Abstract
Background
A workforce crisis exists in global surgery. One solution is task‐shifting, the delegation of surgical tasks to non‐physician clinicians or associate clinicians (ACs). Although several studies have shown that ACs have similar postoperative outcomes compared with physicians, little is known about their surgical training. This study aimed to characterize the surgical training and experience of ACs compared with medical officers (MOs) in Tanzania.
Methods
All surgical care providers in Pwani Region, Tanzania, were surveyed. Participants reported demographic data, years of training, and procedures assisted and performed during training. They answered open‐ended questions about training and post‐training surgical experience. The median number of training cases for commonly performed procedures was compared by cadre using Wilcoxon rank sum and Student's t tests. The researchers performed modified content analysis of participants' answers to open‐ended questions on training needs and experiences.
Results
A total of 21 ACs and 12 MOs participated. ACs reported higher exposure than MOs to similar procedures before their first independent operation (median 40 versus 17 cases respectively; P = 0·031). There was no difference between ACs and MOs in total training surgical volume across common procedures (median 150 versus 171 cases; P = 0·995). Both groups reflected similarly upon their training. Each cadre relied on the other for support and teaching, but noted insufficient specialist supervision during training and independent practice.
Conclusions
ACs report similar training and operative experience compared with their physician colleagues in Tanzania.
Abstract
Antecedentes
La falta de cirujanos en determinadas áreas geográficas es flagrante. Una posible solución es el intercambio de tareas, es decir, la delegación de tareas quirúrgicas en personal sanitario no médico o en clínicos asociados (associate clinicians, AC). Si bien varios estudios han demostrado que los AC obtienen resultados postoperatorios similares a los de los médicos, hay poco información acerca de su entrenamiento quirúrgico. Este estudio tuvo como objetivo caracterizar la capacitación quirúrgica y la experiencia de los AC en comparación con los médicos titulados (medical officer, MO) en Tanzania.
Métodos
En este estudio, se encuestaron todos los proveedores de atención quirúrgica de la Región de Pwani, Tanzania. Los participantes proporcionaron datos demográficos, años de entrenamiento y número y tipo de procedimientos realizados y a los que se había asistido durante el periodo de capacitación. Además, respondieron a preguntas abiertas sobre el entrenamiento y su experiencia quirúrgica posterior al entrenamiento. Se comparó la mediana del número de procedimientos más realizados por cada grupo mediante la suma de rangos de Wilcoxon y la prueba de la t de Student. Los investigadores realizaron un análisis del contenido de las respuestas a las preguntas abiertas sobre las necesidades y la experiencia durante la etapa de entrenamiento.
Resultados
En el estudio participaron 21 ACs y 12 MOs. Los CA estuvieron expuestos a un mayor número procedimientos del mismo tipo antes de efectuar su primera operación de forma independiente en comparación con los OM (40 versus 17 casos, P = 0,031). No hubo diferencias en el volumen operatorio total de los procedimientos comunes entre los AC y los MO (150 versus 171 casos, P = 0,995). Las opiniones de los dos grupos sobre el entrenamiento fueron similares. Los dos grupos se dieron soporte entre ellos, pero quedó patente que la supervisión por parte de un especialista durante el entrenamiento y la práctica independiente era insuficiente.
Conclusiones
En Tanzania, los asociados clínicos tienen entrenamientos y experiencias quirúrgicas similares a las de sus colegas médicos.
Introduction
The Lancet Commission on Global Surgery estimates that five billion people lack access to safe and affordable surgical and anaesthesia care worldwide1. The disparity between access to surgical care and need for essential surgery is most pronounced in low‐ and middle‐income countries (LMICs), especially in sub‐Saharan Africa1. This is due in part to shortages in human resources for health in the region. A minimum workforce density of 20 surgeons, obstetricians and anaesthetists per 100 000 population is needed to ensure access to safe and affordable surgical care1. In Tanzania, there are just 0·35 surgeons,
obstetricians and anaesthetists per 100 000 population, compared with 64·56 per 100 000 population in the USA2, 3.
Task‐shifting represents one solution to the global surgical workforce crisis. Task‐shifting is defined by the WHO as ‘the rational redistribution of tasks among health workforce teams … from highly qualified workers to health workers with shorter training and fewer qualifications in order to make more efficient use of the available human resources for health’4. The scope of practice and training of non‐physician clinicians (NPCs), also known as associate clinicians (ACs), is variable across different countries. Some act solely as assistants to physicians (task‐sharing), whereas others provide a full range of services independent of direct physician supervision (task‐shifting). Although this method of labour reallocation is present in most healthcare systems worldwide, its application to surgical care is unique to sub‐Saharan Africa. In some hospitals in Malawi, Mozambique and Tanzania, ACs perform 75 per cent or more of all basic and essential surgical procedures5, 6, 7. ACs are faster and cheaper to train, are more likely to work and remain working in rural areas where need is greatest, and have similar obstetric and non‐obstetric outcomes compared with physician counterparts6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, with rare exception19.
Despite supporting evidence, concerns remain about adequacy of training of non‐specialist surgical care providers20, 21. For instance, Choo and colleagues20 found that medical officers (MOs) in Ghana had limited experience in performing surgical procedures under supervision despite providing most of the surgical care at district hospitals throughout the country. No studies have specifically investigated case volumes or experience of ACs during surgical training. Training practices are important to understand in established systems of task‐shifting in order to determine provider preparedness for independent practice and to identify potential areas for improvement within educational systems. Such findings could inform the practical implementation of surgical task‐shifting programmes, and enhance safety and sustainability. The present study aimed to characterize and compare the education and training of the physician and non‐physician surgical workforce in Pwani Region, Tanzania, through quantification of surgical experience during training and analysis of provider perceptions of preparedness for independent practice.
Methods
Tanzania was selected as the site for this study owing to its long history of training and utilizing ACs to deliver medical and surgical care. Currently, four cadres of surgical care provider exist in Tanzania: clinical officers (COs), assistant medical officers (AMOs), MOs and surgeons (Table 1)2, 22. In Tanzania, COs are graduates of secondary school who have completed 3 years of additional training to provide medical and minor surgical care. High‐performing COs with several years of clinical experience are selected to attend 2 years of AMO school, where they are trained to perform basic obstetric and general surgical procedures. For this analysis, COs and AMOs were grouped together as ACs. MOs are physicians who have completed medical school and 1 year of general internship, during which they receive some training in surgery. In Tanzania, MOs often perform surgical procedures, but differ from ACs in that their formal training in surgery occurs after medical school during internship. MOs have more in‐depth exposure to medical knowledge through classes in anatomy and other subjects. Both ACs and MOs differ from specialist surgeons in that they do not have the breadth and depth of surgical training found in a formal residency programme.
Table 1.
| Cadre | Schooling | Postgraduate training | Scope of surgical practice |
|---|---|---|---|
| Clinical officer | Secondary school, clinical officer school (3 years) | On the job | + |
| Assistant medical officer | Secondary school, clinical officer school (3 years), AMO school (2 years) | On the job | +++ |
| Medical officer | Secondary school, medical school (5 years) | General internship (1 year); on the job | +++ |
| Specialist surgeon | Secondary school, medical school (5 years) | Surgical residency (3–4 years) | +++++ |
Over the past two decades, Tanzania has implemented a series of healthcare reforms to increase the workforce of skilled healthcare providers, resulting in a sevenfold increase in physicians trained annually compared with 199223. A 2017 survey23, however, found neither a net increase in the population nor an increase in the geographical distribution of doctors practising in Tanzania. Today, most physicians practise in urban settings, leaving a majority of the population with a minority of the doctors23. Thus, training more physicians is not enough in Tanzania. Increased focus on retention and alternative solutions such as task‐shifting is critical as well.
This study was conducted in Pwani Region, Tanzania, one of the poorest regions in the country24. At the time of the study, there were five district hospitals, one mission hospital and one regional referral hospital in operation, serving a population of 1·1 million individuals25.
Survey methodology and ethics
Written surveys tailored to the training experience of each cadre were created with overlapping themes and identical questions to allow cross‐comparison. The surveys consisted of 48 questions for ACs, 55 questions for MOs, and 47 questions for surgeons (Appendices [Link], [Link], [Link], supporting information).
Each survey included questions on demographic data, educational history, self‐reported numbers of procedures assisted and performed at each level of training, and current surgical activity. Participants were questioned specifically about the first operation they performed independently and how many of the same procedure they were exposed to during training before this operation. The surveys also included open‐ended questions aimed at understanding the experience of training through descriptions of on‐the‐job training experiences, reflections on early operative experiences, queries about decision‐making and barriers to patient care, and questions about teaching and mentorship practices. By using a combination of closed and open‐ended questions it was possible to obtain a more comprehensive understanding of the experience of training and operating independently, as case numbers do not fully explain the experience and adequacy of training. All care providers performing surgery at the seven hospitals in Pwani Region were contacted in person and surveyed on‐site by one author. Anonymity was guaranteed regarding the analysis and publication of results.
Muhimbili University of Health and Allied Sciences Directorate of Research and Publications Committee, the Tanzania Commission for Science and Technology, and the University of California, San Francisco Committee on Human Research approved the study. Written informed consent was obtained for all study participants before inclusion.
Statistical analysis
The numbers of procedures assisted and performed throughout training were quantified by procedure type. χ2, Fisher's exact, Wilcoxon rank sum and Student's t tests were used as appropriate to compare AC and MO demographics, total operative experiences during training, and experience performing the six most common procedures, including caesarean section, hydrocelectomy, inguinal hernia repair, exploratory laparotomy, appendicectomy and hysterectomy. These procedures were identified based on previous research performed by this research team in Pwani11. Providers were also asked about total experience with other procedures, including bowel resection and anastomosis, cholecystectomy, mastectomy, prostatectomy, splenectomy and colostomy.
Analyses were performed using Stata® 14.0 (StataCorp, College Station, Texas, USA). Two‐sided P < 0·050 was considered to indicate statistical significance. Missing data from responders were excluded from analysis. Open‐ended responses were analysed using modified conventional content analysis26. Responses from both cadres of providers were collated into one document. One author reviewed the text three times and then performed close reading with open coding and memoing to identify patterns in responses, emphasizing words and concepts used repeatedly by respondents. These repeated words and concepts were clustered and named as resultant themes. Themes were compared between ACs and MOs. Quotations that were deemed characteristic of the identified themes or otherwise interesting were identified and presented separately.
Results
All 34 surgical care providers completed the surveys, representing 100 per cent of the surgical workforce at the time of the study. Twelve providers were MOs, 21 were ACs, and one was a specialist surgeon. The response from the single specialist surgeon, who functioned mostly in an administrative role, was excluded to protect anonymity.
Both cadres of provider were mostly men (Table 2). ACs were older (P < 0·001) and had been in practice for 7 years longer than MOs (P = 0·008).
Table 2.
Demographics and years of experience of associate clinicians and medical officers
| Associate clinician (n = 21) | Medical officer (n = 12) | P † | |
|---|---|---|---|
| Age (years)* | 46 (43–51) | 33 (30–40) | < 0·001 |
| Sex ratio (M : F) | 18 : 3 | 9 : 3 | 0·374‡ |
| Time from completion of formal training (years)* | 11 (6–12) | 4 (2–4) | 0·008 |
| Time at current hospital (years)* | 10 (3–16) | 3 (2–8) | 0·057 |
| Time from first independent operation (years)* | 11 (4–18) | 4 (2–8) | 0·058 |
Values are median (i.q.r.).
Wilcoxon rank sum test, except
Fisher's exact test.
Operative experience
There was no difference in case volume by specific procedure (assisted and performed under supervision) for ACs and MOs before independent practice (Fig. 1). Although the number of caesarean sections assisted during training between ACs and MOs was similar (25 (i.q.r. 10–40) versus 18 (15–24) respectively; P = 0·329), ACs performed significantly fewer under supervision (5 (2–20) versus 40 (7–46) respectively; P = 0·005). For total operative experience, there was no difference in the number of procedures between ACs and MOs during training (150 (97–206) versus 171 (102–188); P = 0·995) (Table 3). The number of assisted procedures, procedures performed under supervision, and the total operative exposure during training were similar between cadres (Table 3).
Figure 1.
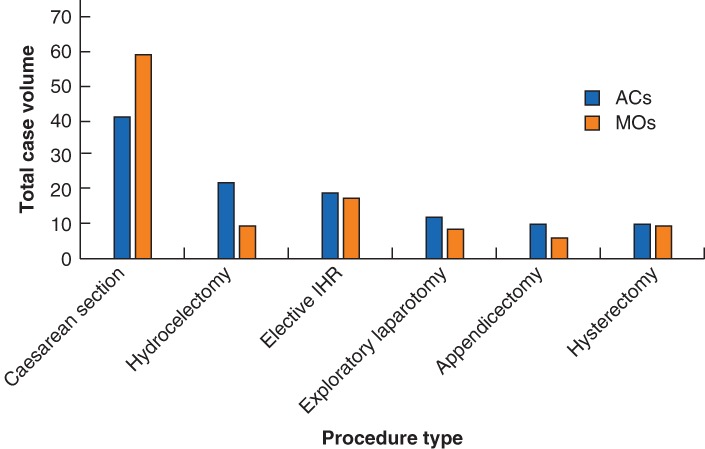
Operative participation by associate clinicians and medical officers during their entire training Values are median number of procedures assisted and performed under supervision by the 12 associate clinicians (ACs) and 21 medical officers (MOs). IHR, inguinal hernia repair.
Table 3.
Total number of procedures assisted and performed under supervision during training
| Associate clinician | Medical officer | P * | |
|---|---|---|---|
| Assisted | 123 (81–158) | 98·5 (70–110) | 0·089 |
| Supervised | 37 (11–47) | 61 (11–99) | 0·224 |
| Total | 150 (97–206) | 171 (102–188) | 0·995 |
Values are median (i.q.r.).
Wilcoxon rank sum test.
In general, AC training case volume occurred equally across formal and informal on‐the‐job training (75 (i.q.r. 44–103) formal versus 63 (24–124) informal cases; P = 0·753), whereas most MO training case volume occurred during the formal school curriculum, with fewer postgraduate on‐the‐job cases (112 (80–182) formal versus 7 (1–51) informal cases; P < 0·001).
Before their first independent operations, ACs had significantly higher exposure to similar operations than MOs (40 (24–55) versus 17 (13–44) cases respectively; P = 0·031) (Table 4).
Table 4.
Similar operations performed before first independent operation
| Associate clinician | Medical officer | P * | |
|---|---|---|---|
| Assisted | 30 (15–50) | 13 (10–35) | 0·075 |
| Supervised | 6 (3–12) | 4 (2–6) | 0·143 |
| Total | 40 (24–55) | 17 (13–44) | 0·031 |
Values are median (i.q.r.).
Wilcoxon rank sum test.
Operative experience of bowel resection and anastomosis, cholecystectomy, mastectomy, prostatectomy, splenectomy and colostomy was limited. The median operative experience for each of these procedures was fewer than seven for each cadre of providers.
Qualitative analysis
Similar themes arose from the survey responses of ACs and MOs. Four themes were identified: interdependence during training and practice; early independence with limited supervision; care limitations due to inexperience and infrastructural deficiencies; and desire for continuing education. These themes were consistent throughout the educational histories of the participants.
Interdependence during training and practice
Qualitative analysis demonstrated fluidity and cooperation between the different provider cadres during training, with both cadres learning from, teaching and supervising each other. Nine of the 21 ACs noted significant involvement of MOs in their on‐the‐job education, and seven of the 12 MOs stated they were trained by ACs extensively during their internship and on‐the‐job training. Intraoperative supervision was performed by both cadres, for both cadres, with participants noting a mix of supervisors during their first operations, from COs up to specialist surgeons. MOs, however, noted more specialist surgeon involvement in their formal internship training compared with ACs. MOs noted a high level of independence after internship, and four of the 12 MOs received no additional on‐the‐job training at their first posting (Table 5, quotation 1).
Table 5.
Interdependence during training and practice
| 1 | I do things on my own at the expense of many patients not making it. It's painful and frustrating. You constantly think about the patient … Main teacher but only showed me one when I assisted and I was expected to do on my own. Never performed under supervision. | MO |
| 2 | Yes, I teach new ACs or MOs who are just starting. We give a surgical orientation because internship is not enough training for them to know how to do surgery. We even teach COs to do surgery. I was taught by a CO. | AC |
| 3 | In the old days, it was only me and one other AC doing procedures. We teach others so we don't have to work as hard. | MO |
MO, medical officer; AC, associate clinician; CO, clinical officer.
Once operating independently, ACs and MOs both took up the role of teaching students of each provider cadre. Sixteen of 21 ACs trained MOs during their career, and five of the 12 MOs stated that they trained ACs at their hospital (Table 5, quotations 2 and 3). Both cadres also noted interdependence when required to operate outside their comfort zone (Table 6, quotation 2, and Table 7, quotation 5).
Table 6.
Early independence with limited supervision
| 1 | The first time I assisted a surgery, I felt dizzy like I was going to collapse. This first procedure I did went OK, I knew what I was doing because I had assisted a lot of C sections. I didn't know what it would feel like to be a surgeon. | MO |
| 2 | When you see procedures, you think they are simple but when you do them, you find some are simple and some are complex. Last week, I had to call an AC into the OR who has more experience than me. | MO |
| 3 | I was scared because I had to do the surgeries alone. Even anaesthesia said, ‘Where's the surgeon?’ I was sweating and nervous. At one point, I almost called my boss to help me but it went OK. I followed my first patients very closely. I even visited the patients at home. I am now an expert in hernia. | AC |
| 4 | Sometimes the procedure looks easy when you are assisting; when you perform you are really sweating, with time, your hands become flexible. | AC |
| 5 | I had a patient who bled after a C section and the uterus was torn. I was scared … I kept clamping things and they kept bleeding. I was fumbling and then I finally controlled the bleeding. I was afraid – I thought the patient might die. | MO |
| 6 | One time, I had difficulty and had to do a hysterectomy. The patient was bleeding but it went OK. I had never done that before and had only seen three. | AC |
| 7 | I started to operate independently. It was difficult. I came across a hernia and it was direct not indirect. I couldn't find the sac, and that was my first time to come across this. I had only read about it in a book and I didn't have anyone to ask. I just did a Bassini repair. I learned so much from that procedure – you think an operation is simple then it's different than you expect, and you have to be prepared. | AC |
| 8 | Only did C section in internship, assisted on lots of other cases … It takes a long time for someone to be qualified in surgery. MDs have more technical knowledge, ACs have experience. | MO |
MO, medical officer; AC, associate clinician; OR, operating room.
Table 7.
Care limitations due to inexperience and infrastructural deficiencies
| 1 | Here, our main issue is anaesthesia care. Sometimes I have to leave the operating theatre to control anaesthesia, patient is not asleep during operation, have to do two things at once, it's very difficult. Sometimes we are pushed to operate because the patient is going to die without the operation. | AC |
| 2 | We have no specialists, they won't come to a district hospital, poor instruments, didn't plan this area as a theatre, buildings are poor, scrub area is poor. | AC |
| 3 | No anaesthetist, need more trained staff, need better equipment, suction machine not working, power goes off and we have no generator, do most laps without suction, hard to control bleeding when you have no lights, can't see. I'm a surgeon, paediatrician, and health secretary. | AC |
| 4 | Poor equipment and infrastructure, have to operate with the window open, no anaesthetist, just got a machine last week but no one can operate it, sterility is a problem in the theatre and ward and leads to wound infections. | MO |
| 5 | I usually just have to do it. I watch YouTube, call for assistance, we go in pairs. When you come here, you are an MD, everybody is looking at you and people expect you to do surgery when you haven't been taught. We learn at the expense of the patient. My early patients were not so lucky though now I'm more comfortable and my patients are luckier. | MO |
| 6 | You are forced to do things to help the patients, because you can't refer them to MNH [Muhimbili National Hospital in Dar es Salaam]. We are very far; patient could die on the way and sometimes relatives refuse to transfer the patient … I have to have courage, I can't leave or transfer the patient, because it won't help them. | AC |
| 7 | Difficult to refer cases because [my hospital] is geographically isolated and patients have low SES, need to operate to prevent complications. | MO |
AC, associate clinician; MO, medical officer; SES, socioeconomic status.
Early independence with limited supervision
Early independent surgical experiences were similar for the two groups. Although almost all participants reflected that their first independent operation went well, there were consistent reports across both cadres of these operations being stressful and of cases not being as simple as they thought they were during training (Table 6, quotations 1–4).
Both groups noted difficulties and complications early, probably related to their relative inexperience (Table 6, quotations 5–8), but felt they learned from each of these cases and improved. In general, both cadres started with simple cases and progressed to more complex procedures, relying on former classmates and colleagues (both ACs and MOs) when they needed assistance (Table 6, quotation 2, and Table 7, quotation 5). Throughout these reflections on early challenges, both groups demonstrated passion for surgery, noting a love for the profession, yearning for improvement and expressing care for patient outcomes.
Despite relative inexperience, members of both groups were required to perform operations without supervision early on owing to personnel and resource constraints. Half of the MOs operated independently within 1 month of the start of their internship. Nine of 21 ACs and eight of the 12 MOs operated independently immediately upon arrival at their first posting.
Care limitations due to infrastructural deficiencies and inexperience
Participants commonly cited limited resources at their respective hospitals, including lack of safe anaesthesia and intensive care, suboptimal surgical tools and sterilization, and few well trained support staff (Table 7, quotations 1–4). This forced providers to take on multiple roles, distracting from surgical practice (Table 7, quotations 1 and 3).
Even with more experience later during their careers, limited exposure to certain cases remained a barrier to high‐quality care. Both cadres of providers felt uncomfortable performing laparotomy and hysterectomy. Members of both groups also noted a preference to transfer patients with orthopaedic and abdominal trauma due to complexity, but had reservations about transfer time and the risks of referral. For emergency patients, these providers felt compelled to operate outside their comfort zone given limited specialist availability and the alternative of detrimental transit times and possible loss to follow‐up (Table 7, quotations 1, 5 and 7). For difficult cases, both cadres sought assistance from colleagues (ACs and MOs), and consulted other sources including telemedicine, books, YouTube® (San Bruno, California, USA) and surgical specialists (when available) (Table 7, quotation 5). Such support systems, however, were not always available, and many providers noted having no specialists around to assist in or guide their care (Table 7, quotations 2 and 5).
Desire for continuing education
All surveyed ACs and MOs noted a need for continuing education. Throughout the survey, participants endorsed discomfort handling certain situations and a need for hands‐on training from specialists. Despite this, few of the participants noted the existence of continuing education exercises beyond weekly rounds. Both groups were split over whether such programmes should be held at their respective hospitals or at outside institutions (Table 8, quotations 1 and 2). Both ACs and MOs noted that in‐house training would be more reflective of their day‐to‐day experiences and resource constraints, with less financial burden upon the institution. Many, however, also had a desire to train at outside institutions, where they would be free from distracting patient obligations and exposed to new and more complex cases that they did not get much experience with at their home hospitals.
Table 8.
Desire for continuing education
| 1 | It would be better to attend a workshop in another place, because there are better teachers other places with more experience and you get exposure to different things. | AC |
| 2 | Better to have sessions at [home hospital], because outside the environment is different. | MO |
AC, associate clinician; MO, medical officer.
Discussion
This study described the training and experience of the surgical workforce in Pwani Region, Tanzania. The results indicate that ACs had similar operative experience during training compared with MOs. Reflections of the study participants demonstrated that, in Tanzania's current system of task‐shifting, there is cooperation and fluidity between these two cadres of provider, but insufficient supervision during training and limited to no access to specialist surgeons. Both groups reflected similarly upon their preparation to operate independently, early operative experiences, limitations to current practice, and needs for continuing medical education.
Opponents of task‐shifting suggest that non‐physician providers are trained inadequately or inferior at surgical management compared with physicians21. This study questions these concerns, demonstrating similar training experience for MOs and ACs in Tanzania, in line with this team's previous research in Pwani Region11, which showed equivalent surgical outcomes for physician and non‐physician providers, further supporting the safety of surgical task‐shifting. Neither MOs nor non‐physician clinicians (ACs) have surgical training comparable to that of a specialist surgeon27, 28. Thus, both are clear examples of task‐shifting.
Interestingly, AC surgical training cases occurred equally across formal training and informal ‘on‐the‐job’ training, whereas MOs had the highest volume of operative experience during their formal internship training and less while on the job. Although medical education for physicians is comprehensive, their postgraduate surgical experience appears to be more limited than that of their non‐physician counterparts in Tanzania. The precise mix of clinical knowledge and technical skills needed in modern surgical training is still a matter of debate. A recent study29 compared training experience and surgical outcomes of non‐university‐trained surgeons and university‐trained surgeons in the USA. It found significant differences in training case patterns but no difference in operative outcomes between the two groups. Although specialist surgeons are ideal care providers as they have both the requisite knowledge and experience, this study demonstrates that ACs and MOs can work synergistically to meet both requirements in systems where the supply of surgeons is limited.
Increasingly, assessing quality of care has become a focus of global health delivery30. Measures of surgical care quality and outcomes in LMICs are currently inadequate30. Increasing access to surgical care is a main goal of global surgery, but this must be done in conjunction with monitoring outcomes and measures to ensure quality. The concept of quality in surgical care delivery has important applications to this study. Although ACs and MOs had a similar volume of training cases, it was impossible to assess the quality of the training each group received. Furthermore, the case volume for both cadres, though similar, may be inadequate. The precise volume of training cases required to attain proficiency for essential surgical procedures is unknown, but neither group attained the minimum case volume required for graduation from general surgery residency in the USA31. The authors recommend that global surgery programmes utilizing task‐shifting for training closely follow patient‐level outcomes to assure care quality.
Although this study found no difference in the training of MO and AC surgical providers, ethical concerns are raised about the early independence and limited supervision of both groups. In both cadres, reports of early complications and feeling compelled to operate outside the comfort zone were common. In addition, most providers were not comfortable managing all essential surgical conditions, including two of the three bellwether procedures, laparotomy and open fracture management. The bellwether procedures are often used as benchmarks to indicate ‘the presence of resources needed to treat an appropriate range of surgical conditions at first‐level hospitals … to ensure delivery of emergency and essential surgical care’32. Greater supervision during training and enhanced availability of specialist surgeons during practice should be prioritized to increase capability in provision of essential surgical care. Currently, universal availability of a specialist at each district hospital is unrealistic. Steps such as implementation of telemedicine systems to assist decision‐making, incentives for specialists to do rural rotations, and continuing education programmes could, however, be used to improve supervision during training and during management of complex cases that cannot be safely referred to regional hospitals. Expanded formal training for ACs and MOs at a regional referral hospital could help increase preparedness for a greater variety of complicated surgical conditions. Periodic provider rotation to training hospitals could ensure continuous exposure to complex cases. Specialist providers along with multidisciplinary teams, including anaesthetists and nurses, could also rotate periodically to district hospitals to provide continuing education via lectures, simulation and hands‐on training. Finally, further expansion of educational programmes for ACs to emphasize medical knowledge, and for MOs to emphasize surgical training, may help improve quality.
Despite similar training and outcomes between ACs and MOs, the volume of surgery is still exceedingly low in Pwani Region, with just 461 procedures per 100 000 population, or 7·5 per cent of the estimated need of 6145 per 100 000 population in this region of Africa1, 11. Across all obstetric and non‐obstetric major surgical procedures, this was equivalent to 70 procedures per care provider during the year11. This is much lower than expected productivity for a surgical care provider, indicating that the extra productivity allotted by an additional cadre of providers is not adequate on its own. Deficiencies in material resources, anaesthesia, nursing and support staff, along with patient access challenges, are probably contributing as well. Thus, retention and support programmes for physician providers and more equitable geographical distribution of specialists must be implemented in conjunction with policies that address systemic resource deficits and patient‐level barriers to surgical care23, 33. Surgical task‐shifting is but one solution to the insufficient provision of surgical care in low‐resource settings.
This study certainly has limitations. The retrospective nature of the survey may have resulted in recall bias, which prevented more granular evaluation of differences in AC and MO training. Future research could be performed to quantify training experience prospectively through maintenance of case logs, which would improve comprehension of the depth and breadth of surgical training in Tanzania. Such monitoring would simultaneously function to improve surgical education and patient safety as well. The internal validity of the present study is high, as all surgical service providers in Pwani Region were included. The external validity is less clear, as the study was restricted to only one of Tanzania's 20 regions. Many MOs and ACs are trained centrally, so formal training experiences are probably comparable to those of providers outside Pwani Region. The on‐the‐job training and experiences, however, may differ between rural and urban settings. It is likely that the situation in other rural parts of Tanzania is similar. Future research could analyse this on a national or regional level.
Disclosure
The authors declare no conflict of interest.
Supporting information
Appendix S1. Surgical training and educational needs survey for assistant medical officers
Appendix S2. Surgical training and educational needs survey for medical officers
Appendix S3. Surgical training and educational needs survey for surgeons
Presented in abstract form to a meeting of the West African College of Surgeons, Banjul, The Gambia, February 2018, and the Global Surgery Conference, Stockholm, Sweden, October 2018
Funding information
Department of Surgery, University of California, San Francisco
References
- 1. Meara JG, Leather AJ, Hagander L, Alkire BC, Alonso N, Ameh EA et al Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet 2015; 386: 569–624. [DOI] [PubMed] [Google Scholar]
- 2. The Lancet Commission on Global Surgery . Global Indicator Initiative – Dataset: Indicator 2; 2017. https://www.lancetglobalsurgery.org/indicators [accessed 28 May 2019].
- 3. Marks IH, Kamali P, Khan MA, Tahboub H, Cairney Hill J, Zaim C et al. Data for the Sustainable Development of Surgical Systems: a Global Collaboration; 2016. http://docs.wixstatic.com/ugd/346076_c853bd6c09d34ed6bca4b9b622d69de3.pdf [accessed 17 September 2017].
- 4. Global Health Workforce Alliance . Task Shifting: Global Recommendations and Guidelines; 2008. https://www.who.int/workforcealliance/knowledge/resources/taskshifting_guidelines/en/ [accessed 17 September 2017].
- 5. Kruk ME, Wladis A, Mbembati N, Ndao‐Brumblay SK, Hsia RY, Galukande M et al Human resource and funding constraints for essential surgery in district hospitals in Africa: a retrospective cross‐sectional survey. PLoS Med 2010; 7: e1000242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wilhelm TJ, Thawe IK, Mwatibu B, Mothes H, Post S. Efficacy of major general surgery performed by non‐physician clinicians at a central hospital in Malawi. Trop Doct 2011; 41: 71–75. [DOI] [PubMed] [Google Scholar]
- 7. Pereira C, Mbaruku G, Nzabuhakwa C, Bergström S, McCord C. Emergency obstetric surgery by non‐physician clinicians in Tanzania. Int J Gynaecol Obstet 2011; 114: 180–183. [DOI] [PubMed] [Google Scholar]
- 8. Mullan F, Frehywot S. Non‐physician clinicians in 47 sub‐Saharan African countries. Lancet 2007; 370: 2158–2163. [DOI] [PubMed] [Google Scholar]
- 9. Nyamtema AS, Pemba SK, Mbaruku G, Rutasha FD, van Roosmalen J. Tanzanian lessons in using non‐physician clinicians to scale up comprehensive emergency obstetric care in remote and rural areas. Hum Resour Health 2011; 9: 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. McCord C, Mbaruku G, Pereira C, Nzabuhakwa C, Bergstrom S. The quality of emergency obstetrical surgery by assistant medical officers in Tanzanian district hospitals. Health Aff (Millwood) 2009; 28: w876–w885. [DOI] [PubMed] [Google Scholar]
- 11. Beard JH, Oresanya LB, Akoko L, Mwanga A, Mkony CA, Dicker RA. Surgical task‐shifting in a low‐resource setting: outcomes after major surgery performed by nonphysician clinicians in Tanzania. World J Surg 2014; 38: 1398–1404. [DOI] [PubMed] [Google Scholar]
- 12. Chilopora G, Pereira C, Kamwendo F, Chimbiri A, Malunga E, Bergström S. Postoperative outcome of caesarean sections and other major emergency obstetric surgery by clinical officers and medical officers in Malawi. Hum Resour Health 2007; 5: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wilson A, Lissauer D, Thangaratinam S, Khan KS, MacArthur C, Coomarasamy A. A comparison of clinical officers with medical doctors on outcomes of caesarean section in the developing world: meta‐analysis of controlled studies. BMJ 2011; 342: d2600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chu KM, Ford NP, Trelles M. Providing surgical care in Somalia: a model of task shifting. Confl Health 2011; 5: 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Tyson AF, Msiska N, Kiser M, Samuel JC, Mclean S, Varela C et al Delivery of operative pediatric surgical care by physicians and non‐physician clinicians in Malawi. Int J Surg 2014; 12: 509–515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chao TE, Sharma K, Mandigo M, Hagander L, Resch SC, Weiser TG et al Cost‐effectiveness of surgery and its policy implications for global health: a systematic review and analysis. Lancet Glob Health 2014; 2: e334–e345. [DOI] [PubMed] [Google Scholar]
- 17. Milland M, Bolkan H. Surgical task shifting in Sierra Leone: a controversial attempt to reduce maternal mortality. BJOG 2015; 122: 155. [DOI] [PubMed] [Google Scholar]
- 18. Bolkan HA, van Duinen A, Waalewijn B, Elhassein M, Kamara T, Deen GF et al Safety, productivity and predicted contribution of a surgical task‐sharing programme in Sierra Leone. Br J Surg 2017; 104: 1315–1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hounton SH, Newlands D, Meda N, De Brouwere V. A cost‐effectiveness study of caesarean‐section deliveries by clinical officers, general practitioners and obstetricians in Burkina Faso. Hum Resour Health 2009; 7: 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Choo S, Perry H, Hesse AA, Abantanga F, Sory E, Osen H et al Surgical training and experience of medical officers in Ghana's district hospitals. Acad Med 2011; 86: 529–533. [DOI] [PubMed] [Google Scholar]
- 21. Galukande M, Kaggwa S, Sekimpi P, Kakaire O, Katamba A, Munabi I et al Use of surgical task shifting to scale up essential surgical services: a feasibility analysis at facility level in Uganda. BMC Health Serv Res 2013; 13: 292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. United Republic of Tanzania . Ministry of Health Curriculum for Assistant Medical Officer; 2000. http://www.almc.habari.co.tz/amo/AMO_Curriculum.pdf [accessed 17 September 2017].
- 23. Sirili N, Kiwara A, Gasto F, Goicolea I, Hurtig AK. Training and deployment of medical doctors in Tanzania post‐1990s health sector reforms: assessing the achievements. Hum Resour Health 2017; 15: 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. United Republic of Tanzania . Coast Region Socioeconomic Profile; 2007. http://www.tanzania.go.tz/regions/COAST.pdf [accessed 17 September 2017].
- 25. United Republic of Tanzania . Basic Demographic and Socio‐Economic Profile, Pwani Region, 2012. http://tanzania.countrystat.org/fileadmin/user_upload/countrystat_fenix/congo/docs/2012%20Tanzania%20Population%20and%20Housing%20Census‐Basic%20Demographic%20and%20Socio‐Economic%20Profile.pdf [accessed 17 September 2017].
- 26. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005; 15: 1277–1288. [DOI] [PubMed] [Google Scholar]
- 27. Bergström S, McPake B, Pereira C, Dovlo D. Workforce innovations to expand the capacity for surgical services In Disease Control Priorities. Volume 1: Essential Surgery (3rd edn), Debas HT, Donkor P, Gawande A, Jamison DT, Kruk ME, Mock CN, eds. World Bank Publications: Washington, 2015; 307–316. [PubMed] [Google Scholar]
- 28. Beard JH, Ohene‐Yeboah M, deVries CR, Schecter WP. Hernia and hydrocele In Disease Control Priorities. Volume 1: Essential Surgery (3rd edn), Debas HT, Donkor P, Gawande A, Jamison DT, Kruk ME, Mock CN, eds. World Bank Publications: Washington, 2015; 151–172. [Google Scholar]
- 29. Sellers MM, Keele LJ, Sharoky CE, Wirtalla C, Bailey EA, Kelz RR. Association of surgical practice patterns and clinical outcomes with surgeon training in university‐ or nonuniversity‐based residency program. JAMA Surg 2018; 153: 418–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Akachi Y, Kruk ME. Quality of care: measuring a neglected driver of improved health. Bull World Health Organ 2017; 95: 465–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Accreditation Council for Graduate Medical Education . Defined Category Minimum Numbers for General Surgery Residents and Credit Role https://www.acgme.org/Portals/0/DefinedCategoryMinimumNumbersforGeneralSurgeryResidentsandCreditRole.pdf [accessed 17 September 2017].
- 32. O'Neill KM, Greenberg SL, Cherian M, Gillies RD, Daniels KM, Roy N et al Bellwether procedures for monitoring and planning essential surgical care in low‐ and middle‐income countries: caesarean delivery, laparotomy, and treatment of open fractures. World J Surg 2016; 40: 2611–2619. [DOI] [PubMed] [Google Scholar]
- 33. Goodell AJ, Kahn JG, Ndeki SS, Kaale E, Kaaya EE, Macfarlane SB. Modeling solutions to Tanzania's physician workforce challenge. Glob Health Action 2016; 9: 31597. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Surgical training and educational needs survey for assistant medical officers
Appendix S2. Surgical training and educational needs survey for medical officers
Appendix S3. Surgical training and educational needs survey for surgeons


