Abstract
Penetrating atherosclerotic ulcers (PAUs) of the aorta are defined as atherosclerotic lesions with aortic intima and media ulceration, which may lead to a complete rupture of the adventitial wall. The present article aimed to report an unusual case of a surgically treated patient with abdominal aorta PAU with an illustration of the key features and to review and analyze the existing literature data. PAUs typically develop in elderly and hypertensive patients and in patients with advanced atherosclerosis. Although originally described for the descending thoracic aorta, a similar clinicopathological entity also occurs in the abdominal aorta. Patients with symptoms of a PAU should be treated immediately if they are fit for surgery. Exceptive observation by imaging modalities is necessary in patients with asymptomatic small (<2 cm) PAU, with or without focal dissection.
Keywords: Penetrating atherosclerotic ulcer, Abdominal aorta, Acute aortic syndrome
INTRODUCTION
A penetrating atherosclerotic ulcer (PAU) is an atherosclerotic lesion frequently observed in the descending thoracic aorta (DTA) and abdominal aorta (AA) in severe atherosclerotic patients. PAUs were first reported by Shennan in 1934 [1] and is currently included in the category of acute aortic syndrome (AAS) including overt aortic dissection (AD), PAU, and intramural hematoma (IMH) with a prevalence of 2% to 7% of AAS [2–4].
Although the exact pathogenesis is largely unknown, a PAU is thought to be formed secondary to aortic plaque rupture, which could cause an aortic intimal tear or aortic rupture. Several factors may be involved with the entrance-tear formation in AAS including the aortic root motion, the geometry of the aorta, wall stress, intrinsic aortic tissue abnormalities, and aortic plaque rupture [5–8].
PAUs are asymptomatic and confined to the intimal layer, and progressive penetration into the elastic lamina and the media may lead to a great spectrum of clinical conditions with a variety of behaviors. A PAU may be self-limited to the aortic intima due to the fibrotic component of the atheromatous plaque with the development of a small, circumscribed area of ulceration, while in other cases, the lesion may extend up to the outer aortic wall, causing focal AD. Moreover, one of the complications of PAUs is IMH formation that can result to pseudoaneurysm or saccular aneurysm (SA) with a risk of aortic rupture [4,9].
The natural history of PAUs remains elusive, and the optimal therapeutic regimen is controversial. While asymptomatic cases of PAU may be managed conservatively with close follow-up, endovascular repair is actually the gold standard for complicated PAUs of the DTA. At the level of the AA, a PAU is often managed by open repair. We present a case of surgically treated PAU at the level of the infrarenal aorta. An extensive literature review (1974 to 2015) is conducted to discuss the management of PAUs of the AA.
CASE
A 69-year-old male patient was referred to vascular division complaining of sharp pain specifically located at the right lumbar area for the past 1 month. On physical examination, the patient had intact and symmetrical pulses in the upper and lower extremities and no signs of palpable abdominal mass. His personal medical history revealed arterial hypertension and hyperlipidemia. The patient had a 45 pack-year smoking history. The laboratory test revealed a slight increase in white blood cells (WBCs, 11,500/μL; normal range, 5,000/μL-10,000/μL) and C-reactive protein (CRP, 3 mg/dL; normal range, <0.5 mg/dL) and slight decrease in hemoglobin (Hb, 13 g/dL; normal range, 13.8–17.2 g/dL).
Contrast-enhanced computed tomography (CT) scan images from the abdominal and thoracic area revealed the presence of a SA in the anatomical region of the AA mimicking a windsock (Fig. 1) and a large IMH and aortic wall thickening and calcification, findings compatible with a PAU (Fig. 2, 3). Considering the relatively good health status of the patient, we decided to perform open surgery. The aortic repair consisted of the replacement of the diseased aortic segment by a tubular Dacron graft (Fig. 4). The patient had an uncomplicated postoperative course and was discharged from the hospital on the 5th postoperative day. According to the histopathological report, there was diffuse ulceration of the intima and thrombus underneath the atherosclerotic intima and media layers (Fig. 5).
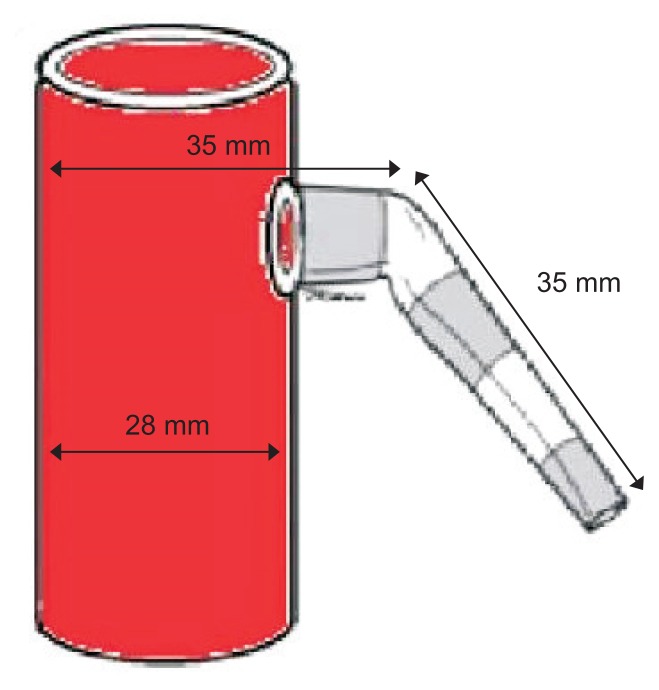
Fig. 1.
The dimensions of the penetrating atherosclerotic ulcer mimicking a windsock as assessed by computed tomography imaging.
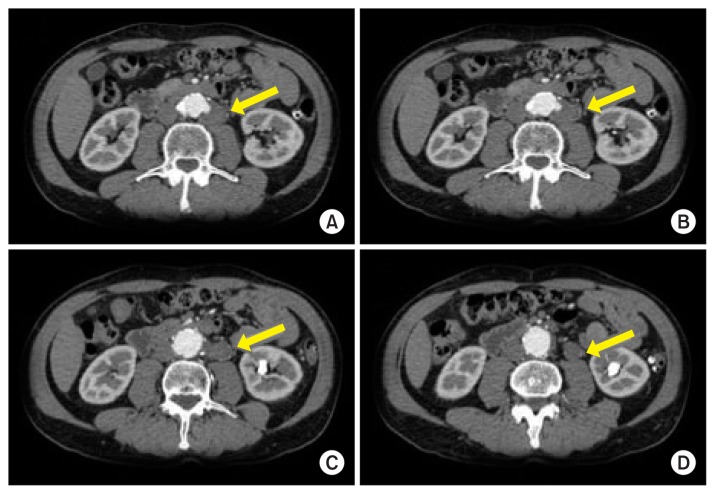
Fig. 2.
(A–D) Contrast-enhanced computed tomography images of the abdominal and thoracic area revealed the presence of a saccular aneurysm (arrows) and a large intramural hematoma, findings compatible with a penetrating atherosclerotic ulcer.
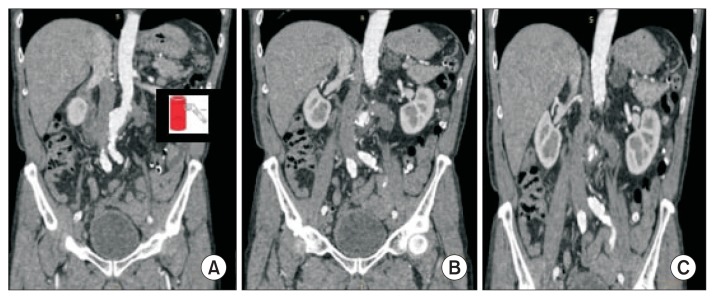
Fig. 3.
(A–C) Axial images as assessed by computed tomography imaging of the abdomen revealed the presence of a saccular aneurysm in the anatomical region of the abdominal aorta mimicking a windsock.
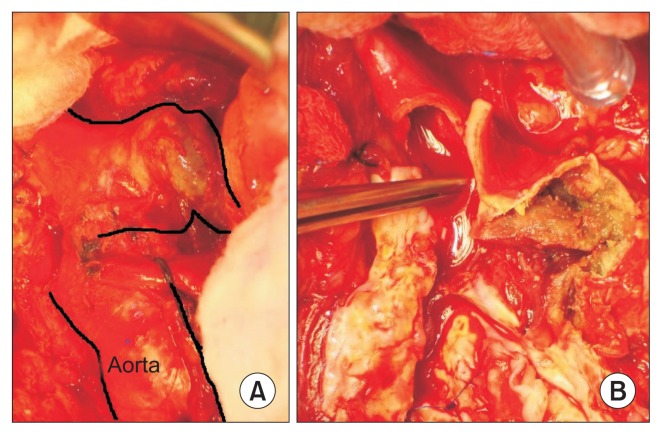
Fig. 4.
(A, B) Intraoperative images of the penetrating atherosclerotic ulcer.
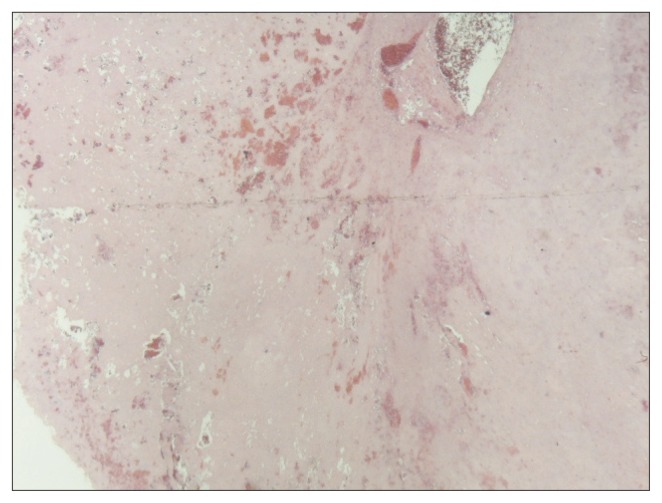
Fig. 5.
Histopathological image revealed arterial wall with atherosclerotic lesions with diffuse ulceration of the intima and thrombus underneath the atherosclerotic intima and media layers (H&E, ×20).
DISCUSSION
AAS was defined as a clinical entity by Vilacosta et al. [10] and Vilacosta and San Román [11], who described three different pathophysiological mechanisms presenting in a similar clinical manner. This disease occurs mainly in elderly patients, between the sixth and eighth decades of life. PAUs occur mainly in the DTA, and it is usually associated with hypertension (approximately 94% of cases) and smoking habit. Most of these patients have other atherosclerotic disease manifestations, and half of these patients have a history of thoracic aortic aneurysm or abdominal aortic aneurysm. The clinical picture mimics the symptomatology of a classic AD, with anterior chest pain in the ulcers of the ascending aorta and interscapular or back pain in lesions located at the DTA. Unlike classical dissection, ischemia or embolization in the limbs or other organs is less common [12,13].
However, a PAU exhibits a greater risk of rupture [12–14]. On CT and magnetic resonance imaging, PAUs are characterized by a contrast-filled crater that communicates with the aortic lumen [15]. The usual description on computed tomography angiography (CTA) includes the measurement of the maximum aortic diameter at the ulcer site, the depth of the ulcer, and the length of the intimal defect (width) at the ulcer site, while the growth rate in abdominal PAU is about 3 mm/y [15,16]. A coexisting extra-aortic hematoma, which measures >20 mm in width or >10 mm in depth or which progresses into a total abdominal aortic diameter, all are considered complicated PAUs [9,15,16]. Some authors extend the definition of PAUs to ulcerative lesions not extending beyond the aortic wall [17,18].
Nevertheless, according to the Mayo Clinic Classification, the three radiological diagnostic criteria for PAUs on contrast-enhanced CT scans are a transmural rupture with extra-aortic hematoma, a well-defined ulcer crater in the aortic wall, and a subadventitial SA extending beyond the wall of the aorta [2]. Vorp et al. [19] reported the importance of the shape and symmetry, in addition to the size, in evaluating the risk of rupture.
Despite these efforts, there is still a paucity of predictors of the natural history and the behavior of PAUs, and no standard treatment has been established [13].
A PAU may progress into SA, focal AD, or aortic rupture. At the level of the AA, SA formation is observed more often than focal dissection. Hollier et al. [20] recommended surgical intervention for asymmetrical SAs, irrespective of their size, considering the risk of rupture. It has been recommended that treatment should be performed as early as possible in relatively young and fit patients.
Isolated dissection of the AA is rarely observed (0.4% to 2% of all ADs) [19]. The presence of a PAU may favor the development of focal abdominal AD. The onset of this dissection is often acute, with abdominal and low back pain, though some cases remain asymptomatic and are incidentally detected.
Fluid-structure interaction analysis concluded that low wall shear stress (lower than 1.5 N/m2) and high shear stress oscillation (oscillatory shear index=0.13) over the cardiac cycle in the PAU region could be considered key hemodynamic factors that result in the rupture of the PAU [20].
The differential diagnoses include inflammatory abdominal aortic aneurysm (IAAA) and inflammatory aortitis, such as Takayasu arteritis, giant cell arteritis, Behçet disease, Kawasaki disease, rheumatoid arthritis, sarcoidosis, Cogan syndrome, ankylosing spondylitis, systemic lupus erythematosus, and Wegener’s granulomatosis.
An IAAA is defined by an unusually thickened aneurysm wall, shiny white peri-aneurysmal and retroperitoneal fibrosis, and dense adhesions of the adjacent intra-abdominal structures. The differential diagnoses are established by negative bacterial blood cultures, negative skin test, negative serological tests, the localization of the AA, and the typical anatomical features on CTA, while biopsy may be warranted to exclude malignancy. The patients with inflammatory aortitis must be prescribed with immunosuppressive therapy, which is based on the risk of rupture related to aneurysm dimension and the presence of secondary organ vascular insufficiency related to fibrotic stenosis, before and after the surgical intervention.
Invasive treatment (open surgery or endovascular stent grafting) is indicated in acute or symptomatic cases, while course observation using periodic evaluation by imaging techniques is recommended for asymptomatic or chronic cases of small (<2 cm) PAUs [20]. Open surgical repair with graft interposition is associated with higher operative morbidity and mortality due to the patient’s poor general condition and comorbidities. On the contrary, endovascular stent grafting is a less invasive procedure and is more appropriate for such frail patients. Since a PAU is a focal lesion, an adequate landing zone is almost present. Therefore, the risk of migration or endoleak is low, although the presence of IMH appears to delay the effectiveness of endovascular therapy. Furthermore, an open surgery may be preferred for younger, healthier patients in whom there is much less difference in operative risk between the two strategies and for patients whose long-term durability is important. Herein, we report a distinctive case of an open surgically treated patient with AA PAU, considering the parameters that support open surgical intervention.
1) Literature review
To identify clinical studies reporting cases and/or series of patients with a PAU, an electronic MEDLINE, Scopus, and Google Scholar literature search was performed from 1974 (first publication of penetrating aortic ulcer) to 2015 using the keywords “penetrating atherosclerotic ulcers,” “abdominal aorta,” and their combinations, and the search was summarized according to age, sex, risk factors, clinical manifestations, and treatment. Due to the extreme heterogeneity of the studies, no weighted estimations, comparisons, and correlations have been performed.
Literature review revealed mainly case reports of PAUs at the level of the AA and a rare series of greater than 10 cases. We collected 298 published cases of PAUs of the AA (Table 1) [12,13,17,18,21–61].
Table 1.
Cases and/or series of PAUs stratified according to the year of publication, number of patients, age, sex, risk factors, and treatment characteristics
| Study (reference) | Number of patients | Mean age (y) | Sex (male/female) | Risk | Treatment |
|---|---|---|---|---|---|
| Lagaay [21] | 3 | 58 | 3/0 | HTN-CAD | ABI (2)-tube (1) |
| Cornud et al. [22] | 1 | 53 | 1/0 | CAD | Tube |
| Barbier et al. [23] | 1 | 73 | 0/1 | NA | ABI |
| Aschraft et al. [24] | 1 | 60 | 0/1 | HTN-PAD | Tube |
| Nora and Hollier [25] | 1 | 56 | 1/0 | HTN | Surgical interposition graft |
| Barba et al. [26] | 1 | 37 | 1/0 | NA | Surgical interposition graft |
| Rothwell and Lane [27] | 1 | 72 | 1/0 | HTN | Tube |
| Harris et al. [13] | 10 | 74 | 10/0 | HTN-CKD-CAD | Medical (3), surgical interposition graft (7) |
| Origuchi et al. [28] | 4 | 59 | 3/1 | HTN (1) | ABI (3)-tube (1) |
| Goldstein et al. [29] | 1 | 67 | 1/0 | HTN-CAD | Dacron aorto-iliac graft |
| Moriyama et al. [30] | 1 | 74 | 1/0 | HTN | Woven Dacron aorto-iliac graft |
| Taylor nd Kalman [31] | 4 | 73 | 4/0 | HTN-CAD-PAD | Tube Dacron (2)-Dacron patch (2) |
| Hayashi et al. [32] | 1 | 73 | 1/0 | NA | Medical |
| Quint et al. [33] | 1 | NA | Medical | ||
| Toda et al. [34] | 2 | 70 | 2/0 | HTN-CAD-PAD | Surgical interposition graft |
| Farooq et al. [35] | 2 | 68 | 2/0 | HTN (2)-PAD | ABI (1)-tube (1) |
| Ganaha et al. [12] | 31 | 71 | 15/16 | HTN | Interposition stent graft |
| Tsuji et al. [17] | 4 | 79.5 | 4/0 | HTN (4)-CAD (2) | EVAR (4) |
| Vasquez et al. [36] | 1 | 81 | 1/0 | HTN (1) | Stent graft |
| Saiki et al. [37] | 1 | 81 | 0/1 | HTN (1) | Resection graft (AFB) |
| Feld et al. [38] | 1 | 68 | 1/0 | CKD | EVAR (1) |
| Minor et al. [39] | 2 | 55 | 2/0 | HTN-CAD-PAD | ABI (2) |
| Ventura et al. [40] | 1 | 68 | 0/1 | HTN (1) | ABI |
| Takagi et al. [41] | 1 | 64 | 1/0 | NA | Surgical interposition graft |
| Batt et al. [18] | 8 | 70 | 7/1 | HTN (4)-CAD (3)-PAD (6) | Surgical interposition graft (5) (tube 3-Dacron aorto-iliac graft 2)- EVAR (3) |
| Chernenkov et al. [42] | 1 | 80 | 1/0 | HTN | Tube |
| Tanigushi et al. [43] | 1 | 82 | 0/1 | CAD | Hemashield tube, left aortorenal bypass |
| Sensi et al. [44] | 11 | 76.7 | 10/1 | HTN (9)-CKD (1)-CAD (6) | ABI (4)-tube (1)- EVAR (6) |
| Eggebrecht et al. [45] | 22 | 69.1 | 16/6 | HTN (2)-CKD (9)-CAD (12) | EVAR (22) |
| Thalheimer et al. [46] | 1 | 57 | 1/0 | HTN-CAD-PAD | Tube (1) |
| Dalainas et al. [47] | 2 | 68.6 | 2/0 | HTN (2)-CKD (2)-CAD (5) | EVAR (2) |
| Piffaretti et al. [48] | 13 | 73 | 12/1 | HTN (13)-CKD (2)-CAD (2)-PAD (6) | EVAR (13) |
| Fyntanidou et al. [49] | 4 | 67 | 4/0 | HTN (4)-CKD (1)-CAD (1) | EVAR (4) |
| Lindblad et al. [50] | 19 | 72 | 16/3 | NA | EVAR (19) |
| Afifi et al. [51] | 1 | 76 | 0/1 | HTN-CAD-PAD | EVAR (1) |
| Hyhlik-Dürr et al. [52] | 20 | 72 | 20/0 | HTN (19)-CKD (4)-CAD (8) | EVAR (20) |
| Kutsukata et al. [53] | 1 | 64 | 0/1 | HTN | Dacron aorto-iliac graft (1) |
| Ferro et al. [54] | 1 | 64 | 0/1 | HTN-CAD | EVAR (1) |
| Kainuma et al. [55] | 1 | 67 | 1/0 | HTN | EVAR (1) |
| Nathan et al. [56] | 20 | NA | EVAR (10)-open repair (10) | ||
| Sadeghi-Azandaryani et al. [57] | 1 | 76 | 1/0 | HTN-CAD | EVAR (1) |
| Kazan et al. [58] | 3 | 71 | 2/1 | HTN (1)-CAD | EVAR (3) |
| Palombo et al. [59] | 3 | 67 | 3/0 | HTN (3)-CKD (2)-CAD (4)-PAD (2) | EVAR (3) |
| Papazoglou et al. [60] | 1 | 69 | 1/0 | HTN | EVAR |
| Georgiadis et al. [61] | 19 | 70 | 18/1 | HTN (18)-CKD (8)-CAD (11)-PAD (9) | EVAR (19) |
| Total | 230 | 49/164 (29.9%)a | 115/164 (70.1%)b |
PAUs, penetrating atherosclerotic ulcers; HTN, hypertension; CAD, coronary artery disease; ABI, aortoiliac graft; NA, not available; PAD, peripheral arterial disease; CKD, chronic kidney disease; EVAR, endovascular aneurysm repair; AFB, axillary bifemoral bypass; IMH, intramural hematoma; SA, saccular aneurysm.
Surgical treatment,
endovascular repair.
The median age of the patients was 72 years, and PAUs are almost dominated by males (90.3%). Hypertension (80%) and concomitant coronary or peripheral arterial occlusive disease (30.7%) are very common. Asymptomatic PAUs are incidentally detected in 40.3% of the reported cases. Most patients with a PAU of the AA complain of pain (43.8%). A minority (11.9%) of patients present with a hypovolemic shock, secondary to the rupture of a complicated PAU. Most authors reported endovascular stent graft repair as the treatment of choice (62%), while conservative management was chosen only for 2.6% of the patients. Open surgical repair was performed in 35.4% of patients.
In conclusion, PAUs usually develop in the thoracic aorta but can similarly occur in the AA and may progress into focal AD, SA, or aortic rupture. Symptomatic PAU; large, profound (>2 cm) PAU; and complicated PAU of the AA (evolving to a SA or focal AD) require surgical treatment if the patient is fit for surgery. In this case, we performed an open surgery due to younger age and good general condition of the patient; the type of the graft or bifurcated tube depends on the PAU location and the condition of the arterial wall. The endovascular approach is a less invasive alternative to open surgery, with excellent short-term outcomes according to the recent literature. However, currently there are insufficient long-term studies for PAU.
Footnotes
CONFLICTS OF INTEREST
The authors have nothing to disclose.
REFERENCES
- 1.Shennan T. Dissecting aneurysms. London: His Majesty’s Stationery Office; 1934. [Google Scholar]
- 2.Stanson AW, Kazmier FJ, Hollier LH, Edwards WD, Pairolero PC, Sheedy PF, et al. Penetrating atherosclerotic ulcers of the thoracic aorta: natural history and clinicopathologic correlations. Ann Vasc Surg. 1986;1:15–23. doi: 10.1016/S0890-5096(06)60697-3. [DOI] [PubMed] [Google Scholar]
- 3.Tumelero RT, Duda NT, Tognon AP, Panata L, Teixeira JC, Giongo JB. Endovascular stent-graft treatment of penetrating aortic ulcer. Arq Bras Cardiol. 2011;96:e20–e23. doi: 10.1590/S0066-782X2011000200015. [DOI] [PubMed] [Google Scholar]
- 4.Coady MA, Rizzo JA, Hammond GL, Pierce JG, Kopf GS, Elefteriades JA. Penetrating ulcer of the thoracic aorta: what is it? How do we recognize it? How do we manage it? J Vasc Surg. 1998;27:1006–1015. doi: 10.1016/S0741-5214(98)70003-5. [DOI] [PubMed] [Google Scholar]
- 5.Poullis MP, Warwick R, Oo A, Poole RJ. Ascending aortic curvature as an independent risk factor for type A dissection, and ascending aortic aneurysm formation: a mathematical model. Eur J Cardiothorac Surg. 2008;33:995–1001. doi: 10.1016/j.ejcts.2008.02.029. [DOI] [PubMed] [Google Scholar]
- 6.Beller CJ, Labrosse MR, Thubrikar MJ, Robicsek F. Finite element modeling of the thoracic aorta: including aortic root motion to evaluate the risk of aortic dissection. J Med Eng Technol. 2008;32:167–170. doi: 10.1080/03091900600687672. [DOI] [PubMed] [Google Scholar]
- 7.Robicsek F, Thubrikar MJ. Hemodynamic considerations regarding the mechanism and prevention of aortic dissection. Ann Thorac Surg. 1994;58:1247–1253. doi: 10.1016/0003-4975(94)90523-1. [DOI] [PubMed] [Google Scholar]
- 8.Angouras D, Sokolis DP, Dosios T, Kostomitsopoulos N, Boudoulas H, Skalkeas G, et al. Effect of impaired vasa vasorum flow on the structure and mechanics of the thoracic aorta: implications for the pathogenesis of aortic dissection. Eur J Cardiothorac Surg. 2000;17:468–473. doi: 10.1016/S1010-7940(00)00382-1. [DOI] [PubMed] [Google Scholar]
- 9.Geisbüsch P, Kotelis D, Weber TF, Hyhlik-Dürr A, Kauczor HU, Böckler D. Early and midterm results after endovascular stent graft repair of penetrating aortic ulcers. J Vasc Surg. 2008;48:1361–1368. doi: 10.1016/j.jvs.2008.07.058. [DOI] [PubMed] [Google Scholar]
- 10.Vilacosta I, San Román JA, Aragoncillo P, Ferreirós J, Mendez R, Graupner C, et al. Penetrating atherosclerotic aortic ulcer: documentation by transesophageal echocardiography. J Am Coll Cardiol. 1998;32:83–89. doi: 10.1016/S0735-1097(98)00194-6. [DOI] [PubMed] [Google Scholar]
- 11.Vilacosta I, San Román JA. Acute aortic syndrome. Heart. 2001;85:365–368. doi: 10.1136/heart.85.4.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ganaha F, Miller DC, Sugimoto K, Do YS, Minamiguchi H, Saito H, et al. Prognosis of aortic intramural hematoma with and without penetrating atherosclerotic ulcer: a clinical and radiological analysis. Circulation. 2002;106:342–348. doi: 10.1161/01.CIR.0000022164.26075.5A. [DOI] [PubMed] [Google Scholar]
- 13.Harris JA, Bis KG, Glover JL, Bendick PJ, Shetty A, Brown OW. Penetrating atherosclerotic ulcers of the aorta. J Vasc Surg. 1994;19:90–98. doi: 10.1016/S0741-5214(94)70124-5. [DOI] [PubMed] [Google Scholar]
- 14.Buffolo E, Pessa CJN. [Penetrating atherosclerotic aortic ulcers and intramural aortic hematoma - a present review]. Rev Soc Cardiol Estado de São Paulo. 2001;11:1053–1059. Portuguese. [Google Scholar]
- 15.Hansen NJ. Computed tomographic angiography of the abdominal aorta. Radiol Clin North Am. 2016;54:35–54. doi: 10.1016/j.rcl.2015.08.005. [DOI] [PubMed] [Google Scholar]
- 16.Gifford SM, Duncan AA, Greiten LE, Gloviczki P, Oderich GS, Kalra M, et al. The natural history and outcomes for thoracic and abdominal penetrating aortic ulcers. J Vasc Surg. 2016;63:1182–1188. doi: 10.1016/j.jvs.2015.11.050. [DOI] [PubMed] [Google Scholar]
- 17.Tsuji Y, Tanaka Y, Kitagawa A, Hino Y, Taniguchi T, Sugimoto K, et al. Endovascular stent-graft repair for penetrating atherosclerotic ulcer in the infrarenal abdominal aorta. J Vasc Surg. 2003;38:383–388. doi: 10.1016/S0741-5214(03)00139-3. [DOI] [PubMed] [Google Scholar]
- 18.Batt M, Haudebourg P, Planchard PF, Ferrari E, Hassen-Khodja R, Bouillanne PJ. Penetrating atherosclerotic ulcers of the infrarenal aorta: life-threatening lesions. Eur J Vasc Endovasc Surg. 2005;29:35–42. doi: 10.1016/j.ejvs.2004.09.025. [DOI] [PubMed] [Google Scholar]
- 19.Vorp DA, Raghavan ML, Webster MW. Mechanical wall stress in abdominal aortic aneurysm: influence of diameter and asymmetry. J Vasc Surg. 1998;27:632–639. doi: 10.1016/S0741-5214(98)70227-7. [DOI] [PubMed] [Google Scholar]
- 20.Hollier LH, Taylor LM, Ochsner J. Recommended indications for operative treatment of abdominal aortic aneurysms. Report of a subcommittee of the Joint Council of the Society for Vascular Surgery and the North American Chapter of the International Society for Cardiovascular Surgery. J Vasc Surg. 1992;15:1046–1056. doi: 10.1016/0741-5214(92)90462-H. [DOI] [PubMed] [Google Scholar]
- 21.Lagaay MB. Spontaneous rupture of non aneurysmatic abdominal aorta. J Cardiovasc Surg. 1974;15:490–493. [PubMed] [Google Scholar]
- 22.Cornud F, Grenier P, Brauner M, Couffinhal JC, Parrot AM, Nahum H. [Rupture of an atheromatous plaque in a non-ectatic sub-renal aorta without evidence of an infectious process (author’s transl)]. J Radiol. 1980;61:285–286. French. [PubMed] [Google Scholar]
- 23.Barbier J, Vouhe P, Carretier M, Montaz N. [Spontaneous rupture of the aorta through an atheromatous plaque. A case]. Presse Med. 1983;12:1303. French. [PubMed] [Google Scholar]
- 24.Ashcraft WC, McCallum T, Gullickson D, Fulton RL. Spontaneous rupture of the normal diameter atherosclerotic aorta. J Ky Med Assoc. 1984;82:159–162. [PubMed] [Google Scholar]
- 25.Nora JD, Hollier LH. Contained rupture of the suprarenal aorta. J Vasc Surg. 1987;5:651–654. doi: 10.1016/0741-5214(87)90235-7. [DOI] [PubMed] [Google Scholar]
- 26.Barba A, Escribano JV, García-Alfageme A. [Ulcerated plaque in the terminal aorta as a source of recurrent embolism in the young patient]. Angiologia. 1990;42:59–62. Spanish. [PubMed] [Google Scholar]
- 27.Rothwell JM, Lane C. Spontaneous rupture of the non-aneurysmal atherosclerotic abdominal aorta. Am Surg. 1993;59:451–452. [PubMed] [Google Scholar]
- 28.Origuchi N, Shigematsu H, Nunokawa M, Yasuhura H, Muto T. Spontaneous perforation of a non-aneurysmal atherosclerotic abdominal aorta or femoral artery. Cardiovasc Surg. 1996;4:351–355. doi: 10.1016/0967-2109(95)00093-3. [DOI] [PubMed] [Google Scholar]
- 29.Goldstein DJ, Flores RM, Todd GJ. Rupture of a nonaneurysmal atherosclerotic infrarenal aorta. J Vasc Surg. 1997;26:700–703. doi: 10.1016/S0741-5214(97)70073-9. [DOI] [PubMed] [Google Scholar]
- 30.Moriyama Y, Yamamoto H, Hisatomi K, Matsumoto H, Shimokawa S, Toyohira H, et al. Penetrating atherosclerotic ulcers in an abdominal aortic aneurysm: report of a case. Surg Today. 1998;28:105–107. doi: 10.1007/BF02483620. [DOI] [PubMed] [Google Scholar]
- 31.Taylor BV, Kalman PG. Saccular aortic aneurysms. Ann Vasc Surg. 1999;13:555–559. doi: 10.1007/s100169900297. [DOI] [PubMed] [Google Scholar]
- 32.Hayashi H, Matsuoka Y, Sakamoto I, Sueyoshi E, Okimoto T, Hayashi K, et al. Penetrating atherosclerotic ulcer of the aorta: imaging features and disease concept. Radiographics. 2000;20:995–1005. doi: 10.1148/radiographics.20.4.g00jl01995. [DOI] [PubMed] [Google Scholar]
- 33.Quint LE, Williams DM, Francis IR, Monaghan HM, Sonnad SS, Patel S, et al. Ulcerlike lesions of the aorta: imaging features and natural history. Radiology. 2001;218:719–723. doi: 10.1148/radiology.218.3.r01mr24719. [DOI] [PubMed] [Google Scholar]
- 34.Toda R, Moriyama Y, Iguro Y, Matsumoto H, Masuda H, Ueno T. Penetrating atherosclerotic ulcer. Surg Today. 2001;31:32–35. doi: 10.1007/s005950170216. [DOI] [PubMed] [Google Scholar]
- 35.Farooq MM, Kling K, Yamini D, Gelabert HA, Baker JD, Freischlag JA. Penetrating ulceration of the infrarenal aorta: case reports of an embolic and an asymptomatic lesion. Ann Vasc Surg. 2001;15:255–259. doi: 10.1007/s100160010062. [DOI] [PubMed] [Google Scholar]
- 36.Vasquez J, Poultsides GA, Lorenzo AC, Foster JE, Drezner AD, Gallagher J. Endovascular stent-graft placement for nonaneurysmal infrarenal aortic rupture: a case report and review of the literature. J Vasc Surg. 2003;38:836–839. doi: 10.1016/S0741-5214(03)00557-3. [DOI] [PubMed] [Google Scholar]
- 37.Saiki M, Nishimura K, Ikebuchi M, Hiroe T, Tachibana M, Kanaoka Y, et al. Mycotic abdominal aortic pseudoaneurysm caused by a penetrating atherosclerotic ulcer: report of a case. Surg Today. 2003;33:698–701. doi: 10.1007/s00595-003-2560-0. [DOI] [PubMed] [Google Scholar]
- 38.Feld RS, Sullivan E, Morrison P. Thrombin injection for failed stent graft repair of perforated atherosclerotic aortic ulcer. J Vasc Surg. 2003;37:194–197. doi: 10.1067/mva.2003.19. [DOI] [PubMed] [Google Scholar]
- 39.Minor ME, Menzoian JO, Raffetto JD. Noninfectious saccular abdominal aortic aneurysm--a report of two cases. Vasc Endovascular Surg. 2003;37:353–358. doi: 10.1177/153857440303700507. [DOI] [PubMed] [Google Scholar]
- 40.Ventura M, Mastromarino A, Cucciolillo L, Calvisi G, Spartera C. Abdominal aortic intramural hematoma related to penetrating ulcer: an inappropriate indication for endovascular repair? J Endovasc Ther. 2003;10:392–396. doi: 10.1177/152660280301000237. [DOI] [PubMed] [Google Scholar]
- 41.Takagi H, Mori Y, Fukumoto Y, Umeda Y, Nachi S, Hirose H. Progressive acute abdominal aortic syndrome. EJVES Extra. 2004;7:11–12. doi: 10.1016/S1533-3167(03)00108-0. [DOI] [Google Scholar]
- 42.Chernenkov V, Tonev A, Maximov D, Nikolov D, Stoinova V. Spontaneous rupture of a nonaneurysmal infrarenal abdominal aorta due to penetrating ulcer. EJVES Extra. 2005;10:101–103. doi: 10.1016/j.ejvsextra.2005.04.007. [DOI] [Google Scholar]
- 43.Taniguchi I, Morimoto K, Miyasaka S, Marumoto A, Aoki T. Penetrating atherosclerotic ulcer in the juxtarenal abdominal aorta and coronary artery disease: emergency one-stage repair with off-pump coronary surgery. Jpn J Thorac Cardiovasc Surg. 2005;53:505–509. doi: 10.1007/s11748-005-0097-4. [DOI] [PubMed] [Google Scholar]
- 44.Sensi L, Pisano E, Magnoni F, Pilato A, Pedrini L. Endovascular and surgical repair for penetrating ulcers of the abdominal aorta. Ital J Vasc Endovasc Surg. 2006;13:87–93. [Google Scholar]
- 45.Eggebrecht H, Herold U, Schmermund A, Lind AY, Kuhnt O, Martini S, et al. Endovascular stent-graft treatment of penetrating aortic ulcer: results over a median follow-up of 27 months. Am Heart J. 2006;151:530–536. doi: 10.1016/j.ahj.2005.05.020. [DOI] [PubMed] [Google Scholar]
- 46.Thalheimer A, Larena-Avellaneda A, Buhler C, Meyer D, Franke S. Spontaneous perforation of a nonaneurysmal infrarenal aorta. Ann Vasc Surg. 2007;21:79–83. doi: 10.1016/j.avsg.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 47.Dalainas I, Nano G, Medda M, Bianchi P, Casana R, Ramponi F, et al. Endovascular treatment of penetrating aortic ulcers: mid-term results. Eur J Vasc Endovasc Surg. 2007;34:74–78. doi: 10.1016/j.ejvs.2007.02.025. [DOI] [PubMed] [Google Scholar]
- 48.Piffaretti G, Tozzi M, Lomazzi C, Rivolta N, Caronno R, Castelli P. Endovascular repair of abdominal infrarenal penetrating aortic ulcers: a prospective observational study. Int J Surg. 2007;5:172–175. doi: 10.1016/j.ijsu.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 49.Fyntanidou B, Massa E, Papachristodoulou A, Karatziou C, Karatziou H, Megalopoulos A, et al. Endovascular repair of infrarenal abdominal aorta penetrating atherosclerotic ulcers: review of our experience. EJVES Extra. 2008;16:4–9. doi: 10.1016/j.ejvsextra.2008.07.002. [DOI] [Google Scholar]
- 50.Lindblad B, Holst J, Kölbel T, Ivancev K. What to do when evidence is lacking--implications on treatment of aortic ulcers, pseudoaneurysms and aorto-enteric fistulae. Scand J Surg. 2008;97:165–173. doi: 10.1177/145749690809700220. [DOI] [PubMed] [Google Scholar]
- 51.Afifi R, Salamon T, Manhaim D, Kvasha V, Karmeli R. Endovascular repair of ruptured aortic penetrating ulcer via carotid artery. Ann Vasc Surg. 2009;23:536.e1–e3. doi: 10.1016/j.avsg.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 52.Hyhlik-Dürr A, Geisbüsch P, Kotelis D, Böckler D. Endovascular repair of infrarenal penetrating aortic ulcers: a single-center experience in 20 patients. J Endovasc Ther. 2010;17:510–514. doi: 10.1583/10-3063.1. [DOI] [PubMed] [Google Scholar]
- 53.Kutsukata N, Mashiko K, Matsumoto H, Sakamoto Y. A case of spontaneous rupture of nonaneurysmal left iliac artery due to penetrating atherosclerotic ulcer. J Nippon Med Sch. 2010;77:123–125. doi: 10.1272/jnms.77.123. [DOI] [PubMed] [Google Scholar]
- 54.Ferro C, Rossi UG, Petrocelli F, Seitun S, Robaldo A, Mazzei R. Penetrating atherosclerotic ulcer of the abdominal aorta involving the celiac trunk origin and superior mesenteric artery occlusion: endovascular treatment. Cardiovasc Intervent Radiol. 2011;34(Suppl 2):S40–S43. doi: 10.1007/s00270-010-0041-6. [DOI] [PubMed] [Google Scholar]
- 55.Kainuma S, Kuratani T, Kin K, Sawa Y. Endovascular aortic repair for spontaneous rupture of a non-aneurysmal infrarenal aorta. Interact Cardiovasc Thorac Surg. 2011;13:526–528. doi: 10.1510/icvts.2011.280198. [DOI] [PubMed] [Google Scholar]
- 56.Nathan DP, Boonn W, Lai E, Wang GJ, Desai N, Woo EY, et al. Presentation, complications, and natural history of penetrating atherosclerotic ulcer disease. J Vasc Surg. 2012;55:10–15. doi: 10.1016/j.jvs.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 57.Sadeghi-Azandaryani M, Strube H, Heyn J, Steckmeier B, Reiser MF, Treitl M. Penetrating aortic ulcer in the infrarenal stent-graft landing zone: treatment with coils and the ethylene vinyl alcohol copolymer onyx. J Endovasc Ther. 2011;18:123–129. doi: 10.1583/10-3226MR.1. [DOI] [PubMed] [Google Scholar]
- 58.Kazan V, Jamil T, Beyrouti R, Nazzal M. Penetrating abdominal aortic ulcers: case reports and review of the literature. Vascular. 2011;19:346–350. doi: 10.1258/vasc.2011.cr0278. [DOI] [PubMed] [Google Scholar]
- 59.Palombo D, Lucertini G, Robaldo A, Pane B, Spinella G. Treatment of penetrating aortic ulcer by endoprosthesis: a single center experience. Int Angiol. 2012;31:54–61. [PubMed] [Google Scholar]
- 60.Papazoglou KO, Karkos CD, Giagtzidis IT, Kalogirou TE, Eliescu A. Spontaneous rupture of the visceral abdominal aorta: endovascular management using the periscope graft technique. J Endovasc Ther. 2012;19:558–562. doi: 10.1583/12-3912R.1. [DOI] [PubMed] [Google Scholar]
- 61.Georgiadis GS, Trellopoulos G, Antoniou GA, Georgakarakos EI, Nikolopoulos ES, Pelekas D, et al. Endovascular therapy for penetrating ulcers of the infrarenal aorta. ANZ J Surg. 2013;83:758–763. doi: 10.1111/ans.12074. [DOI] [PubMed] [Google Scholar]