Abstract
Purpose
Given limited data available on long-term outcomes in 22q11.2 deletion syndrome (22q11.2DS), we investigated mortality risk in adults with this microdeletion syndrome.
Methods
We studied 309 well-characterized adults (age ≥17 years) with 22q11.2DS and their 1014 unaffected parents and siblings, using a prospective case–control design. We used Cox proportional hazards regression modeling and Kaplan–Meier curves to investigate effects of the 22q11.2 deletion and its associated features on all-cause mortality and survival.
Results
The 22q11.2 deletion (hazard ratio [HR] 8.86, 95% CI 2.87–27.37) and major congenital heart disease (CHD; HR 5.03, 95% CI 2.27–11.17), but not intellectual disability or psychotic illness, were significant independent predictors of mortality for adults with 22q11.2DS compared with their siblings. Amongst those with 22q11.2DS, there were 31 deaths that occurred at a median age of 46.4 (range 18.1–68.6) years; a substantial minority had outlived both parents. Probability of survival to age 45 years was approximately 72% for those with major CHD, and 95% for those with no major CHD (p < 0.0001).
Conclusion
For adults with 22q11.2DS, the 22q11.2 deletion and more severe forms of CHD both contribute to a lower life expectancy than family-based expectations. The results have implications for genetic counseling and anticipatory care.
Keywords: DiGeorge syndrome, velocardiofacial syndrome, prognosis, schizophrenia, heart defects
INTRODUCTION
22q11.2 deletion syndrome (22q11.2DS) (OMIM 188400/192430) is the most common microdeletion syndrome, affecting an estimated 1 in 3000–4000 live births. Overall penetrance of features associated with 22q11.2 deletion syndrome is very high but there is wide phenotypic variability.1 Associated features may be of early or later onset, and may include congenital anomalies, developmental delay, somatic medical conditions, and psychiatric illnesses such as schizophrenia.1 In studies primarily involving pediatric samples, the reported overall mortality in 22q11.2DS was 4% in one study and 14% in another, with median ages of death of 5 months and 3.4 months, respectively, most commonly involving serious heart defects.2,3 Given advances in diagnostic and pediatric care over recent decades, the vast majority of patients survive into adulthood.3,4 Therefore, long-term outcome data are of importance to patients, families, and clinicians. About a decade ago, we reported that adults with 22q11.2DS died prematurely relative to their unaffected siblings.5 However, this study lacked the power to determine whether there were significant effects of major features of 22q11.2DS, such as congenital heart disease (CHD). Understanding how such variables affect mortality in 22q11.2DS could allow us to identify patients at higher risk for premature death and inform clinical practice.
In the current study, we employed a prospective case–control design to investigate the degree to which the 22q11.2 deletion, and its major associated features, may increase the risk of mortality in adults with 22q11.2DS compared with their siblings and parents. We predicted that major CHD,6 and potentially other 22q11.2DS-associated features such as intellectual disability,7 could increase risk for all-cause mortality, independent of the global effects of the 22q11.2 deletion.
MATERIALS AND METHODS
We prospectively studied all-cause mortality and survival in adults with 22q11.2DS compared with that of their unaffected siblings and parents. Informed consent was obtained in writing, and the study was approved by the local research ethics boards of hospitals (Centre for Addiction and Mental Health and University Health Network) affiliated with the University of Toronto.
Adults with 22q11.2DS
We included all 309 consenting individuals with 22q11.2DS (148 male, 161 female) who were 17 years or older as of 31 December 2017 and confirmed to have a typical chromosome 22q11.2 deletion (i.e., including the LCR22A-LCR22B region, most commonly involving the 2.5-Mb LCR22A-LCR22D region)1 by standard methods, as previously described.5,8 All patients were ascertained through a specialty clinic for adults with 22q11.2DS (The Dalglish Family 22q Clinic or the Clinical Genetics Research Program, Toronto, Canada), through referrals (from genetics, psychiatric, or other sources) and/or active screening, mostly at an adult congenital cardiac clinic.8 We retained 100 adults (of 102, i.e., excluding two subjects with atypical 22q11.2 deletions) where there were 12 deaths (compared with none in their siblings).5 Ethnicity was characterized as European (n = 260, 84.1%) or non-European descent, with the latter comprising Asian (n = 24, 7.8%), African (n = 10, 3.2%), or other including mixed (n = 15, 4.9%) ethnicity. Of the 309 subjects from 291 families, 275 were singleton affected individuals, 28 were from 14 families with two affected individuals, and there were two families with three affected individuals.
Unaffected siblings
For this study, there were 469 unaffected siblings (231 male, 238 female), comprising 383 full and 86 half (38 maternal, 48 paternal) siblings, of the 22q11.2DS group who met our inclusion criteria.5 Included siblings had survived to age 17 years or older as of 31 December 2017, had sufficient clinical data available for analyses, and had evidence they were unaffected with a 22q11.2 deletion:5,9 negative molecular result for the 22q11.2 deletion (n = 46 siblings), the respective affected proband was known to have a de novo 22q11.2 deletion (n = 253 siblings), or deemed to have a probable de novo 22q11.2 deletion (136 siblings), or where the respective affected proband had an inherited 22q11.2 deletion, the sibling did not meet clinical screening criteria for 22q11.2DS (n = 34 siblings).5,9 These methods excluded 49 siblings with inadequate molecular and/or clinical screening data; 22 (7.1%) of the 309 subjects with 22q11.2DS had no siblings to include in the study.
Unaffected parents
We included 545 unaffected parents (277 mothers, 268 fathers) of the patients with 22q11.2DS in the study. These comprised parents of subjects with confirmed (n = 316 parents) or probable (n = 150 parents) de novo 22q11.2 deletions, or where there was no suspicion the parent had the 22q11.2 deletion based on clinical screening criteria (n = 79 parents).9
Outcome measures
All-cause mortality was the primary outcome measure and survival was defined as years since age 17.0 years, with age recorded to the nearest 0.1 year as of 31 December 2017, death, or date at last contact for families lost to follow-up. Online obituary searches supplemented the available clinical data on mortality for the 1323 subjects in this study (n = 309 with 22q11.2DS and their 1014 relatives). To establish the cause of death, we obtained medical records and postmortem results where available.5,10 A natural death from a presumed cardiac cause occurring within a short period of time, in a person without any prior fatal conditions, was defined as sudden cardiac death.11 We did not assess for specific genes, such as TANGO2, that may relate to various causes of death.12
We also assessed whether certain clinical features of 22q11.2DS increased the risk of mortality in these patients. For this, we used data available from comprehensive medical and psychiatric records for the patients with 22q11.2DS, and collateral history from participating relatives.8,13 Extensive family history data and regular updates from family contacts provided sufficient information for siblings and parents with respect to all predictor variables. We selected 22q11.2DS-related features based on their potential to contribute to mortality and where we had data for the entire sample: CHD, intellectual disability, and psychotic illness.7,14–17 As before, we classified CHD by structural complexity and deemed those with moderate or complex conditions as major CHD (n = 112) (refs. 5,6); this included most commonly tetralogy of Fallot (n = 80, 71.4%). A DSM-IV diagnosis of moderate to severe mental retardation was classified as intellectual disability.18,19 Psychotic illness was defined as lifetime DSM-IV diagnosis of any psychotic disorder (e.g., schizophrenia, schizoaffective, other nonaffective psychotic disorder, or psychotic mood disorder).19 We also used age at laboratory diagnosis in the model to account for possible effects associated with late diagnosis (e.g., lack of typical congenital features that can prompt early diagnosis).8 In post hoc analyses, we compared mortality results for the subgroup (n = 100) studied in our previous paper5 to those for the more recently ascertained cohort (n = 209) of adults with 22q11.2DS; there were no significant differences between these subgroups on prevalence of female sex, major CHD, intellectual disability, or psychotic illness (data not shown).
Statistical analyses
The main comparisons were between the 22q11.2DS cohort and unaffected siblings. We used Cox proportional hazards modeling to calculate hazard ratios (HR) for all-cause mortality using the following predictor variables: 22q11.2 deletion status, major CHD,5 psychotic illness,15 intellectual disability,14 and sex. For the model examining mortality within the 22q11.2DS cohort we used the same predictor variables, and age at laboratory diagnosis8 instead of 22q11.2 deletion. Kaplan–Meier curves were constructed to assess survival in the 22q11.2DS cohort compared with their unaffected siblings and parents. For descriptive statistics, we used Fisher’s exact tests (FETs), χ2 tests, and Wilcoxon two-sample tests, as appropriate. The data met the assumptions of the test. Statistical analyses were performed using SAS 9.3 (SAS Institute, Cary, NC). Two-tailed p values <0.05 were considered statistically significant.
RESULTS
There were 1323 individuals from 291 families included in the study, 309 adults with 22q11.2DS and their 1014 relatives. Individuals with 22q11.2DS and their families were followed for up for 0.1 to 21.5 (median 5.3) years, reflecting both the long-term follow-up and active ongoing recruitment in our study. Table 1 summarizes the demographic and clinical variables for the sample studied. The prevalence of psychotic illness and major CHD among unaffected siblings and parents (Table 1) was consistent with general population expectations.6,20
Table 1.
Demographic and clinical factors for 309 adults with 22q11.2 deletion syndrome (22q11.2DS) and their unaffected siblings (n = 469) and parents (n = 545)
| Variables | 22q11.2DS (n = 309) | Unaffected siblings (n = 469) | 22q11.2DS vs. unaffected siblings | Unaffected parents (n = 545) | 22q11.2DS vs. unaffected parents | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | FET | df | p | n | % | FET | df | p | |
| Female sex | 161 | 52.1 | 238 | 50.7 | 0.14 | 1 | 0.71 | 277 | 50.8 | 0.13 | 1 | 0.72 |
| Major CHDa | 112 | 36.2 | 0 | - | 198.58 | 1 | <0.0001 | 0 | - | 218.06 | 1 | <0.0001 |
| Psychotic illnessb | 119 | 38.5 | 5 | 1.1 | 194.94 | 1 | <0.0001 | 5 | 0.9 | 224.54 | 1 | <0.0001 |
| Intellectual disabilityc | 28 | 9.1 | 1 | 0.2 | 40.64 | 1 | <0.0001 | 0 | - | 51.06 | 1 | <0.0001 |
| Median | Range | |||||||||||
| Age at laboratory diagnosis (years)d | 17.0 | 0.1–67.0 | - | - | - | - | ||||||
Significant findings are indicated in bold font.
CHD congenital heart disease, FET Fisher’s exact test.
aModerate or complex CHD, defined using standard criteria.6
bPsychotic illness included schizophrenia, schizoaffective disorder, other nonaffective psychotic disorder, or psychotic mood disorder, as previously defined.19
cModerate to severe intellectual disability, as previously defined.19
dAge at molecular cytogenetic diagnosis (e.g., fluorescence in situ hybridization and typical 22q11.2 deletion region probe) or microarray diagnosis of a typical 22q11.2 deletion in years.8
There were 31 (13 male, 18 female) adults with 22q11.2DS (10.0%) who had died, at a median age of 46.4 (range 18.1–68.6) years. Six (4 male, 2 female) unaffected siblings (1.3%) had died at a median age of 58.3 (range 23.6–83.0) years and 79 (48 male, 31 female) unaffected parents (14.5%) had died at a median age of 64.6 (range 17.4–93.0) years. For the 30 deceased adults with 22q11.2DS for whom we had parental data, 13 (43.3%) had died while both parents were living, 10 (33.3%) while one parent was still living, and seven (23.3%) had outlived both parents.
Risk factors for all-cause mortality in 22q11.2DS
Consistent with our hypothesis, the Cox proportional hazards model for all-cause mortality comparing 22q11.2DS with unaffected siblings was highly significant (Table 2). The 22q11.2 deletion (HR 8.86, 95% CI 2.87–27.37, p = 0.0002) and the presence of a major CHD (HR 5.03, 95% CI 2.27–11.17, p < 0.0001) were independent factors associated with increased risk of all-cause mortality in adults with 22q11.2DS, when controlling for other covariates (Table 2). There were no significant effects of intellectual disability, psychotic illness, or sex on mortality.
Table 2.
Cox regression models for mortality risk in 309 adults with 22q11.2 deletion syndrome (22q11.2DS)
| Variables | Mortality risk for 309 adults with 22q11.2DS compared with their 469 unaffected siblingsa | Mortality risk within the cohort of 309 adults with 22q11.2DSb | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coefficient | SE | Wald χ2 | p | HR | 95% CI | Coefficient | SE | Wald χ2 | p | HR | 95% CI | |
| 22q11.2 deletion | 2.18 | 0.58 | 14.36 | 0.0002 | 8.86 | 2.87–27.37 | - | - | - | - | - | - |
| Major CHDc | 1.62 | 0.41 | 15.79 | <0.0001 | 5.03 | 2.27–11.17 | 1.56 | 0.43 | 13.14 | 0.0003 | 4.77 | 2.05–11.10 |
| Age at laboratory diagnosisd | - | - | - | - | - | - | -0.07 | 0.02 | 8.66 | 0.0032 | 0.94 | 0.90–0.98 |
| Intellectual disabilitye | 0.76 | 0.51 | 2.20 | 0.14 | 2.14 | 0.78–5.87 | 0.91 | 0.52 | 2.99 | 0.08 | 2.48 | 0.89–6.93 |
| Psychotic illnessf | 0.37 | 0.39 | 0.90 | 0.34 | 1.45 | 0.68–3.10 | 0.25 | 0.37 | 0.46 | 0.50 | 1.29 | 0.62–2.69 |
| Female sex | 0.12 | 0.35 | 0.11 | 0.74 | 1.12 | 0.57–2.21 | 0.28 | 0.40 | 0.48 | 0.49 | 1.32 | 0.60–2.92 |
Significant findings are indicated in bold font.
CHD congenital heart disease, CI confidence interval, HR hazard ratio, SE standard error.
aLikelihood ratio for model: χ2 = 71.98, df = 5, p < 0.0001.
bLikelihood ratio for model: χ2 = 28.65, df = 5, p < 0.0001.
cModerate or complex congenital heart disease (CHD), defined using standard criteria.6
dAge at molecular cytogenetic diagnosis (e.g., fluorescence in situ hybridization and typical 22q11.2 deletion region probe) or microarray diagnosis of a typical 22q11.2 deletion.8
eModerate to severe intellectual disability, as previously defined.19
fPsychotic illness included schizophrenia, schizoaffective disorder, other nonaffective psychotic disorder, or psychotic mood disorder, as previously defined.19
Results of the Cox proportional hazards model within the 22q11.2DS cohort were similar. Major CHD was a significant risk predictor of all-cause mortality (HR 4.77, 95% CI 2.05–11.10, p = 0.0003, Table 2). As expected,8 later age at laboratory diagnosis of a 22q11.2 deletion was associated with a significantly lower risk of all-cause mortality when controlling for other factors (HR 0.94, 95% CI 0.90–0.98, p = 0.0032, Table 2). Although results for other variables were nonsignificant, the effect of intellectual disability was at the trend level in this model (Table 2). A post hoc analysis that added a variable to account for the 100 adults previously studied5 versus the 209 subjects more recently ascertained did not materially change the regression results, and there was no statistically significant difference in the proportion with all-cause mortality, or in median age at death, between these subgroups (data not shown).
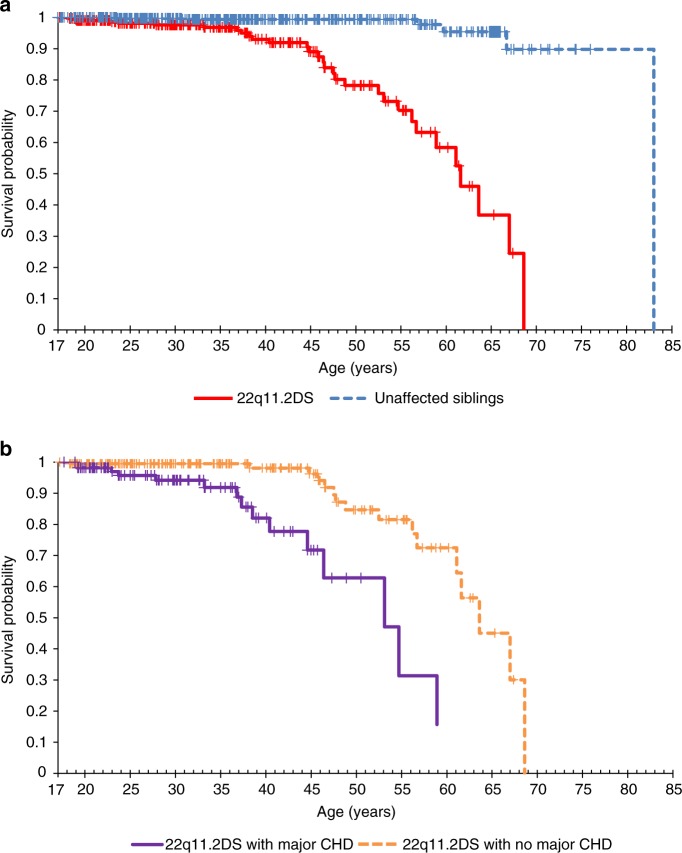
Survival in 22q11.2DS
Kaplan–Meier curves showed significantly lower survival in adults with 22q11.2DS compared with their unaffected siblings (Fig. 1a; log rank χ2 = 59.7, df = 1, p < 0.0001). Results were similar in comparisons with unaffected parents, for both fathers (log rank χ2 = 55.4, df = 1, p < 0.0001) and mothers (log rank χ2 = 68.4, df = 1, p < 0.0001) (Supplementary Figures 1a and 1b, respectively).
Fig. 1. Survival curves for adults with 22q11.2 deletion syndrome (22q11.2DS; n = 309) compared with their unaffected siblings (n = 469), as well as for adults with 22q11.2DS with (n = 112) and without (n = 197) major congenital heart disease (CHD).
(a) Survival curve for adults with 22q11.2 deletion syndrome (22q11.2DS; n = 309) compared with their unaffected siblings (n = 469). Kaplan–Meier curves show the significantly lower survival in adults with 22q11.2DS (solid line) compared with their unaffected siblings (dashed line) (log rank χ2 = 59.7, df = 1, p < 0.0001). (b) Survival curve for adults with 22q11.2 deletion syndrome (22q11.2DS) with (n = 112) and without (n = 197) major congenital heart disease (CHD). Within the 22q11.2DS cohort, the Kaplan–Meier curves show a significant effect on survival of major CHD (solid line) compared with the simple or no CHD subgroup (dashed line) (log rank χ2 = 19.5, df = 1, p < 0.0001).
Within the 22q11.2DS cohort, there was a significant effect of major CHD on survival that was apparent by early adulthood (Fig. 1b; log rank χ2 = 19.5, df = 1, p < 0.0001). The probability of survival to ages 40 and 50 years was approximately 82% and 63%, respectively, for those with major CHD, and 98% and 85%, respectively, for those with no major CHD (Fig. 1b). Patients with a major CHD died at a significantly younger median age (37.3, range 19.0–58.9, years; n = 15 of 112, 13.4%) compared with those with no major CHD (50.7, range 18.1–68.6, years; n = 16 of 197, 8.1%; Z = 2.89, p = 0.0039). There was a nonsignificant trend for longer survival in the more recently ascertained subgroup of 209 individuals compared with those ascertained 10 or more years ago (log rank χ2 = 3.47, df = 1, p = 0.0623) (ref. 5).
Cause of death
Table 3 shows causes of death for the 31 adults with 22q11.2DS who had died and the relationship to complexity of CHD. The most common causes of death in 22q11.2DS were cardiovascular in nature (n = 22, 71.0%). Although heart failure and arrhythmia were only documented for those with major CHD, sudden cardiac death (n = 12, 38.7%) appeared prevalent regardless of CHD severity (Table 3). Cancer, not observed in our original study,5 was tied for the third most common cause of death. To the best of our knowledge, patients who died were receiving routine medical care, and not actively using recreational drugs (excluding cigarettes).
Table 3.
Cause of death in 31 adults with 22q11.2 deletion syndrome (22q11.2DS) and relationship to congenital heart disease complexity
| Number of deaths | ||||||
|---|---|---|---|---|---|---|
| Cause of death | Age at death: range in years (median) | Total | Congenital heart disease (CHD) complexitya | |||
| No major CHD | Major CHD | |||||
| None | Simple | Moderate | Complex | |||
| Cardiovascular | ||||||
| Sudden cardiac death | 22.9–67.0 (47.1) | 12 | 5 | 2 | 3 | 2 |
| Heart failure | 19.0–58.9 (36.8) | 7 | 0 | 0 | 3 | 4 |
| Arrhythmia | 23.7, 33.2, 54.7 | 3 | 0 | 0 | 1 | 2 |
| Cancerb | 46.4, 47.5, 63.6 | 3 | 2 | 0 | 1 | 0 |
| Other | ||||||
| Stroke | 44.6, 68.6 | 2 | 1 | 0 | 1 | 0 |
| Pneumonia | 52.5, 61.1 | 2 | 2 | 0 | 0 | 0 |
| Septic shock | 18.1 | 1 | 0 | 1 | 0 | 0 |
| Suicide | 38.2 | 1 | 1 | 0 | 0 | 0 |
| Total, any causec | 31 | 11 | 3 | 9 | 8 | |
aCHD categorized using levels of structural complexity, defined using standard criteria.6
bDeaths from cancers were one each of lung (male, aged 63.6 years), breast (female, aged 47.5 years), and cervical (female, aged 46.4 years).
cOf these 31 deaths, 12 were previously reported: sudden cardiac death (n = 6), heart failure (n = 2), and one each of pneumonia, septic shock, stroke, and suicide5.
Given that all deaths in our 22q11.2DS cohort occurred under age 70 years and thus could be considered premature,21 we examined the cause of death in this age range for unaffected siblings and parents. For the four of five siblings where we could determine cause of death, two were sudden cardiac deaths (males, aged 30.8 and 56.8 years), one an accidental death (male, 23.6 years), and one ovarian cancer (female, 59.7 years). Of 47 parents who had died prematurely (28 fathers, 19 mothers; median age at death 56.8, range 17.4–69.7, years; 15 with insufficient data on cause), the most common known cause was cancer (n = 14, 29.8%). The second most common causes were cardiovascular (n = 9, 19.1%: myocardial infarction [n = 3], two each of arrhythmia, sudden cardiac death, and cardiac surgical complications). The remaining 9 parents died of accidents (n = 3), drug overdose (n = 2), and one each of suicide, ruptured gallbladder, complications due to diabetes mellitus, and bacterial endocarditis. Notably, 16 (30.8%) of these 52 premature deaths involved relatives of the 31 adults with 22q11.2DS who had died.
DISCUSSION
To our knowledge, this is the largest study of all-cause mortality and survival in adults with 22q11.2DS. Using siblings and parents as comparison groups, the results showed that the 22q11.2 deletion was a significant factor in both mortality risk and reduced survival. The median age at death observed was 46.4 years, and all deaths occurred before the age of 70 years in this still relatively young sample. Nonetheless, a substantial minority of patients with 22q11.2DS had outlived both of their parents. As for other genetic conditions,22 congenital cardiac disease was an additional independent risk factor for all-cause mortality. These results collectively are likely to be important for genetic counseling and have implications for patients, and their families and caregivers.
Clinical features and their effect on mortality
On average, adults with 22q11.2DS in the cohort studied had a median age at death about 35 years younger than a respective Canadian norm of 81.7 years.21 Those with major CHD died on average about 44 years younger.21 Nonetheless, the overall median age at death was approximately 5 years older than that reported 10 years ago for the initial subsample of 100 patients.5 Also, the current results suggested a trend toward increasing survival of adults with 22q11.2DS in a more recently ascertained subgroup. As for other genetic conditions,22 and as suggested by other studies of younger cohorts, one may expect further gains in survival in 22q11.2DS related to advances in technology with regard to cardiac and other pediatric surgery and to early diagnosis.23–25 As people with genetic syndromes and intellectual disability live longer, issues pertaining to multimorbidity arise26 and the related burden of ongoing care that often falls to caregivers.27 These issues may be of interest to policy makers to ensure adequate health-care management for these growing populations.7,14,17,27
The other 22q11.2DS features investigated did not show significant independent effects on mortality risk once the global effects of 22q11.2 deletion and major CHD were accounted for. This may not be surprising for psychotic illness, given that a recent Canadian population-based study reported mean age at death of 76.7 years for individuals with schizophrenia, approximately 8 years younger than those without schizophrenia,28 but far older than our cohort with 22q11.2DS. Results for intellectual disability14 had a small independent effect on mortality though did not reach statistical significance. This may be related to effect size, and perhaps the regular follow-up care for our cohort in contrast to the general population with intellectual disability, where barriers to accessing health care and preventable causes contribute to mortality.14,29
Causes of death
The top causes of death in 22q11.2DS were cardiovascular in nature, accounting for 70.1% of deaths observed to date. Consistent with our previous report,5 sudden cardiac death remained the most common cause of mortality. This is far greater than the estimated general population prevalence of 60 per 100,000 individuals,5,30 even if one considers only the 7 (3.6%) of 197 individuals with no major CHD who died of this cause. In the absence of major structural cardiac causes, the etiology of these sudden deaths is unclear, as in the general population, and may relate to arrhythmia predisposition.30,31 Interestingly, emerging evidence suggests that rare, biallelic pathogenic variants of TANGO2, a gene in the 22q11.2 region involved in mitochondrial function, are associated with arrhythmias, seizures, metabolic disturbances, and premature death, usually in childhood.12 Studies of this gene on the intact allele in 22q11.2DS, including reported recurrent single-nucleotide and structural variants,12 may shed light on whether TANGO2 is related to vulnerability to sudden death. Another consideration is the phenomenon of sudden unexpected death in epilepsy (SUDEP), given the elevated prevalence of epilepsy in 22q11.2DS (~10%).1,4,32 However, we note that amongst the deceased patients with 22q11.2DS, four had epilepsy and of these only one had a sudden unexpected death.
As in recent studies of adult outcome in CHD,33 individuals in our 22q11.2DS cohort are now living long enough to die of cancer, the leading cause of death in Canada (median age at diagnosis 66 years).34,35 The three individuals in our study who died of cancer did so at a younger age than population expectations for median age of death for those specific cancers (lung, breast, and cervical).35 These results are consistent with previous reports of possible predisposition for malignancy in children with 22q11.2DS.1,36,37 Larger samples will be needed to determine whether there is an increased vulnerability and whether this may relate to T-cell deficits, and/or aberrant immune surveillance, that could predispose to carcinogenic viruses such as Epstein–Barr virus or human papillomavirus (HPV).35,36 Nonetheless, the findings collectively signify the need for vigilance. This includes encouraging active preventive measures such as the HPV vaccine, routine cancer screening including Pap smears, and counseling on smoking cessation for individuals with 22q11.2DS.36 This is similar to preventive care recommendations for individuals from disadvantaged populations for whom access to health care may be a barrier.14,15,29 Similarly, the high risk (about 1 in 4) of psychotic illness in 22q11.2DS necessitates vigilance to ensure prompt diagnosis and effective treatment,4,38 with active monitoring for suicidality and metabolic parameters that may increase mortality risk.4,28,38–40
Advantages and limitations
This is the largest study of adult mortality in 22q11.2DS to date. In contrast to an earlier, smaller study,5 power was sufficient to detect significant effects of major CHD independent of those for the 22q11.2 deletion. There were however several limitations. By design, the focus on adults meant that the sample was biased towards individuals with 22q11.2DS who survived to adulthood. Although pediatric research indicates this is by far the norm now for 22q11.2DS,1,4 there may also be some tendency to relatively less severe phenotypes; we attempted to account for this by selecting predictor variables such as major CHD and age at laboratory diagnosis. On the other hand, ascertainment was mainly through congenital cardiac centers and neuropsychiatric and genetics-based referrals that could tend to bias the sample toward certain phenotypes. In addition, the overall 22q11.2DS sample was relatively young, despite up to 21 years of follow-up. Incomplete information on de novo status of the 22q11.2 deletion is inevitable given the adult sample used; however, we have addressed this as before with published clinical screening methods.9 Nonetheless, some affected siblings and parents may have been inadvertently included; however, this likely would have only modestly affected the level of statistical significance. The results may not be entirely generalizable to regions without publicly funded health care and/or a specialty center for adults with 22q11.2DS. Also, with respect to determining cause of death, pathology reports were available for just 10 of 31 deaths and this may be a particular limitation given the high prevalence of apparent sudden cardiac death for which we had only four autopsies.
Conclusions and future directions
The results of this study demonstrate that, compared with their closest relatives, individuals with 22q11.2DS had a higher risk of all-cause mortality that was significantly related to both global effects of the 22q11.2 deletion and more complex CHD that is often associated with the syndrome. Future studies would benefit from investigating predictors of mortality in larger samples of 22q11.2DS, including those without CHD and older individuals, to detect more subtle effects on mortality. Incorporating molecular genetic and/or relevant marker data, and prospectively collected natural history, could help pinpoint parameters amenable to targeted management. With advances in earlier detection and diagnosis of 22q11.2DS, a greater understanding of long-term outcomes including mortality will benefit patients, families, clinicians, and policy makers.
Supplementary information
Acknowledgements
The authors thank the patients and their families for their participation, colleagues for referring patients, and research assistants and students who assisted in the collection of data for the study. We dedicate this research to all the patients with 22q11.2DS who have died but continue to help us understand this condition. This work was supported by the Canadian Institutes of Health Research (CIHR) (MOP-313331 and MOP-111238 to A.S.B.), and the Clinician-Scientist Program at the University of Toronto (L.V.). A.S.B. holds the Dalglish Chair in 22q11.2 Deletion Syndrome at the University of Toronto and University Health Network.
Disclosure
The authors declare no conflicts of interest.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version of this article (10.1038/s41436-019-0509-y) contains supplementary material, which is available to authorized users.
References
- 1.McDonald-McGinn DM, Sullivan KE, Marino B, et al. 22q11.2 deletion syndrome. Nat Rev Dis Primers. 2015;1:1–46. doi: 10.1038/nrdp.2015.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Campbell IM, Sheppard SE, Crowley TB, et al. What is new with 22q? An update from the 22q and You Center at the Children’s Hospital of Philadelphia. Am J Med Genet A. 2018;176:2058–2069. doi: 10.1002/ajmg.a.40637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Repetto GM, Guzman ML, Delgado I, et al. Case fatality rate and associated factors in patients with 22q11 microdeletion syndrome: a retrospective cohort study. BMJ Open. 2014;4:1–5. doi: 10.1136/bmjopen-2014-005041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fung WL, Butcher NJ, Costain G, et al. Practical guidelines for managing adults with 22q11.2 deletion syndrome. Genet Med. 2015;17:599–609. doi: 10.1038/gim.2014.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bassett AS, Chow EW, Husted J, et al. Premature death in adults with 22q11.2 deletion syndrome. J Med Genet. 2009;46:324–330. doi: 10.1136/jmg.2008.063800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Billett J, Cowie MR, Gatzoulis MA, et al. Comorbidity, healthcare utilisation and process of care measures in patients with congenital heart disease in the UK: cross-sectional, population-based study with case-control analysis. Heart. 2008;94:1194–1199. doi: 10.1136/hrt.2007.122671. [DOI] [PubMed] [Google Scholar]
- 7.Arvio M, Salokivi T, Bjelogrlic-Laakso N. Age at death in individuals with intellectual disabilities. J Appl Res Intellect Disabil. 2017;30:782–785. doi: 10.1111/jar.12269. [DOI] [PubMed] [Google Scholar]
- 8.Palmer LD, Butcher NJ, Boot E, et al. Elucidating the diagnostic odyssey of 22q11.2 deletion syndrome. Am J Med Genet A. 2018;176:936–944. doi: 10.1002/ajmg.a.38645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bassett AS, Chow EW. 22q11 deletion syndrome: a genetic subtype of schizophrenia. Biol Psychiatry. 1999;46:882–891. doi: 10.1016/S0006-3223(99)00114-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Butcher NJ, Kiehl TR, Hazrati LN, et al. Association between early-onset Parkinson disease and 22q11.2 deletion syndrome: identification of a novel genetic form of Parkinson disease and its clinical implications. JAMA Neurol. 2013;70:1359–1366. doi: 10.1001/jamaneurol.2013.3646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Braunwald E, Libby P, Bonow RO, et al. Braunwald’s heart disease: a textbook of cardiovascular medicine. 8th ed. St. Louis, MO: Saunders; 2007.
- 12.Dines JN, Golden-Grant K, LaCroix A, et al. TANGO2: expanding the clinical phenotype and spectrum of pathogenic variants. Genet Med. 2019;21:601–607. doi: 10.1038/s41436-018-0137-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bassett AS, Chow EW, Husted J, et al. Clinical features of 78 adults with 22q11 deletion syndrome. Am J Med Genet A. 2005;138:307–313. doi: 10.1002/ajmg.a.30984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hosking FJ, Carey IM, Shah SM, et al. Mortality among adults with intellectual disability in England: comparisons with the general population. Am J Public Health. 2016;106:1483–1490. doi: 10.2105/AJPH.2016.303240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Olfson M, Gerhard T, Huang C, et al. Premature mortality among adults with schizophrenia in the United States. JAMA Psychiatry. 2015;72:1172–1181. doi: 10.1001/jamapsychiatry.2015.1737. [DOI] [PubMed] [Google Scholar]
- 16.Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. 2015;72:334–341. doi: 10.1001/jamapsychiatry.2014.2502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Verheugt CL, Uiterwaal CS, van der Velde ET, et al. Mortality in adult congenital heart disease. Eur Heart J. 2010;31:1220–1229. doi: 10.1093/eurheartj/ehq032. [DOI] [PubMed] [Google Scholar]
- 18.Chow EW, Watson M, Young DA, Bassett AS. Neurocognitive profile in 22q11 deletion syndrome and schizophrenia. Schizophr Res. 2006;87:270–278. doi: 10.1016/j.schres.2006.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Butcher NJ, Chow EW, Costain G, et al. Functional outcomes of adults with 22q11.2 deletion syndrome. Genet Med. 2012;14:836–843. doi: 10.1038/gim.2012.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Perala J, Suvisaari J, Saarni SI, et al. Lifetime prevalence of psychotic and bipolar I disorders in a general population. Arch Gen Psychiatry. 2007;64:19–28. doi: 10.1001/archpsyc.64.1.19. [DOI] [PubMed] [Google Scholar]
- 21.Decady Y, Greenberg L. Ninety years of change in life expectancy. Health at a glance. 2014. https://www150.statcan.gc.ca/n1/pub/82-624-x/2014001/article/14009-eng.htm. Accessed 1 December 2018.
- 22.Zhu JL, Hasle H, Correa A, et al. Survival among people with Down syndrome: a nationwide population-based study in Denmark. Genet Med. 2013;15:64–69. doi: 10.1038/gim.2012.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Best KE, Rankin J. Long-term survival of individuals born with congenital heart disease: a systematic review and meta-analysis. J Am Heart Assoc. 2016;5:1–16. doi: 10.1161/JAHA.115.002846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Karamlou T, McCrindle BW, Williams WG. Surgery insight: late complications following repair of tetralogy of Fallot and related surgical strategies for management. Nat Clin Pract Cardiovasc Med. 2006;3:611–622. doi: 10.1038/ncpcardio0682. [DOI] [PubMed] [Google Scholar]
- 25.Liberman RF, Getz KD, Lin AE, et al. Delayed diagnosis of critical congenital heart defects: trends and associated factors. Pediatrics. 2014;134:373–381. doi: 10.1542/peds.2013-3949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bayen E, Possin KL, Chen Y, et al. Prevalence of aging, dementia, and multimorbidity in older adults with Down syndrome. JAMA Neurol. 2018;75:1399–1406. doi: 10.1001/jamaneurol.2018.2210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Karas D, Costain G, Chow E, Bassett A. Perceived burden and neuropsychiatric morbidities in adults with 22q11.2 deletion syndrome. J Intellect Disabil Res. 2014;58:198–210. doi: 10.1111/j.1365-2788.2012.01639.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gatov E, Rosella L, Chiu M, Kurdyak PA. Trends in standardized mortality among individuals with schizophrenia, 1993-2012: a population-based, repeated cross-sectional study. CMAJ. 2017;189:1177–1187. doi: 10.1503/cmaj.161351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.O’Leary L, Cooper SA, Hughes-McCormack L. Early death and causes of death of people with intellectual disabilities: a systematic review. J Appl Res Intellect Disabil. 2018;31:325–342. doi: 10.1111/jar.12417. [DOI] [PubMed] [Google Scholar]
- 30.Kuriachan VP, Sumner GL, Mitchell LB. Sudden cardiac death. Curr Probl Cardiol. 2015;40:133–200. doi: 10.1016/j.cpcardiol.2015.01.002. [DOI] [PubMed] [Google Scholar]
- 31.Yousuf O, Chrispin J, Tomaselli GF, Berger RD. Clinical management and prevention of sudden cardiac death. Circ Res. 2015;116:2020–2040. doi: 10.1161/CIRCRESAHA.116.304555. [DOI] [PubMed] [Google Scholar]
- 32.Whitney R, Donner EJ. Risk factors for sudden unexpected death in epilepsy (SUDEP) and their mitigation. Curr Treat Options Neurol. 2019;21:1–14. doi: 10.1007/s11940-019-0547-4. [DOI] [PubMed] [Google Scholar]
- 33.Diller GP, Kempny A, Alonso-Gonzalez R, et al. Survival prospects and circumstances of death in contemporary adult congenital heart disease patients under follow-up at a large tertiary centre. Circulation. 2015;132:2118–2125. doi: 10.1161/CIRCULATIONAHA.115.017202. [DOI] [PubMed] [Google Scholar]
- 34.Canadian Cancer Statistics Advisory Committee. Canadian cancer statistics. 2018. http://cancer.ca/Canadian-Cancer-Statistics-2018-EN. Accessed 1 December 2018.
- 35.Noone A, Howlader N, Krapcho M, et al. SEER cancer statistics review, 1975-2015. https://seer.cancer.gov/csr/1975_2015/. Accessed 1 December 2018.
- 36.Stevens T, van der Werff Ten Bosch J, De Rademaeker M, et al. Risk of malignancy in 22q11.2 deletion syndrome. Clin Case Rep. 2017;5:486–490. doi: 10.1002/ccr3.880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lambert MP, Arulselvan A, Schott A, et al. The 22q11.2 deletion syndrome: cancer predisposition, platelet abnormalities and cytopenias. Am J Med Genet A. 2018;176:2121–2127. doi: 10.1002/ajmg.a.38474. [DOI] [PubMed] [Google Scholar]
- 38.Butcher NJ, Fung WL, Fitzpatrick L, et al. Response to clozapine in a clinically identifiable subtype of schizophrenia. Br J Psychiatry. 2015;206:484–491. doi: 10.1192/bjp.bp.114.151837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Voll SL, Boot E, Butcher NJ, et al. Obesity in adults with 22q11.2 deletion syndrome. Genet Med. 2017;19:204–208. doi: 10.1038/gim.2016.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch Gen Psychiatry. 2007;64:1123–1131. doi: 10.1001/archpsyc.64.10.1123. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.