Abstract
Background
Early substance use threatens many American Indian/Alaska Native (AI/AN) communities, as it is a risk factor for maladaptive use and adverse health outcomes. Marijuana is among the first substances used by AI/AN youth and its use becomes widespread during adolescence. Interventions that delay or reduce marijuana use hold the promise of curbing substance disorders and other health risk disparities in AI/AN populations.
Objectives
We evaluated the effectiveness of the Circle of Life (COL) program in reducing marijuana use among young AI adolescents. COL is a culturally tailored, theory-based Human Immunodeficiency Virus (HIV) and sexually transmitted disease (STD) intervention shown to delay sexual initiation among AI youths.
Methods
We conducted secondary analyses of data from a school-based group randomized trial conducted between 2006 and 2007 in all 13 middle schools on a rural, Northern Plains reservation (N=635, 47% female). We used discrete-time survival analysis (DTSA) to assess COL effectiveness on risk for marijuana initiation among AI youths and latent growth curve modeling (LGCM) to evaluate effects on frequency of marijuana use over time.
Results
DTSA models showed that the overall risk of marijuana initiation was 17.3% lower in the COL group compared to the Control group. No intervention effect on frequency of marijuana use emerged in LGCM analyses.
Conclusion
COL is a multifaceted, culturally tailored, skills-based program effective in preventing marijuana uptake among AI youth.
Despite variability by region and tribe, many American Indian/Alaska Native (AI/AN) communities in the U.S. experience significant disparities in substance use disorders (1–3). Hospital admissions for substance use treatment in the U.S. disproportionately involve AI/AN adults and the percentage of AI/AN adults needing treatment is higher than that among all other racial/ethnic groups, regardless of age, gender, or rural/urban residence (4). In the general population, 24% of AI/ANs aged 12 and older report past year use of federally classified illicit substances compared to the national average of 17% (5).
Substance use often starts at young ages in AI/AN settings (6–9) and early initiation is an important risk factor for maladaptive patterns of use later in life as well as an array of other adverse health, social, and family outcomes (10–13). Marijuana is a particular concern, as it is often the first substance taken up by AI/AN youth (8) and its use becomes widespread during adolescence (8–9, 14–16). In national surveys, 22% of AI/AN high school students report marijuana use before age 13 (compared to 7% of white and 12% of black and Hispanic students) and 36% report current use (compared to 20% of white and 29% of black and Hispanic students) (14). Stanley et al. (9) reported that the lifetime prevalence of marijuana use among AI youth attending schools on or near reservations was dramatically higher than that observed nationally in the 2009–2011 Monitoring the Future (MTF) survey (56% vs. 16%; 61% vs. 33%; and 68% vs. 44% for 8th, 10th and 12th grade AI and U.S. students, respectively). Risk of marijuana initiation among AI students was also elevated over that of white students living in the same reservation communities and attending the same schools (15). In another reservation study, marijuana use among middle school students from a Northern Plains Tribe preceded alcohol use and prevalence increased from 17% to 52% among boys and from 10% to 58% among girls between ages 10 and 13 (8). More than 40% of the students in that reservation sample followed a trajectory of either continuously high marijuana use or increasingly high use during pre-adolescence (16).
The risks associated with adolescent marijuana use are exacerbated by its co-occurrence with other unhealthy behaviors (6–7,17–18,20–21), including unsafe sexual activity, which is also elevated among AI/AN youth (14) and contributes to disparities in HIV and other sexually transmitted diseases (STDs) (19). Programs that delay or reduce marijuana use at early ages hold the promise of substantially reducing substance use disparities in AI/AN populations as well as the risky behaviors and harmful consequences associated with that use. Despite calls for coordinated prevention efforts, intervention studies typically focus on single risk behaviors instead of addressing the range of health risk behaviors common among adolescents – both in the general population and in AI/AN communities specifically (6,7,18,22). Even when prevention programs address common determinants and therefore have the potential for broad impacts, few studies have evaluated effects on multiple behaviors and even fewer demonstrated positive impacts (23).
Culturally tailored health promotion programs are needed to effectively address the multitude of risk behaviors that threaten the positive development of AI/AN youth, including substance use and sexual risk behavior. The current study addresses this need by evaluating the effectiveness of the Circle of Life (COL) program in reducing marijuana use among young AI adolescents. COL is a prevention program developed specifically for AI youth that incorporates Social Cognitive Theory (SCT) and uses a skills-building approach to promote healthy choices (24, 25). COL has previously demonstrated effectiveness in delaying sexual initiation in sample of AI middle-school youths living on a Northern Plains reservation (26). Given its theoretical foundation, cultural specificity, and broad-based skills orientation, the COL program is a strong candidate for positively impacting other health risk behaviors among AI youth, including substance use. We used data from the original trial to assess the effectiveness of COL exposure on risk for initiation of marijuana use among AI middle school students and on the trajectory of marijuana use over time.
Methods
Study Design
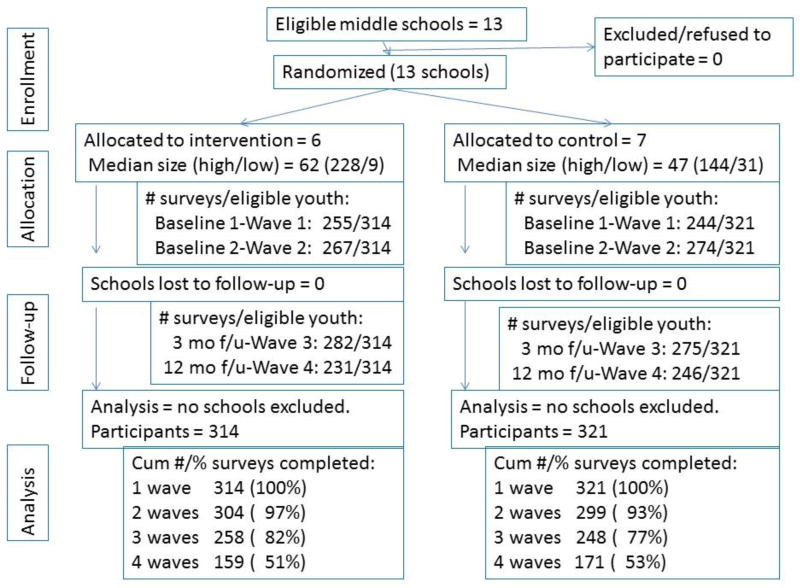
This study reports secondary analyses of data collected in a school-based group randomized trial (GRT) conducted between 2006 and 2007 in all 13 middle schools on a rural, Northern Plains reservation. Randomization occurred at the school level because the intervention was designed for classroom delivery and threat of contamination was high within schools. In consultation with tribal community partners, the trial used a longitudinal wait-listed design that provided an opportunity for all seventh and eighth graders to be exposed to the COL program within a period of 12 months (24–26; see Figure 1). Using the random number generator function in Excel, six schools were randomly assigned to receive the intervention in the first phase of the study (‘COL’ group), which took place within 3 months in fall 2006. Seven schools participated in the second phase (‘Control’ group). Outcomes were assessed in spring 2006 (Baseline 1), fall 2006 (Baseline 2), winter 2007 (3 months post-intervention), and fall 2007 (12 months post-intervention and before the COL implementation in wait-listed schools). Additional details about the project rationale and design are available elsewhere (24–26).
Figure 1.
Circle of Life Group Randomized Trial CONSORT Diagram
Participant Sample
Participants were students in the seventh or eighth grade in 2006 at one of the 13 middle schools located on a Northern Plains Indian reservation in one of the poorest regions in the United States. Student enrollment varied widely across the 13 schools. The four public schools, two private schools, and seven federally operated schools were balanced between study arms. Youths who completed at least one assessment during the study period were included in the final sample regardless of whether they completed a pre-intervention assessment. Eligibility was based on youth assent and parent/guardian consent. The study was approved by the Colorado Multiple Institutional Review Board and by the Research Review Board that provides oversight of research for this tribe.
Intervention
COL is a 30 hour health education and youth development curriculum that was developed by AI/AN educators and extensively reviewed by parents, education specialists, and health experts from a wide range of AI/AN communities and organizations (24,25). It integrates theories of behavior change, including SCT and the Theory of Planned Behavior, into a curriculum based on AI/AN cultural knowledge, values, stories, illustrations, historical figures, practices, and teachings (25). COL emphasizes responsibility to one’s family and community as well as the role of the community in preventing HIV/AIDS and other diseases (see Table 1). Traditional AI/AN beliefs about adolescence as a critical period for personal empowerment and self-mastery form the core of the program, along with a focus on strengthening and balancing the spiritual, emotional, physical and mental aspects of individuals, as symbolized by the traditional AI/AN Medicine Wheel. Guidance is also available for adapting program components to align with specific local AI/AN cultural contexts, as necessary. Program content and activities are designed to empower AI/AN middle school youth with an appreciation of the importance of personal responsibility (volition) and to build communication, decision-making, peer resistance, and refusal skills that promote a wide range of healthy behaviors and discourage risky ones. Qualified community members were hired and trained to teach the course. To monitor implementation fidelity, teachers kept logs of program activities and participated in weekly meetings with the project supervisor to review instructional challenges and accomplishments and discuss consistency across instructors.
Table 1.
'Circle of Life' Program: Excerpted Content and Sample Activities.
| Module | Unit | Topics | Sample Activities |
|---|---|---|---|
| 1. Young People are the Pioneers of New Ways (Provides the conceptual framework for the COL curriculum) | 1. Young People are the Pioneers of New Ways | 1. Young Adolescents Should Expect Changes and Challenges as They Grow Up | Chief Dan George Speaks About the Challenges of Adolescence |
| 2. It is Important that Adolescents Learn to Take Responsibility for their Actions | Read About the Courage and Character of SuAnne Big Crow | ||
| 2. Strive for Balance in the Circle of Life | 3. All Four Parts of the Circle of Life Need to be Strong and Balanced | Understanding the Circle of Life | |
| 4. Each of Us Needs to Exercise Our Volition | Linking Strengths to Volition | ||
|
| |||
| 2: Protect the Balance of Your Circle of Life: Know What Is Dangerous to Your Health. (Provides the factual framework for HIV/STDs) | 1. Diseases that Can Harm your Circle of Life | 1. Essential Facts about HIV/AIDS and other STDs | Facts and Fictions /Transmission and Prevention |
| 2. Looking at the Numbers | 2. Statistics on HIV/AIDS and other STDs in Indian Country | What Do Statistics Really Mean? | |
|
| |||
| Module 3: Keep your Personal Circle of Life Strong. Don’t Take Risks With Your Health! (Provides the groundwork for risky situation avoidance skills). | 1. Identifying and Understanding New Feelings | 1. Adolescents Should Expect to Experience New and Intensified Feelings | What’s Normal? /Identifying Feelings |
| 2. It is Important that Adolescents be Able to Identify Their Feelings and Take Responsibility for Them | |||
| 2. Recognizing Risky Situations and Behaviors | 1. Learn to Recognize Risky Situations that Should be Avoided | Recognizing Risky Situations/Stories From A Talking Circle | |
| 2. Identify Specific Behaviors that Increase the Risk of HIV/AIDS and other STDs | Health Risk Thermometer | ||
|
| |||
| Module 4: Respect Yourself-Be True to Who You Really Are. (Facilitates Development of Skills for Avoiding Risky Behaviors). | 1. Decision Making Skills | 1. Skill Acquisition and Practice | Decision Making=Smart Thinking: SODA: Stop, Options, Decide, Act |
| 2. Communication Skills | 1. Skill Acquisition and Practice | Communication Styles- What Works Best?//Assertiveness Role Plays | |
| 3. Refusal Skills | 1. Skill Acquisition and Practice | Refusal=Exercising Volition to Protect Your Circle//Refusal Role Plays | |
|
| |||
| Module 5: Celebrate the Power of Your Circle. (Reinforcement Program Material). | 1. Taking Responsibility for Your Own Behavior | 1. Importance of Making Good Judgments, Assuming Personal Responsibility for Behavior and Resisting Pressure to Engage in Risky Behavior | Celebrate the Power of Your Circle. Use that Power to Stay Healthy. |
| 2. Celebrating the Transition of Adolescence | 2. American Indian and Other Cultural Rites of Passage from Childhood to Adulthood | Adolescence and the Circle of Life | |
Outcome Measures
Youths were asked at each wave of data collection if they had used marijuana at least once in their life. Youths who responded affirmatively were asked their age at first use and the number of times they used it in the past month. In order to minimize recall bias, we used data from the first wave at which use was reported to create an age of first marijuana use variable. Per the Whitesell et al. (8) protocol: a) for youths who reported having ever used marijuana at baseline and who reported an age of first use, we used that age as the initiation age; b) for youths who reported marijuana use at baseline but gave no age of first use, we used age at baseline as the best available estimate of initiation age; c) if youths reported no history of marijuana use at baseline or if data were missing, we went to the subsequent wave and followed the same process to determine initiation age; and d) if youths reported no history of marijuana use at any wave, age of marijuana initiation was coded as missing.
Among youths who reported lifetime use of marijuana at any study wave, 85% consistently reported use at all subsequent waves and 51% were consistent in their reports of age at first use. Among inconsistent age reporters, all but 12 reported first use between ages 12–14 and therefore would have been included in the DTSA as a marijuana initiator sometime after intervention exposure but before the end of the study period. Missing data on age of first use was minimal – 3–4 cases at each wave.
We also created a measure of current marijuana use based on responses to the open-ended question about the number of times marijuana was used in the past month. Youths who reported no lifetime use of marijuana or no use in the past month at a given wave received a score of zero on the measure for that wave. Cases with missing data on lifetime use or past month use at a given wave were coded as missing. To correct for a positive skew resulting from a minority of extreme scores, we collapsed reports of 30 times per month and higher.
Analysis
We used IBM SPSS Statistics v. 22 to construct analysis variables and to carry out all descriptive analyses (27). We used Mplus v.7.31 (28) to estimate discrete-time survival analysis (DTSA) models examining the effect of COL exposure on risk of marijuana initiation between ages 12–14. DTSA is a time-to-event analysis appropriate for discrete time intervals such as age. It begins with all cases that did not report an event (e.g., marijuana initiation) at baseline and estimates the risk of experiencing the event at each interval within the study period (29). In preparation for our DTSA analysis, we recoded age at first marijuana use into a series of dichotomous (0/1) indicators reflecting first reported marijuana use at age 12, age 13 or age 14. Youths received a zero (0) on each indicator if they had not yet reported marijuana use at that age, a one (1) if they did report use at that age, or a missing value (9) if they had initiated marijuana use at an earlier age. Because age 12 was the earliest point at which the intervention was delivered, we left-censored youths who initiated marijuana prior to that age (Total: n =157, 24.7%; COL: n =78, 24.8%; Control: n =79, 24.6%). Overall, 214 youths (33.7%; COL: n =119, 37.9%; Control: n =95, 29.6%) reported no use of marijuana through the end of the study period and received a zero (0) on all marijuana initiation indicators.
Initial DTSA analyses compared the fit of models assuming proportional odds (i.e., constant intervention effect across ages 12–14) either with or without frailty (residual variance) versus non-proportional odds (i.e., variable intervention effect across ages 12–14). Comparisons were based on the Akaike Information Criterion (AIC) and the Bayesian Information Criterion (BIC); lower values on each represent better fit. In our final model, we compared the hazard of marijuana initiation at ages 12, 13 and 14 between youths in the COL and Control groups. Model estimates reflect the probability that those who had not used marijuana before each age would start using at that age. A hazard of .40 for marijuana initiation at age 13 would mean that four in 10 youths who had not used marijuana before their 12th birthday would be expected to start using before age 13. We included participant sex as a covariate in our initial DTSA models and then estimated separate models for boys and girls.
In our second set of analyses, we estimated a series of linear latent growth curve (LGCM) models in Mplus v.7.31 (28) to assess the effect of COL exposure on the trajectory of past month frequency of marijuana use (coded 0–30+ times) reported at Waves 2 through 4 (30). We excluded Wave 1 data so the resulting trajectories would not be influenced by pre-intervention trends in marijuana use. LGCM is a powerful tool for examining intra-individual change in a latent construct (e.g., level of marijuana use) and estimating the impact of key exposures on individual differences in those temporal trends (31). We first assessed the ‘normative’ trajectory of past month marijuana use among Control group participants and then estimated the same trajectory among COL participants. On the third step, we conducted a combined analysis that simultaneously estimated the normative growth trajectory and the degree to which it was altered by intervention exposure. Intervention effectiveness would be demonstrated by a statistically significant reduction (i.e., a negative coefficient) in the slope of marijuana frequency over time. We set the treatment effect as linear over time and, following the Muthén & Curran approach (30), specified that effect as fixed (i.e., as having no variation across individuals).1 On the fourth and final step, we evaluated the interaction between the intervention effect and Wave 2 marijuana frequency in order to assess the differential effectiveness of the intervention as a function of initial levels of marijuana frequency.
We used maximum likelihood estimation in all LGCM analyses and defined the intercept (initial status) as the second pre-intervention assessment at Wave 2. We initially included participant sex as a covariate in all LGCM models and also conducted all analyses separately for boys and girls. We found no significant effects for participant sex so we removed it from the overall models. The results of the sex-specific models were largely identical to those of the overall models, so we report only the latter here. Results from the sex-specific models are available upon request from the corresponding author.
In all DTSA and LGCM analyses, we used a “sandwich-estimator” (type=complex in Mplus, version 7.3) to adjust for clustering at the school level (28). For missing data, we used full information maximum likelihood (FIML) procedures, which have been shown to provide unbiased and efficient estimates for missing data (32). All analyses were conducted using intention-to-treat principles.
Results
Eighty one percent of parents/guardians were located and asked to allow their children to participate. Nearly all (98%) consented and 90% of youths assented. The Wave 1 sample included 71% of the middle-school population on the reservation. Among the 635 youths who completed one or more outcome assessments, 52% (n=330) completed all four and 80% (n=506) completed three or more. Across the intervention and control groups, 499 youths (79%) participated at Wave 1; 541 (85%) at Wave 2; 557 (88%) at Wave 3; and 477 (75%) at Wave 4. There were no significant differences between the intervention and control groups in the number of participants at each wave (p = .11, p = .91, p = .11, p = .37 for Waves 1 through 4, respectively) nor was there a difference in the total number of assessments completed (Ms = 3.3 vs. 3.2 for the COL and Control group, respectively; p = .40) (see Figure 1). Nearly half (47%) of the 635 participants who contributed one or more outcome assessments were female and the average Wave 1 age was 12.5 years. There were no group differences in sex or age at baseline (p’s > .20).
Table 2 shows descriptive statistics on lifetime history and past month frequency of marijuana use at each wave. The percentage of youths who ever used marijuana increased over the study period, from 40% – 57%. Prevalence at Wave 1 was significantly lower in the COL group compared to the Control group, overall (p <.05) and among boys (p <.05). There were no differences between COL and Control group participants in reports of age of first marijuana use at either of the pre-intervention assessments (Wave 1: Ms=11.2 vs. 11.3, respectively [p=.54] and Wave 2: Ms=11.7 vs 11.4, respectively, [p=.15]). Average frequency of marijuana use also increased over time, from 1.5–2.8 times per month. Use was less frequent in the COL group than in the Control group through Wave 3. These Wave 1 to Wave 3 differences in marijuana frequency were more pronounced among boys but not statistically significant, either overall or among boys separately (all p’s =.14–.92).
Table 2.
Marijuana Use among American Indian Middle School Youths, Northern Plains Region, 2006–2007 By COL Intervention Status
| Intervention Status | |||||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| COLb | Controlc | ||||||
|
|
|||||||
| Outcome | Totala | Total | Male | Female | Total | Male | Female |
| Ever Used Marijuana | n (%)d | n (%)d | n (%)d | n (%)d | n (%)d | n (%)d | n (%)d |
|
| |||||||
| Wave 1 (n=499) | 168 (39.6) | 76 (34.7) | 35 (33.0) | 41 (36.3) | 92 (44.9) | 53 (49.0) | 39 (40.2) |
| Wave 2 (n=541) | 213 (47.0) | 101 (43.0) | 43 (39.4) | 58 (46.0) | 112 (51.4) | 61 (52.1) | 51 (50.5) |
| Wave 3 (n=557) | 251 (52.2) | 122 (50.2) | 56 (47.5) | 66 (52.8) | 129 (54.2) | 66 (53.2) | 63 (55.3) |
| Wave 4 (n=477) | 228 (56.6) | 112 (57.1) | 60 (60.0) | 52 (54.2) | 116 (56.0) | 58 (52.7) | 58 (59.8) |
|
| |||||||
| Marijuana Frequency (Past Mos., 0–30+) | M (sd) | M (sd) | M (sd) | M (sd) | M (sd) | M (sd) | M (sd) |
|
| |||||||
| Wave 1 (n=499) | 1.48 (4.7) | 1.33 (4.6) | 1.43 (5.3) | 1.24 (3.8) | 1.65 (4.8) | 1.80 5.3) | 1.48 (4.3) |
| Wave 2 (n=541) | 2.18 (5.5) | 1.81 (5.0) | 1.80 (5.2) | 1.81 (4.8) | 2.60 (6.1) | 2.88 (6.5) | 2.27 (5.5) |
| Wave 3 (n=557) | 2.49 (6.1) | 2.30 (5.9) | 2.10 (6.2) | 2.48 (5.7) | 2.69 (6.3) | 3.15 (7.1) | 2.18 (5.3) |
| Wave 4 (n=477) | 2.77 (6.3) | 2.74 (6.4) | 2.67 (6.2) | 2.82 (6.6) | 2.81 (6.3) | 3.18 (7.3) | 2.37 (4.9) |
635 youths participated in at least one wave of data collection
COL=Intervention Group. N =314, 161 males, 153 females
Control=Control Group. N=321:176 males,145 females
Percents are based on the number of cases with non-missing data on marijuana use at each wave
There was no evidence of attrition-related bias. Baseline characteristics were similar among youths who participated in the first post-intervention assessment (49% female; M age = 12.50; 37% ever used marijuana; and M frequency of marijuana use in the past month = 1.16) and youths who participated in the second post-intervention assessment (45% female; M age = 12.45; 34% ever used marijuana; and M frequency of marijuana use in the past month = 1.29). Patterns were similar in both the COL and Control groups.
Risk of Marijuana Initiation
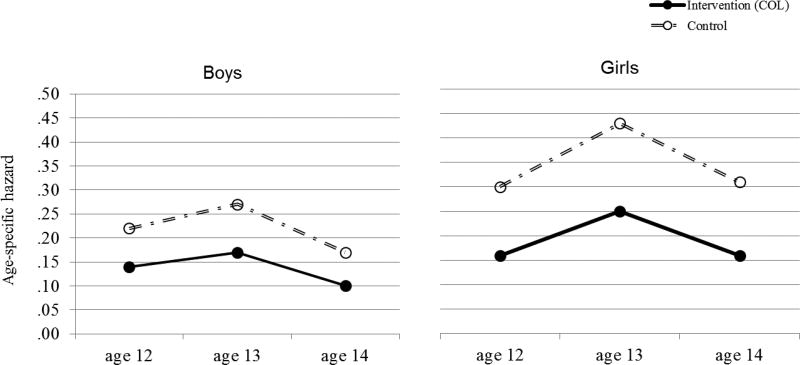
Due to left-censoring of participants who initiated marijuana use before the age of 12 and because of missing data on analysis variables, the sample size for the DTSA analysis was N=443 (Control Group N=226; Intervention Group N=217). AIC and BIC values from our preliminary DTSA models showed that a frailty model based on a proportional odds assumption provided the best fit. In the final model that included both intervention status and participant sex, the overall risk of marijuana initiation was 17.3% lower in the COL group than in the Control group (unstandardized log beta coefficient = −1.11, SE = 0.40, p < .01, standardized log beta coefficient = −.19). In addition, after controlling for intervention status, girls had a 15% higher risk of marijuana initiation compared to boys (unstandardized log beta coefficient = 0.81, SE = 0.39, p < .05, standardized log beta coefficient = .14). As shown in Figure 2, sex-specific analyses revealed that the intervention reduced the risk of marijuana initiation by 19% among boys (unstandardized log beta coefficient = −.59, SE = 0.26, p< .03, standardized log beta coefficient = −.21) and by 24% among girls (unstandardized log beta coefficient = −.81, SE=0.41, p< .05, standardized log beta coefficient = −.28).
Figure 2.
Hazard curve for initiation of marijuana, by COL intervention status and participant sex (with school cluster)
Frequency of Marijuana Use Over Time
Due to missing data on analysis variables, the sample size for the LGCM analysis was N=571 (Control Group N=292; Intervention Group N=279). Model fit statistics and parameter estimates from the LGCM analyses are presented in Table 3. Fit was adequate for all models. Marijuana use at Wave 2 was more frequent among Control group participants compared to COL participants (intercepts = 2.97 and 1.98, respectively). In the ‘normative model’ based on the Control group only (Model 1), frequency of marijuana use showed little change over the study period; slope = .03, ns. In contrast, the intervention group (Model 2) showed a significant increase over time in marijuana use (slope = .54, p<.0001). In the combined models, the effect of COL on change over time in marijuana frequency was positive but not statistically significant (slopes = .26 [ns] and .28 [ns] in Models 3 and 4, respectively). The interaction of COL * Wave 2 marijuana frequency was likewise nonsignificant (slope = .03).
Table 3.
Fit Statistics and Parameter Estimates for Linear Growth Curve Models of Past Month Marijuana Frequency
| Model | Χ2 | AICa | Adj BICb |
CFIc | RMSEAd | SRMRe | Inter- cept |
Slope | COLf Effect |
COLf X Initial (Wave 2) Status |
|
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Control (n=292) | 0.17 | 3925 | 3928 | 1.0 | .000 | 0.01 | 2.97g | 0.03 | n/a | n/a |
| 2 | COL (n=279) | 0.33 | 3913 | 3916 | 1.0 | .000 | 0.02 | 1.98g | 0.54g | n/a | n/a |
| 3 | Two-Group (n=571) | 1.67 | 7838 | 7850 | 1.0 | .000 | 0.04 | 2.38g | 0.21 | 0.26 | n/a |
| 4 | Two-Group w/Inter (n=571) | 1.60 | 7840 | 7853 | 1.0 | .000 | 0.04 | 2.38g | 0.22 | 0.28 | 0.03 |
Akaike Information Criterion
Bayesian information criterion
Comparative Fit Index
Root Mean Square Error of Approximation
Standardized Root Mean Square Residual
COL=Intervention Group.
p<.0001
Discussion
This secondary analysis of data from a school-based group randomized trial showed that AI youths who received the ‘Circle of Life’ (COL) intervention, a culturally-tailored HIV prevention program, were significantly less likely than their non-intervention counterparts to initiate marijuana use at ages 12, 13, and 14 if they had not already done so at each age. The effect was observed for both boys and girls although the positive impact was somewhat more pronounced among girls who were at greater risk for initiation at each age. These findings extend the results from the original trial, which showed that COL was effective in delaying sexual initiation among AI youths (26).
There was no evidence of an intervention effect on the frequency with which existing marijuana users engaged in the behavior. Prior to intervention exposure, marijuana users in the COL group used less frequently than those in the Control group. Over the study period, marijuana use among COL participants increased to a normative level approximating that of Control group participants.
Since COL was developed as a universal preventive program rather than an intervention specifically designed for high risk youth or those who are already using substances, it is perhaps not surprising that program impacts on marijuana uptake did not generalize to reductions in current use. It could be that the focus on volition and balance of the four parts of the Medicine Wheel were not salient to youth already using marijuana. Supplemental (booster) intervention content and/or increased program intensity with emphasis on changing behavior may be needed to extend the positive impact of the COL program to youths already engaged in risky behaviors.
Nevertheless, the results of this investigation point to the importance of delivering COL to preadolescents before risky behavior begins to emerge. This is consistent with the findings reported by Kaufman et al. (26), showing that the COL program was maximally effective in delaying sexual initiation among youths exposed at younger ages. Delaying the onset of substance use through early intervention exposure is a critical part of curbing problematic patterns of use later in life as well as preventing other risk behaviors that emerge secondary to substance use (6–13). This is particularly important for marijuana since its initiation among youths in this tribal population occurs earlier than that of other substances (8).
The results of this investigation address calls to move beyond interventions with singular impacts toward programs capable of influencing a broader range of risk behaviors that cluster together in adolescence (6) They contribute to a small but emerging literature on youth prevention programs that are effective in improving both substance use and sexual risk behavioral outcomes (22, 23). Programs previously shown to be effective in this regard were multifaceted interventions that address risk and protective factors at multiple levels, including individual, peer, family, school, and community (23). While COL was designed for middle school youth in the classroom, it is integrative and multilayered. This configuration, along with a solid theoretical foundation and cultural grounding, highlights the COL program as a promising intervention for reducing health disparities among AI youths.
Further establishing the broad effectiveness of COL requires additional steps, including evaluation of program impact on other forms of substance use (e.g., alcohol use, tobacco use) and related risk behaviors. Investigation into the mechanisms by which COL impacts risk behaviors is also warranted - both to inform theoretical models of behavior change and to better understand the essential components of the intervention program. It will also be useful to more fully explore the effects of COL exposure on the reduction of risk behaviors among youths already engaged in those behaviors. Such information is important to determine if program effects are limited to risk prevention or if they also generalize to harm reduction among youths already engaged in risk behavior. Finally, understanding the mechanisms underlying the sex-specific effects of the COL is another important area of exploration.
The current findings must be considered in light of several limitations in study methodology. Although the COL program was developed with input from a wide range of tribal representatives, the original trial was conducted in only one tribal setting and we cannot unequivocally assert that the program will be similarly effective in other AI/AN tribal settings. In addition, the tribal setting for the research included a finite number of schools that could be randomized to each study arm (<20), which reduced the statistical power of our analyses. Moreover, our outcome measures may have been subject to recall and other biases associated with self-reports and our assessment of past month marijuana use was limited to a single item frequency measure. The conservative nature of the tests may have underestimated the true impact of the COL intervention on marijuana initiation and/or contributed to our failure to find program effects on the frequency of marijuana use.
Despite these limitations, the present study affirms the value of the COL program as a multifaceted, culturally tailored, skills-based program for preventing marijuana use among AI youth. The current evidence that COL is effective in reducing risk for marijuana use, in combination with its previously demonstrated impact on sexual risk behaviors, has important implications for low-resource settings where comprehensive prevention programs are needed to efficiently and cost-effectively address the range of risk behavior that threatens the health of young people.
Acknowledgments
We thank the schools and the tribal community for their ongoing support, and are grateful to the parents, guardians, and youths who gave so generously of their time. This project reflects the dedicated work of the project staff, led by Jennifer Desserich, and community members Angela Sam, and Cindy Wheeler, without whom the extensive data collection necessary to this longitudinal project would not have been possible. We acknowledge the support of the National Institute of Mental Health (R01 MH069086; Kaufman, PI); the Bureau of Indian Education, Division of Performance and Accountability; the National Institute on Drug Abuse (R01 DA027665; Whitesell, PI); and the Office of Adolescent Health (TP2AH000003; Kaufman, PI). The views expressed are solely those of the authors and do not necessarily represent the policies of any supporting agencies.
Footnotes
Financial Disclosures: The authors report no relevant financial conflicts.
This specification was used by Muthén and Curran (1997) for model identification purposes.
References
- 1.Gonzales K, Roeber J, Kanny D, Tran A, Saiki C, Johnson H, Yeoman K, Safranek T, Creppage K, Lepp A, Miller T, Tarkhashvili N, Lynch KE, Watson JR, Henderson D, Christenson M, Geiger SD. Alcohol-attributable deaths and years of potential life lost — 11 states, 2006–2010. MMWR. 2014;63:213–216. [PMC free article] [PubMed] [Google Scholar]
- 2.Whitesell NR, Beals J, Big Crow C, Mitchell CM, Novins DK. Epidemiology and etiology of substance use among American Indians and Alaska Natives: risk, protection, and implications for prevention. Am J Drug Alcohol Abuse. 2012;38(5):376–382. doi: 10.3109/00952990.2012.694527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jarman D, Naimi TS, Nelson DE, Brewer RD, et al. Alcohol-attributable deaths and years of potential life lost among American Indians and Alaska Natives — United States, 2001–2005. MMWR. 2008;57:938–941. [PubMed] [Google Scholar]
- 4.Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. The NSDUH Report: Need for and Receipt of Substance Use Treatment among American Indians or Alaska Natives. Nov, 2012. [Google Scholar]
- 5.Center for Behavioral Health Statistics and Quality. Behavioral Health Trends in the United States: Results from the 2014 National Survey on Drug Use and Health (HHS Publication No. SMA 15-4927, NSDUH Series H-50) 2015 Retrieved from http://www.samhsa.gov/data/
- 6.Ramisetty-Mikler S, Ebama MS. Alcohol/drug exposure, HIV-related sexual risk among urban American Indian and Alaska Native youth: evidence from a national survey. J Sch Health. 2011;81:671–679. doi: 10.1111/j.1746-1561.2011.00643.x. [DOI] [PubMed] [Google Scholar]
- 7.de Ravello L, Everett Jones S, Tulloch S, Taylor M, Doshi S. Substance use and sexual risk behaviors among American Indian and Alaska Native high school students. J Sch Health. 2014;84:25–32. doi: 10.1111/josh.12114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Whitesell NR, Kaufman CE, Keane EM, Big Crow C, Shangreau C, Mitchell CM. Patterns of substance use initiation among young adolescents in a Northern Plains American Indian tribe. Am J Drug Alcohol Ab. 2012;38(5):383–388. doi: 10.3109/00952990.2012.694525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stanley LR, Harness SD, Swaim RC, Beauvais F. Rates of substance use of American Indian students in 8th, 10th, and 12th grades living on or near reservations: update, 2009–2012. Public Health Rep. 2014;129:156–163. doi: 10.1177/003335491412900209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kunitz SJ. Risk factors for polydrug use in a Native American population. Subst Use Misuse. 2008;43:331–339. doi: 10.1080/10826080701202783. [DOI] [PubMed] [Google Scholar]
- 11.Windle M, Spear LP, Fuligni AJ, Angold A, Brown JD, Pine D, Smith GT, Giedd J, Dahl RE. Transitions into underage and problem drinking: developmental processes and mechanisms between 10 and 15 years of age. Pediatrics. 2008;121:S273–S289. doi: 10.1542/peds.2007-2243C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Whitesell NR, Beals J, Mitchell CM, Manson SM, Turner RJ AI-SUPERPFP Team. Childhood exposure to adversity and risk of substance-use disorder in two American Indian populations: the meditational role of early substance-use initiation. J. Stud. Alcohol Drugs. 2009;70:971–981. doi: 10.15288/jsad.2009.70.971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stueve A, O’Donnell LN. Early alcohol initiation and subsequent sexual and alcohol risk behaviors among urban youths. Am J Public Health. 2005;95:887–893. doi: 10.2105/AJPH.2003.026567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. [Accessed 10/8/15];Youth online: high school YRBS. 2015 http://www.cdc.gov/healthyyouth/data/yrbs/results.htm.
- 15.Stanley LR, Swaim RC. Initiation of alcohol, marijuana, and inhalant use by American-Indian and white youth living on or near reservations. Drug Alcohol Depen. 2015;155:90–98. doi: 10.1016/j.drugalcdep.2015.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Whitesell NR, Asdigian NL, Kaufman CE, Big Crow C, Shangreau C, Keane EM, Mousseau AC, Mitchell CM. Trajectories of substance use among young American Indian adolescents: patterns and predictors. J Youth Adolesc. 2014;43(3):437–53. doi: 10.1007/s10964-013-0026-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jackson JM, Seth P, DiClemente RJ, Lin A. Association of depressive symptoms and substance use with risky sexual behavior and sexually transmitted infections among African American female adolescents seeking sexual health care. Am J Public Health. 2015;105:2137–2142. doi: 10.2105/AJPH.2014.302493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shaughnessy L, Doshi SR, Everett Jones S. Attempted suicide and associated health risk behaviors among Native American high school students. J Sch Health. 2004;74(5):177–182. doi: 10.1111/j.1746-1561.2004.tb08217.x. [DOI] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention. [Accessed 10/8/15];HIV/AIDS among American Indians and Alaska Natives. 2015 http://www.cdc.gov/hiv/group/racialethnic/aian/index.html.
- 20.Kaufman CE, Desserich J, Big Crow CK, Holy Rock B, Keane E, Mitchell CM. Culture, context, and sexual risk among Northern Plains American Indian youth. Soc Sci Med. 2007;64:2152–2164. doi: 10.1016/j.socscimed.2007.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leston JD, Jessen CM, Simons BC. Alaska native and rural youth views of sexual health: a focus group project on sexually transmitted diseases, HIV/AIDS, and unplanned pregnancy. Am Indian Alaska Nat. 2012;19(1):1–14. doi: 10.5820/aian.1901.2012.1. [DOI] [PubMed] [Google Scholar]
- 22.Eaton NR, Thompson RG, Jr, Hu M, Goldstein RB, Saha TD, Hasin DS. Regularly drinking alcohol before sexual activity in a nationally representative sample: prevalence, sociodemographics, and associations with psychiatric and substance use disorders. Am J Public Health. 2015;105:1387–1393. doi: 10.2105/AJPH.2015.302556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jackson C, Geddes R, Haw S, Frank J. Interventions to prevent substance use and risky sexual behaviour in young people: a systematic review. Addiction. 2011;107(4):733–747. doi: 10.1111/j.1360-0443.2011.03751.x. [DOI] [PubMed] [Google Scholar]
- 24.Kaufman CE, Mitchell CM, Beals J, Desserich JA, Wheeler C, Keane EM, Whitesell NR, Sam A, Sedey C. Circle of Life: rationale, design, and baseline results of an HIV prevention intervention among young American Indian adolescents of the Northern Plains. Prev Sci. 2010;11(1):101–112. doi: 10.1007/s11121-009-0153-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kaufman CE, Litchfield A, Schupman E, Mitchell CM. Circle of Life HIV/AIDS-prevention intervention for American Indian and Alaska Native youth. Am Indian Alaska Nat. 2012;19(1):140–53. doi: 10.5820/aian.1901.2012.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kaufman CE, Whitesell NR, Keane EM, Desserich JA, Giago C, Sam A, Mitchell CM. Effectiveness of Circle of Life, an HIV-preventive intervention for American Indian middle school youths: a group randomized trial in a Northern Plains tribe. Am J Pub Hlth. 2014;104(6):e106–e112. doi: 10.2105/AJPH.2013.301822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.IBM Corp. Released. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp; 2013. [Google Scholar]
- 28.Muthén LK, Muthén BO. Mplus User’s Guide. Seventh. Los Angeles, CA: Muthén & Muthén; 1998–2012. [Google Scholar]
- 29.Muthén B, Masyn K. Discrete time survival mixture analysis. J Educ Behav Stat. 2005;30(1):27–58. [Google Scholar]
- 30.Muthén B, Curran P. General longitudinal modeling of individual differences in experimental designs: a latent variable framework for analysis and power estimation. Psych Meth. 1997;2:371–402. [Google Scholar]
- 31.Kline RB. Principles and Practice of Structural Equation Modeling. 3. London: The Guilford Press; 2011. [Google Scholar]
- 32.Allison PD. Missing data techniques for structural equation modeling. J Abnorm Psychol. 2003;112(4):545–557. doi: 10.1037/0021-843X.112.4.545. [DOI] [PubMed] [Google Scholar]