Abstract
Background and Purpose: Decision algorithms for large vessel occlusions in the anterior circulation remain unconfirmed for acute basilar artery occlusion (aBAO). The aim of this study was to investigate procedural parameters, patient characteristics, functional outcome, and survival in dependency of the time window to recanalization from symptom onset. Furthermore predictors of outcome were identified.
Materials and Methods: Retrospectively 231 patients with aBAO treated with endovascular treatment (EVT) between November 2008 and February 2019 were identified in a prospectively maintained single center stroke database. Baseline characteristics such as age, cardiovascular risk factors, NIHSS at admission, pre-interventional PC-ASPECTS, periprocedural parameters such as time to recanalization, duration of treatment, extent of reperfusion, collateral status, and occlusion patterns, as well as post-interventional 24 h NIHSS and post-interventional ICH were evaluated. Target variables were mRS at 90 days and mortality over 90 days.
Results: Good outcome (mRS 0–2) was attained in 29.5% (n = 68) of patients, overall mortality was 36.8% (n = 85). In mulitivariate analyses patients with time to reperfusion beyond 6 h had a more than half fold decreased chance of good outcome [OR 0.47 95% CI (0.23–0.95) p < 0.05]. The odds for good outcome were reduced by almost 2/3 if post-interventional imaging revealed intracerebral hemorrhage [OR 0.28 95% CI (0.08–0.98)]. Unfavorable outcome was noted in 100% (n = 14) of patients with symptomatic ICH. Risk for death was reduced by more than 80% if collaterals were present [0.16 95% CI (0.03–0.87)] and if recanalization was successful (TICI 2b-3) [OR 0.19 95% CI (0.05–0.78)]. The odds for survival were 5-fold higher in patients with no post-interventional hemorrhages present [OR 5.35 95% CI (2.2–1.58)].
Conclusion: This study might contribute to explaining the ambiguous findings regarding the validity of the 6 h time window in aBAO, suggesting that collateral status impacts the odds of survival in the time window to recanalization beyond 6 h. In our study recanalization within 6 h from symptom onset was associated with good outcome. Successful recanalization (TICI 2b-3a) was necessary for good outcome and survival, post-interventional ICH was highly associated with unfavorable outcome. This might ease the decision making for EVT.
Keywords: stroke, posterior circulation, outcome, basilar artery occlusion, time window to treatment
Introduction
The overwhelmingly positive trial results favoring mechanical thrombectomy over thrombolysis have represented one of the most important advances in stroke care for decades. However, there are still numerous questions that need to be answered. The positive trials all enrolled patients with anterior circulation strokes and therefore, the advantage of mechanical thrombectomy in large vessel thromboembolic occlusion in the posterior circulation is yet to be determined. Acute basilar artery occlusion (aBAO) is one of the most devastating subtypes of stroke with a mortality rate of more than 30% following mechanical thrombectomy (mTE) (1, 2). The factors relating to this high level of mortality are still unknown. However, this should be compared to mortality rates of up to 90% if left untreated (3, 4) as well as high rates of ambulatory outcome (3, 5, 6). As aBAO accounts for only 1% of all stroke types (7) both data collection and designing randomized controlled trials are challenging. Appropriate selection of patients for mTE remains problematic using the data currently available. Nevertheless, despite methodological limitations, successful recanalization in aBAO is endorsed as a key factor for survival and functional outcome (8–10) as recently reported in a study with 51 patients, IV thrombolysis alone failed to achieve recanalization in thrombi exceeding a length of 13 mm in aBAO (11). This study is based on data from a large real-world single center registry with 231 patients who underwent endovascular treatment (EVT). The purpose was to investigate the ambiguous findings regarding the time window from symptom onset to treatment. Therefore, procedural parameters and patient characteristics including collateral status and pathophysiological properties such as occlusion patterns were assessed and stratified by time to recanalization\reperfusion (TICI 2b-3) (TTR) from symptom onset. Functional outcome and survival after 90 days were studied, stratified by the time window to treatment.
Methods
We retrospectively identified all consecutive patients in our prospectively maintained single center stroke database who had undergone EVT for an aBAO between November 2008 and February 2019. Inclusion criteria included proven aBAO on CT or MR angiography, treatment with or without IV rtPA, use of accepted endovascular treatment strategies with either stent-retrievers, aspiration or a combination of both. No limit was placed on the admission NIHSS or the age of the patient. Exclusion criteria were if patients had a basilar artery occlusion due to an aneurysm, dissection, in-stent thrombosis, non-occlusive thrombi, and failed attempts as well as manifest brain tissue damage not compatible with life or spontaneous recanalization in aBAO. In total 46 patients were excluded. Endovascular treatment is always our first line treatment for an aBAO and was attempted regardless of age, time from stroke onset and unknown stroke onset. Patients had either been admitted directly to our comprehensive tertiary care neurological center or had arrived as inter-hospital transfers from secondary care hospitals in surrounding areas after undergoing baseline imaging (computed tomography or magnetic resonance imaging). All patients underwent an mTE using either stent-retrievers or aspiration.
Study Population
Baseline characteristics including demographics (age and sex), cardiovascular risk factors including smoking, cholesterol levels, hypertension, diabetes mellitus, and the NIHSS at admission were recorded. Furthermore, an Alberta Stroke Program Early CT Score (PC-ASPECTS) for the posterior circulation was derived from each patient's CT or MRI scan by an independent reviewer (JR) not party to any of our patient information, according to the method described in literature (12).
The time of symptom onset to recanalization (TTR) was recorded and categorized into up to 6 h and over 6 h, with the latter group including patients with unknown time of onset and last seen well beyond 6 h.
Endovascular Procedures
All patients were treated in the neuro-angiography suites under general anesthesia and were therefore sedated and intubated irrespective of their clinical status at admission. The devices used to achieve recanalization were at the discretion of the operator. Procedures were performed via the right common femoral route as standard using a 6F sheath. A brachial access route was used in patients if femoral access was not successful. Balloon guide catheters were not used as standard due to the location of the occlusions in the posterior circulation. The standard guide catheters included 6F Guider Softip (Boston Scientific) and 5F Envoy (Cordis). The microcatheters used in mechanical thrombectomy were either RapidTransit or Prowler Select Plus (Cordis, now Cerenovus); Trevo pro 18 MC (Stryker) or Velocity (Penumbra), The standard microguidewires were Synchro2 0.014” (Stryker) or pORTAL (phenox). Navien A+ 0.058” ID (Medtronic) and SOFIA Plus 0.070” ID (Microvention) were used for aspiration thrombectomies. Mechanical thrombectomy was performed with Solitaire FR (Medtronic) or pRESET (phenox). The earliest cases in the subset (2008–2009) used pCRC (phenox) or BONnet (phenox)devices.
The procedure time was defined as groin puncture time to final angiographic run. The date of treatment was recorded to test for any longitudinal effect on the clinical outcome.
Anatomical Assessment
The site of the arterial occlusion was defined in a binary way with either “patent” or “occluded” assigned to each artery, encompassing occlusion of the proximal, middle, distal third, or whole of the basilar artery as per standard nomenclature (13). The presence of collateral pathways was also assessed and recorded by noting unilateral or bilateral collateral flow in the aBAO via the posterior inferior cerebellar artery (PICA) and the superior cerebellar artery (SCA) pathway or the posterior communicating arteries (PCOMA) (Figure 1).
Figure 1.
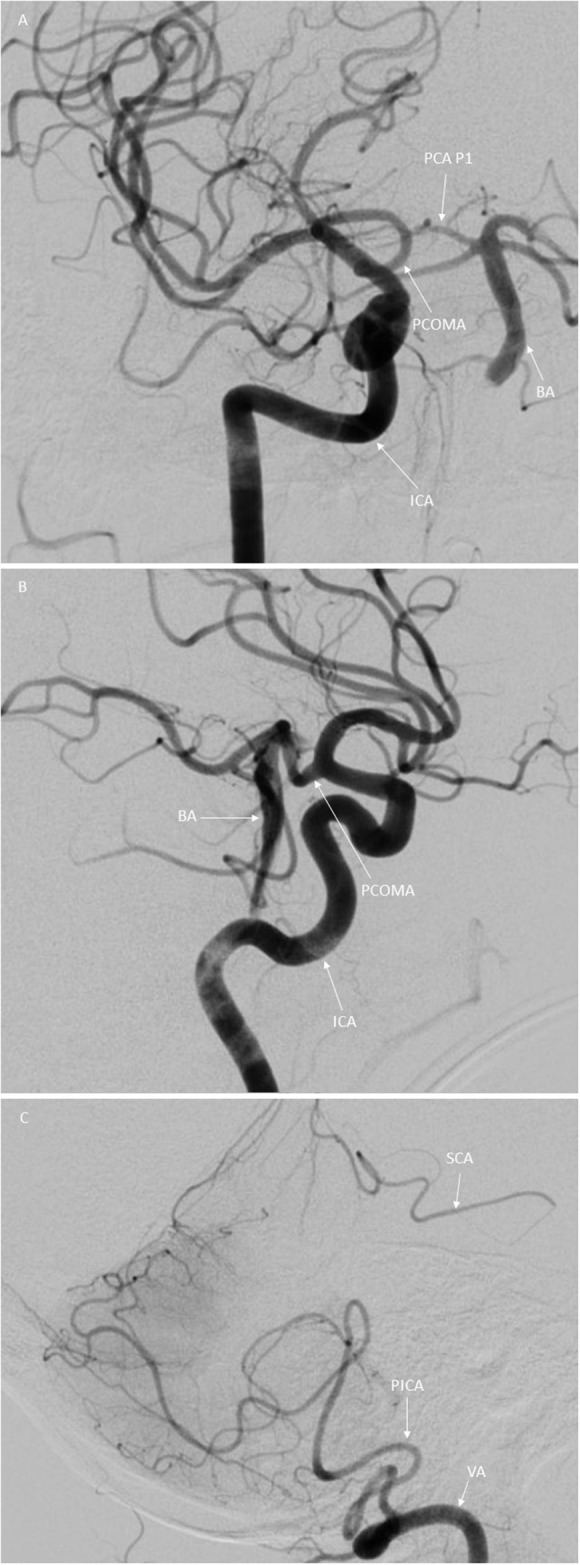
Illustration of the variants in collateral flow in aBAO in digital subtraction angiography in posterior anterior (A) and lateral (B,C) view. (A,B) Basilar artery (BA) with proximal occlusion indicated by the arrow. Right internal carotid artery (ICA) indicated by the arrow. Posterior communicating artery (PCOMA) indicated by the arrow. Posterior cerebral artery, first segment (PCA P1) indicated by the arrow (C) Right SCA-PICA collateral, right superior cerebellar artery (SCA) indicated by the arrow, right posterior inferior cerebellar artery indicated by the arrow and the right vertebral artery (VA).
Each branch and segment of the basilar artery was reviewed as above and its patency or lack thereof noted. Both the occlusion sites and collateral status were obtained retrospectively from the angiographic DSA images by two independent reviewers (HH, JR) who were not party to the 90-day mRS. Successful recanalization was defined as TICI 2b-3. Any intraoperative or periprocedural complications were recorded.
Post-procedural Hemorrhage
Intracranial hemorrhage (ICH) after EVT was assessed by CT and/or MRI and was rated as “asymptomatic” or “symptomatic.” “Symptomatic” was defined according to ECASS II criteria (14). Each data set was then labeled “no hemorrhage,” “asymptomatic hemorrhage,” or “symptomatic hemorrhage.” These labels were used in the statistical analysis.
All post-interventional CT or MRI images were reviewed by an independent reviewer (JR), blinded to our patient information.
Post-procedural Follow-Up and Outcome
Post-interventional treatment management included admission to the neuro-intensive care unit or hyper acute stroke unit with routine follow-up imaging comprising either CT or MRI scans at 24–36 h and a 24 h NIHSS if possible. The mRS was assessed 24 h after EVT, at discharge, and at 90 days. The 90-day mRS was evaluated either within a follow-up clinic appointment or via telephone by trained research nurses or members of the neurological team.
Statistical Analysis
Continuous variables were expressed as mean ± SD or median (interquartile range [IQR]) and categorical variables as numbers (percentage). Fisher's exact test was used in univariate analysis to determine whether functional outcome was independent of each variable tested. The odds ratio was outputted for each variable calculated.
Survival and functional outcome analysis for multiple variables was performed for both the ≤ 6 h time window and the >6 h time window. For the >6 h group the collateral status was drawn up (Figure 2). At this point, it shall be mentioned that this is no Kaplan Meier analysis as the follow up time is the same for every patient. The follow up interval for survival was recorded at baseline until 90 days of survival. A qualified stroke and study nurse obtained the mRS information via phone interview. Patients lost to follow up were excluded from this study.
Figure 2.
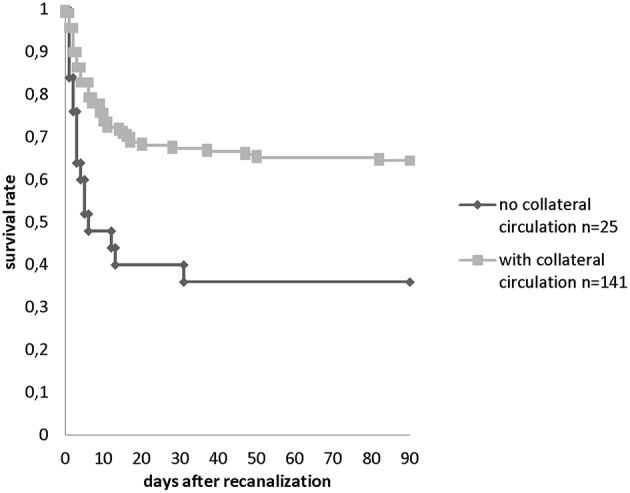
Survival rate within 90 days in patients with collaterals (n = 133 PCOMA and n = 8 SCA-PICA) and without collaterals (n = 25) observed in the >6 h TTR group.
AUC-ROC curves were calculated for admission NIHSS and 24 h NIHSS, pre-interventional PC-APECTS as per CCT or cMRI.
Wilcoxon matched pairs signed rank test was performed to test for a difference in the median NIHSS improvement (assessed at admission and 24 h after admission) stratified by mRS 0–2 and mRS 3–6.
Reliability of interobserver agreement was calculated to enable assessment of occlusion patterns and collateral status using Cohen's kappa. Value ranges from 0–0.20 as slight, 0.21–0.40 as fair, 0.41–0.60 as moderate, 0.61–0.80 as substantial, and 0.81–1 as almost perfect agreement (15).
Any data sets with discrepancies were reviewed in a group with mutual agreement achieved in each case.
A separate multivariate analysis (logistic regression) was performed for 87 patients to analyze for separate influence of early neurological improvement (assessed in NIHSS improvement) on functional outcome and mortality.
To analyze for separate influence of different covariates (gender, age, hypertension, collateral status, PCOMA status, SCA-PICA collateral status, time to recanalization, year of treatment, TICI score, and post-interventional hemorrhage) on functional outcome and mortality at 90 days logistic regression models were applied.
Level of significance was set at p < 0.05.
The program Stata/IC 13.1 for Windows (StataCorp LP, College Station, Texas, USA) was used for the statistical analysis.
Results
Background and Demographic Data
We identified 231 patients (100%) that met our inclusion criteria. Mortality at 90 days was 36.8% (n = 85), favorable outcome (mRS 90d 0–2) was achieved in 29.4% (n = 68). The median (min. – max.) age was 75 (19–110) years, with the majority of patients being male (n = 131, 57%). Pre-and post-interventional NIHSS at 24 h was available for 87 (100%) patients. 56 (64%) patients had a NIHSS ≥9. Out of these 56 patients 32.1% (n = 17) had early neurological improvement <9. The median NIHSS at admission was 14 [(0–42) n = 155]. Median 24 h NIHSS was 6 [(0–33) n = 110]. The median time to recanalization from symptom onset was 6.4 h (2.5–20.4). Only a minority of 31 patients (9.4%) received iv rtPA as the vast majority (165, 71.4%) received treatment beyond 6 h from symptom onset. In the latter group, stroke onset had not been witnessed for 81 (35.1%) patients.
Stroke Burden/PC-ASPECTS Pre-interventional
Pre-interventional PC-ASPECTS with MRI were attained for 62 (26.8%) patients. For the majority of patients (n = 155, 67%) a score for pre-interventional PC-ASPECTS had to be reached via CCT.
A pre-interventional PC-ASPECTS of ≤ 7 was recorded for 24 patients based on MRI and for 13 patients using CCT. A pre-interventional ASPECTS of >7 was determined for 38 patients using MRI and for 181 patients based on CCT.
Collaterals
Cohen's Kappa for interobserver agreement was 0.84 for the sites of occlusion and 0.91 for the collateral status.
Collateral supply was analyzed, with the dataset stratified into two groups by time to recanalization (TTR). One hundred ninety seven patients (85.3%) had collaterals. One hundred eighty three patients (79.3%) had at least one PCOMA. Thirty five patients (15.1%) were being supplied via the PICA-superior cerebellar artery (SCA) pathway. In the over 6 h group, 133 patients (57.6%) had a collateralization via at least one PCOMA while in the under 6 h TTR subgroup, 50 patients (21.6%) had at least one PCOMA.
Collateral status and pre-interventional stroke burden depicted by pre-interventional PC-ASPECTS was inconsistent regarding prediction of functional outcome and mortality. The median PC-ASPECTS with CCT was 10 irrespective of collateral status. This finding is due to the technical weakness of CCT for acute stroke in posterior fossa.
In cMRI Median PC-ASPECTS was eight if collaterals were present and 7.5 with no collaterals. This marginal effect was most likely caused by the small number of pre-interventional cMRI scans.
Occlusion Patterns
The most frequent occlusion pattern was the distal third 69.7% (n = 161) followed by occlusion of the middle third (17.3% n = 40) and the proximal third (3.4% n = 8). It was most common for one third of the basilar trunk to be occluded (45.6% n = 151), while occlusion of two thirds was seen in 25.1% of cases (n = 58). Total occlusion of the basilar trunk was recorded in 22 patients (9.5%) (Table 1).
Table 1.
1a Mortality over 90 days (mRS90d 0–5 vs. 6) occlusion patterns. 1b Survival over 90 days (mRS90d 0– vs. 6) and collateral status.
| n | % | mRS 0–5 | mRS 6 | OR (95%-KI) | p-value* | p-value** | ||
|---|---|---|---|---|---|---|---|---|
| A | ||||||||
| Occlusion basilar trunk | Total | 22 | 9.5 | 12 (54.5%) | 10 (45.5%) | Ref. | 0.474 | |
| 2/3 | 58 | 25.1 | 40 (69.0%) | 18 (31.0%) | 0.54 (0.20–1.48) | 0.295 | ||
| 1/3 | 151 | 65.4 | 100 (66.2%) | 51 (33.8%) | 0.61 (0.25–1.51) | 0.341 | ||
| Occlusion 1/3 | Distal | 122 | 80.8 | 79 (64.8%) | 43 (35.2%) | Ref. | 0.105 | |
| Middle | 21 | 13.9 | 13 (61.9%) | 8 (38.1%) | 1.13 (0.43–2.95) | 0.809 | ||
| Prox | 8 | 5.3 | 8 (100%) | 0 (0%) | - | 0.052 | ||
| Time to recanalization >6 h | Total | 4 | 6.1 | 1 (25.0%) | 3 (75.0%) | Ref. | 0.036 | |
| 2/3 | 24 | 36.4 | 21 (87.5%) | 3 (12.5%) | 0.05 (0.00–0.63) | 0.022 | ||
| 1/3 | 38 | 57.6 | 30 (78.9%) | 8 (21.1%) | 0.09 (0.01–0.99) | 0.049 | ||
| B | ||||||||
| Collateral status | No collaterals | 34 | 14.7 | 15 (44.1%) | 19 (55.9%) | Ref. | 0.006 | |
| Collaterals present | 197 | 85.3 | 137 (69.5%) | 60 (30.5%) | 0.35 (0.16–0.73) | |||
| PCOMA | Both patent | 112 | 49.8 | 85 (75.9%) | 27 (24.1%) | Ref. | 0.002 | |
| 1 patent | 71 | 31.6 | 42 (59.2%) | 29 (40.8%) | 2.17 (1.14–4.13) | 0.021 | ||
| Absent | 42 | 18.7 | 20 (47.6%) | 22 (52.4%) | 3.46 (1.64–7.30) | 0.002 | ||
| SCA PICA | Absent | 195 | 84.8 | 129 (66.2%) | 66 (33.8%) | Ref. | 0.442 | |
| 1 patent | 18 | 7.8 | 13 (72.2%) | 5 (27.8%) | 0.75 (0.26–2.20) | 0.795 | ||
| Both patent | 17 | 7.4 | 9 (52.9%) | 8 (47.1%) | 1.74 (0.64–4.72) | 0.296 | ||
| PCOMA status in distal occlusion | Both patent | 76 | 49.0 | 56 (73.7%) | 20 (26.3%) | Ref. | 0.008 | |
| 1 patent | 46 | 29.7 | 30 (65.2%) | 16 (34.8%) | 1.49 (0.67–3.31) | 0.413 | ||
| Absent | 33 | 21.3 | 14 (42.4%) | 19 (57.6%) | 3.80 (1.61–8.99) | 0.002 | ||
| PCOMA status stratified by time to recanalization >6 h | Patent | 82 | 50.9 | 58 (70.7%) | 24 (29.3%) | Ref. | 0.003 | |
| Patent/absent | 50 | 31.1 | 29 (58.0%) | 21 (42.0%) | 1.75 (0.84–3.66) | 0.185 | ||
| Absent | 29 | 18.0 | 10 (34.5%) | 19 (65.5%) | 4.59 (1.86–11.34) | 0.001 | ||
| Non-witnessed | Patent | 40 | 50.6 | 26 (65.0%) | 14 (35.0%) | Ref. | 0.070 | |
| PCOMA | Patent/absent | 25 | 31.6 | 15 (60.0%) | 10 (40.0%) | 1.24 (0.44–3.49) | 0.793 | |
| Absent | 14 | 17.7 | 4 (28.6%) | 10 (71.4%) | 4.64 (1.22–17.69) | 0.028 | ||
| Witnessed | Patent | 72 | 49.3 | 59 (81.9%) | 13 (18.1%) | Ref. | 0.006 | |
| PCOMA | Patent/absent | 46 | 31.5 | 27 (58.7%) | 19 (41.3%) | 3.19 (1.38–7.42) | 0.010 | |
| Absent | 28 | 19.2 | 16 (57.1%) | 12 (42.9%) | 3.40 (1.30–8.92) | 0.019 | ||
Global p-value,
p-value for each subgroup if exceeding more than two subgruops.
Treatment Time and Time to Recanalization
The median duration of treatment was 1.4 h (0.9–2.3). In 38.4% (n = 88) of cases, treatment was longer than 1 h but shorter than 2 h. In 26.2% (n = 60) of patients, treatment procedures lasted over 2 h. There was no effect regarding prediction of functional outcome and mortality.
Stent retrievers were used for 77.5% of patients (n = 179) whereas aspiration was used as the primary method of mTE in 15.2% (n = 35).
In 64.5% of patients, mTICI 2b-3 was achieved after 1 passage. At the end of the procedure, mTICI 2b-3 was achieved in 93.5% of patients (n = 221).
From 2008 to 2010, the pCRC device was predominantly used for mTE (47.2% n = 17), followed by Solitaire stent retrievers (25% n = 9), pBONNET stent retrievers (22.2% n = 8) and a few pREset devices (5.6% n = 2). In 2011 to 2013, pREset devices were used in most cases (86.5%, n = 90) followed by Solitaire (6.7% n = 7) and pBONNET devices (5.8%, n = 6) another 1% were other devices.
From 2014 to 02/2019, in most cases (42.8% n = 39) the pREset device was used followed by SOFIA Plus aspiration catheters (38.5% n = 35). In 14.2% of cases (n = 13) pREset in combination with SOFIA Plus aspiration catheters were used. In 4.3% (n = 4) of procedures, other stent retriever devices were used.
Pre and Post-op Clinical and Radiological Follow-Up
Asymptomatic ICH occurred in 8.7% (n = 20) and symptomatic ICH was seen in 6% (n = 14) of patients.
Statistical Analysis
Good Outcome mRS 90 days 0–2 vs. 3–6.
Bivariate analysis comparing good clinical outcome (mRS 0–2) with poor clinical outcome (mRS 3–6) showed no gender effect (Table 2). A positive history of smoking (n = 25 10.8%) was associated with a good outcome (p = 0.02) and diabetes mellitus (n = 61) was associated with poor outcome (p = 0.001) (Table 2). Neither a history of hypertension (p = 0.7) nor hypercholesterolaemia had an effect on clinical outcome (Table 2). The location of the clot in the proximal, middle, or distal third of the basilar artery did not have statistical significance for functional outcome nor did clots involving 2/3rds of the basilar artery or total occlusions (Table 3). Furthermore, there was no difference regarding different occlusion patterns of the cerebellar arteries (PICA, anterior inferior cerebellar artery AICA, SCA). NIHSS assessment at baseline could predict functional outcome. Compared to patients with 0–4 NIHSS points, patients with an NIHSS range beginning at 12 points had next to no chance of a good functional outcome. None of the patients with a baseline NIHSS (n = 155) of ≥28 had a good functional outcome (Table 2).
Table 2.
Functional outcome at 90 days (mRS90d 0–2 vs. 3–6) and baseline characteristics.
| n | % | mRS 3–6 | mRS 0–2 | OR (95%-KI) | p-value* | p-value** | ||
|---|---|---|---|---|---|---|---|---|
| Gender | Female | 100 | 43.3 | 67 (67.0%) | 33 (33.0%) | Ref. | 0.311 | |
| Male | 131 | 56.7 | 96 (73.3%) | 35 (26.7%) | 0.74 (0.42–1.31) | |||
| Age | <70 | 79 | 34.2 | 50 (63.3%) | 29 (36.7%) | Ref. | 0.155 | |
| 70–79 | 84 | 36.4 | 60 (71.4%) | 24 (28.6%) | 0.69 (0.36–1.33) | 0.316 | ||
| ≥80 | 68 | 29.4 | 53 (77.9%) | 15 (22.1%) | 0.49 (0.23–1.02) | 0.071 | ||
| Symptom onset | Non-witnessed | 82 | 35.5 | 64 (78.0%) | 18 (22.0%) | Ref. | 0.071 | |
| Witnessed | 149 | 64.5 | 99 (66.4%) | 50 (33.6%) | 1.80 (0.96–3.36) | |||
| Diabetes mellitus | No | 128 | 67.7 | 79 (61.7%) | 49 (38.3%) | Ref. | 0.001 | |
| Yes | 61 | 32.3 | 52 (85.2%) | 9 (14.8%) | 0.28 (0.13–0.62) | |||
| Cholesterol | No | 130 | 68.8 | 94 (72.3%) | 36 (27.7%) | Ref. | 0.130 | |
| Yes | 59 | 31.2 | 36 (61.0%) | 23 (39.0%) | 1.67 (0.87–3.20) | |||
| Smoker | No | 159 | 86.4 | 115 (72.3%) | 44 (27.7%) | Ref. | 0.020 | |
| Yes | 25 | 13.6 | 12 (48.0%) | 13 (52.0%) | 2.83 (1.20–6.69) | |||
| Hypertension | No | 38 | 17.4 | 28 (73.7%) | 10 (26.3%) | Ref. | 0.844 | |
| Yes | 180 | 82.6 | 127 (70.6%) | 53 (29.4%) | 1.17 (0.53–2.58) | |||
| Pre-PCASPECT cMRI | ≤ 7 | 24 | 38.7 | 18 (75.0%) | 6 (25.0%) | Ref. | 0.188 | |
| >7 | 38 | 61.3 | 22 (57.9%) | 16 (42.1%) | 2.18 (0.70–6.79) | |||
| Pre-PCASPECT cCT | ≤ 7 | 13 | 8.4 | 10 (76.9%) | 3 (23.1%) | Ref. | 0.760 | |
| >7 | 142 | 91.6 | 101 (71.1%) | 41 (28.9%) | 1.35 (0.35–5.19) | |||
| Admission NIHSS | 0–4 | 27 | 17.4 | 7 (25.9%) | 20 (74.1%) | Ref. | <0.001 | 0.067 |
| 5–11 | 35 | 22.6 | 18 (51.4%) | 17 (48.6%) | 0.33 (0.11–0.98) | <0.001 | ||
| 12–22 | 53 | 34.2 | 44 (83.0%) | 9 (17.0%) | 0.07 (0.02–0.22) | <0.001 | ||
| 23–27 | 18 | 11.6 | 16 (88.9%) | 2 (11.1%) | 0.04 (0.01–0.24) | <0.001 | ||
| ≥28 | 22 | 14.2 | 22 (100%) | 0 (0%) |
Global p-value,
p-value for each subgroup if exceeding more than two subgruops.
Table 3.
Functional outcome at 90 days (mRS90d 0–2 vs. 3–6), occlusion patterns, and collateral status.
| n | % | mRS 3–6 | mRS 0–2 | p-value* | OR (95%-KI) | p-value** | ||
|---|---|---|---|---|---|---|---|---|
| Occlusion basilar trunk | Total | 22 | 9.5 | 15 (68.2%) | 7 (31.8%) | 0.791 | Ref. | |
| 2/3 | 58 | 25.1 | 43 (74.1%) | 15 (25.9%) | 0.75 (0.26–2.19) | 0.588 | ||
| 1/3 | 151 | 65.4 | 105 (69.5%) | 46 (30.5%) | 0.94 (0.36–2.46) | 1.000 | ||
| Occlusion 1/3 | Distal | 122 | 80.8 | 87 (71.3%) | 35 (28.7%) | 0.571 | Ref. | |
| Middle | 21 | 13.9 | 13 (6–1.9%) | 8 (38.1%) | 1.53 (0.58–4.02) | 0.442 | ||
| Proximal | 8 | 5.3 | 5 (62.5%) | 3 (37.5%) | 1.49 (0.34–6.61) | 0.691 | ||
| n | % | mRS 3–6 | mRS 0–2 | OR (95%-KI) | p-value* | p-value** | ||
| Collateral status | No collaterals | 34 | 14.7 | 29 (85.3%) | 5 (14.7%) | Ref. | 0.043 | |
| Collaterals | 197 | 85.3 | 134 (68.0%) | 63 (32.0%) | 2.73 (1.01–7.39) | |||
| PCOMA | Patent | 112 | 49.8 | 70 (62.5%) | 42 (37.5%) | Ref. | 0.049 | |
| Patent/absent | 71 | 31.6 | 53 (74.6%) | 18 (25.4%) | 0.57 (0.29–1.09) | 0.107 | ||
| Absent | 42 | 18.7 | 34 (81.0%) | 8 (19.0%) | 0.39 (0.17–0.93) | 0.034 | ||
| SCA PICA | Absent | 195 | 84.8 | 139 (71.3%) | 56 (28.7%) | Ref. | 0.757 | |
| 1 patent | 18 | 7.8 | 12 (66.7%) | 6 (33.3%) | 1.24 (0.44–3.48) | 0.787 | ||
| Both patent | 17 | 7.4 | 11 (64.7%) | 6 (35.3%) | 1.35 (0.48–3.85) | 0.584 | ||
| PCOMA status in distal occlusion | Both patent | 76 | 49.0 | 47 (61.8%) | 29 (38.2%) | Ref. | 0.034 | |
| 1 patent | 46 | 29.7 | 35 (76.1%) | 11 (23.9%) | 0.51 (0.22–1.16) | 0.116 | ||
| Absent | 33 | 21.3 | 28 (84.8%) | 5 (15.2%) | 0.29 (0.10–0.84) | 0.024 | ||
| PCOMA status in proximal and middle occlusion | Both patent | 29 | 60.4 | 19 (65.5%) | 10 (34.5%) | Ref. | 0.397 | |
| 1 patent | 18 | 37.5 | 13 (72.2%) | 5 (27.8%) | 0.73 (0.20–2.68) | 0.753 | ||
| Absent | 1 | 2.1 | 0 (0%) | 1 (100%) | 0.367 | |||
| Non-witnessed onset and | Patent | 40 | 50.6 | 27 (67.5%) | 13 (32.5%) | Ref. | 0.130 | |
| PCOMA | Patent/absent | 25 | 31.6 | 22 (88.0%) | 3 (12.0%) | 0.28 (0.07–1.13) | 0.080 | |
| Absent | 14 | 17.7 | 12 (85.7%) | 2 (14.3%) | 0.35 (0.07–1.80) | 0.302 | ||
| Witnessed onset and | Patent | 72 | 49.3 | 43 (59.7%) | 29 (40.3%) | Ref. | 0.205 | |
| PCOMA | Patent/absent | 46 | 31.5 | 31 (67.4%) | 15 (32.6%) | 0.72 (0.33–1.56) | 0.440 | |
| Absent | 28 | 19.2 | 22 (78.6%) | 6 (21.4%) | 0.40 (0.15–1.12) | 0.103 | ||
| Time to recanalization ≤ 6 h | Patent | 30 | 46.9 | 15 (50.0%) | 15 (50.0%) | Ref. | 0.483 | |
| Patent/absent | 21 | 32.8 | 14 (66.7%) | 7 (33.3%) | 0.50 (0.16–1.60) | 0.266 | ||
| Absent | 13 | 20.3 | 8 (61.5%) | 5 (38.5%) | 0.63 (0.16–2.38) | 0.526 |
Global p-value,
p-value for each subgroup if exceeding more than two subgruops.
This finding was more marked in NIHSS assessment at 24 h (n = 110), as none of these patients assessed with NIHSS ≥ 23 achieved a good functional outcome (Table 4).
Table 4.
Functional outcome at 90 days (mRS90d 0–2 vs. 3–6) and post-interventional outcome screening.
| n | % | mRS 3–6 | mRS 0–2 | OR (95%-KI) | p-value* | p-value** | ||
|---|---|---|---|---|---|---|---|---|
| NIHSS at 24 h | 0–4 | 42 | 38.2 | 12 (28.6%) | 30 (71.4%) | Ref. | <0.001 | |
| 5–11 | 20 | 18.2 | 10 (50.0%) | 10 (50.0%) | 0.40 (0.13–1.21) | 0.155 | ||
| 12–22 | 28 | 25.5 | 26 (92.9%) | 2 (7.1%) | 0.03 (0.01–0.15) | <0.001 | ||
| 23–27 | 17 | 15.5 | 17 (100%) | 0 (0%) | <0.001 | |||
| ≥28 | 3 | 2.7 | 3 (100%) | 0 (0%) | 0.032 | |||
| Post-interventional ICH | No | 193 | 85.0 | 131 (67.9%) | 62 (32.1%) | Ref. | 0.014 | |
| Yes | 34 | 15.0 | 30 (88.2%) | 4 (11.8%) | 0.28 (0.09–0.84) | |||
| Post-interventional sICH | No | 190 | 93.1 | 136 (71.6%) | 54 (28.4%) | 0.023 | ||
| Yes | 14 | 6.9 | 14 (100%) | 0 (0%) |
Global p-value,
p-value for each subgroup if exceeding more than two subgruops.
A trend was observed for pre-interventional PC-ASPECTS. Patients with a cMRI PC-ASPECTS of >7 had a twofold chance of a good functional outcome. This effect was not significant due to the small sample size in MRI. Pre-interventional PC-ASPECTS using CT scans were inconclusive (Table 2).
AUC-ROC analysis of duration of treatment as a continuous variable did not differ in terms of predictive value regarding functional outcome. Neither did pre-interventional PC-ASPECT with CT or MRI.
Out of 87 patients with baseline and 24 h NIHSS 31 patients (35.6%) experienced good outcome and 56 patients (64.4%) had an unfavorable outcome. The median 24 h NIHSS for the patient group with favorable outcome was two compared to 20 in the group with unfavorable outcome. The difference in median of pre-interventional and 24 h NIHSS was significant (p < 0.001).
NIHSS at admission and at 24 h had a very good and significant discriminative power regarding good functional outcome in AUC-ROC analysis (ROC p < 0.001). AUC for each was >0.8.
Patients with TTR beyond 6 h had less than half the chance of good outcome (p = 0.025) compared to patients with a TTR of <6 h (Table 5). Patients with collaterals had an almost triple likelihood of a good outcome (p = 0.043) (Table 3). The probability of a good functional outcome was reduced by more than half if PCOMA was absent (Table 3). There was also a slight, non-significant correlation of a good outcome and PICA-SCA collaterals being present, whether these were unilateral or bilateral (Table 3).
Table 5.
Functional outcome at 90 days (mRS90d 0–2 vs. 3–6) and procedural parameters.
| n | % | mRS 0–2 | mRS 3–6 | OR (95%-KI) | p-value* | p-value** | ||
|---|---|---|---|---|---|---|---|---|
| Time to recanalization [h] | ≤ 6 h | 66 | 28.6 | 39 (59.1%) | 27 (40.9%) | Ref. | 0.025 | |
| >6 h | 165 | 71.4 | 124 (75.2%) | 41 (24.8%) | 0.48 (0.26–0.88) | |||
| Witnessed | Non-witnessed | 82 | 35.5 | 64 (78.0%) | 18 (22.0%) | Ref. | 0.071 | |
| Witnessed | 149 | 64.5 | 99 (66.4%) | 50 (33.6%) | 1.80 (0.96–3.36) | |||
| ≤ 6 h | Witnessed | 65 | 100.0 | 38 (58.5%) | 27 (41.5%) | |||
| >6 h | Non-witnessed | 82 | 49.4 | 64 (78.0%) | 18 (22.0%) | Ref. | 0.474 | |
| Witnessed | 84 | 50.6 | 61 (72.6%) | 23 (27.4%) | 1.34 (0.66–2.73) | |||
| Duration of | <1 h | 81 | 35.4 | 53 (65.4%) | 28 (34.6%) | Ref. | 0.256 | |
| Treat. [h] | ≥1 h | 88 | 38.4 | 62 (70.5%) | 26 (29.5%) | 0.79 (0.41–1.52) | 0.512 | |
| ≥2 | 60 | 26.2 | 47 (78.3%) | 13 (21.7%) | 0.52 (0.24–1.13) | 0.133 | ||
| Year of treatment | 2008–2010 | 36 | 15.6 | 32 (88.9%) | 4 (11.1%) | Ref. | 0.009 | |
| 2011–2019 | 195 | 84.4 | 131 (67.2%) | 64 (32.8%) | 3.91 (1.32–11.55) |
Global p-value,
p-value for each subgroup if exceeding more than two subgruops.
Surprisingly, the odds of a good functional outcome were reduced by 70% if PCOMA was absent through a distal occlusion in the basilar artery. However, the proximal or middle third being occluded did not have any effect on good functional outcome, this finding is most likely due to a small sample size (Table 3).
Post-interventional hemorrhage decreased the likelihood of good functional outcome by more than 70% This latter effect was particularly pronounced in patients with symptomatic post-interventional intracranial hemorrhages (sICH) as 100% did not achieve good functional outcomes (Table 4).
Multivariate analysis revealed both the time to recanalization and ICH to be predictors for functional outcome at 90 days. The likelihood of a good outcome was reduced by half if TTR was >6 h and by more than 70% if post-interventional hemorrhage was found (Table 6).
Table 6.
Multivariate analysis mRS 0–2 vs. 3–6 (n = 208).
| OR (95%-KI) | p-value* | ||
|---|---|---|---|
| Gender | Male vs. female | 0.85 (0.44–1.64) | 0.634 |
| Age | 70–79 vs <70 | 0.64 (0.29–1.41) | 0.268 |
| ≥80 vs. <70 | 0.56 (0.24–1.29) | 0.173 | |
| Hypertension | Yes vs. no | 1.17 (0.51–2.73) | 0.709 |
| Collaterals | Present vs. not present | 1.01 (0.17–5.92) | 0.995 |
| Time to recanalization | >6 h vs. ≤ 6 h | 0.47 (0.23–0.95) | 0.036 |
| Year of treatment | From 2011 vs. 2008–2010 | 3.95 (1.14–13.66) | 0.030 |
| Post image hemorrhage | Yes vs. No | 0.28 (0.08–0.98) | 0.046 |
| PCOMA status | Unilateral vs. bilateral | 0.54 (0.27–1.11) | 0.094 |
| Non vs. bilateral | 0.43 (0.09–1.97) | 0.275 |
Global p-value.
Patients treated from 2011 to the beginning of 2019 had an almost fourfold likelihood of a good outcome in comparison to patients treated in the earlier period of 2008–2010 (Table 6).
In a separate multivariate analysis with 87 patients NIHSS improvement was an independent predictor for good functional outcome [OR 1.28 (1.14–1.45) p < 0.001]. Latter finding should be interpreted with caution as the NIHSS was more likely missing for patients with mRS 90d 3–6.
Mortality
In bivariate analysis Risk of death over 90 days was high if the NIHSS had a value of 12–22 points, both for NIHSS at admission and at 24 h after admission. In each case, there was a 6-fold risk compared to patients with an NIHSS of 0–4 (Table 7).
Table 7.
Mortality over 90 days (mRS90d 0–5 vs. 6) and baseline assessment.
| n | % | mRS 0–5 | mRS 6 | OR (95%-KI) | p-value* | p-value** | ||
|---|---|---|---|---|---|---|---|---|
| Gender | Female | 100 | 43.3 | 70 (70.0%) | 30 (30.0%) | Ref. | 0.265 | |
| Male | 131 | 56.7 | 82 (62.6%) | 49 (37.4%) | 1.39 (0.80–2.43) | |||
| Alter | <70 | 79 | 34.2 | 56 (70.9%) | 23 (29.1%) | Ref. | 0.467 | |
| 70–79 | 84 | 36.4 | 52 (61.9%) | 32 (38.1%) | 1.50 (0.78–2.89) | 0.249 | ||
| ≥80 | 68 | 29.4 | 44 (64.7%) | 24 (35.3%) | 1.33 (0.66–2.66) | 0.480 | ||
| Pre-interventional NIHSS | 0–4 | 27 | 17.4 | 24 (88.9%) | 3 (11.1%) | Ref. | 0.005 | |
| 5–11 | 35 | 22.6 | 28 (80.0%) | 7 (20.0%) | 2.00 (0.46–8.64) | 0.491 | ||
| 12–22 | 53 | 34.2 | 29 (54.7%) | 24 (45.3%) | 6.62 (1.77–24.80) | 0.002 | ||
| 23–27 | 18 | 11.6 | 11 (61.1%) | 7 (38.9%) | 5.09 (1.10–23.61) | 0.064 | ||
| ≥28 | 22 | 14.2 | 12 (54.5%) | 10 (45.5%) | 6.67 (1.53–28.97) | 0.010 | ||
| Pre-interventional Aspect MRI | ≤ 7 | 24 | 38.7 | 13 (54.2%) | 11 (45.8%) | Ref. | 0.051 | |
| >7 | 38 | 61.3 | 30 (78.9%) | 8 (21.1%) | 0.32 (0.10–0.97) | |||
| Pre-interventional Aspect CT | ≤ 7 | 13 | 8.4 | 9 (69.2%) | 4 (30.8%) | Ref. | 1.000 | |
| >7 | 142 | 91.6 | 93 (65.5%) | 49 (34.5%) | 1.19 (0.35–4.06) |
Global p-value,
p-value for each subgroup if exceeding more than two subgruops.
Adjusted for 90-day mortality, the odds of death were reduced by more than half if collaterals were present. Collateral status did matter in the TTR over 6 h subgroup. The odds were reduced by 65 percent when compared to patients with no collaterals (Table 1).
If PCOMA was absent, the likelihood of death was 3.4 times as high as for patients with bilateral PCOMA present (Table 1). Patients with unilateral PCOMA had double the risk of dying compared to patients with bilateral PCOMA (Table 1). Stratified by occlusion patterns, patients with an occluded distal third had almost a four times higher risk of death if their PCOMA were also absent compared to patients who still had recourse to bilateral PCOMA (Table 1). Also considering the time window to treatment, the patients in the >6 h TTR subgroup whose PCOMA were also absent had a 4.5 times higher likelihood of dying compared to members of the same subgroup who still had both PCOMA present (Table 1). Furthermore, in bivariate analysis, the PCOMA status showed a trend toward helping predict mortality in strokes with both unwitnessed and witnessed onsets. This effect was significant for witnessed onsets and almost for unwitnessed. The likelihood of death was more than threefold higher if PCOMA was absent (Table 1).
Regarding occlusion patterns observed in the ≤ 6 h TTR the likelihood for death was reduced to more than 90% in comparison to total occlusion if partial occlusion was noted. This effect was not observed in the >6 h TTR (Table 1).
For patients in the TTR >6 h subgroup, we observed that likelihood of death was increased by a factor of 2.4 compared to the TTR within 6 h group (Table 8).
Table 8.
Mortality over 90 days (mRS90d 0–5 vs. 6) and periprocedural parameters.
| n | % | mRS 0–5 | mRS 6 | OR (95%-KI) | p-value* | p-value** | ||
|---|---|---|---|---|---|---|---|---|
| TTR [h] | ≤ 6 h | 65 | 28.1 | 52 (80.0%) | 13 (20.0%) | Ref. | 0.005 | |
| >6 h-m | 166 | 71.9 | 100 (60.2%) | 66 (39.8%) | 2.64 (1.33–5.23) | |||
| pCRC device | No | 214 | 92.6 | 146 (68.2%) | 68 (31.8%) | Ref. | 0.014 | |
| yes | 17 | 7.4 | 6 (35.3%) | 11 (64.7%) | 3.94 (1.39–11.11) | |||
| TICI score | 0–2a | 12 | 5.2 | 3 (25.0%) | 9 (75.0%) | Ref. | 0.004 | |
| 2b-3 | 219 | 94.8 | 149 (68.0%) | 70 (32.0%) | 0.16 (0.04–0.60) | |||
| Time to recanalization >6 h | 0–2a | 11 | 6.7 | 2 (18.2%) | 9 (81.8%) | Ref. | 0.007 | |
| 2b-3 | 154 | 93.3 | 98 (63.6%) | 56 (36.4%) | 0.13 (0.03–0.61) | |||
| Year of treatment | 2008–2010 | 36 | 15.6 | 16 (44.4%) | 20 (55.6%) | Ref. | 0.007 | |
| 2011–2019 | 195 | 84.4 | 136 (69.7%) | 59 (30.3%) | 0.35 (0.17–0.72) |
Global p-value,
p-value for each subgroup if exceeding more than two subgruops.
Looking at TICI scores, patients with a TICI of 2b-3 had a 80% lower probability of dying in comparison to patients with a TICI of 0–2a (Table 8).
If post-interventional hemorrhage occurred, these patients had an over 4-fold probability of dying. This effect was even more pronounced in patients with symptomatic hemorrhage (Table 9).
Table 9.
Survival over 90 days (mRS90d 0–5 vs. 6) and post-interventional outcome.
| n | % | mRS 0–5 | mRS 6 | p-value* | OR (95%-KI) | p-value** | ||
|---|---|---|---|---|---|---|---|---|
| NIHSS at 24 h | 0–4 | 42 | 38.2 | 38 (90.5%) | 4 (9.5%) | Ref. | <0.001 | |
| 5–11 | 20 | 18.2 | 19 (95.0%) | 1 (5.0%) | 0.50 (0.05–4.84) | 1.000 | ||
| 12–22 | 28 | 25.5 | 17 (60.7%) | 11 (39.3%) | 6.15 (1.70–22.22) | 0.006 | ||
| 23–27 | 17 | 15.5 | 4 (23.5%) | 13 (76.5%) | 30.87 (6.69–142.48) | <0.001 | ||
| ≥28 | 3 | 2.7 | 2 (66.7%) | 1 (33.3%) | 4.75 (0.34–65.52) | 0.304 | ||
| Post – interventional ICH | No | 193 | 85.0 | 136 (70.5%) | 57 (29.5%) | Ref. | <0.001 | |
| Yes | 34 | 15.0 | 12 (35.3%) | 22 (64.7%) | 4.37 (2.03–9.45) | |||
| Post – interventional sICH | No | 190 | 93.1 | 128 (67.4%) | 62 (32.6%) | Ref. | <0.001 | |
| Yes | 14 | 6.9 | 3 (21.4%) | 11 (78.6%) | 7.57 (2.03–28.21) |
Global p-value,
p-value for each subgroup if exceeding more than two subgruops.
Furthermore patients who were treated from the beginning of 2011 had mortality reduced to 0.35 (0.14–0.65) (p < 0.009) compared to patients treated in the years 2008–2010 (Table 8).
In multivariate analysis, independent influencing factors for mortality were post-interventional ICH (p < 0.001), collateral status (p = 0.03), and TICI score (p = 0.02) (Table 10). In a separate multivariate analysis with 87 patients NIHSS improvement was an independent predictor for mortality [OR 0.84 (0.77–0.92) p < 0.001]. Latter finding should be interpreted with caution as the NIHSS was more likely missing for patients with mRS 90d 3–6.
Table 10.
Multivariate analysis mortality (n = 208).
| OR (95%-KI) | p-value* | ||
|---|---|---|---|
| Gender | Male vs. female | 1.46 (0.74–2.9) | 0.277 |
| Age | 70–79 vs. <70 | 1.68 (0.75–3.79) | 0.208 |
| ≥80 vs. <70 | 1.29 (0.52–3.2) | 0.589 | |
| Hypertension | Yes vs. no | 0.78 (0.32–1.91) | 0.582 |
| Collaterals | Present vs. not present | 0.16 (0.03–0.87) | 0.034 |
| Time to recanalization | >6 h vs. ≤ 6 h | 1.98 (0.8–4.93) | 0.141 |
| Year of treatment | From 2011 vs. 2008–2010 | 0.57 (0.21–1.58) | 0.280 |
| Post-image hemorrhage | Yes vs. No | 5.35 (2.20–12.98) | <0.001 |
| PCOMA status | Unilateral vs. bilateral | 2.89(1.37–6.09) | 0.005 |
| Non vs. bilateral | 0.99 (0.22–4.53) | 0.994 | |
| TICI | 2b-3 vs. 0–2a | 0.19 (0.05–0.78) | 0.021 |
Global p-value.
Discussion
In our study on aBAO certain trends correlating to good functional outcome and to mortality over 90 days were observed.
In this respect, the 6 h TTR and post-interventional hemorrhage were most predictive for functional outcome at 90 days. In bivariate analysis, collateral status, diabetes mellitus, smoking status, year of treatment, admission NIHSS and 24 h NIHSS could predict functional outcome.
As regards mortality, in multivariate analysis the strongest predictive power was found for collateral/PCOMA status, post-interventional hemorrhage, and TICI score. In bivariate analysis, the following variables were associated with mortality over 90 days: collateral status (in particular collateral status in the beyond 6 h TTR group), devices used, year of treatment, sICH, admission NIHSS and 24 h NIHSS. The observed mortality rate was in line with other reports (1, 2).
The success of multiple recent trials (16–22) has led to mechanical thrombectomy becoming the gold standard of treatment for proximal large vessel occlusion of the anterior circulation. There are currently no randomized controlled trials to suggest that mechanical thrombectomy is a superior standard treatment for occlusions of the posterior circulation. Many centers perform mechanical thrombectomy for acute occlusions of the posterior circulation. However, the optimal selection criteria are yet to be identified. The current American Heart Association guidelines define them as a groin puncture time within 6 h of symptom onset with causative occlusion of the basilar artery (class IIb; level of evidence C) (23). There is conflicting evidence on the importance of the timing in aBAO. Several previous reports have suggested recanalization ≤ 6 h (24, 25) improves outcome whilst others have suggested the 6 h time window has little effect (2, 26, 27). The largest multicenter study with 592 patients in aBAO reported the worst outcome if recanalization took over 9 h (3). The same research group found that their patients had the best outcome if time to recanalization was <6 h (24). Recently published data (28) with 376 patients from the same registry found that time to treatment of more than 6 h was predictive of poor outcome. A multicenter report (27) with 100 patients found that time to treatment of <6 h was predictive of favorable outcome in patients with TICI 2b-3 after intervention.
Antithetically, there are findings from a large single center report with 184 patients by Strbian et al. (26) that suggest time to recanalization does not predict outcome. There was no information on the extent of the occlusion in aBAO or on collateral status and only a minority of patients−7%—received endovascular treatment. The Endostroke multi-center study (2) encompassing 148 patients could not predict outcome through time to recanalization. Information on the collateral status of individuals treated beyond 6 h was not collected. A recently published study (27) with 215 patients from two endovascular centers also could not predict outcome based on time of onset to treatment. Collateral status and type of occlusion were not factors considered.
In our study, patients with recanalization within <6 h from symptom had the best outcome. This finding is in line with the BASICS registry.
Now the reasonable question for the ambiguous findings regarding the TTR arises. Subsequently potential causes shall be discussed.
Collateral Status
It is widely accepted that pial collaterals are important in preserving brain tissue in anterior circulation strokes. However, published literature for aBAO in this context is scarce.
A study (29) with 149 patients found that PCOMA status could predict outcome at 1 month. Furthermore, there are few grading systems under discussion that link PCOMA status and clot burden to functional outcome (30, 31). None of these studies link their findings to the TTR.
In our study, we could observe the pronounced impact of collateral status on functional outcome and mortality, in particular in the >6 h TTR group. This might be due to the fact that collaterals become more vital the longer a vessel occlusion is present.
In terms of occlusion patterns it is a surprising finding that the presence of collaterals when the distal third is occluded is associated with both a good functional outcome and with reduced mortality. This might be pathophysiologically explained by head loss in the basilar artery and the subsequent suction effect from the anterior circulation via PCOMA. The missing effect of collaterals on other occlusion patterns is most likely a sample size issue. Moreover, distal occlusions were most frequently seen.
Another controversial debate in aBAO concerns thrombus length, functional outcome and survival. In a small study (32) with 32 patients, thrombus length was an independent marker for an unfavorable outcome. Other studies investigating length were not in line with this finding (33–35), however, two of these studies were explicitly looking at monosegmental occlusion of the basilar trunk. The one study (35) considering occlusion of two segments or more had a small sample size of 40 patients and found a trend of improved outcome or survival related to the extent of the occlusion in aBAO.
In our study, the extent to which the basilar artery was occluded did not predict functional outcome but could predict mortality if applied to the ≤ 6 h time window to treatment. Latter finding should be interpreted with caution as only three patients had a total occlusion.
In our study, successful reperfusion conveyed through a TICI score was a separate predictor for mortality. This finding, that patients with successful recanalization had a lower mortality rate, is in line with current literature (27). A limitation of our finding is the small sample size in the unsuccessful reperfusion group.
Pre-and Post-interventional Assessments
Rangaraju et al. (28) found that NIHSS at 24–48 h could predict functional outcome for 1 month in aBAO. Our study confirms this finding, extends the validity of this finding to 90 days and adds admission NIHSS as a further powerful tool to predict functional outcome over 90 days.
The results regarding early neurologic improvement were inconclusive due to a small sample size. Nevertheless a trend toward NIHSS improvement and functional outcome as well as mortality was observed.
In current literature, pre ASPECT scores for the posterior circulation are the subject of discussion. All share the view that native CCT is not suitable for evaluation of the PC-ASPECT. As in our study the vast majority received pre-interventional CCT pre-interventional PC-ASPECT scores were not predictive of functional outcome. Nevertheless, in the small number of patients who has a pre-interventional cMRI, a trend for predicting functional outcome using the PC-ASPECT score could indeed be seen. This latter trend is in line with current findings in literature (12, 36).
As recently published, symptomatic intracranial hemorrhage is associated with an unfavorable outcome (37, 38). In our study, intracranial hemorrhage was highly predictive for both an unfavorable functional outcome and for mortality. This might be due to the high percentage (41%) of symptomatic hemorrhages among ICH cases.
Furthermore, the year of treatment showed an impact on both functional outcome and mortality in bivariate analysis. This can be ascribed to the old fashioned pCRC devices still pre-dominantly used in mechanical thrombectomies in the period 2008–2010.
Furthermore, various patient characteristics are currently being discussed as possible predictors of outcome. A positive smoking status is being considered as a predictor of good outcome and is also known as the smoking paradox (27, 39). In our study, only 25 patients were smokers and generally relatively young, which might explain the better outcome (38, 40). Furthermore, this correlation disappeared in multivariate analysis.
In our cohort, diabetes mellitus was a predictor for poor functional outcome in bivariate analysis. Most reports (7, 25, 27, 28, 39, 41) on this topic are not in line with this observation in aBAO, instead suggesting that HbA1c could be a better parameter for comparison. Our data did not include information on HbA1c.
Limitations of this study are the retrospective single center design. A strength of this study is its sample size, to date the highest to be published from a single center.
Conclusion
Our data suggest that the time window to treatment, collateral status, reperfusion status, extent of occlusion and ICH in aBAO can predict functional outcome and mortality.
The most important finding of this study is that the time window to successful treatment seems to be dependent on collateral status and extent of occlusion. These findings may serve as an explanation for the ambiguous findings regarding the validity of the 6 h time window in aBAO. They might also be helpful for decision making regarding EVT in aBAO, especially as an increasing number of patients are being referred from primary or secondary care hospitals to specialized neuro centers where time from symptom onset is often considered when deciding how to best treat an aBAO. Furthermore, baseline NIHSS, NIHSS at 24 h and post-interventional ICH were good predictors for mRS at 90 days.
Data Availability
The datasets generated for this study are available on request to the corresponding author.
Ethics Statement
The study was approved by the ethics committee of the Regional Medical Board Baden-Württemberg, project number F-2012-077.
Patient consent was not obtained as data were analyzed anonymously.
Author Contributions
JR and HH contributed to the conception and design of the work, literature search, analysis and interpretation, and article drafting. MA, VH, PB, HB, and HH contributed to critical revision. All authors gave final approval of the version to be published.
Conflict of Interest Statement
MA and PB have proctoring and consulting agreements with phenox GmbH. HH is co-founder and shareholder of phenox GmbH and femtos GmbH. JR, VH, and HB report no potential conflict of interest.
Acknowledgments
The authors are most grateful to L. Bloom for language revision of the manuscript. Hiltrud Niggemann for her support in statistical analysis and Casjupea Knispel, stroke and study nurse of the Neuroradiological Clinic for participating in data collection and data maintenance.
References
- 1.Gory B, Eldesouky I, Sivan-Hoffmann R, Rabilloud M, Ong E, Riva R, et al. Outcomes of stent retriever thrombectomy in basilar artery occlusion: an observational study and systematic review. J Neurol Neurosurg Psychiatry. (2016) 87:520–5. 10.1136/jnnp-2014-310250 [DOI] [PubMed] [Google Scholar]
- 2.Singer OC, Berkefeld J, Nolte CH, Bohner G, Haring H-P, Trenkler J, et al. Mechanical recanalization in basilar artery occlusion: the ENDOSTROKE study. Ann Neurol. (2015) 77:415–24. 10.1002/ana.24336 [DOI] [PubMed] [Google Scholar]
- 3.Schonewille WJ, Wijman CA, Michel P, Rueckert CM, Weimar C, Mattle HP, et al. Treatment and outcomes of acute basilar artery occlusion in the Basilar Artery International Cooperation Study (BASICS): a prospective registry study. Lancet Neurol. (2009) 8:724–30. 10.1016/S1474-4422(09)70173-5 [DOI] [PubMed] [Google Scholar]
- 4.Lindsberg PJ, Mattle HP. Therapy of basilar artery occlusion: a systematic analysis comparing intra-arterial and intravenous thrombolysis. Stroke. (2006) 37:922–8. 10.1161/01.STR.0000202582.29510.6b [DOI] [PubMed] [Google Scholar]
- 5.Schonewille WJ, Algra A, Serena J, Molina CA, Kappelle LJ. Outcome in patients with basilar artery occlusion treated conventionally. J Neurol Neurosurg Psychiatry. (2005) 76:1238–41. 10.1136/jnnp.2004.049924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hacke W, Zeumer H, Ferbert A, Brückmann H, del Zoppo GJ. Intra-arterial thrombolytic therapy improves outcome in patients with acute vertebrobasilar occlusive disease. Stroke. (1988) 19:1216–22. 10.1161/01.STR.19.10.1216 [DOI] [PubMed] [Google Scholar]
- 7.Mattle HP, Arnold M, Lindsberg PJ, Schonewille WJ, Schroth G. Basilar artery occlusion. Lancet Neurol. (2011) 10:1002–14. 10.1016/S1474-4422(11)70229-0 [DOI] [PubMed] [Google Scholar]
- 8.Kumar G, Shahripour RB, Alexandrov AV. Recanalization of acute basilar artery occlusion improves outcomes: a meta-analysis. J Neurointerv Surg. (2015) 7:868–74. 10.1136/neurintsurg-2014-011418 [DOI] [PubMed] [Google Scholar]
- 9.Huo Y, Phan K, Phan S, Jia F, Mortimer A. Outcomes of endovascular treatment of basilar artery occlusion in the stent retiever era: a systematic review and meta-analysis. J Vasc Interv Radiol. (2016) 27:S97 10.1016/j.jvir.2015.12.256 [DOI] [PubMed] [Google Scholar]
- 10.Chiang C-C, Dumitrascu OM, Wingerchuk DM, O'Carroll CB. Acute basilar artery occlusion. Does recanalization improve clinical outcome? A critically appraised topic. Neurologist. (2018) 23:71–4. 10.1097/NRL.0000000000000156 [DOI] [PubMed] [Google Scholar]
- 11.Janssen H, Brückmann H, Killer M, Heck S, Buchholz G, Lutz J. Acute basilar thrombosis: recanalization following intravenous thrombolysis is dependent on thrombus length. PLoS ONE. (2018) 13:e0193051. 10.1371/journal.pone.0193051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tei H, Uchiyama S, Usui T, Ohara K. Posterior circulation ASPECTS on diffusion-weighted MRI can be a powerful marker for predicting functional outcom. J Neurol. (2010) 257:767–73. 10.1007/s00415-009-5406-x [DOI] [PubMed] [Google Scholar]
- 13.Archer CR, Horenstein S. Basilar artery occlusion: clinical and radiological correlation. Stroke. (1977) 8:383–90. 10.1161/01.STR.8.3.383 [DOI] [PubMed] [Google Scholar]
- 14.Hacke W, Kaste M, Fieschi C, von Kummer R, Davalos A, Meier D, et al. Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Second European-Australasian Acute Stroke Study Investigators. Lancet. (1998) 352:1245–51. 10.1016/S0140-6736(98)08020-9 [DOI] [PubMed] [Google Scholar]
- 15.Gwet K. Handbook of Inter-Rater Reliability. 2nd ed Gaithersburg, MD: Advanced Analytics, LLC; (2010). [Google Scholar]
- 16.Campbell BCV, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. (2015) 372:1009–18. 10.1056/NEJMoa1414792 [DOI] [PubMed] [Google Scholar]
- 17.Saver JL, Goyal M, Diener H-C. Stent-retriever thrombectomy for stroke. N Engl J Med. (2015) 373:1078. 10.1056/NEJMc1508744 [DOI] [PubMed] [Google Scholar]
- 18.Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. (2015) 372:2296–306. 10.1056/NEJMoa1503780 [DOI] [PubMed] [Google Scholar]
- 19.Berkhemer OA, Fransen PSS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. (2015) 372:11–20. 10.1056/NEJMoa1411587 [DOI] [PubMed] [Google Scholar]
- 20.Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. (2015) 372:1019–30. 10.1056/NEJMoa1414905 [DOI] [PubMed] [Google Scholar]
- 21.Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. (2018) 378:708–18. 10.1056/NEJMoa1713973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. (2018) 378:11–21. 10.1056/NEJMoa1706442 [DOI] [PubMed] [Google Scholar]
- 23.Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC, et al. 2015 American Heart Association/American stroke association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American. Stroke. (2015) 46:3020–35. 10.1161/STR.0000000000000074 [DOI] [PubMed] [Google Scholar]
- 24.Vergouwen MDI, Algra A, Pfefferkorn T, Weimar C, Rueckert CM, Thijs V, et al. Time is brain(stem) in basilar artery occlusion. Stroke. (2012) 43:3003–6. 10.1161/STROKEAHA.112.666867 [DOI] [PubMed] [Google Scholar]
- 25.Mokin M, Sonig A, Sivakanthan S, Ren Z, Elijovich L, Arthur A, et al. Clinical and procedural predictors of outcomes from the endovascular treatment of posterior circulation strokes. Stroke. (2016) 47:782–8. 10.1161/STROKEAHA.115.011598 [DOI] [PubMed] [Google Scholar]
- 26.Strbian D, Sairanen T, Silvennoinen H, Salonen O, Kaste M, Lindsberg PJ. Thrombolysis of basilar artery occlusion: impact of baseline ischemia and time. Ann Neurol. (2013) 73:688–94. 10.1002/ana.23904 [DOI] [PubMed] [Google Scholar]
- 27.Bouslama M, Haussen DC, Aghaebrahim A, Grossberg JA, Walker G, Rangaraju S, et al. Predictors of good outcome after endovascular therapy for vertebrobasilar occlusion stroke. Stroke. (2017) 48:3252–7. 10.1161/STROKEAHA.117.018270 [DOI] [PubMed] [Google Scholar]
- 28.Rangaraju S, Jovin TG, Frankel M, Schonewille WJ, Algra A, Kappelle LJ, et al. Neurologic examination at 24 to 48 hours predicts functional outcomes in basilar artery occlusion stroke. Stroke. (2016) 47:2534–40. 10.1161/STROKEAHA.116.014567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.van der Hoeven EJ, McVerry F, Vos JA, Algra A, Puetz V, Kappelle LJ, et al. BASICS registry investigators. collateral flow predicts outcome after basilar artery occlusion: the posterior circulation collateral score. Int J Stroke. (2016) 11:768–75. 10.1177/1747493016641951 [DOI] [PubMed] [Google Scholar]
- 30.Alemseged F, Shah DG, Diomedi M, Sallustio F, Bivard A, Sharma G, et al. The basilar artery on computed tomography angiography prognostic score for basilar artery occlusion. Stroke. (2017) 48:631–7. 10.1161/STROKEAHA.116.015492 [DOI] [PubMed] [Google Scholar]
- 31.Da Ros V, Meschini A, Del Giudice C, Garaci F, Neuroradiology A, Stanzione P, et al. Proposal for a vascular computed tomography-based grading system in posterior circulation stroke : a single-center experience. J Stroke Cerebrovasc Dis. (2016) 25:368–77. 10.1016/j.jstrokecerebrovasdis.2015.10.008 [DOI] [PubMed] [Google Scholar]
- 32.Gilberti N, Gamba M, Premi E, Costa A, Vergani V, Delrio I, et al. Endovascular mechanical thrombectomy in basilar artery occlusion: variables affecting recanalization and outcome. J Neurol. (2016) 263:707–13. 10.1007/s00415-016-8047-x [DOI] [PubMed] [Google Scholar]
- 33.Shu L, Riedel C, Meyne J, Jansen O, Jensen-Kondering U. Successful recanalization in acute basilar artery occlusion treated with endovascular therapy is independent of thrombus length. J Neurointerv Surg. (2017) 9:1047–52. 10.1136/neurintsurg-2016-012634 [DOI] [PubMed] [Google Scholar]
- 34.Brandt T, von Kummer R, Müller-Küppers M, Hacke W. Thrombolytic therapy of acute basilar artery occlusion. Variables affecting recanalization and outcome. Stroke. (1996) 27:875–81. 10.1161/01.STR.27.5.875 [DOI] [PubMed] [Google Scholar]
- 35.Arnold M, Nedeltchev K, Schroth G, Baumgartner RW, Remonda L, Loher TJ, et al. Clinical and radiological predictors of recanalisation and outcome of 40 patients with acute basilar artery occlusion treated with intra-arterial thrombolysis. J Neurol Neurosurg Psychiatry. (2004) 75:857–62. 10.1136/jnnp.2003.020479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Khatibi K, Nour M, Tateshima S, Jahan R, Duckwiler G, Saver J, et al. Posterior circulation thrombectomy – pcASPECT score applied to pre-intervention MRI can accurately predict functional outcome. World Neurosurg. (2019) 129:e566–71. 10.1016/j.wneu.2019.05.217 [DOI] [PubMed] [Google Scholar]
- 37.Valentino F, Gentile L, Terruso V, Mastrilli S, Aridon P, Ragonese P, et al. Frequency and determinants for hemorrhagic transformation of posterior cerebral stroke: posterior ischemic stroke and hemorrhagic transformation. BMC Res Notes. (2017) 10:1–6. 10.1186/s13104-017-2889-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Phan K, Phan S, Huo YR, Jia F, Mortimer A. Outcomes of endovascular treatment of basilar artery occlusion in the stent retriever era: a systematic review and meta-analysis. J Neurointerv Surg. (2016) 8:1107–15. 10.1136/neurintsurg-2015-012089 [DOI] [PubMed] [Google Scholar]
- 39.Kufner A, Nolte CH, Galinovic I, Brunecker P, Kufner GM, Endres M, et al. Smoking-thrombolysis paradox: recanalization and reperfusion rates after intravenous tissue plasminogen activator in smokers with ischemic stroke. Stroke. (2013) 44:407–13. 10.1161/STROKEAHA.112.662148 [DOI] [PubMed] [Google Scholar]
- 40.Hussein HM, Niemann N, Parker ED, Qureshi AI. Searching for the smoker's paradox in acute stroke patients treated with intravenous thrombolysis. Nicotine Tob Res. (2017) 19:871–6. 10.1093/ntr/ntx020 [DOI] [PubMed] [Google Scholar]
- 41.Nagel S, Kellert L, Möhlenbruch M, Bösel J, Rohde S, Ringleb P. Improved clinical outcome after acute basilar artery occlusion since the introduction of endovascular thrombectomy devices. Cerebrovasc Dis. (2013) 36:394–400. 10.1159/000356185 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.


