Abstract
Emergency airway management is one of the vital resuscitative procedures undertaken in the emergency department (ED). Despite its clinical and research importance in the care of critically ill and injured patients, earlier studies have documented suboptimal intubation performance and high adverse event rates with a wide variation across the EDs. The optimal emergency airway management strategies remain to be established and their dissemination to the entire nation is a challenging task. This article reviews the current published works on emergency airway management with a focus on the use of airway management algorithms as well as the importance of first‐pass success and systematic use of rescue intubation strategies. Additionally, the review summarizes the current evidence for each of the important airway management processes, such as assessment of the difficult airway, preparation (e.g., positioning and oxygenation), intubation methods (e.g., rapid sequence intubation), medications (e.g., premedications, sedatives, and neuromuscular blockades), devices (e.g., direct and video laryngoscopy and supraglottic devises), and rescue intubation strategies (e.g., airway adjuncts and rescue intubators), as well as the airway management in distinct patient populations (i.e., trauma, cardiac arrest, and pediatric patients). Well‐designed, rigorously conducted, multicenter studies that prospectively and comprehensively characterize emergency airway management should provide clinicians with important opportunities for improving the quality and safety of airway management practice. Such data will not only advance research into the determination of optimal airway management strategies but also facilitate the development of clinical guidelines, which will, in turn, improve the outcomes of critically ill and injured patients in the ED.
Keywords: Airway management, emergency department, rapid sequence intubation, rescue intubation, video laryngoscopy
Introduction
Emergency airway management is a central part of emergency medicine practice. The first priority for managing an acutely unstable patient is securing the airway. Approximately 0.5–1% of emergency department (ED) patients require intubation for various conditions, such as respiratory failure, cardiac arrest, and altered mental status.1, 2, 3 Emergency airway management in the ED is often challenging for the emergency physician because multiple ED‐specific factors, for example, vomiting, facial/neck trauma, immobilized cervical spine, and chest compression for resuscitation, contribute to intubation success and failure. To achieve rapid and successful intubation for these high‐risk ED patients, understanding the current evidence on emergency airway management is essential.
Until the 1990s, emergency airway management had been carried out based on the evidence in the anesthesia field. The milestone of emergency airway management is the foundation of the National Emergency Airway Registry (NEAR) – a multicenter registry that aims to prospectively characterize the emergency airway management practices in the EDs across North America.4, 5, 6, 7, 8 Since its inception, the knowledge based on other large multicenter registries, including the Korean Emergency Airway Management Registry (KEAMR) and Japanese Emergency Airway Network (JEAN) registry,6, 9, 10 have also advanced the ED airway management, in parallel to the advent of intubation techniques and devices, such as rapid sequence intubation (RSI),6, 7, 8 video laryngoscopies (VLs),11, 12, 13 and supraglottic devices.14, 15, 16, 17 Consequently, the performance of emergency airway management with the use of these approaches is indicative of the competence of emergency physicians managing the critically ill.
The current evidence on emergency airway management emphasizes the importance of first‐pass success,9, 18, 19, 20 refuting multiple intubation attempts for patients who require an intubation in the ED. Indeed, failed first intubation attempts are associated with a higher risk of adverse events, higher failure rates at the subsequent attempts, lower probability of return of spontaneous circulation (ROSC) during the early resuscitation, and prolonged time to achieve ROSC.9, 18, 19, 20, 21 Despite its importance, studies have shown that the first‐pass success rate varies across the countries and is suboptimal in Japanese EDs. For example, in large multicenter registries, the first‐pass success rates were 83% in North America (from NEAR),8 in South Korea (from KEAMR),22 and 71% in Japan (from JEAN).10 Furthermore, there was a high degree of variation in the first‐pass success rates across the Japanese EDs, ranging from 40% to 83%.10
Systematic preparation and assessment for difficult airways are the keys for achieving successful intubations. The current evidenced‐based algorithms are based primarily on anesthesia experiences23 targeting elective intubations, and hence might not be applicable to ED patients with various conditions (e.g., cardiac arrest).24 Additionally, emergency physicians might not have sufficient time to obtain medical history or to thoroughly assess the airway before an intubation attempt because of time pressure and the patient's condition.25
In this context, this article reviews current published works on emergency airway management with a focus on the importance of first‐pass success, the use of airway management algorithms, and preparation, as well as the systematic use of rescue intubation strategies.
Airway management algorithm and difficult airways
Several algorithms have been proposed for emergency airway management17, 26, 27, 28 based on the universal emergency airway algorithm (Fig. 1).29 The purpose of the algorithm is neither a tool for decision of intubation nor a “cookbook” that describes the procedures for intubation. The goals of the algorithm are to promote rapid decision‐making, reduce errors, and improve the quality of airway management.29 In emergency airway management, identification of the difficult airway is a crucial step to achieve first‐pass success and avoid encountering a “cannot intubate, cannot ventilate” situation.6, 18, 19, 30 The presence of difficult airway is a key branch point to achieve safe, successful intubation (Fig. 1).
Figure 1.
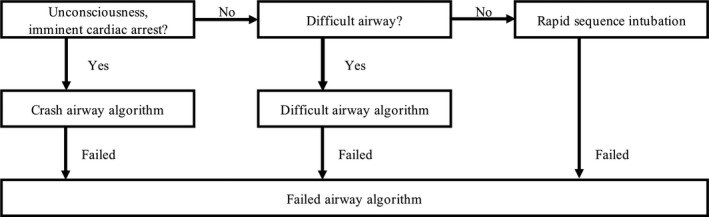
Universal airway algorithm. This algorithm shows how the emergency airway algorithms work together. The upper stage is the main algorithm. If the patient is in imminent cardiac arrest or unresponsive, it shifts to the crash airway algorithm. If a difficult airway is suspected, it shifts to the difficult airway algorithm. When these algorithms cannot succeed, it shifts to the failed airway algorithm.
Definition of difficult airway
Although the impact of a difficult airway is widely recognized, there are no standardized definitions for difficult airway in the ED setting. As the definition of difficult airway varies across studies, the incidence of the difficult airway is as wide as 2% to 27%.31, 32, 33, 34, 35, 36, 37, 38 Difficult airway is generally divided into several dimensions:29 (i) difficult laryngoscopy, (ii) difficult bag‐mask ventilation, (iii) difficult extraglottic devices (EGD), (iv) difficult cricothyroidotomy. Of these, a particularly important dimension is difficult laryngoscopy.
Difficult laryngoscopy
The level of intubation difficulty depends on the degree of glottic view with laryngoscopy. Cormack and Lehane (C‐L) grade is the most widely used system to categorize the degree of visualization of larynx with laryngoscopy. The C‐L grades 3 and 4 are highly correlated with difficult or failed intubations.29 However, as identification of the C‐L grade needs to insert the laryngoscopy, clinicians should estimate the level of intubation difficulty before attempting the intubation.
Prediction of difficult laryngoscopy in the ED
According to the latest meta‐analysis of prediction of difficult laryngoscopy in the operating room, the upper lip bite test is the best predictor.23 If the lower incisors cannot bite the upper lip at all (class 3), the likelihood of difficult laryngoscopy will be very high (positive likelihood ratio of 14, specificity of 0.96).23 As for the widely used Mallampati score, the positive likelihood ratio was 4 with the specificity of 0.87 in the Mallampati class 3–4.23 However, ED patients who require airway management are frequently unable to follow commands (e.g., patients with cardiac arrest and altered mental status). Indeed, studies have shown that the Mallampati score were measured in only 30% of patients who underwent intubation in the ED.25, 39 Therefore, the difficult laryngoscopy assessment tool for the ED setting should be concise and can be undertaken without patient cooperation. The LEMON criteria devised by the National Emergency Airway Management Course are an assessment system with consideration for the use in the resuscitation room (Table 1).29 However, the original LEMON criteria included the Mallampati score; a modified LEMON criteria excluding this score has been proposed36 and validated externally.37 This modified LEMON criteria is concise, and the absence of any items in the criteria indicates the absence of difficult laryngoscopy with a high sensitivity (85.7%) and negative predictive value (98.2%).31
Table 1.
“LEMON” mnemonic for predicting difficult laryngoscopy
| L – Look externally | Look at the patient externally for characteristics that are known to cause difficult laryngoscopy, intubation, or ventilation |
| E – Evaluate the 3‐3‐2 rule | Inter‐incisor distance: at least patient's three fingerbreadths |
| Hyoid mental distance: at least patient's three fingerbreadths | |
| Thyroid to floor of mouth distance: at least patient's two fingerbreadths | |
| M – Mallampati | The hypopharynx views are graded by the Mallampati classification: class I, soft palate, uvula, fauces, and pillars visible; class II, soft palate, uvula, and fauces visible; class III, soft palate and base of uvula visible; and class IV, only hard palate visible |
| O – Obstruction | Any condition that can cause an obstruction of the airway makes laryngoscopy and ventilation difficult. Such conditions are epiglottis, tumors, abscesses, and trauma |
| N – Neck mobility | Patients in hard‐collar neck immobilization have no neck movement are therefore harder to intubate |
Preparation
Sufficient preparation in emergency airway management includes identifying the difficult airway (see “Airway management algorithm” and “Difficult airway”), developing an airway management plan, and assembling all necessary personnel, equipment, and medications. Table 2 shows the mnemonic “STOP‐MAID” to help clinicians remember the tools and steps for intubation.40 The preparation also includes the rescue methods for failed intubations.
Table 2.
“STOP‐MAID” mnemonic for preparation in emergency airway management
| S | Suction |
| T | Tools for intubation (laryngoscope blades, handle) |
| O | Oxygen |
| P | Positioning |
| M | Monitors, including electrocardiography, pulse oximetry, blood pressure, EtCO2, and esophageal detectors |
| A | Assistant; Ambu‐bag with face mask; airway devices (different sized endotracheal tubes 10 mL syringe, stylets); assessment of airway difficulty |
| I | Intravenous access |
| D | Drugs for pretreatment, induction, neuromuscular blockade (and any adjuncts) |
Preoxygenation
Desaturation and subsequent hypoxemia during intubation are associated with serious complications (e.g., myocardial ischemia and unfavorable neurological outcomes).41, 42, 43 The main goals of preoxygenation are to extend the duration of safe apnea and to prevent hypoxemia during the apneic phase of intubation.
Preoxygenation method: Unsupported ventilation
Preoxygenation is typically carried out with tidal volume breathing (i.e., normal depth and rate of ventilation) for at least 3 min, or with vital capacity breaths (i.e., eight deep breaths over 1 min). Oxygen sources without pressure support, also referred to as unsupported ventilation, include facemask with reservoir, bag valve mask (BVM), and adjunctive nasal cannula. A facemask with reservoir is the most frequently used oxygen source for preoxygenation in the ED,42 while it delivers only 60–70% FiO2 at flow rates of 15 L/min. A BVM with functional one−way valves connected to a reservoir is used for preoxygenation. In patients with adequate spontaneous ventilation, it is not necessary to squeeze the bag, but a tight mask seal must be achieved to deliver high FiO2. By contrast, in patients with inadequate spontaneous ventilation, preoxygenation should be undertaken using gentle positive pressure ventilation with BVM. In the intensive care unit (ICU) setting, patients receiving ventilation with BVM during the interval between induction and laryngoscopy had higher oxygen saturations and lower rates of severe hypoxemia than those receiving no ventilation.44
Preoxygenation method: Apneic oxygenation
Apneic oxygenation uses nasal cannula to supply oxygen to the nasopharynx during intubation to maintain oxygenation in the absence of patient respiratory effort. The practice could reduce the incidence of hypoxemia during intubation and improve the first‐pass success rate in the ED.45
Proper positioning
Although intubation is commonly undertaken in the supine position, recent published reports suggest that elevating the patient's head to a more upright position (20–45°) could improve preoxygenation, increase the probability of first‐pass success, and decrease intubation‐related adverse events (e.g., hypoxemia).46, 47, 48, 49
Non‐invasive ventilation
Non‐invasive ventilation (NIV) should be considered in cases where sufficient oxygenation cannot be achieved with unsupported ventilation and there are no contraindications (e.g., respiratory arrest or altered mental status). Preoxygenation with NIV increases end‐expiratory lung volume due to the alveolar recruitment induced by positive airway pressure and maximizes the efficacy of preoxygenation efforts. Although limited evidence exists in the ED, the rate of severe hypoxemia was lower in NIV delivered by facemask compared with standard BVM for preoxygenation in patients with acute hypoxemic respiratory failure.50
High‐flow nasal cannula
A high‐flow nasal cannula provides heated and fully humidified gas mixtures to patients through a nasal cannula interface. High‐flow nasal cannula delivers continuous high gas flow resulting in higher FiO2 than with standard oxygen, and maintains oxygenation during the apneic phase of intubation. As high‐flow nasal cannula is a relatively recent development, its benefit for preoxygenation remains controversial.51, 52, 53
Delayed sequence intubation
Delayed sequence intubation has been proposed as an alternative to RSI for the use in patients with altered mental status preventing adequate preoxygenation.54 The technique of delayed sequence intubation temporally separates the administration of induction agents from that of neuromuscular blockades (NMBs) to allow adequate pre‐intubation oxygenation and preparation. Ketamine is the currently preferred induction agent because of its dissociative properties and established safety margins. A prospective observational study found that delayed sequence intubation allowed the provision of preoxygenation and denitrogenation to patients who were intolerant of traditional means of preoxygenation.55
Intubation methods
Rapid sequence intubation
Selecting an appropriate intubation method, such as RSI or non‐RSI (e.g., intubation with sedatives or intubation without medications), is critical and the intubator needs to consider not only the patient condition but also the environmental factors, including the available equipment (e.g., rescue devices) and pharmacologic agents, and staffing (e.g., experienced intubators). Rapid sequence intubation is the standard method in emergency airway management for patients without an anticipated difficult airway.40 The technique involves the simultaneous administration of a sedative and NMB. In the prehospital setting, the more inclusive term of “drug‐assisted intubation” is widely used for any use of medications to facilitate tracheal intubation, with or without the use of NMB (i.e., intubation with the use of NMB is RSI). Studies indicate that RSI is more successful than intubation with sedatives alone both in the prehospital and ED settings. For example, compared to the non‐RSI methods, RSI has consistently shown a higher success rate and lower or equal adverse event rate in patients without difficult airway characteristics in the ED.7, 56, 57, 58 Nevertheless, the rate of RSI use in ED patients varies across countries: 85% in North America,59 in South Korea,22 and 53% in Japan:60 Moreover, in Japan, the rate of RSI use also varied across the EDs, ranging from 0% to 79% in 2010–2011.10 Rapid sequence intubation is the standard method for emergency airway management, but non‐RSI is an appropriate choice in some cases (including patients with a difficult airway) by allowing the patient to maintain respiratory drive (Airway Management Algorithm and Difficult Airway for the prediction of difficult airway). The medications frequently used for RSI are summarized in Table 3.
Table 3.
Medications for airway management in the emergency department
| Medications | Dose | Onset | Duration of action | Beneficial characteristics | Potential adverse effects | Major indications |
|---|---|---|---|---|---|---|
| Premedication should be given 2–3 min before intubation | ||||||
| Lidocaine | 1.5 mg/kg | NA | NA | Reduce intracranial and bronchospastic response† by intubation | Potential cardiac arrest in patients with a high‐grade atrioventricular block |
Head injury Unknown mechanism injury with an elevated ICP |
| Fentanyl | 1–3 μg/kg given over 30–60 s | NA | NA | Reduce sympathetic response |
Respiratory depression Hypotension |
Elevated ICP Cardiovascular disease |
| Sedatives | ||||||
| Etomidate‡ | 0.3 mg/kg | 15–45 s | 3–12 min |
Rapid onset and short acting Limited effects on hemodynamics |
Potential adrenocortical suppression Myoclonus Neuroexcitation |
Most commonly used for emergency RSI Not used for the maintenance of sedation after intubation |
| Ketamine | 1–2 mg/kg | 45–60 s | 10–20 min |
Reduction in airway resistance Catecholamine release |
Increased blood pressure and heart rate |
Hemodynamically stable patient with severe bronchospasm Septic shock Used for non‐RSI for patients with an expected difficult airway |
| Midazolam | 0.1–0.3 mg/kg | 30–60 s | 15–30 min |
Amnesic properties Anticonvulsant effects |
Hypotension Respiratory depression |
May be used for post‐intubation sedation |
| Propofol | 1.5–3 mg/kg | 15–45 s | 5–10 min |
Rapid onset and short acting Reduction in airway resistance |
Myocardial depression and peripheral vasodilation Dose‐related hypotension |
Obstructive airway diseases Status epilepticus Post‐intubation sedation |
| Thiopental | 3 mg/kg | <30 s | 5–10 min | Cerebroprotective and anticonvulsive |
Vasodilation and myocardial depression Relatively contraindicated in reactive airway disease |
Rarely used |
| Neuromuscular blockades | ||||||
| Succinylcholine | 1.5 mg/kg | 45 s | 5–9 min | Rapid onset and offset, and short acting |
Absolutely contraindicated in patients with malignant hyperthermia history, neuromuscular disease, and hyperkalemia Stroke, onset of >72 h Rhabdomyolysis Burn, onset of >72 h Denervation syndrome |
Essentially all patients except contraindication |
| Rocuronium | 1 mg/kg | 45–60 s | 45 min |
Rapid onset and long acting Reversal by sugammadex |
Caution with difficult airway | If succinylcholine contraindicated |
Little evidence to support the use of lidocaine with a goal of reducing bronchospasm.
Not approved in Japan.
RSI, rapid sequence induction; ICP, intracranial pressure; NA, not applicable.
Surgical intubation
When a successful intubation cannot be achieved by laryngoscopy and available adjuncts, a surgical intubation, such as cricothyroidotomy61 and transtracheal needle ventilation must be carried out.62, 63
Supportive techniques
Recent reports have supported the use of ultrasonography to confirm the correct and timely placement of an endotracheal tube.64, 65 Ultrasound enables us to identify sonoanatomy of the upper airway and facilitates the assessment of airway anatomy for difficult intubation, tube placement and depth, and assessment of airway size.64
Although cricoid pressure had been used to reduce the risk of aspiration during intubation, it may be unnecessary to undertake RSI safely.66, 67 Likewise, there is no concrete evidence on the use of the backward, upward, rightward pressure (BURP) method to improve the glottis view during intubation.68, 69, 70
Medications
Except for several specific conditions (e.g., cardiac arrest), the use of premedications, sedatives, and NMBs are used to optimize intubation conditions (e.g., glottic visualization and immobilization), mitigate physiologic responses, protect patients from intubation‐related adverse events (e.g., tachycardia) and reflexive actions (e.g., gagging, coughing) during intubation, and provide sedation and amnesia. The characteristics of each medication are summarized in Table 3.
Premedications
Premedication is generally given at least 3 min prior to intubation. In critical cases, the premedication can be given <3 min before the intubation, or omitted entirely. Lidocaine is used for reducing the risk of bronchospasm when β2 agonist therapy has not been given.40 Fentanyl can mitigate the cardiovascular effects of sympathetic nervous system stimulation but has a potential risk of hypotension.71 Of note, atropine is not used for premedication in adults but it should be available as a rescue medication if bradycardia occurs.
Sedatives
A short‐acting i.v. drug with sedative or combined sedative, analgesic, and amnestic properties is necessary for intubation. Although etomidate is frequently used for intubation in North America, it is not approved in some countries (e.g., Japan).26 In this case, ketamine is considered a good alternative to etomidate.72, 73 Benzodiazepines (e.g., midazolam) are widely used in Japan,21 and can be used as an infusion for long‐term sedation. Propofol is also a commonly used sedative but it can cause cardiovascular depression leading to hypotension.74
Neuromuscular blockades
Succinylcholine has a rapid onset property but is contraindicated in several conditions, such as patients with burn, musculoskeletal crush injury, spinal cord injury, or renal failure (Table 3). Rocuronium has been increasingly used given its advantages, including rapid onset action, minimal adverse effects, broader eligibility than succinylcholine, and capability of rapid reversal using sugammadex.8, 60 A recent large observational study reported no differences in the first‐pass success rate and intubation‐related adverse events between succinylcholine and rocuronium use for RSI in the ED.75
Devices
Direct laryngoscopy and VL
Direct laryngoscopy (DL) has been used as the standard device for intubation over decades, but the evolution of VL has advanced airway management.7, 8, 22, 60, 76, 77, 78, 79, 80, 81, 82, 83 Table 4 summarizes the advantages and disadvantages of VL in comparison with DL. Studies have reported the superiority of VL over DL in the ED. More specifically, compared to DL use, VL use is associated with a better laryngeal visualization, higher first‐pass success rate, shorter time to successful intubation, and lower rate of intubation‐related adverse events (e.g., esophageal intubation) in general ED patients,8, 60, 76, 77, 81, 82 and patients with trauma,22 difficult airway,78, 79 and cardiac arrest.83 Furthermore, the use of VL is also associated with a lower force to oral structures84, 85, 86, 87 regardless of the experience of the intubator.60, 80, 82 In Japan, the rate of VL use on the first intubation attempt has increased from 2% in 2010 to 40% in 2016.60
Table 4.
Advantages and disadvantages of video laryngoscopy over direct laryngoscopy
| Advantages | Disadvantages |
|---|---|
|
Improved laryngeal view in patients with a limited mouth opening, neck mobility, or difficult airway Faster time to achieve a successful intubation Useful tool for teaching and training in airway education Lower risk at inducing local tissue injury Permitting others to share of the view and help facilitate intubations Higher overall and first success rate, especially in difficult airway, cardiac arrest, and intubations by less experienced providers Lower risk of esophageal intubation |
Variable learning curve and multiple devices available requiring different skills Obscured view by fogging, secretions, or blood in the airway Loss of depth perception Expensive cost |
Adjunct devices
Extraglottic devices
Extraglottic devices (e.g., laryngeal masks and laryngeal tubes) provide effective oxygenation and ventilation without entering the trachea. Extraglottic devices can be used as a “transitional” device, until a definitive airway is established, when intubation cannot be successfully achieved or the patient has a difficult airway.
Bougie
The tracheal tube introducer, also known as the bougie, is used to facilitate intubation in patients with poor laryngoscopic views. When the bougie is used, it is generally in combination with RSI, and can be used in conjunction with DLs, VLs, or fiberoptic intubation devices. In particular, the bougie is beneficial when the epiglottis is visible but the vocal chords cannot be visualized.88 A recent randomized controlled trial found that the use of a bougie, compared with a tracheal tube and stylet, resulted in a significantly higher first‐pass success rate among patients undergoing emergency airway management.89, 90
Rescue intubation
As discussed above, although first‐pass success is the primary goal of emergency airway management, the rate of failed first intubation attempts remains high, at 17–32% in the ED.6, 7, 8, 10, 18, 60, 91 Therefore, early and systematic rescue intubation approaches should be prepared in advance of the first intubation attempt (e.g., use of alternative methods, devices, and change in intubators). Figure 1 shows the airway algorithm.
Rescue methods
Rapid sequence intubation is not only the primary method but also the principal backup method when the initially utilized intubation method fails in the ED.4, 9, 18 Studies using large multicenter registries have reported that RSI was used in 20% of first rescue intubation attempts18 and was a factor associated with a higher second‐attempt success rate.91 When a failed airway occurs and oxygenation cannot be maintained, immediate rescue cricothyrotomy is indicated. Rescue surgical methods, including cricothyrotomy, are required in 0.2–0.5% of all emergency intubations in the ED.6, 7, 10, 60
Devices
Video laryngoscopy has become the first choice of intubation in the ED,8, 60 instead of DL. Video laryngoscopy generally improves the view of the glottis, without the need to align the airway axes to achieve a direct view from outside the patient's mouth, and can be considered as a rescue device. Nevertheless, the superiority of VL over DL for rescue intubation remains controversial.9, 76, 92, 93
Adjuncts (EGDs and bougie):
Extraglottic devices
As summarized in “Devices”, EGDs (e.g., laryngeal masks and laryngeal tubes) should be prepared in advance of initiating an intubation. Extraglottic devices are used as rescue devices after a failed intubation attempt to provide oxygenation and ventilation until a definitive airway is established. Although the use of EGDs as rescue devices is infrequent practice in the ED, emergency physicians should be familiar with the EGDs.4, 18
Bougie
As summarized in “Devices”, a bougie is an alternative device for rescue intubation. Bougies are used to facilitate intubation in patients with poor laryngoscopic views or after a failed intubation attempt.
Intubators
In the ED, emergency physicians play major roles on emergency airway management, including those requiring rescue techniques. The international anesthesia consensus recommends the use of alternative approaches, such as use of experienced intubators for subsequent intubation attempts after a failed first attempt.33 It is clinically plausible that an experienced intubator is likely to intubate more successfully than a novice intubator. This approach is also supported by the data from a large multicenter registry. For example, second intubation attempts by a single intubator, compared with those by alternate intubators, were associated with a decreased success rate.94 Likewise, rescue intubation by emergency physicians or senior physicians is also associated with a higher probability of success at the second attempt.91
Special circumstance: Patients with trauma
One of the priorities in critically injured patients in the ED is intubation with the aim to protect the airway, deliver sufficient oxygen, and maintain adequate ventilation. Approximately 10–30% of intubations in the ED were undertaken for patients with trauma,3, 8, 60 with a first‐pass success rate ranging from 64% to 86%.22, 95, 96, 97, 98, 99, 100
Specific issues in patients with trauma
Intubation for patients with trauma is challenging due to its urgency, anatomical distortion, oral secretion and blood, the risk of vomiting, and hemodynamic instability.101, 102 Additionally, all critically injured patients should be treated as having a cervical spine injury until proven otherwise, which also makes the intubation more difficult by inhibiting the optimal positioning for intubation. To overcome these challenges, several approaches have been proposed.
Intubation methods
Rapid sequence intubation (see also Intubation methods above) has been recommended for patients with trauma by both international and Japanese clinical practice guidelines unless difficult laryngoscopy is anticipated.103, 104 Rapid sequence intubation is used for patients with trauma in up to 85% in North America,1, 103 whereas that is used in 36% in Japan.95
Medications
Similar to airway management in the general ED population, etomidate, ketamine, propofol, and midazolam are commonly used sedatives for patients with trauma (see Medications).105 Ketamine has a preferable cardiorespiratory safety profile.106, 107 Ketamine has been considered contraindicated in patients with head trauma due to the concern of increasing intracranial pressure,108 but the current evidence to refute ketamine use is not strong.109, 110, 111, 112 Reports have suggested that ketamine does not reduce regional glucose metabolism or augment oxygen consumption but could benefit patients with an intracranial injury by a catecholamine‐mediated increase in cerebral perfusion. Propofol and benzodiazepines have been used for hemodynamically stable patients with trauma with a caution for their negative inotropic effects. Neuromuscular blockade is used as a part of RSI, for example, succinylcholine has been the first choice for patients with trauma due to its rapid onset action and short half‐life.103
Devices
Although the use of VL has been increasing in the ED,8, 60 there is a concern for the vulnerability of VL in patients with trauma where the airway could be contaminated by blood and vomitus.113 Although VL can provide better a glottic visualization compared to DL,92 VL should be used cautiously in this patient population according to the clinical practice guidelines for trauma management.103, 104
Special circumstance: Cardiac arrest
In the ED, up to 40% of intubations were carried out in patients with cardiac arrest.3, 8, 22, 60 Although the best intubation strategy during cardiopulmonary resuscitation (CPR) has not been established,114, 115 intubation is considered the definitive method to secure the airway.116, 117, 118 However, the conditions unique to this population, for example, continuous chest compression during CPR116, 117, 119, 120 and regurgitation, successful emergency airway management is a challenge. Indeed, studies have reported that the first‐pass success rate ranges from 36% to 94% and the adverse events rate ranges from 9% to 27% in this population,9, 83, 121, 122, 123, 124 and that patients with failed first intubation attempts have a lower probability of achieving ROSC, prolonged time to achieve ROSC, and decreased probability of ROSC during the first 15 min compared to those who had a first‐pass success.9
Devices
The use of VL in patients with cardiac arrest could improve the first‐pass success rate and minimize the chest compression interruption when compared to DL.83, 124 For example, in the recent multicenter study from Japan, the use of VL was associated with an increased first‐pass success rate compared to DL among novice intubators, but not among experienced intubators. Similar findings have been reported in single‐center studies from South Korea.123, 124
Intubators
The experience of the intubator affects first‐pass success.122 Experienced intubators have a higher first‐pass success rate compared to inexperienced intubators (82% versus 36%) in patients with cardiac arrest.122 Therefore, the clinical practice guidelines recommend intubation for patients with cardiac arrest should be carried out by a highly skilled intubator.116, 117 Although the definition of experience intubator is not standardized, >240 intubation experiences were expected to achieve a 90% success rate without a prolonged chest compression interruption (<10 s) and complication.122
Special circumstance: Children
As intubation for children is a rare event (e.g., 2–33/10,000 ED visits),125, 126, 127, 128 emergency physicians are likely unfamiliar with airway management in children. Additionally, the highly stressed clinical situation within limited resources might further contribute to low success rates and errors, such as miscalculation for medication doses.129 Indeed, the first‐pass success rate in children aged <18 years was 60% (and 50% in children aged <2 years) in Japanese EDs,130 whereas the rate was 74% in overall ED patients.60 In other studies, the first‐pass success rates in children varied from 39% to 78%.56, 125, 128, 131, 132, 133 Furthermore, published works have shown that the intubator's experience plays a major role in first‐pass success in children. Pediatric emergency medicine attending physicians had a higher success rate (89%), compared with pediatric emergency medicine fellows (43%) and pediatric residents (35%).132
Specific issues in children
The principles of airway management for children in the ED are the same as for adults. The major challenges for airway management in children are largely attributable to age‐related issues, including the airway anatomy, choice of intubation devices and tubes, and the calculation for appropriate dose of medications. To promptly secure the airway, length‐based resuscitation tape (e.g., Broselow pediatric emergency tape) should be used to determine the appropriate equipment sizes and medication doses.134, 135, 136, 137
To successfully achieve intubation, emergency physicians must consider unique pediatric features. In children, the lower functional residual volume and higher oxygen metabolism cause hypoxia more quickly than adults.29, 138 Although it has been reported that RSI improves the success rate in children similar to adults,56, 130 intubation without RSI (e.g., awake intubation with preserved spontaneous respiration) is undertaken more frequently compared to adults.56, 128, 130, 139 Additionally, apneic oxygenation was associated with a lower risk of hypoxemia during intubation of children in the ED.140
Difficult airway in children
Although there is limited evidence on airway management for children in the ED, approximately 9% of children had difficult airway (required three or more attempts by attending or fellow providers) in the pediatric ICU setting.38 Infants and young children have relatively large oropharyngeal structures (i.e., tongue, tonsils, and adenoids) and occiput, which lead to an upper airway obstruction. Additionally, the larger and floppier epiglottis and superior laryngeal position make visualization of the vocal chords difficult.29, 138 History of difficult airway and signs of upper airway obstruction have been reported as a risk factor of difficult airway.38
Summary and future directions
In 1998, Walls and colleagues founded the NEAR.4, 5, 6, 7, 8 Their data not only provided high‐quality evidence on emergency airway management in the earlier decades, but also revealed the competence of emergency physicians in the care of critically ill and injured patients in the ED. Their findings have defined the role of emergency physicians and proved their worth, thereby playing a pivotal role in the history of emergency medicine in the USA.141
Over the past decade, the NEAR group has also made a substantial impact on the international emergency medicine research community, including the KEAMR22, 91, 142, 143 and JEAN groups.10, 13, 18, 19, 21, 31, 58, 60, 71, 73, 94, 95, 130, 144, 145, 146, 147 For example, the JEAN study is a multicenter prospective effort that is run by the Japanese Emergency Medicine Network (JEMNet) (http://jemnet.asia/wp/). JEAN has enrolled >10,000 children and adults across geographically diverse EDs in Japan, and comprehensively characterized emergency airway management with a >95% capture rate. During this decade, the JEAN study has significantly contributed to airway management research by determining, for example, the association of multiple intubation attempts with a higher risk of intubation‐related adverse events,19 the association of repeated intubation attempts by a single intubator with a decreased success rate,94 and overall improvement in the airway management performance in Japanese EDs in the 2010s.60 These findings underscore the importance of first‐pass success and support strategies to maximize the probability of first‐pass success as well as the systematic use of rescue intubation strategies.
Yet, despite the ubiquitous presence of current emergency medicine practice, many fundamental questions on emergency airway management remain to be elucidated. For example, what are the optimal intubation techniques to achieve the best outcome in different patient populations who require emergency airway management? What are the minimal competency thresholds for resident physicians and board‐certified emergency physicians? These important knowledge gaps provide many opportunities for further investigations. Ideal randomized controlled trials (i.e., randomized experiments with a well‐defined treatment, full adherence to the assigned treatment, double‐blind assignment, and no loss to follow‐up) has been considered as “the gold standard” to establish the causal relations between a treatment (e.g., airway management strategy) and patient outcome. Yet, such trials are methodologically and logistically challenging in the ED setting. Additionally, published works have also shown that subjects who are enrolled into the controlled trial framework could be systematically different from general populations.148 Alternatively, high‐quality observational data reflect the natural setting of a real population and clinical practice, and hence enhance the generalizability of inferences. Furthermore, the recent advent of causal models with the use of counterfactual concepts (e.g., g‐methods including marginal structural models) have enabled us to robustly infer causal relations between a specific airway management technique and patient outcomes using observational data (i.e., without data from a randomized controlled trial).149
We believe that, in collaborative efforts between research teams that are adept at generating high‐quality science,82, 84, 86, 150, 151, 152, 153, 154 such investigations will provide emergency physicians with important opportunities for improving the quality and safety of airway management practice. For researchers and professional organizations, the gained knowledge will not only advance research into the determination of optimal airway management strategies but also facilitate the development of high‐quality clinical guidelines as well as their dissemination to the EDs nationally, which will, in turn, improve the outcomes of critically ill and injured patients in the ED.
Disclosure
Approval of the research protocol: N/A.
Informed consent: N/A.
Registry and the registration no. of the study/trial: N/A.
Animal studies: N/A.
Conflict of interest: None.
Funding information
No funding information provided.
References
- 1. Sakles JC, Laurin EG, Rantapaa AA, Panacek EA. Airway management in the emergency department: a one‐year study of 610 tracheal intubations. Ann. Emerg. Med. 1998; 31: 325–32. [DOI] [PubMed] [Google Scholar]
- 2. Wongyingsinn M, Songarj P, Assawinvinijkul T. A prospective observational study of tracheal intubation in an emergency department in a 2300‐bed hospital of a developing country in a one‐year period. Emerg. Med. J. 2009; 26: 604–8. [DOI] [PubMed] [Google Scholar]
- 3. Kerslake D, Oglesby AJ, Di Rollo N et al Tracheal intubation in an urban emergency department in Scotland: a prospective, observational study of 3738 intubations. Resuscitation 2015; 89: 20–4. [DOI] [PubMed] [Google Scholar]
- 4. Bair AE, Filbin MR, Kulkarni RG, Walls RM. The failed intubation attempt in the emergency department: analysis of prevalence, rescue techniques, and personnel. J. Emerg. Med. 2002; 23: 131–40. [DOI] [PubMed] [Google Scholar]
- 5. National Emergency Airway Registry. [cited 1 Mar 2019]. Available from: http://www.nearstudy.net.
- 6. Sagarin MJ, Barton ED, Chng YM, Walls RM, National Emergency Airway Registry I . Airway management by US and Canadian emergency medicine residents: a multicenter analysis of more than 6,000 endotracheal intubation attempts. Ann. Emerg. Med. 2005; 46: 328–36. [DOI] [PubMed] [Google Scholar]
- 7. Walls RM, Brown CA 3rd, Bair AE, Pallin DJ, Investigators NI. Emergency airway management: a multi‐center report of 8937 emergency department intubations. J. Emerg. Med. 2011; 41: 347–54. [DOI] [PubMed] [Google Scholar]
- 8. Brown CA 3rd, Bair AE, Pallin DJ, Walls RM, Investigators NI . Techniques, success, and adverse events of emergency department adult intubations. Ann. Emerg. Med. 2015; 65: 363–70. e361. [DOI] [PubMed] [Google Scholar]
- 9. Kim J, Kim K, Kim T et al The clinical significance of a failed initial intubation attempt during emergency department resuscitation of out‐of‐hospital cardiac arrest patients. Resuscitation 2014; 85: 623–7. [DOI] [PubMed] [Google Scholar]
- 10. Hasegawa K, Hagiwara Y, Chiba T et al Emergency airway management in Japan: Interim analysis of a multi‐center prospective observational study. Resuscitation 2012; 83: 428–33. [DOI] [PubMed] [Google Scholar]
- 11. Butler JM, Clancy M, Robinson N, Driscoll P. An observational survey of emergency department rapid sequence intubation. Emerg. Med. J. 2001; 18: 343–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Brown CA 3rd, Bair AE, Pallin DJ, Laurin EG, Walls RM, National Emergency Airway Registry I . Improved glottic exposure with the Video Macintosh Laryngoscope in adult emergency department tracheal intubations. Ann. Emerg. Med. 2010; 56: 83–8. [DOI] [PubMed] [Google Scholar]
- 13. Okamoto H, Goto T, Wong ZSY et al Comparison of video laryngoscopy versus direct laryngoscopy for intubation in emergency department patients with cardiac arrest: a multicentre study. Resuscitation 2018; 136: 70–7. [DOI] [PubMed] [Google Scholar]
- 14. Rosenberg MB, Phero JC, Becker DE. Essentials of airway management, oxygenation, and ventilation: part 2: advanced airway devices: supraglottic airways. Anesth. Prog. 2014; 61: 113–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wang HE, Szydlo D, Stouffer JA et al Endotracheal intubation versus supraglottic airway insertion in out‐of‐hospital cardiac arrest. Resuscitation 2012; 83: 1061–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wang HE, Schmicker RH, Daya MR et al Effect of a strategy of initial laryngeal tube insertion vs endotracheal intubation on 72‐hour survival in adults with out‐of‐hospital cardiac arrest: a randomized clinical trial. JAMA 2018; 320: 769–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sun F, Wang Y, Ma S et al Clinical consensus of emergency airway management. J. Thorac. Dis. 2017; 9: 4599–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Goto T, Gibo K, Hagiwara Y et al Multiple failed intubation attempts are associated with decreased success rates on the first rescue intubation in the emergency department: a retrospective analysis of multicentre observational data. Scand. J. Trauma Resusc. Emerg. Med. 2015; 23: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hasegawa K, Shigemitsu K, Hagiwara Y et al Association between repeated intubation attempts and adverse events in emergency departments: an analysis of a multicenter prospective observational study. Ann. Emerg. Med. 2012; 60: 749–54. e742. [DOI] [PubMed] [Google Scholar]
- 20. Sakles JC, Chiu S, Mosier J, Walker C, Stolz U. The importance of first pass success when performing orotracheal intubation in the emergency department. Acad. Emerg. Med. 2013; 20: 71–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Inoue A, Okamoto H, Hifumi T et al The incidence of post‐intubation hypertension and association with repeated intubation attempts in the emergency department. PLoS ONE 2019; 14: e0212170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Cho YS, Cho J, Chung HS, Korean Emergency Airway Registry I . Assessment of emergency airway management techniques in Korea using an online registration system: a multicenter study. J. Emerg. Med. 2015; 48: 1–9. [DOI] [PubMed] [Google Scholar]
- 23. Detsky ME, Jivraj N, Adhikari NK et al Will this patient be difficult to intubate?: the rational clinical examination systematic review. JAMA 2019; 321: 493–503. [DOI] [PubMed] [Google Scholar]
- 24. Eberhart LH, Arndt C, Cierpka T, Schwanekamp J, Wulf H, Putzke C. The reliability and validity of the upper lip bite test compared with the Mallampati classification to predict difficult laryngoscopy: an external prospective evaluation. Anesth. Analg. 2005; 101: 284–9, table of contents. [DOI] [PubMed] [Google Scholar]
- 25. Levitan RM, Everett WW, Ochroch EA. Limitations of difficult airway prediction in patients intubated in the emergency department. Ann. Emerg. Med. 2004; 44: 307–13. [DOI] [PubMed] [Google Scholar]
- 26. Sudrial J, Birlouez C, Guillerm AL, Sebbah JL, Amathieu R, Dhonneur G. Difficult airway management algorithm in emergency medicine: do not struggle against the patient, just skip to next step. Emerg. Med. Int. 2010; 2010: 826231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pradhan D, Bhattacharyya P. Difficult airway management from emergency department till intensive care unit. Indian J. Crit. Care Med. 2015; 19: 557–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Higgs A, McGrath BA, Goddard C et al Guidelines for the management of tracheal intubation in critically ill adults. Br. J. Anaesth. 2018; 120: 323–52. [DOI] [PubMed] [Google Scholar]
- 29. Walls RM. Manual of Emergency Airway Management, 4th edn Philadelphia, PA: Lippincot Williams and Wilkins, 2012. [Google Scholar]
- 30. Goto T, Watase H, Morita H et al Repeated attempts at tracheal intubation by a single intubator associated with decreased success rates in emergency departments: an analysis of a multicentre prospective observational study. Emerg. Med. J. 2015; 32: 781–6. [DOI] [PubMed] [Google Scholar]
- 31. Hagiwara Y, Watase H, Okamoto H, Goto T, Hasegawa K, Japanese Emergency Medicine Network I . Prospective validation of the modified LEMON criteria to predict difficult intubation in the ED. Am. J. Emerg. Med. 2015; 33: 1492–6. [DOI] [PubMed] [Google Scholar]
- 32. Adnet F, Borron SW, Racine SX et al The intubation difficulty scale (IDS): proposal and evaluation of a new score characterizing the complexity of endotracheal intubation. Anesthesiology 1997; 87: 1290–7. [DOI] [PubMed] [Google Scholar]
- 33. Apfelbaum JL, Hagberg CA, Caplan RA et al Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology 2013; 118: 251–70. [DOI] [PubMed] [Google Scholar]
- 34. Benumof JL. Management of the difficult adult airway. With special emphasis on awake tracheal intubation. Anesthesiology 1991; 75: 1087–110. [DOI] [PubMed] [Google Scholar]
- 35. Crosby ET, Cooper RM, Douglas MJ et al The unanticipated difficult airway with recommendations for management. Can. J. Anaesth. 1998; 45: 757–76. [DOI] [PubMed] [Google Scholar]
- 36. Reed MJ. Can an airway assessment score predict difficulty at intubation in the emergency department? Emerg. Med. J. 2005; 22: 99–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Soyuncu S, Eken C, Cete Y, Bektas F, Akcimen M. Determination of difficult intubation in the ED. Am. J. Emerg. Med. 2009; 27: 905–10. [DOI] [PubMed] [Google Scholar]
- 38. Graciano AL, Tamburro R, Thompson AE, Fiadjoe J, Nadkarni VM, Nishisaki A. Incidence and associated factors of difficult tracheal intubations in pediatric ICUs: a report from National Emergency Airway Registry for Children: nEAR4KIDS. Intensive Care Med. 2014; 40: 1659–69. [DOI] [PubMed] [Google Scholar]
- 39. Bair AE, Caravelli R, Tyler K, Laurin EG. Feasibility of the preoperative mallampati airway assessment in emergency department patients. J. Emerg. Med. 2010; 38: 677–80. [DOI] [PubMed] [Google Scholar]
- 40. Orebaugh SL. Atlas of Airway Management: Techniques and Tools, 2nd edn Philadephia, PA: Lippincot Williams and Wilkins, 2012. [Google Scholar]
- 41. Pourmand A, Robinson C, Dorwart K, O'Connell F. Pre‐oxygenation: implications in emergency airway management. Am. J. Emerg. Med. 2017; 35: 1177–83. [DOI] [PubMed] [Google Scholar]
- 42. Weingart SD, Levitan RM. Preoxygenation and prevention of desaturation during emergency airway management. Ann. Emerg. Med. 2012; 59: 165–75. e161. [DOI] [PubMed] [Google Scholar]
- 43. Mort TC. The incidence and risk factors for cardiac arrest during emergency tracheal intubation: a justification for incorporating the ASA Guidelines in the remote location. J. Clin. Anesth. 2004; 16: 508–16. [DOI] [PubMed] [Google Scholar]
- 44. Casey JD, Janz DR, Russell DW et al Bag‐mask ventilation during tracheal intubation of critically ill adults. N. Engl. J. Med. 2019; 380: 811–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Binks MJ, Holyoak RS, Melhuish TM, Vlok R, Bond E, White LD. Apneic oxygenation during intubation in the emergency department and during retrieval: a systematic review and meta‐analysis. Am. J. Emerg. Med. 2017; 35: 1542–6. [DOI] [PubMed] [Google Scholar]
- 46. Turner JS, Ellender TJ, Okonkwo ER et al Feasibility of upright patient positioning and intubation success rates At two academic EDs. Am. J. Emerg. Med. 2017; 35: 986–92. [DOI] [PubMed] [Google Scholar]
- 47. Khandelwal N, Khorsand S, Mitchell SH, Joffe AM. Head‐elevated patient positioning decreases complications of emergent tracheal intubation in the ward and intensive care unit. Anesth. Analg. 2016; 122: 1101–7. [DOI] [PubMed] [Google Scholar]
- 48. Ramkumar V, Umesh G, Philip FA. Preoxygenation with 20 masculine head‐up tilt provides longer duration of non‐hypoxic apnea than conventional preoxygenation in non‐obese healthy adults. J. Anesth. 2011; 25: 189–94. [DOI] [PubMed] [Google Scholar]
- 49. Lane S, Saunders D, Schofield A, Padmanabhan R, Hildreth A, Laws D. A prospective, randomised controlled trial comparing the efficacy of pre‐oxygenation in the 20 degrees head‐up vs supine position. Anaesthesia 2005; 60: 1064–7. [DOI] [PubMed] [Google Scholar]
- 50. Baillard C, Fosse JP, Sebbane M et al Noninvasive ventilation improves preoxygenation before intubation of hypoxic patients. Am. J. Respir. Crit. Care Med. 2006; 174: 171–7. [DOI] [PubMed] [Google Scholar]
- 51. Miguel‐Montanes R, Hajage D, Messika J et al Use of high‐flow nasal cannula oxygen therapy to prevent desaturation during tracheal intubation of intensive care patients with mild‐to‐moderate hypoxemia. Crit. Care Med. 2015; 43: 574–83. [DOI] [PubMed] [Google Scholar]
- 52. Vourc'h M, Asfar P, Volteau C et al High‐flow nasal cannula oxygen during endotracheal intubation in hypoxemic patients: a randomized controlled clinical trial. Intensive Care Med. 2015; 41: 1538–48. [DOI] [PubMed] [Google Scholar]
- 53. Simon M, Wachs C, Braune S, de Heer G, Frings D, Kluge S. High‐flow nasal cannula versus bag‐valve‐mask for preoxygenation before intubation in subjects with hypoxemic respiratory failure. Respir. Care 2016; 61: 1160–7. [DOI] [PubMed] [Google Scholar]
- 54. Weingart SD. Preoxygenation, reoxygenation, and delayed sequence intubation in the emergency department. J. Emerg. Med. 2011; 40: 661–7. [DOI] [PubMed] [Google Scholar]
- 55. Weingart SD, Trueger NS, Wong N, Scofi J, Singh N, Rudolph SS. Delayed sequence intubation: a prospective observational study. Ann. Emerg. Med. 2015; 65: 349–55. [DOI] [PubMed] [Google Scholar]
- 56. Sagarin MJ, Chiang V, Sakles JC et al Rapid sequence intubation for pediatric emergency airway management. Pediatr. Emerg. Care 2002; 18: 417–23. [DOI] [PubMed] [Google Scholar]
- 57. Kim C, Kang HG, Lim TH, Choi BY, Shin YJ, Choi HJ. What factors affect the success rate of the first attempt at endotracheal intubation in emergency departments? Emerg. Med. J. 2013; 30: 888–92. [DOI] [PubMed] [Google Scholar]
- 58. Okubo M, Gibo K, Hagiwara Y, Nakayama Y, Hasegawa K, Japanese Emergency Medicine Network I . The effectiveness of rapid sequence intubation (RSI) versus non‐RSI in emergency department: an analysis of multicenter prospective observational study. Int. J. Emerg. Med. 2017; 10: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Cahir TM, Bair AE, Pallin DJ, Walls RM, Investigators NI . Techniques, success, and adverse events of emergency department adult intubations. Ann. Emerg. Med. 2015; 65: 363–70. e361. [DOI] [PubMed] [Google Scholar]
- 60. Goto Y, Goto T, Hagiwara Y et al Techniques and outcomes of emergency airway management in Japan: an analysis of two multicentre prospective observational studies, 2010‐2016. Resuscitation 2017; 114: 14–20. [DOI] [PubMed] [Google Scholar]
- 61. Hsiao J, Pacheco‐Fowler V. Videos in clinical medicine. Cricothyroidotomy. N. Engl. J. Med. 2008; 358: e25. [DOI] [PubMed] [Google Scholar]
- 62. Law JA, Broemling N, Cooper RM et al The difficult airway with recommendations for management–part 1–difficult tracheal intubation encountered in an unconscious/induced patient. Can. J. Anaesth. 2013; 60: 1089–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Ihra G, Gockner G, Kashanipour A, Aloy A. High‐frequency jet ventilation in European and North American institutions: developments and clinical practice. Eur. J. Anaesthesiol. 2000; 17: 418–30. [DOI] [PubMed] [Google Scholar]
- 64. Osman A, Sum KM. Role of upper airway ultrasound in airway management. J. Intensive Care 2016; 4: 52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. You‐Ten KE, Siddiqui N, Teoh WH, Kristensen MS. Point‐of‐care ultrasound (POCUS) of the upper airway. Can. J. Anaesth. 2018; 65: 473–84. [DOI] [PubMed] [Google Scholar]
- 66. Birenbaum A, Hajage D, Roche S et al Effect of cricoid pressure compared with a sham procedure in the rapid sequence induction of anesthesia: the IRIS randomized clinical trial. JAMA Surg. 2019; 154: 9–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Algie CM, Mahar RK, Tan HB, Wilson G, Mahar PD, Wasiak J. Effectiveness and risks of cricoid pressure during rapid sequence induction for endotracheal intubation. Cochrane Database Syst. Rev. 2015: CD011656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Takahata O, Kubota M, Mamiya K et al The efficacy of the “BURP” maneuver during a difficult laryngoscopy. Anesth. Analg. 1997; 84: 419–21. [DOI] [PubMed] [Google Scholar]
- 69. Lee AR, Yang S, Shin YH et al A comparison of the BURP and conventional and modified jaw thrust manoeuvres for orotracheal intubation using the Clarus Video System. Anaesthesia 2013; 68: 931–7. [DOI] [PubMed] [Google Scholar]
- 70. Tamura M, Ishikawa T, Kato R, Isono S, Nishino T. Mandibular advancement improves the laryngeal view during direct laryngoscopy performed by inexperienced physicians. Anesthesiology 2004; 100: 598–601. [DOI] [PubMed] [Google Scholar]
- 71. Takahashi J, Goto T, Okamoto H et al Association of fentanyl use in rapid sequence intubation with post‐intubation hypotension. Am. J. Emerg. Med. 2018; 36: 2044–9. [DOI] [PubMed] [Google Scholar]
- 72. Jabre P, Combes X, Lapostolle F et al Etomidate versus ketamine for rapid sequence intubation in acutely ill patients: a multicentre randomised controlled trial. Lancet 2009; 374: 293–300. [DOI] [PubMed] [Google Scholar]
- 73. Hasegawa K, Hagiwara Y, Imamura T et al Increased incidence of hypotension in elderly patients who underwent emergency airway management: an analysis of a multi‐centre prospective observational study. Int. J. Emerg. Med. 2013; 6: 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Searle NR, Sahab P. Propofol in patients with cardiac disease. Can. J. Anaesth. 1993; 40: 730–47. [DOI] [PubMed] [Google Scholar]
- 75. April MD, Arana A, Pallin DJ et al Emergency department intubation success with succinylcholine versus rocuronium: a national emergency airway registry study. Ann. Emerg. Med. 2018; 72: 645–53. [DOI] [PubMed] [Google Scholar]
- 76. Sakles JC, Mosier J, Chiu S, Cosentino M, Kalin L. A comparison of the C‐MAC video laryngoscope to the Macintosh direct laryngoscope for intubation in the emergency department. Ann. Emerg. Med. 2012; 60: 739–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Sakles JC, Mosier JM, Chiu S, Keim SM. Tracheal intubation in the emergency department: a comparison of GlideScope(R) video laryngoscopy to direct laryngoscopy in 822 intubations. J. Emerg. Med. 2012; 42: 400–5. [DOI] [PubMed] [Google Scholar]
- 78. Mosier JM, Stolz U, Chiu S, Sakles JC. Difficult airway management in the emergency department: GlideScope videolaryngoscopy compared to direct laryngoscopy. J. Emerg. Med. 2012; 42: 629–34. [DOI] [PubMed] [Google Scholar]
- 79. Sakles JC, Patanwala AE, Mosier JM, Dicken JM. Comparison of video laryngoscopy to direct laryngoscopy for intubation of patients with difficult airway characteristics in the emergency department. Intern. Emerg. Med. 2014; 9: 93–8. [DOI] [PubMed] [Google Scholar]
- 80. Sakles JC, Javedani PP, Chase E, Garst‐Orozco J, Guillen‐Rodriguez JM, Stolz U. The use of a video laryngoscope by emergency medicine residents is associated with a reduction in esophageal intubations in the emergency department. Acad. Emerg. Med. 2015; 22: 700–7. [DOI] [PubMed] [Google Scholar]
- 81. Vassiliadis J, Tzannes A, Hitos K, Brimble J, Fogg T. Comparison of the C‐MAC video laryngoscope with direct Macintosh laryngoscopy in the emergency department. Emerg. Med. Australas. 2015; 27: 119–25. [DOI] [PubMed] [Google Scholar]
- 82. Sadamori T, Kusunoki S, Otani T et al Airway scope for emergency intubations: usefulness of a new video‐laryngoscope. Hiroshima J. Med. Sci. 2008; 57: 99–104. [PubMed] [Google Scholar]
- 83. Okamoto H, Goto T, Wong ZSY et al Comparison of video laryngoscopy versus direct laryngoscopy for intubation in emergency department patients with cardiac arrest: a multicentre study. Resuscitation 2019; 136: 70–7. [DOI] [PubMed] [Google Scholar]
- 84. Sadamori T, Kusunoki S, Ishida M, Otani T, Tanigawa K. Video laryngoscopy for emergency tracheal intubation during chest compression. Resuscitation 2008; 77: 155–6. [DOI] [PubMed] [Google Scholar]
- 85. Goto T, Koyama Y, Kondo T, Tsugawa Y, Hasegawa K. A comparison of the force applied on oral structures during intubation attempts between the Pentax‐AWS airwayscope and the Macintosh laryngoscope: a high‐fidelity simulator‐based study. BMJ Open 2014; 4: e006416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Liu L, Tanigawa K, Kusunoki S et al Tracheal intubation of a difficult airway using Airway Scope, Airtraq, and Macintosh laryngoscope: a comparative manikin study of inexperienced personnel. Anesth. Analg. 2010; 110: 1049–55. [DOI] [PubMed] [Google Scholar]
- 87. Nakanishi T, Shiga T, Homma Y, Koyama Y, Goto T. Comparison of the force applied on oral structures during intubation attempts by novice physicians between the Macintosh direct laryngoscope, Airway Scope and C‐MAC PM: a high‐fidelity simulator‐based study. BMJ Open 2016; 6: e011039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Kidd JF, Dyson A, Latto IP. Successful difficult intubation Use of the gum elastic bougie. Anaesthesia 1988; 43: 437–8. [DOI] [PubMed] [Google Scholar]
- 89. Driver BE, Prekker ME, Klein LR et al Effect of use of a bougie vs endotracheal tube and stylet on first‐attempt intubation success among patients with difficult airways undergoing emergency intubation: a randomized clinical trial. JAMA 2018; 319: 2179–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Driver B, Dodd K, Klein LR et al The bougie and first‐pass success in the emergency department. Ann. Emerg. Med. 2017; 70: 473–8. e471. [DOI] [PubMed] [Google Scholar]
- 91. Kim JH, Kim YM, Choi HJ, Je SM, Kim E, Korean Emergency Airway Management Registry I . Factors associated with successful second and third intubation attempts in the ED. Am. J. Emerg. Med. 2013; 31: 1376–81. [DOI] [PubMed] [Google Scholar]
- 92. Goksu E, Kilic T, Yildiz G, Unal A, Kartal M. Comparison of the C‐MAC video laryngoscope to the Macintosh laryngoscope for intubation of blunt trauma patients in the ED. Turk. J. Emerg. Med. 2016; 16: 53–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Sakles JC, Mosier JM, Patanwala AE, Dicken JM, Kalin L, Javedani PP. The C‐MAC(R) video laryngoscope is superior to the direct laryngoscope for the rescue of failed first‐attempt intubations in the emergency department. J. Emerg. Med. 2015; 48: 280–6. [DOI] [PubMed] [Google Scholar]
- 94. Goto T, Watase H, Morita H et al Repeated attempts at tracheal intubation by a single intubator associated with decreased success rates in emergency departments: an analysis of a multicentre prospective observational study. Emerg. Med. J. 2015; 32: 781–6. [DOI] [PubMed] [Google Scholar]
- 95. Nakao S, Kimura A, Hagiwara Y, Hasegawa K, Japanese Emergency Medicine Network I . Trauma airway management in emergency departments: a multicentre, prospective, observational study in Japan. BMJ Open 2015; 5: e006623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Park L, Zeng I, Brainard A. Systematic review and meta‐analysis of first‐pass success rates in emergency department intubation: creating a benchmark for emergency airway care. Emerg. Med. Australas. 2017; 29: 40–7. [DOI] [PubMed] [Google Scholar]
- 97. Conroy MJ, Weingart GS, Carlson JN. Impact of checklists on peri‐intubation care in ED trauma patients. Am. J. Emerg. Med. 2014; 32: 541–4. [DOI] [PubMed] [Google Scholar]
- 98. Levitan RM, Rosenblatt B, Meiner EM, Reilly PM, Hollander JE. Alternating day emergency medicine and anesthesia resident responsibility for management of the trauma airway: a study of laryngoscopy performance and intubation success. Ann. Emerg. Med. 2004; 43: 48–53. [DOI] [PubMed] [Google Scholar]
- 99. Bushra JS, McNeil B, Wald DA, Schwell A, Karras DJ. A comparison of trauma intubations managed by anesthesiologists and emergency physicians. Acad. Emerg. Med. 2004; 11: 66–70. [DOI] [PubMed] [Google Scholar]
- 100. Omert L, Yeaney W, Mizikowski S, Protetch J. Role of the emergency medicine physician in airway management of the trauma patient. J. Trauma Acute Care Surg. 2001; 51: 1065–8. [DOI] [PubMed] [Google Scholar]
- 101. Kovacs G, Sowers N. Airway management in trauma. Emerg. Med. Clin. North Am. 2018; 36: 61–84. [DOI] [PubMed] [Google Scholar]
- 102. Estime SR, Kuza CM. Trauma airway management: induction agents, rapid versus slower sequence intubations, and special considerations. Anesthesiol. Clin. 2019; 37: 33–50. [DOI] [PubMed] [Google Scholar]
- 103. Mayglothling J, Duane TM, Gibbs M et al Emergency tracheal intubation immediately following traumatic injury: an Eastern Association for the Surgery of Trauma practice management guideline. J. Trauma Acute Care Surg. 2012; 73: S333–40. [DOI] [PubMed] [Google Scholar]
- 104. Committee of the Japan Association of Trauma‐ tology . The Japan Advanced Trauma Evaluation and Care (JATEC), 5th edn Tokyo: Herusu Shuppan Co., Inc., 2016. [Google Scholar]
- 105. Groth CM, Acquisto NM, Khadem T. Current practices and safety of medication use during rapid sequence intubation. J. Crit. Care 2018; 45: 65–70. [DOI] [PubMed] [Google Scholar]
- 106. Gooding JM, Weng J‐T, Smith RA, Berninger GT, Kirby RR. Cardiovascular and pulmonary responses following etomidate induction of anesthesia in patients with demonstrated cardiac disease. Anesth. Analg. 1979; 58: 40–1. [DOI] [PubMed] [Google Scholar]
- 107. Zed PJ, Abu‐Laban RB, Harrison DW. Intubating conditions and hemodynamic effects of etomidate for rapid sequence intubation in the emergency department: an observational cohort study. Acad. Emerg. Med. 2006; 13: 378–83. [DOI] [PubMed] [Google Scholar]
- 108. Belopavlovic M, Buchthal A. Modification of ketamine‐induced intracranial hypertension in neurosurgical patients by pretreatment with midazolam. Acta Anaesthesiol. Scand. 1982; 26: 458–62. [DOI] [PubMed] [Google Scholar]
- 109. Cohen L, Athaide V, Wickham ME, Doyle‐Waters MM, Rose NG, Hohl CM. The effect of ketamine on intracranial and cerebral perfusion pressure and health outcomes: a systematic review. Ann. Emerg. Med. 2015; 65: 43–51. e42. [DOI] [PubMed] [Google Scholar]
- 110. Zeiler FA, Teitelbaum J, West M, Gillman LM. The ketamine effect on ICP in traumatic brain injury. Neurocrit. Care 2014; 21: 163–73. [DOI] [PubMed] [Google Scholar]
- 111. Upchurch CP, Grijalva CG, Russ S et al Comparison of etomidate and ketamine for induction during rapid sequence intubation of adult trauma patients. Ann. Emerg. Med. 2017; 69: 24–33. e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Wyte SR, Shapiro HM, Turner P, Harris AB. Ketamine‐induced intracranial hypertension. Anesthesiology 1972; 36: 174–6. [DOI] [PubMed] [Google Scholar]
- 113. Arima T, Nagata O, Miura T et al Comparative analysis of airway scope and Macintosh laryngoscope for intubation primarily for cardiac arrest in prehospital setting. Am. J. Emerg. Med. 2014; 32: 40–3. [DOI] [PubMed] [Google Scholar]
- 114. Benger JR, Kirby K, Black S et al Effect of a strategy of a supraglottic airway device vs tracheal intubation during out‐of‐hospital cardiac arrest on functional outcome: the AIRWAYS‐2 randomized clinical trial. JAMA 2018; 320: 779–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Benoit JL, Gerecht RB, Steuerwald MT, McMullan JT. Endotracheal intubation versus supraglottic airway placement in out‐of‐hospital cardiac arrest: a meta‐analysis. Resuscitation 2015; 93: 20–6. [DOI] [PubMed] [Google Scholar]
- 116. Soar J, Nolan JP, Bottiger BW et al European resuscitation council guidelines for resuscitation 2015: section 3. Adult advanced life support. Resuscitation 2015; 95: 100–47. [DOI] [PubMed] [Google Scholar]
- 117. Link MS, Berkow LC, Kudenchuk PJ et al Part 7: adult advanced cardiovascular life support: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015; 132(18 Suppl 2): S444–64. [DOI] [PubMed] [Google Scholar]
- 118. Soar J, Nolan JP. Airway management in cardiopulmonary resuscitation. Curr. Opin. Crit. Care 2013; 19: 181–7. [DOI] [PubMed] [Google Scholar]
- 119. Kleinman ME, Goldberger ZD, Rea T et al 2017 American Heart Association focused update on adult basic life support and cardiopulmonary resuscitation quality: an update to the American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2018; 137: e7–13. [DOI] [PubMed] [Google Scholar]
- 120. Wang HE, Simeone SJ, Weaver MD, Callaway CW. Interruptions in cardiopulmonary resuscitation from paramedic endotracheal intubation. Ann. Emerg. Med. 2009; 54: 645–52. e641. [DOI] [PubMed] [Google Scholar]
- 121. Hiltunen P, Jantti H, Silfvast T, Kuisma M, Kurola J, group FPs . Airway management in out‐of‐hospital cardiac arrest in Finland: current practices and outcomes. Scand. J. Trauma Resusc. Emerg. Med. 2016; 24: 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Kim SY, Park SO, Kim JW et al How much experience do rescuers require to achieve successful tracheal intubation during cardiopulmonary resuscitation? Resuscitation 2018; 133: 187–92. [DOI] [PubMed] [Google Scholar]
- 123. Kim JW, Park SO, Lee KR et al Video laryngoscopy vs. direct laryngoscopy: which should be chosen for endotracheal intubation during cardiopulmonary resuscitation? A prospective randomized controlled study of experienced intubators. Resuscitation 2016; 105: 196–202. [DOI] [PubMed] [Google Scholar]
- 124. Park SO, Kim JW, Na JH et al Video laryngoscopy improves the first‐attempt success in endotracheal intubation during cardiopulmonary resuscitation among novice physicians. Resuscitation 2015; 89: 188–94. [DOI] [PubMed] [Google Scholar]
- 125. Long E, Sabato S, Babl FE. Endotracheal intubation in the pediatric emergency department. Paediatr Anaesth. 2014; 24: 1204–11. [DOI] [PubMed] [Google Scholar]
- 126. Pek JH, Ong GY. Emergency intubations in a high‐volume pediatric emergency department. Pediatr. Emerg. Care 2018; 34: 852–6. [DOI] [PubMed] [Google Scholar]
- 127. Losek JD, Olson LR, Dobson JV, Glaeser PW. Tracheal intubation practice and maintaining skill competency: survey of pediatric emergency department medical directors. Pediatr. Emerg. Care 2008; 24: 294–9. [DOI] [PubMed] [Google Scholar]
- 128. Yurtseven A, Turan C, Kilinc MA, Ulas SE. Frequency and outcomes of endotracheal intubation in the pediatric emergency department. Turk. J. Pediatr. 2017; 59: 524–30. [DOI] [PubMed] [Google Scholar]
- 129. Luten R, Wears RL, Broselow J, Croskerry P, Joseph MM, Frush K. Managing the unique size‐related issues of pediatric resuscitation: reducing cognitive load with resuscitation aids. Acad. Emerg. Med. 2002; 9: 840–7. [DOI] [PubMed] [Google Scholar]
- 130. Goto T, Gibo K, Hagiwara Y et al Factors associated with first‐pass success in pediatric intubation in the emergency department. West. J. Emerg. Med. 2016; 17: 129–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Choi HJ, Je SM, Kim JH, Kim E, Korean Emergency Airway Registry I . The factors associated with successful paediatric endotracheal intubation on the first attempt in emergency departments: a 13‐emergency‐department registry study. Resuscitation 2012; 83: 1363–8. [DOI] [PubMed] [Google Scholar]
- 132. Kerrey BT, Rinderknecht AS, Geis GL, Nigrovic LE, Mittiga MR. Rapid sequence intubation for pediatric emergency patients: higher frequency of failed attempts and adverse effects found by video review. Ann. Emerg. Med. 2012; 60: 251–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Sukys GA, Schvartsman C, Reis AG. Evaluation of rapid sequence intubation in the pediatric emergency department. J. Pediatr. (Rio J) 2011; 87: 343–9. [DOI] [PubMed] [Google Scholar]
- 134. Lubitz DS, Seidel JS, Chameides L, Luten RC, Zaritsky AL, Campbell FW. A rapid method for estimating weight and resuscitation drug dosages from length in the pediatric age group. Ann. Emerg. Med. 1988; 17: 576–81. [DOI] [PubMed] [Google Scholar]
- 135. Luten RC, Wears RL, Broselow J et al Length‐based endotracheal tube and emergency equipment in pediatrics. Ann. Emerg. Med. 1992; 21: 900–4. [DOI] [PubMed] [Google Scholar]
- 136. Hofer CK, Ganter M, Tucci M, Klaghofer R, Zollinger A. How reliable is length‐based determination of body weight and tracheal tube size in the paediatric age group? The Broselow tape reconsidered. Br. J. Anaesth. 2002; 88: 283–5. [DOI] [PubMed] [Google Scholar]
- 137. Agarwal S, Swanson S, Murphy A, Yaeger K, Sharek P, Halamek LP. Comparing the utility of a standard pediatric resuscitation cart with a pediatric resuscitation cart based on the Broselow tape: a randomized, controlled, crossover trial involving simulated resuscitation scenarios. Pediatrics 2005; 116: e326–33. [DOI] [PubMed] [Google Scholar]
- 138. Santillanes G, Gausche‐Hill M. Pediatric airway management. Emerg. Med. Clin. North Am. 2008; 26: 961–75, ix. [DOI] [PubMed] [Google Scholar]
- 139. Bano S, Akhtar S, Zia N, Khan UR, Haq AU. Pediatric endotracheal intubations for airway management in the emergency department. Pediatr. Emerg. Care 2012; 28: 1129–31. [DOI] [PubMed] [Google Scholar]
- 140. Vukovic AA, Hanson HR, Murphy SL, Mercurio D, Sheedy CA, Arnold DH. Apneic oxygenation reduces hypoxemia during endotracheal intubation in the pediatric emergency department. Am. J. Emerg. Med. 2019; 37: 27–32. [DOI] [PubMed] [Google Scholar]
- 141. Wang HE. Emergency airway management: the need to refine – and redefine – the “state of the art”. Resuscitation 2012; 83: 405–6. [DOI] [PubMed] [Google Scholar]
- 142. Choi HJ, Kang HG, Lim TH et al Endotracheal intubation using a GlideScope video laryngoscope by emergency physicians: a multicentre analysis of 345 attempts in adult patients. Emerg. Med. J. 2010; 27: 380–2. [DOI] [PubMed] [Google Scholar]
- 143. Choi HJ, Kim YM, Oh YM et al GlideScope video laryngoscopy versus direct laryngoscopy in the emergency department: a propensity score‐matched analysis. BMJ Open 2015; 5: e007884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Imamura T, Brown CA 3rd, Ofuchi H et al Emergency airway management in geriatric and younger patients: analysis of a multicenter prospective observational study. Am. J. Emerg. Med. 2013; 31: 190–6. [DOI] [PubMed] [Google Scholar]
- 145. Goto Y, Watase H, Brown CA 3rd et al Emergency airway management by resident physicians in Japan: an analysis of multicentre prospective observational study. Acute Med. Surg. 2014; 1: 214–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Sato N, Hagiwara Y, Watase H, Hasegawa K, Japanese Emergency Medicine Network I . A comparison of emergency airway management between neuromuscular blockades alone and rapid sequence intubation: an analysis of multicenter prospective study. BMC Res. Notes 2017; 10: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Yakushiji H, Goto T, Shirasaka W et al Associations of obesity with tracheal intubation success on first attempt and adverse events in the emergency department: an analysis of the multicenter prospective observational study in Japan. PLoS ONE 2018; 13: e0195938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Van Spall HG, Toren A, Kiss A, Fowler RA. Eligibility criteria of randomized controlled trials published in high‐impact general medical journals: a systematic sampling review. JAMA 2007; 297: 1233–40. [DOI] [PubMed] [Google Scholar]
- 149. Hernán MA, Robins JM. Causal Inference. Boca Raton: Chapman & Hall/CRC, 2019. forthcoming. [Google Scholar]
- 150. Ono Y, Tanigawa K, Shinohara K et al Human and equipment resources for difficult airway management, airway education programs, and capnometry use in Japanese emergency departments: a nationwide cross‐sectional study. Int. J. Emerg. Med. 2017; 10: 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Ono Y, Yokoyama H, Matsumoto A, Kumada Y, Shinohara K, Tase C. Surgical airways for trauma patients in an emergency surgical setting: 11 years’ experience at a teaching hospital in Japan. J. Anesth. 2013; 27: 832–7. [DOI] [PubMed] [Google Scholar]
- 152. Ono Y, Kakamu T, Kikuchi H, Mori Y, Watanabe Y, Shinohara K. Expert‐performed endotracheal intubation‐related complications in trauma patients: incidence, possible risk factors, and outcomes in the prehospital setting and emergency department. Emerg. Med. Int. 2018; 2018: 5649476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Ono Y, Sugiyama T, Chida Y et al Association between off‐hour presentation and endotracheal‐intubation‐related adverse events in trauma patients with a predicted difficult airway: a historical cohort study at a community emergency department in Japan. Scand. J. Trauma Resusc. Emerg. Med. 2016; 24: 106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Kuwahara Y, Taguchi S, Kusunoki S, Tanigawa K, Kawamoto M. Use of i‐gel supraglottic airway for emergency airway management by novice personnel in comparison with laryngeal mask airway and tracheal intubation in manikin models. Masui 2013; 62: 592–5. [PubMed] [Google Scholar]


