Abstract
Purpose
The myeloproliferative neoplasms (MPNs), including Polycythemia Vera (PV), Essential Thrombocythemia (ET), and Primary Myelofibrosis (PMF), are characterized by the expansion of the erythroid, megakaryocytic, and granulocytic lineages. A common feature of these disorders is the presence of abnormal megakaryocytes, which have been implicated as causative agents in the development of bone marrow fibrosis. However, the specific contributions of megakaryocytes to MPN pathogenesis remain unclear.
Experimental Design
We used Pf4-Cre transgenic mice to drive expression of JAK2V617F in megakaryocyte lineage-committed hematopoietic cells. We also assessed the critical role of mutant megakaryocytes in MPN maintenance through cell ablation studies in JAK2V617F and MPLW515L BMT models of MPN.
Results
JAK2V617F-mutant presence in megakaryocytes was sufficient to induce enhanced erythropoiesis and promote fibrosis, which leads to a myeloproliferative state with expansion of mutant and non-mutant hematopoietic cells. The increased erythropoiesis was associated with elevated interleukin-6 level, which was also required for aberrant erythropoiesis in vivo. Furthermore, depletion of megakaryocytes in the JAK2V617F and MPLW515L BMT models ameliorated polycythemia and leukocytosis in addition to expected effects on megakaryopoiesis.
Conclusions
Our observations reveal that JAK/STAT pathway activation in megakaryocytes induces myeloproliferation and is necessary for MPN maintenance in vivo. These observations indicate that MPN clone can influence the behavior of the wild type hematopoietic milieu, at least in part via altered production of pro-inflammatory cytokines and chemokines. Our findings resonate with patients who present with a clinical MPN and a low JAK2V617F allele burden, and support the development of MPN therapies aimed at targeting megakaryocytes.
Keywords: Hematological malignancies, Leukemia, Myeloproliferative neoplasms, Megakaryocytes, JAK2
Introduction
The MPNs are clonal hematopoietic stem cell (HSC) disorders characterized by the expansion of mature myeloid elements. The most common genetic alteration is JAK2V617F, which is found in > 95% of all patients with PV, and in 50–60% of ET/PMF cases (1–4). Expression of this mutation in cell lines causes transformation to cytokine-independent growth and constitutive activation of downstream STAT signaling (2,3), and expression of JAK2V617F in the hematopoietic compartment is sufficient to cause MPN in mouse models (5–8). These observations, along with gene expression studies in primary patient samples (9), establish aberrant JAK/STAT signaling as a central molecular hallmark of MPN pathogenesis. Clonality studies using MPN patient samples have traced driver mutations, including JAK2V617F, to the HSC compartment, regardless of clinical phenotype (10). Furthermore, JAK2V617F can be detected across the hematopoietic ontogeny (11,12). This implies that JAK2V617F can have differential effects on discrete cell types, such as progenitor cells versus mature lineage-committed cells (13). However, most studies performed to date have investigated the effects of JAK2V617F when expressed throughout hematopoiesis.
We initiated this study to explore the contributions of mutant megakaryocytes to MPN pathogenesis. In many ET/PMF patients, JAK2V617F manifests primarily in the megakaryocyte (Mk) lineage, with less significant involvement of erythroid and myeloid cells as determined by mutant allele burden profiling (14) of specific hematopoietic subsets. Furthermore, aberrant megakaryopoiesis is a pathological hallmark of MPN, regardless of clinical subtype (15). These abnormal megakaryocytes are known to secrete increased levels of pro-inflammatory cytokines and other factors (such as TGF-β), which presumably contribute to various MPN-related pathologies, such as bone marrow fibrosis (16,17). Megakaryocytes are also regulators of HSC quiescence (18,19), and we previously revealed that Jak2-deficient Mks negatively regulate stem/progenitor cell expansion in vivo (20). These observations raise the possibility that JAK2V617F-mutant Mks promote MPN pathogenesis, at least in part, by influencing the biology of non-clonal (JAK2 wild type) cells. Indeed, earlier work has revealed that Jak2V617F-mutant megakaryocytes promote hyper-proliferation of the stem/progenitor cell pool via the TPO/MPL signaling axis (21,22). However, it remains unclear if Jak2V617F-mutant megakaryocytes can affect non-clonal hematopoietic cells, how they mediate these effects, and if Jak2V617F-mutant megakaryocytes are required for maintenance of the disease state.
To this end, we crossed a conditional Jak2V617F knock-in mouse where mutant Jak2 is expressed from the endogenous murine locus, with Pf4-Cre transgenic mice to produce a model wherein Jak2V617F is expressed specifically in megakaryocyte lineage-committed cells (13,23). While steady-state megakaryopoiesis was significantly elevated as expected, we unexpectedly observed that Jak2-mutant Mks/platelets significantly increased steady-state erythropoiesis and were capable of initiating a myeloproliferative disorder through cell non-autonomous mechanisms.
Materials and Methods
Mouse lines and breeding
All mice used in this study were on the C57BL/6 background. Floxed heterozygous Jak V617F/+ knock-in animals (a gift of Dr. Ann Mullally (13)) were bred with Pf4-Cre transgenic mice (a gift of Dr. Radek Skoda(23)) to induce Jak2V617F expression in megakaryocyte lineage-committed cells. Vav-Cre (Stock# 008610) and Mx1-Cre (Stock# 003556) transgenic mice were purchased from Jackson Laboratory (Bar Harbor, ME) and bred with Jak2V617F/+ mice to induce pan-hematopoietic Jak2V617F expression. For megakaryocyte depletion studies, iDTR mice (which harbor a conditional Cre-inducible diphtheria toxin receptor (DTR) (24)) were obtained from Jackson Laboratory (Stock# 007900) and crossed to Pf4-Cre+ mice. For lineage tracing studies, mTmG Cre switch reporter mice (25) were obtained from Jackson Laboratory (Stock# 007676) and bred to Jak2V617F/+; Pf4-Cre+ mice to confirm lineage-specific Cre expression. Animal studies were approved by the IACUC of both Northwestern University and Memorial Sloan Kettering Cancer Center.
Antibodies and reagents
Antibodies used to characterize mouse cell surface makers by flow cytometry include: mouse PE/Cy7-CD41 (Cat# 25–0411-80) and APC-Gr1 (Cat# 17–5931-82) were purchased from eBioscience. Mouse PE-CD42b antibody (Cat# M040–3) was purchased from Emfret Analytics (Wurzburg, Germany). Antibodies for mouse APC-Ter119 (Cat# 116211), PE/Cy7-CD71 (Cat# 113811), FITC-Mac1 (Cat# 101205), APC/Cy7-cKit (Cat# 105825), FITC-Sca1 (Cat# 108105), PerCP/Cy5.5-FcγR (Cat# 101323), PE-CD150 (Cat# 115903), APC-CD105 (Cat# 120413) and PE-CD34 (Cat# 128609) were purchased from BioLegend (San Diego, CA). PE-Phospho-Stat5 (Cat# 5387) antibody was purchased from Cell Signaling (Danvers, MA). Rabbit polyclonal Von Willebrand Factor (VWF) antibody (Cat# A008229–5) used for immunohistochemistry was purchased from Agilent Technologies (Santa Clara, CA). Recombinant mouse stem cell factor (mSCF, Cat# 250–03), recombinant human EPO (hEPO, Cat# 100–64), recombinant mouse IL-3 (mIL-3, Cat# 213–13), recombinant human TPO (hTPO, Cat# 300–18), recombinant mouse Cxcl1 (mCxcl1, Cat# 250–01), and recombinant mouse Cxcl2 (mCxcl2, Cat# 250–15) were purchased from Peprotech (Rocky Hill, NJ).
Flow cytometry
Bone marrow and spleen cells were harvested from mice. Surface marker staining for mouse CD41, CD42b, Ter119, CD71, Gr1, and Mac1 was performed by incubating cells in antibodies diluted in PBS + 0.5% BSA for 30 minutes. To characterize the myelo-erythroid stem/progenitor cell compartment, bone marrow cells were stained as follows: cells were first stained using a mouse hematopoietic progenitor enrichment kit (Stemcell Technologies; Vancouver BC) containing CD5, CD11b/Mac1, CD19, CD45R, Gr1, and Ter119. Cells were then incubated with Pacific Blue-conjugated streptavidin and simultaneously with antibodies against cKit, Sca1, FcγR, CD41, CD150, and CD105 as previously described (26).
Levels of phosphorylated Stat5 were determined as previously described (8). For intracellular phospho-protein analysis, freshly isolated whole bone marrow cells were first resuspended in 1 mL RPMI + 1% BSA and incubated at 37°C for 1 hour. Cells were then stimulated with hEPO (1 U/mL) or hTPO (10 ng/mL) with or without mIL-3 (10 ng/mL) for 10 minutes. Labelling for surface antigens was performed. Cells were then fixed in 16% paraformaldehyde at room temperature for 10 minutes, washed twice with PBS + 2% BSA, and permeabilized in ice-cold 95% methanol for 10 minutes. Cells were then stained immediately with PE-phospho-Stat5 in the dark at room temperature for 20 minutes and immediately analyzed.
FACS data were acquired using an LSR II flow cytometer (BD Biosciences) and analyzed using FlowJo software version 9.9.4 (Tree star; Ashland, OR). Cells were sorted using a FACS Aria (BD Biosciences).
IL-6 blockade
Age- and gender-matched symptomatic Jak2V617F/+; Pf4-Cre+ mice were randomized to receive an antibody against mouse IL-6 (R&D Systems, cat. # MAB406) at 0.3 mg/kg or PBS every other day by intraperitoneal (i.p.) injection for 6 weeks. Jak2V617F/+; Pf4-Cre+ mice were classified as symptomatic if peripheral blood analysis indicated an elevated (>60%) hematocrit.
Hematopoietic stem/progenitor cell transplantation
Retroviruses were generated by transfecting Plat-E cells with MIGR1 containing either human MPLW515L or JAK2V617F using Fugene VI (Roche Life Sciences; Indianapolis, IN) according to the manufacturer’s instructions. Viral supernatant was harvested at forty-eight hours post-transfection. cKit+ HSPCs were isolated from mouse bone marrow using microbeads (Cat# 130–091-224, Miltenyi Biotech Inc.; Auburn, CA), and transduced by mixing cells in viral supernatant with 8 μg/mL polybrene (Cat# TR-1003-G, MilliporeSigma, Burlington, MA) and centrifuging the mixture for 2 500 rpm for 90 minutes at 32°C. Transduced cells were cultured overnight, and transduction efficiency was confirmed by assessing GFP expression using flow cytometry. Three hundred thousand GFP+ cells were transplanted in to lethally irradiated (11 Gy) recipient C57BL/6 mice via tail vein injection.
To assess disease transplantability, bone marrow cells were collected from Jak2V617F/+; Pf4-Cre+ mice (CD45.2) or wild type (WT) (CD45.1). Two million Jak2V617F/+; Pf4-Cre+ and WT bone marrow cells were transplanted into lethally irradiated two-month old WT mice at a ratio of 90:10 or 10:90.
Allele-specific qPCR
Relative levels of Jak2V617F and Jak2WT were measured using a previously-established protocol (13). RNA was isolated from purified cell populations using Trizol reagent (Cat# 15596026, ThermoFisher Scientific), and cDNA was generated using a Verso cDNA synthesis kit (Cat# AB-1453/B, ThermoFisher Scientific). Relative quantification of Jak2V617F and Jak2WT transcripts was then performed with SYBR Green reagents (Cat# 4913850001, Sigma) using the Applied Biosystems QuantStudio 7 real-time system. The following primer sequences were used: Jak2WT forward primer 5’- TTTGAATTATGGTGTCTGCG; Jak2V617F forward primer 5’- TTTGAATTATGGTGTCTGCT; Jak2 common reverse primer 5’- CAGGTATGTATCCAGTGATCC.
Cytokine measurements
Levels of circulating cytokines were performed using a Luminex-based Mouse 32-Plex Cytokine Kit (Cat# MCYTMAG-70K-PX32, EMD Millipore, Billerica, MA). Analysis was performed on serum samples that were prepared according to Millipore’s instructions. In brief, peripheral blood was collected and allowed to clot for 30 minutes. Afterwards, blood samples were centrifuged at 1000 x g for 10 minutes. Serum samples were then aliquoted (~25 μL) in to clean tubes and frozen at −80°C until analysis. Before analysis, samples were diluted 1:2 in serum matrix and assayed according to the manufacturer’s instructions. Data were acquired using the FlexMAP 3D system and xPONENT software (Luminex; Austin, TX), and analyzed using MILLIPLEX Analyst software (EMD Millipore) as previously described(27). Single-plex cytokine-specific ELISAs (R&D Systems), including Cxcl1 (Cat# MKC00B), Cxcl2 (Cat# MM200), Ccl11 (Cat # MME00) and IL-6 (Cat# M6000B), were then used to validate the changes observed in individual cytokines.
Colony formation assays
EPO-dependent colony formation was assessed using cytokine-free methylcellulose-based media (Cat# m3234, Stemcell Technologies) supplemented with mSCF (10 ng/mL), hEPO (10 U/mL), and varying concentrations of mIL-6, mCxcl1, or mCxcl2. LSKs or MEPs were sorted from 6–8-week-old WT C57Bl/6 mice and seeded at 3 000 cells per well in triplicate. For erythroid colony formation assays (BFU-E), mouse splenocytes were seeded at 50 000 cells per well in triplicate using m3436 media (Stemcell Technologies) supplemented with hEPO. In all assays, colony formation was scored at 7–10 days after plating.
Histopathology
Tissues were fixed in 10% neutral buffered formalin, embedded in paraffin, and stained with hematoxylin and eosin to assess gross cellular histology or reticulin to assess fibrosis. For VWF immunohistochemistry, antigen retrieval was achieved by incubating slides in 1X target retrieval solution (Cat# S1699, Dako North America; Carpinteria, CA) at 98°C for 30 minutes in a water bath. Sections were stained for VWF (Cat# GA52761–2, Dako North America) overnight at 4°C at a dilution of 1:200, then incubated with rabbit HRP (Cat# M4U534, Biocare Medical; Concord, CA) for 15 minutes before the addition of chromogen DAB (Cat # BDB2004; Biocare). Sections were then counterstained with hematoxylin. All slide images were obtained on a Leica (Wetzlar, Germany) DM4000B microscope equipped with a Leica DFC320 color digital camera.
Statistics
Different groups were reported as mean ± SEM or mean ± SD and compared using unpaired two-sided Student’s t-test. When multiple comparisons were necessary, one-way or two-way ANOVA with post-test Bonferroni correction was used. Statistical significance was established when P < 0.05, labeled as *, and P < 0.01, labeled as **. All analysis was performed using GraphPad Prism. Statistical analysis of survival was performed via the Kaplan-Meier method, with significance determined using the Mantel-Cox long-rank test. Group sizes were determined by power calculation, to determine the sample size needed to achieve an 80% chance of detecting a significant different (P < 0.05) between groups. The researchers who analyzed the samples for flow cytometry and histology were not aware of the genotypes.
Results
Pf4-Cre drives expression of Jak2V617F selectively in the megakaryocyte lineage
To study the role of megakaryocytes in MPN pathogenesis, we generated Jak2V617F/+; Pf4-Cre+ mice where mutant Jak2 is expressed from the endogenous Jak2 locus specifically in megakaryocyte lineage-committed cells (8,23). Our model is distinct from prior studies, which employed a transgenic Jak2V617F model, where Jak2 is expressed at non-physiologic levels from a non-specific integration site (21). Prior studies have suggested that Pf4 is expressed at low levels in HSPCs(28,29), which raises the possibility that the Cre-mediated recombination (and subsequent expression of Jak2V617F) occurs prior to megakaryocyte lineage-commitment in our model. We took several approaches to confirm the specificity of Pf4-Cre in our model. First, we performed allele-specific qPCR on sorted cell populations to assess Jak2V617 expression across the hematopoietic ontogeny. We sorted long-term HSCs, bivalent Mk/erythroid progenitor cells (Pre-MegE), erythroid progenitor cells (Pro-ERY), Mk progenitors (MkP) as previously described (26), in addition to whole bone marrow mononuclear cells (MNCs), CD41+ Mks, and platelets from Jak2V617F/+; Pf4-Cre+ mice, and performed allele-specific qPCR for Jak2V167F. We could not detect significant expression of Jak2V617F in MNCs, LT-HSCs, Pre-MegEs, or Pro-ERYs, whereas we could detect significant levels of Jak2V617F in MkPs, and equal levels of Jak2V617F and Jak2WT in CD41+ Mks and platelets (Fig. 1A). As Jak2V617F could only be detected in megakaryocyte lineage-committed populations and was not detectable in earlier progenitor compartments or in erythroid lineage-committed cell types, we could thus conclude that the Pf4 promoter drives Cre expression specifically in megakaryocyte lineage-committed cells.
Figure 1.
Pf4-Cre drives megakaryocyte (Mk) lineage-restricted Jak2V617F expression. (A) Allele-specific qPCR quantifying the ratio of VF mutant to WT Jak2 in either whole mouse bone marrow mononuclear cells (MNCs) after red cell lysis or sorted hematopoietic lineages from Jak2 V617F/+; Pf4-Cre+ mice or age-matched Jak2+/+ controls (n=4 mice per group). Sorted populations include LT-HSCs, Pre-MegEs, Pro-ERYs, MkPs, CD41+ Mks, and platelets. (B) Flow cytometric analysis of Cre reporter expression (% tdTomato+ (Cre–) vs. % GFP+(Cre+)) in the LSKs, MEPs, erythroid (CD71+/Ter119+) cells, and Mks (CD41+) bone marrow compartments of Jak2 V617F/+; Pf4-Cre+; mTmG+ mice (n=8 mice, aged 8–16 weeks). (C-D) Assessment of phospho-Stat5 levels by intracellular flow cytometry in stimulated and unstimulated (C) CD41+ and (D) CD71+ spleen cells from Pf4-Cre+ mice. Flow cytometry plots are representative of 4 independent experiments. N=3 animals per group, mice were 20 weeks old. Bar graphs depict mean +/− SD. **P < 0.01, by one-way ANOVA.
We also employed the mTmG Cre switch reporter mouse (25) to confirm the lineage-specificity of Pf4-Cre. In this model, a double-fluorescent Cre reporter cassette is within the Rosa26 locus. Prior to Cre-mediated recombination, tdTomato is expressed. In Cre-positive cells, the locus undergoes a recombination event that switches the cassette to express GFP. Therefore, Cre-negative cells will be tdTomato+, while Cre-positive cells will be GFP+. We crossed Jak2V617F/+; Pf4-Cre+ mice with mTmG+/+ mice, which were then subjected to extensive flow cytometric analysis in order to survey reporter expression across hematopoiesis. No significant population of GFP+ cells could be detected in the LSK compartment, in Mk/Erythroid progenitors (MEPs) or in CD71+/Ter119+ erythroid cells, whereas the CD41+ Mk compartment was ~99% GFP+ (Fig. 1B).
Jak2V617F causes constitutive downstream activation of Stat5 (3,8). We therefore sought to further confirm Jak2V617F expression at the functional level by assessing levels of phosphorylated Stat5 (pStat5) by intracellular flow cytometry. In CD41+ Mk cells from Jak2V617F/+; Pf4-Cre+ mice, basal levels of pStat5 were similar to levels observed in hTPO-stimulated cells (with or without mIL-3) (Fig. 1C). In contrast, basal pStat5 levels in Jak2V617F/+; Pf4-Cre+ CD71+ erythroid cells were similar to levels observed in Jak2+/+; Pf4-Cre+ CD71+ cells (Fig. 1D). These observations provide compelling evidence that Pf4-Cre is active exclusively in megakaryocytes, and thus drives Jak2V617F expression in megakaryocyte lineage-committed cells.
Jak2V617F-mutant Mks confer a PV-Like phenotype with alterations in HSPCs
Since the Jak2V617F allele used in our model causes a distinct phenotype from the transgenic allele used by Zhan et al, which was not expressed from the endogenous locus (21), we assessed whether physiologic expression of Jak2V617F in Mks would induce a MPN phenotype. We monitored the peripheral blood counts of Jak2V617F/+; Pf4-Cre+ mice for 200 days, and observed progressive and significant increases in the platelet counts, as well as an increase in the hematocrit and hemoglobin levels (Fig. 2A–C). We were not able to detect a significant population of Cre+ (GFP+) cells by flow cytometry (Fig. 1B), and additional allele-specific qPCR on sorted CD71+/Ter119+ cells confirmed that this population was Jak2+/+ (Supplementary Fig. S1). Therefore, the aberrant erythropoiesis in our model is due to the interactions of Jak2V617F-mutant Mks with the Jak2WT hematopoietic milieu and not due to the outgrowth of a select subset of Pf4+ HSPCs.
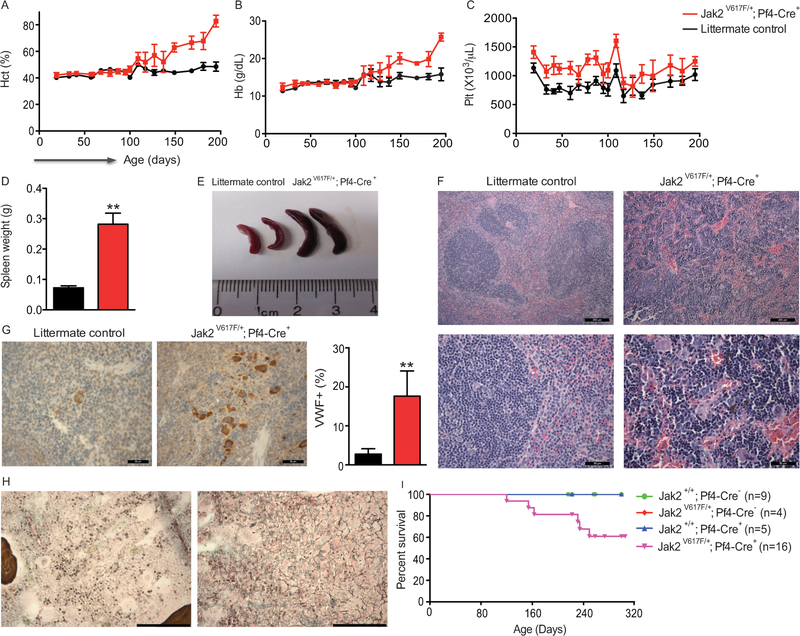
Figure 2.
Mk-specific expression of Jak2V617F leads to polycythemia. (A-C) Peripheral blood counts of Jak2 V617F/+; Pf4-Cre+ mice and littermate controls were monitored for 200 days. Jak2 V617F/+; Pf4-Cre+ mice showed significant increases in (A) hematocrit, (B) hemoglobin, and (C) platelet counts over the monitoring period (P < 0.01, by two-way ANOVA). (D-E) Jak2V617F/+; Pf4-Cre+ mice also displayed splenomegaly (increased spleen weight (D) and size (E)). (F) H&E staining revealed histopathological changes in splenic architecture (Scale bars depict 100 microns in the upper panel, 50 microns in the lower panel), as well as (G) increased VWF+ cells (Scale bars = 50 microns). (H) Reticulin staining revealed bone marrow fibrosis (Scale bars = 50 microns). In (D-H), mice were female and 6 months old. Results are representative of 2 independent experiments. N=6 animals per group. Bar graphs and line graphs depict mean ± SEM. (I) Kaplan-Meier survival curve (p=0.0374).
Further analysis of the hematopoietic compartment at 6 months revealed evidence of an overt MPN. We observed splenomegaly (Fig. 2D, E), along with marked changes in splenic architecture, coupled with a profound increase in erythroid progenitors, white pulp expansion, increased megakaryocytes, and marked fibrosis (Fig. 2F–H). We also observed impaired survival in Jak2V617F/+; Pf4-Cre+ mice relative to littermate controls (Fig. 2I). We noted that the peripheral phenotype in our model emerged with a significantly longer latency than what is typically seen in models of pan-hematopoietic JakV167F expression. We thus compared Jak2V617F/+; Pf4-Cre+ mice to Jak2V617F/+; Vav-Cre+ mice (where Jak2V617F is expressed in every hematopoietic cell). While fully penetrant and similar, the disease phenotype of Jak2V617F/+; Pf4-Cre+ was less severe (Supplementary Fig. S2), suggesting other cell types expressing JAK2V617F also contribute to the phenotype in Jak2V617F/+; Vav-Cre+ mice.
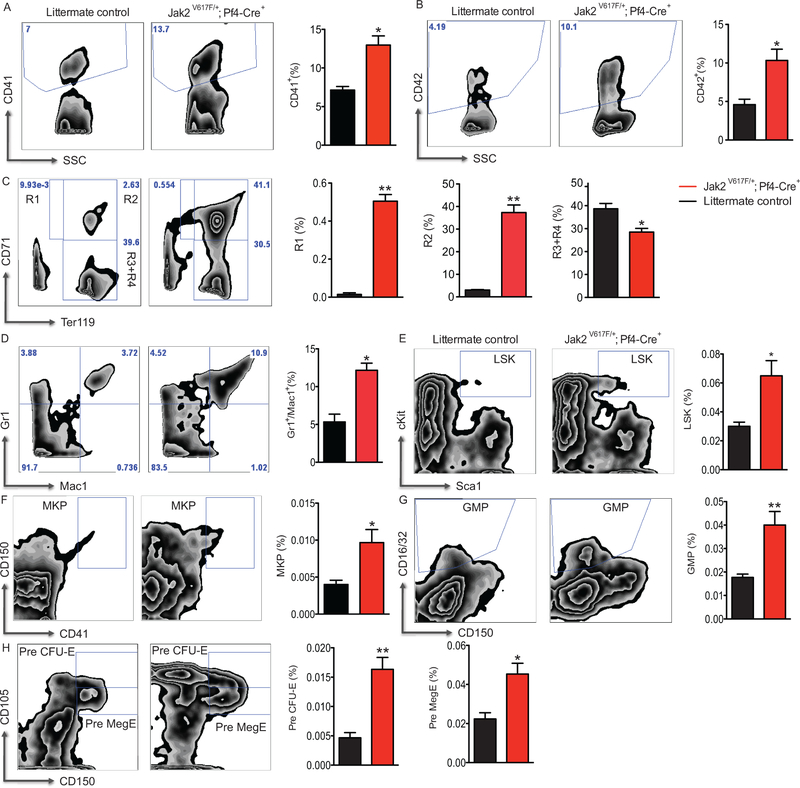
As expected, flow cytometry confirmed the histopathological observation of megakaryocytic expansion in the bone marrow and spleen (Fig. 3A, B and Supplementary Fig. S3A, B). Jak2V617F/+; Pf4-Cre+ mice displayed a robust expansion of Jak2WT immature erythroid cells (Ter119low/CD71high R1 and Ter119high/CD71high R2 cells) (30,31) in the spleen (Fig. 3C) and in the R1 population in the bone marrow (Supplementary Fig. S3C). The granulocyte lineage was also expanded in both organs (Fig. 3D and Supplementary Fig. S3D). Analysis of the HSPC compartment confirmed the finding that Jak2V617F Mks cause HSPC expansion (21). Lin–Sca1+cKit+ (LSK) HSPCs were expanded in bone marrow and spleen (Fig. 3E and Supplementary Fig. S3E). Downstream myeloid progenitor populations were also expanded, and skewed towards the Mk/erythroid lineage (Fig. 3F–H, Supplementary Fig.s S3F–H). Splenic progenitor cells from Jak2V617F/+; Pf4-Cre+ mice also produced more BFU-E, CFU-Mk and CFU-Myeloid colonies in vitro (Supplementary Fig. S4A–C).
Figure 3.
Mk-restricted Jak2V617F expression results in tri-lineage expansion. Flow cytometric analysis of spleens from 6-month-old Jak2 V617F/+; Pf4-Cre+ mice revealed that Jak2V617F expression in Mks increased (A) CD41+ and (B) CD42+ Mks, as well as (C) immature erythroid cells (R1 and R2 populations), and (D) Mac1+/Gr1+ myeloid cells in the spleen. Further profiling of the HSPC compartment showed increased (E) LSKs, (F) MkPs, (G) granulomonocytic progenitors (GMPs), as well as (H) Pre-CFU-E and Pre-MegEs in Jak2 V617F/+; Pf4-Cre+ mice relative to littermate controls. Representative flow plots are shown, and results are representative of 2 independent experiments. n=6 animals per group. Bar graphs depict mean ± SEM. * P < 0.05, ** P < 0.01 by unpaired two-sided Student’s T test.
Since overt MPN appeared in the Jak2V617F/+; Pf4-Cre+ model after a relatively long latency period (~20 weeks), we analyzed the composition of the hematopoietic compartment prior to symptom onset. Young asymptomatic Jak2V617F/+; Pf4-Cre+ showed only enhanced megakaryopoiesis (increased platelet counts) (Supplementary Fig. S5A) and Mk expansion in both spleen (Supplementary Fig. S6A–B) and bone marrow (Supplementary Fig. S7A–B). All other compartments were comparable to littermate controls (Supplementary Fig. S6C–K, S7C–K). No tissue abnormalities or fibrosis were apparent upon histological examination (Supplementary Fig. S5G–I). These data suggest that the duration of exposure to Jak2V617F Mks is an important factor to MPN development, and that the effect of mutant Mks on the HSPC niche occurs is exerted over time. Furthermore, LSK and MEP cells sorted from symptomatic Jak2 V617F/+; Pf4-Cre+ mice did not show EPO hypersensitivity, which is an established feature of PV (Supplementary Fig. S4D, E). This observation, combined with the long latency period, strongly suggests that Jak2V617F-mutant Mks can promote neoplastic growth of Jak2WT cells in a cell non-autonomous manner.
The PV-like phenotype is transplantable
In order to investigate if the Jak2V617F-mutant Mks is cell non-autonomous, we performed bone marrow transplantation experiments. We transplanted lethally irradiated recipients with either 90% or 10% Jak2 V617F/+; Pf4-Cre+-derived bone marrow mixed with wild type support, and monitored recipients for symptom onset. Only recipients receiving 90% Jak2 V617F/+; Pf4-Cre+-derived bone marrow showed signs of the PV phenotype (elevated hematocrits and hemoglobin, splenomegaly, expanded erythroid populations, expanded white pulp) observed in primary mice (Fig. 4A, B, F, G, and H). Platelet counts were elevated over time in recipients receiving 90% Jak2 V617F/+; Pf4-Cre+-derived bone marrow (Fig. 4C), and neither group showed significant leukocytosis (Fig. 4D). These data support our hypothesis that the observed phenotype is mediated by mutant Mks in a cell non-autonomous manner.
Figure 4.
Polycythemia in mice with Mk-restricted Jak2V617F expression is transplantable. Two million Jak2V617F/+; Pf4-Cre+ (CD45.2) and WT (CD45.1) bone marrow cells were transplanted into lethally irradiated female two-month old WT (CD45.1) mice at a ratio of 90:10 or 10:90. The Jak2V617F/+; Pf4-Cre+ donors were female six-month old mice. (A-E) Hematological indices including (A) hematocrit, (B) hemoglobin, (C) platelet, and (D) white blood cell counts in peripheral blood and (E) CD45.2 cell chimerism were measured at indicated times. Line graphs depict mean ± SEM. 90:10 vs 10:90, P < 0.01 by two-way ANOVA (A, B, C, E). (F) Recipients of 90:10 bone marrow cells showed increased spleen weights. (G) Flow cytometric analysis showed that recipients of 90:10 cells had increased number erythroid populations in the spleen. H&E staining of spleen sections from recipients of 90:10 bone marrow revealed disruption of splenic architecture (H). Scale bars depict 100 microns. Bar graphs depict mean ± SEM. **P < 0.01 by the unpaired two-sided Student’s t test. n=4 animals per group. Data are representative of 2 independent experiments.
Mutant Mk-derived IL-6 mediates enhanced erythropoiesis
Mks secrete numerous cytokines and chemokines that regulate the behavior of neighboring cells, including HSPCs (18,19,32–34). We hypothesized that mutant Mks could secrete factors that influence the differentiation and proliferation of HSPCS to promote the neoplastic growth of Jak2WT cells. Milliplex cytokine/chemokine profiling of sera revealed increases in the circulating levels of several cytokines and chemokines, including IL-6, Ccl11, Cxcl1, and Cxcl2 (Fig. 5A), in Jak2 V617F/+; Pf4-Cre+ mice relative to littermate controls. ELISA measurements validated a four-fold increase in IL-6 (Fig. 5B), which is upregulated in Jak2V617F mutant Mks isolated from PV patients (35), as well as significant increases in Ccl11, Cxcl1, and Cxcl2 (Supplementary Fig. S8A–C). In order to confirm that Jak2 V617F/+; Pf4-Cre+ Mks are a source of IL-6, we quantified IL-6 mRNA expression in FACS isolated CD41+ Mks, and found that IL-6 transcripts were markedly elevated in Jak2 V617F/+; Pf4-Cre+ bone marrow Mks (Fig. 5C). We next sought to determine if any of these factors could independently promote increased erythropoiesis, and thus contribute to the polycythemia observed in our model. We cultured Jak2WT HSPCs (sorted LSKs or MEPs) in methylcellulose under erythroid colony-promoting conditions, and exogenous IL-6 treatment (but not Cxcl1 or Cxcl2) increased EPO-dependent colony formation (Fig. 5D, E and Supplementary Fig. S8D, E). MEPs only responded 2-fold to increased IL-6 levels, while LSKs showed a > 15-fold increase. These data suggest that LSKs are more responsive to IL-6, and that (Mk-derived) IL-6 acts on uncommitted HSPCs as well as on erythroid progenitors.
Figure 5.
Jak2V617F-mutant Mk-derived IL-6 enhances erythropoiesis. (A) Multiplexed serum profiling (Luminex) of 32 cytokines/chemokines in sera from 5-month-old Jak2 V617F/+; Pf4-Cre+ mice and littermate controls showed significant increases in Ccl11 (Eotaxin), Cxcl1 (KC), Cxcl2 (MIP-2), and IL-6. Data shown are representative of 2 independent experiments. (B) ELISA confirming the increase in serum IL-6 levels observed in Jak2 V617F/+; Pf4-Cre+ mice. (C) IL-6 mRNA expression is elevated in CD41+ megakaryocytes sorted from Jak2 V617F/+; Pf4-Cre+ mice relative to littermate controls. IL-6 transcript levels were normalized to Gapdh. (A-C) N = 4 mice per group. (B-C) Results are representative of 3 independent experiments. (D-E) IL-6 increased BFU-E formation from wild type HSPCs, (D) LSKs and (E) MEPs, in a dose-dependent manner. LSK/MEP populations were FACS sorted from 6–8-week-old WT C57BL/6 mice. (F-H) Three pairs of 16–20-week-old male or female Jak2 V617F/+; Pf4-Cre+ mice were treated with either an antibody against IL-6 or PBS for 6 weeks. (F) IL-6 blockade markedly reduced BFU-E formation by splenocytes in vitro. Concordant decreases in the splenic erythroid progenitors (G) Pre-CFU-E and Pre-MegE populations and (H) immature erythroid (R1 and R2) populations were also observed by flow cytometry. (D-H) Results are representative of 2 independent experiment. * P < 0.05, ** P < 0.01 by unpaired two-sided Student’s T-test.
To assess a potential requirement for elevated IL-6 in our model, we treated Jak2 V617F/+; Pf4-Cre+ mice with an antibody against IL-6. The antibody was well-tolerated, as treated animals showed so significant weight loss (Supplementary Fig. S9). While treatment did not change peripheral blood counts (Supplementary Fig. S9), IL-6 blockade suppressed erythropoiesis (Fig. 5F–H). Treated splenocytes also formed fewer erythroid colonies (BFU-E), indicative of decreased erythroid progenitors (Fig. 5F). Accordingly, analysis of the spleens revealed a reduced frequency of erythroid progenitor cells (Pre-CFU-E and Pre-MegE) (Fig. 5G) in antibody-treated mice. Furthermore, IL-6 blockade significantly reduced the proportion of immature R1 and R2 erythroid cell populations (Fig. 5H). We also treated age and gender-matched Jak2WT littermate controls to assess the requirement of IL-6 on steady-state erythropoiesis, and observed a similar effect (Supplementary Fig. S10). These data demonstrate that increased IL-6 contributes to the aberrant expansion of Jak2WT erythroid cells observed in our model.
Our data suggest that Mks are a source of IL-6 in our model. However, this does not preclude the possibility that additional cell types could contribute to the increase in IL-6. Circulating platelets could also activate mature myeloid cells, or erythroblastic island macrophages, thus potentiating the disease phenotype. In order to determine if activated myeloid cells or erythroblastic island macrophages could serve as contributing sources of IL-6, we also examined IL-6 expression in sorted mature F4/80+ macrophages or bulk Gr1+/Mac1+ myeloid cells (Supplementary Fig. S11A, B). IL-6 expression was not elevated in these populations which suggests that Jak2V617F-mutant Mks are the primary contributor to the systemic increase in IL-6 observed in our model.
Mks are required for MPN maintenance
Given that Jak2 V617F-mutant MKs are sufficient to cause aberrant erythropoiesis (21,22), we next sought to determine if the Mk lineage is necessary for disease maintenance. We first crossed a Cre-inducible Diphtheria toxin receptor transgenic mouse (iDTR+/−) with Pf4-Cre+ mice to generate a model for selective Mk depletion(23,24). We then retrovirally transduced progenitor cells from either iDTR+/−; Pf4-Cre+ mice or iDTR+/−; Pf4-Cre- controls with Jak2V617F, and transplanted infected cells into irradiated recipients. As expected, Jak2V617F-transduced mice developed the characteristic PV-like phenotype, which is characterized by elevated hematocrit and hemoglobin (Fig. 6A). Diphtheria toxin (DT) treatment significantly reduced both the platelet counts and the megakaryocytes in iDTR+/−; Pf4-Cre+ mice (Fig. 6A–C, F, G). Mk/platelet loss was accompanied by a significant decrease in disease indicators, specifically in hematocrit/hemoglobin levels (Fig. 6A). Furthermore, we observed a significant reduction the terminally-differentiated mature erythroid compartment (R3+R4 populations) in both bone marrow and spleen following DT treatment/Mk depletion (Fig. 6D, E). Importantly, DT treatment also resulted in a significant reduction in IL-6 levels (Supplementary Fig. S12), further confirming Il-6 as a central mediator of the cell non-autonomous erythropoiesis observed in this model. We did not observe any significant effect of Mk depletion on white blood cell counts (Fig. 6A). However, white blood cell counts are only modestly elevated in this MPN model.
Figure 6.
Mk depletion attenuates myeloproliferation. Bone marrow cells from 8–10 week of iDTR+/−; Pf4-Cre+ or iDTR+/−; Pf4-Cre- control mice were transduced with either (A-G) MIGR1-JAK2V617F-GFP or (H-M) MIGR1-MPLW515L-GFP, and transplanted into WT recipient mice. In JAK2V617F-GFP recipients, diphtheria toxin (DT; 10 μg/kg) was administered 5 weeks post-transplant to initiate Mk depletion. Mice were sacrificed for analysis 10 days after DT treatment. (A) Mk depletion significantly decreased platelet counts, hematocrit, and hemoglobin in peripheral blood (P < 0.01 by two-way ANOVA), while white blood cell counts were unaffected. (B-E) Mk depletion significantly reduced the CD41+ Mk compartment and terminally-differentiated mature erythroid compartment (R3+R4 populations) in bone marrow (BM) and spleen (Sp). H&E staining of (F) bone marrow and (G) spleen sections after Mk ablation showed markedly fewer Mks and restoration of splenic architecture (Scale bars depict 50 microns; n=5 iDTR+/−; Pf4-Cre- controls and 3 iDTR+/−; Pf4-Cre+ mice). (H-M) DT (10 μg/kg) was administered to MIGR1-MPLW515L-GFP recipients 28 days post-transplant to initiate Mk depletion. (H) Mk ablation significantly reduced platelets and white blood cell counts (P < 0.01 by two-way ANOVA), while hematocrit was unchanged in this model. (I) Spleen weights were also significantly reduced following Mk depletion in iDTR+/−; Pf4-Cre+ mice compared to iDTR+/−; Pf4-Cre- controls. (J-L) DT treatment decreased CD41+ megakaryocytes in both the bone marrow and spleen, and myeloid progenitor cells in the spleen in iDTR+/−; Pf4-Cre+ mice. (M) H&E stained spleen showed DT treatment reduced megakaryocytes and partially restore the normal architecture of spleen in iDTR+/−; Pf4-Cre+ mice. Scale bars depict 50 microns. n=6 animals per group. Mice were sacrificed 7 days after initiation of DT treatment. Bar graphs and line graphs depict mean ± SEM. *P < 0.05, **P < 0.01. Results shown are representative of 2 independent experiments.
In order to explore the larger relevance of aberrant JAK/STAT pathway activation in Mks to MPN maintenance, we repeated the Mk depletion studies using a second MPN transplant model: the MPLW515L bone marrow transplant model. MPLW515L mutation is detected in Jak2WT ET/PMF patients, and also acts as a driver of MPN via constitutive activation of JAK2 and downstream STAT signaling. Retroviral overexpression of MPLW515L in vivo results in a penetrant, rapid, and lethal myeloproliferative disease that is characterized by thrombocytosis, leukocytosis, and splenomegaly (without evident polycythemia) (36)(Fig. 6H, I). Mk depletion in MPLW515L-expressing in iDTR+/−; Pf4-Cre+ mice reduced Mk numbers in the bone marrow and spleen (Fig. 6J, K), as well as reduced platelet counts (Fig. 6H). Leukocyte counts and spleen weight were also significantly reduced (Fig. 6H, I). Mk depletion also caused a significant decrease in Lineage– cKit+Sca1– myeloid progenitor cells in the bone marrow (Fig. 6L), as well as restoration of splenic architecture (Fig. 6M). Therefore, Mk depletion significantly reduced disease burden in a model of MPLW515L-driven MPN. Together with our findings from the Jak2V617F transplant model, this reveals an unexpected role of Mks in MPN.
Discussion
In this study, we developed a megakaryocyte lineage-specific Jak2V617F knock-in mouse model to investigate the role of mutant megakaryocytes in MPN pathogenesis. Our data, consonant with studies of non-physiologic Jak2V617F expression in MKs with less clear phenotypes (21,22), establishes that mutant Mks interact with the wild type hematopoietic milieu to both initiate and sustain MPN. Our model is characterized by a strong PV-like phenotype, including: impaired overall survival, splenomegaly, and aberrant erythropoiesis (elevated hemoglobin and hematocrit, and expansion of the erythroid progenitor compartments). It is worth noting that the phenotypic changes, while characteristic of PV in general, were far less pronounced than the phenotype of established pan-hematopoietic Jak2V617F models and occurred after a longer latency period. Therefore, we conclude that Jak2V617F-mutant Mks are sufficient to generate a PV phenotype, and that Jak2V617F-mutant Mks promote cell non-autonomous myelo-erythroid expansion which likely contributes to MPN in concert with clonal expansion of mutant cells in different lineages. These observations are consistent with genetic and clinical correlative studies in a cohort of MPN patients with a low JAK2V617F allele burden. These studies reported impaired clinical outcome and disease progression in a cohort of ET/MF patients, even though their hematopoietic compartment was comprised of a relatively low fraction of Jak2V617F-mutant cells (37,38). Furthermore, additional studies have revealed that JAK2V617F allele burden shows little to no correlation with disease phenotype.
Pro-inflammatory cytokines and chemokines are frequently elevated in MPN patients, and increased levels of circulating cytokines are associated with adverse survival. This cytokine-driven inflammatory state is hypothesized to be a key contributing cause of the constitutional symptoms of MPN. We initially observed that Jak2V617F-mutant Mks caused low level inflammation by histopathology, including increased bone marrow fibrosis and expansion of the splenic white pulp. This led us to hypothesize that Jak2V617F-mutant Mks/platelets could potentiate a myeloproliferative state via aberrant production of pro-inflammatory cytokines/chemokines. Indeed, we observed that Jak2V617F-mutant Mks significantly elevated circulating levels of 4 discrete pro-inflammatory cytokines/chemokines: IL-6, Ccl11, Cxcl1, and Cxcl2. Of these factors, only IL-6 supported increased erythroid differentiation in vitro, which implicates this inflammatory mediator as a key promoter of MPN pathogenesis. Consistent with our observations, elevated IL-6 levels are correlated with splenomegaly, survival, and JAK2 mutation status in MPN patients (39). Furthermore, the improvement in constitutional symptoms seen with JAK2 inhibition in these patients correlated with reductions in serum IL-6. A previous report has implicated IL-6 in mediating the myeloproliferative phenotype observed in miR-146a knockout mice (40).
Mks could promote aberrant erythropoiesis either directly, via increased production of these factors, or indirectly, by recruiting and activating myeloid cells. We found that Jak2V617F-mutant Mks show increased expression of IL-6, and that IL-6 blockade using a neutralizing antibody significantly impeded erythropoiesis in vivo.
In their transgenic model, Zhan et al reported an ET-like MPN phenotype with expansion of the stem/progenitor cell pool (21). Our model displays several notable differences – primarily the PV-like and inflammatory aspects of the observed phenotype. These studies provide compelling in vivo evidence that Jak2V617F-mutant Mks can promote the expansion of the wild type hematopoietic compartment. We expanded upon this to show that Mk-derived factors, such as IL-6, mediate (at least partially) the cell non-autonomous role of Mks in MPN pathogenesis. We also established a broader role for Mks in MPN maintenance by employing Mk ablation in two established MPN models. Mk depletion in both the JAK2V617F and MPLW515L bone marrow transplant MPN models significantly blunted the polycythemia and leukocytosis phenotypes of either model respectively. This demonstrates that Mks are necessary for MPN maintenance in vivo. It also suggests that the contributions of MPN Mks are not driver mutation-specific, and are a broader consequence of JAK/STAT pathway hyperactivation with a critical role for JAK-STAT activation in Mks.
Collectively, our findings confirm and provide further mechanistic insight into the role of the megakaryocyte lineage in MPN pathogenesis. We demonstrate that mutant Mks are directly involved in MPN initiation and maintenance in vivo, and that Mks can promote the heterotypic expansion of wild type HSPCs via aberrant cytokine production. These data support a novel model for MPN pathogenesis, in which MPN manifests as a genetically and phenotypically heterogeneous hematopoietic disorder, with both mutant and wild type cells contributing to the pathogenic ecosystem. We expect that similar mechanisms underlie the development of other myeloid neoplasms as well as in non-hematopoietic malignancies, where malignant transformation is driven by a complex interplay between discrete clonal cell populations. Our findings also contribute to the collective understanding of how MPN patients with a low frequency of mutant cells can present with fulminant disease, and highlight the therapeutic potential of targeting these cellular interactions (such as Mks and the HSPC niche) to achieve improved therapeutic benefit in MPN.
Supplementary Material
Translational relevance.
Genetic analysis of myeloproliferative neoplasms (MPNs) patients indicates that the hematopoietic system of MPN patients is a heterogeneous mixture of mutant clone-derived and wild-type cells. This raises the possibility that the MPN clone can interact with non-clonal hematopoietic cells to promote myeloproliferation. We reveal an unexpected role of JAK2V617F-mutant megakaryocytes in the establishment and maintenance of MPN. Mutant megakaryocytes promote increased erythropoiesis and induce a myeloproliferative state in part due to aberrant production of Interleukin-6 (IL-6). We also demonstrate that megakaryocytes are necessary for maintenance of the MPN state, and that IL-6 blockade significantly reduces the cell non-autonomous erythroid expansion. Collectively, these observations provide novel insight into the pathogenic basis of low allele burden MPN cases, where patients present with significant myeloproliferation with relatively few mutant cells. They also provide support for the future development of therapeutic agents targeting megakaryocytes as a critical strategy to improve outcomes for MPN patients.
Acknowledgements
This work was supported by grants from the NIH (1F99CA212481-01 to BW; CA108671 to RL and JDC; HL112792 to JDC, NCI R50CA211534 to QJW) and the Samuel Waxman Cancer Research Foundation. This work was supported in part by MSKCC Support Grant/Core Grant P30 CA008748. We thank the Pathology Core Facility of the Robert Lurie Comprehensive Cancer Center of Northwestern University for processing mouse tissues and performing H&E and reticulin staining. R.L.L. is on the supervisory board of Qiagen and is a scientific advisor to Loxo, Imago, C4 Therapeutics and Isoplexis, which each includes an equity interest. He receives research support from and consulted for Celgene and Roche, he has received research support from Prelude Therapeutics, and he has consulted for Incyte, Novartis, Astellas, Morphosys and Janssen. He has received honoraria from Lilly and Amgen for invited lectures and from Gilead for grant reviews.
Financial Support: This work was supported by grants from the NIH (1F99CA212481-01 to BW; CA108671 to RL and JDC; HL112792 to JDC; NCI R50CA211534 to QJW) and the Samuel Waxman Cancer Research Foundation.
Conflict of interest statement
R.L.L. is on the supervisory board of Qiagen and is a scientific advisor to Loxo, Imago, C4 Therapeutics and Isoplexis, which each includes an equity interest. He receives research support from and consulted for Celgene and Roche, he has received research support from Prelude Therapeutics, and he has consulted for Incyte, Novartis, Astellas, Morphosys and Janssen. He has received honoraria from Lilly and Amgen for invited lectures and from Gilead for grant reviews. J.D.C. receives research funding from Forma Therapeutics and Scholar Rock, is a consultant for Sierra Oncology, and the scientific advisor of the MPN Research Foundation.
Footnotes
The remaining authors declare no conflicts of interest.
References
- 1.Baxter EJ, Scott LM, Campbell PJ, East C, Fourouclas N, Swanton S, et al. Acquired mutation of the tyrosine kinase JAK2 in human myeloproliferative disorders. Lancet 2005;365:1054–61. [DOI] [PubMed] [Google Scholar]
- 2.James C, Ugo V, Le Couédic J-P, Staerk J, Delhommeau F, Lacout C, et al. A unique clonal JAK2 mutation leading to constitutive signalling causes polycythaemia vera. Nature 2005;434:1144–8. [DOI] [PubMed] [Google Scholar]
- 3.Levine RL, Wadleigh M, Cools J, Ebert BL, Wernig G, Huntly BJP, et al. Activating mutation in the tyrosine kinase JAK2 in polycythemia vera, essential thrombocythemia, and myeloid metaplasia with myelofibrosis. Cancer Cell 2005;7:387–97. [DOI] [PubMed] [Google Scholar]
- 4.Kralovics R, Passamonti F, Buser AS, Teo S-S, Tiedt R, Passweg JR, et al. A gain-of-function mutation of JAK2 in myeloproliferative disorders. N Engl J Med 2005;352:1779–90. [DOI] [PubMed] [Google Scholar]
- 5.Akada H, Yan D, Zou H, Fiering S, Hutchison RE, Mohi MG. Conditional expression of heterozygous or homozygous Jak2V617F from its endogenous promoter induces a polycythemia vera-like disease. Blood 2010;115:3589–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li J, Spensberger D, Ahn JS, Anand S, Beer PA, Ghevaert C, et al. JAK2 V617F impairs hematopoietic stem cell function in a conditional knock-in mouse model of JAK2 V617F-positive essential thrombocythemia. Blood 2010;116:1528–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marty C, Lacout C, Martin A, Hasan S, Jacquot S, Birling M-C, et al. Myeloproliferative neoplasm induced by constitutive expression of JAK2V617F in knock-in mice. Blood 2010;116:783–7. [DOI] [PubMed] [Google Scholar]
- 8.Mullally A, Lane SW, Ball B, Megerdichian C, Okabe R, Al-Shahrour F, et al. Physiological Jak2V617F expression causes a lethal myeloproliferative neoplasm with differential effects on hematopoietic stem and progenitor cells. Cancer Cell 2010;17:584–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rampal R, Al-Shahrour F, Abdel-Wahab O, Patel JP, Brunel J-P, Mermel CH, et al. Integrated genomic analysis illustrates the central role of JAK-STAT pathway activation in myeloproliferative neoplasm pathogenesis. Blood 2014;123:e123–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jamieson CHM, Gotlib J, Durocher JA, Chao MP, Mariappan MR, Lay M, et al. The JAK2 V617F mutation occurs in hematopoietic stem cells in polycythemia vera and predisposes toward erythroid differentiation. Proc Natl Acad Sci USA 2006;103:6224–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ishii T, Bruno E, Hoffman R, Xu M. Involvement of various hematopoietic-cell lineages by the JAK2V617F mutation in polycythemia vera. Blood 2006;108:3128–34. [DOI] [PubMed] [Google Scholar]
- 12.Delhommeau F, Dupont S, Tonetti C, Massé A, Godin I, Le Couédic J-P, et al. Evidence that the JAK2 G1849T (V617F) mutation occurs in a lymphomyeloid progenitor in polycythemia vera and idiopathic myelofibrosis. Blood 2007;109:71–7. [DOI] [PubMed] [Google Scholar]
- 13.Mullally A, Poveromo L, Schneider RK, Al-Shahrour F, Lane SW, Ebert BL. Distinct roles for long-term hematopoietic stem cells and erythroid precursor cells in a murine model of Jak2V617F-mediated polycythemia vera. Blood 2012;120:166–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Passamonti F, Rumi E. Clinical relevance of JAK2 (V617F) mutant allele burden. Haematologica 2009;94:7–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ciurea SO, Merchant D, Mahmud N, Ishii T, Zhao Y, Hu W, et al. Pivotal contributions of megakaryocytes to the biology of idiopathic myelofibrosis. Blood 2007;110:986–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zahr AA, Salama ME, Carreau N, Tremblay D, Verstovsek S, Mesa R, et al. Bone marrow fibrosis in myelofibrosis: pathogenesis, prognosis and targeted strategies. Haematologica 2016;101:660–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wen QJ, Yang Q, Goldenson B, Malinge S, Lasho T, Schneider RK, et al. Targeting megakaryocytic-induced fibrosis in myeloproliferative neoplasms by AURKA inhibition. Nat Med 2015;21:1473–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bruns I, Lucas D, Pinho S, Ahmed J, Lambert MP, Kunisaki Y, et al. Megakaryocytes regulate hematopoietic stem cell quiescence through CXCL4 secretion. Nat Med 2014;20:1315–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhao M, Perry JM, Marshall H, Venkatraman A, Qian P, He XC, et al. Megakaryocytes maintain homeostatic quiescence and promote post-injury regeneration of hematopoietic stem cells. Nat Med 2014;20:1321–6. [DOI] [PubMed] [Google Scholar]
- 20.Meyer SC, Keller MD, Woods BA, LaFave LM, Bastian L, Kleppe M, et al. Genetic studies reveal an unexpected negative regulatory role for Jak2 in thrombopoiesis. Blood 2014;124:2280–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhan H, Ma Y, Lin CHS, Kaushansky K. JAK2(V617F)-mutant megakaryocytes contribute to hematopoietic stem/progenitor cell expansion in a model of murine myeloproliferation. Leukemia 2016;30:2332–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang Y, Lin CHS, Kaushansky K, Zhan H. JAK2V617F Megakaryocytes Promote Hematopoietic Stem/Progenitor Cell Expansion in Mice Through Thrombopoietin/MPL Signaling. Stem Cells 2018;36:1676–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tiedt R, Schomber T, Hao-Shen H, Skoda RC. Pf4-Cre transgenic mice allow the generation of lineage-restricted gene knockouts for studying megakaryocyte and platelet function in vivo. Blood 2007;109:1503–6. [DOI] [PubMed] [Google Scholar]
- 24.Buch T, Heppner FL, Tertilt C, Heinen TJAJ, Kremer M, Wunderlich FT, et al. A Cre-inducible diphtheria toxin receptor mediates cell lineage ablation after toxin administration. Nat Methods 2005;2:419–26. [DOI] [PubMed] [Google Scholar]
- 25.Muzumdar MD, Tasic B, Miyamichi K, Li L, Luo L. A global double-fluorescent Cre reporter mouse. Genesis 2007;45:593–605. [DOI] [PubMed] [Google Scholar]
- 26.Pronk CJH, Rossi DJ, Månsson R, Attema JL, Norddahl GL, Chan CKF, et al. Elucidation of the phenotypic, functional, and molecular topography of a myeloerythroid progenitor cell hierarchy. Cell Stem Cell 2007;1:428–42. [DOI] [PubMed] [Google Scholar]
- 27.Kleppe M, Kwak M, Koppikar P, Riester M, Keller M, Bastian L, et al. JAK-STAT pathway activation in malignant and nonmalignant cells contributes to MPN pathogenesis and therapeutic response. Cancer Discov 2015;5:316–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Calaminus SDJ, Guitart AV, Guitart A, Sinclair A, Schachtner H, Watson SP, et al. Lineage tracing of Pf4-Cre marks hematopoietic stem cells and their progeny. Freson K, editor. PLoS ONE 2012;7:e51361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pertuy F, Aguilar A, Strassel C, Eckly A, Freund J-N, Duluc I, et al. Broader expression of the mouse platelet factor 4-cre transgene beyond the megakaryocyte lineage. J Thromb Haemost 2015;13:115–25. [DOI] [PubMed] [Google Scholar]
- 30.Leung CG, Xu Y, Mularski B, Liu H, Gurbuxani S, Crispino JD. Requirements for survivin in terminal differentiation of erythroid cells and maintenance of hematopoietic stem and progenitor cells. J Exp Med 2007;204:1603–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Socolovsky M, Nam H, Fleming MD, Haase VH, Brugnara C, Lodish HF. Ineffective erythropoiesis in Stat5a(−/−)5b(−/−) mice due to decreased survival of early erythroblasts. Blood 2001;98:3261–73. [DOI] [PubMed] [Google Scholar]
- 32.Nakamura-Ishizu A, Takubo K, Kobayashi H, Suzuki-Inoue K, Suda T. CLEC-2 in megakaryocytes is critical for maintenance of hematopoietic stem cells in the bone marrow. J Exp Med 2015;212:2133–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Storan MJ, Heazlewood SY, Heazlewood CK, Haylock DN, Alexander WS, Neaves RJ, et al. Brief Report: Factors Released by Megakaryocytes Thrombin Cleave Osteopontin to Negatively Regulate Hematopoietic Stem Cells. Stem Cells 2015;33:2351–7. [DOI] [PubMed] [Google Scholar]
- 34.Domingues MJ, Cao H, Heazlewood SY, Cao B, Nilsson SK. Niche Extracellular Matrix Components and Their Influence on HSC. J Cell Biochem 2017;118:1984–93. [DOI] [PubMed] [Google Scholar]
- 35.Wickenhauser C, Thiele J, Lorenzen J, Schmitz B, Frimpong S, Schramm K, et al. Polycythemia vera megakaryocytes but not megakaryocytes from normal controls and patients with smokers polyglobuly spontaneously express IL-6 and IL-6R and secrete IL-6. Leukemia 1999;13:327–34. [DOI] [PubMed] [Google Scholar]
- 36.Pikman Y, Lee BH, Mercher T, McDowell E, Ebert BL, Gozo M, et al. MPLW515L is a novel somatic activating mutation in myelofibrosis with myeloid metaplasia. PLoS Med. 2006;3:e270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moliterno AR, Williams DM, Rogers O, Spivak JL. Molecular mimicry in the chronic myeloproliferative disorders: reciprocity between quantitative JAK2 V617F and Mpl expression. Blood 2006;108:3913–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tefferi A, Lasho TL, Huang J, Finke C, Mesa RA, Li CY, et al. Low JAK2V617F allele burden in primary myelofibrosis, compared to either a higher allele burden or unmutated status, is associated with inferior overall and leukemia-free survival. Leukemia 2008;22:756–61. [DOI] [PubMed] [Google Scholar]
- 39.Tefferi A, Vaidya R, Caramazza D, Finke C, Lasho T, Pardanani A. Circulating interleukin (IL)-8, IL-2R, IL-12, and IL-15 levels are independently prognostic in primary myelofibrosis: a comprehensive cytokine profiling study. J Clin Oncol 2011;29:1356–63. [DOI] [PubMed] [Google Scholar]
- 40.Zhao JL, Rao DS, O’Connell RM, Garcia-Flores Y, Baltimore D. MicroRNA-146a acts as a guardian of the quality and longevity of hematopoietic stem cells in mice. Elife 2013;2:e00537. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.