Abstract
Stress experienced by either partner in a couple can have a negative impact on each partner’s health, but most dyadic research on stress and health focuses on different-sex couples. We examined relationship functioning as a mechanism underlying the longitudinal actor and partner effects of stress on depression and substance use problems among 109 young male same-sex couples. There were significant indirect actor effects of internalized stigma and microaggressions on depression and alcohol use problems through negative relationship interactions. Participants who reported higher levels of internalized stigma and microaggressions reported more negative relationship interactions, which in turn was associated with reporting greater depression and alcohol use problems. In contrast, none of the indirect partner effects were significant. Findings implicate negative relationship interactions as a mechanism linking minority stress to health, but raise questions about the influence of partner stress on individual health among young male same-sex couples.
Keywords: same-sex couples, dyadic, stress, depression, substance use
Gay and bisexual men are at increased risk for negative mental health outcomes such as depression and problematic substance use (Bostwick, Boyd, Hughes, & McCabe, 2010; Marshal et al., 2011; Marshal et al., 2008; McCabe, Hughes, Bostwick, West, & Boyd, 2009). For example, in a nationally representative sample, 36–38% of gay and bisexual men met criteria for lifetime major depression compared to 15% of heterosexual men (Bostwick et al., 2010) and 17–20% of gay and bisexual men met criteria for past-year alcohol dependence compared to 6% of heterosexual men (McCabe et al., 2009). Sexual minorities also experience unique stressors related to their sexual orientation (Meyer, 2003), which have been identified as risk factors for depression and substance use (Bostwick, Boyd, Hughes, West, & McCabe, 2014; Goldbach, Tanner-Smith, Bagwell, & Dunlap, 2013; Mustanski, Andrews, & Puckett, 2016). However, research on minority stress and health has typically focused on sexual minority individuals with limited attention to same-sex couples. This represents a critical gap in our understanding of sexual minority health, given that research on different-sex couples has demonstrated that stress experienced by either partner can have a negative impact on each partner’s health (Randall & Bodenmann, 2009; Story & Bradbury, 2004). As such, examining the associations between stress and health among same-sex couples can advance our understanding of these processes and inform interventions.
Numerous studies have demonstrated that discrimination and victimization are associated with depression (Feinstein, Goldfried, & Davila, 2012; Mays & Cochran, 2001; Mustanski et al., 2016; Ngamake, Walch, & Raveepatarakul, 2016; Swann, Minshew, Newcomb, & Mustanski, 2016) and substance use among sexual minority individuals (Bontempo & D’ Augelli, 2002; Darwich, Hymel, & Waterhouse, 2012; Espelage, Aragon, Birkett, & Koenig, 2008; Goldbach et al., 2013; Phillips et al., 2017; Wong, Weiss, Ayala, & Kipke, 2010). Research has also demonstrated that the internalization of negative attitudes toward sexual minorities is associated with depression (see Newcomb & Mustanski, 2010), but findings have been mixed for substance use (see Brubaker, Garrett, & Dew, 2009). Although numerous studies have examined minority stress as a risk factor for depression and substance use, few have done so among same-sex couples. Relationship scholars have proposed that stress experienced by either partner can have a negative impact on each partner’s health (Randall & Bodenmann, 2009; Story & Bradbury, 2004) and research has demonstrated that individual and partner stress can both influence one’s own depression among different-sex couples (Falconier, Nussbeck, Bodenmann, Schneider, & Bradbury, 2015; Howe, Levy, & Caplan, 2004; Rayens & Reed, 2014; Rook, Dooley, & Catalano, 1991). Research has also demonstrated that relationship distress and alcohol use problems are interdependent and can exacerbate each other (Levitt & Cooper, 2010; Rodriguez, Neighbors, & Knee, 2014) and that individual and partner stress can both influence one’s own problem drinking among different-sex couples (Falconier, Huerta, & Hendrickson, 2016).
Given that same-sex couples experience unique stressors, there is additional potential for partner stress to impact one’s own health. LeBlanc, Frost, and Wight (2015) proposed a conceptual model to describe how stress can influence health and relationship functioning among same-sex couples, noting the lack of dyadic research in this population. In an exception, Frost and Fingerhut (2016) found that individual exposure to negative same-sex marriage campaign messages was associated with negative affect and relationship dissatisfaction among same-sex couples, but partner exposure was not associated with one’s own affect or satisfaction. Additionally, Randall and colleagues found that workplace minority stress was associated with anxiety among female same-sex couples, but only for those who reported low partner supportive dyadic coping (i.e., the perception of their partner as helping to reduce their own stress) (Randall, Totenhagen, Walsh, Adams, & Tao, 2017). However, although they used dyadic data, they did not test partner effects. These findings raise questions about the extent to which partner stress influences one’s own health among same-sex couples, highlighting the need for additional research.
Even less attention has been paid to the mechanisms underlying these associations. Given that stress has a negative impact on relationship functioning (Randall & Bodenmann, 2009; Story & Bradbury, 2004) and health (Hammen, 2005; Howe et al., 2004) and that relationship functioning is also associated with health (Proulx, Helms, & Buehler, 2007; Whisman, 2007, 2013), stress may influence health among couples by compromising relationship functioning. Howe et al. (2004) described this as the relationship disruption model, proposing that stress can increase relationship conflict and decrease relationship quality, in turn contributing to couples’ distress. LeBlanc et al. (2015) also suggested that minority stress can influence relational stress (e.g., dissatisfaction, conflict), which in turn can compromise partners’ health. Consistent with this, a meta-analysis found that minority stress was associated with lower relationship well-being among sexual minorities (Cao et al., 2017) and there is some evidence that partner minority stress is associated with worse relationship functioning among same-sex couples (Mohr & Fassinger, 2006; Otis, Rostosky, Riggle, & Hamrin, 2006).
Our own recent work (blinded) has also found that individual stress is associated with worse relationship functioning among young male same-sex couples, especially for those in longer relationships, and that having a partner with higher internalized stigma is associated with more negative relationship interactions (e.g., conflict, negative communication). As such, relationship functioning may be a mechanism through which stress influences health among young male same-sex couples. The goals of the current study were to extend our prior work with this sample to examine relationship functioning as a mechanism underlying the longitudinal actor and partner effects of stress on health among young male same-sex couples. We examined multiple types of stress (general stress, internalized stigma, microaggressions, victimization, and outness), several health outcomes (depression, alcohol use problems, and marijuana use problems), and two aspects of relationship functioning (relationship quality and negative relationship interactions). We hypothesized that there would be significant indirect actor and partner effects of stress on depression and substance use problems through relationship quality and negative relationship interactions.
Method
Participants and Procedures
The current analyses used data from an ongoing longitudinal cohort study of multilevel influences on HIV and substance use among young gay, bisexual, and other men who have sex with men (MSM). Data collection began in February 2015 and the current analyses used data through August 2018. To achieve a multiple cohort, accelerated longitudinal design (Duncan, Duncan, & Hops, 1996), young MSM who had participated in one of two previous cohort studies were contacted and invited to join the current study and a new cohort of young MSM was recruited as well. As in the prior cohorts, the new cohort was recruited using various methods such as venue-based recruitment (e.g., community-based organizations that serve LGBT individuals), social media (e.g., Facebook), and snowball sampling. All cohort members were required to meet the following criteria: 16–29 years old, assigned male at birth, English-speaking, and reported a sexual minority identity (e.g., gay, bisexual) or sex with a man in the past year. Cohort members were allowed to recruit their serious partners at each visit; those who met the eligibility criteria were invited to join the cohort, while those who did not (e.g., partners who were assigned female at birth or older than 29) were invited to participate in a one-time visit.
We used data from each couple’s first, second, and third visits for the current longitudinal analyses. Given that cohort members invited their partners to participate, there was a period of time in between most partners’ assessments (Mdn. = 5.5 days). The sample started with 313 dyads, but 204 dyads were excluded because: dyadic data was only available for one visit (130 dyads); partners came from a three-person relationship (3 dyads); one partner was present in two different dyads at two different visits (i.e., they entered a new relationship), in which case we only included data from their first dyad (6 dyads); one partner was a cisgender woman (22 dyads); and partners did not agree that their relationship was serious (43 dyads). The final analytic sample included 109 dyads (218 individuals) who had data from at least two visits (with 66 dyads who had data from three visits), which resulted in a total of 568 observations across all participants and assessments.
Participants in the analytic sample ranged in age from 16–50 (M = 22.85, SD = 4.01). Most participants were cisgender men, but 11 dyads included a transgender partner. The racial/ethnic composition of the sample was 33.0% Black, 30.7% Latino, 27.5% White, and 8.7% other. Of note, the high proportions of Black and Latino participants is consistent with the overall racial/ethnic distribution of the city in which the study was conducted (U.S. Census Bureau, 2017). Most participants identified as gay (79.4%), followed by bisexual (15.1%) and other (5.5%). Highest level of education included less than high school (8.7%), high school (25.7%), some college (48.2%), college (12.4%), and graduate school (5.0%). Most participants (79.7%) were HIV-negative based on testing at the couple’s first study visit. Most couples were concordant HIV-negative (74.3%) and the rest were concordant HIV-positive (9.2%) or discordant (16.5%). Relationship length ranged from less than one month to 10.16 years (M = 1.27 years, SD = 1.51 years); 31.2% of participants lived with their partner.
As part of the ongoing longitudinal study, participants completed a psychosocial survey, a network interview, and biomedical specimen collection. Most measures were administered to the entire sample, but some were added later in the data collection process or only administered at some visits. As such, the analytic sample size varied for some analyses (described below). Participants were compensated $50 per visit. All procedures were approved by the Institutional Review Board. Following emerging open science guidelines (Schönbrodt, Maier, Heene, & Zehetleitner, 2015), we have made the data and syntax associated with this article publicly available (https://doi.org/10.21985/N2VR0V).
Measures
Demographics.
Participants reported their age, race/ethnicity, sexual orientation, highest level of education, living situation, and relationship length. Partners’ reports of relationship length were highly correlated (r = .85, p < .001), so we used their mean.
General stress.
The 10-item version of the Perceived Stress Scale (Roberti, Harrington, & Storch, 2006) was used to assess general stress. Participants were asked, “In the past month, how often have you [item]?” Example items included: “Felt difficulties were piling up so high that you could not overcome them” and “Felt that you were unable to control the important things in your life.” Items were rated on a 5-point scale (0 = never, 4 = very often) and summed. Scores could range from 0 to 40 (α = .78 in the analytic sample). Roberti et al. (2006) provided evidence of internal consistency (α = .89) and validity (e.g., a significant association with anxiety).
Internalized stigma.
A measure adapted from the Homosexual Attitudes Inventory (Nungesser, 1983) and the Internalized Homosexual Stigma Scale (Ramirez-Valles, Kuhns, Campbell, & Diaz, 2010) was used to assess internalized stigma. Puckett et al. (2017) identified three factors: desire to be heterosexual, fear of coming out, and fear of stereotypical perception; as recommended, the 8-item “desire to be heterosexual” factor was used to assess internalized stigma. Participants were asked how much they agreed with statements such as, “Sometimes I wish I were not gay.” Items were rated on a 4-point scale (1 = strongly disagree, 4 = strongly agree) and averaged. Scores could range from 1 to 4 (α = .89 in the analytic sample). Puckett et al. (2017) provided evidence of internal consistency (α = .88-.90 across time points) and validity (e.g., significant associations with fear of coming out and fear of stereotypical perception). We had data on this variable for 475 out of 568 observations (83.6% of the total number of observations) because it was not administered at every visit; of these, data were missing for two additional observations.
Microaggressions.
The six-item “anti-gay attitudes and expressions” subscale of the Sexual Orientation Microaggression Inventory (Swann et al., 2016) was used to assess microaggressions. Participants were asked, “In the past 6 months, how often have you had the following experiences?” Example items included: “You heard someone say ‘that’s so gay’ in a negative way” and “Someone expressed a stereotype (e.g., ‘Gay men are so good at fashion’).” Items were rated on a 5-point scale (1 = not at all, 5 = about every day) and averaged. Scores could range from 1 to 5 (α = .86 in the analytic sample). Swann et al. (2016) provided support for a bi-factor model (i.e., a general factor and four specific factors), including reliability and validity (e.g., a significant association with victimization). Data was missing on this variable for one observation.
Victimization.
Six items were selected from a 10-item measure of victimization (Mustanski et al., 2016). Participants were asked, “In the past six months, how many times [item] because you are or were thought to be gay, bisexual, or transgender?” Items included: (1) have you been threatened with physical violence; (2) have you had an object thrown at you; (3) have you been punched, kicked, or beaten; (4) have you been threatened with a knife, gun, or another weapon; (5) has someone chased or followed you; and (6) has your property been damaged. Items were rated on a 4-point scale (0 = never, 3 = three times or more) and averaged. Scores could range from 0 to 3 (α = .86 in the analytic sample). Mustanski et al. (2016) provided evidence of internal consistency (α > .76 across time points) and validity (e.g., significant associations with major depressive disorder and posttraumatic stress disorder). Data was missing on this variable for one observation.
Outness.
Participants were asked, “How out are you to people around you?” Response options included: 0 (not out to anyone), 1 (only out to a few select people), 2 (out to most people), and 3 (out to everyone). We had data on this variable for 474 out of 568 observations (83.4% of the total number of observations) because it was not administered at every visit; of these, data were missing for three additional observations.
Depression.
The 8-item PROMIS Depression Short Form 8a (Choi, Schalet, Cook, & Cella, 2014; Pilkonis et al., 2011) was used to assess depression symptoms in the past week. The items focus on the emotional and cognitive manifestations of depression (e.g., sadness, worthlessness) rather than somatic symptoms (e.g., changes in appetite and sleep). Items were rated on a 5-point scale (1 = never, 5 = always) and summed. Scores could range from 8 to 40 (α = .94 in the analytic sample). Pilkonis et al. (2011) provided evidence of internal consistency (α = .95) and validity (e.g., a significant association with another measure of depression).
Alcohol use problems.
The Alcohol Use Disorders Identification Test (AUDIT) (Saunders, Aasland, Babor, de la Fuente, & Grant, 1993) was used to assess alcohol use problems in the past six months. The AUDIT includes 10 items that are rated on different scales. For example, the item, “How often do you have a drink containing alcohol?” was rated on a 5-point scale (1 = never, 5 = 4 or more times a week), and the item, “How often do you have six or more drinks on one occasion?” was rated on a different 5-point scale (0 = never, 4 = daily or almost daily). Responses were summed and could range from 0 to 40 (α = .82 in the analytic sample). Hays, Merz, and Nicholas (1995) provided evidence of internal consistency (α = .83) and validity (e.g., significant associations with other measures of alcohol use problems). Scores of 0–7 reflect low-risk drinking or abstinence, 8–15 reflect alcohol use in excess of low-risk guidelines, 16–19 reflect harmful and hazardous drinking, and 20 or greater reflect possible alcohol dependence (Babor, Higgins-Biddle, Saunders, & Monteiro, 2001).
Marijuana use problems.
The Cannabis Use Disorders Identification Test – Revised (CUDIT-R) (Adamson et al., 2010) was used to assess marijuana misuse and problems in the past six months. The CUDIT-R includes eight items that are rated on different scales. For example, the item, “How often do you use marijuana?” was rated on a 5-point scale (1 = never, 5 = 4 or more times a week), and the item, “Have you ever thought about cutting down, or stopping, your use of marijuana?” was rated on a 3-point scale (1 = never, 2 = yes, but not in the past 6 months, 3 = yes, during the past 6 months). Responses were summed and could range from 0 to 32 (α = .75). Adamson et al. (2010) provided evidence of internal consistency (α = .91) and validity (e.g., a significant association with recent marijuana use frequency). Scores of 13 or greater reflect problematic use (Adamson et al., 2010). Data was missing on this variable for one observation.
Relationship functioning.
As described in (blinded), relationship functioning was modeled as two correlated latent variables. This measurement model fit the data well and the standardized factor loadings were high. We used the same measurement model to represent the mediators in the current analyses. The first latent variable—relationship quality—was indicated by three items used to assess satisfaction, trust, and commitment (Hendrick, 1988). Data were missing on all three items for two observations. The second latent variable—negative relationship interactions—was indicated by the 2-item conflict subscale of the Revised Dyadic Adjustment Scale (Busby, Christensen, Crane, & Larson, 1995) and the 8-item negative communication subscale of the Communication Skills Test (Buzzella, Whitton, & Tompson, 2012; Jenkins & Saiz, 1995). Busby et al. (1995) provided evidence of the conflict subscale’s internal consistency and the measure’s validity (e.g., a significant correlation with marital adjustment), and Buzzella et al. (2012) provided evidence of the negative communication subscale’s internal consistency (α = .85-.90 across time points) and validity (e.g., a significant correlation with relationship quality). We had data on conflict for 440 out of 568 observations (77.5% of the total number of observations) and we had data on negative communication for 492 out of 568 observations (86.6% of the total number of observations) because they were added later in the data collection process.
Data Analysis
Analyses were conducted in Mplus Version 8 using robust maximum likelihood estimation. Multilevel modeling was used to account for the non-independence of dyadic data. Missing data were handled using full information maximum likelihood, which uses all available data, produces more accurate parameter estimates than listwise/pairwise deletion and mean substitution, and yields relatively unbiased parameters with moderate amounts of missing data (Enders & Bandalos, 2001; Schlomer, Bauman, & Card, 2010). First, the data were restructured such that each of the lagged observations included data for the stressor, the health outcome, and the mediators at time t-1 as well as the health outcome and the mediators at time t. This resulted in a total of 436 lagged observations from 109 dyads. Depending on the amount of missing data on the stress variable, the analytic sample ranged from 322–436 observations from 102–109 dyads. To reduce the risk of Type I error, the Benjamini-Hochberg procedure was used to correct p values for all analyses (Benjamini & Hochberg, 1995).
Second, we used multilevel structural equation modeling to test a series of lagged direct effect Actor-Partner Interdependence Models (i.e., without mediators) (Kenny, Kashy, & Cook, 2006). Each lagged direct effect model tested the actor and partner effects of one stressor (at time t-1) on one health outcome (at time t). Each lagged direct effect model controlled for relationship length and the health outcome at time t-1. Dyad members were treated as indistinguishable; a single actor effect (i.e., the actor’s outcome regressed on the actor’s predictor) and a single partner effect (i.e., the actor’s outcome regressed on the partner’s predictor) were estimated for each pair of predictors and outcomes.
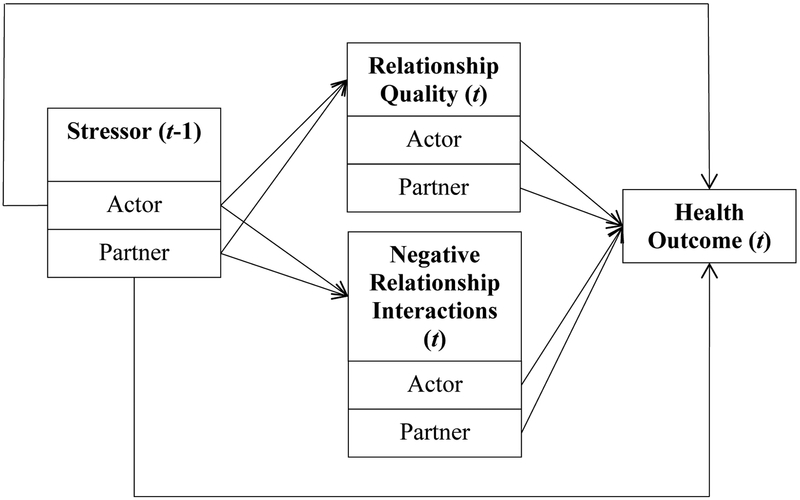
Third, we used the same approach to test a series of lagged indirect effect Actor-Partner Interdependence Models (i.e., with mediators). Each lagged indirect effect model tested the extent to which there were indirect effects of one stressor (at time t-1) on one health outcome (at time t) through relationship quality and negative relationship interactions (at time t). Each lagged indirect effect model controlled for relationship length as well as relationship quality, negative relationship interactions, and the health outcome at time t-1. Actor and partner effects were estimated for the associations between the stressor and the health outcome, the stressor and each of the two mediators, and each of the two mediators and the health outcome. As such, each indirect effect model tested eight indirect effects. Figure 1 depicts a conceptual representation of the model. Consistent with previous tests of longitudinal mediation using dyadic data (e.g., Manne, Badr, & Kashy, 20120), we used a one-wave lag (i.e., we modeled the predictor at time t-1, the mediators at time t, and the outcome at time t, controlling for the mediators and the outcome at time t-1). This approach enabled us to utilize longitudinal data from all of the dyads in our sample who had at least two visits, including the 60.5% who had data from three visits.
Figure 1.
Conceptual depiction of the longitudinal Actor-Partner Interdependence Models used to test the indirect effects. Dyad members were treated as indistinguishable. Each model tested the indirect actor and partner effects of one stressor on one health outcome through relationship quality and negative relationship interactions. Of note, each model controlled for relationship length, the actor and partner levels of relationship quality and negative relationship interactions at the previous time point (time t-1), and the actor level of the health outcome at the previous time point (time t-1). t and t-1 refer to the time point at which the variables were measured, with t-1 referring to the time point before time t.
The significance of the indirect effects was tested using the Monte Carlo Method for Assessing Mediation (MacKinnon, Lockwood, & Williams, 2004), which is similar to the parametric bootstrap approach (Efron & Tibshirani, 1986) and can be used with multilevel models (Bauer, Preacher, & Gil, 2006). Parameter estimates and standard errors are used to simulate random draws from the distributions for the paths included in the indirect effect (i.e., the path from the predictor to the mediator and the path from the mediator to the outcome) and the product of these values is computed. This was repeated 20,000 times and the resulting distribution was used to estimate 95% confidence intervals. Confidence intervals that do not include zero are significant at an alpha-level of .05.
Finally, we conducted sensitivity analyses to examine whether our results were affected by couples with a transgender partner (n = 11) or a partner older than 29 (n = 9). The pattern of results remained the same; all of the significant effects remained significant.
Results
Means, standard deviations, individual-level bivariate correlations, and intraclass correlations are presented in Table 1. Individual-level bivariate correlations indicated that general stress was associated with all three health outcomes. Additionally, internalized stigma was associated with depression and alcohol use problems, microaggressions were associated with depression and marijuana use problems, and victimization was associated with marijuana use problems. In contrast, outness was not associated with any health outcomes. Lower relationship quality was also associated with depression and marijuana use problems, and negative relationship interactions were associated with all three health outcomes.
Table 1.
Means, Standard Deviations, Intraclass Correlations, and Individual-Level Bivariate Correlations
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 11 | 12 | 13 |
|---|---|---|---|---|---|---|---|---|---|---|
| Stressors | ||||||||||
| 1. General Stress | - | |||||||||
| 2. Internalized stigma | .31** | - | ||||||||
| 3. Microaggressions | .20** | .30** | - | |||||||
| 4. Victimization | .12* | 22** | .26** | - | ||||||
| 5. Outness | −.09 | −.29** | −.11 | −.11 | - | |||||
| Relationship Functioning | ||||||||||
| 6. Relationship Quality | −.29** | −.35** | −.20** | .01 | .12 | - | ||||
| 7. Negative Relationship Interactions | .26** | .30** | .38** | .11 | −.06 | −.64** | - | |||
| Mental Health | ||||||||||
| 8. Depression | .41** | .19* | 23** | .09 | .01 | −.41** | .48** | - | ||
| 9. Alcohol use problems | .20** | .08 | .16** | .16 | .02 | −.06 | .22** | .28** | - | |
| 10. Marijuana use problems | .15** | .18** | .10 | .23** | −.05 | −.13* | .17* | .12 | .18** | - |
| M | 16.08 | 1.57 | 1.95 | .52 | 2.49 | .00 | .00 | 13.85 | 5.14 | 6.54 |
| SD | 2.87 | .38 | .32 | .42 | .32 | .76 | .98 | 3.71 | 2.80 | 4.44 |
| Range | 0–40 | 1–4 | 1–5 | 0–3 | 0–3 | - | - | 8–40 | 0–40 | 0–32 |
| ICC | .22 | .19 | .39 | .14 | .19 | .27 | .58 | .31 | .36 | .49 |
Note. ICC = intraclass correlation.
p < .05;
p < .01.
None of the actor or partner effects in the lagged direct effect models were significant; these non-significant results are not reported. However, significant indirect effects can occur in the absence of significant direct effects (Kenny & Judd, 2014; Rucker, Preacher, Tormala, & Petty, 2011). As such, consistent with recommendations (Rucker et al., 2011), we continued to test lagged indirect effect models. Unstandardized path coefficients for the lagged indirect effect models are presented in Table 2 and estimates of indirect effects and 95% confidence intervals for the significant indirect effects are presented in-text.
Table 2.
Path Coefficients for Indirect Effects Models of Stressors on Outcome (Depression/AUDIT/CUDIT) Via Relationship Functioning
| Depression | AUDIT | CUDIT | |||||
|---|---|---|---|---|---|---|---|
| Model | Association | Actor | Partner | Actor | Partner | Actor | Partner |
| General Stress | General Stress → RQ | −.01 (.01) | −.01 (.01) | −.01 (.01) | −.01 (.01) | −.01 (.01) | −.01 (.01) |
| General Stress → NRI | .01 (.01) | −.01 (.01) | .01 (.01) | −.01 (.01) | .01 (.01) | −.002 (.01) | |
| RQ → Outcome | −.53 (.84) | −.11 (.88) | .47 (.38) | −.14 (.55) | .15 (.87) | −.19 (.84) | |
| NRI → Outcome | 2.99 (.86)** | −.67 (.73) | .93 (.40)* | −.08 (.48) | .38 (.76) | .34 (.68) | |
| General Stress → Outcome | .18 (.07)* | .01 (.06) | .01 (.04) | −.03 (.03) | .07 (.05) | −.05 (.05) | |
| Internalized Stigma | Internalized Stigma → RQ | −.18 (.07)** | −.04 (.07) | −.18 (.07)** | −.04 (.07) | −.18 (.07)** | −.04 (.07) |
| Internalized Stigma → NRI | .29 (.09)** | −.17 (.09) | .29 (.09)** | −.17 (.09) | .28 (.09)** | −.17 (.09) | |
| RQ → Outcome | −.91 (.82) | .11 (.81) | .15 (.57) | .10 (.57) | −.84 (.86) | −.38 (.84) | |
| NRI → Outcome | 1.92 (.71)** | −.22 (.70) | 1.12 (.47)* | .03 (.48) | .10 (.71) | .63 (.69) | |
| Internalized Stigma → Outcome | .11 (.63) | −1.02 (.61) | −.24 (.43) | −.18 (.43) | .56 (.63) | −.91 (.63) | |
| Microaggressions | Microaggressions → RQ | −.06 (.04) | .01 (.04) | −.06 (.04) | .01 (.04) | −.05 (.04) | .01 (.04) |
| Microaggressions → NRI | .30 (.08)** | −.07 (.07) | .30 (.08)** | −.07 (.07) | .30 (.08)** | −.07 (.07) | |
| RQ → Outcome | −.65 (.86) | −.30 (.83) | .45 (.38) | −.10 (.52) | .08 (.85) | −.13 (.82) | |
| NRI → Outcome | 2.95 (.86)** | −.66 (.73) | .86 (.40)** | −.06 (.45) | .48 (.78) | .22 (.68) | |
| Microaggressions → Outcome | −.28 (.46) | .12 (.44) | .21 (.31) | −.07 (.22) | −.04 (.45) | .06 (.37) | |
| Victimization | Victimization → RQ | .05 (.03) | .02 (.03) | .04 (.03) | .02 (.03) | .04 (.03) | .02 (.03) |
| Victimization → NRI | .01 (.05) | −.01 (.04) | .01 (.05) | −.02 (.04) | .01 (.05) | −.01 (.04) | |
| RQ → Outcome | −.73 (.83) | −.40 (.86) | .47 (.39) | −.07 (.51) | −.06 (.82) | −.27 (.79) | |
| NRI → Outcome | 2.86 (.82)** | −.74 (.73) | .98 (.42)* | −.11 (.46) | .40 (.75) | .12 (.62) | |
| Victimization → Outcome | .10 (.26) | .26 (.31) | −.04 (.26) | −.08 (.20) | .66 (.33) | .27 (.23) | |
| Outness | Outness → RQ | .12 (.05)* | .001 (.04) | .12 (.05)* | .001 (.04) | .12 (.05)** | .001 (.04) |
| Outness → NRI | −.10 (.07) | −.03 (.08) | −.10 (.07) | −.03 (.08) | −.10 (.07) | −.04 (.08) | |
| RQ → Outcome | −1.00 (.97) | .07 (1.00) | −.04 (.46) | −.03 (.62) | −.77 (.99) | −.26 (.88) | |
| NRI → Outcome | 1.99 (.87)* | −.43 (.91) | 1.07 (.55) | −.01 (.60) | .40 (.90) | .44 (.72) | |
| Outness → Outcome | .23 (.46) | .58 (.48) | .13 (.36) | .24 (.34) | −.19 (.48) | .11 (.45) | |
RQ = relationship quality; NRI = negative relationship interactions. Coefficients presented are unstandardized regression coefficients (and standard errors).
There were significant indirect effects of actor-reported internalized stigma on actor-reported depression (estimate = .56; 95% CI [.10, 1.19]) and alcohol use problems (estimate = .32; 95% CI [.04, .72]) through actor-reported negative relationship interactions. Participants who reported more internalized stigma reported increases in negative relationship interactions, which in turn were associated with reporting greater depression and alcohol use problems. There were also significant indirect effects of actor-reported microaggressions on actor-reported depression (estimate = .89; 95% CI [.32, 1.59]) and alcohol use problems (estimate = .26; 95% CI [.03, .53] through actor-reported negative relationship interactions. Participants who reported more microaggressions reported increases in negative relationship interactions, which in turn were associated with reporting greater depression and alcohol use problems. In contrast, none of the indirect effects through relationship quality were significant and none of the indirect partner effects were significant. Finally, in the context of the lagged indirect effect models, the direct actor effect of general stress on depression was significant even though the indirect effects through relationship quality and negative relationship interactions were not significant. Participants who reported more general stress reported increases in depression.
Discussion
To address the lack of dyadic research on stress and health among same-sex couples, we examined relationship functioning as a mechanism underlying the longitudinal actor and partner effects of stress on depression and substance use problems among young male same-sex couples. Although none of the actor or partner effects in the lagged direct effect models were significant, four of the indirect actor effects were significant. Specifically, internalized stigma and microaggressions were associated with increases in negative relationship interactions, which in turn were associated with greater depression and alcohol use problems. These findings support theories suggesting that individual stress can influence health by contributing to dyadic processes such as conflict in one’s relationship (Howe et al., 2004; LeBlanc et al., 2015). In contrast, none of the indirect actor effects through relationship quality were significant. Conflict can occur in satisfying and dissatisfying relationships, so it may have a stronger influence on health than relationship quality does. However, lower relationship quality was associated with depression and marijuana use problems in our bivariate analyses. These findings suggest that relationship quality may have an influence on health, but it does not explain the link between stress and health in this population.
Additionally, in the context of the lagged indirect effect models, we also found that one’s own general stress was associated with increases in depression. This finding highlights the importance of considering general stress as a risk factor for negative health outcomes among young male same-sex couples. However, the indirect actor effects of general stress on depression through relationship functioning were not significant, suggesting that general stress influences depression through different pathways. Given that research on sexual minority health rarely accounts for general stress (for an exception, see Rosario, Rotheram-Borus, & Reid, 1996), it will be important for future research to examine other potential mechanisms through which general stress influences depression in this population (e.g., emotional regulation difficulties).
Despite evidence of significant individual-level bivariate correlations between stressors and health outcomes, none of the actor or partner effects in our lagged direct effect models (i.e., without mediators) were significant. This suggests that there were significant associations between higher levels of stressors and higher levels of negative health outcomes at the same time point, but that higher levels of stressors were not associated with increases in negative health outcomes at the subsquent time point (i.e., six-months later). Given that there has been relatively limited longitudinal research on these associtations, it wil be important for future research to continue to examine the extent to which minority stress influences health across different intervals of time.
Of note, it is well described in the literature that significant indirect effects can occur in the absence of significant direct effects for several reasons (e.g., opposing indirect effects can obscure a direct effect; Rucker et al., 2011). Given that our models tested indirect effects of positive and negative aspects of relationship functioning, it is possible that these competing influences suppressed the presence of direct effects. Additionally, simulations studies have demonstrated that power to detect an unmediated effect is lower than power to detect an indirect effect, especailly when the unmediated effect is small (r = .20) and the paths from the predictor to the mediator and from the mediator to the outcome are larger (r = .40) (Rucker et al., 2011; Kenny & Judd, 2013). In this case, 19–44% of unmediated effects may not be significant despite the presence of a significant indirect effect, even with 100–200 participants (Rucker et al., 2011). This suggests that we may not have been able to detect unmediated effects due, at least in part, to reduced statistical power for unmediated effects compared to indirect effects (Rucker et al., 2011; Kenny & Judd, 2013). It will be important for future studies to determine whether the lack of unmediated effects was due to suppression by competing indirect effects or power differenes between unmediated and indirect effects.
We are not aware of any previous studies that have examined partner effects of stress on health among same-sex couples. In a related study, Frost and Fingerhut (2016) found that individual exposure to negative same-sex marriage campaign messages was associated with negative affect and relationship dissatisfaction, but partner exposure was not associated with one’s own affect or satisfaction. Similarly, we did not find support for partner effects of stress on health. Although research on different-sex couples suggests that partner stress can influence one’s own health (Falconier et al., 2015; Howe et al., 2004; Rayens & Reed, 2014; Rook et al., 1991), relatively few studies have tested partner effects in the context of Actor-Partner Interdependence Models. In an exception, McNeil, Fincham, and Beach (2014) did not find partner effects of discrimination on depression among African American couples. In contrast, Rayens and Reed (2014) found a significant partner effect of stress on depression for married men, but not women. Given that their sample was comprised of older married couples, partner stress may not have an impact on one’s own health until later in life when relationships become more interdependent (Arnett, 2007; Laursen & Jensen Campbell, 1999). Consistent with this, a recent study found that partner stress had a negative impact on relationship functioning for adult couples, but not adolescent couples (Breitenstein, Milek, Nussbeck, Davila, & Bodenmann, 2017).
Clinical Implications
These findings have implications for interventions focused on sexual minority individuals and same-sex couples. Given that individual experiences of minority stress influenced health by contributing to relationship conflict, interventions for sexual minorities may be enhanced by addressing both minority stress and relational influences on health. This may be particularly important for younger sexual minorities who may have limited relationship experience and skills. Further, while stigma-related experiences tend to decrease as young sexual minority men get older, the mental health consequences of these experiences persist (Pachankis et al., 2018). As such, addressing them early in development has the potential to reduce their long-term influences on relationship functioning and health. Relationship education programs have been developed to teach same-sex couples relationship skills (e.g., effective communication, conflict resolution) and strategies to cope with their unique stressors (Buzzella et al., 2012; Whitton & Buzzella, 2012; Whitton, Weitbrecht, Kuryluk, & Hutsell, 2016). Relationship education has also been combined with HIV prevention to improve sexual and relationship health among young male same-sex couples (Newcomb et al., 2017). Our findings suggest that improving individual abilities to cope with stress may have downstream effects on reducing relationship conflict and improving health among young male same-sex couples. As such, our findings support the potential benefits of relationship education for this population. Similar to relationship education, interventions for sexual minority individuals (as opposed to same-sex couples) can also address the influence of stress on relationship conflict and health. These interventions can teach individuals how to limit the extent to which stress influences their relationships (e.g., using effective coping strategies rather than taking stress out on one’s partner) as a way to improve individual health.
Limitations
Several limitations should be taken into account when interpreting the current findings. First, although our sample was diverse, it was a non-probability sample and it will be important to replicate our findings in other samples of young male same-sex couples. Second, given that several measures were not administered to the full sample, we may have been underpowered to detect significant effects. However, several of our significant effects included measures that were not administered to the full sample and Monte Carlo simulations indicated that we had adequate power to detect actor and partner effects of small to moderate size and the resulting indirect effects. Third, our analyses were longitudinal, but our mediators and outcomes were measured at the same time point because only a subset of participants had data from three visits. As such, additional longitudinal research is needed to model all of the variables at different time points. Of note, we conceptualized relationship functioning as a predictor of health, but these associations are likely bidirectional. Still, our conceptualization is consistent with evidence that stronger effects are observed when relationship functioning is the predictor and health is the outcome (Braithwaite & Holt-Lunstad, 2017). Fourth, there are numerous potential mechanisms linking stress to health among young male same-sex couples. Our data shed light on one mechanism, but it will be important to examine additional mechanisms. Finally, future research should examine moderators of the associations between stress and health, such as age, race/ethnicity, sexual identity, and cohabitation. This is especially important given that racial/ethnic minority gay and bisexual men can experience stress related to their race/ethnicity as well as their sexual orientation.
Conclusion
The current findings provide evidence that individual experiences of minority stress contribute to depression and alcohol use problems among young male same-sex couples, and that negative relationship interactions function as an underlying mechanism. In contrast, we did not find any support for partner experiences of stress having an influence on one’s own health. As one of the first studies to examine the extent to which stress influences health through relationship functioning among young male same-sex couples, it will be important for future research to continue to examine these associations and their underlying mechanisms. In sum, our findings highlight the importance of considering minority stress and relationship functioning in order to understand the health of young male same-sex couples.
Acknowledgements:
This work was supported by a grant from the National Institute on Drug Abuse (U01DA036939; PI: Mustanski). Brian A. Feinstein’s time was also supported by grants from the National Institute on Drug Abuse (F32DA042708; K08DA045575; PI: Feinstein). The funding agency was not involved in study design, in the collection, analysis, and interpretation of data, in the writing of the report, and in the decision to submit the article for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agency.
References
- Adamson SJ, Kay-Lambkin FJ, Baker AL, Lewin TJ, Thornton L, Kelly BJ, & Sellman JD (2010). An improved brief measure of cannabis misuse: The Cannabis Use Disorders Identification Test-Revised (CUDIT-R). Drug and Alcohol Dependence, 110, 137–143. [DOI] [PubMed] [Google Scholar]
- Arnett JJ (2007). Emerging adulthood: What is it, and what is it good for? Child Development Perspectives, 1, 68–73. [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, & Monteiro MG (2001). The Alcohol Use Disorders Identification Test: Guidelines for use in primary health care. Geneva, Switzerland: World Health Organization. [Google Scholar]
- Bauer DJ, Preacher KJ, & Gil KM (2006). Conceptualizing and testing random indirect effects and moderated mediation in multilevel models: New procedures and recommendations. Psychological Methods, 11, 142–163. [DOI] [PubMed] [Google Scholar]
- Bontempo DE, & D’ Augelli AR (2002). Effects of at-school victimization and sexual orientation on lesbian, gay, or bisexual youths’ health risk behavior. Journal of Adolescent Health, 30, 364–374. [DOI] [PubMed] [Google Scholar]
- Bostwick WB, Boyd CJ, Hughes TL, & McCabe SE (2010). Dimensions of sexual orientation and the prevalence of mood and anxiety disorders in the United States. American Journal of Public Health, 100, 468–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostwick WB, Boyd CJ, Hughes TL, West BT, & McCabe SE (2014). Discrimination and mental health among lesbian, gay, and bisexual adults in the United States. American Journal of Orthopsychiatry, 84, 35–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braithwaite S, & Holt-Lunstad J (2017). Romantic relationships and mental health. Current Opinion in Psychology, 13, 120–125. [DOI] [PubMed] [Google Scholar]
- Breitenstein CJ, Milek A, Nussbeck FW, Davila J, & Bodenmann G (2017). Stress, dyadic coping, and relationship satisfaction in late adolescent couples. Journal of Social and Personal Relationships. doi: 10.1177/0265407517698049 [DOI] [Google Scholar]
- Brubaker MD, Garrett MT, & Dew BJ (2009). Examining the relationship between internalized heterosexism and substance abuse among lesbian, gay, and bisexual individuals: A critical review. Journal of LGBT Issues in Counseling, 3, 62–89. [Google Scholar]
- Busby DM, Christensen CM, Crane DR, & Larson JH (1995). A revision of The Dyadic Adjustment Scale for use with distressed and nondistressed couples: Construct hierarchy and multidimensional scales. Journal of Marital and Family Therapy, 21, 289–308. [Google Scholar]
- Buzzella BA, Whitton SW, & Tompson MC (2012). A preliminary evaluation of a relationship education program for male same-sex couples. Couple and Family Psychology: Research and Practice, 1, 306–322. [Google Scholar]
- Cao H, Zhou N, Fine M, Liang Y, Li J, & Mills-Koonce WR (2017). Sexual minority stress and same-sex relationship well-being: A meta-analysis of research prior to the U.S. nationwide legalization of same-sex marriage. Journal of Marriage and Family. doi: 10.1111/jomf.12415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi SW, Schalet B, Cook KF, & Cella D (2014). Establishing a common metric for depressive symptoms: linking the BDI-II, CES-D, and PHQ-9 to PROMIS depression. Psychological Assessment, 26, 513–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darwich L, Hymel S, & Waterhouse T (2012). School avoidance and substance use among lesbian, gay, bisexual, and questioning youths: The impact of peer victimization and adult support. Journal of Educational Psychology, 104, 381–392. [Google Scholar]
- Duncan SC, Duncan TE, & Hops H (1996). Analysis of longitudinal data within accelerated longitudinal designs. Psychological Methods, 1, 236–248. [Google Scholar]
- Efron B, & Tibshirani R (1986). Bootstrap methods for standard errors, confidence intervals, and other measures of statistical accuracy Statistical Science, 1, 54–75. [Google Scholar]
- Espelage DL, Aragon SR, Birkett M, & Koenig BW (2008). Homophobic teasing, psychological outcomes, and sexual orientation among high school students: What influence do parents and schools have? School Psychology Review, 37, 202–216. [Google Scholar]
- Falconier MK, Huerta M, & Hendrickson E (2016). Immigration stress, exposure to traumatic life experiences, and problem drinking among first-generation Latino couples. Journal of Social and Personal Relationships, 33, 469–492. [Google Scholar]
- Falconier MK, Nussbeck F, Bodenmann G, Schneider H, & Bradbury T (2015). Stress from daily hassles in couples: its effects on intradyadic stress, relationship satisfaction, and physical and psychological well-being. Journal of Marital and Family Therapy, 41, 221–235. [DOI] [PubMed] [Google Scholar]
- Feinstein BA, Goldfried MR, & Davila J (2012). The relationship between experiences of discrimination and mental health among lesbians and gay men: An examination of internalized homonegativity and rejection sensitivity as potential mechanisms. Journal of Consulting and Clinical Psychology, 80, 917–927. [DOI] [PubMed] [Google Scholar]
- Feinstein BA, & Newcomb ME (2016). The role of substance use motives in the associations between minority stressors and substance use problems among young men who have sex with men. Psychology of Sexual Orientatation and Gender Diversity, 3, 357–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frost DM, & Fingerhut AW (2016). Daily exposure to negative campaign messages decreases same-sex couples’ psychological and relational well-being. Group Processes & Intergroup Relations, 19, 477–492. [Google Scholar]
- Goldbach JT, Schrager SM, Dunlap SL, & Holloway IW (2015). The application of minority stress theory to marijuana use among sexual minority adolescents. Substance Use and Misuse, 50, 366–375. [DOI] [PubMed] [Google Scholar]
- Goldbach JT, Tanner-Smith EE, Bagwell M, & Dunlap S (2014). Minority stress and substance use in sexual minority adolescents: A meta-analysis. Prevention Science, 15, 350–363. [DOI] [PubMed] [Google Scholar]
- Hammen C (2005). Stress and depression. Annual Review of Clinical Psychology, 1, 293–319. [DOI] [PubMed] [Google Scholar]
- Hays RD, Merz JF, & Nicholas R (1995). Response burden, reliability, and validity of the CAFE, Short MAST, and AUDIT alcohol screening measures. Behavior Research Methods, Instrucments, & Computers, 27, 277–280. [Google Scholar]
- Hendrick SS (1988). A generic measure of relationship satisfaction. Journal of Marriage and the Family, 50, 93–98. [Google Scholar]
- Howe GW, Levy ML, & Caplan RD (2004). Job loss and depressive symptoms in couples: common stressors, stress transmission, or relationship disruption? Journal of Family Psychology, 18, 639–650. [DOI] [PubMed] [Google Scholar]
- Jenkins N, & Saiz CC (1995). The Communication Skills Test. University of Denver. [Google Scholar]
- Kenny DA, & Judd CM (2014). Power anomalies in testing mediation. Psychological Science, 25, 334–339. [DOI] [PubMed] [Google Scholar]
- Kenny DA, Kashy DA, & Cook WL (2006). Dyadic data analysis. New York: Guilford Press. [Google Scholar]
- Laursen B, & Jensen Campbell LA (1999). The nature and functions of social exchange in adolescent romantic relationships In Furman W, Brown BB, & Feiring C (Eds.), The development of romantic relationships in adolescence (pp. 51–74). New York, NY: Cambridge University Press. [Google Scholar]
- LeBlanc AJ, Frost DM, & Wight RG (2015). Minority stress and stress proliferation among same-sex and other marginalized couples. Journal of Marriage and Family, 77, 40–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levitt A, & Cooper ML (2010). Daily alcohol use and romantic relationship functioning: evidence of bidirectional, gender-, and context-specific effects. Personality and Social Psychology Bulletin, 36, 1706–1722. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, & Williams J (2004). Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research, 39, 99–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshal MP, Dietz LJ, Friedman MS, Stall R, Smith HA, McGinley J, … Brent DA (2011). Suicidality and depression disparities between sexual minority and heterosexual youth: A meta-analytic review. Journal of Adolescent Health, 49, 115–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshal MP, Friedman MS, Stall R, King KM, Miles J, Gold MA, … Morse JQ (2008). Sexual orientation and adolescent substance use: A meta-analysis and methodological review. Addiction, 103, 546–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mays VM, & Cochran SD (2001). Mental health correlates of perceived discrimination among lesbian, gay, and bisexual adults in the United States. American Journal of Public Health, 91, 1869–1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Hughes TL, Bostwick WB, West BT, & Boyd CJ (2009). Sexual orientation, substance use behaviors and substance dependence in the United States. Addiction, 104, 1333–1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeil SN, Fincham FD, & Beach SR (2014). Does spousal support moderate the association between perceived racial discrimination and depressive symptoms among African American couples? Family Process, 53, 109–119. [DOI] [PubMed] [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129, 674–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr JJ, & Fassinger RE (2006). Sexual orientation identity and romantic relationship quality in same-sex couples. Personality and Social Psychological Bulletin, 32, 1085–1099. [DOI] [PubMed] [Google Scholar]
- Mustanski B, Andrews R, & Puckett JA (2016). The effects of cumulative victimization on mental health among lesbian, gay, bisexual, and transgender adolescents and young adults. American Journal of Public Health, 106, 527–533. doi: 10.2105/AJPH.2015.302976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newcomb ME, Macapagal KR, Feinstein BA, Bettin E, Swann G, & Whitton SW (2017). Integrating HIV prevention and relationship education for young same-sex male couples: A pilot trial of the 2GETHER intervention. AIDS and Behavior, 21, 2464–2478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newcomb ME, & Mustanski B (2010). Internalized homophobia and internalizing mental health problems: a meta-analytic review. Clinical Psychology Review, 30, 1019–1029. [DOI] [PubMed] [Google Scholar]
- Ngamake ST, Walch SE, & Raveepatarakul J (2016). Discrimination and sexual minority mental health: Mediation and moderation effects of coping. Psychology of Sexual Orientation and Gender Diversity, 3, 213–226. [Google Scholar]
- Nungesser LG (1983). Homosexual acts, actors, and identities. New York, NY: Praeger. [Google Scholar]
- Otis MD, Rostosky SS, Riggle EDB, & Hamrin R (2006). Stress and relationship quality in same-sex couples. Journal of Social and Personal Relationships, 23, 81–99. [Google Scholar]
- Phillips G 2nd, Turner B, Salamanca P, Birkett M, Hatzenbuehler ML, Newcomb ME, … Mustanski B (2017). Victimization as a mediator of alcohol use disparities between sexual minority subgroups and sexual majority youth using the 2015 National Youth Risk Behavior Survey. Drug and Alcohol Dependence, 178, 355–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D, & Group PC (2011). Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS(R)): Depression, anxiety, and anger. Assessment, 18, 263–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proulx CM, Helms HM, & Buehler C (2007). Marital quality and personal well-being: A meta-analysis. Journal of Marriage and Family, 69, 576–593. [Google Scholar]
- Puckett JA, Newcomb ME, Ryan DT, Swann G, Garofalo R, & Mustanski B (2017). Internalized homophobia and perceived stigma: A validation study of stigma measures in a sample of young men who have sex with men. Sexuality Research & Social Policy, 14, 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramirez-Valles J, Kuhns LM, Campbell RT, & Diaz RM (2010). Social integration and health: community involvement, stigmatized identities, and sexual risk in Latino sexual minorities. Journal of Health and Social Behavior, 51, 30–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randall AK, & Bodenmann G (2009). The role of stress on close relationships and marital satisfaction. Clinical Psychology Review, 29, 105–115. [DOI] [PubMed] [Google Scholar]
- Randall AK, Totenhagen CJ, Walsh KJ, Adams C, & Tao C (2017). Coping with workplace minority stress: Associations between dyadic coping and anxiety among women in same-sex relationships. Journal of Lesbian Studies, 21, 70–87. [DOI] [PubMed] [Google Scholar]
- Rayens MK, & Reed DB (2014). Predictors of depressive symptoms in older rural couples: the impact of work, stress and health. Journal of Rural Health, 30, 59–68. [DOI] [PubMed] [Google Scholar]
- Roberti JW, Harrington LN, & Storch EA (2006). Further psychometric support for the 10 item version of the Perceived Stress Scale. Journal of College Counseling, 9, 135–147. [Google Scholar]
- Rodriguez LM, Neighbors C, & Knee CR (2014). Problematic alcohol use and marital distress: An interdependence theory perspective. Addiction Research & Theory, 22, 294–312. [Google Scholar]
- Rook K, Dooley D, & Catalano R (1991). Stress transmission: The effects of husbands’ job stressors on the emotional health of their wives. Journal of Marriage & the Family, 53, 165–177. [Google Scholar]
- Rosario M, Rotheram-Borus MJ, & Reid H (1996). Gay-related stress and its correlates among gay and bisexual male adolescents of predominantly black and Hispanic background. Journal of Community Psychology, 24, 136–159. [Google Scholar]
- Rucker DD, Preacher KJ, Tormala ZL, & Petty RE (2011). Mediation analysis in social psychology: Current practices and new recommendations. Social and Personality Psychology Compass, 5, 359–371. [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, & Grant M (1993). Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction, 88, 791–804. [DOI] [PubMed] [Google Scholar]
- Schönbrodt FD, Maier M, Heene M, & Zehetleitner M (2015). Voluntary commitment to research transparency. Retrieved from http://www.researchtransparency.org [Google Scholar]
- Story LB, & Bradbury TN (2004). Understanding marriage and stress: essential questions and challenges. Clinical Psychology Review, 23, 1139–1162. [DOI] [PubMed] [Google Scholar]
- Swann G, Minshew R, Newcomb ME, & Mustanski B (2016). Validation of the Sexual Orientation Microagression Inventory in a diverse sample of LGBT youth. Archives of Sexual Behavior, 45, 1289–1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whisman MA (2007). Marital distress and DSM-IV psychiatric disorders in a population-based national survey. Journal of Abnormal Psychology, 116, 638–643. [DOI] [PubMed] [Google Scholar]
- Whisman MA (2013). Relationship discord and the prevalence, incidence, and treatment of psychopathology. Journal of Social and Personal Relationships, 30, 163–170. [Google Scholar]
- Whitton SW, & Buzzella BA (2012). Using relationship education programs with same-sex couples: A preliminary evaluation of program utility and needed modifications. Marriage & Family Review, 48, 667–688. [Google Scholar]
- Whitton SW, Weitbrecht EM, Kuryluk AD, & Hutsell DW (2016). A randomized waitlist-controlled trial of culturally sensitive relationship education for male same-sex couples. Journal of Family Psychology, 30, 763–768. [DOI] [PubMed] [Google Scholar]
- Wong CF, Weiss G, Ayala G, & Kipke MD (2010). Harassment, discrimination, violence, and illicit drug use among young men who have sex with men. AIDS Education and Prevention, 22, 286–298. [DOI] [PMC free article] [PubMed] [Google Scholar]