Supplemental Digital Content is available in the text
Keywords: meta-analysis, simultaneous bilateral THA, staged bilateral THA
Abstract
Background:
Total hip arthroplasty (THA) relieves pain and restores function in patients with severe rheumatoid arthritis and osteoarthritis. Over the past few decades, several authors have attempted to assess the efficacy and safety of simultaneous bilateral THA compared with staged bilateral THA. The purpose of this meta-analysis is to compare the mortalities and complications between simultaneous bilateral THA and staged bilateral THA.
Methods:
A literature search to identify eligible studies was undertaken to identify all relevant articles published until August 2018. We included studies that compared simultaneous bilateral THA and staged bilateral THA and their effects on mortality and complications. The outcomes included mortality, the occurrence of deep venous thrombosis (DVT), the occurrence of pulmonary embolism (PE), respiratory complications, cardiovascular complications, digestive system complications and the occurrence of dislocation. Stata 12.0 was used for the meta-analysis.
Results:
Nineteen studies involving 59,257 patients were identified; among them, 16,758 patients were selected for treatment with simultaneous bilateral THA, and 42,499 patients were chosen for the purpose of staged bilateral THA. The meta-analysis results demonstrated that there was no significant difference between simultaneous bilateral THA and staged bilateral THA in terms of mortality (risk ratio [RR] = 1.15, 95% CI = 0.76, 1.74; P = .520). Compared with staged bilateral THA, simultaneous bilateral THA was associated with a reduction in the occurrence of DVT, PE and respiratory complications (P < .05). There were no significant differences in the cardiovascular complications, digestive system complications or the occurrence of dislocation and infection (P = .057).
Conclusions:
We observed that the prevalence of DVT, PE and respiratory complications was considerably lower with the use of simultaneous bilateral THA than with the use of staged bilateral THA. Thus, simultaneous bilateral THA is a considerably safer procedure than staged bilateral THA in selected THA patients.
1. Introduction
Simultaneous bilateral total hip arthroplasty (THA) was initially proposed by Jaffe and Charnley in 1971.[1] THA relieves pain and restores function in patients with severe rheumatoid arthritis and osteoarthritis.[2] In the past 3 decades, several scholars have attempted to investigate the efficacy and safety of simultaneous bilateral THA compared with staged bilateral THA.[3] Furthermore, some previous studies have reported that simultaneous bilateral THA leads to a reduction in the duration of hospitalization, shorter durations of anesthesia and surgical procedures and faster rehabilitation times, as well as an improvement in cost-effectiveness.[4,5] However, it has been revealed that simultaneous bilateral THA is associated with an increased rate of complications, including occurrences of deep-vein thrombosis (DVT),[6] as well as increased medical morbidities, thus leading to suboptimal functional outcomes.[7]
Several clinical trials have attempted to assess the outcomes of simultaneous bilateral THA and staged bilateral THA; however, most of them involved relatively small cohorts of patients; thus, their results failed to indicate considerable statistical achievements.[8] A recent meta-analysis reported the advantages of simultaneous bilateral THA compared with staged bilateral THA.[3] However, this analysis only compared several complications but did not consider the mortality that is associated with THA. Furthermore, several important studies were omitted in this meta-analysis.
Thus, it was necessary to conduct a meta-analysis that comprehensively compared the mortalities and complications between simultaneous bilateral THA and staged bilateral THA. The purpose of this meta-analysis was to compare the mortalities and complications associated with simultaneous bilateral THA and staged bilateral THA.
2. Materials and methods
2.1. Search strategies
In this study, a literature search was carried out using the PubMed, Embase, Web of Science, Cochrane Library and Chinese Wanfang databases to identify all relevant research papers published until August 2018, with these identified studies evaluating the patients’ outcomes as well as the simultaneous bilateral THA and staged bilateral THA procedures that were undertaken. No further restrictions were applied except that the language of the publications was limited to English, as only English documents can be easily searched in the well-known medical databases. Reports related to simultaneous bilateral THA and staged bilateral THA were included regardless of whether unilateral THA was involved in the comparison. The following Medical Subject Headings (MeSH) and terms were used in the search process: “bilateral total hip arthroplasty”, “staged total hip arthroplasty”, and “total hip arthroplasty”. The list of references for each comparative study and the relevant reviews were manually examined to explore additional relevant studies.
2.2. Inclusion criteria
-
1.
Settings and design: randomized controlled trials (RCTs) and non-RCTs of simultaneous bilateral THA and staged bilateral THA in THA patients.
-
2.
Study subjects: Patients who suffered from THA.
-
3.
Interventions: The experimental group was administered simultaneous bilateral THA, and the control group was administered staged bilateral THA.
-
4.
Outcome indicators: Mortality, the occurrence of DVT, the occurrence of PE, respiratory complications, cardiovascular complications, digestive system complications, the occurrence of dislocation and the occurrence of infection.
2.3. Data extraction
Data were independently extracted after all eligible studies were involved. All patients’ medical information was recorded. The recorded data included the age and sex of the patients. The primary outcomes of interest were the rate of mortality and the incidence of complications (i.e., total, systemic, local, cardiac, respiratory, and digestive complications; pulmonary embolism (PE); DVT; and hip dislocation).
2.4. Study quality
The qualities of all included RCTs were independently assessed by 2 reviewers on the basis of the Cochrane Handbook for Systematic Reviews of Interventions, version 5.1.0 (http://www.cochrane-handbook.org/).[9] A total of 7 domains were used to assess the overall quality: random sequence generation, allocation concealment, the blinding of the participants and personnel, the blinding of outcome assessments, incomplete outcome data, selective reporting and other biases. Each domain was measured as having a low bias, an unclear bias or a high bias. The Newcastle-Ottawa quality scale (NOS) was used to assess the risks of bias for the prospective cohort studies and the retrospective observational studies. The NOS included 3 categories (selection, comparability and exposure/outcome). Furthermore, a score equal to 9 indicated the highest quality study.
2.5. Statistical analyses
Study-specific risk ratios (RRs) and associated 95% confidence intervals (CIs), which accounted for the discontinuous variables within the study, were pooled by using a random-effects model, in which the within-study and between-study variations were also taken into account. Weighted mean differences (WMDs) and weighted mean difference statistical methods were used for the continuous variables, in which a fixed effect model was initially utilized; in cases where the P value belonging to the heterogeneity test was less than .1 or the I2 > 50%, a random-effect model was replaced with the previous modality. In addition, sensitivity analyses were carried out to evaluate the reliability of the achieved results.
Furthermore, a sensitivity analysis was utilized to determine whether the modifications of the meta-analysis criteria may have affected the results. No single study was observed to qualitatively affect the summary RRs based on the output achieved through the use of the sensitivity analysis. Forest plots were used to present the results of the individual studies, and from a statistical perspective, the effect size was eliminated. All statistical analyses were performed by using Stata software (StataCorp LLC, TX).
3. Results
3.1. Search results
A flowchart describing the studies that were reviewed in the current research paper is shown in Figure 1. In total, nineteen studies[4,8,10–26] involving 59,257 patients were identified; among them, 16,758 patients were selected for simultaneous bilateral THA, and 42,499 patients were chosen for the purpose of staged bilateral THA. The details of all studies are listed in Table 1. Furthermore, the characteristics of the preoperative patients did not exhibit significant differences between the groups, with an exception of the patients in the simultaneous bilateral THA group.
Figure 1.
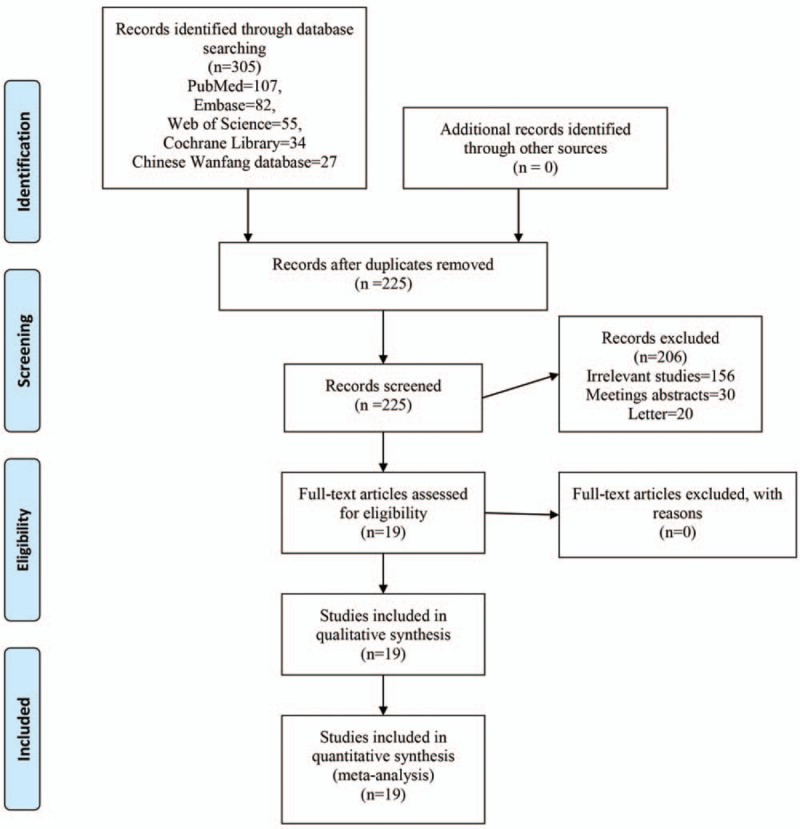
Flow of trials in the meta-analysis.
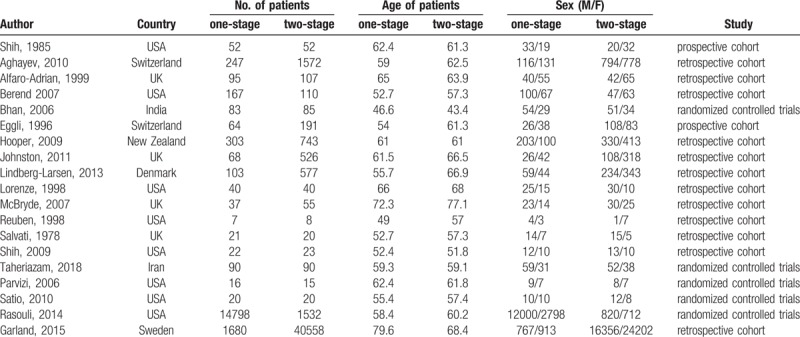
Table 1.
General characteristic of the included studies.
3.2. Quality assessment
The quality assessment for the included studies is presented in Figure 2 and Supplement S1. Only 1 study did not state the random sequence generation or the allocation concealment, and this study was indicated as having an unclear risk of bias. None of the studies reported the blinding of the participants or the personnel. The NOS scores for the non-RCTs ranged from 5 to 7, which indicated that all of the included non-RCTs had moderate qualities (Supplement S2).
Figure 2.
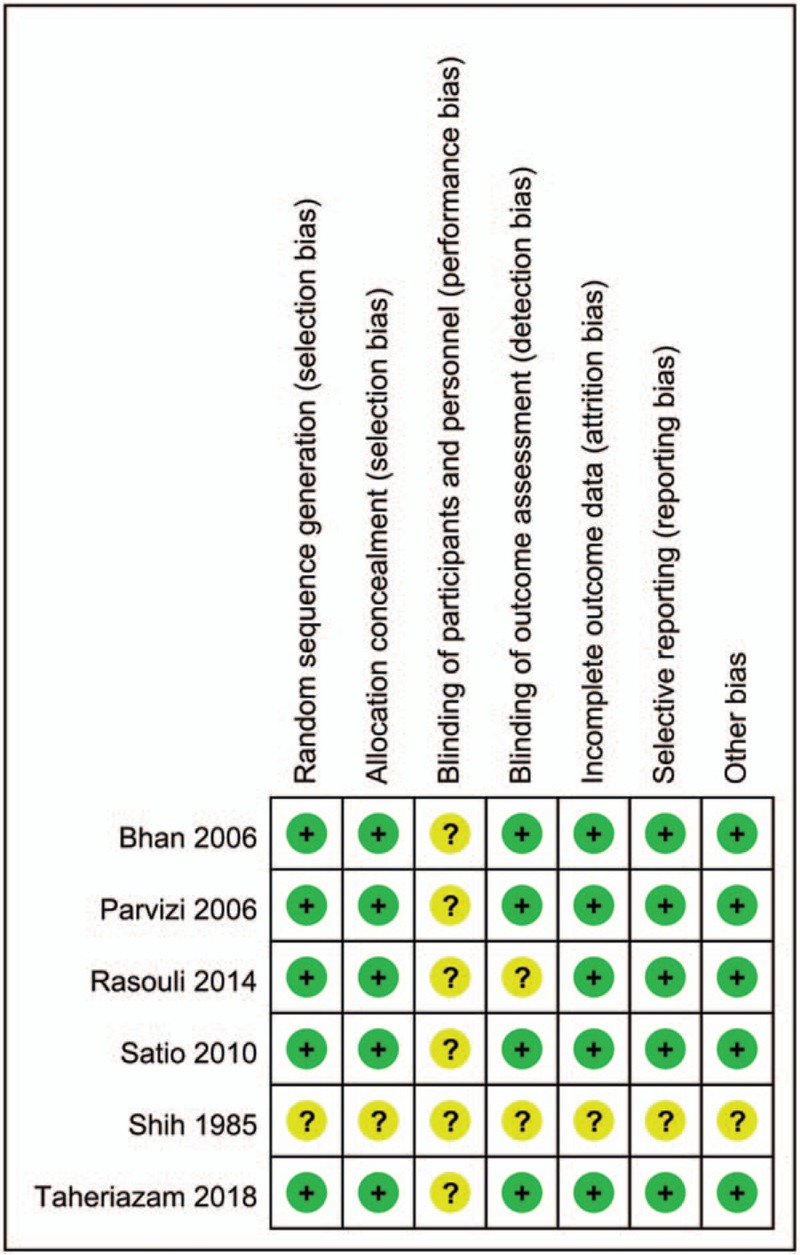
The risk of bias summary: +, no bias; –, bias; ?, bias unknown.
3.3. Mortality
Twelve studies (33,176 THA patients) were included for the mortality analysis. There was no significant difference between the simultaneous bilateral THA and the staged bilateral THA groups in terms of the mortality (RR = 1.15, 95% CI = 0.76, 1.74; P = .520, Fig. 3).
Figure 3.
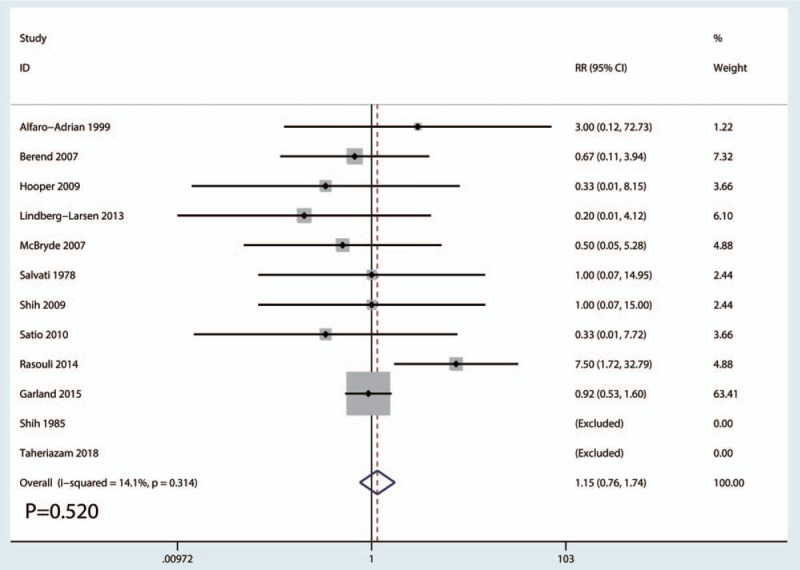
Forest plots of the included studies comparing the occurrence of mortality.
3.4. Occurrence of DVT
Ten studies involving 38,201 patients were included for the DVT complication analysis. Compared with staged bilateral THA, simultaneous bilateral THA was associated with a reduction in the occurrence of DVT (RR = 0.37, 95% CI = 0.4, 0.56; P = .000, Fig. 4).
Figure 4.
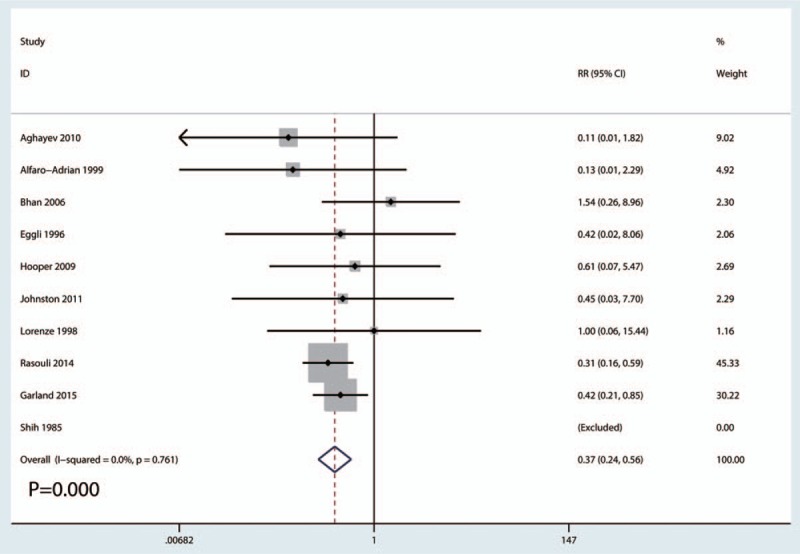
Forest plots of the included studies comparing the occurrence of DVT. DVT = deep venous thrombosis.
3.5. Occurrence of PE
Ten studies involving 21,142 patients were included for the analysis of the occurrence of PE. Compared with staged bilateral THA, simultaneous bilateral THA was associated with a reduction in the occurrence of PE (RR = 0.39, 95% CI = 0.23, 0.67; P = .001, Fig. 5)
Figure 5.
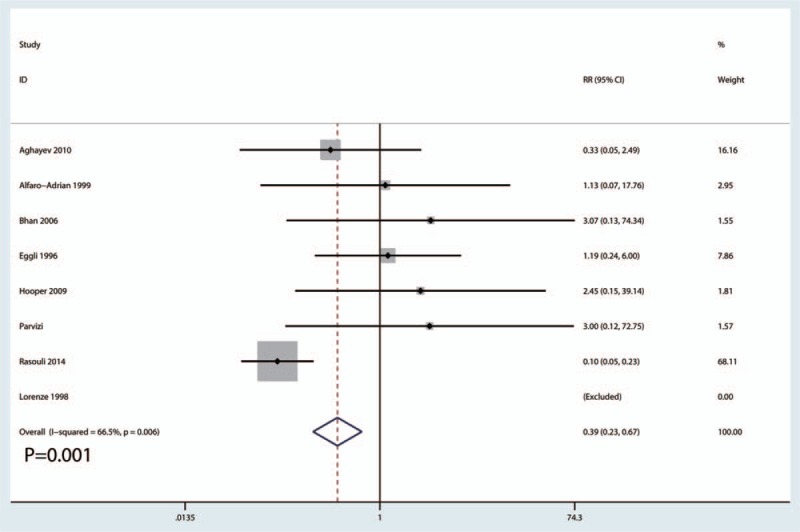
Forest plots of the included studies comparing the occurrence of PE. PE = pulmonary embolism.
3.6. Respiratory complications
Ten studies involving 38,860 patients were included for the analysis of the occurrence of respiratory complications. Compared with staged bilateral THA, simultaneous bilateral THA was associated with a reduction in respiratory complications (RR = 0.31, 95% CI = 0.21, 0.46; P = .000, Fig. 6).
Figure 6.
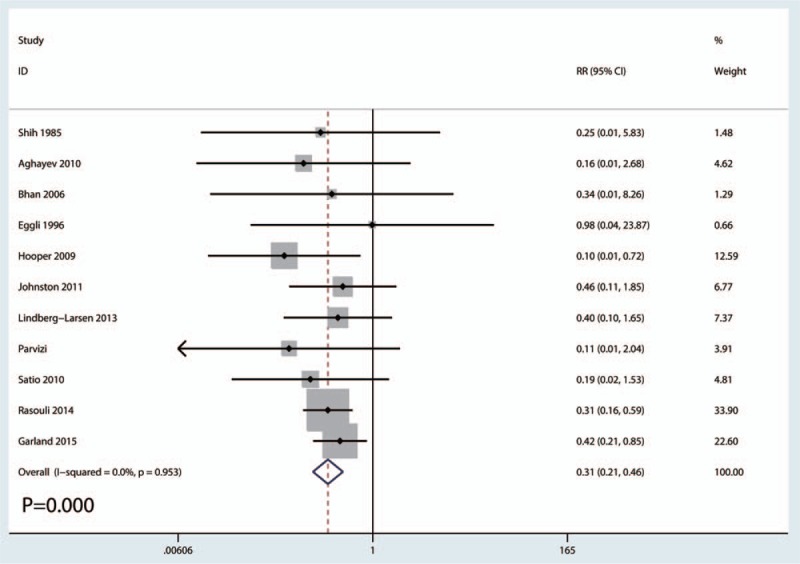
Forest plots of the included studies comparing respiratory complications.
3.7. Cardiovascular complications
Ten studies involving 18,314 patients were included for the analysis of the occurrence of cardiovascular complications. There was no significant difference between staged bilateral THA and simultaneous bilateral THA in terms of cardiovascular complications (RR = 1.03, 95% CI = 0.48, 2.19; P = .943, Fig. 7).
Figure 7.
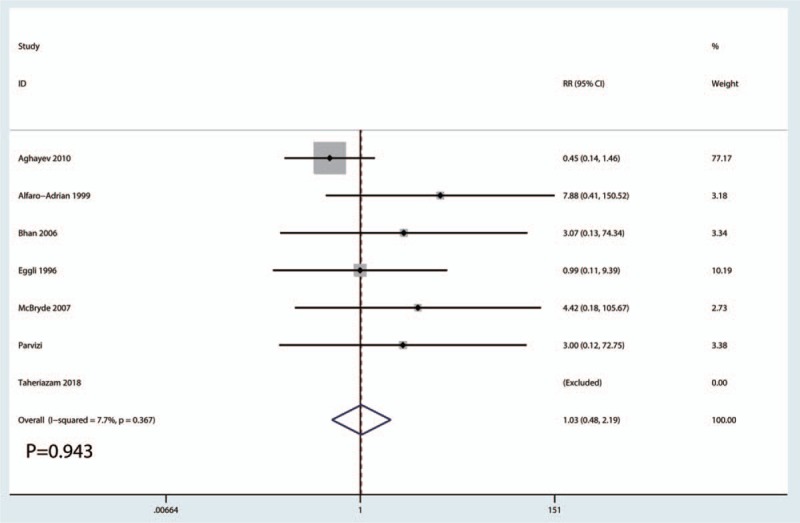
Forest plots of the included studies comparing cardiovascular complications.
3.8. Digestive system complications
Ten studies involving 2732 patients were included for the analysis of the occurrence of digestive system complications. There was no significant difference between staged bilateral THA and simultaneous bilateral THA in terms of digestive system complications (RR = 0.90, 95% CI = 0.46, 1.76; P = .764, Fig. 8).
Figure 8.
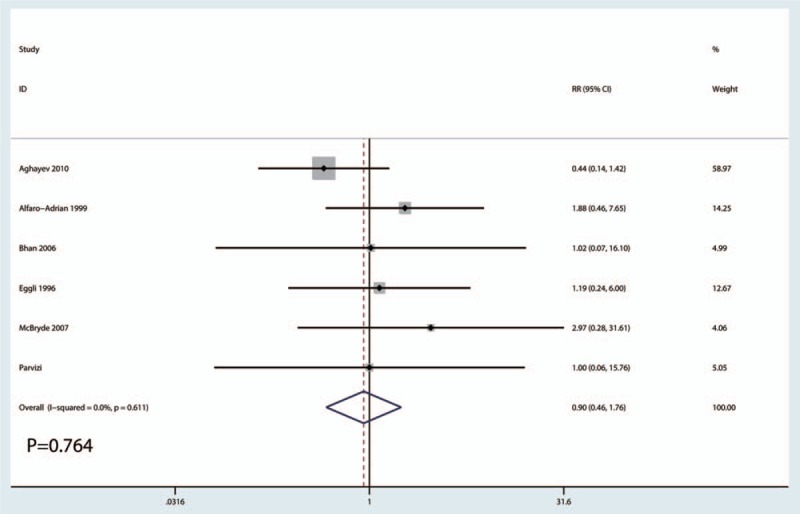
Forest plots of the included studies comparing digestive system complications.
3.9. Occurrence of dislocation
Ten studies involving 3983 patients were included for the analysis of the occurrence of dislocation. There was no significant difference between staged bilateral THA and simultaneous bilateral THA in terms of the occurrence of dislocation (RR = 1.69, 95% CI = 0.99, 2.91; P = .055, Fig. 9).
Figure 9.
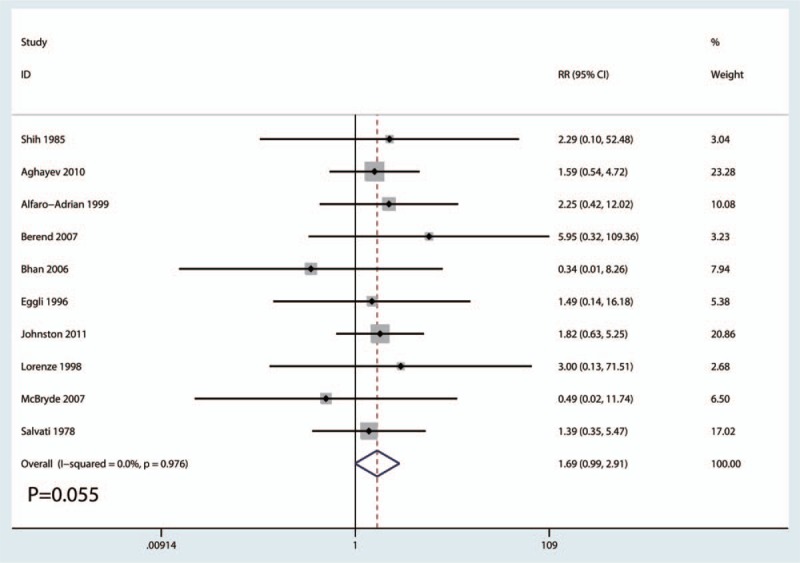
Forest plots of the included studies comparing the occurrence of dislocation.
3.10. Occurrence of infection
Eight studies reported the occurrence of infection. There was no significant difference between staged bilateral THA and simultaneous bilateral THA in terms of the occurrence of infection (RR = 1.50, 95% CI = 0.99, 2.27; P = .057, Fig. 10).
Figure 10.
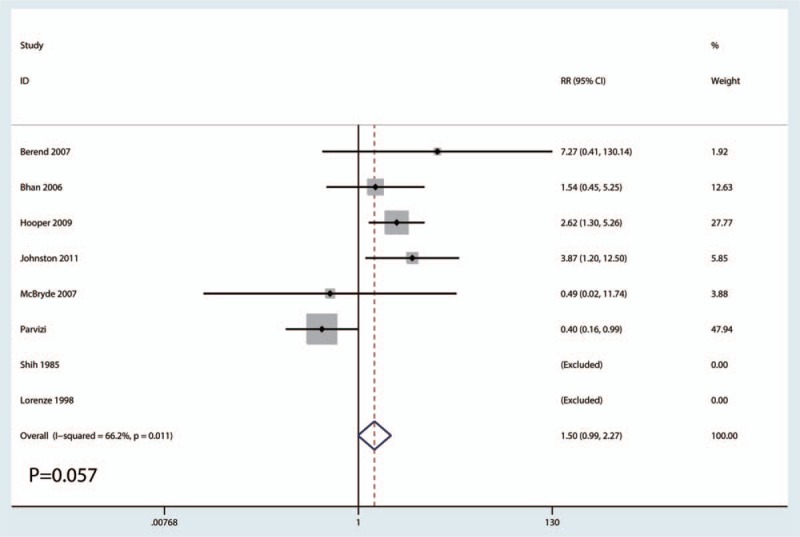
Forest plots of the included studies comparing the occurrence of infection.
3.11. Subgroup analyses, sensitivity analyses, and publication biases
The subgroup analyses indicated that there were significant differences between the staged bilateral THA and simultaneous bilateral THA groups in terms of study type (RCTs vs non-RCTs, Supplement S3) and follow-up duration (short-term follow-up vs long-term follow-up, Supplement S4).
The sensitivity analyses, which involved the omission of each study in turn, did not alter the outcomes. Supplement S5 displays the details of the sensitivity analyses.
For the meta-analysis of staged bilateral THA and simultaneous bilateral THA for the occurrence of mortality, there was no evidence of publication bias via the inspection of the funnel plots and the formal statistical tests (Egger test, P = .55, Supplement S6; Begg test, P = .71, Supplement S7).
4. Discussion
As far as we know, this current meta-analysis is the most recent analysis with the largest sample size that compares the mortalities and postoperative complications between bilateral simultaneous and staged THA procedures. The final results indicated that, compared with bilateral staged THA, bilateral simultaneous THA was associated with a reduction in the occurrence of DVT, PE, respiratory complications and cardiovascular complications. There were no significant differences in the occurrence of mortality, digestive system complications or dislocations between the 2 groups.
First, we identified the occurrence of mortality as a primary outcome. The results demonstrated that there was no significant difference between the bilateral simultaneous THA and staged THA groups in terms of mortality. In fact, the occurrence of mortality was largely dependent on the follow-up duration and the included ages of the patients. There was a significant difference between the bilateral staged THA and simultaneous THA groups for the follow-up duration (short-term follow-up vs long-term follow-up). Since the ages in the included studies varied from each other, a subgroup analysis could not be performed.
Haverkamp et al[27] conducted a meta-analysis comparing bilateral THA and staged bilateral THA in terms of mortality. The results were similar to our results; they observed that there was no significant difference in mortality between the two groups. Compared with staged bilateral THA, simultaneous bilateral THA was associated with a reduction in respiratory complications. One-stage bilateral THA patients experienced longer surgical times; thus, these patients may be associated with more respiratory complications.
The meta-analysis revealed that simultaneous bilateral THA was associated with a reduction in the occurrence of DVT and PE compared with staged bilateral THA. Tsiridis et al[28] demonstrated no statistically significant differences in the rates of thromboembolic events. During a prolonged surgical procedure, increased blood loss can induce Virchow triad and result in a venous thromboembolism (VTE). Furthermore, it has been demonstrated that the highest insult occurs during the insertion of the femoral component. Therefore, a bilateral simultaneous THA would be expected to double the risk of thromboembolic phenomena. Ritter and Stringern et al[6] reported that these results can be used to improve perioperative venous thromboembolic prophylaxis and the early mobilization of patients in the intensive care unit (ICU), as well as in developing hypotensive anesthesia and modern cementing techniques.
In our study, we observed no significant differences in cardiovascular or digestive system complications. However, Alfaro-Adrian et al[14] reported a higher incidence of cardiovascular complications in the bilateral simultaneous THA group than in the bilateral staged THA group. Parvizi et al[25] reported a higher incidence of cardiovascular and digestive system complications in the bilateral staged THA group. The other studies demonstrated no significant differences between the bilateral simultaneous THA and bilateral staged THA groups.
Finally, we compared the occurrence of dislocation and infection. The results demonstrated that there were no significant differences in the occurrence of dislocation or infection between the bilateral simultaneous THA and bilateral staged THA groups. Shao et al[3] observed that staged bilateral THA was associated with a higher incidence of infection than bilateral simultaneous THA. Additionally, they also observed that there was no significant difference in the occurrence of dislocation between the 2 groups.
There were several limitations of the meta-analysis in the presented study.
-
1.
Only 19 studies (RCTs and non-RCTs) were included, and an ideal meta-analysis would only contain RCTs.
-
2.
The follow-up period was relatively short, and a long-term follow-up is necessary to identify long-term complications.
-
3.
There was heterogeneity among the included studies, and we performed a sensitivity analysis to identify the source of the heterogeneity.
-
4.
We could not determine whether there was a publication bias for the final outcomes.
-
5.
The patients had different ages and sexes, which could result in a selection bias.
5. Conclusion
In conclusion, the occurrence of DVT, PE and respiratory complications was considerably higher in the staged bilateral THA group than in the simultaneous bilateral THA group. Additionally, no significant differences were observed regarding mortality, digestive complications or hip dislocation.
Author contributions
Conceptualization: Liangku Huang.
Data curation: Yuben Xu.
Formal analysis: Tao Xu.
Funding acquisition: Tao Xu.
Software: Peng Li, Zandong Zhao.
Validation: Lei Xia, Zandong Zhao.
Writing – original draft: Peng Li.
Writing – review & editing: Liangku Huang, Yuben Xu, Lei Xia.
Supplementary Material
Footnotes
How to cite this article: Huang L, Xu T, Li P, Xu Y, Xia L, Zhao Z. Comparison of mortality and complications between bilateral simultaneous and staged total hip arthroplasty. Medicine 2019;98:39(e16774).
Abbreviations: CIs = confidence intervals, DVT = deep venous thrombosis, ICU = intensive care unit, NOS = Newcastle-Ottawa quality scale, RR = risk ratio, THA = total hip arthroplasty, VTE = venous thromboembolism, WMD = weighted mean difference.
The authors have no funding and conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Jaffe WL, Charnley J. Bilateral Charnley low-friction arthroplasty as a single operative procedure. A report of fifty cases. Bull Hosp Joint Dis 1971;32:198–214. [PubMed] [Google Scholar]
- [2].Zhu XT, Chen L, Lin JH. Selective COX-2 inhibitor versus non-selective COX-2 inhibitor for the prevention of heterotopic ossification after total hip arthroplasty: A meta-analysis. Medicine (Baltimore) 2018;97:e11649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Shao H, et al. Bilateral total hip arthroplasty: 1-Stage or 2-Stage? A meta-analysis. J Arthroplasty 2017;32:689–95. [DOI] [PubMed] [Google Scholar]
- [4].Reuben JD, et al. Cost comparison between bilateral simultaneous, staged, and unilateral total joint arthroplasty. J Arthroplasty 1998;13:172–9. [DOI] [PubMed] [Google Scholar]
- [5].Odum SM, et al. A cost-utility analysis comparing the cost-effectiveness of simultaneous and staged bilateral total knee arthroplasty. J Bone Joint Surg Am 2013;95:1441–9. [DOI] [PubMed] [Google Scholar]
- [6].Ritter MA, Stringer EA. Bilateral total hip arthroplasty: a single procedure. Clin Orthop Relat Res 1980;185–90. [PubMed] [Google Scholar]
- [7].Wykman A, Olsson E. Walking ability after total hip replacement. A comparison of gait analysis in unilateral and bilateral cases. J Bone Joint Surg Br 1992;74:53–6. [DOI] [PubMed] [Google Scholar]
- [8].Bhan S, Pankaj A, Malhotra R. One- or two-stage bilateral total hip arthroplasty: a prospective, randomised, controlled study in an Asian population. J Bone Joint Surg Br Vol 2006;88:298–303. [DOI] [PubMed] [Google Scholar]
- [9].GS, H.J., Cochrane handbook for systematic reviews of interventions version 5.1.0. [http://handbook.cochrane.org/] 2011. [Google Scholar]
- [10].Shih CH, Ho WB. One-stage versus two-stage bilateral autophor ceramic total hip arthroplasty. Clin Orthop Relat Res 1985;141–5. [PubMed] [Google Scholar]
- [11].Salvati EA, Hughes P, Lachiewicz P. Bilateral total hip-replacement arthroplasty in one stage. J Bone Joint Surg Am 1978;60:640–4. [PubMed] [Google Scholar]
- [12].Eggli S, Huckell CB, Ganz R. Bilateral total hip arthroplasty: one stage versus two stage procedure. Clin Orthop Relat Res 1996;108–18. [PubMed] [Google Scholar]
- [13].Lorenze M, et al. A comparison of the cost effectiveness of one-stage versus two-stage bilateral total hip replacement. Orthopedics 1998;21:1249–52. [DOI] [PubMed] [Google Scholar]
- [14].Alfaro-Adrian J, et al. One- or two-stage bilateral total hip replacement. J Arthroplasty 1999;14:439–45. [DOI] [PubMed] [Google Scholar]
- [15].Berend KR, Lombardi AV, Jr, Adams JB. Simultaneous vs staged cementless bilateral total hip arthroplasty: perioperative risk comparison. J Arthroplasty 2007;226 Suppl 2:111–5. [DOI] [PubMed] [Google Scholar]
- [16].McBryde CW, et al. One- or two-stage bilateral metal-on-metal hip resurfacing arthroplasty. J Bone Joint Surg Br 2007;89:1144–8. [DOI] [PubMed] [Google Scholar]
- [17].Hooper GJ, et al. Bilateral total joint arthroplasty: the early results from the New Zealand National Joint Registry. J Arthroplasty 2009;24:1174–7. [DOI] [PubMed] [Google Scholar]
- [18].Shih LY, Wong YC, Shih HN. One-stage hip arthroplasty and bone grafting for bilateral femoral head osteonecrosis. Clin Orthop Relat Res 2009;467:1522–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Aghayev E, et al. Simultaneous bilateral hip replacement reveals superior outcome and fewer complications than two-stage procedures: a prospective study including 1819 patients and 5801 follow-ups from a total joint replacement registry. BMC Musculoskelet Disord 2010;11:245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Johnston LR, Clift BA, Abboud RJ. Bilateral simultaneous hip replacement versus bilateral sequential hip replacement. A 7-year data review. Orthop Nurs 2011;30:119–23. quiz 124-5. [DOI] [PubMed] [Google Scholar]
- [21].Lindberg-Larsen M, et al. Simultaneous and staged bilateral total hip arthroplasty: a Danish nationwide study. Arch Orthop Trauma Surg 2013;133:1601–5. [DOI] [PubMed] [Google Scholar]
- [22].Taheriazam A, et al. Bilateral total hip arthroplasty: one-stage versus two-stage procedure. Hip Int 2018;1120700018773427. [DOI] [PubMed] [Google Scholar]
- [23].Rasouli MR, et al. Perioperative morbidity and mortality following bilateral total hip arthroplasty. J Arthroplasty 2014;29:142–8. [DOI] [PubMed] [Google Scholar]
- [24].Saito S, et al. One- versus two-stage bilateral total hip arthroplasty. Orthopedics 2010;33: [DOI] [PubMed] [Google Scholar]
- [25].Parvizi J, et al. Bilateral total hip arthroplasty: one-stage versus two-stage procedures. Clin Orthop Relat Res 2006;453:137–41. [DOI] [PubMed] [Google Scholar]
- [26].Garland A, et al. Early postoperative mortality after simultaneous or staged bilateral primary total hip arthroplasty: an observational register study from the Swedish Hip Arthroplasty Register. BMC Musculoskelet Disord 2015;16:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Haverkamp D, et al. One stage bilateral total hip arthroplasty, is it safe? A meta-analysis. Hip Int 2010;20:440–6. [DOI] [PubMed] [Google Scholar]
- [28].Tsiridis E, et al. The safety and efficacy of bilateral simultaneous total hip replacement: an analysis of 2063 cases. J Bone Joint Surg Br 2008;90:1005–12. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


