Abstract
This study aimed to compare the catastrophic health expenditure (CHE) and impoverishment of type 2 diabetes mellitus (T2DM) patients between 2 ethnic groups and explore the contribution of associated factors to ethnic differences in CHE and impoverishment in Ningxia Hui Autonomous Region, China.
A cross-sectional study was conducted in 2 public hospitals from October 2016 to June 2017. Data were collected by interviewing eligible Hui and Han T2DM inpatients and reviewing the hospital electronic records. Both CHE and impoverishment were measured by headcount and gap. The contributions of associated factors to ethnic differences were analyzed by the Blinder–Oaxaca decomposition technique.
Both the CHE and impoverishment of Hui patients before and after reimbursement were significantly higher than those of Han patients. The ethnic differences in CHE and impoverishment headcount after reimbursement were 11.9% and 9.8%, respectively. The different distributions of associated factors between Hui and Han patients contributed to 60.5% and 35.7% of ethnic differences in CHE and impoverishment, respectively. Household income, occupation, and region were significant contributing factors.
Hui T2DM patients suffered greater CHE and impoverishment than Han patients regardless of reimbursements from health insurance. Differences in socioeconomic status between Hui and Han patients were the main factors behind the ethnic differences.
Keywords: Blinder–Oaxaca decomposition, catastrophic health expenditure, impoverishment, type 2 diabetes mellitus
1. Introduction
The global prevalence of diabetes mellitus (DM) has been rapidly increasing as a result of ageing populations, lifestyle changes, and associated rapid unplanned urbanization.[1] 90% to 95% of the increased DM burden is type 2 diabetes mellitus (T2DM).[2,3] The lifelong assessment or treatment of T2DM and its complications account for substantial medical and nonmedical costs and productivity loss among patients, households, and society.[4,5] Although some countries have health insurance systems which cover some of the DM costs, high out-of-pocket (OOP) payments for T2DM are still a problem for many patients due to inefficient risk-sharing mechanisms or low household economics attributing to catastrophic health expenditure (CHE) and impoverishment.[6,7]
CHE and impoverishment due to T2DM impact disproportionately those who are socially and economically vulnerable, including ethnic minorities.[8,9] Studies have also found that ethnic minorities were more likely to have uncontrolled T2DM and complications due to various factors including predisposing genetic factors, geographical barriers, low socioeconomic status, and different cultural beliefs.[10–12] These ethnic minorities were also more susceptible to financial risks than the general populations.[7] Substantial financial hardships create barriers to health services utilization for T2DM among ethnic minorities, leading to more serious health problems.[13,14]
China became the global epicenter of the DM epidemic with 11.6% of the national adult population with T2DM in 2010.[15] People with T2DM suffer significantly higher personal and family economic burdens compared with nondiabetic people in China.[16] The proportion of OOP payments for T2DM in total health expenditures in China has been reduced after introduction of 3 basic medical insurance schemes in 2011 which cover almost all of the Chinese population.[17] However, the households with T2DM patients under these insurance schemes suffered financial hardship when the patients received DM-related health services. Three previous studies in China reported high rates of catastrophic health expenditure among DM patients, but impoverishment was not measured and the majority of participants lived in rural areas.[8,18,19] Ethnic minorities are approximately 8.5% of the total population in China. The Hui ethnic minority is the second largest ethnic group in China, mostly living in Ningxia province. All health insurance plans have been similarly implemented regardless of general population or ethnic minorities.[20]
Understanding the ethnic differences in financial risk imposed by health payments and the factors associated with these differences could lead to more effective efforts to reduce this problem.[21] However, to date there have been only a few studies which have attempted to assess differences in financial risk between general populations and ethnic minorities. This study aimed to assess ethnic differences in CHE and impoverishment of T2DM patients and explore the contribution of associated factors to ethnic differences in CHE and impoverishment in Ningxia Hui Autonomous Region, China. The findings from this study provide useful information for the country's consideration of resource allocation to ensure effective universal health coverage for T2DM patients, particularly among ethnic minorities.
2. Methods
2.1. Study design and setting
A cross-sectional study was conducted in 2 large tertiary public hospitals located in the capital city of Yinchuan of Ningxia Hui Autonomous Region, China from October 13, 2016 to June 19, 2017. The research was approved by the Human Research Ethics Committee, Faculty of Medicine, Prince of Songkla University, and the Medical Ethics Committee, Ningxia Medical University. Both of the study hospitals provide healthcare services to the entire population of Ningxia province. Primary care for T2DM in Ningxia is limited, thus hospital-based services are the main healthcare services for T2DM.
There are 3 basic public medical insurance schemes available to the residents of Ningxia, namely, the New Rural Cooperative Medical System (NRCMS), the Urban Resident Basic Medical Insurance Scheme (URBMI), and the Urban Employee Basic Medical Insurance Scheme (UEBMI).[22] The target populations for the NRCMS, URBMI, and UEBMI schemes are rural residents, urban residents, and urban employees, respectively.[23] Benefit packages cover both inpatient and outpatient care, but the reimbursement rates are different, ranging from 40% to 90% depending on the type of insurance scheme and hospital where the services are received.[24]
2.2. Participants
All patients aged 18 years or above, diagnosed as T2DM for ≥12 months with the International Classification of Disease 10th version (ICD-10) coding E11, and admitted to the participating hospitals during the study period, were included. Patients with other serious illnesses or who were unable to communicate effectively were excluded.
The sample size was calculated using a formula for comparing the proportion of CHE between Hui and Han patients. A previous study with the same estimation measurement standards showed that the incidence of CHE for diabetes patients in developing countries was about 17% [6]. With an estimation of 12% difference in CHE, we assumed figures of 22% CHE among Hui patients and 10% CHE among Han patients. Given a type I error of 5% and a power of 90%, ≥211 Hui patients and 211 Han patients were required. Allowing for a 10% nonresponse rate, 240 Hui patients and 240 Han patients were recruited for this study. Due to the effect of T2DM complications on healthcare expenditures, we enrolled similar numbers of patients with complications between the Hui and Han ethnic groups.
2.3. Variable definitions and measurements
We defined the annual healthcare expenditures for T2DM as including both the medical and nonmedical costs incurred by patients and family members for transportation, accommodation, and also costs of productivity loss for both outpatient and inpatient T2DM services in the prior 12 months. OOP payments were reduced by the amount of any health insurance reimbursement from annual healthcare expenditures. CHE and impoverishment due to payments for T2DM health care were the main outcome measures, and were measured in terms of the headcount (incidence) and gap (intensity) before and after reimbursement from their health insurance.
The CHE headcount was calculated based on the percentage of individuals whose healthcare payments equaled or exceeded 40% of a household's capacity to pay.[25] The household's capacity to pay was calculated as the difference between household consumption expenditures and subsistence consumption expenditures. The household consumption expenditures referred to the spending on all goods and services in the prior 12 months in a household. Subsistence expenditures were calculated as the average food expenditures of a household whose food expenditures share of total household expenditures was within the 45th to 55th percentile range, adjusted for household size according to a consumption equivalence scale (actual household size0.56). The mean CHE gap reflects the CHE intensity which measures the average degree by which payments, expressed as the proportion of the capacity to pay, exceed the threshold 40%.
Impoverishment describes how far a household is pushed below the poverty line due to health payments, and the possibility that health payments may push households who are already poor even further into poverty. Headcount poverty was defined as the proportion of households whose consumption expenditures fell below the poverty line. The normalized poverty gap (NPG) reflects the intensity of poverty which measures the extent to which individuals on average fall below the poverty line and is expressed as a proportion of the poverty threshold. The international poverty line of 1.9$ per capita per day was used in this study. The incidence and intensity of impoverishment were defined, respectively, as the differences in headcount poverty and NPG between the prepayment and postpayment states.
The main independent variable of interest was ethnicity (Hui or Han). The other independent variables were demographic and socioeconomic factors, clinical indictors, and healthcare utilization figures which may have influenced the study outcomes. The demographic and socioeconomic factors comprised the patient's sex, age, education, occupation, place of residence, type of health insurance (NRCMS, URBMI or UEBMI, other type and no insurance), household income quintile, household size, having a laborer in the household, having one or more elderly members of the household aged 60 or over, and having a family member or members with one or more chronic diseases. Clinical indictors consisted of the duration of T2DM, treatment with insulin, and number of complications. Number of complications was categorized as no complications, single complication, and multiple complications. In cases where the number of complications was not clear from the medical records, the patient's physician was consulted. Healthcare utilization was categorized by the frequency of outpatient visits and inpatient admissions and the distance to the nearest healthcare facility.
2.4. Data collection
The eligible patients based on the criteria were identified from all admitted patients in the Health Information Systems (HIS) of the 2 study hospitals during the study period. Before they were discharged from the hospital, the interviewer approached and invited them to participate in the study. After they were informed of the study goals and signed the consent form, they were interviewed face-to-face using a structured questionnaire which gathered personal and household information and patient/family costs. In addition, some clinical information and the medical costs of the hospital were also checked from the HIS.
2.5. Statistical analyses
Data analyses were performed using R version 3.4.1 (R Foundation for Statistical Computing, Vienna, Austria) and Stata version 14.2 (StataCorp, College Station, TX). All costs were converted from Chinese Yuan (CNY) to United States dollars (USD) using the exchange rate of 6.66 CNY per USD. The comparisons of headcount of CHE and impoverishment between Hui and Han patients were analyzed using chi-square test. The gaps in CHE and impoverishment between Hui and Han patients were analyzed using unpaired t test.
The associations of ethnicity with the headcounts of CHE and impoverishment after reimbursement were adjusted with other independent factors using multiple logistic regression. For this part of the analysis, the data from 18 patients (3.8%) who had no insurance or other types of insurance were excluded due to their small number, resulting in 462 patients with public medical insurance being analyzed. The independent factors showing a P < .2 in univariate analysis were initially entered into a multiple logistic regression model using backward selection. Significant factors with a P <.05 remained in the final model.
Significant factors from the final multiple regression model were further analyzed using the Blinder–Oaxaca decomposition technique to explore the most important factors contributing to ethnic differences. The Blinder–Oaxaca decomposition method is a common technique for decomposing differences in outcomes between different population groups.[26] This method is useful to evaluate the variance or contribution of distribution of observed characteristics between 2 groups to the outcome difference.[27,28]
3. Results
During the study period, there were 748 T2DM patients admitted to the study hospitals of which 87 were excluded because of admission due to other diseases than DM. Of the remaining 661 T2DM patients, 181 (27.4%) were not available for an interview, leaving 240 Hui and 240 Han patients to be interviewed and their data analyzed.
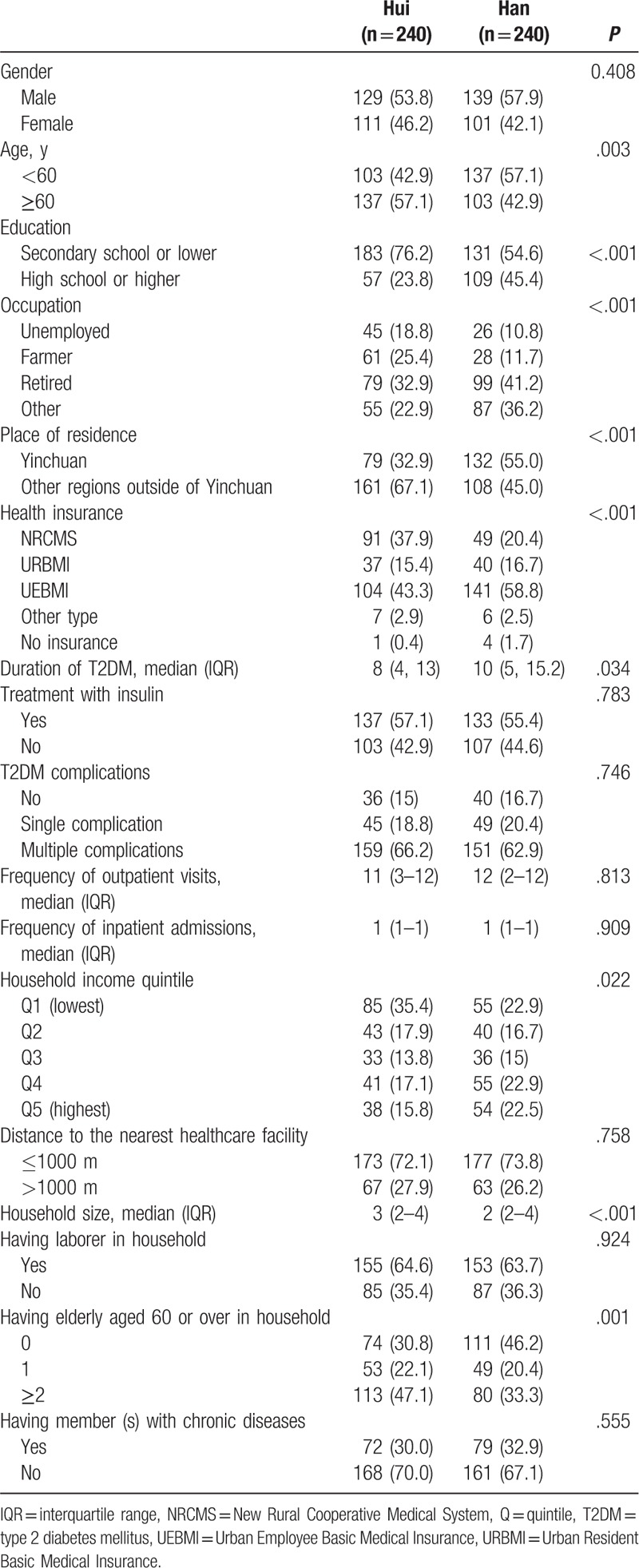
The characteristics of the study patients with T2DM and their households by ethnicity are shown in Table 1. The Hui patients were significantly more likely to have higher age and lower education, be unemployed or a farmer from other regions outside of Yinchuan, be insured by the NRCMS, have a shorter duration of T2DM, and live in a household with lower income, larger size, and more elderly persons compared with the Han patients. The health expenditures for the Hui T2DM patients were significantly lower than for the Han patients in both annual total healthcare expenditure (median $2052, IQR 1454–3686 vs median $2794, IQR 1732–3777, P = .001) and OOP payments (median $1140, IQR 702–1946 vs median $1508, IQR 1027–2344, P < .001). The capacity to pay of the Han patients’ households was significantly higher than in the Hui patients’ households (median $7355, IQR 4038–11141 vs median $4082 IQR 2410–7254, P < .001).
Table 1.
Characteristics of study patients and their households.
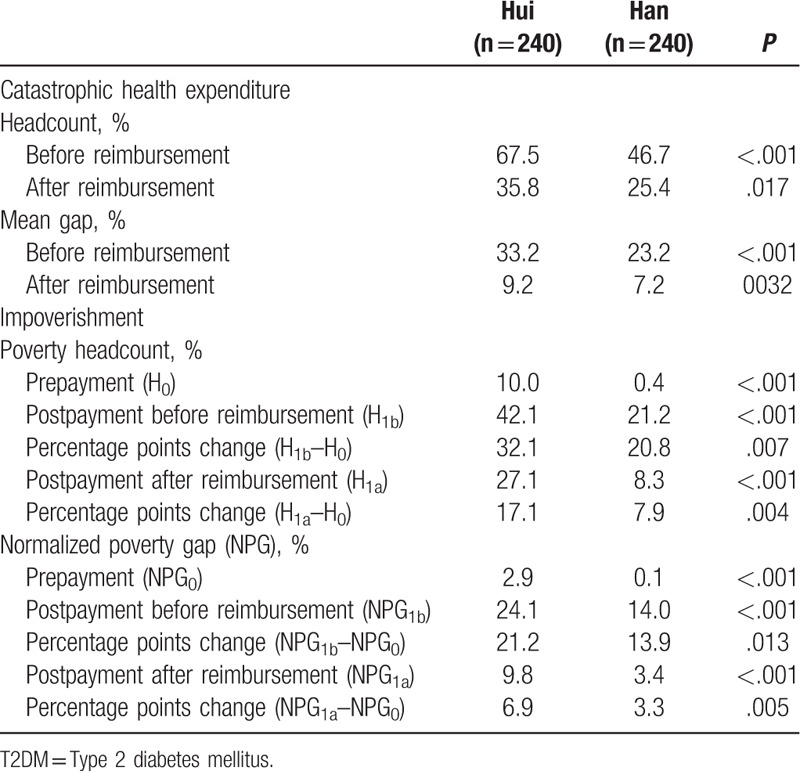
CHE and impoverishment due to utilizing health care for T2DM in the Hui patients were significantly higher than in the Han patients both before and after reimbursement from their health insurance (Table 2). After reimbursement from the health insurance, the CHE headcount and mean gap decreased roughly by 50% and 70%, respectively, for both the Hui and Han patients. The poverty headcount of impoverishment was reduced by 46% for the Hui patients and 62% for the Han patients and the NPG was reduced by 67% for the Hui patients and 76% for the Han patients.
Table 2.
Catastrophic health expenditure and impoverishment due to utilizing health care for T2DM between Hui and Han T2DM patients.
The factors associated with the CHE headcount after reimbursement and decomposition of ethnic difference using multiple logistic regression and the Blinder–Oaxaca decomposition are shown in Table 3. The crude odds of CHE in the Hui patients was significantly higher than in the Han patients, but there was no significant ethnic difference in CHE headcount after adjusting for patient's occupation, household income, T2DM complications, and frequency of outpatient visits and inpatient admissions. Patients who were unemployed, farmers, or retired; those with multiple complications, higher frequency of outpatient visits, and inpatient admissions; and those having lower household income were significantly more likely to have CHE. The difference in CHE headcounts between the Hui and Han patients was 11.9%, 60.5% of which could be explained by the different distributions of the associated factors between the 2 groups. If the distribution of household income or occupation in the Hui patients was the same as in the Han patients, the CHE headcounts would be decreased by 3.4% and 2.1%, respectively.
Table 3.
Factors associated with the catastrophic headcount after reimbursement and decomposition of ethnic disparity (n = 462).

Table 4 presents the factors associated with the impoverishment headcounts after reimbursement and decomposition of ethnic differences. The crude odds of impoverishment in the Hui patients was significantly higher than in the Han patients, but there was no significant ethnic difference in impoverishment headcount after adjusting for sex, household income, and place of residence. Female patients, those in the lowest household income quantile, or those from other regions outside of Yinchuan were more likely to be impoverished. The difference in impoverishment headcount between the Hui and Han patients was 9.8%, 35.7% of which could be explained by the different distributions of the associated factors between the Hui and Han patients. If the distribution of household income and region in the Hui patients was the same as in the Han patients, the headcounts of impoverishment would be reduced by 1.7% and 1.6%, respectively.
Table 4.
Factors associated with the impoverishment headcount after reimbursement and decomposition of ethnic disparity (n = 462).

4. Discussion
The Hui T2DM patients suffered from CHE and impoverishment more than the Han T2DM patients both before and after health insurance reimbursements. The differences between the Hui and Han patients in CHE and impoverishment headcounts were 11.9% and 9.8%, respectively, after reimbursement from the public medical insurance schemes. The distribution of associated factors between the Hui and Han patients contributed to 60.5% and 35.7% of the ethnic differences in CHE and impoverishment, respectively. Household income, occupation, or living in the capital city were the factors that contributed significantly to these differences.
Although belonging to one of the public medical health insurance plans reduced the risk of CHE and impoverishment in both the Hui and Han T2DM patients, the risk reduction in the Hui patients was similar to or lower than in the Han patients. This could be explained by weaker capacity to pay and harder poverty in the pre-payment states in the Hui patients compared with the Han patients. It is a challenge for the country to ensure universal health coverage in all different groups of the population, particularly among ethnic minorities.[21]
A comprehensive literature search found no studies similar to ours that directly assessed ethnic differences in CHE or impoverishment due to utilizing health care for T2DM patients. However, 2 studies related to economic burdens in ethnic minorities were found. One study from Myanmar assessed CHE due to healthcare spending for any illnesses using the same measurements as our study.[29] Another study from Mali measured catastrophic OOP payments due to the use of emergency obstetric care using different measurements.[30] Although various measurements of CHE or different types of healthcare utilization were examined in these studies, their results showed higher CHE in ethnic minorities than in the majority population, similar to the findings in our study. A previous study from China measured the CHE of DM patients, but the participants were from the Han majority population.[19] The study found that the incidence of catastrophic health expenditures was lower than in our study. This was because we measured both direct medical and indirect illness-related costs, and thus our study more accurately assessed the actual expenditures of the households.
Higher odds ratios of CHE and impoverishment in the Hui than the Han patients were not significant in multiple logistic regression. However, total differences of CHE and impoverishment between ethnicities were significant when the Blinder–Oaxaca decomposition analysis was performed. This could be explained by the adjustment of decomposing effects of different characteristics between the Hui and Han patients from this analysis technique.[26]
Household income and occupation were the most important factors associated with an ethnic difference in CHE, which was similar to the findings in previous studies measuring CHE from healthcare expenses related to diabetes and other chronic diseases.[8,31,32] It was not surprising to find that Hui patients are more likely to be unemployed or have no or low income. Likewise, low household income and not living in Yinchuan were the main contributors to ethnic differences in impoverishment. These findings were supported by data showing that the per capita disposable income of people in Yinchuan was higher than in other regions of Ningxia.[33] The proportion of patients living in other regions outside of Yinchuan was higher in the Hui than the Han patients, thus the Hui patients had more indirect costs.
The number of complications, outpatient and inpatient visits, and females were significant factors of CHE or impoverishment in multiple logistic regression. However, those factors were not significant contributors to ethnic differences by the Blinder–Oaxaca decomposition analysis. This shows that the conventional regression models are not sufficient to identify the associated factors contributing to a given difference, thus it is a strength of our study that we used of the Blinder–Oaxaca decomposition analysis to assess ethnic differences. Moreover, direct medical and indirect healthcare-related costs including the costs of productivity loss were measured to evaluate CHE and impoverishment between Hui and Han patients in one area of China.
There were some limitations to the study. First, indirect costs and cost of productivity loss for the use of health services due to T2DM within the previous 12 months were collected by self-reporting, thus some recall bias in the participants who did not keep a diary of their expenditures may have happened. Second, only the T2DM patients using the services from 2 main public hospitals in Yinchuan city were measured; therefore, the findings may not be generalizable, However, these 2 hospitals are the main hospitals providing inpatient services to the entire population of Ningxia province. Finally, the total unexplained difference in impoverishment due to ethnic differences was higher than half, indicating other factors need to be explored. Difficulty in interpreting unexplained differences is the main shortcoming of decomposition techniques.[34–36] The analysis of ethnic differences in catastrophic health expenditure and impoverishment used in our study can be applied to other countries where aim to explore the inequalities in seeking health care among different ethnicities.
5. Conclusions
Hui T2DM patients suffered more CHE and impoverishment than Han patients regardless of health insurance reimbursements. Higher CHE or impoverishment rates were found in patients with low socioeconomic status and poor health with more healthcare utilization. Differences in socioeconomic factors between Hui and Han patients were the main cause of ethnic differences in CHE and impoverishment in T2DM healthcare patients.
Acknowledgments
This study was part of a doctoral thesis in epidemiology of the first author at Prince of Songkla University in Thailand. We would like to thank all of the nurses and doctors who helped with data collection. We also thank Mr. Dave Patterson of the International Affairs Office, Faculty of Medicine, Prince of Songkla University for English editing of this manuscript. The study was funded by a grant from the China Medical Board under the project “A second collaborative program to improve the health research capacity of western medical universities in China (14–181)” through the Epidemiology Unit, Prince of Songkla University and the Graduate School, Prince of Songkla University, and Ningxia Medical University Scientific Research Project (no. XY201732).
Author contribution
Conceptualization: Xian Sun, Tippawan Liabsuetrakul.
Data curation: Xian Sun, Tippawan Liabsuetrakul.
Formal analysis: Xian Sun, Tippawan Liabsuetrakul.
Funding acquisition: Xian Sun, Tippawan Liabsuetrakul.
Investigation: Xian Sun, Xiaomin Xie, Ping Liu.
Methodology: Xian Sun, Tippawan Liabsuetrakul, Xiaomin Xie, Ping Liu.
Project administration: Xian Sun, Tippawan Liabsuetrakul.
Software: Xian Sun, Tippawan Liabsuetrakul.
Supervision: Tippawan Liabsuetrakul.
Writing – original draft: Xian Sun, Tippawan Liabsuetrakul.
Writing – review & editing: Xian Sun, Tippawan Liabsuetrakul, Xiaomin Xie, Ping Liu.
Tippawan Liabsuetrakul orcid: 0000-0001-7687-5629.
Footnotes
Abbreviations: CHE = catastrophic health expenditure, CI = confidence interval, IQR = interquartile range, NPG = normalized poverty gap, NRCMS = New Rural Cooperative Medical System, OOP = out-of-pocket, OR = odds ratio, Q = quintile, ref. = reference, SE = standard error, T2DM = type 2 diabetes mellitus, UEBMI = Urban Employee Basic Medical Insurance Scheme, URBMI = Urban Resident Basic Medical Insurance Scheme.
How to cite this article: Sun X, Liabsuetrakul T, Xie X, Liu P. Catastrophic health expenditure and impoverishment for type 2 diabetes mellitus patients in a multiethnic province in China using a Blinder-Oaxaca decomposition. Medicine. 2019;98:39(e17376).
The authors have no conflicts of interest to disclose.
References
- [1].NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 2016;387:1513–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Deshpande AD, Harris-Hayes M, Schootman M. Epidemiology of diabetes and diabetes-related complications. Phys Ther 2008;88:1254–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Olokoba AB, Obateru OA, Olokoba LB. Type 2 diabetes mellitus: a review of current trends. Oman Med J 2012;27:269–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Rodbard HW, Green AJ, Fox KM, et al. Impact of type 2 diabetes mellitus on prescription medication burden and out-of-pocket healthcare expenses. Diabetes Res Clin Pract 2010;87:360–5. [DOI] [PubMed] [Google Scholar]
- [5].Fox KM, Grandy S. Out-of-pocket expenses and healthcare resource utilization among individuals with or at risk of diabetes mellitus. Curr Med Res Opin 2008;24:3323–9. [DOI] [PubMed] [Google Scholar]
- [6].Smith-Spangler CM, Bhattacharya J, Goldhaber-Fiebert JD. Diabetes, its treatment, and catastrophic medical spending in 35 developing countries. Diabetes Care 2012;35:319–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Okoronkwo IL, Ekpemiro JN, Onwujekwe OE, et al. Socioeconomic inequities and payment coping mechanisms used in the treatment of type 2 diabetes mellitus in Nigeria. Niger J Clin Pract 2016;19:104–9. [DOI] [PubMed] [Google Scholar]
- [8].Gwatidzo SD, Stewart Williams J. Diabetes mellitus medication use and catastrophic healthcare expenditure among adults aged 50+ years in China and India: results from the WHO study on global AGEing and adult health (SAGE). BMC Geriatr 2017;17:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Okoronkwo IL, Ekpemiro JN, Okwor EU, et al. Economic burden and catastrophic cost among people living with type2 diabetes mellitus attending a tertiary health institution in south-east zone, Nigeria. BMC Res Notes 2015;8:527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Lanting LC, Joung IM, Mackenbach JP, et al. Ethnic differences in mortality, end-stage complications, and quality of care among diabetic patients: a review. Diabetes Care 2005;28:2280–8. [DOI] [PubMed] [Google Scholar]
- [11].Riste L, Khan F, Cruickshank K. High prevalence of type 2 diabetes in all ethnic groups, including Europeans, in a British inner city: relative poverty, history, inactivity, or 21st century Europe? Diabetes Care 2001;24:1377–83. [DOI] [PubMed] [Google Scholar]
- [12].Piccolo RS, Pearce N, Araujo AB, et al. The contribution of biogeographical ancestry and socioeconomic status to racial/ethnic disparities in type 2 diabetes mellitus: results from the Boston Area Community Health Survey. Ann Epidemiol 2014;24:648–54. 654.e651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Egede LE. Race, ethnicity, culture, and disparities in health care. J Gen Intern Med 2006;21:667–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Scheppers E, van Dongen E, Dekker J, et al. Potential barriers to the use of health services among ethnic minorities: a review. Fam Pract 2006;23:325–48. [DOI] [PubMed] [Google Scholar]
- [15].Xu Y, Wang L, He J, et al. Prevalence and control of diabetes in Chinese adults. JAMA 2013;310:948–59. [DOI] [PubMed] [Google Scholar]
- [16].Wang W, McGreevey WP, Fu C, et al. Type 2 diabetes mellitus in China: a preventable economic burden. Am J Manag Care 2009;15:593–601. [PubMed] [Google Scholar]
- [17].Huang Y, Vemer P, Zhu J, et al. Economic burden in Chinese patients with diabetes mellitus using electronic insurance claims data. PLoS One 2016;11:e0159297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Liu X, Sun X, Zhao Y, et al. Financial protection of rural health insurance for patients with hypertension and diabetes: repeated cross-sectional surveys in rural China. BMC Health Serv Res 2016;16:481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Niu Y. Current Status and Influencing Factors of Catastrophic Health Expenditure in Diabetic Patients Among Urban and Rural Residents: A Study in Shandong, China. Jinan, Shandong: Department of Social Medicine and Maternal & Child health Shandong University; 2017. [Google Scholar]
- [20].Hougaard JL, Osterdal LP, Yu Y. The Chinese healthcare system: structure, problems and challenges. Appl Health Econ Health Policy 2011;9:1–3. [DOI] [PubMed] [Google Scholar]
- [21].Saksena P, Hsu J, Evans DB. Financial risk protection and universal health coverage: evidence and measurement challenges. PLoS Med 2014;11:e1001701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Hao Y. Universal health insurance coverage for 1.3 billion people: what accounts for China's success? Health Policy 2015;119:1145–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Si L, Jiang QC. Challenges to the Chinese health insurance system: users’ and service providers’ perspectives. Chin Med J (Engl) 2015;128:571–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Sun Y, Gregersen H, Yuan W. Chinese health care system and clinical epidemiology. Clin Epidemiol 2017;9:167–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Xu K, Evans DB, Kawabata K, et al. Household catastrophic health expenditure: a multicountry analysis. Lancet 2003;362:111–7. [DOI] [PubMed] [Google Scholar]
- [26].Jann B, Zürich E, Zürich S. The Blinder–Oaxaca decomposition for linear regression models. Stata J 2008;8:453–79. [Google Scholar]
- [27].Sinning M, Hahn M, Bauer T. The Blinder–Oaxaca decomposition for nonlinear regression models. Stata J 2008;8:480–92. [Google Scholar]
- [28].Fairlie RW. An extension of the Blinder-Oaxaca decomposition technique to logit and probit models. J Econ Soc Meas 2005;30:305–16. [Google Scholar]
- [29].Htet S, Fan V, Alam K, et al. Financial risks from ill health in Myanmar: evidence and policy implications. Asia Pac J Public Health 2015;27:418–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Arsenault C, Fournier P, Philibert A, et al. Emergency obstetric care in Mali: catastrophic spending and its impoverishing effects on households. Bull World Health Organ 2013;91:207–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Choi JW, Choi JW, Kim JH, et al. Association between chronic disease and catastrophic health expenditure in Korea. BMC Health Serv Res 2015;15:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Rezapour A, Vahedi S, Khiavi FF, et al. Catastrophic Health Expenditure of Chronic Diseases: Evidence from Hamadan, Iran. Int J Prev Med 2017;8:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Bureau of Statistics of Ningxia Hui Autonomous Region (BSNX). Per capita disposable income of residence from regions in Ningxia in 2015. Stat Econ 2015;4:64–6. [Google Scholar]
- [34].Mehta HB, Rajan SS, Aparasu RR, et al. Application of the nonlinear Blinder-Oaxaca decomposition to study racial/ethnic disparities in antiobesity medication use in the United States. Res Social Adm Pharm 2013;9:13–26. [DOI] [PubMed] [Google Scholar]
- [35].Holmes GM, Freburger JK, Ku LJ. Decomposing racial and ethnic disparities in the use of postacute rehabilitation care. Health Serv Res 2012;47(3 Pt 1):1158–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Sarpong EM, Miller GE. Racial and ethnic differences in childhood asthma treatment in the United States. Health Serv Res 2013;48(6 Pt. 1):2014–36. [DOI] [PMC free article] [PubMed] [Google Scholar]


