Abstract
Colorectal cancer is the most common cancer in Japan. Approximately 10%-20% of the patients with colorectal cancer present with large bowel obstruction, and those who present with malignant colonic obstruction (MCO) require urgent decompression because MCO can cause electrolytic fluid imbalance, colonic necrosis, bacterial translocation, and death. Placement of colonic stents (self-expandable metallic stents) for MCO is a major and standard endoscopic treatment that has been available since 2012 in Japan. This review presents the current conditions and future prospects of this procedure based on the literature. The current indication of colonic stent placement is malignant colorectal stenosis. One of the purposes of using stents is palliative treatment; further, its advantages over emergency surgery with colostomy include avoidance of colostomy, relief of obstruction, shorter hospitalization, and better quality of life. In addition, stent placement can also be used as a bridge to surgery since the duration of the hospitalization is shorter and postoperative complications, colostomy rates, and mortality rates are lower with elective than with emergency surgery. Although recent studies have reported low complication rates related to colonic stents, complications may still occur, highlighting the importance of good preparation, adequate staffing, backup systems, and informed consent. The current major problem related to colonic stents is the lack of evidence on patients' long-term prognoses for bridge to surgery purposes, awaiting the results of ongoing clinical research.
Keywords: colonic stent, obstructive colorectal cancer, CROSS, malignant colorectal obstruction
Introduction
Colorectal cancer is the most common cancer in Japan1), and it is one of the most common cancers worldwide2). Approximately 10%-20% of colorectal cancer patients present with large bowel obstruction3-6), and it is not rare because of the recent increase in colorectal cancer incidence in Japan.
Malignant colonic obstruction (MCO) due to colorectal cancer requires urgent decompression as a malignant gastrointestinal emergency. If not adequately treated, MCO can lead to electrolytic fluid imbalance, colonic necrosis, bacterial translocation, and death. Therefore, colonic stents have been widely used in recent years as an alternative treatment to decompression with colostomy surgery.
In patients undergoing curative resection, it has been reported that the prognosis does not differ between obstructive and non-obstructive cancers in stage-specific comparisons7). However, colorectal cancers that present with obstruction generally have a poorer prognosis than those that are non-obstructive because far-advanced cases are more common, even in the same stage8,9).
Evaluation of MCO
There is currently no established method for the evaluation of colonic obstruction/stenosis in MCO. Although Nagula et al. reported a colon obstruction score based on abdominal pain, abdominal distension, stool frequency, etc. that is evaluated from 0 to 15 points, it is not commonly used because of its complexity10).
The ColoRectal Obstruction Scoring System (CROSS) was developed in 2012 by the Japan Colonic Stent Safe Procedure Research Group as a simple, generally applicable technique for the assessment of colonic obstruction and stenosis; it has been published on the Research Group's home page (http://colon-stent.com/; Table 1)11). The scores of the CROSS system are based on the patient's oral intake and abdominal symptoms. Palliative use of colonic stents is indicated for patients with a CROSS score between 0 and 3, with a score between 0 and 1 indicating that stenting as a bridge to surgery (BTS) is appropriate. The CROSS system facilitates decision-making regarding the therapeutic strategies for patients with obstructive colorectal cancers and enables evaluation of their efficacy.
Table 1.
The ColoRectal Obstruction Scoring System (CROSS).
| Level of oral intake | Score |
|---|---|
| Requiring continuous decompressive procedure | 0 |
| No oral intake | 1 |
| Liquid or enteral nutrient | 2 |
| Soft solids, low-residue, and full diet with symptoms of stricture | 3 |
| Soft solids, low-residue, and full diet without symptoms of stricture† | 4 |
†Symptoms of stricture contain abdominal pain/cramps, abdominal distension, nausea, vomiting, constipation, and diarrhea which are related to gastrointestinal transit.
Indications and Contraindications of Colonic Stents
Many cases of MCO need colostomies, which have a negative impact on the patient's quality of life (QOL). To address this problem, the Japanese doctor, Dr. Dohmoto, introduced colonic stents into the rectum in the early 1990s as a palliative measure to decompress the colon when curative resection was not an option12). The indications for colonic stents then expanded to include pre-operative decompression as a BTS when curative resection was indicated13,14). In 2010, the World Society of Emergency Surgery and the American Society for Gastrointestinal Endoscopy guidelines recommended decompression with colonic stents as a standard treatment for MCO15,16).
The introduction of colonic stents to Japan occurred in 2012. In Japan there are now four types of colonic stents manufactured in three countries available (Figure 2). Since the extension and radial force of each type of stent differs, they must be selected according to the patient's condition. Colonic stents are today indicated for palliative treatment of cases of MCO that present with stenosis or obstruction, including recurrence at the anastomotic site following colorectal cancer surgery, metastatic recurrence, and obstructive unresectable cancers. The primary sites of malignancy include not only colorectal cancer but also pancreatic, gastric, and ovarian cancer among others.
Figure 1.
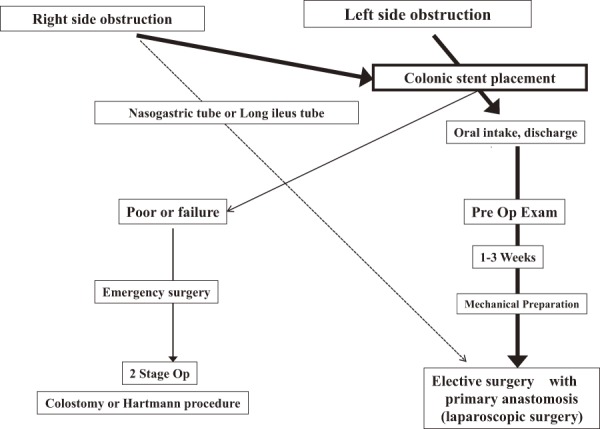
Strategy for Curative Obstructive Colorectal Cancers.
Figure 2.

Colonic stents in Japan (2019).
Another indication for colonic stents is as a BTS to avoid emergency surgery for colorectal cancer patients who present with bowel obstruction by providing pre-operative resolution of the stenosis or obstruction.
Contraindications for colonic stents include complex or elongated stenosis, hemorrhage, severe inflammation, or perforations. In addition, use of colonic stents is contraindicated for benign stenosis or obstruction under the Japanese health insurance system. Some small series of colonic stent placements for benign disease have been reported, but the incidence of complications was high17-19).
The design of current stents is not appropriate for benign stenosis, and there are many issues, such as the best time and method to remove the stent after the stenosis is released. In the future, a stent suitable for use in benign stenosis is needed.
There is a high likelihood of pain and distress when the stent margin approaches the pectinate line of the anal canal; therefore, the use of colonic stents for rectal stenosis near the anal verge is inappropriate. It has also been reported that pain or an uncomfortable sensation is likely when a colonic stent is placed within 5 cm of the anal verge20-22) or within 5 cm of the dentate line23).
In western countries, most stents are placed in the left-side colon, and there have been few reports of the utility of right-sided colonic stent placement. On the other hand, in Japan, right-sided stent placement is relatively common24), and more reports of its utility are gradually appearing25).
Transanal Drainage: Colonic Stent versus Transanal Drainage Tubes
When surgical cure of an obstructive colorectal cancer is possible, one must consider resolution of the bowel obstruction, enhancement of surgical safety, and achievement of a complete cure.
Surgery for an obstructed bowel is prone to contaminating surgery with possibilities of higher than usual surgical complications and mortality26). Since one-stage anastomosis is associated with high risks of dehiscence and other postoperative complications, many cases require colostomy, which adversely affects the patient's QOL.
The ideal approach involves avoiding emergency surgery by conservative treatment to resolve the bowel obstruction and then deciding on elective surgery following improvement in the patient's general condition. However, decompression of the large intestine into the small intestine may be impeded by the ileocecal valve, which prevents reflux, when nasogastric or long ileus tubes are used. Thus, colonic stents have been used as a BTS to address this issue since the 1990s because the pre-operative decompression occurs through the anus as the bridge to elective surgery13). Currently, this transanal approach to pre-operative decompression involves the use of colonic stents13) or transanal drainage tubes27).
Only one study has compared colonic stents and transanal drainage using a two-group design that was not a randomized, controlled trial28). Table 2 shows a comparison between colonic stents and transanal drainage tubes in Japan.
Table 2.
Comparison between Colonic Stents and Transanal Drainage Tubes for BTS.
| Colonic stent | Transanal drainage tube | |
|---|---|---|
| Success rate | Feasible | Feasible |
| Decompression | Fast | Slow |
| Management | Easy | Difficult |
| Odor | Non | Yes |
| Oral intake | Possible | Difficult |
| QOL | Good | Poor |
| Influence to the tumor | Invasive? | Possibility of local recurrence? |
| Proximal site perforation | Minimum | 10%? |
| Long term placement | Possible | Difficult |
The lumens of transanal drainage tubes are narrower than those of colonic stents, which results in a longer time for bowel obstruction to resolve and difficulty in starting solid meals when transanal drainage tubes are used. Further, they require frequent washing with warm water and are used over consecutive days, which indicate the difficulties in medical management and the negative effect on the patient's QOL. On the other hand, colonic stents might be better from the perspective of examining lesions on the proximal side and of patients' QOL because their management is easier and solid food can be taken after placement. When colonic stenting is used as a BTS for patients with obstructive colorectal cancer, it helps improve their nutritional status and mechanical bowel preparation, and it permits primary anastomosis without stoma creation and even laparoscopic surgery.
Figure 1 shows our current therapeutic strategy for managing patients with obstructive colorectal cancers. The standard approach begins with colonic stenting, which is then followed by laparoscopic surgery independent of the location of the obstruction on the right or left side29,30).
Short-term Outcomes of Colonic Stents
In a systematic review of colonic stents, the median technical success rate was 96.2% (range: 66.6% to 100%), and the median clinical success rate was 92% (range: 46% to 100%)31). In a report from European multinational registries, satisfactory outcomes were also achieved, with technical and clinical success rates of 98% and 94%, respectively, and an overall complication rate of 7.8% (perforation: 3%; stent migration: 1.2%; hemorrhage: 0.6%)32). The results of this meta-analysis, which included eight studies and 601 patients, showed significantly lower colostomy and ICU admission rates, a significantly higher primary anastomosis rate, and significantly lower surgical complication and anastomotic leakage rates with stent insertion, with no adverse impacts on mortality or long-term outcomes33). Thus, the use of colonic stents for MCO as a BTS can avoid colostomies and reduce surgical complications. In Japan, the Japan Colonic Stent Safe Procedure Research Group conducted a multi-center, prospective, clinical study that reported technical and clinical success rates of 97.9% and 95.5%, respectively, with a perforation rate of 2%, demonstrating that colonic stents can be safely inserted in Japan24). In an analysis of factors related to difficult stent placement using the same database, Kuwai et al. concluded that technical challenges must be anticipated in cases with peritoneal carcinomatosis, a CROSS score of 0, or expansive strictures; in such cases, experienced clinicians should perform self-expandable metallic stent (SEMS) placement34).
Long-term Outcomes of Colonic Stents
With stent placement, there have been some concerns over metastases or a worse prognosis due to direct invasion of the tumor (such as stent encroachment into the tumor). However, in my view, the results of a study performed with my colleagues35) and of a study from the United Kingdom36) demonstrated no adverse effect on long-term outcomes. Another meta-analysis also reported that stent placement had no adverse effects on perioperative mortality or long-term outcomes33). However, a study by Sabbagh et al.37) in 2013 involving 87 patients with left-sided MCO showed that patients who underwent stenting as a BTS had significantly poorer overall and 5-year survivals than patients undergoing surgery only, with a 5-year cancer-specific mortality of 48% with stent placement and 21% with surgery. These results suggested that stents may have an adverse effect on long-term outcomes in colorectal cancer patients37). However, that study was a retrospective investigation of cancer mortality rates, with a higher prevalence of synchronous distant metastasis in the stent placement group (37.5%) than in the surgery-only group (10.2%). Furthermore, there was a low success rate (81%) in the stent group.
Nevertheless, the European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline does not recommend using stenting as a BTS as the standard treatment for symptomatic left-sided MCO because of the possible adverse effects on long-term outcomes38). However, this guidance was based on data from studies that showed relatively poor success and high complication rates, including perforation, following colonic stenting, and poor stent placement might be related to poor long-term outcomes. In response, the “Japan Colonic Stent Safe Procedure Research Group's Comments on the ESGE Clinical Guidance” have now been published on the group's web site. They stress that the conclusion on BTS stents may be premature because international studies conducted with an oncological primary endpoint and providing a high level of evidence are still lacking.
In fact, a randomized, controlled trial endorsed by the European Association for Endoscopic Surgery conducted in Italy recently compared colonic stents and emergency surgery39). While there was no difference in long-term outcomes, the primary endpoint was a short-term outcome, and it does not appear that the study will produce a change in the above-stated ESGE guidance. Furthermore, a meta-analysis in 2017 that included seven studies with 1,333 patients reported no significant differences in recurrence, 3-year mortality, and 5-year mortality rates between a BTS group and an emergency surgery group. They concluded that the best treatment option for left-sided MCOs is a BTS in centers with the appropriate skill40). Belgian prospective 10-year survival data after endoscopic stent placement as a BTS in patients with obstructive colon cancer showed that colon stenting before surgery was effective and did not have a negative effect on survival outcomes when the patients were treated with curative intent41). However, such evidence is not suitable to change the ESGE Clinical Guidance, and further randomized, controlled studies are needed to compare survival after stenting with that after primary resection.
The World Society of Emergency Surgery renewed the guidelines on colon and rectal cancer emergencies and concluded that for obstructive left colon carcinoma, SEMS, when available, offers interesting advantages as compared to emergency surgery; however, the positioning of SEMS in surgically treatable cases is still accompanied by some long-term oncologic disadvantages, which are still under analysis42), and a “non-inferiority” RCT with survival as primary end point would be the appropriate method to correctly investigate long-term outcomes after stenting as BTS versus emergency surgery.
With this background, the Japan Colonic Stent Safe Procedure Research Group started two multi-center clinical studies to provide appropriate evidence. One is a retrospective study, ‘A study on colonic decompression as BTS for stage II/III obstructive colon cancer: retrospective multi-center observational study’ (the CODOMO study), and the other is a prospective, randomized, controlled trial, ‘Colonic stent for “Bridge to Surgery” comparing treatment with non-stenting surgery in stage II/III obstructive colon cancer’ (the COBRA trial).
The CODOMO study was closed in 2018, and the results will become available in 2019. The COBRA trial was started in 2017 and is ongoing.
In the palliative setting, a new systematic review and meta-analysis that included four RCT studies totaling 125 patients reported that there was no difference in the 30-day mortality and mean survival days between the emergency surgery group and the stent placement group. This was the first systematic review to include only RCTs in the palliative setting, and the conclusion was that colonic stent placement may be an alternative to surgery, with early hospital discharge and a lower risk of permanent stoma as its advantages43). The conclusion is the same in the ESGE clinical guideline38).
Colonic stents are strongly recommended as a treatment option for palliation of malignant colorectal obstruction.
Conclusions
Of the currently available endoscopic and interventional radiology treatments, colonic stenting can have dramatic efficacy; patients brought to the hospital by ambulance can walk and eat soon after the treatment. However, many unclear points remain about colonic stents, such as which patients have a high risk of perforation, the advisability of chemotherapy after stent placement, and the patients' long-term prognosis. Approximately 30% to 40% of the patients with long-term stent placement have some incidental symptoms, and re-intervention or other surgical procedures such as the stent-in-stent procedure are often required. These details must be carefully explained to all patients before stenting, and regular patient monitoring is needed following stent placement. The endoscopic treatment team and the surgical team must collaborate in both treatment and monitoring patient progress.
Disclaimer
Yoshihisa Saida is one of the Associate Editors of Journal of the Anus, Rectum and Colon and on the journal's Editorial Board. He was not involved in the editorial evaluation or decision to accept this article for publication at all.
Conflicts of Interest
There are no conflicts of interest.
References
- 1.Center for Cancer Control and Information Services, National Cancer Center. Cancer Statistics in Japan, 2017. [cited 2019 Feb 20]. Available from: https://ganjoho.jp/en/professional/statistics/brochure/2017_en.html.
- 2.Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin. 2011 Mar; 61(2): 69-90. [DOI] [PubMed] [Google Scholar]
- 3.Jullumstrø E, Wibe A, Lydersen S, et al. Colon cancer incidence, presentation, treatment and outcomes over 25 years. Colorectal Dis. 2011 May; 13(5): 512-8. [DOI] [PubMed] [Google Scholar]
- 4.Winner M, Mooney SJ, Hershman DL, et al. Incidence and predictors of bowel obstruction in elderly patients with stage IV colon cancer: a population-based cohort study. JAMA Surg. 2013 Aug; 148(8): 715-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yeo HL, Lee SW. Colorectal emergencies: review and controversies in the management of large bowel obstruction. J Gastrointest Surg. 2013 Nov; 17(11): 2007-12. [DOI] [PubMed] [Google Scholar]
- 6.Cheynel N, Cortet M, Lepage C, et al. Trends in frequency and management of obstructing colorectal cancers in a well-defined population. Dis Colon Rectum. 2007 Oct; 50(10): 1568-75. [DOI] [PubMed] [Google Scholar]
- 7.Hasegawa K, Sugihara K, Enomoto M, et al. [A study of obstructive colorectal cancer]. Jpn J Gastroenterol Surg. 2000 Jun; 33(6): 709-15. Japanese. [Google Scholar]
- 8.Kamigaki T, Shimada E, Urakawa T. [A clinicopathological study of colorectal cancer with bowel obstruction]. Jpn J Gastroenterol Surg. 1993 Jan; 26(1): 76-81. Japanese. [Google Scholar]
- 9.Yang Z, Wang L, Kang L, et al. Clinicopathologic characteristics and outcomes of patients with obstructive colorectal cancer. J Gastrointest Surg. 2011 Jul; 15(7): 1213-22. [DOI] [PubMed] [Google Scholar]
- 10.Nagula S, Ishill N, Nash C, et al. Quality of life and symptom control after stent placement or surgical palliation of malignant colorectal obstruction. J Am Coll Surg. 2010 Jan; 210(1): 45-53. [DOI] [PubMed] [Google Scholar]
- 11.Saida Y. [A review of colonic stents]. Gastroenterol Endosc. 2013 Jan; 55(1): 3-11. Japanese [Google Scholar]
- 12.Dohmoto M. [New method: endoscopic implantation of rectal stent in palliative treatment of malignant stenosis]. Endosc Dig. 1991 Nov; 3(11): 1507-12. Japanese. [Google Scholar]
- 13.Saida Y, Sumiyama Y, Nagao J, et al. Stent endoprosthesis for obstructing colorectal cancers. Dis Colon Rectum. 1996 May; 39(5): 552-5. [DOI] [PubMed] [Google Scholar]
- 14.Trompetas V. Emergency management of malignant acute left-sided colonic obstruction. Ann R Coll Surg Engl. 2008 Apr; 90(3): 181-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ansaloni L, Andersson RE, Bazzoli F, et al. Guidelines in the management of obstructing cancer of the left colon: consensus conference of the world society of emergency surgery (WSES) and peritoneum and surgery (PnS) society. World J Emerg Surg. 2010 Dec; 5(1): 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.ASGE Standards of Practice Committee, Harrison ME, Anderson MA, et al. The role of endoscopy in the management of patients with known and suspected colonic obstruction and pseudo-obstruction. Gastrointest Endosc. 2010 Apr; 71(4): 669-79. [DOI] [PubMed] [Google Scholar]
- 17.Small AJ, Young-Fadok TM, Baron TH. Expandable metal stent placement for benign colorectal obstruction: outcomes for 23 cases. Surg Endos. 2008 Feb; 22(2): 454-62. [DOI] [PubMed] [Google Scholar]
- 18.Geiger TM, Miedema BW, Tsereteli Z, et al. Stent placement for benign colonic stenosis: case report, review of the literature, and animal pilot data. Int J Colorectal Dis. 2008 Oct: 23(10): 1007-12. [DOI] [PubMed] [Google Scholar]
- 19.Keränen I, Lepistö A, Udd M, et al. Outcome of patients after endoluminal stent placement for benign colorectal obstruction. Scand J Gastroenterol. 2010 Jun; 45(6): 725-31. [DOI] [PubMed] [Google Scholar]
- 20.Pothuri B, Guirguis A, Gerdes H, et al. The use of colorectal stents for palliation of large-bowel obstruction due to recurrent gynecologic cancer. Gynecol Oncol. 2004 Dec; 95(3): 513-17. [DOI] [PubMed] [Google Scholar]
- 21.Ptok H, Meyer F, Marusch F, et al. Palliative stent implantation in the treatment of malignant colorectal obstruction. Surg Endosc. 2006 Jun; 20(6): 909-14. [DOI] [PubMed] [Google Scholar]
- 22.Song HY, Kim JH, Kim KR, et al. Malignant rectal obstruction within 5 cm of the anal verge: is there a role for expandable metallic stent placement? Gastrointest Endosc. 2008 Oct; 68(4): 713-20. [DOI] [PubMed] [Google Scholar]
- 23.Mergener K, Kozarek RA. Stenting of the gastrointestinal tract. Dig Dis. 2002; 20(2): 173-81. [DOI] [PubMed] [Google Scholar]
- 24.Matsuzawa T, Ishida H, Yoshida S, et al. A Japanese prospective multicenter study of self-expandable metal stent placement for malignant colorectal obstruction: short-term safety and efficacy within 7 days of stent procedure in 513 cases. Gastrointest Endosc. 2015 Oct; 82(4): 697-707. [DOI] [PubMed] [Google Scholar]
- 25.Amelung FJ, Consten ECJ, Siersema PD, et al. A population-based analysis of three treatment modalities for malignant obstruction of the proximal colon: Acute resection versus stent or stoma as a bridge to surgery. Ann Surg Oncol. 2016 Oct; 23(11): 3660-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Barillari P, Aurello P, De Angelis R, et al. Management and survival of patients affected with obstructive colorectal cancer. Int Surg. 1992 Oct-Dec; 77(4): 251-55. [PubMed] [Google Scholar]
- 27.Lelcuk S, Ratan J, Klausner JM, et al. Endoscopic decompression of acute colonic obstruction. Avoiding staged surgery. Ann Surg. 1986 Mar; 203(3): 292-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li CY, Guo SB, Wang NF. Decompression of acute left-sided malignant colorectal obstruction: comparing transanal drainage tube with metallic stent. J Clin Gastroenterol. 2014 May-Jun; 48(5): e37-42. [DOI] [PubMed] [Google Scholar]
- 29.Frago R, Ramirez E, Millan M, et al. Current management of acute malignant large bowel obstruction: a systematic review. Am J Surg. 2014 Jan; 2017(1): 127-38. [DOI] [PubMed] [Google Scholar]
- 30.Enomoto T, Saida Y, Takabayashi K, et al. Open surgery versus laparoscopic surgery after stent insertion for obstructive colorectal cancer. Surg Today. 2016 Dec; 46(12): 1383-86. [DOI] [PubMed] [Google Scholar]
- 31.Watt AM, Faragher IG, Griffin TT, et al. Self-expanding metallic stents for relieving malignant colorectal obstruction: a systematic review. Ann Surg. 2007 Jul; 246(1): 24-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jimenez-Perez J, Casellas J, Garcia-Cano J, et al. Colonic stenting as a bridge to surgery in malignant large-bowel obstruction: a report from two large multinational registries. Am J Gastroenterol. 2011 Dec; 106(12): 2174-80. [DOI] [PubMed] [Google Scholar]
- 33.Zhang Y, Shi J, Shi B, et al. Self-expanding metallic stent as a bridge to surgery versus emergency surgery for obstructive colorectal cancer: a meta-analysis. Surg Endosc. 2012 Jan; 26(1): 110-19. [DOI] [PubMed] [Google Scholar]
- 34.Kuwai T, Yamaguchi T, Imagawa H, et al. Factors related to difficult self-expandable metallic stent placement for malignant colonic obstruction: A post-hoc analysis of a multicenter study across Japan. Dig Endosc. 2019 Jan; 31(1): 51-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Saida Y, Sumiyama Y, Nagao J, et al. Long-term prognosis of preoperative “bridge to surgery” expandable metallic stent insertion for obstructive colorectal cancer: comparison with emergency operation. Dis Colon Rectum. 2003 Oct; 46(10): S44-9. [DOI] [PubMed] [Google Scholar]
- 36.Tilney S, Lovegrove RE, Purkayastha S, et al. Comparison of colon stenting and open surgery for malignant large bowel obstruction. Surg Endosc. 2007 Feb; 21(2): 225-33. [DOI] [PubMed] [Google Scholar]
- 37.Sabbagh C, Browet F, Diouf M, et al. Is stenting as “a bridge to surgery” an oncologically safe strategy for the management of acute, left-sided, malignant, colonic obstruction? A comparative study with a propensity score analysis. Ann Surg. 2013 Jul; 258(1): 107-15. [DOI] [PubMed] [Google Scholar]
- 38.van Hooft JE, van Halsema EE, Vanbiervliet G, et al. Self-expandable metal stents for obstructing colonic and extracolonic cancer: European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. Endoscopy. 2014 Nov; 46(11): 990-1053. [DOI] [PubMed] [Google Scholar]
- 39.Arezzo A, Balague C, Targarona E, et al. Colonic stenting as a bridge to surgery versus emergency surgery for malignant colonic obstruction: results of a multicentre randomised controlled trial (ESCO trial). Surg Endosc. 2017 Aug; 31(8): 3297-305. [DOI] [PubMed] [Google Scholar]
- 40.Ceresoli M, Allievi N, Coccolini F, et al. Long-term oncologic outcomes of stent as a bridge to surgery versus emergency surgery in malignant left side colonic obstructions: a meta-analysis. J Gastrointest Oncol. 2017 Oct; 8(5): 867-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Verstockt B, Van Driessche A, De Man M, et al. Ten-year survival after endoscopic stent placement as a bridge to surgery in obstructing colon cancer. Gastrointest Endosc. 2018 Mar; 87(3): 705-13. [DOI] [PubMed] [Google Scholar]
- 42.Pisano M, Zorcolo L, Merli C, et al. 2017 WSES guidelines on colon and rectal cancer emergencies: obstruction and perforation. World J Emerg Surg. 2018 Dec; 13(1): 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ribeiro IB, Bernardo WM, Martins BDC, et al. Colonic stent versus emergency surgery as treatment of malignant colonic obstruction in the palliative setting: a systematic review and meta-analysis. Endosc Int Open. 2018 May; 6(5): E558-67. [DOI] [PMC free article] [PubMed] [Google Scholar]


