Abstract
This study investigated the effects of an antimicrobial peptide (AMP), cLF36, on growth performance and the histophysiological changes of the intestine in E. coli-challenged broiler chickens. A total number of 360 day old male chicks were randomly assigned to 4 groups of 6 replicates as follows: T1) negative control diet based on corn-soybean meal without E. coli challenge and additives; T2) positive control diet based on corn-soybean meal and challenged with E. coli without any additives; T3) positive control diet challenged with E. coli and supplemented with 20 mg AMP (cLF36)/kg diet; T4) positive control diet challenged with E. coli and supplemented with 45 mg antibiotic (bacitracin methylene disalicylate)/kg diet. Results showed that T3 improved growth performance and the jejunal morphology of E. coli-challenged chickens similar to those of T4. While antibiotic non-selectively decreased the population of ileal bacteria, AMP increased the population of Lactobacillus spp. and decreased harmful bacteria in the ileum of E. coli-challenged chickens. Supplementing E. coli-challenged chickens with AMP improved the gene expression of immune cells and upregulated the expression of tight junction proteins compared to other challenged groups. In conclusion, although cLF36 beneficially affected growth performance and the intestinal morphology of E. coli-challenged chickens similar to those of the antibiotic group, this AMP drastically improved the intestinal microbiome, immune cells, and junctional proteins compared to other E. coli-challenged birds, and can be nominated as an alternative for growth promoter antibiotics.
Subject terms: Bacterial infection, Infection
Introduction
Escherichia coli (E. coli) is a Gram-negative anaerobic bacterium which may play significant roles as the commensal inhabitant of the gastrointestinal microbiota of poultry1,2, while pathogenic strains of E. coli can induce intestinal or extra-intestinal diseases3. Enteric diseases resulting from the colonization of pathogenic E. coli in the gastrointestinal tract of farm animals including poultry causes organ lesion, perihepatitis, airsacculitis, and pericarditis4, which lead to growth retardation, mortality and eventually significant economic losses. A common solution to compensate such growth delay is to add antibiotic growth promoters to feed or water of birds, while antibiotic residues in poultry products and the emergence of antibiotic-resistant pathogens have caused consumers concerns5. These concerns have resulted in restriction or ban of antibiotic growth promoters in the poultry industry of many countries, especially in Europe6,7. Antimicrobial peptides (AMPs) have been recently introduced as potential alternatives to antibiotic growth promoters8.
In general, AMPs are small biological molecules (<10 kDa) containing 12–50 amino acids and having broad-spectrum antimicrobial activity against bacteria, some viruses, and fungi9. The beneficial effects of AMPs on growth performance, gut morphology, nutrient digestibility, intestinal microflora and immune functions of farm animals have been shown previously10–12. More recently, a potent chimeric peptide has been extracted from camel lactoferrin (cLF36) in our lab; its antibacterial13,14 and anticancer15 characteristics have been demonstrated in previous in vitro studies. Although previous research studied the effects of AMPs on different health attributes of animal models in normal conditions, little data is available regarding the effects of AMPs on E. coli-challenged animals, to the best of our knowledge. Therefore, the objective of the present study was to evaluate cLF36 as an alternative to growth promoter antibiotics on growth performance and intestinal morphology microflora, immune cells, and barrier proteins in broiler chickens challenged with E. coli, as an animal model for infectious disease.
Results
Growth performance
The effects of treatments on growth performance attributes are shown in Table 1. Challenging chickens with E. coli decreased (P < 0.05) ADG and impaired (P < 0.05) FCR compared to the NC group. Birds receiving antibiotic had the highest (P < 0.05) daily gain at each rearing interval and over the whole period, while AMP-fed birds had similar weight gain to the NC over the whole experimental period. Although antibiotic increased (P < 0.05) ADFI compared to other treatments at first 10 days of age, none of the treatments affected feed intake at the end of the experiment. Supplementing challenged chickens with AMP improved (P < 0.05) FCR compared to the NC group while having similar results as the antibiotic group.
Table 1.
Effects of treatments on growth performance of broiler chickens from 0 to 24 days of age.
| Treatment | ADG2 (g) | ADFI (g) | FCR (g/g) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 0–10 | 11–24 | 0–24 | 0–10 | 11–24 | 0–24 | 0–10 | 11–24 | 0–24 | |
| NC1 | 16.18b | 47.60b | 63.80b | 22.18b | 74.70 | 96.46ab | 1.37b | 1.56b | 1.51b |
| PC | 15.08c | 44.56c | 59.64c | 22.42b | 74.76 | 94.38b | 1.48a | 1.67a | 1.58a |
| AMP | 16.98ab | 48.16b | 65.12b | 22.52b | 72.12 | 92.62b | 1.33b | 1.50b | 1.42c |
| Antibiotic | 17.32a | 50.60a | 67.92a | 23.86a | 76.64 | 100.50a | 1.38b | 1.51b | 1.48bc |
| SEM3 | 0.222 | 0.541 | 0.737 | 0.185 | 0.632 | 0.923 | 0.017 | 0.019 | 0.015 |
| P-value | 0.001 | 0.001 | 0.001 | 0.005 | 0.077 | 0.006 | 0.007 | 0.005 | 0.001 |
a,bValues within a column with different letters differ significantly (P < 0.05).
1NC: negative control group received corn-soybean meal diet without any challenge and additives; PC: positive control group received NC diet inoculated with E. coli without any additives; AMP: PC received group supplemented with 20 mg antimicrobial peptide/ kg diet; Antibiotic: PC received group supplemented with 45 mg antibiotic (bacitracin methylene disalicylate)/ kg diet.
2ADG: average daily gain; ADFI: average daily feed intake; FCR: feed conversion ratio.
3SEM: standard error of means (results are given as means of 6 pens of 15 birds/treatment).
Intestinal morphology
Table 2 summarizes the effects of treatments on villi morphology in the jejunum of chickens. Birds challenged with E. coli had lower (P < 0.05) VH, thinner (P < 0.05) VW, and lesser (P < 0.05) VSA compared to the NC birds. At 24 days of age, antibiotic and AMP improved (P < 0.05) VH and VSA compared to control group. Experimental diets had no significant effects on CD and VH/CD at either 10 or 24 days of age.
Table 2.
Effects of treatments on villi morphology (µm) in the jejunum of broiler chickens at 10 and 24 days of age.
| Treatment | Day 10 | Day 24 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| VH2 | VW | CD | VH/CD | VSA (mm) | VH | VW | CD | VH/CD | VSA (mm) | |
| NC1 | 583a | 161a | 144 | 4.31 | 295.76a | 1017b | 174a | 187 | 5.68 | 557.02b |
| PC | 455b | 141b | 125 | 3.65 | 201.10b | 827c | 153b | 201 | 5.04 | 396.92c |
| AMP | 643a | 177a | 138 | 4.84 | 356.50a | 1167a | 187a | 171 | 6.06 | 671.47a |
| Antibiotic | 640a | 172a | 121 | 5.11 | 326.72a | 1175a | 186a | 180 | 6.49 | 688.78a |
| SEM3 | 22.512 | 3.958 | 6.602 | 0.286 | 16.473 | 38.576 | 4.249 | 10.575 | 0.314 | 32.201 |
| P-value | 0.004 | 0.001 | 0.610 | 0.306 | 0.001 | 0.001 | 0.001 | 0.816 | 0.448 | 0.001 |
a,bValues within a column with different letters differ significantly (P < 0.05).
1NC: negative control group received corn-soybean meal diet without any challenge and additives; PC: positive control group received NC diet inoculated with E. coli without any additives; AMP: PC received group supplemented with 20 mg antimicrobial peptide/kg diet; Antibiotic: PC received group supplemented with 45 mg antibiotic (bacitracin methylene disalicylate)/kg diet.
2VH: villus height; VW: villus width; CD: crypt depth; VH/CD: the ratio of VH to CD; VSA: villus surface area.
3SEM: standard error of means (results are given as means (n = 12) for each treatment).
Bacterial population
The effects of experimental diets on ileal bacterial populations are shown in Table 3. Challenging chickens with E. coli increased (P < 0.05) the population of harmful bacteria (i.e. E. coli and Clostridium spp.) and decreased (P < 0.05) the colonization of beneficial bacteria (i.e. Lactobacillus spp. and Bifidobacterium spp.) compared to the NC group. At d 10, antibiotic decreased (P < 0.05) the population of Lactobacillus spp. and Bifidobacterium spp., while this antibiotic-supplemented diet reduced (P < 0.05) all bacterial populations at d 24 compared to the NC group. Birds supplemented with AMP had the highest (P < 0.05) population of Lactobacillus spp. and showed a decrease (P < 0.05) in the ileal colonization of E. coli and Clostridium spp. at 24 days of age as compared to birds fed the PC diet.
Table 3.
Effects of treatments on ileal microflora (log10 CFU g−1) in broilers at 10 and 24 days of age.
| Treatments | Day 10 | Day 24 | ||||||
|---|---|---|---|---|---|---|---|---|
| E. coli | Lactobacillus spp. | Bifidobacterium spp. | Clostridium spp. | E. coli | Lactobacillus spp. | Bifidobacterium spp. | Clostridium spp. | |
| NC1 | 4.05b | 6.84ab | 7.04a | 1.55bc | 4.50b | 7.13b | 7.45a | 1.70b |
| PC | 5.25a | 5.71bc | 5.21b | 2.17a | 5.51a | 6.24c | 5.96bc | 2.10a |
| AMP | 4.03b | 7.23a | 6.35ab | 1.80b | 4.13bc | 8.51a | 6.90ab | 1.67b |
| Antibiotic | 4.04b | 5.36c | 5.36b | 1.35c | 3.21c | 6.21c | 6.11c | 1.32c |
| SEM2 | 0.179 | 0.231 | 0.256 | 0.087 | 0.237 | 0.187 | 0.219 | 0.077 |
| P-value | 0.015 | 0.001 | 0.015 | 0.001 | 0.001 | 0.004 | 0.005 | 0.001 |
a–cValues within a column with different letters differ significantly (P < 0.05).
1NC: negative control group received corn-soybean meal diet without any challenge and additives; PC: positive control group received NC diet inoculated with E. coli without any additives; AMP: PC received group supplemented with 20 mg antimicrobial peptide/kg diet; Antibiotic: PC received group supplemented with 45 mg antibiotic (bacitracin methylene disalicylate)/kg diet.
2SEM: standard error of means (results are given as means (n = 12) for each treatment).
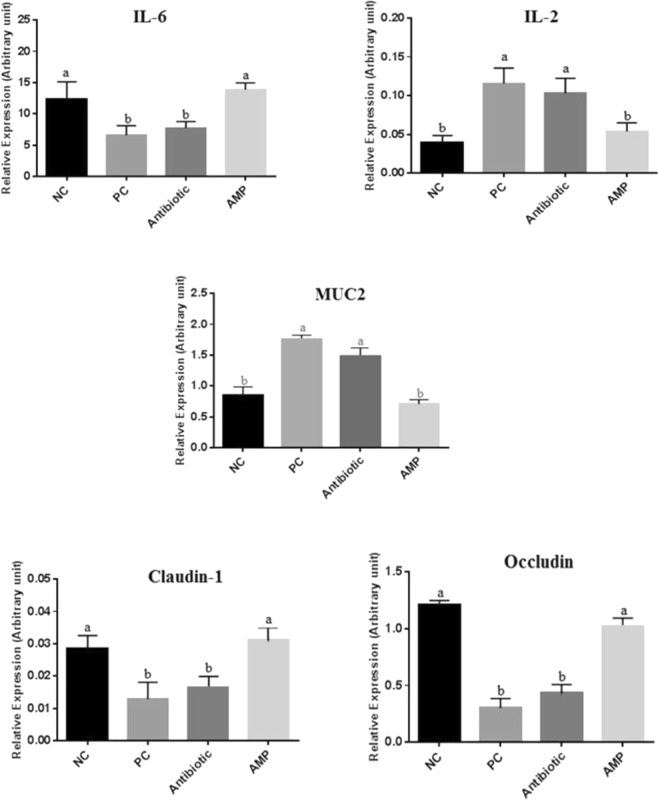
Gene expression of immune cells and tight junction proteins
The effects of experimental diets on gene expression of immune cells and tight junction proteins are shown in Fig. 1. Challenging chickens with E. coli increased (P < 0.05) IL-2 and MUC2 expression, but decreased (P < 0.05) IL-6 expression in the jejunum compared to the NC chickens. Adding AMP to the diet resulted in a reduction (P < 0.05) of IL-2 and MUC2 expression and upregulated (P < 0.05) the expression of IL-6 in the jejunum of E. coli-challenged chickens. Chickens challenged with E. coli had the lowest (P < 0.05) expression pattern of claudin-1 and occludin in the jejunum, while supplementing the diet with antibiotic upregulated (P < 0.05) the expression of tight junction proteins in the jejunum of E. coli-challenged birds. Furthermore, adding antibiotic to the diet of E. coli-challenged chickens did not affect the regulation of immune cells and tight junction proteins in the intestine.
Figure 1.
Effects of treatments on the expression of different genes in the jejunum of broiler chickens on day 24. Samples were analyzed using qPCR, and GAPDH and β-actin were used as the reference genes. Abbreviations as follows: IL-6, interleukin 6; IL-2, interleukin 2; MUC2, mucin 2; NC, negative control birds received a corn-soybean meal basal diet without AMPs, antibiotic and E. coli challenge; PC, positive control birds received NC diet and orally challenged with one ml of E. coli containing 1 × 108 cfu/ml; Antibiotic, birds received PC diet and supplemented with 45 mg antibiotic (bacitracin methylene disalicylate)/kg diet; AMP, birds received PC diet and supplemented with 20 mg peptide/kg diet. The letters on the bar mean show significant difference (P < 0.05).
Discussion
Increasing concerns of antibiotic resistance have encouraged scientists to search for antibiotic alternatives having the beneficial effects of antibiotics on growth performance and health criteria while preventing transmission of resistance to microbial populations, like those observed in AMPs. The present study was conducted to assess the potency of a new source of peptides to replace antibiotics in the diet of E. coli-challenged broiler chickens based on data obtained from productive and health attributes. In agreement with previous studies16,17, the current findings showed that challenging chickens with E. coli retarded growth and impaired performance, while supplementing the diet with AMP attenuated the negative effects of E. coli and improved FCR similar to those of antibiotic-fed birds. The beneficial effects of AMPs on growth performance of broilers under normal11,18 and stressful conditions19 have been observed previously that is consistent with the results of the present study. The morphological characteristics of villi in the jejunum of birds were investigated to find the possible metabolic and physiological action of AMPs on the growth performance of E. coli-challenged birds.
The morphology of villi in the small intestine is known as an indicator of gut health11. In addition, the intestinal lumen is the main site of nutrients absorption which directly depends on villus morphology and surface area20. Morphological analysis in the present study showed that AMP and antibiotic increased VH and VSA in E. coli-challenged birds compared to the control group, which is in agreement with previous studies11,12. Consistent with the present results, Liu et al.21 and Bao et al.18 reported that supplementing the diet with AMPs extracted from pig intestine and rabbit sacculus rotundus, respectively, improved villus morphology in the duodenum and jejunum of broiler chickens. In general, an increase in VH leads to a greater VSA which increases nutrient absorption from the intestinal lumen22 and consequently increases growth performance in birds. In the current study, birds supplemented with peptide and antibiotic had better morphological characteristics compared to the control and E. coli-challenged chickens, which resulted in significant improvement in growth performance.
The intestinal microbiome can significantly affect host gut health through various mechanisms such as nutrients absorption, villi morphology, intestinal pH, mucosal immunity, and transporter gene expression23,24. In the present study, we examined the effects of treatments on the population of two beneficial (Lactobacillus spp. and Bifidobacterium spp.) and two pathogenic (E. coli and Clostridium spp.) bacteria in the ileum of chickens. Antibiotics decreased the population of all bacteria, while AMP significantly improved the community of beneficial bacteria and reduced the colonization of harmful ones in the ileum, which is consistent with previous studies25,26. Bacitracin methylene disalicylate exerts its antibacterial activity on the bacterial ribosome subunit resulting in protein synthesis inhibition27. This decreases the number of bacteria and microbial damage in the gut, since this antibiotic has a wide range of antibacterial action and does not distinguish between types of bacteria27,28 While the definite mechanism by which AMPs can affect the microbial population in the gut has not been found, the suggested mechanism explaining the antimicrobial activity of peptides in controlling the microbial community has been attributed to different surface charges of peptides and pathogens. In detail, AMPs have a net positive charge helping them to electrostatically attach to negatively charged bacterial membranes either to destroy these membranes through physical disruption and/or enzymatic digestion or to pass through the lipid bilayer without exerting any damage. This may interfere with intracellular functions like enzyme activity blockage or inhibiting protein and nucleic acid synthesis29. Our previous results showed that the AMP studied in the current experiment can attach to the bacterial membrane through electrostatic interactions and physically disrupt bacterial bilayer membranes13–15. Consistent with the previous studies30–32, the current results showed that AMP can selectively inhibit the growth of bacteria in the gut which may demonstrate the substantial competitive advantage of cLF36 in comparison to antibiotics.
The invasion of pathogenic bacteria into intestinal epithelial cells and mucosal layer induce the gastrointestinal immune cells to produce cytokines which play different roles in the immune responses to pathogens33. IL-6 is a multifunctional cytokine that promotes B cell differentiation and T cell activation34. Interestingly, IL-6 can play both pro- (i.e. trans-signaling) and anti- (i.e. classic signaling) inflammatory roles under certain conditions depending on the priority of inflammatory response and the pathophysiological context35,36. In agreement with previous findings29,37, supplemented AMP upregulated the expression of IL-6 in the jejunum of E. coli-challenged chickens in the current study. It has been shown that AMPs can induce the differentiation of bone marrow-derived dendritic cells in the intestine to secrete IL-6 against pathogenic bacteria to protect the intestinal layer from ulceration38,39, which may explain the high expression of IL-6 observed in AMP-supplemented group in the current study.
IL-2 is another key cytokine involved in the cellular immune response by T-cell proliferation and the induction of T regulatory responses, and also in the stimulation of B lymphocytes proliferation and immunoglobulin secretion40. In the current study, the expression of IL-2 in the jejunum of chickens was upregulated in response to E. coli challenge, which is in agreement with previous studies in pig and chicken models41,42. Supplementation of AMP to the diet downregulated the expression of IL-2 in the jejunum of E. coli-challenged chickens, which may suggest the anti-inflammatory effect of cLF36 in the intestine, which has been reported for other kinds of AMPs29,37.
Chickens challenged with E. coli in the present study showed an upregulated expression of MUC2, which is in line with previous reports43,44. It was shown that the expression of MUC2 increased in the infectious challenge to secrete more mucin from goblet cells into the intestinal lumen to support the protective layer between the invading bacteria and the epithelial cells45. Adding AMP to the diet downregulated the expression of MUC2 in the jejunum of challenged chickens, which may be attributed to the significant inhibitory effect of cLF36 on E. coli colonization in the intestine (as described above), which is in agreement with previous observation46. In the current study, antibiotic did not attenuate the negative effects of E. coli on MUC2 expression, which is consistent with previous findings showed that antibiotics may eliminate invading pathogens from the intestinal environment, but be unable to restore the normal circumstances of the intestine after pathogen removal47.
It has been well-documented that pathogenic bacteria like E. coli attack the intercellular barriers and disrupt tight junction proteins including claudin-1 and occludin through various mechanisms including chemical degradation by bacterial proteases48,49 or biochemical alterations of actomyosin ring by phosphorylation50 or dephosphorylation51. This is consistent with the current observations that E. coli-challenged birds showed a drastic decrease in the expression of claudin-1 and occludin in the jejunum. However, AMP upregulated the expression of claudin-1 and occludin in the jejunum of E. coli-challenged chickens, which is in agreement with previous studies52,53 reporting AMPs to improve the intestinal epithelial integrity and permeability in the context of E. coli challenge. Although the exact regulatory mechanism of AMPs on tight junction proteins has not been found yet, two possible theories have been suggested. The first theory implies that AMPs may directly activate regulatory proteins (i.e. Rho family) in the intestine of E. coli-challenged mice that increases the expression of junctional proteins and enhances the epithelial barrier function52,54. The second theory deals with the antibacterial effects of AMPs on pathogens that decrease the junctional protein disruption and improve the epithelial barrier integrity55. Interestingly, antibiotic did not increase the expression of claudin-1 and occludin in the jejunum of E. coli-challenged chickens in the current study, while we expected that antibiotic upregulated the junctional proteins due to the antibacterial nature of antibiotics (based on the second above-mentioned theory regarding AMP’s antibacterial effects). In agreement with the present findings, Yi et al.54 demonstrated that antibiotics did not influence the expression of tight junction proteins after pathogens elimination, maybe due to perturbing the intestinal microbial population. Therefore, the findings of present and previous52,54 studies may strengthen the possibility of the first theory attributing the beneficial effects of AMPs on epithelial tight junctions to the expression of regulatory proteins, rather than AMPs’ antimicrobial effects.
In conclusion, the results of the present study suggest that an antimicrobial peptide, cLF36, derived from camel milk can improve growth performance, ameliorate the intestinal morphology changes, and restore gut microbial balance in chickens challenged with E. coli. In addition, supplemented cLF36 may enhance the immune response to E. coli challenge through regulating the expression of cytokines and mucin. Also, cLF36 can improve the intestinal integrity of E. coli-challenged chickens by upregulating the expression of tight junction proteins. Therefore, cLF36 can be introduced as an alternative to growth enhancer antibiotics, based on its beneficial effects observed in the current study, while more research is required to find other contributing aspects of this AMP.
Methods
All experimental protocols involving animals in the present study were approved by Institutional Animal Care and Use Committee of Ferdowsi University of Mashhad (Protocol number 3/42449) and performed following relevant guidelines and regulations to minimize animal pain, suffering, and distress.
Birds, treatments, and experimental design
Three hundred and sixty 1-day-old male chicks (Cobb 500) were purchased from a local commercial hatchery, weighed and randomly placed in floor pens (1.1 m × 1.3 m) covered with wood shavings. Birds were assigned to 4 treatments with 6 replicates containing 15 birds in each replicate. Treatments were as follow: (1) negative control (NC) birds received a corn-soybean meal basal diet without AMPs, antibiotic, and E. coli challenge; (2) positive control (PC) birds received the NC diet and were orally challenged with one ml of E. coli containing 1 × 108 cfu/mL; (3) birds received the PC diet supplemented with 20 mg peptide/kg diet (AMP); (4) birds received PC diet and supplemented with 45 mg antibiotic (bacitracin methylene disalicylate)/kg diet (antibiotic). All diets were in mash form and formulated to meet or exceed the minimum requirements of Cobb 500 (Table 4). Birds had free access to feed and water throughout the experiment and the temperature was set at 32 °C for the first 3 days and then gradually reduced to 21 °C by day 25 which kept constant to the end of the experiment (day 24). The lighting program consisted of 23 L:1D during the first 5 days and then gradually changed to 16 L:8D on day 10 and kept constant to the end of the experiment.
Table 4.
Composition of experimental diets.
| Ingredient (%)1 | Starter (0–10 days) | Grower (11–24 days) |
|---|---|---|
| Corn | 56.81 | 58.16 |
| Soybean meal (44.0%) | 36.01 | 34.85 |
| Soybean oil | 3.18 | 3.35 |
| Dicalcium phosphate | 1.79 | 1.65 |
| Limestone | 0.97 | 0.93 |
| Salt | 0.35 | 0.30 |
| Mineral-vitamin premix2 | 0.50 | 0.50 |
| DL-Methionine | 0.17 | 0.15 |
| L-Lysine HCl | 0.22 | 0.12 |
| Calculated nutrients | ||
| AME (kcal/kg) | 3000 | 3025 |
| Crude protein (%) | 21.0 | 19.0 |
| Calcium (%) | 0.90 | 0.84 |
| Available phosphorus (%) | 0.45 | 0.42 |
| Sodium (%) | 0.16 | 0.16 |
| Methionine (%) | 0.50 | 0.47 |
| Methionine + cysteine (%) | 0.98 | 0.86 |
| Lysine (%) | 1.32 | 1.18 |
1Antibiotic (45 mg bacitracin methylene disalicylate/kg diet) and peptide (20 mg/kg diet) were added on top and thoroughly mixed.
2Added per kg of feed: vitamin A, 7,500 UI; vitamin D3 2100 UI; vitamin E, 280 UI; vitamin K3, 2 mg; thiamine, 2 mg; riboflavin, 6 mg; pyridoxine, 2.5 mg; cyanocobalamin, 0.012 mg, pantothenic acid, 15 mg; niacin, 35 mg; folic acid, 1 mg; biotin, 0.08 mg; iron, 40 mg; zinc, 80 mg; manganese, 80 mg; copper, 10 mg; iodine, 0.7 mg; selenium, 0.3 mg.
AMP production
The AMP used in the present study was derived from camel lactoferrin (cLF) consisting of 42 amino acids which was generated in our lab recently (for more details regarding the peptide cLF chimera production, review previous works13–15). Briefly, preparation of recombinant plasmid vector was conducted through transforming synthetic cLFchimera into DH5α bacterium13–15. Next, the latter bacterial colonies were cultured to harvest plasmid extraction. Then, the recombinant vector was transferred into E. coli (DE3) as an expression host and cultured in 2 mL Luria-Bertani broth (LB) medium for overnight according to standard protocol56. In the next step, cultured materials were inoculated in 50 mL LB and incubated at 37 °C with shaking at 200 rpm. Then, isopropyl-β-D-thiogalactopyranoside (IPTG) was added to a final concentration of 1 mM and incubated at 37 °C for 6 h after IPTG induction. Periplasmic protein was collected at different times after IPTG induction (2, 4 and 6 h) according to the method described by de Souza Cândido et al.57 and analyzed on 12% SDS-PAGE. To purify expressed peptide, Ni-NTA agarose column was used based on the manufacturer’s instruction (Thermo, USA). The quality of purified recombinant peptide was assessed on a 12% SDS-PAGE gel electrophoresis, while the Bradford method58 was used to analyze the quantity of recombinant peptide. More recently, an E. coli expression system14 was developed in our laboratory that is able to produce 0.42 g/L of recombinant peptide. In the current study, 4 g peptide previously obtained from the recombinant E. coli were purified, lyophilized, and thoroughly mixed with 1 kg soybean meal and then supplemented to the relevant experimental diets. The inhibitory effects of this AMP on various plant13 and poultry14 pathogens were recently observed in in vitro.
E. coli challenge
The method of E. coli challenge was explained in details elsewhere17 with some minor differences. In summary, a suspension of E. coli (ATCC 31616) was cultured on MacConkey agar plates (Merck, Germany) for 24 h at 37 °C, and pink, round medium-sized colonies were picked as E. coli suspect colonies to prepare the inocula. Next, E.coli K99 was inoculated in LB medium and incubated at 37 °C for 24 h. Cell bacteria density was determined in the medium by the subculture of bacteria after making a serial dilution. Bacteria were adjusted to 108 cfu/ml by diluting in 0.5% peptone solution. On d 7, chicks were orally challenged with 1 ml of prepared inoculation containing 1 × 108 cfu E. coli, while non-challenged chicks received 1 ml of sterile peptone water.
Growth performance
Body weight (BW) and feed remaining of each pen were weighed on days 10 and 24 to measure the average daily gain (ADG), average daily feed intake (ADFI) and feed conversion ratio (FCR) over the specific and entire periods of experiment (0–10, 11–24, and 0–24 days of age). Mortality per pen was recorded daily in order to adjust FCR accordingly.
Sample collection
Two birds from each pen (12 birds/treatment) were randomly selected on days 10 and 24, euthanized by cervical dislocation, the viscera was excised, the intestine was discreetly separated from the whole viscera, and the adherent materials were precisely removed. The ileum was gently pressed to aseptically collect ileal content into sterile tubes for microbiological analysis. A section (about 5 cm) from mid-jejunal tissues was meticulously separated for morphological analysis. A 2 cm section from the mid-jejunum was detached, rinsed in cold phosphate-buffered saline (PBS), immediately immersed in RNAlater (Qiagen, Germantown, MD) and stored at −20 °C for subsequent gene expression determination.
Intestinal morphology
The method described by Daneshmand et al.59 was used to prepare samples for morphometry analysis. In summary, jejunal and ileal samples were stored in a 10% formaldehyde phosphate buffer for 48 h. Then, the samples were trimmed and processed on a tissue processor (Excelsior™ AS, Thermo Fisher Scientific, Loughborough, UK), fixed in paraffin using an embedder (Thermo Fisher Histo Star Embedder, Loughborough, UK) and cut with a microtome (Leica HI1210, Leica Microsystems Ltd., Wetzlar, Germany) to a slice of 3 μm, placed on a slide and dehydrated on a hotplate (Leica ASP300S, Leica Microsystems Ltd., Wetzlar, Germany). Then, the prepared samples were dyed with hematoxylin and eosin and examined under a microscope (Olympus BX41, Olympus Corporation, Tokyo, Japan). A total of 8 slides were prepared from the jejunal segment per bird, and 10 individual well-oriented villi were measured per prepared slide (80 villi/bird). The average of slide measurements per sample was stated as a mean for each bird. Villus width (VW) was measured at the base of each villus; villus height (VH) from the top of the villus to the villus-crypt junction, crypt depth (CD) from the base of the adjacent villus to the sub-mucosa, the ratio of VH to CD and villus surface area were calculated.
Microbial count
The method explained by Kermanshahi et al.60 was used to count the populations of E. coli, Clostridium spp., Lactobacillus spp., and Bifidobacterium spp. in the collected ileal content. Briefly, the ileal contents of a sample were thoroughly mixed, serially diluted 10-fold from 10−1 to 10−7 with sterile PBS and homogenized for 3 minutes. Then, dilutions were plated on different agar mediums. Regarding the enumeration of bacteria, Lactobacillus spp. and Clostridium spp. dilutions were plated on MRS agar (Difco, Laboratories, Detroit, MI) and SPS agar (Sigma, Germany) and anaerobically cultured at 37 °C for 48 h. Black colonies in SPS agar medium were recorded as the count of Clostridium spp. Eosin Methylene Blue (EMB) agar (Merck, Darmstadt, Germany) and BSM agar (Sigma-Aldrich, Germany) were used to cultivate E. coli and Bifidobacterium spp. respectively, and incubated at 37 °C for 24 h. All microbiological analyses were performed in triplicate, average values were used for statistical analyses and results were expressed in colony-forming units (Log10 cfu/g of ileal content).
RNA extraction and gene expression
The procedure of RNA extraction and gene expression was described previously61. In summary, total RNA was extracted from chicken jejunum sampled on day 24 using the total RNA extraction kit (Pars Tous, Iran) following the manufacturer’s instructions. Purity and quality of extracted RNA were evaluated using an Epoch microplate spectrophotometer (BioTek, USA) based on 260/230 and 260/280 wavelength ratios, respectively. Genomic DNA was removed using DNase I (Thermo Fisher Scientific, Austin, TX, USA). The complementary DNA (cDNA) was synthetized from 1 µg of total RNA using the Easy cDNA synthesis kit (Pars Tous, Iran) following the manufacturer’s protocol.
Gene expression of two references (GAPDH and β-actin) and five targets (Interleukin-1 [IL-1], IL-6, mucin2 [MUC2], Claudin-1 [CLDN1], and Occludin [OCLN]) genes were determined by quantitative real-time PCR (qRT-PCR) based on MIQE guidelines62. Each reaction was performed in a total volume of 20 μl in duplicate using an ABI 7300 system (Applied Biosystems, Foster City, CA) and 2 × SYBR Green Real Time-PCR master mix (Pars Tous, Iran). Primer details are shown in Table 5. All primers were designed according to MIQE criteria62 regarding amplification length and intron spanning. All efficiencies were between 90 and 110% and calculated R2 was 0.99 for all reactions. The method 2−ΔΔCt Ct63 was used to calculate relative gene expression in relation to the reference genes (GAPDH and β-actin).
Table 5.
Sequences of primer pairs used for amplification of the target and reference genes1.
| Gene2 | Strand | Sequence (5′ → 3′) | Ta | Product size (bp) | GenBank Accession No. |
|---|---|---|---|---|---|
| IL-2 | Forward | TTATGGAGCATCTCTATCATCAGCA | 63 | 122 | XM_01576098.1 |
| Reverse | CCTGGGTCTCAGTTGGTGTGTAG | ||||
| IL-6 | Forward | CTGTTCGCCTTTCAGACCTACC | 63 | 141 | NM_204628.1 |
| Reverse | GACCACTTCATCGGGATTTATCA | ||||
| MUC2 | Forward | ATGCGATGTTAACACAGGACTC | 60 | 110 | BX930545 |
| Reverse | GTGGAGCACAGCAGACTTTG | ||||
| CLDN1 | Forward | CATACTCCTGGGTCTGGTTGGT | 60 | 100 | NM_001013611.2 |
| Reverse | GACAGCCATCCGCATCTTCT | ||||
| OCLDN | Forward | CGCAGTCCAGCGGTTACTA | 58 | 178 | NM_205128.1 |
| Reverse | AGGATGACGATGAGGAACCCA | ||||
| GAPDH | Forward | TTGTCTCCTGTGACTTCAATGGTG | 63 | 128 | NM_204305 |
| Reverse | ACGGTTGCTGTATCCAAACTCAT | ||||
| β-Actin | Forward | CCTGGCACCTAGCACAATGAA | 63 | 175 | NM_205518.1 |
| Reverse | GGTTTAGAAGCATTTGCGGTG |
1For each gene the primer sequence for forward and reverse (5′ → 3′), the product size (bp), and the annealing temperature (Ta) in °C are shown.
2IL-, interleukin-; MUC2, mucin2; CLDN1, claudin1, OCLDN, occludin; GAPDH, Glyceraldehyde 3-phosphate dehydrogenase.
Statistical analysis
Data were statistically analyzed in a completely randomized design by ANOVA using the General Linear Model (GLM) procedure of SAS (SAS Inst., Inc., Cary, NC). Tukey’s test was used to compare differences among means of treatments and P values < 0.05 were considered to be significant.
Author Contributions
A.D. performed the experiment and wrote the main manuscript text. H.K. contributed to the experimental design. M.H.S. contributed to the writing of the manuscript. A.J. analysed the data and contributed to the experimental design. M.A. performed the experiment. All authors approved the submitted version.
Data Availability
All data generated or analysed during this study are included in this published article.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Nakazato G, De Campos TA, Stehling EG, Brocchi M. Virulence factors of avian pathogenic Escherichia coli (APEC) Pesq. Vet. Bras. 2009;29:479–486. doi: 10.1590/S0100-736X2009000700001. [DOI] [Google Scholar]
- 2.Dheilly A, Bouder A, Le Devendec L, Hellard G, Kempf I. Clinical and microbial efficacy of antimicrobial treatments of experimental avian colibacillosis. Vet. Microbiol. 2011;149:422–9. doi: 10.1016/j.vetmic.2010.11.033. [DOI] [PubMed] [Google Scholar]
- 3.Dho-Moulin M, Fairbrother JM. Avian pathogenic Escherichia coli (APEC) Vet. Res. 1999;30:299–316. [PubMed] [Google Scholar]
- 4.Barnes, H. J. & Gross, W. B. Colibacillosis. In Diseases of Poultry (ed. 10th) 131–141 (Iowa State University Press, 1997).
- 5.Vandemaele F, Goddeeris BM, Vereecken M. Incidence and antibiotic resistance of pathogenic Escherichia coli among poultry in Belgium. Vet. Rec. 2002;151:355–356. doi: 10.1136/vr.151.12.355. [DOI] [PubMed] [Google Scholar]
- 6.European Commission, Regulation No. 1831. Preprint at: http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2003:268:0029:0043:EN:PDF (2003).
- 7.Khan SH, Iqbal J. Recent advances in the role of organic acids in poultry nutrition. J. Appl. Anim. Res. 2016;44:359–369. doi: 10.1080/09712119.2015.1079527. [DOI] [Google Scholar]
- 8.Wang S, Zeng X, Yang Q, Qiao S. Antimicrobial peptides as potential alternatives to antibiotics in food animal industry. Int. J. Mol. Sci. 2016;17:E603. doi: 10.3390/ijms17050603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lai Y, Gallo RL. AMPed up immunity: How antimicrobial peptides have multiple roles in immune defense. Trends Immunol. 2009;30:131–141. doi: 10.1016/j.it.2008.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yoon JH, et al. Effects of dietary supplementation with antimicrobial peptide-P5 on growth performance, apparent total tract digestibility, faecal and intestinal microflora and intestinal morphology of weanling pigs. J. Sci. Food Agric. 2013;93:587–592. doi: 10.1002/jsfa.5840. [DOI] [PubMed] [Google Scholar]
- 11.Choi SC, et al. Effects of dietary supplementation with an antimicrobial peptide-P5 on growth performance, nutrient retention, excreta and intestinal microflora and intestinal morphology of broilers. Anim. Feed Sci. Technol. 2013;85:78–84. doi: 10.1016/j.anifeedsci.2013.07.005. [DOI] [Google Scholar]
- 12.Choi SC, et al. An antimicrobial peptide-A3: Effects on growth performance, nutrient retention, intestinal and faecal microflora and intestinal morphology of broilers. Br. Poult. Sci. 2013;54:738–746. doi: 10.1080/00071668.2013.838746. [DOI] [PubMed] [Google Scholar]
- 13.Tanhaeian A, Ahmadi FS, Sekhavati MH, Mamarabadi. M. Expression and purification of the main component contained in camel milk and its antimicrobial activities against bacterial plant pathogens. Probiotics Antimicrob. Proteins. 2018;10:1–7. doi: 10.1007/s12602-018-9416-9. [DOI] [PubMed] [Google Scholar]
- 14.Tanhaeian A, Azghandi M, Razmyar J, Mohammadi E, Sekhavati MH. Recombinant production of a chimeric antimicrobial peptide in E. coli and assessment of its activity against some avian clinically isolated pathogens. Microb. Pathog. 2018;122:73–78. doi: 10.1016/j.micpath.2018.06.012. [DOI] [PubMed] [Google Scholar]
- 15.Tanhaeian Abbas, Jaafari Mahmoud Reza, Ahmadi Farajollah Shahriari, Vakili‐Ghartavol Roghayyeh, Sekhavati Mohammad Hadi. Secretory Expression of a Chimeric Peptide in Lactococcus lactis: Assessment of its Cytotoxic Activity and a Deep View on Its Interaction with Cell-Surface Glycosaminoglycans by Molecular Modeling. Probiotics and Antimicrobial Proteins. 2018;11(3):1034–1041. doi: 10.1007/s12602-018-9496-6. [DOI] [PubMed] [Google Scholar]
- 16.Matsuda K, Chaudhari AA, Lee JH. Avian colibacillosis caused by an intestinal pathogenic Escherichia coli isolate from calf diarrhea. Res. Vet. Sci. 2010;89:150–152. doi: 10.1016/j.rvsc.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 17.Khodambashi Emami N, Daneshmand A, Naeini SZ, Graystone EN, Broom LJ. Effects of commercial organic acid blends on male broilers challenged with E. coli K88: performance, microbiology, intestinal morphology, and immune response. Poult. Sci. 2017;96:3254–3263. doi: 10.3382/ps/pex106. [DOI] [PubMed] [Google Scholar]
- 18.Bao H, et al. Effects of pig antibacterial peptides on growth performance and intestine mucosal immune of broiler chickens. Poult. Sci. 2009;88:291–297. doi: 10.3382/ps.2008-00330. [DOI] [PubMed] [Google Scholar]
- 19.Hu F, et al. Effects of antimicrobial peptides on growth performance and small intestinal function in broilers under chronic heat stress. Poult. Sci. 2017;96:798–806. doi: 10.3382/ps/pew379. [DOI] [PubMed] [Google Scholar]
- 20.Hampson DJ. Alteration in piglet small intestinal structure at weaning. Res. Vet. Sci. 1986;40:32–40. doi: 10.1016/S0034-5288(18)30482-X. [DOI] [PubMed] [Google Scholar]
- 21.Liu T, et al. Effects of rabbit sacculus rotundus antimicrobial peptides on the intestinal mucosal immunity in chickens. Poult. Sci. 2008;87:250–254. doi: 10.3382/ps.2007-00353. [DOI] [PubMed] [Google Scholar]
- 22.Caspary WF. Physiology and pathophysiology of intestinal absorption. Am. J. Clin. Nutr. 1992;55:299–308. doi: 10.1093/ajcn/55.1.299s. [DOI] [PubMed] [Google Scholar]
- 23.Apajalahti J, Kettunen A, Graham H. Characteristics of the gastrointestinal microbial communities, with special reference to the chicken. World’s Poult. Sci. J. 2004;60:223–232. doi: 10.1079/WPS20040017. [DOI] [Google Scholar]
- 24.Castanys-Muñoz E, Martin MJ, Vazquez E. Building a beneficial microbiome from birth. Adv. Nutr. 2016;7:323–30. doi: 10.3945/an.115.010694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tang JYH, MohamadGhazali F, AbdulAziz S, Nishibuchi M, Radu S. Comparison of thermophilic Campylobacter spp. occurrence in two types of retail chicken samples. Int. Food Res. J. 2009;16:277–288. [Google Scholar]
- 26.Ohh SH, et al. Effects of potato (Solanum tuberosum L. cv.golden valley) protein on performance, nutrient metabolizability, and cecal microflora in broilers. Arch. Geflügelk. 2010;74:30–35. [Google Scholar]
- 27.Proctor A, Phillips GJ. Differential effects of bacitracin methylene disalicylate (BMD) on the distal colon and cecal microbiota of young broiler chickens. Front. Vet. Sci. 2019;6:114. doi: 10.3389/fvets.2019.00114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Koltes DA, et al. Effects of bacitracin methylene disalicylate and diet change on gastrointestinal integrity and endotoxin permeability in the duodenum of broiler chicken. BMC Res. Notes. 2017;10:470. doi: 10.1186/s13104-017-2781-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Muniz LR, Knosp C, Yeretssian G. Intestinal antimicrobial peptides during homeostasis, infection, and disease. Front. Immun. 2012;3:310. doi: 10.3389/fimmu.2012.00310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ocana VS, de Ruiz Holgado AA, Nader-Macias ME. Growth inhibition of Staphylococcus aureus by H2O2-producing Lactobacillus paracasei subsp. paracasei isolated from the human vagina. FEMS Immunol. Med. Microbiol. 1999;23:87–92. doi: 10.1016/S0928-8244(98)00116-3. [DOI] [PubMed] [Google Scholar]
- 31.Perdigon G, Fuller R, Raya R. Lactic acid bacteria and their effect on the immune system. Curr. Issues Intest. Microbiol. 2001;2:27–42. [PubMed] [Google Scholar]
- 32.Alakomi HL, et al. Lactic acid permeabilizes gram-negative bacteria by disrupting the outer membrane. Appl. Environ. Microbiol. 2000;66:2001–2005. doi: 10.1128/AEM.66.5.2001-2005.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kayamuro H, et al. Interleukin1 family cytokines as mucosal vaccine adjuvants for induction of protective immunity against influenza virus. J. Virol. 2010;84:12703–12712. doi: 10.1128/JVI.01182-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kishimoto T. IL-6, from its discovery to clinical applications. Int. Immunol. 2010;22:347–352. doi: 10.1093/intimm/dxq030. [DOI] [PubMed] [Google Scholar]
- 35.Scheller J, Chalaris A, Schmidt-Arras D, Rose-John S. The pro- and anti-inflammatory properties of the cytokine interleukin-6. Biochim. Biophys. Acta. 2011;1813:878–888. doi: 10.1016/j.bbamcr.2011.01.034. [DOI] [PubMed] [Google Scholar]
- 36.Dann SM, et al. IL-6-dependent mucosal protection prevents establishment of a microbial niche for attaching/effacing lesion-forming enteric bacterial pathogens. J. Immunol. 2008;180:6816–6826. doi: 10.4049/jimmunol.180.10.6816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kolls JK, McCray PB, Jr., Chan YR. Cytokine-mediated regulation of antimicrobial proteins. Nat. Rev. Immunol. 2008;8:829–835. doi: 10.1038/nri2433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Davidson DJ, et al. The cationic antimicrobial peptide LL-37 modulates dendritic cell differentiation and dendritic cell induced T cell polarization. J. Immunol. 2004;172:1146–1156. doi: 10.4049/jimmunol.172.2.1146. [DOI] [PubMed] [Google Scholar]
- 39.Kamble NM, Jawale CV, Lee JH. Activation of chicken bone marrow-derived dendritic cells induced by a Salmonella enteritidis ghost vaccine candidate. Poult. Sci. 2016;95:2274–2280. doi: 10.3382/ps/pew158. [DOI] [PubMed] [Google Scholar]
- 40.Malek TR. The biology of interleukin-2. Annu. Rev. Immunol. 2008;26:453–79. doi: 10.1146/annurev.immunol.26.021607.090357. [DOI] [PubMed] [Google Scholar]
- 41.Zhang F, et al. Dietary N-carbamylglutamate supplementation boosts intestinal mucosal immunity in Escherichia coli challenged piglets. Plos One. 2013;8:e66280. doi: 10.1371/journal.pone.0066280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wang S, et al. Prevention of Escherichia coli infection in broiler chickens with Lactobacillus plantarum B1. Poult Sci. 2017;96:2576–2586. doi: 10.3382/ps/pex061. [DOI] [PubMed] [Google Scholar]
- 43.McGuckin MA, Linden SK, Sutton P, Florin TH. Mucin dynamics and enteric pathogens. Nat. Rev. Microbiol. 2011;9:265–278. doi: 10.1038/nrmicro2538. [DOI] [PubMed] [Google Scholar]
- 44.Zapata D, Rodríguez B, Ramírez M, López A, Parra J. Escherichia coli lipopolysaccharide affects intestinal mucin secretion in weaned pigs. Rev. Colomb. Ciencias Pecuar. 2015;28:209–217. [Google Scholar]
- 45.de Barros Moreira Filho AL, et al. High Incubation Temperature and Threonine Dietary Level Improve Ileum Response Against Post-Hatch Salmonella Enteritidis Inoculation in Broiler Chicks. PLoS ONE. 2015;10:e0131474. doi: 10.1371/journal.pone.0131474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gao X, et al. Chronic stress promotes colitis by disturbing the gut microbiota and triggering immune system response. Proc. Natl. Acad. Sci. USA. 2018;115:E2960–E2969. doi: 10.1073/pnas.1720696115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gadde U, et al. The effects of direct-fed microbial supplementation, as an alternative to antibiotics, on growth performance, intestinal immune status, and epithelial barrier gene expression in broiler chickens. Probiotics Antimicrob. Proteins. 2017;9:397–405. doi: 10.1007/s12602-017-9275-9. [DOI] [PubMed] [Google Scholar]
- 48.Van Itallie CM, Anderson JM. Architecture of tight junctions and principles of molecular composition. Semin. Cell Dev. Biol. 2014;36:157–165. doi: 10.1016/j.semcdb.2014.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang Q, et al. Enteropathogenic Escherichia coli changes distribution of occludin and ZO-1 in tight junction membrane microdomains in vivo. Microb. Pathog. 2010;48:28–34. doi: 10.1016/j.micpath.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 50.Ugalde-Silva P, Gonzalez-Lugo O, Navarro-Garcia F. Tight junction disruption induced by type 3 secretion system effectors injected by enteropathogenic and enterohemorrhagic Escherichia coli. Front. Cell. Infect. Microbiol. 2016;6:87. doi: 10.3389/fcimb.2016.00087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Simonovic I, Rosenberg J, Koutsouris A, Hecht G. Enteropathogenic Escherichia coli dephosphorylates and dissociates occludin from intestinal epithelial tight junctions. Cell. Microbiol. 2000;2:305–315. doi: 10.1046/j.1462-5822.2000.00055.x. [DOI] [PubMed] [Google Scholar]
- 52.Yi H, et al. High therapeutic efficacy of cathelicidin-WA against postweaning diarrhea via inhibiting inflammation and enhancing epithelial barrier in the intestine. Sci. Rep. 2016;6:25679. doi: 10.1038/srep25679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yu H, et al. Protective ability of biogenic antimicrobial peptide microcin j25 against enterotoxigenic Escherichia Coli-induced intestinal epithelial dysfunction and inflammatory responses IPEC-J2 cells. Front. Cell. Infect. Microbiol. 2018;8:242. doi: 10.3389/fcimb.2018.00242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yi H, Hu W, Chen S, Lu Z, Wang YJ. Cathelicidin-WA improves intestinal epithelial barrier function and enhances host defense against enterohemorrhagic Escherichia coli O157:H7 infection. Immunol. 2017;198:1696–1705. doi: 10.4049/jimmunol.1601221. [DOI] [PubMed] [Google Scholar]
- 55.Robinson K, Deng Z, Hou Y, Zhang G. Regulation of the intestinal barrier function by host defense peptides. Front. Vet. Sci. 2015;2:57. doi: 10.3389/fvets.2015.00057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sambrook, J., Fritsch, E. F. & Maniatis, T. Molecular Cloning: a Laboratory Manual (second ed.) (Cold spring harbor laboratory press, 1989).
- 57.de Souza Cândido E, et al. The use of versatile plant antimicrobial peptides in agribusiness and human health. Peptides. 2014;55:65–78. doi: 10.1016/j.peptides.2014.02.003. [DOI] [PubMed] [Google Scholar]
- 58.Bradford MM. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal. Biochem. 1976;72:248–254. doi: 10.1016/0003-2697(76)90527-3. [DOI] [PubMed] [Google Scholar]
- 59.Daneshmand A, Kermashahi H, Danesh Mesgaran M, King AJ, Ibrahim SA. Effect of purine nucleosides on growth performance, gut morphology, digestive enzymes, serum profile and immune response in broiler chickens. Br. Poult. Sci. 2017;58:536–543. doi: 10.1080/00071668.2017.1335859. [DOI] [PubMed] [Google Scholar]
- 60.Kermanshahi H, et al. Effects of acidified yeast and whey powder on performance, organ weights, intestinal microflora, and gut morphology of male broilers. Braz. J. Poult. Sci. 2017;19:309–316. doi: 10.1590/1806-9061-2016-0351. [DOI] [Google Scholar]
- 61.Kermanshahi H, Ghofrani Tabari D, Khodambashi Emami N, Daneshmand A, Ibrahim SA. Effect of in ovo injection of threonine on immunoglobulin A gene expression in the intestine of Japanese quail at hatch. J. Anim. Physiol. Anim. Nutr. 2017;101:10–14. doi: 10.1111/jpn.12543. [DOI] [PubMed] [Google Scholar]
- 62.Bustin SA, et al. The MIQE guidelines: minimum information for publication of quantitative real-time PCR experiments. Clin. Chem. 2009;55:611–622. doi: 10.1373/clinchem.2008.112797. [DOI] [PubMed] [Google Scholar]
- 63.Pfaffl MW. A new mathematical model for relative quantification in real-time RT-PCR. Nucleic Acids Res. 2001;29:45e–45. doi: 10.1093/nar/29.9.e45. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analysed during this study are included in this published article.