Abstract
The authors report a rare variation of the vasculature in the upper limbs of an 84-year-old male cadaver. A high bifurcation of the brachial artery occurred bilaterally at the proximal one-third of each arm. The radial arteries were larger than the ulnar arteries and gave origin to the common interosseous arteries. At the cubital fossa, the ulnar arteries traversed medial to the median nerves, continuing superficial to all forearm muscles except the palmaris longus tendon, characteristic of superficial brachioulnar arteries. The aforementioned variations have rarely been reported in previous literature and demonstrate important clinical significance in relation to accidental intra-arterial injections, errors in blood pressure readings, as well as orthopedic, plastic, and vascular surgeries of the upper limbs.
Keywords: Superficial brachioulnar artery, Brachial artery, Ulnar artery, Radial artery, High bifurcation
Introduction
The brachial artery is a continuation of the axillary artery which typically begins at the inferior border of the teres major muscle and serves as the main source of arterial blood supply to the upper limb. As the brachial artery descends distally down the brachium, multiple branches give rise to functionally and clinically relevant arterial anastomoses. At the level of the cubital fossa on the anterior aspect just deep to the bicipital aponeurosis, the brachial artery divides into the radial and ulnar arteries. These arterial branches further contribute to the arterial anastomosis that surrounds the elbow resulting in a network of collateral circulation that allows blood to perfuse the antebrachial region when the elbow flexes [1].
Anatomical variations in this branching pattern have been well documented; however, the majority of these variations occur in the radial artery [2] followed by the ulnar artery, with only around 2.26% exhibiting a superficial brachioulnar artery (SBUA) variation [3,4]. SBUA is defined as an ulnar artery with a high origin coursing over the forearm flexor muscles, but deep to the brachial fascia [2,4,5]. The bilateral SBUA with a variant relation to the forearm muscles as found in this case is rarely reported in the literature [3]. This report aims to expand upon previous literature and provide additional insight into the field of clinical anatomy while educating physicians about possible presentations and potential risks associated with these variations.
Case Report
An atypical anatomical variation in the bifurcation of the brachial artery was observed bilaterally in an 84-year-old Caucasian male while dissecting during the Essential Clinical Anatomy and Development course at Marian University College of Osteopathic Medicine. Detailed dissection was implemented to preserve the course and branching of the arteries and the median nerve.
The description of vasculature was noted on both the upper limbs. The brachial arteries bifurcated at the proximal third of the brachium instead of at the cubital fossa. The brachial artery traversed lateral to the median nerve before splitting into brachioradial and brachioulnar arteries. The brachioradial artery was larger than the brachioulnar artery. The brachioradial artery coursed lateral to the median nerve, and entered the brachium. The common interosseous artery, which normally branches off the ulnar artery, originated from the brachioradial artery. The brachioulnar artery traversed medial to the median nerve and superficial to all forearm muscles except the palmaris longus tendon, before terminating as the superficial palmar arch. Major anastomoses between the radial and ulnar arteries were observed as the superficial and deep palmar arches.
Using Reeves acrylic paint, the major arteries were painted in red and the median nerve in yellow. The anatomical variation was subsequently photographed for documentation (Fig. 1).
Fig. 1. Right (A) and left (B) upper limbs. 1, brachial artery; 2. brachioradial artery; 3, superficial brachioulnar artery; 4, common interosseous artery; 5, superficial palmar arch; 6, median nerve; 7, ulnar nerve; 8, musculocutaneous nerve; 9, coracobrachialis; 10, biceps brachii; 11, triceps brachii; 12, brachioradialis; 13, pronator teres (cut); 14, flexor carpi radialis; 15, palmaris longus; 16, flexor carpi ulnaris; 17, flexor digitorum superficialis; 18, flexor pollicis longus; 19, anterior interosseous artery.
Discussion
While anatomical variations in arterial supply to the upper extremities are common, this case presented with a less common combination of both a superficial ulnar artery and a high bifurcation of the brachial artery, which is referred to as an SBUA [2]. This variation may be observed alongside a brachial artery that divides into the radial and common interosseous arteries. The SBUA is clinically significant due to its potential for accidental intra-arterial injections if mistaken for the cubital vein [6].
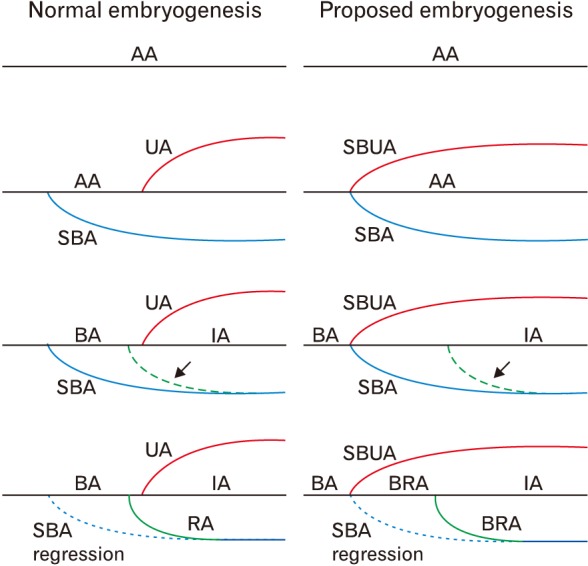
The primordial vascular pattern consists of a primary axial artery and its branches. The vascular pattern changes as the limbs develop, chiefly as a result of vessels sprouting from existing vessels [7]. During Carnegie stage 12 of development, an initial capillary plexus grows into the limb bud from the seventh intersegmental artery. By stage 17, the brachial artery is seen as a continuation of the axillary artery which extends to the elbow. By stage 18, the radial artery begins its development more proximal to the ulnar artery, later regressing and establishing its final attachment near the ulnar artery around the cubital fossa [8]. Variations in upper extremity vasculature are thought to be due to failures in persistence, enlargement, and differentiation of early capillary networks which would otherwise remain as capillaries or regress [4]. The high bifurcation of the brachial artery is likely the result of unusual induction and branching of primitive vascular plexuses [9]. The persistence of an early radial artery could form a brachioradial artery. The brachioulnar artery may originate from disruption during embryogenesis, causing improper regression, retention, or even reappearance of the artery proximally in the upper limb [8]. Differential vascular pathways stem from variable angioblast induction by vascular growth factors (such as vascular endothelial growth factor) along specific routes. The earliest vessels present as a central artery draining into a peripheral marginal sinus and peripheral venous channels. The angioblasts collect into a marginal sinus beneath the apical ectodermal ridge and are induced to branch out from the limb bud to their destination in the upper extremity [10]. Variable developmental hemodynamics during angiogenic sprouting may yield primitive vasculature which persists, fuses, absorbs or regresses in unusual patterns [11]. An early, high bifurcation of the brachial artery, as observed in this case, may result. A schematic representation of the normal and proposed embryogenesis, in this case, is shown in Fig. 2.
Fig. 2. Normal embryogenesis and proposed embryogenesis of donor. AA, axis artery; UA, ulnar artery; SBUA, superficial brachioulnar artery; SBA, superficial brachial artery; BA, brachial artery; IA, interosseous artery; RA, radial artery; BRA, brachioradial artery. Arrow indicates anastomotic BRA.
While the incidence of a brachioradial artery is occasionally seen in the literature (~11.34%), a brachioulnar artery is less commonly seen (~3.03%) [2]. A case of the brachioulnar artery was reported to course superficial to biceps aponeurosis [12] but the artery was deep to the aponeurosis in our donor. The positioning of structures traversing through the cubital fossa is often seen as biceps tendon, brachial artery and median nerve moving from the lateral to the medial side [1]. In this case, the vascular variations caused an atypical arrangement with the median nerve coursing between radial and ulnar arteries. Preoperative angiogram in flap surgery may help to trace the course of a variant artery and discover its site of origin [4]. The vascular variations are often accompanied by nervous and muscular variations of the upper limb [13], but this particular case revealed isolated arterial variations. Although finding an SBUA is rare, it holds strong clinical significance in preventing accidental intra-arterial injections since the SBUA can be easily mistaken as a vein [4,14]. This presents a risk of accidental arterial cannulation and subsequent limb ischemia [14].
The high early split of the brachial artery is clinically important with respect to orthopedic, plastic, and vascular surgeries of the upper limbs [15]. The location of the SBUA may be of great importance during free radial forearm flap or coronary bypass surgeries where the radial artery may be used as a conduit, leaving the ulnar artery as the only remaining blood supply to the arm [5]. The variation may also cause complicated blood pressure readings due to the presence of two arteries, where typically only the brachial artery would be seen before splitting in the cubital fossa [15]. Medical providers should consider the possibility of superficial forearm arteries when the radial or ulnar pulses cannot be palpated in their typical location [4].
Acknowledgements
The authors would like to thank the donor and his family and the Division of Biomedical Sciences of Marian University College of Osteopathic Medicine for their support and assistance.
Footnotes
- Conceptualization: LP.
- Data acquisition: MS.
- Data analysis or interpretation: JS, SSV.
- Drafting of the manuscript: KS, EP, SSV.
- Critical revision of the manuscript: SSV.
- Approval of the final version of the manuscript: all authors.
Conflicts of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Drake RL, Vogl AW, Mitchell AW. Gray's anatomy for students. 3rd ed. Philadelphia, PA: Churchill Livingstone/Elsevier; 2015. [Google Scholar]
- 2.Rodríguez-Niedenführ M, Vázquez T, Nearn L, Ferreira B, Parkin I, Sañudo JR. Variations of the arterial pattern in the upper limb revisited: a morphological and statistical study, with a review of the literature. J Anat. 2001;199(Pt 5):547–566. doi: 10.1046/j.1469-7580.2001.19950547.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McCormack LJ, Cauldwell EW, Anson BJ. Brachial and antebrachial arterial patterns; a study of 750 extremities. Surg Gynecol Obstet. 1953;96:43–54. [PubMed] [Google Scholar]
- 4.Casal D, Pais D, Toscano T, Bilhim T, Rodrigues L, Figueiredo I, Aradio S, Angélica-Almeida M, Goyri-O'Neill J. A rare variant of the ulnar artery with important clinical implications: a case reportssion of genes involved in lipid metabolism in human adipose tissue. BMC Res Notes. 2012;5:660. doi: 10.1186/1756-0500-5-660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Senanayake KJ, Salgado S, Rathnayake MJ, Fernando R, Somarathne K. A rare variant of the superficial ulnar artery, and its clinical implications: a case report. J Med Case Rep. 2007;1:128. doi: 10.1186/1752-1947-1-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.D'Costa S, Shenoy BM, Narayana K. The incidence of a superficial arterial pattern in the human upper extremities. Folia Morphol (Warsz) 2004;63:459–463. [PubMed] [Google Scholar]
- 7.Moore KL, Persaud TV, Torchia MG. Before we are born. 9th ed. Philadelphia, PA: Elsevier; 2016. [Google Scholar]
- 8.Rodríguez-Niedenführ M, Burton GJ, Deu J, Sañudo JR. Development of the arterial pattern in the upper limb of staged human embryos: normal development and anatomic variations. J Anat. 2001;199:407–417. doi: 10.1046/j.1469-7580.2001.19940407.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chakravarthi KK, Ks S, Venumadhav N, Sharma A, Kumar N. Anatomical variations of brachial artery: its morphology, embryogenesis and clinical implications. J Clin Diagn Res. 2014;8:AC17–AC20. doi: 10.7860/JCDR/2014/10418.5308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carlson BM. Human embryology and developmental biology. 5th ed. Philadelphia, PA: Elsevier/Saunders; 2014. [Google Scholar]
- 11.Jurjus A, Sfeir R, Bezirdjian R. Unusual variation of the arterial pattern of the human upper limb. Anat Rec. 1986;215:82–83. doi: 10.1002/ar.1092150112. [DOI] [PubMed] [Google Scholar]
- 12.Krishnamurthy A, Kumar M, Nayak SR, Prabhu LV. High origin and superficial course of ulnar artery: a case report. Firat Tip Dergisi. 2006;11:66–67. [Google Scholar]
- 13.Catli MM, Ozsoy U, Kaya Y, Hizay A, Yildirim FB, Sarikcioglu L. Four-headed biceps brachii, three-headed coracobrachialis muscles associated with arterial and nervous anomalies in the upper limb. Anat Cell Biol. 2012;45:136–139. doi: 10.5115/acb.2012.45.2.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chin KJ, Singh K. The superficial ulnar artery: a potential hazard in patients with difficult venous access. Br J Anaesth. 2005;94:692–693. doi: 10.1093/bja/aei548. [DOI] [PubMed] [Google Scholar]
- 15.Mehta V, Arora J, Suri RK, Rath G. Unilateral anomalous arterial pattern of human upper limb: anatomical description and clinical implications. Sultan Qaboos Univ Med J. 2008;8:227–230. [PMC free article] [PubMed] [Google Scholar]