Abstract
Objective:
Traumatic brain injury (TBI) sustained in childhood is associated with poor social outcomes. This study investigated the role of theory of mind (ToM) as a mediator of the relation between TBI and peer rejection/victimization and reciprocated friendships, as well as the moderating effect of parental nurturance on those relationships.
Method:
Participants were children ages 8 to 13 (M = 10.45, SD = 1.47), including 13 with severe TBI, 39 with complicated mild/moderate TBI, and 32 children with orthopedic injuries. Data on peer rejection/victimization and friendship were collected in school classrooms using the Extended Class Play and friendship nominations. Parents rated parental nurturance using the Child-Rearing Practices Report. Finally, ToM was measured based on children’s average performance across three tasks measuring different aspects of ToM.
Results:
Severe TBI was associated with poorer ToM, greater peer rejection/victimization, and fewer reciprocated friendships. ToM mediated the relation between severe TBI and peer rejection/victimization (i.e., severe TBI predicted poorer ToM, which in turn predicted greater rejection/victimization). Parental nurturance significantly moderated this relation, such that the mediating effect of ToM was significant only at low and average levels of parental nurturance, for both severe and complicated mild/moderate TBI groups. Neither the mediating effect of ToM nor the moderating effect of parental nurturance was significant for reciprocated friendships.
Conclusion:
High parental nurturance may mitigate the negative effects of ToM deficits on risk of peer rejection/victimization among children with TBI. Interventions designed to increase parental nurturance or ToM may promote better social outcomes among children with TBI.
Keywords: Paediatrics, Traumatic Brain Injury, Social Outcomes, Reciprocated Friendships, Peer Rejection/Victimization, Theory of Mind, Parenting
Introduction
Traumatic brain injury (TBI) is a leading cause of morbidity and mortality in children and adolescents (Schneier, Shields, Hostetler, Xiang, & Smith, 2006). Annually, more than one million children sustain a TBI resulting in hospital care in the United States (Langlois, Rutland-Brown, & Thomas, 2005). Childhood TBI is associated with an increased risk of a variety of negative outcomes in several domains ( Rosema, Crowe, & Anderson, 2012; Schwartz et al., 2003). In particular, disruptions in social functioning have been reported by parents to be one of the most debilitating problems for children after a TBI (Rosema, Crowe, & Anderson, 2012). Impairments in social functioning after childhood TBI are of concern because poor social functioning can lead to psychological distress, social isolation, and lower self-esteem, which may subsequently lead to lowered quality of life (Anderson & Beauchamp, 2012).
Research on social outcomes indicates that children with TBI, particularly severe TBI, exhibit persistent problems in social information processing, peer relationships, self-esteem, and social adjustment, with attendant feelings of social isolation and loneliness (Rosema, Crowe, & Anderson, 2012; Yeates et al., 2007; Ganesalingam et al., 2011). Two studies (Hung et al., 2017; Yeates et al., 2013) have shown that children with severe TBI are especially vulnerable to peer rejection and victimization, compared to children with orthopedic injuries (OI). Children with severe TBI also have fewer reciprocated friendships among school classmates (Yeates et al., 2013). These findings have important implications for development, as early peer rejection can place children at increased risk for maladjustment in the classroom, poor academic achievement, and attention problems (Ladd & Burgess, 2001), while reciprocated friendship is an important predictor of positive adjustment (Kingery, Erdley, & Marshall, 2011; Rubin, Bukowski, & Bowker, 2015).
Yeates and colleagues (2007) proposed an integrative model of social competence in childhood brain disorders. The model differentiates among three levels of social competence: social information processing, social interaction, and social adjustment. Childhood brain disorders can affect performance at all three levels, which are interrelated and influence one another (e.g., social information processing affects social interaction). Both injury-related and non-injury related factors are identified in the model as potential moderators of the effect of childhood brain disorder on social competence. Injury-related factors include the severity of brain disorder, while non-injury factors include environmental influences, such as the family environment and parenting style.
Theory of mind (ToM) is an important aspect of social information processing, and contributes significantly to social competence in general. ToM involves the ability to reason about the mental state of onself and others, and to use this information to understand what others are thinking and feeling and to predict how others will act (Wellman, Cross and Watson, 2001). ToM includes not only cognitive aspects (e.g., understanding the content of what others are thinking, or cognitive ToM), but also understanding the emotional states of others (i.e., affective ToM), as well as the use of social communication to influence the mental and emotional states of others (i.e., conative ToM) (Dennis et al., 2013). ToM emerges in early childhood and continues to develop through late childhood and into mid adolescence (Wellman et al., 2001; Sodian, 2011).
Impairments in ToM have been demonstrated among children with TBI (Ryan et al., 2016; Dennis et al., 2013). ToM impairments can hamper one’s ability to understand the emotions and intentions of others during social interactions, thus interfering with peer relationships and negatively affecting social adjustment (Yeates et al., 2014). ToM has been identified as a mediator of the association between injury severity and social adjustment among children with TBI, such that children with severe TBI performed more poorly on measures of ToM, which in turn predicted poorer parent reported social adjustment (Robinson et al., 2014). Furthermore, better performance on ToM tasks predicts less rejection/victimization after childhood TBI (Yeates et al., 2014).
Environmental factors, such as parenting style, can also affect social competence. For instance, studies have shown that a positive, nurturing relationship with a primary caregiver is associated with successful functioning within peer groups during childhood and adolscence (Brophy-Herb et al., 2011; Booth-LaForce et al., 2006). In contrast, harsh and insensitive parenting has been shown to be associated with peer group difficulties, such as peer victimization, aggression, and unsupportive friendships (Ladd & Ladd, 1998; Park et al., 2005). In children with TBI, parenting style has been found to moderate the association between injury and peer social adjustment. Specifically, Root and colleagues (2016) reported that, at lower levels of parental nurturance, children with TBI were more likely to be rejected by their peers. Furthermore, higher levels of harsh, punitive parenting are related to higher ratings of behavioural and cognitive dysregulation in children with TBI compared to children with OI (Potter et al., 2011).
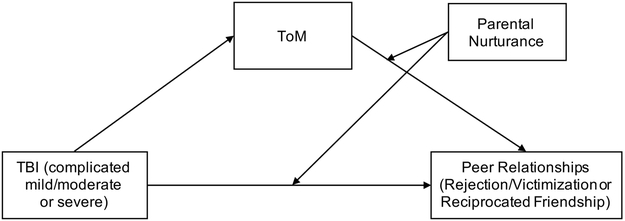
In sum, children with TBI are vulnerable to poor social outcomes. They are more likely to be rejected by their peers and to have fewer reciprocated friendships. Social information processing skills, such as ToM, have been found to mediate the relationship between TBI and social adjustment. Additionally, parenting style has been found to moderate the association between injury and social outcome. However, the manner in which ToM and parenting style act jointly to predict peer victimization/rejection and friendship remains unclear, because they have previously been examined in isolation. Therefore, the current study sought to examine the roles of ToM and parental nurturance in the prediction of social outcomes in children with complicated mild, moderate, and severe TBI, using ecologically-derived classroom data to assess peer relationships. ToM was predicted to mediate the relationship between TBI and peer relationships (i.e., TBI would predict ToM, which in turn would predict peer rejection/victimization and reciprocated friendships), and parental nurturance was hypothesized to moderate ToM’s relationship to peer outcomes (i.e., higher levels of parental nurturance would weaken the relationship of ToM to peer rejection/victimization and reciprocated friendship). Parental nurturance also was predicted to moderate the direct relationship between injury and peer relationships, such that the effects of TBI on peer relationships would be weakened in the presence of higher levels of parental nurturance. The proposed moderated mediation model is depicted in Figure 1.
Figure 1.
Proposed moderated mediation model.
Methods
Study Design and Overview
Data were drawn from a larger parent project, entitled Social Outcomes in Kids with Brain Injury (SOBIK). SOBIK was a cross-sectional, multi-site observational cohort study that examined social outcomes in children with TBI. From April 2007 to December 2011, participants were recruited from children’s hospitals at three metropolitan sites, including the Hospital for Sick Children in Toronto (Canada), Nationwide Children’s Hospital in Columbus (United States), and Rainbow Babies and Children’s Hospital and MetroHealth Medical Center in Cleveland (United States).
Participants
Eligible participants included children who had been hospitalized for either TBI or OI, were from 8- to 13- years of age at the time of participation, and were injured between 12 and 63 months prior to participation. Participants in the current study were restricted to the 84 children from the total sample of 143 from the larger study for whom classroom data were obtained (n = 13 of 25 with severe TBI, n = 39 of 57 with complicated mild/moderate TBI, and n = 32 of 61 with OI). The availability of classroom data did not differ as a function of injury group, sex, race, socioeconomic status (SES), age at injury, or age at assessment. Injury severity for TBI participants was assessed using the Glasgow Coma Scale (GCS; Teasdale & Jennette, 1974). TBI severity ranged from complicated mild to severe based on assessment at the time of injury. Complicated mild TBI was defined as a GCS score of 13 to 15 and associated neuroimaging abnormalities, moderate TBI was defined as a GCS score of 9 to 12, and severe TBI was defined as a GCS score of 3 to 8. A depressed skull fracture was sufficient to permit inclusion in the complicated mild TBI group, although only three children met eligibility for complicated mild TBI based solely on a depressed skull fracture. Based on research suggesting that children with complicated mild and moderate TBI demonstrate similar outcomes (Kashluba et al., 2008), these children were combined into a single complicated mild/moderate TBI group. The OI group consisted of children who sustained a non-head injury (e.g., thorax, upper extremity, lower extremity) that required hospital admission but was not associated with loss of consciousness or other indications of brain injury (e.g., skull or facial fractures).
The following exclusion criteria applied to both the TBI and OI groups: (a) history of any serious injury requiring medical treatment besides the target injury (for the OI group, no previous history of TBI); (b) neurological disorder or intellectual disability prior to the target injury; (c) any injury resulting from child abuse or assault; (d) history of severe psychiatric disorder requiring hospitalization prior to the target injury; (e) sensory or motor impairment that prevented valid administration of study measures; (f) primary language other than English; and (g) contraindication to MRI (e.g., orthodontic appliances). Children attending full-time special education classes were excluded because the reliability and validity of classroom data for such classrooms is not established. Children with a history of premorbid learning or attention problems were not excluded.
Among eligible children who were approached about participating in the larger SOBIK study, 82 (47%) of those with TBI and 61 (26%) of those with OI agreed to enroll. The rate of participation was significantly higher for the TBI group than for the OI group. No significant differences were found between those who agreed to participate versus those who declined in terms of age at injury, age at initial contact, sex, race, or census tract measures of SES that included mean family income, percentage of minority heads of household, and percentage of households below the poverty line. Participants and non-participants also did not differ on measures of injury severity (i.e., mean length of hospital stay, median Glasgow Coma Scale score for children with TBI).
Procedures
Site-specific Institutional Review Boards approved all study procedures prior to recruitment, and informed parental consent and child assent were obtained prior to participation. All participants completed an assessment that included measures of children’s social cognition (i.e., ToM) and cognitive ability (i.e., IQ), as well as parental ratings of child-rearing practices (i.e., parental nurturance). Classroom data was then collected at the schools of the participants. To collect classroom data, school principals were sent written information about the study, and then contacted by telephone to obtain their permission to contact participants’ teachers. A teacher meeting was held to explain the study. Teachers distributed and collected parental consent forms from students. The study was described to students as a study of friendships without mentioning TBI or identifying the target child as the participant. Classroom data was not collected during the first 2 months of the school year to ensure that children were familiar with one another before completing ratings. The TBI and OI groups did not differ in the average number of months that had passed during the school year before classroom data collection (M = 6.30; SD = 2.09). Parental consent was obtained for 82% of available classmates, of whom 96% were present on the day of data collection; therefore, 79% of classmates participated. Classroom data were provided by 1598 children in 87 elementary and middle school classrooms. On average, 18.4 students (SD = 4.7; range = 7-30) participated in each class.
Laboratory Measures
Theory of Mind (ToM).
ToM was measured based on average performance across three tasks measuring different aspects of ToM: cognitive ToM (i. e., concerned with the child’s understanding of false beliefs, as measured by the Jack and Jill task; Dennis et al., 2013), affective ToM (i.e., concerned with the child’s understanding of the difference between internal emotional experience and emotive communication, as measured by the Emotional and Emotive Faces task; Dennis et al., 1998, 2013), and conative ToM (i.e., concerned with the child’s understanding of how indirect speech acts are used to influence the listener, as measured by the Irony and Empathy task; Dennis et al., 2001). We have shown previously that the magnitude of group differences (i.e., OI versus severe TBI versus mild/moderate TBI) on the three subtypes of ToM did not differ (i.e., the interaction of group and subtype of ToM was not significant), and in a preliminary factor analysis we showed that the three ToM subtype scores loaded highly onto one factor (Dennis et al., 2013; Wolfe et al., 2014). Therefore, individual scores on each ToM task were transformed to percentage correct, and a composite score was generated for each participant by averaging the percentage correct across the three tasks.
Parental Nurturance.
Parental nurturance was assessed using the Child Rearing Practices Report (CRPR; Rickel & Biasatti, 1982), which was completed by mothers. Items on the CRPR are measured on a 6-point Likert scale and assess the primary caregiver’s child-rearing practices, yielding two factor-derived subscales: nurturing parenting (14-items; e.g., “I respect my child’s opinion and encourage him/her to express it”; α = .77 for TBI & .70 for OI; Root et al., 2016), and restrictive parenting (12 items; e.g., “I control my child by warning him/her that bad things might happen”; α = .79 for TBI & .81 for OI; Root et al., 2016). For the purpose of this study, only scores for parental nurturance were included in analyses. Higher scores are indicative of higher parental nurturance.
IQ.
Overall cognitive ability was measured using the two-subtest short form of the Weschler Abbreviated Scale of Intelligence (Wechsler, 1999), which includes the Vocabulary and Matrix Reasoning subtests to estimate IQ.
Classroom Measures
Extended Class Play (ECP).
Participants and their classmates completed an extended version of the Revised Class Play (RCP; Masten, Morison, & Pellegrini, 1985) in their classrooms. Children were instructed to pretend they were the directors of an imaginary class play and to nominate their classmates for 31 hypothetical roles (e.g., “someone whose feelings get hurt easily”, “a person who gets into fights a lot”, etc.). Children nominated one boy and one girl within their classroom for each role. Item scores were standardized within sex and within classroom to adjust for class size and participation rates as well as possible gender stereotyping. Five subscales have been identified through factor analysis of nominations for the 31 roles (i.e., Popular-Sociable, Prosocial, Aggressive, Rejected-Victimized, and Shy-Withdrawn). The subscales demonstrate adequate reliability and validity when used with samples of school-aged children (Rubin et al., 2006). The current study focused on the rejection/victimization subscale, which is derived from 8 roles (e.g., “someone who has mean things said to them”, “someone who has trouble making friends”). Tallies of nominations received from classmates for each role were standardized (M = 0; SD = 1) within sex in each class to adjust for unequal class size and participation rates as well as to eliminate possible gender stereotyping. The resulting scores reflect nominations relative to same-sex peers.
Reciprocated friendship.
Reciprocated friendship was measured by having participants and their classmates provide nominations for their three “best friends” in the class (Bukowski, Hoza, & Boivin, 1994). A reciprocated friendship reflects instances in which two children mutually nominated each other as a “best friend”; thus, reciprocated friendship scores could range from 0 to 3, with 0 being no reciprocated friendships and 3 meaning that all three nominated “best friends” were reciprocated friendships. For the purpose of the analyses in the current study, children were classified as either having at least one reciprocated friendship or having no reciprocated friendships in the classroom (i.e., the variable was dichotomized).
Data Analysis
All data analyses were conducted using IBM SPSS, Version 24. Moderated mediation analyses were conducted using the SPSS PROCESS macro versions 2 (Hayes, 2012) and 3 (Hayes, 2017). SPSS PROCESS macro version 2 was used to analyze the reciprocated friendship data, because version 3 does not permit analyses of dichotomous dependent variables. Separate path models were tested for each peer outcome (i.e., rejection/victimization or reciprocated friendship). The following effects were examined: direct effects of TBI on ToM, TBI on peer relationship variables, and ToM on peer relationship variables; indirect effect of TBI on peer relationships variables as mediated by ToM; the moderating effect of parental nurturance on (a) the relation between TBI and peer relationship variables, and (b) the relations between ToM and peer relationship variables. The significance of the overall model also was assessed.
In this model, the moderation of both the direct and indirect effects of TBI on peer relationships was tested. Moderation of the indirect effect, known as moderated mediation, means that the indirect effect is conditional and, thus, differs in size and strength as a function of the moderator (i.e., parental nurturance). We used the index of moderated mediation to test for the significance of these effects (Hayes, 2015). The recommended 5000 bootstrap sample was used for estimation. Effects were considered statistically significant if the 90% confidence interval did not contain zero, because our hypotheses were directional (i.e., one-tailed).
Prior to analyses, all continuous predictors were grand mean-centered for interpretability. Age at assessment was treated as a covariate in the model, as ToM emerges early in childhood and continues to develop through late childhood and into mid-adolescence (Wellman et al., 2001; Sodian, 2011). Because epidemiological studies indicate the risk of TBI is highest for children of lower SES and minority status (Langlois, Rutland-Brown, & Thomas, 2005), SES was not treated as a covariate in data analyses, given that the SES differences appeared to be intrinsic to the injury groups. When a covariate is an attribute of a disorder, or is intrinsic to the condition, correcting for differences can be potentially misleading. For similar reasons, IQ was not treated as a covariate in primary data analyses, as it is associated with injury severity. Group differences in IQ cannot be separated from the effects of a TBI (Dennis et al., 2009). Group differences among demographic and injury characteristics were examined using analysis of variance (ANOVA) and chi-square for continuous and categorical variables, respectively.
Results
Demographics and Injury Characteristics
Demographic and injury characteristics for the three injury groups are summarized in Table 1. The groups did not differ in sex, race, age at injury, age at assessment, or time from injury to assessment. The groups differed significantly in Full Scale IQ and SES, with the severe TBI group having the lowest mean IQ and SES. The groups also differed on the distribution of mechanism of injury, χ2 (4) = 18.76, p = .001, with injuries arising from motorized vehicles being most common among the severe TBI group (62% for severe TBI, 31% for complicated mild/moderate TBI, 6% for OI) and those arising during sports and recreational events being most common among the OI group (23% for severe TBI, 41% for mild/moderate TBI, 75% for OI).
Table 1.
Group demographics and injury characteristics
| Group | ||||||
|---|---|---|---|---|---|---|
| OI (n =32) | Mild/Moderate TBI (n = 39) | Severe TBI (n= 13) | ||||
| n | % | n | % | n | % | |
| Sex (male) | 20 | 62.5 | 25 | 64.1 | 7 | 53.8 |
| Racea | ||||||
| White | 29 | 90.6 | 33 | 84.6 | 8 | 61.5 |
| Black | 0 | 0.0 | 1 | 2.6 | 2 | 15.4 |
| Multiracial | 2 | 6.3 | 3 | 7.7 | 0 | 0.0 |
| M | SD | M | SD | M | SD | |
| Age at injury (years) | 7.84 | 1.97 | 8.10 | 1.84 | 7.24 | 2.28 |
| Age at assessment (years) | 10.57 | 1.62 | 10.57 | 1.31 | 9.81 | 1.47 |
| Time from injury to assessment (years) | 2.73 | 1.07 | 2.47 | 1.21 | 2.57 | 1.20 |
| SES composite standard score* | 0.44 | 0.94 | −0.08 | 1.07 | −0.60 | 0.49 |
| Full-Scale IQb * | 112.25 | 12.74 | 99.33 | 14.59 | 91.54 | 12.66 |
| Lowest Glasgow Coma Sale score* | 14.03 | 1.68 | 3.85 | 1.86 | ||
Note. OI = orthopedic injury; TBI = traumatic brain injury; SES = socioeconomic status.
Race was not available for 9 participants.
IQ measured using the two-subtest version of Wechsler Abbreviated Scale of Intelligence.
Groups differ significantly, p < .05.
Peer Relationships
Rejection/Victimization.
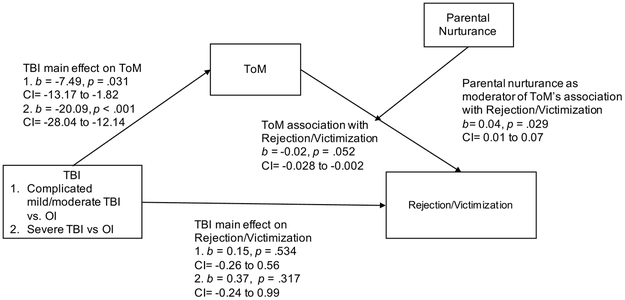
Average within group correlations between study measures are presented in Table 2. The results of the moderated-mediation analysis for peer rejection/victimization indicate that the overall model accounted for a significant proportion of variance (R2 = 19.05%), F(8,75) = 2.21, p = .036. Moderated-mediation was significant, such that parental nurturance moderated the relation between ToM and peer rejection/victimization, F (1,75)= 4.70, p = .033, and accounted for 5.08% of the variance in the model. However, parental nurturance did not moderate the direct effect of injury on peer rejection/victimization, F(2,75) = .085, p = .919. The model was therefore re-estimated to test the more parsimonious model presented in Figure 2 (i.e., restricting the moderating effect of parental nurturance to the relation between ToM and peer rejection/victimization).
Table 2.
Average within group correlations between study measures.
| CRPR Nurturance | Rejection/Victimization | Reciprocated Friendship | ||||
|---|---|---|---|---|---|---|
| r | p | r | p | r | p | |
| ToM | −.038 | .733 | −.172 | .120 | .099 | .373 |
| CRPR Nurturance | - | - | −.097 | .383 | −.091 | .413 |
| Rejection/Victimization | - | - | - | - | −.269* | .014 |
| Reciprocated Friendship | - | - | - | - | - | - |
Note. CRPR = Child Rearing Practices Report Questionnaire
Significant correlation, p < .05.
Figure 2.
Moderated-mediation model depicting the relationship between TBI and peer rejection/victimization, as mediated by ToM and moderated by parental nurturance. Age at injury was treated as a covariate in the model (ToM: t = 5.39, p < .001; Rejection/Victimization: t = 0.48, p = 0.63). ‘1’ indicates values for mild/moderate TBI and ‘2’ indicates values for severe TBI.
Overall, the re-estimated model accounted for a significant proportion of variance (R2 =18.87%) in peer rejection/victimization, F(6,77) = 2.98, p = .011. Both TBI groups differed significantly from the OI group on ToM (OI M = 67.29, SD = 14.58; mild/moderate TBI M = 59.78, SD = 17.52; severe TBI M = 42.75, SD = 18.40). The index of moderated mediation was significant for both the complicated mild/moderate TBI group (b = −.30, CI90 = −.759 to −0.001) and the severe TBI group (b = −.80, CI90 = −1.60 to −.07), such that parental nurturance moderated the mediating effect of ToM on peer rejection/victimization. Moderated mediation accounted for 5.25% of the variance in the model, F(1,77) = 5.00, p = .029. The moderated-mediation model is presented in Figure 2, and relative conditional indirect effects are summarized in Table 3 . At low (i.e., one standard deviation below the overall sample mean) and average levels of parental nurturance, ToM significantly mediated the relation between injury and peer rejection/victimization; however, at high levels of parental nurturance (i.e., one standard deviation above the overall sample mean), ToM no longer mediated this relation. In other words, lower ToM predicted greater peer victimization at low and average levels of parental nurturance, but not at high levels. No significant direct effects of TBI on peer rejection/victimization were observed when moderated-mediation was taken into account in the model, F(2,77) = .52, p = .59.
Table 3.
Relative conditional indirect effects of complicated mild/moderate and severe TBI on peer rejection/victimization via ToM.
| Parental nurturance (Percentile) |
Indirect Effect | SE | LLCI90 | ULCI90 |
|---|---|---|---|---|
| Complicated Mild/Moderate TBI vs. OI | ||||
| 16th | .239 | .171 | .018 | .560 |
| 50th | .117 | .084 | .007 | .275 |
| 84th | −.006 | .068 | −.125 | .099 |
| Severe TBI vs.OI | ||||
| 16th | .641 | .339 | .128 | 1.229 |
| 50th | .313 | .182 | .052 | .641 |
| 84th | −.015 | .165 | −.259 | .266 |
Note. OI = orthopedic injury; TBI = traumatic brain injury; ToM = Theory of Mind
Reciprocated Friendship.
No significant moderated-mediation was observed for reciprocated friendship for either complicated mild/moderate TBI (b = .093, CI90 = −.43 to 1.03) or severe TBI (b = .014, CI90 = −2.86 to 2.16). The role of parental nurturance as a moderator of the association between ToM and reciprocated friendship was dropped from the model, and the model was re-estimated to investigate whether ToM mediated the relation between injury and reciprocated friendship for either TBI group. ToM did not mediate the relation between injury and reciprocated friendships for either complicated mild/moderate TBI vs. OI (b = −.15, CI90 = −.57 to .041) or severe TBI vs. OI (b = −.43, CI90 = −1.21 to .22). Relative to children with OI, severe TBI was associated with a lower likelihood of having a reciprocated friendship (b = −1.92, CI90 = −3.30 to −.54), but this was not true for complicated mild/moderate TBI (b = −.44, CI90 = −1.57 to .69). Additionally, severe TBI was associated with lower ToM scores (b = −18.48, CI90 = −26.25 to −10.69) but complicated mild/moderate TBI was not.
Discussion
The aim of the current study was to examine how ToM and parental nurturance jointly predict peer relationships (i.e., peer rejection/victimization and reciprocated friendship) in children with TBI. The results demonstrate how individual (i.e., ToM) and environmental (i.e., parenting) characteristics interact in their associations with peer relationships after childhood TBI. Our hypotheses were partially supported, as we found that ToM mediated the relation between injury and peer victimization and that parental nurturance moderated this relation for both complicated mild/moderate and severe TBI. More specifically, lower ToM predicted greater peer victimization at low and average levels of parental nurturance, but not at high levels. Contrary to our hypotheses, we found that ToM did not mediate the relation betwen injury and reciprocated friendship, nor did parental nurturance moderate this relation. However, we did find that severe TBI was associated with fewer reciprocated friendships and lower ToM scores.
Peer Rejection/victimization
Our results suggest that high parental nurturance may act as an important buffer of the negative effects of TBI on peer rejection/victimization, in part by moderating the association between ToM and peer rejection/vicitimization. This result is consistent with previous research that has examined the role of parenting in the development of children with TBI (Wade et al., 2011; Yeates et al., 2010). For example, Wade and colleagues (2011) found that parenting quality may foster or impede behavioural recovery following TBI in young children. More specifically, they showed that parental warm responsiveness was associated with lower levels of internalizing and externalizing behaviour, particularly in children with severe TBI. Similarly, Root and colleagues (2016) found a moderating effect of parenting on the relation between TBI and peer victimization, such that mothers who reported higher levels of parental nurturance had children who were rated lower on peer rejection/victimization. However, Root and colleagues (2016) did not include ToM as a mediator in their model, and they used socially typical children rather than children with OI as their comparison sample. In our analysis, parental nurturance did not moderate the direct relationship of TBI to peer rejection/victimization when ToM was taken into account as a mediator, but instead moderated the relation between ToM and rejection/victimization.
Our finding that lower ToM predicted greater peer victimization at low and average levels of parental nurturance, but not at high levels of nurturing parenting, is consistent with research on the importance of parenting in influencing patterns of social information processing in healthy children. Nurturing, non-harsh parenting is associated with more adaptive social cognitive processes for peer conflicts in children with a history of physical abuse (Haskett & Willoughby, 2007). Warm, sensitive, and responsive parenting is also important for facilitating ToM development in healthy children (Yan-Yan & Biao, 2006). Children whose mothers react to peer conflict by engaging in affective perspective taking (e.g., “why do you think the child is picking on you?”) performed better on ToM tasks than mothers who did not use this strategy (Farrant et al., 2012). In our study, children whose parents reported low and average levels of nurturance may have been more vulnerable to the detrimental effects of TBI on ToM, and subsequently at greater risk for peer rejection/victimization than children whose parents reported high levels of nurturance.
Notably, our overall model accounted for approximately 19% of the variance in peer rejection/victimization, representing a medium to large effect by conventional definition. Nevertheless, much variance remains unexplained, and future research on other factors that may predict rejection/victimization after TBI is warranted. For example, behavioural ratings of executive functioning have been found to be associated with social competence following TBI (Ganesalingam et al., 2011).
Reciprocated Friendship
In the current study, ToM did not mediate, and parental nurturance did not moderate, the relation between TBI and reciprocated friendship. However, children with severe TBI were found to have a decreased likelihood of having reciprocated friendship in their classroom compared to OI controls. In addition to being sources of emotional and social support, friendships enable children to learn about behavioural and emotional norms, and are thus crucial elements of child development (Newcomb and Bagwell, 1995). Studies in non-injured children have shown that having at least one reciprocated friendship is important for positive adjustment (Kingery, Erdley and Marshall, 2011; Wojslawowicz Bowker et al., 2006). One possible explanation for why ToM did not mediate the outcome of reciprocated friendship is that this study only examined whether children had at least one reciprocated friendship, and thus did not consider the quality of friendships. Children with better ToM may be able to maintain higher quality friendships (Heverly-Fitt et al., 2014). Previous research has shown that high quality friendships are associated with better psychosocial adjustment in children with TBI, as well as non-injured children (Malcolm et al., 2006; Nangle et al., 2003). Furthermore, by dichotomizing friendship, we reduced variability in our outcome measure. A possible alternative explanation is that factors other than ToM, such as emotional and behavioural regulation, might better account for why children with TBI are less likely to have a reciprocated friendship (Ross et al., 2011).
Strengths and Limitations
The current study has a number of strengths. A variety of informants (e.g., injured children, parents, classmates) were used for key measures (ToM, parental nurturance, peer relationships) to reduce shared rater variance. The study used classroom measures to assess reciprocated friendship and peer victimization, a method that has been widely used by developmental researchers and has been successfully applied with multiple pediatric illness populations (Yeates et al., 2013). This method of data collection enables a more direct measurement of peer relations as compared to adult reports of children’s peer functioning. Furthermore, we obtained a comprehensive assessment of ToM using measures assessing cognitive, affective and conative ToM (Dennis et al., 2013).
The study also had several limitations. The sample size was relatively small, especially in the severe TBI group. Regrettably, classroom data could not be obtained for all children in the larger parent study. Children with and without classroom data did not differ on demographic or injury characteristics, but the small sample size did reduce statistical power, particularly with respect to the dichotomized reciprocated friendship variable. Another limitation is that information on pre-injury peer relationships was not available, because the study was conducted at least 1-year post-injury and retrospective ratings are vulnerable to recall bias. Further, the assessment of parental nurturance was based on a self-report questionnaire. Future research should include additional methods of measuring parenting style, such as direct observations of parent-child interactions. Additionally, we obtained ratings of parental nurturance primarily from mothers, with the remainder provided by fathers or alternate caregivers. Research in typically developing children has shown that fathers play a unique role in their children’s socio-emotional development (Brand and Klimes-Dougan, 2010). For example, in response to their child’s expression of fear or sadness, fathers are more likely than mothers to use dismissive strategies (Klimes-Dougan et al., 2007). Additionally, fathers can act as a buffer between negative maternal behaviours and poor child outcomes (Mezulis, Hyde, & Clark, 2004). Future research is needed to investigate whether paternal and maternal parenting styles differentially affect child social outcomes after TBI. Finally, another limitation to this study was the dichotomization of reciprocated friendship. Future research should investigate whether friendship quality is affected by ToM and parenting style after pediatric TBI.
Conclusions and Clinical Implications
The current findings indicate that high levels of parental nurturance play a protective role in buffering against the negative effects of TBI-related deficits in ToM on peer rejection/victimization. In contrast, at low and average levels of parental nurturance, lower ToM predicted greater peer rejection/victimization for children with both complicated mild/moderate and severe TBI. Thus, interventions designed to increase children’s ToM or parental nurturance may prove beneficial for children with TBI, and clinical trials of such interventions are an important area for future research. ToM did not mediate the effects of TBI on reciprocated friendship, and parental nurturance did not moderate the association of ToM with friendship; however, the finding that children with severe TBI had a decreased likelihood of having at least one reciprocated friendship has significant implications for social adjustment after TBI and suggests a need for future research to elucidate the mechanisms underlying this outcome.
Acknowledgements
We have no conflicts of interest to declare. This work was supported by the National Institute of Child Health and Human Development (Grant 5 R01 HD048946). Keith Yeates is supported by the Ronald and Irene Ward Chair in Pediatric Brain Injury. Preparation of this manuscript was supported by an Alberta Innovates Graduate Studentship to Ms. Deighton and Ms. Laliberte Durish; and a Canadian Institute of Health Research Doctoral Award to Ms. Laliberte Durish.
References
- Anderson V, & Beauchamp MH (2012). Developmental social neuroscience and childhood brain insult: Theory and practice. New York, NY: Guilford Press; Retrieved from https://ebookcentral-proquest-com.ezproxy.lib.ucalgary.ca [Google Scholar]
- Booth-Laforce C, Oh W, Kim AH, Rubin KH, Rose-Krasnor L, & Burgess K (2006). Attachment, self-worth, and peer-group functioning in middle childhood. Attachment & Human Development, 8(4), 309–325. doi: 10.1080/14616730601048209 [DOI] [PubMed] [Google Scholar]
- Brand AE, & Klimes-Dougan B (2010). Emotion socialization in adolescence: The roles of mothers and fathers. New Directions for Child and Adolescent Development, 2010(128), 85–100. doi: 10.1002/cd.270 [DOI] [PubMed] [Google Scholar]
- Brophy-Herb HE, Schiffman RF, Bocknek EL, Dupuis SB, Fitzgerald HE, Horodynski M, … & Hillaker B (2011). Toddlers' social-emotional competence in the contexts of maternal emotion socialization and contingent responsiveness in a low-income. Social Development, 20(1), 73–92. doi: 10.1111/j.1467-9507.2009.00570.x [DOI] [Google Scholar]
- Bukowski WM, Hoza B, & Boivin M (1994). Measuring friendship quality during pre-and early adolescence: The development and psychometric properties of the Friendship Qualities Scale. Journal of Social and Personal Relationships, 11(3), 471–484. doi: 10.1177/0265407594113011 [DOI] [Google Scholar]
- Dennis M, Simic N, Bigler ED, Abildskov T, Agostino A, Taylor HG, … & Yeates KO (2013). Cognitive, affective, and conative theory of mind (ToM) in children with traumatic brain injury. Developmental Cognitive Neuroscience, 5, 25–39. doi: 10.1016/j.dcn.2012.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis M, Francis DJ, Cirino PT, Schachar R, Barnes MA, & Fletcher JM (2009). Why IQ is not a covariate in cognitive studies of neurodevelopmental disorders. Journal of the International Neuropsychological Society : JINS, 15(3), 331–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis M, Barnes MA, Wilkinson M, & Humphreys RP (1998). How children with head injury represent real and deceptive emotion in short narratives. Brain and Language, 61(3), 450–483. doi: 10.1006/brln.1997.1886 [DOI] [PubMed] [Google Scholar]
- Dennis M, Purvis K, Barnes MA, Wilkinson M, & Winner E (2001). Understanding of literal truth, ironic criticism, and deceptive praise following childhood head injury. Brain and Language, 78(1), 1–16. doi: 10.1006/brln.2000.2431 [DOI] [PubMed] [Google Scholar]
- Farrant BM, Devine TA, Maybery MT, & Fletcher J (2012). Empathy, perspective taking and prosocial behaviour: The importance of parenting practices. Infant and Child Development, 21(2), 175–188. 10.1002/icd.740 [DOI] [Google Scholar]
- Ganesalingam K, Yeates KO, Taylor HG, Walz NC, Stancin T, and Wade S (2011). Executive functions and social competence in young children 6 months following traumatic brain injury. Neuropsychology, 25, 466–476. doi: 10.1037/a0022768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haskett ME, & Willoughby M (2007). Paths to child social adjustment: Parenting quality and children’s processing of social information. Child: Care, Health and Development, 55(1), 67–77. doi: 10.1111/j.1365-2214.2006.00627.x [DOI] [PubMed] [Google Scholar]
- Hayes AF (2012). PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling [White paper]. Retrieved from http://www.afhayes.com/public/process2012.pdf [Google Scholar]
- Hayes AF (2015). An index and test of linear moderated mediation. Multivariate Behavioral Research, 50, 1–22. doi: 10.1080/00273171.2014.962683 [DOI] [PubMed] [Google Scholar]
- Hayes AF (2017). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York. NY: Guilford Publications. [Google Scholar]
- Heverly-Fitt S, Wimsatt MA, Menzer MM, Rubin KH, Dennis M, Taylor HG, Stancin T, Gerhardt CA, Vannatta K, Bigler ED, & Yeates KO (2014). Friendship quality and psychosocial outcomes among children with traumatic brain injury. Journal of the International Neuropsychological Society, 20, 684–693. doi: 10.1017/S1355617714000393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hung AH, Cassedy A, Schultz HM, Yeates KO, Taylor HG, Stancin T, … & Wade SL (2017). Predictors of long-term victimization after early pediatric traumatic brain injury. Journal of Developmental and Behavioral Pediatrics, 38(1), 49–57. doi: 10.1097/DBP.0000000000000366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashluba S, Hanks RA, Casey JE, & Mills SR (2008). Neuropsychologic and functional outcome after complicated mild traumatic brain injury. Archives of Physical Medicine and Rehabilitation, 89(5), 904–911. [DOI] [PubMed] [Google Scholar]
- Kingery JN, & Erdley CA, & Marshall K,C (2011) Peer acceptance and friendship as predictors of early adolescents’ adjustment across the middle school transition. Merrill-Paimer Quarterly, 57(3), 215–243. [Google Scholar]
- Klimes-Dougan B, Brand AE, Zahn-Waxler C, Usher B, Hastings PD, Kendziora K, & Garside RB (2007). Parental emotion socialization in adolescence: Differences in sex, age and problem status. Social Development, 16(2), 326–342. [Google Scholar]
- Ladd GW, & Burgess KB (2001). Do relational risks and protective factors moderate the linkages between childhood aggression and early psychological and school adjustment? Child Development, 72(5), 1579–1601. doi: / 10.1111/1467-8624.00366 [DOI] [PubMed] [Google Scholar]
- Ladd GW, & Ladd BK (1998). Parenting behaviors and parent-child relationships: Correlates of peer victimization in kindergarten? Developmental Psychology, 34(6), 1450. [DOI] [PubMed] [Google Scholar]
- Langlois JA, Rutland-Brown W, & Thomas KE (2005). The incidence of traumatic brain injury among children in the United States: differences by race. Journal of Head Trauma Rehabilitation, 20(3), 229–238. [DOI] [PubMed] [Google Scholar]
- Malcolm KT, Jensen-Campbell LA, Rex-Lear M, Waldrip AM (2006) Divided we fall: Children’s friendships and peer victimization. Journal of Social and Personal Relationships, 23, 721–740. doi: / 10.1177/0265407506068260 [DOI] [Google Scholar]
- Masten AS, Morison P, & Pellegrini DS (1985). A revised class play method of peer assessment. Developmental Psychology, 21(3), 523. doi: / 10.1207/s15374424jccp2601_7 [DOI] [Google Scholar]
- Mezulis AH, Hyde JS, & Clark R (2004). Father involvement moderates the effect of maternal depression during a child's infancy on child behavior problems in kindergarten. Journal of Family Psychology, 18(4), 575. [DOI] [PubMed] [Google Scholar]
- Nangle DW, Erdley CA, Newman JE, Mason CA, & Carpenter EM (2003). Popularity, friendship quantity, and friendship quality: Interactive influences on children's loneliness and depression. Journal of Clinical Child and Adolescent Psychology, 32(4), 546–555. doi: / 10.1207/S15374424JCCP3204_7 [DOI] [PubMed] [Google Scholar]
- Newcomb AF, & Bagwell CL (1995) Children’s friendship relations: A meta-analytic review. Psychological Bulletin, 117, 306–347. doi: 10.1037//0033-2909.117.2.306 [DOI] [Google Scholar]
- Park JH, Essex MJ, Zahn-Waxler C, Armstrong JM, Klein MH, & Goldsmith HH (2005). Relational and overt aggression in middle childhood: Early child and family risk factors. Early Education & Development, 16(2), 233–258. doi: / 10.1080/10409289.2005.10472869 [DOI] [Google Scholar]
- Potter JL, Wade SL, Walz NC, Cassedy A, Stevens MH, Yeates KO, & Taylor HG (2011). Parenting style is related to executive dysfunction after brain injury in children. Rehabilitation Psychology, 56(4), 351. doi: / 10.1037/a0025445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rickel AU, & Biasatti LL (1982). Modification of the block child rearing practices report. Journal of Clinical Psychology, 35(1), 129–134. [Google Scholar]
- Robinson KE, Fountain-Zaragoza S, Dennis M, Taylor HG, Bigler ED, Rubin K, … & Yeates KO (2014). Executive functions and theory of mind as predictors of social adjustment in childhood traumatic brain injury. Journal of Neurotrauma, 31(22), 1835–1842. doi: / 10.1089/neu.2014.3422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Root AE, Wimsatt M, Rubin KH, Bigler ED, Dennis M, Gerhardt CA, … & Yeates KO (2016). Children with traumatic brain injury: Associations between parenting and social adjustment. Journal of Applied Developmental Psychology, 42, 1–7. doi: / 10.1016/j.appdev.2015.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosema S, Crowe L, & Anderson V (2012). Social function in children and adolescents after traumatic brain injury: A systematic review 1989–2011. Journal of Neurotrauma, 29(7), 1277–1291. doi: / 10.1089/neu.2011.2144 [DOI] [PubMed] [Google Scholar]
- Ross KA, McMillan T, Kelly T, Sumpter R, & Dorris L (2011). Friendship, loneliness and psychosocial functioning in children with traumatic brain injury. Brain Injury, 25(12), 1206–1211. doi: / 10.3109/02699052.2011.609519 [DOI] [PubMed] [Google Scholar]
- Rubin KH, Bukowski WM, & Bowker JC (2015). Children in peer groups In Lerner RM, Bornstein MH, & Leventhal T (Eds.), Handbook of child psychology and developmental science (pp. 175–222). Hoboken, New Jersey: John Wiley & Sons Inc. [Google Scholar]
- Rubin KH, Wojslawowicz JC, Rose-Krasnor L, Booth-LaForce C, & Burgess KB (2006). The best friendships of shy/withdrawn children: Prevalence, stability, and relationship quality. Journal of Abnormal Child Psychology, 34(2), 139–153. doi: / 10.1007/s10802-005-9017-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan NP, Catroppa C, Beare R, Silk TJ, Crossley L, Beauchamp MH, … & Anderson VA (2016). Theory of mind mediates the prospective relationship between abnormal social brain network morphology and chronic behavior problems after pediatric traumatic brain injury. Social Cognitive and Affective Neuroscience, 11(4), 683–692. doi: / 10.1093/scan/nsw007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneier AJ, Shields BJ, Hostetler SG, Xiang H, & Smith GA (2006). Incidence of pediatric traumatic brain injury and associated hospital resource utilization in the United States. Pediatrics, 118(2), 483–492. doi: / 10.1542/peds.2005-2588 [DOI] [PubMed] [Google Scholar]
- Schwartz L, Taylor HG, Drotar D, Yeates KO, Wade SL, & Stancin T (2003). Longterm behavior problems following pediatric traumatic brain injury: prevalence, predictors, and correlates. Journal of Pediatric Psychology, 28(4), 251–263. doi: / 10.1093/jpepsy/jsg013 [DOI] [PubMed] [Google Scholar]
- Sodian B (2011). Theory of mind in infancy. Child Development Perspectives, 5(1), 39–43. doi: / 10.1111/j.1750-8606.2010.00152.x [DOI] [Google Scholar]
- Teasdale G, & Jennett B (1974). Assessment of coma and impaired consciousness. A practical scale. Lancet, 2(7872), 81–84. doi: / 10.1016/S0140-6736(74)91639-0 [DOI] [PubMed] [Google Scholar]
- Wade SL, Cassedy A, Walz NC, Taylor HG, Stancin T, & Yeates KO (2011). The relationship of parental warm responsiveness and negativity to emerging behavior problems following traumatic brain injury in young children. Developmental psychology, 47(1), 119. doi: / 10.1037/a0021028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D Wechsler Abbreviated Scale of Intelligence (WASI). 1999. USA, Psychological Corporation. [Google Scholar]
- Wellman HM, Cross D, Watson J (2001). Meta analysis of theory of mind development: the truth about false belief. Child Development, 72(3), 655–84. doi: / 10.1111/1467-8624.00304 [DOI] [PubMed] [Google Scholar]
- Wolfe KR, Bigler ED, Dennis M, Gerhardt CA, Rubin K, Taylor HG, … & Yeates KO (2014). Self-awareness of peer-rated social attributes in children with traumatic brain injury. Journal of pediatric psychology, 40(3), 272–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wojslawowicz Bowker JC, Rubin KH, Booth-LaForce C, Rose-Krasnor L (2006) Behavioral characteristics associated with stable and fluid best friendship patterns in middle childhood. Merrill-Palmer Quarterly, 52, 671–693. doi: / 10.1353/mpq.2006.0000 [DOI] [Google Scholar]
- Yan-Yan L, & Biao S (2006). Mothers’ parenting style and the development of children’s theory of mind. Chinese Mental Health Journal, 20(1), 5–9. [Google Scholar]
- Yeates KO, Bigler ED, Dennis M, Gerhardt CA, Rubin KH, Stancin T, … & Vannatta K (2007). Social outcomes in childhood brain disorder: a heuristic integration of social neuroscience and developmental psychology. Psychological Bulletin, 133(3), 535. doi: / 10.1037/0033-2909.133.3.535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeates KO, Bigler ED, Abildskov T, Dennis M, Gerhardt CA, Vannatta K, … & Taylor HG (2014). Social competence in pediatric traumatic brain injury: From brain to behavior. Clinical Psychological Science, 2(1), 97–107. doi: / 10.1177/2167702613499734 [DOI] [Google Scholar]
- Yeates KO, Gerhardt CA, Bigler ED, Abildskov T, Dennis M, Rubin KH, … & Vannatta K (2013). Peer relationships of children with traumatic brain injury. Journal of the International Neuropsychological Society, 19(5), 518–527. doi: / 10.1017/S1355617712001531 [DOI] [PubMed] [Google Scholar]
- Yeates KO, Taylor HG, Walz NC, Stancin T, & Wade SL (2010). The family environment as a moderator of psychosocial outcomes following traumatic brain injury in young children. Neuropsychology, 24(3), 345. doi: / 10.1037/a0018387 [DOI] [PMC free article] [PubMed] [Google Scholar]