Abstract
The biochemical demands associated with tumor proliferation prompt neoplastic cells to augment the import of nutrients to sustain their survival and fuel cell growth, with a consequent metabolic remodeling. Fatty acids (FA) are crucial in this process, since they have a dual role as energetic coins and building blocks. Recently, our team has shown that FATP1 has a pivotal role in FA transfer between breast cancer cells (BCCs) and non-cancerous cells in the microenvironment. We aimed to investigate the role of FATP1 in BCCs and also to explore if FATP1 inhibition is a promising therapeutic strategy. In patients’ data, we showed a higher expression of FATP1/SLC27A1 in TNBC, which correlated with a significant decreased overall survival (OS). In vitro, we verified that FA and estradiol stimulated FATP1/SLC27A1 expression in BCCs. Additionally, experiments with estradiol and PHTPP (ER-β antagonist) showed that estrogen receptor-β (ER-β) regulates FATP1/SLC27A1 expression, the uptake of FA and cell viability, in four BCC lines. Furthermore, the inhibition of FATP1 with arylpiperazine 5k (DS22420314) interfered with the uptake of FA and cell viability. Our study, unraveled FATP1 as a putative therapeutic target in breast cancer (BC).
Subject terms: Prognostic markers, Breast cancer
Introduction
Breast cancer (BC) is the most frequent malignant neoplasia in women worldwide, with an estimated 1.7 million cases and 521,900 deaths in 2012, accounting for 25% of all cancer cases and 15% of all cancer deaths among females1. The tumor microenvironment is well recognized to play a major role in the development and progression of cancer2. The non-neoplastic cells of the tumor microenvironment including fibroblasts, adipocytes, immune and endothelial cells seem to be determinant in cancer biology since they act as a functional network in which soluble factors and organic molecules are transiently shared3. Cancer associated fibroblasts (CAFS) may be the predominant cellular component of the tumor microenvironment and are known to express aromatase, a key enzyme in estrogen synthesis, resulting in the production of intra-tumoral estrogen frequently observed in BC4. Moreover, besides being essential for normal growth and differentiation in the mammary gland, estrogen plays an important role in the development and progression of BC5. Estrogen action is mediated by binding to estrogen receptor (ER)-α and/or ER-β which act as transcription factors6. Although encoded by different genes, both isoforms show similar functional and structural characteristics, interacting similarly with endogenous estrogens, mainly 17β-estradiol7. The classification of ER positive and ER negative BCs is based only on the presence of ER-α in their nuclei8, without considering the expression of ER-β. Accordingly, therapies that interfere with estrogen signaling such as estrogen antagonists (tamoxifen) and aromatase inhibitors have been developed and clinically implemented for the treatment of ER-positive BC9. However, these drugs have unwanted side effects in non-target tissues and some carcinomas become resistant10. Presently, only ER-α has been used in a clinical setting, since its protein levels are elevated in BCs compared with normal tissue, while ER-β is being more disregarded. ER-β mRNA was reported to be significantly upregulated in tamoxifen-resistant BCs compared with tamoxifen-sensitive tumors, suggesting a link between ER-β overexpression and tamoxifen resistance11. ER-β prognostic and predictive value remains controversial, however, targeting this receptor in some cases could offer new treatment options for BC patients12. Compared with hormone receptor-positive BCs, triple-negative BCs (TNBC) are associated with a worse prognosis and more aggressive phenotypes13. Since patients with TNBC do not benefit from hormonal based therapies, there is a great need to identify treatment options.
To fulfill the biosynthetic demands associated with proliferation and consequent tumor growth, cells must increase the import of nutrients that is supported and supports a metabolic remodeling14. In a proliferative tumor niche, fatty acids (FA) are crucial since they are both fuel and construction blocks, maintaining cell renewal and division15,16.
Conceptually, adipocytes are the main suppliers of FA, however, we previously reported that cancer associated fibroblasts (CAFs) also function as hubs of FA to supply the needs of cancer cells15. Breast cancer cells (BCCs) exposed to CAFs-conditioned media increased their lipid uptake and the expression of FATP1/SLC27A1 (FA transport protein 1), promoting FA transfer. FATP1 is an integral membrane protein known to enhance the uptake of long-chain and very long-chain FA into cells17. Considering FA transfer from CAFs to BCCs, FATP1 appears to be a suitable candidate to treat BC and a possible marker of disease outcome.
In the present study, we further investigated the role of FATP1 in breast cancer cells (BCCs) survival and behavior and explored a new therapeutic strategy. We demonstrated that FA and estradiol stimulate FATP1/SLC27A1 expression and we unraveled the crucial role of ER-β in FATP1/SLC27A1 regulation and modulation in the uptake of FA. Our in vitro findings were supported by patients’ data showing a higher expression of FATP1/SLC27A1 in more aggressive and invasive BCs. Furthermore, the inhibition of FATP1 with arylpiperazine 5k (DS22420314) interfered with the uptake of FA and cell proliferation, validating the importance of FATP1 as a putative therapeutic target in BC.
Results
FATP1/SLC27A1 expression is associated to triple negative BC (TNBC) and correlates with lower overall survival (OS) and relapse free survival (RFS) times
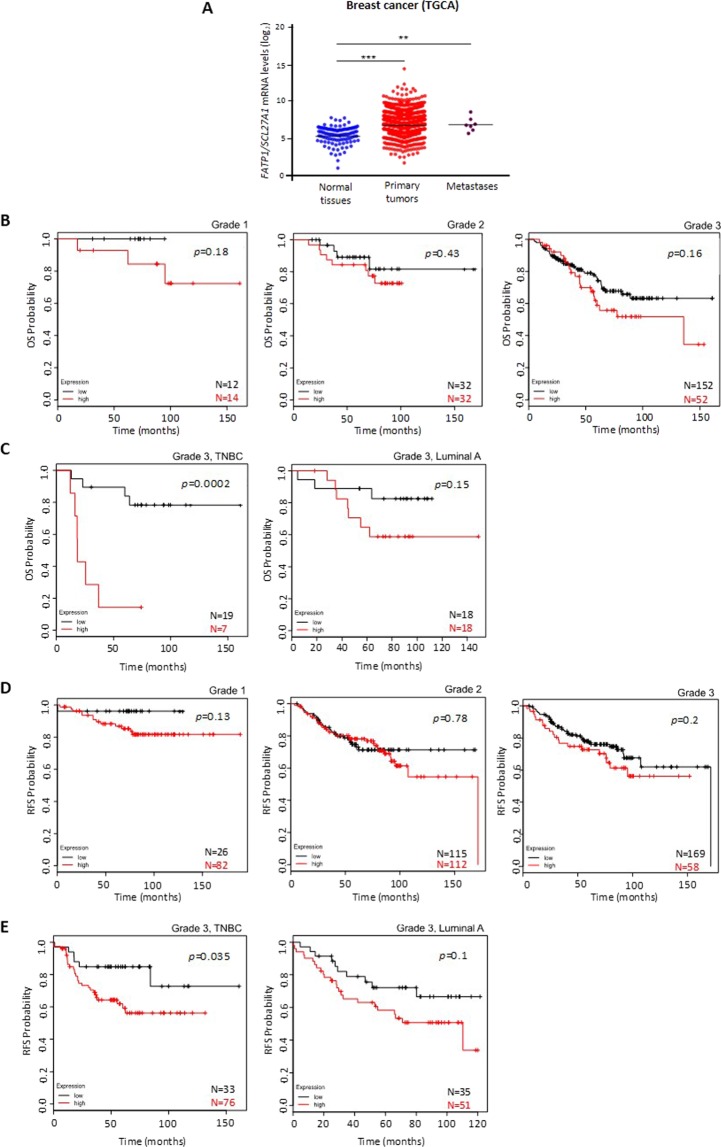
At first, to understand the impact of FATP1/SLC27A1expression in BC patients, we analyzed data extracted from the TCGA database. Considering BC patients and the expression of FATP1/SLC27A1, it was shown that BCs and metastasis express higher levels of FATP1/SLC27A1 than normal breast tissue (Fig. 1A).
Figure 1.
Patients with higher levels of FATP1/SLC27A1 expression have a lower OS and RFS. (A) Analysis of FATP1/SLC27A1 expression profiles in normal breast tissue, primary carcinomas and metastasis, data extracted from the TCGA database. A two-tailed unpaired Student’s t-test with Welch’s correction was used. Comparison of the overall survival (OS) and relapse free survival (RFS) curves of GEO database patients with high levels of FATP1 (red line) and low levels of FATP1 (black line) expression using Kaplan-Meier method. (B) Kaplan-Meier survival curves for patients with BC grade 1 (n = 26), grade 2 (n = 64) and grade 3 (n = 204). (C) Kaplan-Meier survival curves for patients with grade 3, TNBC BC (n = 26) and grade 3, luminal A BC (n = 36). (D) Kaplan-Meier RFS curves for patients with BC grade 1 (n = 108), grade 2 (n = 227) and grade 3 (n = 227). (E) Kaplan-Meier survival curves for patients with grade 3, TNBC BC (n = 108) and grade 3, luminal A BC (n = 86).
To determine the relevance of the expression levels of the FATP1/SLC27A1 gene on the clinical outcome of BC patients, a Kaplan-Meier Plotter analysis18 was employed, using data from Gene Expression Omnibus (GEO) database. Overall survival (OS) in BC patients was determined in grade 1 (N = 26), grade 2 (N = 64) and grade 3 (N = 204), with high (red line) and low (black line) expression of FATP1/SLC27A1. Despite being not significant, a trend in decreased OS was observed with high FATP1/SLC27A1 expression and increased tumor grade (Fig. 1B). Looking at two different subtypes of grade 3 BCs: TNBC (N = 26) and luminal A (N = 36), with respectively high and low levels of FATP1/SLC27A1; the OS was significantly lower in patients with carcinomas with high levels of FATP1/SLC27A1 (Fig. 1C).
Relapse free survival (RFS) time analysis was assessed in grade 1 (N = 108), grade 2 (N = 227) and grade 3 (N = 227) BC patients with high and low expression of FATP1/SLC27A1 (Fig. 1D) and also at the two different subgroups of grade 3 tumors: TNBC and luminal A. Patients with grade 3 disease and with high expression of FATP1/SLC27A1 showed a lower RFS comparing with grade 1 and 2 patients. As shown in Fig. 1E, grade 3 BC patients, with a TNBC (109 patients), with high FATP1/SLC27A1 expression (red line) displayed a significantly lower RFS than patients with low FATP1/SLC27A1 expression (black line). A similar observation was registered for grade 3, luminal A patients (86 patients) but no statistical significance was obtained.
In breast tumor sections, the expression profile of FATP1 protein showed a statistically significant (p = 0.015) association with TNBC subtype of BC (Table 1).
Table 1.
Immunohistochemical analysis of FATP1 expression in BC sections.
| FATP1 positivity | p value | |
|---|---|---|
| TNBC | 65% (13/20) | 0.015 |
| Luminal A | 26.3% (5/19) |
The expression of FATP1 positivity is associated with triple negative BC (TNBC; p = 0.015) but not with luminal A type of BC. Immunohistochemical data was analyzed using univariate analysis (two-tailed t-test) on SPSS software.
Linoleic acid (C18) and estradiol stimulate FATP1 expression and estradiol stimulates the binding of ER-β to FATP1/SLC27A1 promoter
Afterwards, we intended to evaluate the modulation of FATP1/SLC27A1 expression in BCCs. The first screening was performed in MDA-MB-231, which is a TNBC cell line, representing the tumors in which the outcome in the clinical setting was worst and correlated with high expression of FATP1/SLC27A1. As we previously described, FATP1 mediates the uptake of FA by cancer cells15 and because the promoter region of FATP1/SLC27A1 gene has estrogen responsive elements (ERE), we tested the effect of linoleic acid (C18) and estradiol in FATP1/SLC27A1 expression. The TNBC molecular subtype is characterized also by the lack of estrogen receptor, however this characterization is performed only based on ER-α expression, ignoring the ER-β. That is why we thought it would be worth testing the effect of estradiol in FATP1/SLC27A1 expression.
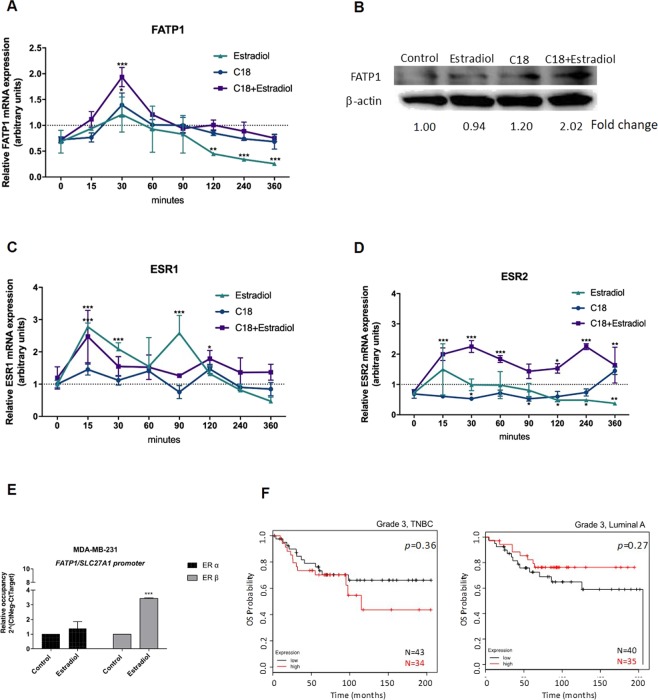
In order to evaluate the modulation of FATP1/SLC27A1, MDA-MB-231 cells were exposed to C18 and estradiol, in separate and in combination. FATP1 mRNA levels were significantly higher in MDA-MB-231 cells after 30 min of stimulation with C18 and C18 plus estradiol (Fig. 2A), indicating that cell lines benefit from FATP1/SLC27A1 expression to cope with the increased levels of C18. The significant decrease of FATP1/SLC27A1 mRNA in cells exposed only to estradiol shows that, without C18 boost, the stimulation of FATP1/SLC27A1 expression by estradiol is not required in this cell line. At the protein levels and reinforcing the role of estradiol and C18 on FATP1/SLC27A1 expression, FATP1 protein levels increase upon C18 and C18 plus estradiol stimuli in a much longer timepoint of 16 h (Fig. 2B).
Figure 2.
Linoleic acid (C18) and estradiol stimulate FATP1/SLC27A1 expression and estradiol stimulates the binding of ER-β to FATP1/SLC27A1 promoter (A) FATP1/SLC27A1, (C) ESR1 and (D) ESR2 expression levels in MDA-MB-231 cells in a pulse chase experiment referenced to the control condition. (B) Western blotting for FATP1 detection, the numbers are indicative of fold change of each condition (normalized for the respective β-actin) in relation to control. (C) ESR1 and (D) ESR2 expression levels in MDA-MB-231 cells in a pulse chase experiment referenced to the control condition. In relative qPCR, hypoxanthine-guanine phosphoribosyltransferase (HPRT) gene was used as housekeeping gene. (E) Relative occupancy of ER-α and ER-β at FATP1/SLC27A1 promoter. Cells were cultured in control and in estradiol conditions and ER-α and ER-β binding was assessed by ChIP. Data are mean ± error bars of biological triplicates, only adherent cells were analyzed, dead cells in culture media were discarded. (F) Kaplan-Meier survival curves for patients with grade 3, TNBC (n = 77) and grade 3, luminal A BC (n = 75) for the ESR2 gene. *p < 0.05 **p < 0.01 ***p < 0.001. (*) represents the statistical analysis in relation to control condition (dot line). For pulse chase qPCR experiments a Two-way ANOVA with Tukey’s test was used.
As aforementioned, FATP1/SLC27A1 gene has ERE sequences in its promoter region, so we also evaluated the pulse chase dynamics of ESR1 (encodes ER-α) and ESR2 (encodes ER-β) genes expression. It was very interesting to see that the expression of ESR2 was significantly higher in cells exposed to C18 + estradiol, in all timepoints (Fig. 2D), whereas ESR1 showed a significant up and down expression in a few timepoints and related to estradiol exposure (Fig. 2C).
In order to find a functional link between ER-α or ER-β with the regulation of FATP1/SLC27A1 gene expression, a ChIP assay was performed. The relative occupancy of ER-β in FATP1/SLC27A1 promoter significantly increased upon estradiol stimulation (Fig. 2E). We observed no differences in the relative occupancy of ER-α in the FATP1/SLC27A1 promoter.
Regarding ESR2 (encoding ER-β) expression in the clinical setting, patients with TNBC (N = 77) with high levels of ESR2 expression showed a lower survival rate, although this association was not significant. The opposite was observed in luminal A group (Fig. 2F).
FATP1/SLC27A1 expression is regulated by ER-β
To confirm the role of ER-β on FATP1/SLC27A1 expression, we assessed FATP1 levels by flow cytometry upon the exposure to an ER-β antagonist (PHTPP) with estradiol and/or C18. For that, we used MDA-MB-231 and also MCF7, a luminal A cell line. In order to exclude the interference of ER-α, cells were also tested with MPP and Fulvestrant, antagonists of ER-α. The concentrations of ER-α and ER-β antagonists and agonists were selected from the literature19–21.
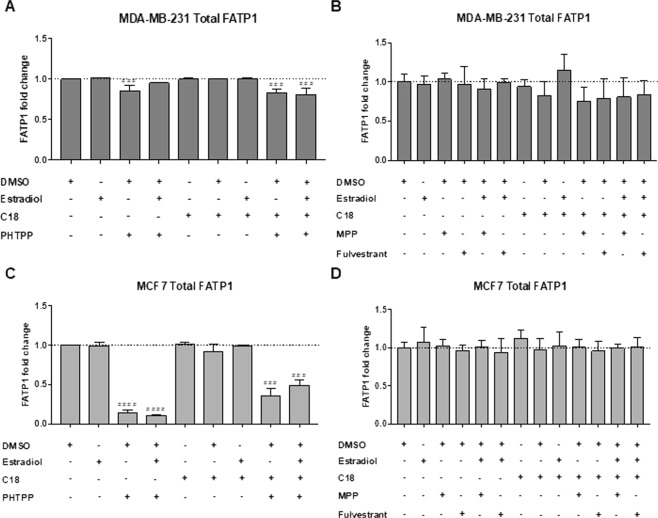
The amount of total FATP1 positive cells was significantly lower when MDA-MB-231 and MCF7 cells were treated with the ER-β antagonist (PHTPP) (Fig. 3A,C). MPP and Fulvestrant (ER-α antagonists) showed non-significant changes in FATP1 levels (Fig. 3B,D).
Figure 3.
FATP1 is downregulated in BCCs treated with PHTPP. BCCs were cultured in control (baseline culture medium represented by the dot line), control DMSO, estradiol and/or C18 conditions, in the presence or absence of PHTPP (A,C) and in the presence or absence of MPP and Fulvestrant (B,D), being analyzed by flow cytometry. Values are referenced to control/DMSO conditions within each cell line. Biological triplicates were tested, only adherent cells were analyzed and dead cells in culture media were discarded. Results are shown as mean ± SD. *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001. (*) represents the statistical analysis in relation to control condition and (#) represents the statistical analysis in relation to DMSO condition. One-way ANOVA with Dunnett’s multiple comparisons test.
Breast cancer (BC) FA uptake is regulated by ER-β
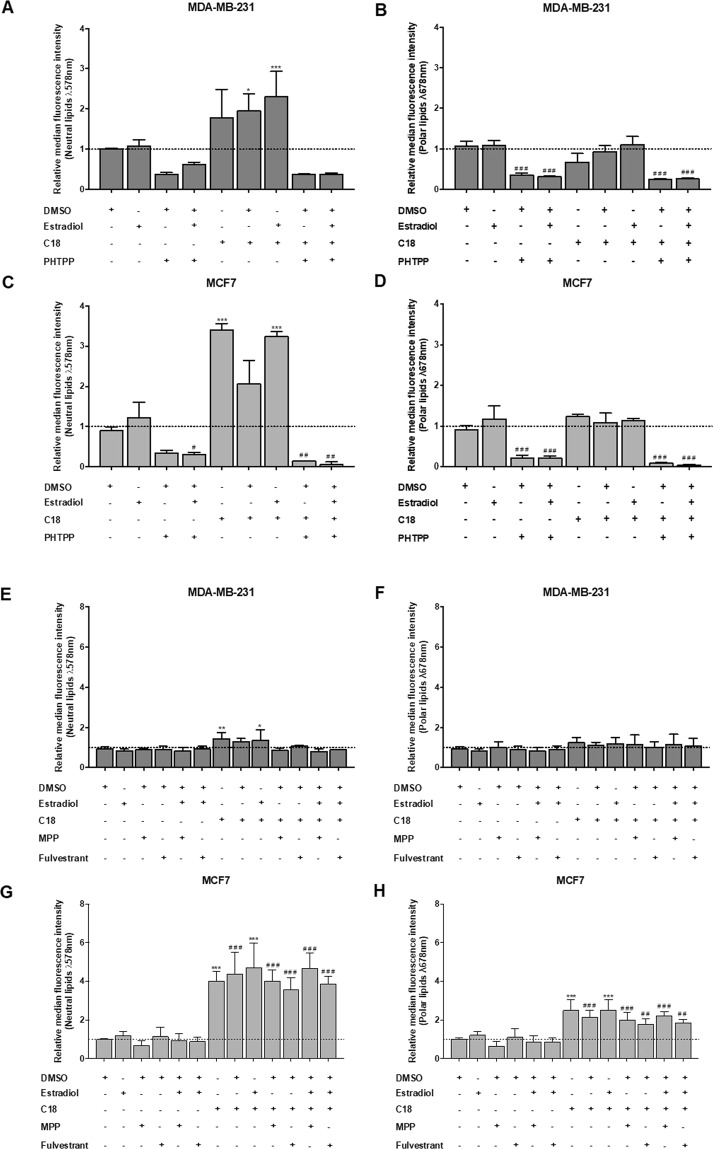
To evaluate if the dynamics of FATP1 regulation, by estradiol, interfere with the FA uptake, a flow cytometry assay was performed using Nile Red labelling (Fig. 4). PHTPP, MPP and Fulvestrant were tested, with and without C18. MDA-MB-231 cells exposed to C18 plus estradiol showed a significant uptake of neutral lipids (Fig. 4A). When cells were exposed to PHTPP, the uptake of FA was decreased, being statistically significant in the polar lipids in both cell lines (Fig. 4A–D). C18 and estradiol in separate led to a higher uptake of neutral lipids in MCF7 cells. The effect of MPP and Fulvestrant in the FA uptake was also evaluated. These antagonists did not interfere with the FA uptake when comparing with the control conditions as shown in Fig. 4E–H. These findings indicate that ER-β is important in the uptake of FA, since its inhibition decreased the levels of FA. We can also observe that C18 in combination with estradiol is associated with an enhanced uptake of FA that might be transported by FATP1.
Figure 4.
MDA-MB-231 and MCF7 cells exposed to PHTPP accumulate less FA. Cells were cultured in control (baseline culture medium represented by the dot line), control DMSO, estradiol and/or C18 conditions, in the presence or absence of PHTPP (A–D) or in the presence or absence of MPP and Fulvestrant (E–H). A flow cytometry analysis of Nile red staining was performed to evaluate the accumulation of neutral (λ 578 nm) and polar (λ 678 nm) lipids. Values are referenced to control/DMSO conditions within each cell line. Biological triplicates were tested, only adherent cells were analyzed and dead cells in culture media were discarded. Results are shown as mean ± SD. *p < 0.05, **p < 0.01, ***p < 0.001. (*) represents the statistical analysis in relation to control condition and (#) represents the statistical analysis in relation to control DMSO condition. One-way ANOVA with Dunnett’s multiple comparisons test.
Breast cancer cells (BCCs) viability is regulated by ER-β
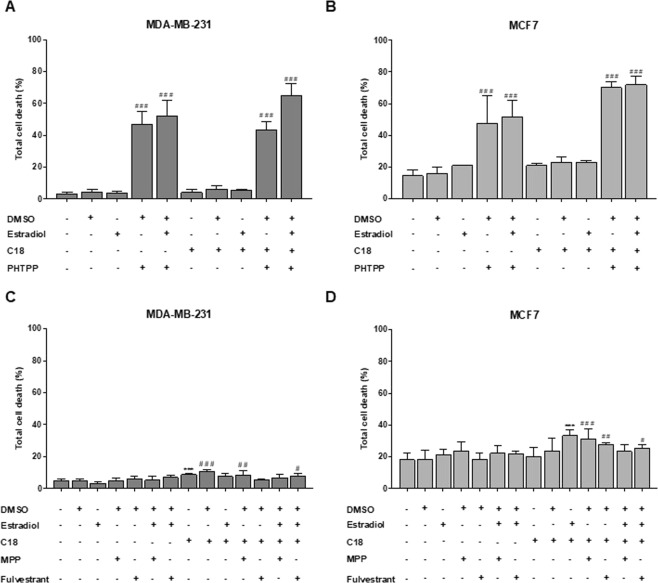
We performed a cell viability assay to evaluate the effect of PHTPP, an ER-β antagonist, in cells cultured in the presence or absence of estradiol with or without C18. Figures 5A,B show that PHTPP, with and without C18, caused a significant increase in cell death in both cell lines while the other conditions did not affect cell viability. Comparing with DMSO condition, MDA-MB-231 and MCF7 cells display similar levels of cell death upon exposure to PHTPP. These results indicate that ER-β plays a role in both cell lines survival.
Figure 5.
PHTPP affects cell viability of MDA-MB-231 and MCF7. Cells were cultured in control, control DMSO, estradiol and/or C18 conditions, in the presence or absence of PHTPP (A,B) or in the presence or absence of MPP and Fulvestrant (C,D) and were analyzed by flow cytometry. Results are shown as mean ± SD. *p < 0.05, **p < 0.01, ***p < 0.001. (#) represents the statistical analysis in relation to DMSO condition. Biological triplicates were tested, adherent cells were dead cells in culture media were analyzed. One-way ANOVA with Dunnett’s multiple comparisons test.
Regarding MPP and Fulvestrant (ER-α antagonists), these compounds affected cell viability in a much lower extent than PHTPP (Fig. 5C,D). These results were expected for MDA-MB231 cell line because it is a TNBC cell line22,23. Regarding the assay testing the effect of MPP and Fulvestrant in MDA-MB-231, we observed that C18 and C18 plus estradiol induced slightly higher levels of cell death, though significant when compared with the control.
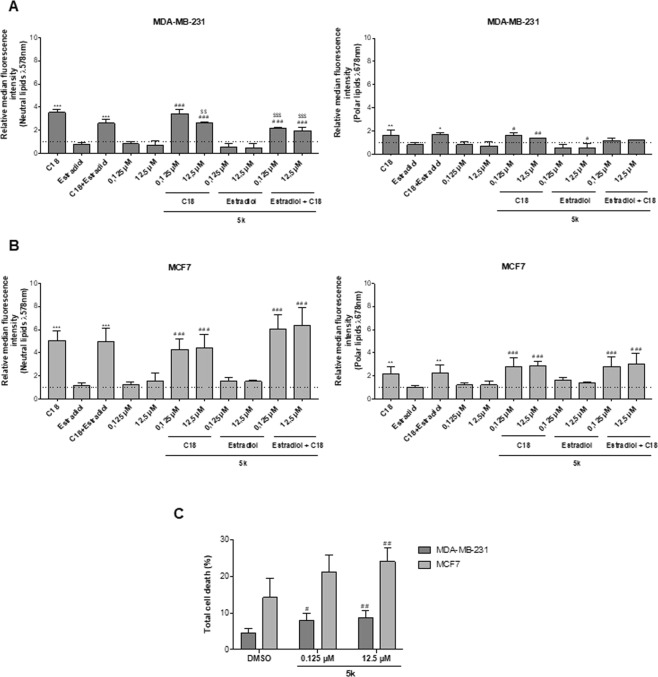
Arylpiperazine 5k (DS22420314) impairs FA uptake and decreases cell viability
Since the results suggested that FA and estradiol, via ER-β, are relevant in the regulation of FATP1/SLC27A1 and since this gene is upregulated in high grade BCs, mainly TNBC, we hypothesized that the pharmacological inhibition of FATP1 might be a strategy to fight cancer. To test this therapeutic approach, cells were exposed to arylpiperazine 5k (DS22420314)24, a compound that acts as a FATP1 inhibitor, interfering with the transport of FA across the cell membrane.
The uptake of FA in cells exposed to arylpiperazine 5k (DS22420314) (0.125 and 12.5 μM) was assessed by flow cytometry using Nile red, in MDA-MB-231 and MCF7 cells cultured in control, control DMSO and estradiol with and without C18. In Fig. 6, C18 exposure led to a significant increase in FA uptake in comparison with control cells (dot line), in both cell lines. MDA-MB-231 cells tended to accumulate less neutral and polar lipids when cultured both in the presence of estradiol and/or 5k (Fig. 6A). A significant decrease in FA uptake was observed in 5k exposed cells comparatively to cells that were only exposed to C18. It is of note that the higher concentration of 5k (12.5 μM) led to a lower uptake of neutral lipids, indicating a dose-dependent effect.
Figure 6.
Arylpiperazine 5k (DS22420314) interferes with FA uptake and cell viability. Cells were cultured in control, control DMSO, estradiol with and without C18 and exposed to arylpiperazine 5k (DS22420314). Nile red labelling was analyzed by flow cytometry in MDA-MB-231 cells (A) and MCF7 cells (B). Cell death assay was performed in cells exposed to arylpiperazine 5k (DS22420314) and compared to control and control DMSO, using flow cytometry using Annexin V and PI (C). Values are referenced to control/DMSO conditions within each cell line. Data are means of biological triplicates. Results are shown as mean ± SD. *p < 0.05, **p < 0.01, ***p < 0.001. (*) represents the statistical analysis in relation to the control condition; (#) statistical analysis in relation to the DMSO condition; ($) statistical analysis in relation to the C18 condition. Biological triplicates were tested, adherent cells were dead cells in culture media were analyzed. The dot line defines the relative median fluorescence intensity for the control conditions. Multiple comparisons were performed using One-way ANOVA with Dunnett’s or Tukey’s test.
MDA-MB-231 exhibited a lower uptake of neutral lipids when cells were cultured in estradiol and 5k, in separate or in combination (Fig. 6A). In MCF7, when 5k was combined with C18 with and without estradiol an accumulation of neutral and polar lipids was observed (Fig. 6B). Thus, the treatment with arylpiperazine 5k (DS22420314) had an impact in lipid uptake in an environment rich in FA, mimicked by C18 supplementation, in MDA-MB-231 cells but not in MCF7 cells.
With the intent of analyzing the effect of arylpiperazine 5k (DS22420314) on cell viability, a cell death assay was carried out. In MDA-MB-231 cells, the total percentage of cell death was significantly higher in cells cultured in the two concentrations of 5k, comparing to control DMSO (Fig. 6C). In the MCF7 cell line, similar results were obtained but only the higher concentration of 5k showed significant higher cell death levels (Fig. 6C).
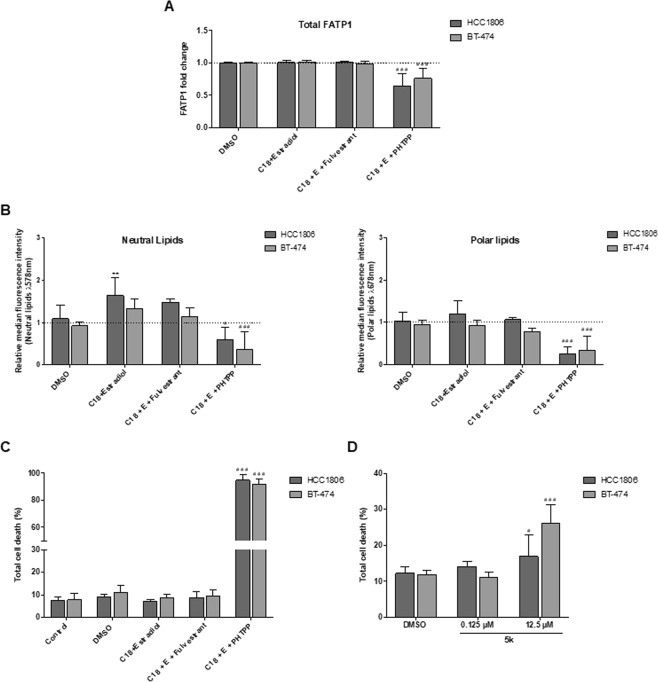
Validation of results in additional breast cancer cell (BCC) lines
In order to confirm the reliability of results within BC context, we performed pivotal assays in two additional BCC lines (HCC1806, TNBC and BT-474, Luminal B).
The effect of the ER-β antagonist (PHTPP) and ER-α antagonist (Fulvestrant) was evaluated in these cells to validate the role of ER-β on FATP1/SLC27 A1 expression. In both cell lines, the amount of total FATP1 positive cells was significantly reduced when ER-β was blocked with the addition of the antagonist PHTPP (Fig. 7A).
Figure 7.
ER-β signaling regulates the expression of FATP1 and FA uptake in BT-474 and HCC1806 cells. BT-474 and HCC1806 cells were cultured in control, control DMSO, estradiol and C18 conditions, in the presence or absence of Fulvestrant and PHTPP (A–C). Cells were also exposed to arylpiperazine 5k and compared to control DMSO (D). Total FATP1/SLC27A1 expression was analyzed by flow cytometry (a). Nile red labelling was analyzed to evaluate the accumulation of neutral (λ 578 nm) and polar (λ 678 nm) lipids by flow cytometry (B). Cell death assay was performed with flow cytometry using Annexin V and PI (C,D). Values are referenced to control/DMSO conditions within each cell line. Results are shown as mean ± SD. *p < 0.05, **p < 0.01, ***p < 0.001. (*) represents the statistical analysis in relation to control condition and (#) represents the statistical analysis in relation to DMSO condition. Biological triplicates were tested, only adherent cells were analyzed and dead cells in culture media were discarded; except in cell death analysis in which adherent and dead cells were analyzed together. Multiple comparisons were performed using One-way ANOVA with Dunnett’s or Tukey’s test.
Regarding lipid uptake, a significant increase in neutral lipids was observed in HCC1806 cells when treated with C18 in combination with estradiol. No further differences were observed among conditions expect for the C18 plus estradiol and PHTPP condition showing a significant decrease in FA accumulation in both cell lines (Fig. 7B) corroborating our previous results.
Cell death analysis was also performed and once again the blockage of ER-β resulted in a significant increase in cell death while the other conditions did not affect cell viability suggesting that ER-β signaling supports BCCs survival (Fig. 7C). Fulvestrant did not affect neither FA accumulation nor cell viability, reinforcing the crucial role of ER-β in BCCs.
To explore the role of arylpiperazine 5k derivative (DS22420314) in cell viability, cells were exposed to two different concentrations of the drug (0.125 μM and 12.5 μM). Total cell death increased significantly in cells exposed to 12.5 μM of 5k (Fig. 7D). Arylpiperazines had a higher impact on BT-474 cells resulting in a greater cell death comparing to HCC1806.
This set of results is in agreement with our previous findings suggesting that ER-β plays an important role in FATP1 regulation and trafficking supporting cell survival.
Discussion
Metabolic remodeling leads to changes in biosynthetic and bioenergetic pathways not only in neoplastic cells but also in non-cancerous cells in the same microenvironment25. This cellular and molecular network sustains the high demand for energy and biomass production which are essential for cancer initiation and progression26. In breast and ovarian cancer cells it was stated that tumor microenvironment promotes tumor growth and provides a rationale for the development of targeted therapies that block cancer metabolism fueled by the microenvironment27,28. Recently, our team15 has published that cancer associated fibroblasts (CAFs) cooperate with BCCs as FA suppliers, in in vitro and in vivo models, through the FA transporter FATP1. Aberrant lipid metabolism has long been recognized as a major metabolic event during cancer development29. However, most of the studies have been focused on de novo lipogenesis as the source for FA required for tumor cell growth, where the role of exogenous FA often disregarded30–32. The present work focuses on the uptake of exogenous FA by BCCs rather than on the de novo FA synthesis, considering the role of FATP1 as a mediator of FA transport. In addition, we also addressed ER-β as a regulator of FATP1/SLC27A1 gene expression.
Most studies have been investigating FATP1 in the context of diet induced obesity, insulin resistance, hyperglycemia, hyperinsulinemia and hypertension33–36. To our knowledge, this is the first study that investigates the role of FATP1 in BC. Besides all the mechanistic experiments, our results also showed a statistically significant association between FATP1 expression and TNBC subtype, based on histochemistry analysis of breast tumors. Moreover, it was found that metabolic genes such as SLC27 genes, including FATP1/SLC27A1, may be altered in metastatic cancer cells and are associated with poor prognosis37, as we observed in results from TCGA and GEO databases for BC. In other cancer contexts, an expression array analysis demonstrated that FATP1/SLC27A1 expression is up-regulated in vitro and in human intrahepatic cholangiocarcinoma samples38. In addition, FATP1/SLC27A1 mRNA was increased in rat hepatomas in comparison with normal liver tissue which correlated with FA uptake rates39. Accordingly, the FATP1 protein expression was evaluated in biopsies of patients with melanoma and it was found that 44% of samples overexpressed FATP1 specifically in the tumor cell compartment40.
Kaplan-Meier curves revealed that patients with upregulated expression of FATP1/SLC27A1 showed lower overall survival (OS) and relapse free survival (RFS) in comparison with patients with low expression of FATP1/SLC27A1 being even more apparent in more advanced stages of the disease (grade 3) (Fig. 1). Moreover, OS in grade 3 triple negative BC patients (TNBC) with high FATP1/SLC27A1 expression was significantly lower than OS in grade 3, luminal A patients. These findings reveal that the FATP1/SLC27A1 gene is undoubtedly relevant on the clinical outcome of BC as more aggressive and invasive carcinomas (TNBC) exhibit a significantly upregulated expression of FATP1/SLC27A1. These results were in agreement with the in vitro assays, since MDA-MB-231 cell line is from TNBC subtype. In that way, FATP1 can be considered as a marker for disease outcome. Interestingly and reinforcing the role of ER-β in the regulation of FATP1/SLC27A1 expression, the TNBC group of tumors expressing high levels of ESR2 showed low OS and the luminal A group showed high OS. Unfortunately, the software used did not allow the multivariate analysis in order to analyze the OS and the RFS in patients that co-express ESR2 and FATP1/SLC27A1. The expression of ER-β and/or FATP1 is a promising way of identifying a subset of tumors in such a heterogeneous and indefinite subtype of BC, TNBC. A shortcoming in the analysis of BC databases is the fact that most of them are organized according to tumors staging and histological type and not the molecular subtype, which would be the element we intend to clarify in this paper issue. We believe the low number of cases classified according to the molecular subtype of BC is the main cause for the non-significant differences in RFS and OS between TNBC and luminal A cases. Nevertheless, the statistical significance in OS and RFS between TNBC grade 3 tumors expressing high levels versus low levels of FATP1/SLC27A1, is a strong indication that FATP1 plays a role in BC progression and outcome, suggesting that its usefulness as an outcome marker and therapeutic target deserves to be explored.
Our team have previously published that MDA-MB-231 exposed to CAFs exhibited a decreased FASN activity and an increased FATP1/SLC27A1 transcriptional expression suggesting that BCCs change their metabolic profile from FA producers to FA gatherers15. Hence, our first experimental approach was to verify the expression of the FATP1/SLC27A1 gene in MDA-MB-231 (TNBC), which is considered a highly aggressive and invasive cell line22,23. We also found that MDA-MB-231 cells exposed to C18 and estradiol showed higher FATP1/SLC27A1 levels (Fig. 2A,B), suggesting that enhanced FATP1/SLC27A1 expression is correlated with more aggressive phenotypes, being in agreement with the increased expression of FATP1/SLC27A1 in TNBC subtype and the association with poor outcome of the disease (Fig. 1). Overall, the pulse chase assay showed that FATP1/SLC27A1 mRNA levels are dynamic, with a significant increase after 30 min of C18 and C18 plus estradiol exposure, indicating that MDA-MB-231 cell line benefits from FATP1/SLC27A1 expression in these conditions (Fig. 2A), to mediate the uptake of FA. Accordingly, cells exposed only to estradiol showed an accentuated and significant decrease of FATP1/SLC27A1 mRNA with time (Fig. 2A). Because, without C18 boost, the stimulation of FATP1/SLC27A1 expression by estradiol is not needed and negative feedback mechanisms may abrogate the expression of FATP1/SLC27A1. However, more detailed experiments on mRNA turnover mechanisms would be necessary. A very interesting observation was the levels of ESR2 gene expression also in the pulse chase assay, showing that in MDA-MB-231 the highest levels of ESR2 mRNA were achieved at 15 min after the stimulus with C18 plus estradiol (Fig. 2D), 15 min prior the significant increase of FATP1/SLC27A1 mRNA levels (Fig. 2A). Also, in this cell line the expression of ESR2 decreases over time in cells exposed to estradiol solely (Fig. 1C), showing synchrony between ESR2 and FATP1/SLC27A1 expression. The 15 min delay between the expression of ESR2 and FATP1/SLC27A1, shows that ESR2 expression is stimulated by estradiol in the presence of C18. ESR2 behaves as an immediate early gene, whose expression is activated by a stimulus, and that afterwards will regulate the expression of FATP1/SLC27A1, a delayed early gene, that will contribute for the metabolic adaptive phenotype. This synergy is typical of the transmission of intracellular signal (from the cell membrane to the nucleus), requiring, as an answer, the expression of first line (immediate early) genes, usually transcription factors as ER-β, and second line (delayed early) genes, in order to fulfill a phenotype that will constitute the response to the initial stimulus41.
Our findings in four BC cell lines, suggest that ER-β is relevant in the modulation of FATP1/SLC27A1 as well as a possible association with ER-β expression and mammary carcinogenesis. ER-α has been studied extensively in familial and sporadic BC but there is limited information on ER-β and its isoforms9,42,43. Studies have reported that ER-β2 expression was increased in invasive carcinomas in comparison with normal glands, in both ER-α−positive and ER-α-negative tumors44 and that cytoplasmic ER-β2 expression correlated with shorter overall survival at 15 years42. Moreover, an association of ER-β1 expression with increased cell proliferation in ER-α-negative BC was also described45. These evidences indicate that ER-β may have a role in the progression of BCs and could potentially serve as a prognostic marker. With the intent of investigating the role of ER-β in FATP1/SLC27A1 regulation, cells were exposed to PHTPP, an ER-β antagonist46 and in order to exclude the interference of ER-α, cells were also tested with MPP47 and Fulvestrant48, ER-α antagonists. As expected, MDA-MB-231 was not affected by ER-α antagonists, since it is a TNBC cell line, and it was previously described that Fulvestrant does not affect this cell line viability21. The inhibition of ER-β strongly induced cell death while the inhibition of ER-α did not change cell death levels, suggesting the crucial role of ER-β in BCCs survival (Figs 5 and 7C).
Interestingly, in the assay testing the effect of MPP and Fulvestrant, we observed that C18 and C18 plus estradiol induced slightly higher levels of cell death in MDA-MB-231, though significant when compared with the control. This observation can be explained because One-way ANOVA analyzes the variance between different groups as a whole, and together Dunnett’s multiple comparisons test are used to compare each of a number of conditions/groups with a single control, considering the relative differences between all groups and finding the ones that are more different from the control49,50. Therefore, as the results for all the conditions in this assay are close to the control, slightly differences between control and C18 conditions are displayed as statistically significant. The same does not happen in the assay testing PHTPP, because there are conditions displaying much higher differences in cell death levels comparing to the control. However, a biological explanation can also be advanced, since we verified in other experiments that C18 and C18 plus estradiol induces an increased percentage of MDA-MB-231 cells in cell cycle S phase, meaning these conditions are stimulating cell proliferation (Supplementary Fig. 1). The increased proliferation rate is often accompanied by an increased cell death as mentioned by Gallaher et al.51.
In terms of lipid uptake, when cells were exposed to PHTPP, the uptake of FA was decreased in all cell lines (Figs 4A–D and 6B) whilst MPP and Fulvestrant did not interfere in the FA uptake (Fig. 4E–H). Hence, ER−β impairment targets the normal functioning of BCCs (Figs 3 and 6C) and leads to a decreased uptake of FA (Figs 4 and 6B).
Exploiting the features of cancer metabolism for cancer detection and treatment is a promising strategy in cancer therapeutics, diagnosis and prevention52. In many tumors like melanoma, breast and prostate cancer, lipids are provided via de novo lipogenesis, with an upregulation of FASN53–55. Inhibition of FASN by either small molecules (C75, orlistat) or small interfering RNA can efficiently suppress tumor cell growth in vitro and xenograft models56–58. Most FASN inhibitors show several adverse and side effects59, however our group has found that MDA-MB-231 exposed to CAFs exhibited a decreased FASN activity and an increased FATP1/SLC27A1 expression15. Meaning that, depending on the microenvironment, increased FASN activity may not be a favorable adaptive mechanism if the cells are able to import FA. Accordingly, the pharmacological inhibition of FATP1 with arylpiperazine 5k (DS22420314)24 might be a strategy to fight cancer. We found that 5k significantly reduced the uptake of FA only in the TNBC cell line, MDA-MB-231 (Fig. 6A), indicating that the 5k compound might be a good inhibitor of FA uptake in cancer cells that express FATP1. The fact that normal cells retain the ability of producing FA15,60 will contribute for low adverse effects of this potential therapy. Regarding cell viability, the total percentage of cell death was significantly higher in cells cultured with 5k derivative, comparing to control DMSO (Figs 6C and 7D). Certainly, new experiments will be needed in order to validate and adjust therapeutic concentrations of arylpiperazine 5k (DS22420314) to treat cancer.
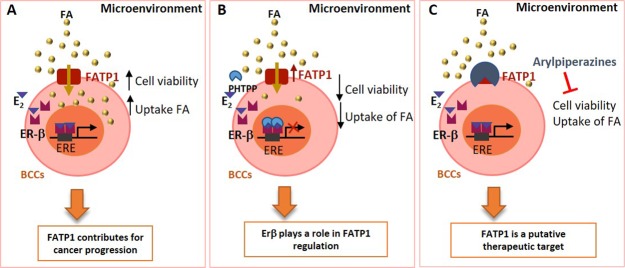
The present study unraveled the crucial role of ER-β in FATP1/SLC27A1 regulation and modulation in the uptake of FA (Fig. 8). Our in vitro findings are validated by patients’ data showing a higher expression of FATP1/SLC27A1 in TNBC cases that conceptually more aggressive and invasive BCs. The inhibition of FATP1 with arylpiperazine 5k (DS22420314) interfered with the uptake of FA and cell viability, consistent with the importance of FATP1 as a putative therapeutic target in BC (Fig. 8). The meaning of ER-β positivity in BC is a matter that should be rescued for investigation.
Figure 8.
Stimulation of ER-β by estradiol contributes to FATP1/SLC27A1 expression and cell survival of breast cancer cells (BCCs). FATP1, whose expression may be controlled by estradiol via ER-β that is a pro-survival element, mediating the transport of Fatty acids (FA), which are essential for BCCs (A). BCCs exposed to PHTPP (ER-β antagonist) show a decreased cell viability and lower uptake of FA suggesting that ER-β controls FATP1/SLC27A1 expression (B). The inhibition of FATP1 with arylpiperazine 5k (DS22420314) interferes with the uptake of FA and cell viability indicating that FATP1 is a putative therapeutic target in BC (C).
Materials and Methods
Bioinformatics analysis
Data from Gene Expression Omnibus (GEO) and The Cancer Genome Atlas (TCGA) databases was used to analyze the gene expression of FATP1/SLC27A1 in BC samples18. Kaplan-Meier curves of overall survival (OS) and recurrence-free survival (RFS) of BC patients were obtained from http://kmplot.com/analysis/.
Morphology and immunohistochemistry analysis
Breast tumor samples were fixed in formaldehyde and embedded in paraffin. Sections (3 µm) were stained with hematoxylin and eosin staining (H&E) (Hematoxylin, Cat. Number CS700, Dako; and Eosin, Cat. Number CS701, Dako) and characterized by immunohistochemistry with anti–FATP1 antibody (Cat. Number MAB3304, R&D system, dilution 1:200 for 16 minutes; pretreatment CC1-24 min; Ventana Medical Systems, Tucson, Arizona, USA) on the BenchMark ULTRA IHC/ISH Automatic staining platform (Ventana Medical Systems) using OptiView DAB IHC Detection Kit (Ventana Medical Systems) with diaminobenzidine as the chromogen to detect antigen expression. Tissue sections were counterstained with Mayer’s hematoxylin before mounting. All antibody dilutions were made in Antibody Diluent Reagent Solution (Cat. Number 003218, Life Technologies). Image acquisition was performed in Digital Microimaging Device Leica DMD108 (version 1.15 Build 704, Leica Microsystems).
Cell lines and culture conditions
Human cell lines from triple-negative BC (TNBC), MDA-MB-231 (HTB-26™, ATCC) and HCC1806 (CRL-2335™, ATCC); from luminal-A BC, MCF7 (HTB-22TM, ATCC), and from luminal B, BT-474 (HTB-20TM, ATCC), were obtained from American Type Culture Collection (ATCC, Manassas, VA, USA). Cells were maintained at 37 °C in a humidified environment of 5% CO2 in Dulbecco’s modified essential medium 1X (DMEM) (41965-039, Gibco, Life Technologies). Medium was supplemented with 10% fetal bovine serum (FBS; S 0615, Merck), 1% Antibiotic-Antimycotic (AA; P06-07300, PAN Biotech) and 50 µg/mL Gentamicin (15750-060, Gibco, Life Technologies). Cells were cultured until an optical confluence of 75–100% before they were detached with 0.05% trypsin-EDTA 1X (25300-054, Invitrogen). Before any in vitro experiment, cells were synchronized under starvation (FBS free culture medium), for 8 h. For experimental conditions cells were cultured in the presence and/or absence of FA (C18:2 - linoleic acid water-soluble, 96 µM; L5900, Sigma Aldrich; from now on called C18) and/or estradiol (1 nM; E4389, Sigma Aldrich) for 16 h. Cells were also exposed to estradiol (1 μM) and/or C18 (96 μM) and/or PHTTP (50 μM, ER-β antagonist; SML1355, Sigma Aldrich) and/or MPP (2 μM, ERα antagonist; M7068, Sigma Aldrich) and/or Fulvestrant (1 μM, ER-α antagonist; I4409, Sigma Aldrich) for 16 h. The concentrations of PHTTP, MPP and fulvestrant were selected according to the literature19–21. The inhibition of FATP1 was assessed by incubating cells with arylpiperazine 5k (DS22420314) (0.125 and 12.5 µM) for 16 h.
Quantitative real-time PCR
RNA was extracted using RNeasy Mini Extraction kit (74,104, Qiagen, Hilden, Germany) and cDNA synthesized from 1 µg RNA and reversely-transcribed by SuperScript II Reverse Transcriptase (18080e44, Invitrogen), both according to the manufacturer’s protocol. Quantitative Real-Time PCR was performed using SYBR Green PCR Master Mix (04707516001, Roche), according to manufacturer’s protocol. Primers used were: FATP1/SLC27A1 primer forward 5′- CAACATGGACGGCAAGGTC -3′ and primer reverse 5′- CAGCAGCTCCATTGTGTCCTC -3′; ESR1 primer forward 5′- GCCAGGCTTTGTGGATTTGAC-3′ and primer reverse 5′- GGAGCAAACAGTAGCTTCCC-3′, and ESR2 primer forward 5′- GATCTTGTTCTGGACAGGGATG-3′ and primer reverse 5′- GGAATTGAGCAGGATCATGGC -3′. Real-time PCR was carried out during 40 amplification cycles, according to manufacturer’s instructions, using a Lightcycler® 480 System instrument (05015243001, Roche). Hypoxanthine-guanine phosphoribosyltransferase (HPRT) was used as housekeeping gene (primer forward: 5′-TGACACTGGCAAAACAATGCA-3′; primer reverse: 5′-GGTCGTTTTTCACCAGCAAGCT-3′). Experiments were performed in biological triplicates and only the adherent cells were analyzed, cells in suspension were rejected.
Western blotting
Cell pellets were lysed in Radio-Immunoprecipitation Assay (RIPA) buffer. Protein concentration was established by Bradford method, using Bio-Rad protein assay reagent (500–0006, Bio-Rad) through spectrophotometric quantification (595 nm). After protein quantification, loading buffer containing 10% SDS, 0.5% bromophenol blue in Tris-HCL (pH 6.8) and 10% β-mercaptoethanol (M3148, Sigma) was added to each cell lysate and boiled at 95–100 °C for 10 min. Total protein (50 µg) was loaded in 12% polyacrylamide gel (Tris-glycine SDS-Polyacrylamide gel) and electrophoresis was carried out in MINI-PROTEAN Tetra Electrophoresis System (Bio-Rad). After, proteins were transferred to an Immun-Blot® PVDF membrane with Trans-Blot® Turbo TM Blotting system. For protein detection, membranes were incubated with primary specific antibodies (mouse anti-human FATP1, 1:1000, MAB3304, R&D systems). Blots were further incubated with secondary antibody IgG-conjugated Horse-raddish peroxidase (HRP; anti-mouse, 1:5000, 31430, Thermo Scientific) and immunoreactive bands were detected by using ECL western blotting substrate (SuperSignal® West Pico Chemiluminescent Substrate (34080, Thermo Scientific) in a ChemiDoc XRS System (Bio-Rad) with Image Lab software. As endogenous control β-actin as used, membranes were re-incubated using mouse anti-human β-actin (1:5000, A5441, Sigma). Experiments were performed in biological triplicates and only the adherent cells were analyzed, cells in suspension were rejected.
Chromatin immunoprecipitation (ChIP)
ChIP was employed to analyze putative interactions between ER-α and ER-β transcription factors and Estrogen Responsive Elements (ERE) sequences in FATP1/SLC27A1 promoter. Those regions localize in 5′UTR (unstranslated reagion) of FATP1/SLC27A1 gene between nucleotides −179 to −406. To crosslink proteins and DNA cells were treated with 37% formaldehyde at a final concentration of 1% (v/v), followed by an incubation with 125 mM glycine (pH 9). Subsequently, cells were scraped, centrifuged at 150 g for 2 min and ChIP lysis buffer (50 mM Tris-HCL (pH 8.0), 10 mM EDT, 1% SDS, 1 Complete, Mini, EDTA-free Protease Inhibitor Cocktail) was added. Cell lysates were sonicated and the size of the chromatin fragments (expected size between 1000 bp and 500 bp) was evaluated by electrophoresis, in a 1.2% (w/v) agarose gel. ChIP assay was performed using OneDay ChIP kit (kch-onedIP-060, Diagenode) according to the manufacturer’s protocol. The chromatin complexes were immunoprecipitated with 1 μl (~1 μg/mL) of specific antibodies: rabbit anti-human ER-α (ab75635; Abcam) and rabbit anti-human ER-β (ab196787; Abcam). Experiments were performed in biological triplicates and only the adherent cells were analyzed, cells in suspension were rejected. The relative occupancy of the immunoprecipitated factors at a specific promoter region was performed by RQ-PCR as described in section 4.2, using primers for FATP1/SLC27A1 promoter (primer forward: 5′-GACTGTTGTAAGATTGGCAGGG-3′; primer reverse: 5′-CTGGGATTGGTCAACTCCTC-3′) and calculated using the following formula:
FATP1 levels by flow cytometry
To evaluate the effects of estradiol, PHTPP, MPP and Fulvestrant, with and without FA in FATP1 expression FATP1 levels (total and membrane protein) were quantified using flow cytometry. Briefly, 1.5 × 105 cells/mL were plated in 24-well plates and after starvation, cells were exposed to PHTPP (2-Phenyl-3-(4-hydroxyphenyl)-5,7-bis(trifluoromethyl)-pyrazolo[1,5-a] pyrimidine), MPP (1,3Bis(4-hydroxyphenyl)-4-methyl-5[4-(2-piperidinylethoxy)phenol]-1H-pyrazole-dihydrochloride) and Fulvestrant ((7α,17β)-7-[9-[(4,4,5,5,5-Pentafluoropentyl)sulfinyl] nonyl]estra-1,3,5(10)-triene -3,17-diol) with or without estradiol and FA, for 16 h. Cells were detached with PBS-EDTA, centrifuged at 230 g for 5 min, at 4 °C and washed with PBS-BSA 0.1% (v/w). Cells were incubated with 100 μL of FATP1 (1:500 in PBS-BSA 0.5%) with (total levels determination) and without (membrane levels determination) 0.1% saponin (v/w) (47036, Sigma Aldrich), for 1 h, at 4 °C. After, PBS-BSA 0.1% was added and cells were centrifuged at 230 g for 5 min, at 4 °C, followed by an incubation of 30 min with anti-mouse IgG- fluorescein (FITC) conjugated (1:1000 in in PBS-BSA 0.5%; A11059, Invitrogen), with and without 0.1% saponin. After, cells were washed, centrifuged and resuspended in 200 μL PBS-BSA 0.1%. Samples were analyzed in FACScalibur (Becton Dickinson) and data analyzed with FlowJo 8.7 software. Experiments were performed in biological triplicates and only the adherent cells were analyzed, cells in suspension were rejected.
Cell death analysis by flow cytometry
After experimental conditions, supernatants were collected and cells were harvested with trypsin and centrifuged at 150 g for 2 min. The cells in suspension were joined to the cells in suspension (in the supernatants) in order to assess the real percentage of cell death. Cell pellets were stained with 0.5 μl Annexin V- fluorescein (FITC)- (640906, BioLegend) in annexin V binding buffer 1X and incubated at RT, in dark for 15 min. After incubation, samples were resuspended in 200 μl PBS 1 × 0.1% (v/w) BSA and centrifuged at 150 g for 2 min. Cells were resuspended in 100 μl of annexin V binding buffer 1 × 2.5 μl propidium iodide (PI, 50 μg/mL; P4170, Sigma-Aldrich) was added and samples were analyzed by flow cytometry (FACScalibur – Becton Dickinson). Sample data was analyzed using FlowJo 8.7 software (https://www.flowjo.com). Experiments were performed in biological triplicates.
Nile red staining
Nile red staining was performed based on Greenspan et al. (1985) and Yao et al. (2011). For flow cytometry analysis, cells were detached with trypsin, washed PBS 1x and stained with Nile Red (1 µg/mL) for 15 min at room temperature. After incubation, cells were centrifuged, PBS 1X was added and samples were analyzed on FACSCalibur flow cytometer (Becton-Dickinson). Data was analyzed using FlowJo software (http://www.flowjo.com/). Experiments were performed in biological triplicates and only the adherent cells were analyzed, cells in suspension were rejected.
Statistical analysis
Statistical analysis was performed using GraphPad Prism 6.0 software (www.graphpad.com). Sample data were presented as the mean (normal distribution) ± SD. Comparisons between data from each group were statistically analyzed by a two-tailed unpaired Student’s t-test and multiple comparisons were performed using One-way ANOVA with Dunnett’s or Tukey’s test. For pulse chase qPCR experiments of FATP1/SLC27A1 mRNA quantification a Two-way ANOVA with Tukey’s test was used. Immunohistochemical data was analyzed using univariate analysis (two-tailed t-test) on SPSS software. Differences between experimental conditions were considered statistically significant at p < 0.05. Experiments were performed in biological triplicates.
Supplementary information
Acknowledgements
The authors thank to Shinozuka Tsuyoshi from Daiichi Sankyo, Japan, for the supply of arylpiperazine 5k (DS22420314). The research was funded by IPOLFG, EPE (FAI 2017) and by iNOVA4Health - UID/Multi/04462/a program financially supported by Fundação para a Ciência e Tecnologia/Ministério da Educação e Ciência, through national funds and co-funded by FEDER under the PT2020 Partnership Agreement and by Fundação para a Ciência e Tecnologia (personal fellowship: PD/BD/128337/2017).
Author Contributions
Cindy Mendes planned and performed experiments and wrote the first draft of the paper; Filipa Lopes-Coelho, Cristiano Ramos, Filipa Martins, Inês Santos, Armanda Rodrigues and Fernanda Silva performed experiments; Saudade André discussed the rational of the project as an expert of breast pathology; Jacinta Serpa is responsible for the design and conception of the research line. All the authors read and contribute for the final version of the paper.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1038/s41598-019-50531-3.
References
- 1.Torre LA, et al. Global Cancer Statistics, 2012. CA Cancer J Clin. 2015;65:87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 2.Whiteside TL. The tumor microenvironment and its role in promoting tumor growth. Oncogene. 2008;27:5904–5912. doi: 10.1038/onc.2008.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Serpa J, Dias S. Metabolic cues from the microenvironment act as a major selective factor for cancer progression and metastases formation. Cell Cycle. 2011;10:180–181. doi: 10.4161/cc.10.2.14476. [DOI] [PubMed] [Google Scholar]
- 4.Yamaguchi Y. Microenvironmental regulation of estrogen signals in breast cancer. Breast Cancer. 2007;14:175–81. doi: 10.2325/jbcs.975. [DOI] [PubMed] [Google Scholar]
- 5.Russo J, Russo IH. The role of estrogen in the initiation of breast cancer. J. Steroid Biochem. Mol. Biol. 2006;102:89–96. doi: 10.1016/j.jsbmb.2006.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee H-R, Kim T-H, Choi K-C. Functions and physiological roles of two types of estrogen receptors, ERα and ERβ, identified by estrogen receptor knockout mouse. Lab. Anim. Res. 2012;28:71–76. doi: 10.5625/lar.2012.28.2.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bao TZ, Han GZ, Shim JY, Wen Y, Jiang XR. Quantitative structure-activity relationship of various endogenous estrogen metabolites for human estrogen receptor α and β subtypes: Insights into the structural determinants favoring a differential subtype binding. Endocrinology. 2006;147:4132–50. doi: 10.1210/en.2006-0113. [DOI] [PubMed] [Google Scholar]
- 8.Craig Allred D, Brown P, Medina D. The origins of estrogen receptor alpha-positive and estrogen receptor alpha-negative human breast cancer. Breast Cancer Res. 2004;6:240–245. doi: 10.1186/bcr938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Heldring Nina, Pike Ashley, Andersson Sandra, Matthews Jason, Cheng Guojun, Hartman Johan, Tujague Michel, Ström Anders, Treuter Eckardt, Warner Margaret, Gustafsson Jan-Åke. Estrogen Receptors: How Do They Signal and What Are Their Targets. Physiological Reviews. 2007;87(3):905–931. doi: 10.1152/physrev.00026.2006. [DOI] [PubMed] [Google Scholar]
- 10.Normanno N, et al. Mechanisms of endocrine resistance and novel therapeutic strategies in breast cancer. Endocr. Relat. Cancer. 2005;12:721–747. doi: 10.1677/erc.1.00857. [DOI] [PubMed] [Google Scholar]
- 11.Speirs V, Malone C, Walton DS, Kerin MJ, Atkin SL. Increased expression of estrogen receptor β mRNA in tamoxifen-resistant breast cancer patients. Cancer Res. 1999;59:5421–4. [PubMed] [Google Scholar]
- 12.Murphy LC, Leygue E. The role of estrogen receptor-β in breast cancer. Semin. Reprod. Med. 2012;30:5–13. doi: 10.1055/s-0031-1299592. [DOI] [PubMed] [Google Scholar]
- 13.Dawson SJ, Provenzano E, Caldas C. Triple negative breast cancers: Clinical and prognostic implications. Eur. J. Cancer. 2009;45:27–40. doi: 10.1016/S0959-8049(09)70013-9. [DOI] [PubMed] [Google Scholar]
- 14.Pavlova NN, Thompson CB. The Emerging Hallmarks of Cancer Metabolism. Cell Metab. 2016;23:27–47. doi: 10.1016/j.cmet.2015.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lopes-Coelho F, André S, Félix A, Serpa J. Breast cancer metabolic cross-talk: Fibroblasts are hubs and breast cancer cells are gatherers of lipids. Mol. Cell. Endocrinol. 2017;462:93–106. doi: 10.1016/j.mce.2017.01.031. [DOI] [PubMed] [Google Scholar]
- 16.Serpa J, et al. Butyrate-rich colonic microenvironment is a relevant selection factor for metabolically adapted tumor cells. J. Biol. Chem. 2010;285:39211–39223. doi: 10.1074/jbc.M110.156026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Glatz JF, Luiken JJ, Bonen A. Membrane Fatty Acid Transporters as Regulators of Lipid Metabolism: Implications for Metabolic Disease. Physiol. Rev. 2010;90:367–417. doi: 10.1152/physrev.00003.2009. [DOI] [PubMed] [Google Scholar]
- 18.Györffy B, et al. An online survival analysis tool to rapidly assess the effect of 22,277 genes on breast cancer prognosis using microarray data of 1,809 patients. Breast Cancer Res. Treat. 2010;123:725–731. doi: 10.1007/s10549-009-0674-9. [DOI] [PubMed] [Google Scholar]
- 19.Oo PS, et al. Estrogen Regulates Mitochondrial Morphology through Phosphorylation of Dynamin-related Protein 1 in MCF7 Human Breast Cancer Cells. ACTA Histochem. Cytochem. 2018;51:21–31. doi: 10.1267/ahc.17034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baker Kimberly Mantzke, Bauer Angela C. Green Tea Catechin, EGCG, Suppresses PCB 102-Induced Proliferation in Estrogen-Sensitive Breast Cancer Cells. International Journal of Breast Cancer. 2015;2015:1–7. doi: 10.1155/2015/163591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li HJ, et al. P2Y2 receptor-mediated modulation of estrogen-induced proliferation of breast cancer cells. Mol. Cell. Endocrinol. 2011;338:28–37. doi: 10.1016/j.mce.2011.02.014. [DOI] [PubMed] [Google Scholar]
- 22.Anders CK, Carey LA. Biology, metastatic patterns, and treatment of patients with triple-negative breast cancer. Clin. Breast Cancer. 2009;9:73–81. doi: 10.3816/CBC.2009.s.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nagaraja GM, et al. Gene expression signatures and biomarkers of noninvasive and invasive breast cancer cells: Comprehensive profiles by representational difference analysis, microarrays and proteomics. Oncogene. 2006;25:2328–38. doi: 10.1038/sj.onc.1209265. [DOI] [PubMed] [Google Scholar]
- 24.Matsufuji T, et al. Arylpiperazines as fatty acid transport protein 1 (FATP1) inhibitors with improved potency and pharmacokinetic properties. Bioorganic Med. Chem. Lett. 2013;23:2560–2565. doi: 10.1016/j.bmcl.2013.02.116. [DOI] [PubMed] [Google Scholar]
- 25.Lopes-Coelho F, Gouveia-Fernandes S, Nunes SC, Serpa J. Metabolic Dynamics in Breast Cancer: Cooperation between Cancer and Stromal Breast Cancer Cells. J. Clin. Breast Cancer Res. 2017;1:1–7. [Google Scholar]
- 26.Lopes-Coelho F, Gouveia-Fernandes S, Serpa J. Metabolic cooperation between cancer and non-cancerous stromal cells is pivotal in cancer progression. Tumor Biol. 2018;40:1–15. doi: 10.1177/1010428318756203. [DOI] [PubMed] [Google Scholar]
- 27.Nieman KM, et al. Adipocytes promote ovarian cancer metastasis and provide energy for rapid tumor growth. Nat. Med. 2011;17:1498–1503. doi: 10.1038/nm.2492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pavlides S, et al. The reverse Warburg effect: Aerobic glycolysis in cancer associated fibroblasts and the tumor stroma. Cell Cycle. 2009;8:3984–4001. doi: 10.4161/cc.8.23.10238. [DOI] [PubMed] [Google Scholar]
- 29.Baenke F, Peck B, Miess H, Schulze A. Hooked on fat: the role of lipid synthesis in cancer metabolism and tumour development. Dis. Model. Mech. 2013;6:1353–1363. doi: 10.1242/dmm.011338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Santos CR, Schulze A. Lipid metabolism in cancer. FEBS J. 2012;279:2610–23. doi: 10.1111/j.1742-4658.2012.08644.x. [DOI] [PubMed] [Google Scholar]
- 31.Currie E, Schulze A, Zechner R, Walther TC, Farese RV. Cellular fatty acid metabolism and cancer. Cell Metab. 2013;18:153–161. doi: 10.1016/j.cmet.2013.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Medes G, Thomas A, Weinhouse S. Metabolism of Neoplastic Tissue. IV. A Study of Lipid Synthesis in Neoplastic Tissue Slices in Vitro. Cancer Res. 1953;13:27–9. [PubMed] [Google Scholar]
- 33.Weinberg, R. A. The Biology of Cancer, 10.1007/s13398-014-0173-7.2 (Garland Science, Taylor & Francis Group, LCC, 2014).
- 34.Guitart M, et al. Fatty Acid Transport Protein 1 (FATP1) localizes in mitochondria in mouse skeletal muscle and regulates lipid and ketone body disposal. PLoS One. 2014;9:e98109. doi: 10.1371/journal.pone.0098109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Johnson AR, et al. Metabolic reprogramming through fatty acid transport protein 1 (FATP1) regulates macrophage inflammatory potential and adipose inflammation. Mol. Metab. 2016;5:506–526. doi: 10.1016/j.molmet.2016.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lobo S, Wiczer BM, Smith AJ, Hall AM, Bernlohr DA. Fatty acid metabolism in adipocytes: functional analysis of fatty acid transport proteins 1 and 4. J. Lipid Res. 2007;48:609–20. doi: 10.1194/jlr.M600441-JLR200. [DOI] [PubMed] [Google Scholar]
- 37.Wu Q, et al. FATP1 Is an Insulin-Sensitive Fatty Acid Transporter Involved in Diet-Induced Obesity FATP1 Is an Insulin-Sensitive Fatty Acid Transporter Involved in Diet-Induced Obesity. Mol. Cell. Biol. 2006;26:3455–3467. doi: 10.1128/MCB.26.9.3455-3467.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nath A, Chan C. Genetic alterations in fatty acid transport and metabolism genes are associated with metastatic progression and poor prognosis of human cancers. Sci. Rep. 2016;6:18669. doi: 10.1038/srep18669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li L, et al. Differential requirement for de novo lipogenesis in cholangiocarcinoma and hepatocellular carcinoma of mice and humans. Hepatology. 2016;63:1900–1913. doi: 10.1002/hep.28508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Blask DE, et al. Melatonin inhibition of cancer growth in vivo involves suppression of tumor fatty acid metabolism via melatonin receptor-mediated signal transduction events. Cancer Res. 1999;59:4693–4701. [PubMed] [Google Scholar]
- 41.Zhang M, et al. Adipocyte-Derived Lipids Mediate Melanoma Progression via FATP Proteins. Cancer Discov. 2018;8:1006–1025. doi: 10.1158/2159-8290.CD-17-1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mann S, et al. Estrogen receptor beta expression in invasive breast cancer. Hum. Pathol. 2001;32:113–118. doi: 10.1053/hupa.2001.21506. [DOI] [PubMed] [Google Scholar]
- 43.Deroo BJ, Buensuceso AV. Minireview: Estrogen Receptor-β: Mechanistic Insights from Recent Studies. Mol. Endocrinol. 2010;24:1703–14. doi: 10.1210/me.2009-0288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Esslimani-Sahla M, et al. Increased estrogen receptor betacx expression during mammary carcinogenesis. Clin Cancer Res. 2005;11:3170–4. doi: 10.1158/1078-0432.CCR-04-2298. [DOI] [PubMed] [Google Scholar]
- 45.O’Neill P. a et al. Wild-type oestrogen receptor beta (ERbeta1) mRNA and protein expression in Tamoxifen-treated post-menopausal breast cancers. Br. J. Cancer. 2004;91:1694–702. doi: 10.1038/sj.bjc.6602183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kim M-J, et al. Effects of 17β-Estradiol and Estrogen Receptor Antagonists on the Proliferation of Gastric Cancer Cell Lines. J Gastric Cancer. 2013;13:172–178. doi: 10.5230/jgc.2013.13.3.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sun J, et al. Antagonists selective for estrogen receptor α. Endocrinology. 2002;143:941–7. doi: 10.1210/endo.143.3.8704. [DOI] [PubMed] [Google Scholar]
- 48.Osborne CK, Wakeling A, Nicholson RI. Fulvestrant: An oestrogen receptor antagonist with a novel mechanism of action. Br. J. Cancer. 2004;90:S2–S6. doi: 10.1038/sj.bjc.6601629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.McHugh ML. Multiple comparison analysis testing in ANOVA. Biochem. Medica. 2011;21:203–209. doi: 10.11613/BM.2011.029. [DOI] [PubMed] [Google Scholar]
- 50.Daniel, W. W. & Cross, C. L. Biostatistics: A foundation for analysis in health sciences. Wiley, 10.1017/CBO9781107415324.004 (2013).
- 51.Gallaher JA, Brown JS, Anderson ARA. The impact of proliferation-migration tradeoffs on phenotypic evolution in cancer. Sci. Rep. 2019;9:2425. doi: 10.1038/s41598-019-39636-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Phan LM, Yeung S-CJ, Lee M-H. Cancer metabolic reprogramming: importance, main features, and potentials for precise targeted anti-cancer therapies. Cancer Biol. Med. 2014;11:1–19. doi: 10.7497/j.issn.2095-3941.2014.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kuhajda FP, et al. Fatty acid synthesis: a potential selective target for antineoplastic therapy. Proc. Natl. Acad. Sci. 1994;91:6379–6383. doi: 10.1073/pnas.91.14.6379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Carvalho MA, et al. Fatty acid synthase inhibition with Orlistat promotes apoptosis and reduces cell growth and lymph node metastasis in a mouse melanoma model. Int. J. Cancer. 2008;123:2557–65. doi: 10.1002/ijc.23835. [DOI] [PubMed] [Google Scholar]
- 55.Loda M, et al. Fatty acid synthase: A metabolic enzyme and candidate oncogene in prostate cancer. J. Natl. Cancer Inst. 2009;101:519–32. doi: 10.1093/jnci/djp030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Alli PM, Pinn ML, Jaffee EM, McFadden JM, Kuhajda FP. Fatty acid synthase inhibitors are chemopreventive for mammary cancer in neu-N transgenic mice. Oncogene. 2005;24:39–46. doi: 10.1038/sj.onc.1208174. [DOI] [PubMed] [Google Scholar]
- 57.Kridel SJ, Axelrod F, Rozenkrantz N, Smith JW. Orlistat Is a Novel Inhibitor of Fatty Acid Synthase with Antitumor Activity. Cancer Res. 2004;64:2070–5. doi: 10.1158/0008-5472.CAN-03-3645. [DOI] [PubMed] [Google Scholar]
- 58.Menendez JA, Vellon L, Colomer R, Lupu R. Pharmacological and small interference RNA-mediated inhibition of breast cancer-associated fatty acid synthase (oncogenic antigen-519) synergistically enhances Taxol (Paclitaxel)-induced cytotoxicity. Int. J. Cancer. 2005;115:19–35. doi: 10.1002/ijc.20754. [DOI] [PubMed] [Google Scholar]
- 59.Jones SF, Infante JR. Molecular pathways: Fatty acid synthase. Clin. Cancer Res. 2015;21:5434–5438. doi: 10.1158/1078-0432.CCR-15-0126. [DOI] [PubMed] [Google Scholar]
- 60.Khnykin D, Miner JH, Jahnsen F. Role of fatty acid transporters in epidermis: Implications for health and disease. Dermatoendocrinol. 2011;3:53–61. doi: 10.4161/derm.3.2.14816. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.