIV negative | Ref | Ref | |||||||
| HIV-positive (antenatal ART) | 0.07 | -0.11; 0.25 | 0.422 | 0.07 | -0.10; 0.24 | 0.436 | |||
| HIV-positive (pre-pregnancy ART) | 0.01 | -0.23; 0.26 | 0.906 | -0.02 | -0.26; 0.21 | 0.833 | |||
| BMI category | |||||||||
| Normal weight | Ref | Ref | |||||||
| Overweight | 0.09 | -0.09; 0.26 | 0.343 | 0.09 | -0.08; 0.26 | 0.301 | |||
| Obese | 0.27 | 0.08; 0.46 | 0.005 | 0.25 | 0.07; 0.43 | 0.008 | |||
| Gestational weight gain | |||||||||
| Rate, kg/week | 0.36 | 0.05; 0.67 | 0.024 | 0.48 | 0.18; 0.78 | 0.002 | |||
| Parity | |||||||||
| Para 0 | Ref | ||||||||
| Para 1 | 0.33 | 0.15; 0.50 | <0.001 | ||||||
| Para ≥2 | 0.32 | 0.13; 0.52 | 0.001 | ||||||
| Gestational age | |||||||||
| Gestational age at birth, weeks | 0.18 | 0.12; 0.24 | <0.001 | ||||||
| R2 per model | 0.008 | 0.035 | 0.137 | ||||||
Values are regression coefficients with 95% confidence intervals
Multiple linear regression analyses; significant results are presented in bold (p<0.05)
The results of hierarchical regression analyses of maternal variables on newborn FMI are presented in Table 3. Traditional diet pattern adherence was associated with lower FMI (-0.13 kg/m3 per +1 SD; P=0.027) after full adjustment for covariates (M3: adjusted for neonate sex, Traditional diet pattern score, HIV/treatment status, BMI, GWG, parity, gestational age at delivery and age at scan). HIV positive (pre-pregnancy ART) vs. HIV negative status was associated with 1.18 kg/m3 (P=0.001) higher neonatal FMI in M2 (adjusted for neonate sex, Traditional diet pattern score, HIV/treatment status, BMI, GWG). This association remained significant in the fully adjusted model (M3: 1.11 kg/m3; P=0.002). Approximately 19% of the variation in newborn FMI was explained in M3.
Table 3. Hierarchical regression for the associations between maternal factors and neonatal fat mass index (n=171).
| FAT MASS INDEX (kg/m3) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Independent Variables | Model 1 | Model 2 | Model 3 | ||||||
| β | 95% CI | P-valueb | β | 95% CI | P-valueb | β | 95% CI | P-valueb | |
| Neonate sex | |||||||||
| Male | Ref | Ref | Ref | ||||||
| Female | 0.44 | 0.04; 0.84 | 0.033 | 0.40 | 0.00; 0.79 | 0.049 | 0.39 | 0.01; 0.78 | 0.044 |
| Maternal dietary pattern | |||||||||
| Traditional pattern score | -0.09 | -0.22; 0.03 | 0.130 | -0.10 | -0.22; 0.02 | 0.086 | -0.13 | -0.25; -0.02 | 0.027 |
| HIV/treatment status | |||||||||
| HIV negative | Ref | Ref | |||||||
| HIV-positive (antenatal ART) | 0.37 | -0.10; 0.84 | 0.123 | 0.29 | -0.17; 0.75 | 0.218 | |||
| HIV-positive (pre-pregnancy ART) | 1.18 | 0.48; 1.87 | 0.001 | 1.11 | 0.42; 1.81 | 0.002 | |||
| Gestational weight gain | |||||||||
| Rate, kg/week | 0.44 | -0.29; 1.18 | 0.238 | 0.46 | -0.26; 1.18 | 0.213 | |||
| BMI category | |||||||||
| Normal weight | Ref | Ref | |||||||
| Overweight | 0.17 | -0.30; 0.65 | 0.469 | 0.20 | -0.26; 0.66 | 0.390 | |||
| Obese | 0.37 | -0.13; 0.87 | 0.147 | 0.24 | -0.25; 0.74 | 0.335 | |||
| Parity | |||||||||
| Para 0 | Ref | ||||||||
| Para 1 | 0.76 | 0.27; 1.25 | 0.002 | ||||||
| Para ≥2 | 0.64 | 0.11; 1.17 | 0.018 | ||||||
| Neonate age | |||||||||
| Gestational age at birth, weeks | 0.09 | -0.08; 0.26 | 0.286 | ||||||
| Age at examination, days | 0.05 | 0.00; 0.10 | 0.035 | ||||||
| R2 per model | 0.043 | 0.121 | 0.194 | ||||||
Values are regression coefficients with 95% confidence intervals
Multiple linear regression analyses; significant results are presented in bold (p<0.05)
Although BMI and GWG were not associated with newborn FMI in any of the presented regression models; we confirmed an interaction between Traditional diet pattern adherence and maternal BMI on FMI (vs. normal weight: overweight*Traditional diet pattern, P=0.203; obese*Traditional diet pattern, P=0.024). Therefore, while dietary pattern adherence was associated with a significant reduction in FMI for infants born to normal weight women (-0.32 kg/m3; P=0.005), these effects were not seen among newborns of overweight or obese women (data not shown).
Discussion
To our knowledge this is the first study to explore the relationships between maternal nutritional status, dietary patterns and HIV/treatment exposure in African women and to examine their effects on neonatal adiposity within the first two weeks of life. We found that, although maternal obesity and GWG were associated with neonatal body composition, they predicted overall birth size rather than increased fat mass in particular. In contrast, adherence to a Traditional dietary pattern during pregnancy was associated with lower WLR and FMI; suggestive of a predominant effect on fat mass in the neonate. Finally, we showed that duration of ART exposure (pre-pregnancy vs. antenatal initiation) in HIV positive women was positively associated with newborn adiposity in this setting.
Our findings build on data previously reported on the association between Traditional dietary pattern adherence and reduced GWG (including odds of excessive weight gain) in this population (10). Here we show that, not only is a dietary pattern high in vegetables, beans and legumes, traditional meats and whole grains associated with beneficial reductions in maternal adiposity during pregnancy, but also in fetal fat deposition. Such effects have important implications for the long term health trajectory of the infant; with previous studies showing a tendency towards tracking of adiposity through infancy, as well as of an increased risk of obesity and elevated metabolic risk profiles (including higher fasting triglyceride concentrations and insulin resistance) in later life (8,9). In addition, while Catalano et al demonstrated a significant correlation between body fat percentage at birth and at childhood follow up (mean age: 8.8 ± 1.8 years), there was no correlation in total weights at these two time points (9). This highlights the importance of neonatal adiposity as a potential predictor for longer-term obesity and metabolic disease risk.
Although the associations between a traditional diet pattern and neonatal WLR and FMI are unique to our study, they are supported by Starling et al who found that intake of a diet pattern with lower consumption of green vegetables and dairy and higher in refined grains was associated with higher birth weight, fat mass and body fat percentage in the US (38). However, conflicting results have also been shown; with typically healthier diet patterns (Mediterranean and Traditional) being associated with higher birth weight and reduced SGA risk, while more processed or Western dietary patterns have been associated with increased risk of SGA and lower weight-for-age z-score in some high income settings (39–43).
The relationship between maternal diet and birth size and adiposity is complex and the variation in findings across populations may reflect an influence of baseline nutritional status on these associations. For example, while energy dense, processed diets have been shown to restrict fetal growth and increase SGA risk in certain populations, they may increase the risk of high birth weight and adiposity in others (42–44). As both ends of the spectrum - i.e. being born too small or too large for gestational age – are associated with long term disease risk (45–48), identifying patterns of intake which facilitate optimal fetal growth and limit excess fat deposition in increasingly urbanised African populations, is critical. Given the high level of urbanisation in Africa - and particularly South Africa - to date, as well as the representativeness of the study population to that of an urban-poor community, our findings contribute substantially to understanding these contexts. Here we confirm that, not only do the effects of maternal dietary patterns on GWG differ across BMI categories (10), but the association between Traditional diet pattern adherence and neonatal adiposity is similarly modified by maternal BMI at baseline; with the effects seen predominantly in the normal weight subgroup. This suggests that, in increasingly obesogenic populations, the beneficial effects of improved diet quality may be limited in women who exhibit excess adiposity and associated metabolic risk profiles prior to conception. Obesity induces a chronic inflammatory state that has been suggested as a key driver of insulin resistance and may intensify the naturally occurring insulin resistant profile during pregnancy (6,49,50). Reduced insulin sensitivity in the obese pregnant woman – and the subsequent increase in availability of glucose and lipids – may potentially facilitate excess substrate transfer to the fetus and, thus, fat deposition irrespective of the current dietary pattern.
While we found no differences in WLR or FMI between infants born to HIV positive women with antenatal ART initiation compared to their HIV negative counterparts, we showed a significant increase in FMI for infants whose mothers were HIV positive and initiated on ART prior to the current pregnancy. These associations were independent of baseline BMI, GWG and diet and therefore suggest a strong treatment effect in this population. ART associated metabolic complications have been widely documented in HIV positive patients, with fat redistribution (reduced subcutaneous and increased central adiposity), impaired glucose tolerance and insulin resistance, as well as dyslipidaemia being common side effects (51,52). Such changes may substantially impact the metabolic risk profile of women prior to conception; further exacerbating the pregnancy associated insulin resistant state and increasing the risk of gestational diabetes mellitus (GDM) and associated complications. These findings have important implications for HIV positive pregnancies in South Africa, during which duration of ART exposure (increasing with each subsequent pregnancy) may elevate the risk profile for both mother and infant in an already high risk population. Targeted monitoring and care strategies are therefore needed in order to minimise the adverse effects of treatment exposure on adiposity and associated metabolic risk in the newborn; with interventions designed to optimise nutritional status and diet quality pre-conception being potentially more vital in these women.
Although we showed significant effects of maternal nutritional status, diet and HIV/treatment exposure on birth size and/or neonatal adiposity, our final models explained only 14% and 19% respectively of the variability in infant outcomes. While maternal adult size, adiposity and metabolic profile are predictive of infant outcomes, these characteristics are highly influenced by a mothers own growth and development; with studies showing strong intergenerational associations between maternal and offspring birth weight (53–56). This suggests that the gestational environment of the mother – and the resulting consequences on maternal birth size and longer term metabolic risk profile – may be an important factor in further explaining differences in neonatal size and adiposity in our study. In addition, there may be other behavioural factors which require exploration in these models, such as physical activity. Although there was no association found between physical activity and birth outcomes (including birth weight and ponderal index) in a previous study of this population (57), any potential indirect effects on birth size – for example through reductions in GWG and/or risk of GDM – as well as possible associations with fetal fat deposition and neonatal adiposity should be explored (51–53).
Other limitations of our study include the use of baseline BMI as a proxy for pre-pregnancy BMI and the variation in timing of maternal anthropometric measurements for assessing maternal GWG as previously described (10). Although first trimester weight has been identified as an adequate proxy for pre-pregnancy weight – correctly classifying 91-95% of women according to pre-pregnancy BMI - BMI specific differences in weight gain during trimester one have been shown (61,62). While use of baseline weight may have resulted in a degree of misclassification in our study, any effects on study findings were likely to be negligible due to the low overall amount of weight gained prior to 14 weeks; particularly in black women at higher BMIs (62). In addition, although the categorisation of pregnant women into three HIV/treatment status groups (i.e. HIV negative, HIV positive (antenatal ART) and HIV positive (pre-pregnancy ART)) allowed for effective comparison of overall treatment exposure in our sample, inclusion of additional measures of duration and/or adherence to ART would allow for more robust comparison of ART exposure on a continuous scale. While we present strong evidence for an effect of ART exposure on neonatal adiposity, use of an objective measure such as viral load – an established proxy for ART adherence/effectiveness (63) - would be beneficial in further explaining the influence of treatment on fetal fat deposition and metabolic risk in future research. Given the focus of our study and the differential patterns of growth (both in fat mass and fat free mass) between pre-term and term infants, we included only term neonates in our analyses (27). While this reduced the final sample size, it allowed for better interpretation of the effects of maternal factors (principally diet and HIV/treatment status) on newborn adiposity. However, future studies should explore these associations in pre-term infants in order to further elucidate the relationships with newborn size and adiposity according to gestational age. Lastly, neonatal body composition was measured using two techniques (Peapod and DXA) within the first two weeks of life which may reduce comparability across the sample; particularly due to the reduced sample size for these objective assessments. However, the comparability between techniques previously shown in this population allowed for correction of DXA to Peapod measurements and therefore equivalent fat mass estimates in the sub-sample (28). Although the variation in day of neonatal body composition assessment must be considered - with physiological weight loss occurring during this period – any changes in body composition are predominantly due to reductions in body water and would therefore have little effect on the comparability of fat mass estimates between subjects (64).
Conclusions
Our findings suggest that increased adherence to a Traditional diet pattern - high in whole grains, beans and legumes, vegetables and traditional meats and low in processed/convenience foods— may reduce neonatal adiposity in urban, black South Africans. However, early intervention to ensure a healthy BMI prior to pregnancy is needed in order to optimise the beneficial effects of diet quality on adiposity and associated metabolic risk for both mother and infant. Although ART initiation and adherence is critical for both maternal and infant health, the effects of treatment exposure on maternal metabolic risk and neonatal adiposity highlights the vulnerability of HIV positive pregnant women and the importance of tailored care in this population. Targeted monitoring and management strategies are therefore necessary to limit treatment-associated effects on in utero fat deposition and to potentially reduce metabolic risk profiles and poor health trajectories of infants in both the short and longer term.
Supplementary Material
Financial Support
The support of the DST-NRF Centre of Excellence (CoE) in Human Development at the University of the Witwatersrand, Johannesburg in the Republic of South Africa towards this research is hereby acknowledged. Opinions expressed and conclusions arrived at, are those of the author and are not to be attributed to the CoE in Human Development.
In addition we acknowledge funding from the UK MRC/DfID African Research Leader Scheme and the South African Medical Research Council.
The aforementioned funders had no role in the design, analysis or writing of this article.
Footnotes
Conflict of Interest
None
Authorship
SVW, KKO and SAN contributed to conceptualisation and design of the work towards this paper; SVW, PTP and SAN facilitated data acquisition; SVW analysed the data and drafted the manuscript; all authors contributed to interpretation of results and/or revision of the manuscript; all authors gave their approval of the final version for submission
References
- 1.Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. The Lancet. 2013 Aug;382(9890):427–51. doi: 10.1016/S0140-6736(13)60937-X. [DOI] [PubMed] [Google Scholar]
- 2.Ruager-Martin R, Hyde MJ, Modi N. Maternal obesity and infant outcomes. Early Hum Dev. 2010 Nov;86(11):715–22. doi: 10.1016/j.earlhumdev.2010.08.007. [DOI] [PubMed] [Google Scholar]
- 3.Wrottesley SV, Lamper C, Pisa PT. Review of the importance of nutrition during the first 1000 days: maternal nutritional status and its associations with fetal growth and birth, neonatal and infant outcomes among African women. J Dev Orig Health Dis. 2016 Apr;7(2):144–62. doi: 10.1017/S2040174415001439. [DOI] [PubMed] [Google Scholar]
- 4.Poston L, Caleyachetty R, Cnattingius S, Corvalán C, Uauy R, Herring S, et al. Preconceptional and maternal obesity: epidemiology and health consequences. Lancet Diabetes Endocrinol. 2016 Dec 1;4(12):1025–36. doi: 10.1016/S2213-8587(16)30217-0. [DOI] [PubMed] [Google Scholar]
- 5.Hunt KJ, Alanis MC, Johnson ER, Mayorga ME, Korte JE. Maternal pre-pregnancy weight and gestational weight gain and their association with birthweight with a focus on racial differences. Matern Child Health J. 2013 Jan;17(1):85–94. doi: 10.1007/s10995-012-0950-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Catalano PM, Thomas A, Huston-Presley L, Amini SB. Increased fetal adiposity: a very sensitive marker of abnormal in utero development. Am J Obstet Gynecol. 2003 Dec;189(6):1698–704. doi: 10.1016/s0002-9378(03)00828-7. [DOI] [PubMed] [Google Scholar]
- 7.Donnelly JM, Lindsay KL, Walsh JM, Horan M, Molloy EJ, McAuliffe FM. Fetal metabolic influences of neonatal anthropometry and adiposity. BMC Pediatr. 2015 Nov 10;15:175. doi: 10.1186/s12887-015-0499-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ay L, Hokken-Koelega ACS, Mook-Kanamori DO, Hofman A, Moll HA, Mackenbach JP, et al. Tracking and determinants of subcutaneous fat mass in early childhood: the Generation R Study. Int J Obes. 2008 Jul;32(7):1050–9. doi: 10.1038/ijo.2008.76. [DOI] [PubMed] [Google Scholar]
- 9.Catalano PM, Farrell K, Thomas A, Huston-Presley L, Mencin P, Mouzon D, et al. Perinatal risk factors for childhood obesity and metabolic dysregulation. Am J Clin Nutr. 2009 Nov 1;90(5):1303–13. doi: 10.3945/ajcn.2008.27416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wrottesley SV, Pisa PT, Norris SA. The influence of maternal dietary patterns on body mass index and gestational weight gain in urban black South African women. Nutrients. 2017 Jul 11;9(7) doi: 10.3390/nu9070732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Popkin BM, Gordon-Larsen P. The nutrition transition: worldwide obesity dynamics and their determinants. Int J Obes. 2004;28(S3):S2–9. doi: 10.1038/sj.ijo.0802804. [DOI] [PubMed] [Google Scholar]
- 12.Popkin BM, Adair LS, Ng SW. Now and then: the global nutrition transition: the pandemic of obesity in developing countries. Nutr Rev. 2012 Jan;70(1):3–21. doi: 10.1111/j.1753-4887.2011.00456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.da Cunha J, Maselli LMF, Stern ACB, Spada C, Bydlowski SP. Impact of antiretroviral therapy on lipid metabolism of human immunodeficiency virus-infected patients: old and new drugs. World J Virol. 2015 May 12;4(2):56–77. doi: 10.5501/wjv.v4.i2.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koethe JR, Grome H, Jenkins CA, Kalams SA, Sterling TR. The metabolic and cardiovascular consequences of obesity in persons with HIV on long-term antiretroviral therapy. AIDS Lond Engl. 2016 Jan 2;30(1):83–91. doi: 10.1097/QAD.0000000000000893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maganga E, Smart LR, Kalluvya S, Kataraihya JB, Saleh AM, Obeid L, et al. Glucose metabolism disorders, HIV and antiretroviral therapy among Tanzanian adults. PLOS ONE. 2015 Aug 19;10(8):e0134410. doi: 10.1371/journal.pone.0134410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li N, Sando MM, Spiegelman D, Hertzmark E, Liu E, Sando D, et al. Antiretroviral therapy in relation to birth outcomes among HIV-infected women: a cohort study. J Infect Dis. 2016 Apr 1;213(7):1057–64. doi: 10.1093/infdis/jiv389. [DOI] [PubMed] [Google Scholar]
- 17.Kim RJ, Rutstein RM. Impact of antiretroviral therapy on growth, body composition and metabolism in pediatric HIV patients. Pediatr Drugs. 2010 Jun 1;12(3):187–99. doi: 10.2165/11532520-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 18.Griffiths PL, Johnson W, Cameron N, Pettifor JM, Norris SA. In urban South Africa, 16 year old adolescents experience greater health equality than children. Econ Hum Biol. 2013 Dec;11(4):502–14. doi: 10.1016/j.ehb.2013.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kagura J, Adair LS, Pisa PT, Griffiths PL, Pettifor JM, Norris SA. Association of socioeconomic status change between infancy and adolescence, and blood pressure, in South African young adults: Birth to Twenty Cohort. BMJ Open. 2016 Mar 30;6(3):e008805. doi: 10.1136/bmjopen-2015-008805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.IOM (Institute of Medicine) and NRC (National Research Council) Weight gain during pregnancy: reexamining the guidelines. Washington, DC: The National Academies Press; 2009. [cited 2015 Jun 3]. p. 2. [Internet] Available from: http://www.nap.edu/download.php?record_id=12584. [PubMed] [Google Scholar]
- 21.Nel J, Steyn N. Report on South African food consumption studies undertaken among different population groups (1983 - 2000): average intakes of foods most commonly consumed. Pretoria, South Africa: Department of Health; 2002. [Google Scholar]
- 22.Steyn NP, Senekal M, Norris SA, Whati L, MacKeown JM, Nel JH. How well do adolescents determine portion sizes of foods and beverages? Asia Pac J Clin Nutr. 2006;15(1):35–42. [PMC free article] [PubMed] [Google Scholar]
- 23.Dennis LK, Snetselaar LG, Nothwehr FK, Stewart RE. Developing a scoring method for evaluating dietary methodology in reviews of epidemiologic studies. J Am Diet Assoc. 2003 Apr 1;103(4):483–7. doi: 10.1053/jada.2003.50081. [DOI] [PubMed] [Google Scholar]
- 24.Zingoni C, Norris SA, Griffiths PL, Cameron N. Studying a population undergoing nutrition transition: a practical case study of dietary assessment in urban South African adolescents. Ecol Food Nutr. 2009 Jun;48(3):178–98. doi: 10.1080/03670240902794713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wrottesley SV, Micklesfield LK, Hamill MM, Goldberg GR, Prentice A, Pettifor JM, et al. Dietary intake and body composition in HIV-positive and -negative South African women. Public Health Nutr. 2014 Jul;17(7):1603–13. doi: 10.1017/S1368980013001808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) - A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009 Apr;42(2):377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Villar J, Puglia FA, Fenton TR, Cheikh Ismail L, Staines-Urias E, Giuliani F, et al. Body composition at birth and its relationship with neonatal anthropometric ratios: the newborn body composition study of the INTERGROWTH-21st project. Pediatr Res. 2017 Aug;82(2):305–16. doi: 10.1038/pr.2017.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wrottesley SV, Pisa PT, Micklesfield LK, Pettifor JM, Norris SA. A comparison of body composition estimates using dual-energy X-ray absorptiometry and air-displacement plethysmography in South African neonates. Eur J Clin Nutr. 2016 Jun 1; doi: 10.1038/ejcn.2016.91. [DOI] [PubMed] [Google Scholar]
- 29.Hamill MM, Ward KA, Pettifor JM, Norris SA, Prentice A. Bone mass, body composition and vitamin D status of ARV-naïve, urban, black South African women with HIV infection, stratified by CD4 count. Osteoporos Int. 2013;24(11):2855–61. doi: 10.1007/s00198-013-2373-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Urlando A, Dempster P, Aitkens S. A new air displacement plethysmograph for the measurement of body composition in infants. Pediatr Res. 2003 Mar;53(3):486–92. doi: 10.1203/01.PDR.0000049669.74793.E3. [DOI] [PubMed] [Google Scholar]
- 31.Yao M, Nommsen-Rivers L, Dewey K, Urlando A. Preliminary evaluation of a new pediatric air displacement plethysmograph for body composition assessment in infants. Acta Diabetol. 2003 Oct;40(Suppl 1):S55–58. doi: 10.1007/s00592-003-0027-9. [DOI] [PubMed] [Google Scholar]
- 32.Fomon SJ, Haschke F, Ziegler EE, Nelson SE. Body composition of reference children from birth to age 10 years. Am J Clin Nutr. 1982 May;35(5 Suppl):1169–75. doi: 10.1093/ajcn/35.5.1169. [DOI] [PubMed] [Google Scholar]
- 33.Koo WW, Massom LR, Walters J. Validation of accuracy and precision of dual energy X-ray absorptiometry for infants. J Bone Miner Res Off J Am Soc Bone Miner Res. 1995 Jul;10(7):1111–5. doi: 10.1002/jbmr.5650100716. [DOI] [PubMed] [Google Scholar]
- 34.Crozier SR, Robinson SM, Borland SE, Inskip HM. Dietary patterns in the Southampton Women’s Survey. Eur J Clin Nutr. 2006 Dec;60(12):1391–9. doi: 10.1038/sj.ejcn.1602469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Crozier SR, Inskip HM, Godfrey KM, Robinson SM. Dietary patterns in pregnant women: a comparison of food frequency questionnaires and four-day prospective diaries. Br J Nutr. 2008 Apr;99(4):869–75. doi: 10.1017/S0007114507831746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tielemans MJ, Erler NS, Leermakers ETM, van den Broek M, Jaddoe VWV, Steegers EAP, et al. A priori and a posteriori dietary patterns during pregnancy and gestational weight gain: the Generation R study. Nutrients. 2015 Nov 12;7(11):9383–99. doi: 10.3390/nu7115476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Englund-Ögge L, Brantsæter AL, Sengpiel V, Haugen M, Birgisdottir BE, Myhre R, et al. Maternal dietary patterns and preterm delivery: results from large prospective cohort study. BMJ. 2014 Mar 4;348:g1446. doi: 10.1136/bmj.g1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Starling AP, Sauder KA, Kaar JL, Shapiro AL, Siega-Riz AM, Dabelea D. Maternal dietary patterns during pregnancy are associated with newborn body composition. J Nutr. 2017 May 24; doi: 10.3945/jn.117.248948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Northstone K, Ness AR, Emmett PM, Rogers IS. Adjusting for energy intake in dietary pattern investigations using principal components analysis. Eur J Clin Nutr. 2008 Jul;62(7):931–8. doi: 10.1038/sj.ejcn.1602789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Timmermans S, Steegers-Theunissen RP, Vujkovic M, den Breeijen H, Russcher H, Lindemans J, et al. The Mediterranean diet and fetal size parameters: the Generation R Study. Br J Nutr. 2012 Oct;108(8):1399–409. doi: 10.1017/S000711451100691X. [DOI] [PubMed] [Google Scholar]
- 41.Thompson JMD, Wall C, Becroft DMO, Robinson E, Wild CJ, Mitchell EA. Maternal dietary patterns in pregnancy and the association with small-for-gestational-age infants. Br J Nutr. 2010 Jun;103(11):1665–73. doi: 10.1017/S0007114509993606. [DOI] [PubMed] [Google Scholar]
- 42.Knudsen VK, Orozova-Bekkevold IM, Mikkelsen TB, Wolff S, Olsen SF. Major dietary patterns in pregnancy and fetal growth. Eur J Clin Nutr. 2008 Apr;62(4):463–70. doi: 10.1038/sj.ejcn.1602745. [DOI] [PubMed] [Google Scholar]
- 43.Colón-Ramos U, Racette SB, Ganiban J, Nguyen TG, Kocak M, Carroll KN, et al. Association between dietary patterns during pregnancy and birth size measures in a diverse population in Southern US. Nutrients. 2015 Feb 16;7(2):1318–32. doi: 10.3390/nu7021318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Coelho Nde LP, Cunha DB, Esteves APP, de Lacerda EMA, Filha MMT. Dietary patterns in pregnancy and birth weight. Rev Saúde Pública. 2015 Sep 29;49 doi: 10.1590/S0034-8910.2015049005403. [Internet] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Meas T, Deghmoun S, Armoogum P, Alberti C, Levy-Marchal C. Consequences of being born small for gestational age on body composition: an 8-year follow-up study. J Clin Endocrinol Metab. 2008;93(10):3804–9. doi: 10.1210/jc.2008-0488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mericq V, Martinez-Aguayo A, Uauy R, Iñiguez G, Van der Steen M, Hokken-Koelega A. Long-term metabolic risk among children born premature or small for gestational age. Nat Rev Endocrinol. 2017 Jan;13(1):50–62. doi: 10.1038/nrendo.2016.127. [DOI] [PubMed] [Google Scholar]
- 47.Harder T, Rodekamp E, Schellong K, Dudenhausen JW, Plagemann A. Birth weight and subsequent risk of type 2 diabetes: a meta-analysis. Am J Epidemiol. 2007 Apr 15;165(8):849–57. doi: 10.1093/aje/kwk071. [DOI] [PubMed] [Google Scholar]
- 48.Boney CM, Verma A, Tucker R, Vohr BR. Metabolic syndrome in childhood: association with birth weight, maternal obesity, and gestational diabetes mellitus. Pediatrics. 2005 Mar;115(3):e290–296. doi: 10.1542/peds.2004-1808. [DOI] [PubMed] [Google Scholar]
- 49.Esser N, Legrand-Poels S, Piette J, Scheen AJ, Paquot N. Inflammation as a link between obesity, metabolic syndrome and type 2 diabetes. Diabetes Res Clin Pract. 2014 Aug 1;105(2):141–50. doi: 10.1016/j.diabres.2014.04.006. [DOI] [PubMed] [Google Scholar]
- 50.Shoelson SE, Herrero L, Naaz A. Obesity, inflammation, and insulin resistance. Gastroenterology. 2007 May 1;132(6):2169–80. doi: 10.1053/j.gastro.2007.03.059. [DOI] [PubMed] [Google Scholar]
- 51.Grinspoon S, Carr A. Cardiovascular risk and body-fat abnormalities in HIV-infected adults. N Engl J Med. 2005 Jan 6;352(1):48–62. doi: 10.1056/NEJMra041811. [DOI] [PubMed] [Google Scholar]
- 52.Stanley TL, Grinspoon SK. Body composition and metabolic changes in HIV-infected patients. J Infect Dis. 2012 Jun 1;205(suppl_3):S383–90. doi: 10.1093/infdis/jis205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kuzawa CW, Eisenberg DTA. Intergenerational predictors of birth weight in the Philippines: correlations with mother’s and father’s birth weight and test of maternal constraint. PLOS ONE. 2012 Jul 27;7(7):e40905. doi: 10.1371/journal.pone.0040905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Currie J, Moretti E. Biology as destiny? Short- and long-run determinants of intergenerational transmission of birth weight. J Labor Econ. 2007 Apr 1;25(2):231–64. [Google Scholar]
- 55.Magnus P, Gjessing HK, Skrondal A, Skjærven R. Paternal contribution to birth weight. J Epidemiol Community Health. 2001 Dec 1;55(12):873–7. doi: 10.1136/jech.55.12.873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Simon DM, Vyas S, Prachand NG, David RJ, Collins JW. Relation of maternal low birth weight to infant growth retardation and prematurity. Matern Child Health J. 2006 Jul;10(4):321–7. doi: 10.1007/s10995-005-0053-z. [DOI] [PubMed] [Google Scholar]
- 57.Watson ED, Brage S, White T, Westgate K, Norris SA, Van Poppel MNM, et al. The influence of objectively measured physical activity during pregnancy on maternal and birth outcomes in urban black South African women. Matern Child Health J. 2018 Mar 7; doi: 10.1007/s10995-018-2504-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pearson JT, Watson ED, Lambert EV, Micklesfield LK. The role of physical activity during pregnancy in determining maternal and foetal outcomes. South Afr J Sports Med. 2015;27(4):93–6. [Google Scholar]
- 59.Jiang H, Qian X, Li M, Lynn H, Fan Y, Jiang H, et al. Can physical activity reduce excessive gestational weight gain? Findings from a Chinese urban pregnant women cohort study. Int J Behav Nutr Phys Act. 2012 Feb 9;9:12. doi: 10.1186/1479-5868-9-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Clapp JF. Exercise during pregnancy. A clinical update. Clin Sports Med. 2000 Apr;19(2):273–86. doi: 10.1016/s0278-5919(05)70203-9. [DOI] [PubMed] [Google Scholar]
- 61.Krukowski RA, West DS, DiCarlo M, Shankar K, Cleves MA, Saylors ME, et al. Are early first trimester weights valid proxies for preconception weight? BMC Pregnancy Childbirth. [cited 2017 Jun 2];2016 Nov 21;16 doi: 10.1186/s12884-016-1159-6. [Internet] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Fontaine PL, Hellerstedt WL, Dayman CE, Wall MM, Sherwood NE. Evaluating BMI-specific trimester weight gain recommendations: differences between black and white women. J Midwifery Womens Health. 2012;57(4):327–35. doi: 10.1111/j.1542-2011.2011.00139.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Myer L, Essajee S, Broyles LN, Watts DH, Lesosky M, El-Sadr WM, et al. Pregnant and breastfeeding women: a priority population for HIV viral load monitoring. PLOS Med. 2017 Aug 15;14(8):e1002375. doi: 10.1371/journal.pmed.1002375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Toro-Ramos T, Paley C, Pi-Sunyer F, Gallagher D. Body composition during fetal development and infancy through the age of 5 years. Eur J Clin Nutr. 2015 Dec;69(12):1279–89. doi: 10.1038/ejcn.2015.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.