Supplemental Digital Content is available in the text.
Background:
Prenatal environmental and social exposures have been associated with decreased birth weight. However, the effects of combined exposures (CEs) in these domains are not fully understood. Here we assessed multi-domain exposures for participants in the Healthy Start study (Denver, CO) and tested associations with neonatal size and body composition.
Methods:
In separate linear regression models, we tested associations between neonatal outcomes and three indices for exposures. Two indices were developed to describe exposures to environmental hazards (ENV) and social determinants of health (SOC). A third index CEs in both domains (CE = ENV/10 × SOC/10). Index scores were assigned to mothers based on address at enrollment. Birth weight and length were measured at delivery, and weight-for-length z-scores were calculated using a reference distribution. Percent fat mass was obtained by air displacement plethysmography.
Results:
Complete data were available for 897 (64%) participants. Median (range) ENV, SOC, and CE values were 31.9 (7.1–63.2), 36.0 (2.8–75.0), and 10.9 (0.4–45.7), respectively. After adjusting for potential confounders, 10-point increases in SOC and CE were associated with 27.7 g (95% confidence interval [CI] = 12.4, 42.9 g) and 56.3 g (19.4 – 93.2 g) decreases in birth weight, respectively. SOC and CE were also associated with decreases in percent fat mass.
Conclusions:
CEs during pregnancy were associated with lower birth weight and percent fat mass. Evidence of a potential synergistic effect between ENV and SOC suggests a need to more fully consider neighborhood exposures when assessing neonatal outcomes.
What this study adds
Prior studies of the effect of poor neighborhood conditions or low environmental quality have demonstrated associations between higher exposures and decreased birth weight. This study confirms these findings and suggests there may be a synergistic effect between neighborhood-level social and environmental determinants of health. In our cohort, mothers with higher combined exposures in the chemical, physical, and social domains gave birth to babies with lower mean birth weights and lower percent fat mass. These results were robust after adjustment for important individual-level factors known to be associated with neonatal size.
Introduction
Neonatal size and body composition are important indicators of both childhood and adult health outcomes. Birth weight is a standard anthropometric measurement used to assess infant health. Longitudinal data on more than 36 million term births in the United States indicated that mean birth weight decreased 52 g between 1990 and 2005.1 Although small changes in birth weight may not have impacts on individual-level health outcomes, trends in birth weight can have important public health impacts. For example, decreases in mean birth weight at the population level correlate with increases in the frequency of babies born with low birth weight (LBW: <2,500 g) and small for gestational age (SGA: below the 10th percentile for each completed week of gestation).1–3 LBW and SGA have been shown to be associated with childhood obesity, asthma, delayed neurodevelopment, and metabolic disorders in adulthood.4–10 In addition to birth weight, other measures of neonatal size such as adiposity (percent fat mass) and weight-for-length (WFL) z-scores are used to assess infant health. Adiposity at birth is a potentially important marker of nutritional status and obesity and metabolic disease risk later in life.11 WFL z-scores, which can be derived from anthropometric measured collected at delivery, are the recommended metric for tracking obesity risk in infants from 0 to 2 years of age.12
Previous studies have identified individual-level factors influencing neonatal birth weight and body composition. These factors include younger or advanced maternal age, obesity, parity, levels of physical activity, race/ethnicity, gestational diabetes, and active smoking, among others.13–15 Environmental hazards such as air pollution have also been associated with decreased birth weight16–18 and increased skinfold thickness.19 Additionally, a small number of studies have identified a role for neighborhood-level exposures in perinatal outcomes.20–22 For example, a meta-analysis of studies reported significant associations between higher neighborhood deprivation score quintiles and SGA.23 The existing literature supports the hypothesis that neighborhood-level exposures affect perinatal outcomes, even when accounting for individual-level risk factors. However, few studies have investigated combined exposures (CEs) in multiple exposure domains, for example, the chemical, physical, and social environments.
We constructed indices that summarize exposures to chemical, physical, and social hazards using a Cumulative Exposure Assessment (CEA) framework that may address the single domain focus of prior studies. One commonly applied CEA approach is to map hazards across a geographic area and generate a semiquantitative measure of exposure by collapsing data into a single unitless index.24 These indices can take advantage of publically available data and are easy for decision-makers and other stakeholders to interpret.24 In addition to their usefulness as a screening tool, these indices are potentially valuable metrics to investigate how CEs might be associated with health outcomes.25
The objectives of this study were to assess CEs to environmental and social hazards at the census tract level during the prenatal period and to test associations with neonatal size and body composition. Our hypotheses were that higher environmental exposures, social exposures, and cumulative exposures would be associated with lower birth weight, higher adiposity (percent fat mass), and higher sex-specific WFL z-scores at birth.
Methods
Study population
The Healthy Start study is a pre-birth longitudinal cohort based in Denver, CO that has been investigating risk factors for childhood obesity and other health outcomes since 2009.26 Pregnant women of 16 years or older expecting singleton births were recruited from the University of Colorado Hospital between 2009 and 2014 (the first and last births occurred in March 2010 and September 2014, respectively) and invited to participate. Two prenatal study visits were conducted at median 17 and 27 weeks of gestation during which expectant mothers completed a physical exam and questionnaires about their diet and lifestyle. Additional data were abstracted from medical records. All mother-child dyads who had a first known address within the study area (n = 1,151 dyads) were eligible for this analysis. The final analytic dataset included n = 897 dyads with complete data on essential outcomes and covariates of interest. The healthy start study protocol was approved by the Colorado Multiple Institutional Review Board.
Study area
The study area consisted of most census tracts within three counties in the Denver Metropolitan area (Adams, Arapahoe, and Denver; Figure 1). Though healthy start participants live throughout the hospital catchment area, this analysis focused on a subset of census tracts for two reasons. First, there was considerable variability in the availability and quality of spatially-resolved data in the region; accordingly, we limited our study area to where reliable data could be obtained. Second, no air quality monitors were available that could provide reliable estimates of our air pollution indicators at the centroids of the two easternmost census tracts (located in Adams and Arapahoe counties). Therefore, we limited the study area to n = 386 (99.4%) census tracts in these counties.
Figure 1.
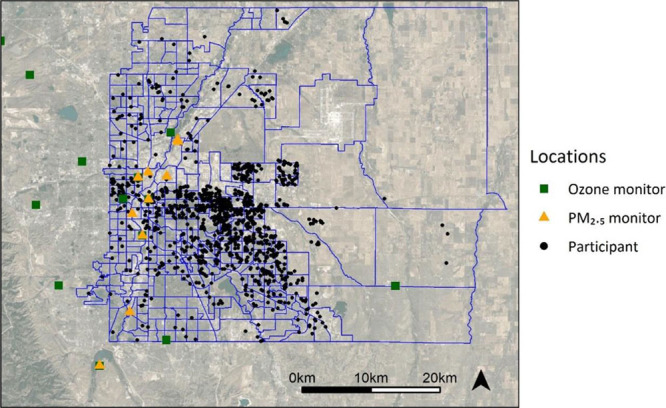
Map of the census tracts included in the study area. Participant locations are approximate.
The study area is located in the Front Range region of the Rocky Mountains and has a combination of topography, meteorology, and sources that create a unique pollution mix.27 Traffic is a predominant source of air pollution, and as a result, the area is currently in nonattainment of the 2008 ozone standard.28 There is also considerable variability in population-level SES and rates of comorbidities, for example, median census tract incomes range from <$10,000 per year to >$250,000, and ZIP code level annual cardiovascular disease hospitalization rates range from 123 to 472 per 10,000.
The spatial unit of analysis for this study was the census tract. This was the smallest unit for which reliable data on social determinants of health were available. Using census tracts also allowed us to retain some of the urban gradients observed for ambient air pollutants.29
Exposure assessment
Indicators of exposure included in the environmental exposure index (ENV) and social exposure index (SOC) were based on indicators selected for CalEnviroScreen 3.0, a screening tool developed by the California Office of Environmental Health Hazard Assessment (Figure 2).30 CalEnviroScreen has successfully been used as an exposure variable in another epidemiology study25 and was selected as a template for our indices because of its reliance on publically available datasets. Below we detail how these data were incorporated into the indices.
Figure 2.
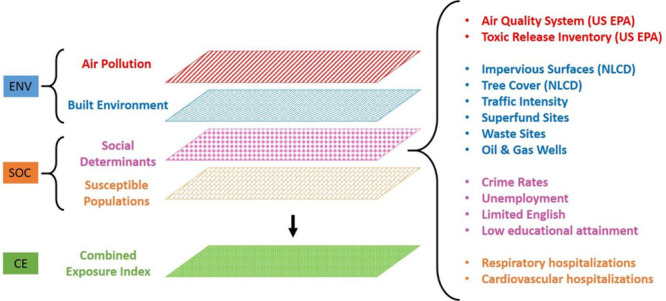
The conceptual model of the exposure variables used to generate the ENV, the SOC, and the CE.
Ambient air pollution
Ambient air pollution exposures were assessed using methods similar to those reported by CalEPA,30 with a modification to account for the timing of pregnancy. Monitoring data for fine particulate matter with an aerodynamic diameter <2.5 μm (PM2.5: 24 hours means every 3 days) and ozone (O3: hourly data) were retrieved from the Environmental Protection Agency’s Air Quality System Data Mart for a 6-year period (2009–2014). Only a limited number of O3 monitors in the state (n = 11) collected measurements during the cold season (October–March). For monitors that did not collect data during the cold season or for monitors with missing data during the warm season, missing hourly concentrations were imputed using predictive mean matching.31 To reduce computational burden and generate more stable estimates of PM2.5 and ozone at each monitor, concentrations at each location were summarized as biweekly means for PM2.5 and biweekly mean daily 8-hour maximum for O3. Ordinary kriging was used to estimate biweekly concentrations at census tract centroids. For each census tract, we included only data from monitors within 40 km of the centroid; the number of monitors used to estimate exposure for each census tract therefore varied. Average exposures for the duration of each pregnancy were assigned to individual mothers based on the conception and delivery dates and the census tract in which the first known address was located.
Environmental hazards
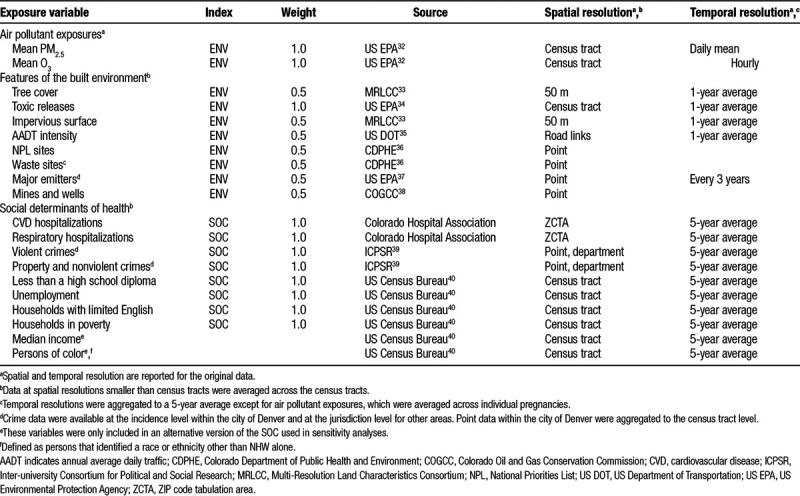
Environmental hazards used in the ENV included (among others): ambient PM2.5 and O3; toxic releases emitted by nearby facilities; the percentage of the census tract surface that is impermeable surfaces; and the density of daily traffic. Data sources and additional details are summarized in Table 1. All ENV indicators except PM2.5 and O3 were summarized at 5-year averages at the census tract level.
Table 1.
Description of data sources used to calculate the CE index
Social exposures
The SOC consisted of indicators of population vulnerability and susceptibility. Vulnerability indicators include demographic characteristics and neighborhood crime rates. Population susceptibility was represented using hospitalization rates for cardiovascular and respiratory diseases. Details on the variables used in the SOC are listed in Table 1. All SOC indicators were summarized at 5-year averages at the census tract level.
Calculating the exposure indices
The ENV and SOC were calculated separately and multiplied to form the CE index. Mothers were assigned exposures based on their census tract using the address at enrollment, and each indicator was converted into a percentile score. Consistent with CalEnviroScreen 3.0, the built environmental and hazardous land use indicator percentile scores were assigned a weight of 0.5.30 Environmental exposure percentile scores were averaged to generate the ENV index, and social exposure percentile scores were averaged to generate the SOC index. Component scores were divided by 10 and multiplied to generate the CE. The ENV, SOC, and CE values could range from 0 to 100, where 100 represents the most exposed index score.
The SOC index included several neighborhood-level socioeconomic indicators but did not use the percentage of the census tract population that identified a race or ethnicity other than non-Hispanic white (NHW) or the median income. These population-level variables are often used in environmental justice studies as a proxy for poor environmental quality.41, 42 However, we included other indicators that may more accurately reflect neighborhood conditions, such as higher exposures to traffic, educational attainment, and limited ability to speak English at the household level.43 To test the sensitivity of our models to omitting these variables, we constructed an alternative SOC (and CE) that included them.
Assessment of neonatal size and body composition
We focused on three neonatal outcomes: birth weight, adiposity (percent fat mass), and sex-specific WFL z-scores. Weight and length at birth were measured at the time of delivery and were taken from medical records. The Healthy Start protocol collected data on body composition using air displacement plethysmography (PEA POD; COSMED, Rome, Italy). Additional details on the PEA POD measurements are available elsewhere.26 Percent fat mass was calculated as the percentage of total body mass that was fat mass.44 Sex-specific WFL z-scores at birth were calculated from the weight and length measured at delivery using a WHO reference population.45,46
Statistical analysis
Summary statistics were used to examine the distributions of variables for healthy start participants. Participants included in the final analytic cohort were compared with those excluded using t tests and chi-squared tests as appropriate. Differences in mean index values by race/ethnicity and maternal education were assessed using analysis of variance and Tukey’s test for pairwise comparisons. An additional analysis (presented in the Supplemental Content; http://links.lww.com/EE/A36) used logistic regression to estimate the odds of living in a high exposure census tract based on maternal race/ethnicity or educational attainment.47
Associations between environmental exposure index, social exposure index, or combined exposure and neonatal size and body composition
For each of the outcomes, we developed separate statistical models for each exposure index (ENV, SOC, and CE). We also included a multivariable model that included both the ENV and SOC exposure indices.
For each model, covariates were included to test the robustness of results to potential confounding bias. We identified potential covariates based on previous studies investigating the effect of neighborhood-level exposures on neonatal outcomes (Table 2).18,20–23,48 We considered a number of maternal characteristics, including race/ethnicity, prepregnancy body mass index (BMI); active smoking and secondhand smoke (SHS) exposure during pregnancy, and educational attainment. We also included two measures of stress and depressive symptoms, Cohen’s Perceived Stress Scale (CPSS) and the Edinburgh Postnatal Depression Scale (EPDS), which were administered to mothers during their prenatal interviews. Infant covariates included gestational age at birth, the season of birth, and sex. For the percent fat mass models, we included the number of days between delivery and PEA POD measurements. We also used stepwise akaike information criterion (AIC) selection49 to reduce the number of model covariates starting with the full set of variables identified in the literature. In the Results section, we present models with all covariates included and the reduced models with only covariates selected by the stepwise AIC process. Regression diagnostics were used to ensure model assumptions were met. Effect sizes are reported for a 10-unit increase in index scores.
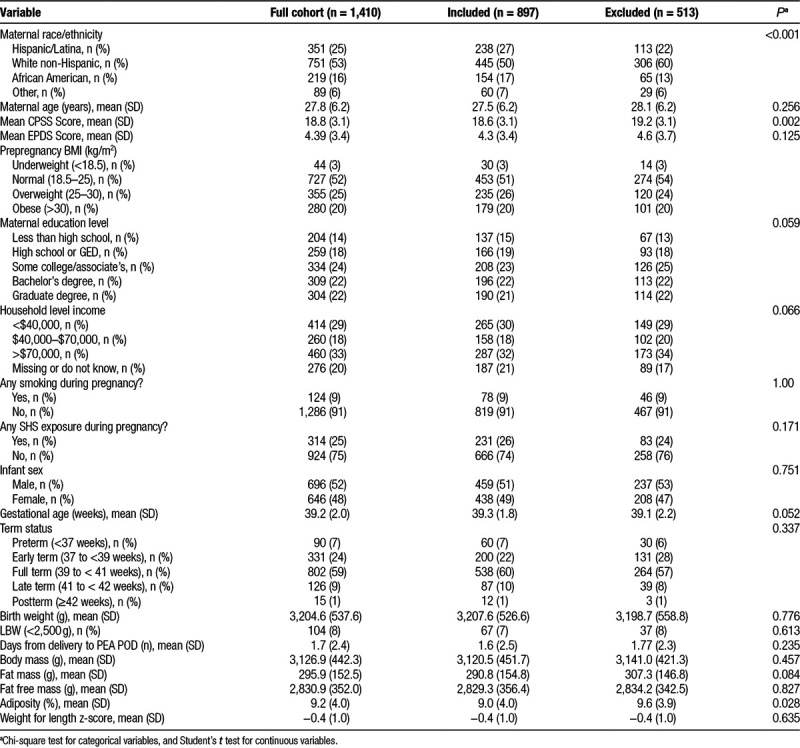
Table 2.
Descriptive statistics for outcome variables and potential covariates by inclusion status.
To assess how the ENV and SOC scores contributed to the effect of CE on neonatal outcomes, we included a secondary analysis where ENV and SOC index values were categorized based on tertiles and tested associations with the birth outcome variables. Participants were assigned to one of nine groups based on their ENV and SOC tertiles. We repeated the linear regression modeling using these categorical variables, with low ENV-low SOC serving as the reference group. We first fit univariate models for exposure categories and birth outcomes and then fit adjusted models using the same covariates described above.
Although the CE is the product of the ENV and SOC indices, it is not a true measure of statistical interaction. Therefore, we also included in a separate linear regression model the term ENV × SOC to understand if a statistical interaction model gave comparable results to the CE models.
All statistical analyses were performed in R.49,50 Maps were generated in R using the sf, ggplot2, viridis, and ggmap packages.51–54 For all regression models presented, we included effect estimates with confidence intervals (CIs) based on a type 1 error rate of 5% (α = 0.05).
Results
Descriptive statistics
Of the 1,410 mother-child dyads included in the healthy start cohort, complete exposure, outcome, and covariate data were available for 897 dyads (64%) (Table 2 and efigure 1; http://links.lww.com/EE/A36). Mothers excluded from the analysis were missing data on several variables, including delivery dates (n = 65), PEA POD measures (n = 154), infant sex (n = 68), CPSS or EPDS scores (n = 175 and 172, respectively), active smoking or SHS exposures (n = 163 and 172, respectively), and maternal age at delivery (n = 47). Compared to mothers with incomplete data, mothers with complete exposure, outcome, and covariate data were less likely to be NHW (pairwise comparison of proportions; P < 0.001) and have slightly lower mean CPSS across pregnancy (t test, P = 0.002). Babies born to mothers without complete exposure and covariate data had higher percent fat mass measures (9.6% vs. 9.0%; t test; P = 0.028). No differences were observed for other sociodemographic or outcome measures.
To assess the potential for selection bias based on exposure we compared with mothers living inside and outside exposure assessment boundary. Compared with mothers without exposure data (n = 259), mothers with first known addresses within the exposure assessment boundary (n = 1,151) were younger, more likely to be Hispanic/Latina or African American (pairwise comparison of proportions; P values < 0.001), and had a shorter interval between delivery and PEA POD (1.6 days vs. 2.2 days; t test; P = 0.008). These mothers also had lower average CPSS scores compared with excluded mothers (P = 0.007). No differences between mothers inside and outside the study area were observed for gestational age, body composition, or the remaining covariates (eTable 1; http://links.lww.com/EE/A36).
Environmental and social exposures varied across the study area (Table 3 and Figure 3). Air pollutant exposures demonstrated low variability across the study area. Average biweekly mean PM2.5 exposures across pregnancy averaged 7.5 µg/m3 (SD = 0.6 µg/m3; coefficient of variation [CV]: 10%) and ranged from 5.9 to 9.1 µg/m3. Biweekly mean daily 8-hour max O3 concentrations displayed similarly low variability, averaging 48.0 ppb (SD = 3.1 ppb; CV = 10%). Lower spatial variability in air pollutant exposures and built environment indicators resulted in moderate variability across ENV scores, which averaged 32.2 (SD = 9.4; CV = 30%) and ranged from 7.1 to 63.2. Social exposures demonstrated a higher degree of variability, for example, violent crime rates ranged from 0.6 to 81.8 incidents per 1,000 persons. The SOC scores displayed greater variability than ENV scores, averaging 36.3 (SD = 16.3; CV = 50%) with a range of 2.8 to 75.0. This increase in the variability of social exposures was reflected in the CE, which averaged 11.9 (SD = 6.8; CV = 60%) and ranged from 0.4 to 45.7. ENV and SOC were weakly correlated (Pearson’s R = 0.12), whereas CE was moderately correlated with ENV (R = 0.60) and highly correlated with SOC (R = 0.83).
Table 3.
Summary of exposure variables assessed at the census tract level for dyads included in the analytical cohort (n = 897).
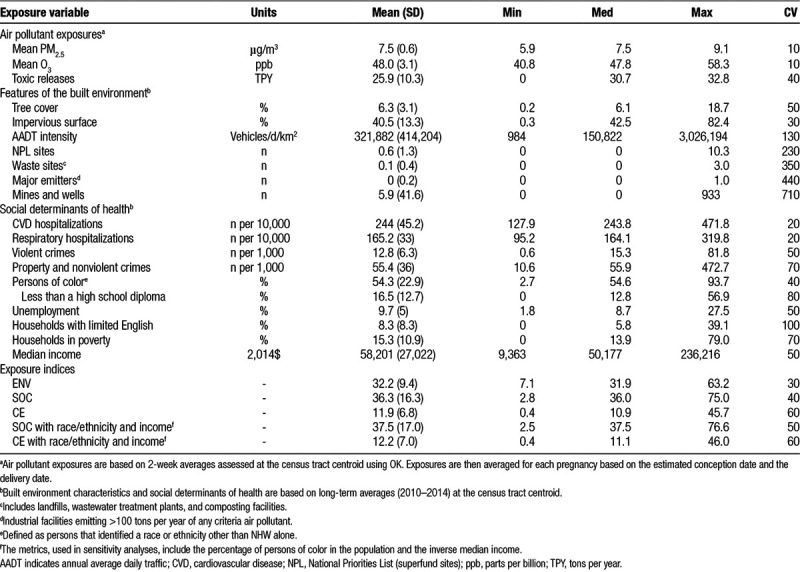
Figure 3.
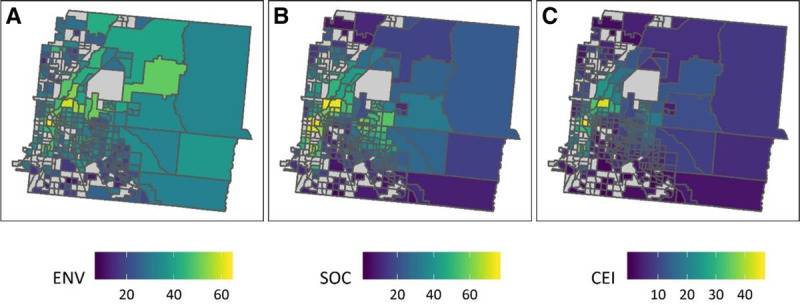
Average ENV, SOC, and CE scores for each census tract. For census tracts with more than one mother, scores were averaged across all mothers living within that census tract. Mothers within the same census tract could have different ENV and CE index scores based on the timing of their pregnancies.
In the supplemental analysis, we found that mothers of color or mothers with lower educational attainment had statistically significantly higher odds of living in a census tract with SOC and CE scores above the 75th percentile relative to NHW mothers or mothers with graduate degrees (eTable 6; http://links.lww.com/EE/A36). These results are discussed further in the Supplemental Content; http://links.lww.com/EE/A36.
Differences in exposure index values were observed based on race/ethnicity and educational attainment (Figure 4 and eTable 2; http://links.lww.com/EE/A36). Mean ENV scores were higher for mothers with advanced degrees compared with mothers with lower educational attainment (Tukey’s P < 0.05). In general, mothers with higher educational attainment tended to have higher average PM2.5 and O3 exposures across their pregnancies, resulting in higher ENV scores overall (eFigure 2; http://links.lww.com/EE/A36). In contrast, SOC and CE scores tended to be higher for mothers with lower socioeconomic status. Mean SOC scores were significantly higher for Latina and African American mothers relative to NHW mothers (all P values < 0.05) and for mothers with lower educational attainment compared with mothers with an advanced degree (all P values < 0.05). Similar patterns were observed for differences in mean CE scores by race/ethnicity and educational attainment.
Figure 4.
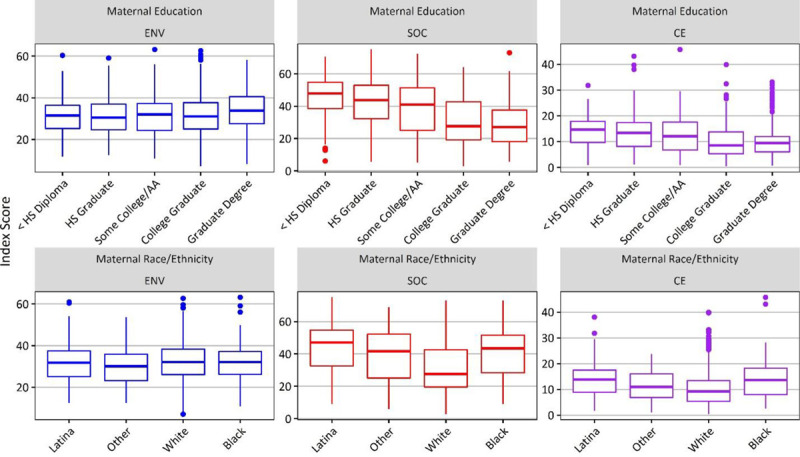
Box plots of ENV, SOC, and CE by maternal race/ethnicity and educational attainment. Includes all mothers with exposure, outcome, and covariate data (n = 897). AA, associate's degree; HS, high school.
Associations between environmental exposure index, social exposure index, or combined exposure and neonatal size and body composition
Prenatal SOC and CE indices were associated with decreased birth weight and percent fat mass (Table 4). After controlling for gestational age (weeks), the season of birth, infant sex, gravidity, prepregnancy BMI, any smoking during pregnancy, and race/ethnicity, a 10 unit increase in SOC was associated with a 27.4 g (95% CI = 12.4, 42.9 g) decrease in birth weight. There were also small associations observed between SOC and percent fat mass; after adjusting for covariates, a 10 unit increase was associated with a 0.3 (95% CI = 0.1, 0.4) percentage point decrease in percent fat mass. Associations between CE and birth weight and percent fat mass were stronger than for SOC alone. After controlling for gestational age (weeks), the season of birth, infant sex, gravidity, maternal age, average EPDS score across pregnancy, prepregnancy BMI, any smoking during pregnancy, race/ethnicity, and education, a 10 unit increase in CE was associated with a 56.3 g (95% CI = 19.4, 93.2 g) decrease in birth weight and a 0.6 (95% CI = 0.2, 1.0) percentage point decrease in percent fat mass. No associations were observed for ENV and any of the outcomes or for any exposure index and WFL z-scores.
Table 4.
Associations (95% CI) between exposure indices and birth outcomes.a

Single index models using the SOC and CE that included the proportion of the census tract population that identified as persons of color and the median income of the census tract produced similar results (eTable 3; http://links.lww.com/EE/A36).
In co-pollutant models, only SOC was a significant predictor of birth weight and percent fat mass. After adjusting for gestational age, infant sex, gravidity, smoking and SHS exposure during pregnancy, the season of birth, race/ethnicity, days between delivery and PEA POD measurements (percent fat mass model only), and ENV scores, a 10 unit increase in SOC was associated with a 20.9 g (95% CI = 6.1, 35.8 g) decrease in birth weight and a 0.2 (95% CI = 0.1, 0.4) percentage point decrease in percent fat mass, respectively.
The stratified analysis based on ENV and SOC tertiles showed that the associations described in Table 4 were driven by exposures in the highest combined ENV and SOC tertiles (eTable 4; http://links.lww.com/EE/A36). Babies born to mothers with SOC scores in the highest tertile and ENV scores in the middle and highest tertiles had significant decreases in birth weight and percent fat mass relative to babies born to mothers in the lowest exposure tertiles. No other significant associations were observed for mothers with other exposure categories.
Results of the sensitivity analysis exploring different specifications for models predicting birth weight or adiposity are summarized in eTable 5; http://links.lww.com/EE/A36. When investigating the main effect for ENV and SOC, including either CE or the statistical interaction term ENV × SOC did not change the coefficient for the main effects.
Discussion
Our results support the growing body of evidence that neighborhood-level factors are associated with neonatal size and body composition. After controlling for individual-level characteristics, we found that mothers who had higher index values for social determinants of health had babies with significantly lower birth weights and lower percent fat mass. We also found that average reductions in birth weights and in percent fat mass were even greater when we considered CEs to environmental hazards and social determinants of health. Though there are few studies looking at combined neighborhood-level environmental and social exposures on neonatal outcomes,55 our results align with other studies suggest high levels of environmental exposures or social disadvantage are associated with LBW.20–23
Our findings that SOC and CE values were higher on average for mothers of color and mothers with lower educational attainment were consistent with other studies on cumulative impacts among environmental justice communities.24,56–59 Contrary to our results, however, a study in California found that the environmental exposures were higher for census tracts with higher degrees of social disadvantage (measured using the proportion of nonwhite residents).47 In our study, lower educational attainment was associated with lower ENV scores (Figure 3). This result was likely partially because of the study area boundaries, and partially because of the distribution of highly educated populations living near the Urban Center of Denver, where traffic exposures and PM2.5 concentrations tend to be highest. Similar patterns of higher environmental exposures for higher SES neighborhoods have been reported for New York City.48,60
A small number of studies have assessed effect modification by neighborhood-level SES or deprivation on the association between air pollution and birth weight. For example, social deprivation scores were found to modify the relationship between nitrogen dioxide and birth weight, with the strongest negative associations for low and high deprivation areas.48 In California, decreases in birth weight associated with air pollutant exposures were significantly greater in neighborhoods with poverty rates >22% compared with neighborhoods with poverty rates <7%.18 Taken with the broader literature, our results suggest there are neighborhood-level effects on neonatal size and body composition that persist even after controlling for individual-level covariates.
We did not observe any associations between any of the indices and WFL z-scores. Although WFL z-scores are the recommended metric for tracking body composition in early childhood (0–2 years),12 a recent study using data from the Healthy Start cohort found that WFL z-scores measured at birth are more strongly correlated with fat-free (lean) mass rather than fat mass, as measured by air displacement plethysmography.61 Given the observed negative associations between the exposure indices and birth weight and percent fat mass, it is likely that these exposures acted on fat mass rather than lean mass to decrease overall birth weight. This finding is consistent with other reports on the effects of prenatal exposures on body composition in the Healthy Start cohort. For example, both higher prenatal perfluoroalkyl and polyfluoroalkyl substances exposures and later-pregnancy maternal blood pressure increases have been shown to be associated with decreased adiposity.62, 63 Reduced adiposity at birth may contribute to long-term health risks risk by contributing to rapid “catch up” growth associated with obesity and metabolic disease later in life.4 Future follow-up of the Healthy Start cohort will help clarify the long-term effects of decreased neonate adiposity on health.
Our results also suggest there is a potential multiplier or synergistic effect, where moderate to high exposures to both environmental hazards and social determinants of health are worse than exposures in either domain. We did not observe associations between ENV scores and any outcomes; however, these exposures influenced birth weight and percent fat mass when included in the CE score despite being relatively low with flat gradients across the region. Evidence of a synergistic effect for ENV and SOC on lower birth weight and percent fat mass in this study suggested that lower environmental exposures, for example, PM2.5 exposures below national standards, may still be important for neonatal outcomes depending on other contextual factors. Future work should apply statistical methods for assessing the health effects of mixtures, for example, Bayesian Kernel Machine Regression, to identify factors driving these associations. The primary advantage of mixtures methods over traditional multi-pollutant (or multi-exposure) models is that BMKR and other techniques are equipped to handle potential model fit issues arising from highly correlated exposures and can identify important interactions (or synergies) between individual exposures.64, 65
Potential mechanisms through which CEs might result in lower birth weights include additive or multiplicative effects from multiple exposures (as discussed above) or increased maternal stress associated with lower quality environments. Poor neighborhood-level conditions have been linked to higher levels of stress,66 which is a risk factor for adverse birth outcomes.67–69 Our analysis used CPSS70 to measure self-reported stress during three prenatal visits. However, the CPSS focuses on individual-level experiences rather than neighborhood context. Observed associations between higher CE scores and lower birth weights may be attributable to maternal stress attributable to neighborhood-level factors not measured by the CPSS.
There are some limitations that should be considered when interpreting the results of this study. First, we elected to use the CalEnviroScreen 3.0 model when developing the exposure indices, which may limit comparability to previous studies. Other constructs for CE indices exist, for example, the Environmental Quality Index and the Neighborhood Deprivation Index.71,72 However, the CalEnviroScreen model included important population-level indicators such as hospitalizations and allowed us to include time-varying air pollutant exposures for each pregnancy. Second, air pollutant exposure assessment relied on area monitoring data, which may not have fully captured the temporal and spatial variability across the study area. Additionally, we used total PM2.5 as an indicator of exposure. There is evidence that specific components of PM2.5 such as elemental carbon may be more strongly tied to outcomes than total PM2.5.73 Similar to other children’s health studies,74 our exposures were based on residential location and averaged over the duration of the pregnancy, which does not account for time-activity patterns. Third, complete residential histories were not available for Healthy Start participants, and exposures are based only on the address at enrollment. Fourth, some potentially important environmental quality indicators, for example, water quality were omitted from the ENV and CE. The selection of environmental quality indicators was informed by previous methods30 but limited by data availability in the area. Fifth, the ENV and CE included indicators that are more relevant to the study region (e.g., oil and gas wells) that may not be applicable to other locations in the United States or elsewhere. Lastly, spatial and temporal resolutions in indicator data were limited by what was publicly available. For example, ACS data are available at smaller spatial scales (e.g., census tracts) only for 5-year average periods75 and NEI data are collected every 3 years. There may be important temporal variabilities in ENV and SOC exposures not accounted for in our analysis. Despite these limitations, our results demonstrate the potential for neighborhood-level environmental and social exposures to affect the neonatal size and body composition and suggest more research using improved exposure assessment is needed to better confirm these findings.
Conclusions
We found CE to environmental hazards and social determinants of health were associated with neonatal size and body composition measured at birth. We also found that associations were stronger for these CEs than with just environmental exposures or social exposures alone. Our results emphasize the need to consider a total environmental and social exposure framework when investigating risk factors for perinatal outcomes that may influence childhood growth and development.
Conflict of interest statement
The authors declare that they have no financial conflict of interest
Supported by grants 5UG3OD023248, R01DK076648, and R01GM121081 from the National Institutes of Health, and RD-839278 from the US Environmental Protection Agency.
The code used to generate the exposure indices will be made available upon request. Personal health and geographical data are protected under an IRB protocol and are not available for distribution.
ACKNOWLEDGMENTS
The Colorado Hospital Association (CHA) provided data used for this project. CHA provided the data only and all conclusions and analysis are those of the authors.
Supplementary Material
Footnotes
Published online 4 April 2019
Supplemental digital content is available through direct URL citations in the HTML and PDF versions of this article (www.environepidem.com).
Sponsorships or competing interests that may be relevant to content are disclosed at the end of the article.
References
- 1.Donahue SMA, Kleinman KP, Gillman MW, Oken E. Trends in Birth Weight and Gestational Length Among Singleton Term Births in the United States. Obstet Gynecol 20101152 Pt 1357–364.doi:10.1097/AOG.0b013e3181cbd5f5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morisaki N, Esplin MS, Varner MW, Henry E, Oken E. Declines in birth weight and fetal growth independent of gestational length. Obstet Gynecol 2013121151–58.doi:http://10.1097/AOG.0b013e318278d014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oken E. Secular Trends in Birthweight. Recent Adv Growth Res Nutr Mol Endocr Perspect 201371103–114.doi:10.1159/000342576 [DOI] [PubMed] [Google Scholar]
- 4.Ong KK, Loos RJF. Rapid infancy weight gain and subsequent obesity: Systematic reviews and hopeful suggestions. Acta Paediatr 2006958904–908.doi:10.1080/08035250600719754 [DOI] [PubMed] [Google Scholar]
- 5.Nam H-K, Lee K-H. Small for gestational age and obesity: epidemiology and general risks. Ann Pediatr Endocrinol Metab 20182319–13.doi:10.6065/apem.2018.23.1.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Longo S, Bollani L, Decembrino L, Di Comite A, Angelini M, Stronati M. Short-term and long-term sequelae in intrauterine growth retardation (IUGR). J Matern-Fetal Neonatal Med Off J Eur Assoc Perinat Med Fed Asia Ocean Perinat Soc Int Soc Perinat Obstet 2013263222–225.doi:10.3109/14767058.2012.715006 [DOI] [PubMed] [Google Scholar]
- 7.van Wassenaer A. Neurodevelopmental consequences of being born SGA. Pediatr Endocrinol Rev PER 200523372–377. [PubMed] [Google Scholar]
- 8.Savchev S, Sanz-Cortes M, Cruz-Martinez R, et al. Neurodevelopmental outcome of full-term small-for-gestational-age infants with normal placental function. Ultrasound Obstet Gynecol 2013422201–206.doi:10.1002/uog.12391 [DOI] [PubMed] [Google Scholar]
- 9.Xu X-F, Li Y-J, Sheng Y-J, Liu J-L, Tang L-F, Chen Z-M. Effect of low birth weight on childhood asthma: a meta-analysis. BMC Pediatr 201414doi:10.1186/1471-2431-14-275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jornayvaz FR, Vollenweider P, Bochud M, Mooser V, Waeber G, Marques-Vidal P. Low birth weight leads to obesity, diabetes and increased leptin levels in adults: the CoLaus study. Cardiovasc Diabetol 201615doi:10.1186/s12933-016-0389-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Demerath EW, Fields DA. Body Composition Assessment in the Infant. Am J Hum Biol Off J Hum Biol Counc 2014263291–304.doi:10.1002/ajhb.22500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Daniels SR, Hassink SG, Nutrition CO. The Role of the Pediatrician in Primary Prevention of Obesity. Pediatrics 20151361e275–e292.doi:10.1542/peds.2015-1558 [DOI] [PubMed] [Google Scholar]
- 13.Valero de Bernabé J, Soriano T, Albaladejo R, et al. Risk factors for low birth weight: a review. Eur J Obstet Gynecol Reprod Biol 200411613–15.doi:10.1016/j.ejogrb.2004.03.007 [DOI] [PubMed] [Google Scholar]
- 14.Sewell MF, Huston-Presley L, Super DM, Catalano P. Increased neonatal fat mass, not lean body mass, is associated with maternal obesity. Am J Obstet Gynecol 200619541100–1103.doi:10.1016/j.ajog.2006.06.014 [DOI] [PubMed] [Google Scholar]
- 15.Harvey NC, Poole JR, Javaid MK, et al. Parental Determinants of Neonatal Body Composition. J Clin Endocrinol Metab 2007922523–526.doi:10.1210/jc.2006-0456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bell ML, Ebisu K, Belanger K. Ambient Air Pollution and Low Birth Weight in Connecticut and Massachusetts. Environ Health Perspect 200711571118–1124.doi:10.1289/ehp.9759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lakshmanan A, Chiu Y-HM, Coull BA, et al. Associations between prenatal traffic-related air pollution exposure and birth weight: Modification by sex and maternal pre-pregnancy body mass index. Environ Res 2015137268–277.doi:10.1016/j.envres.2014.10.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morello-Frosch R, Jesdale BM, Sadd JL, Pastor M. Ambient air pollution exposure and full-term birth weight in California. Environ Health 20109144.doi:10.1186/1476-069X-9–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schembari A, de Hoogh K, Pedersen M, et al. Ambient Air Pollution and Newborn Size and Adiposity at Birth: Differences by Maternal Ethnicity (the Born in Bradford Study Cohort). Environ Health Perspect 2015123111208–1215.doi:10.1289/ehp.1408675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kane JB, Miles G, Yourkavitch J, King K. Neighborhood context and birth outcomes: Going beyond neighborhood disadvantage, incorporating affluence. SSM - Popul Health 20173699–712.doi:10.1016/j.ssmph.2017.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ncube CN, Enquobahrie DA, Albert SM, Herrick AL, Burke JG. Association of neighborhood context with offspring risk of preterm birth and low birthweight: A systematic review and meta-analysis of population-based studies. Soc Sci Med 1982 2016153156–164.doi:10.1016/j.socscimed.2016.02.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nowak AL, Giurgescu C. The Built Environment and Birth Outcomes: A Systematic Review. MCN Am J Matern Child Nurs 201742114–20.doi:10.1097/NMC.0000000000000299 [DOI] [PubMed] [Google Scholar]
- 23.Vos AA, Posthumus AG, Bonsel GJ, Steegers EAP, Denktaş S. Deprived neighborhoods and adverse perinatal outcome: a systematic review and meta-analysis. Acta Obstet Gynecol Scand 2014938727–740.doi:10.1111/aogs.12430 [DOI] [PubMed] [Google Scholar]
- 24.Solomon GM, Morello-Frosch R, Zeise L, Faust JB. Cumulative Environmental Impacts: Science and Policy to Protect Communities. Annu Rev Public Health 20163783–96.doi:10.1146/annurev-publhealth-032315-021807 [DOI] [PubMed] [Google Scholar]
- 25.Vieira VM, Villanueva C, Chang J, Ziogas A, Bristow RE. Impact of community disadvantage and air pollution burden on geographic disparities of ovarian cancer survival in California. Environ Res 2017156388–393.doi:10.1016/j.envres.2017.03.057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harrod CS, Chasan-Taber L, Reynolds RM, et al. Physical activity in pregnancy and neonatal body composition: the Healthy Start study. Obstet Gynecol 20141242 Pt 1257–264.doi:10.1097/AOG.0000000000000373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vedal S, Hannigan MP, Dutton SJ, et al. The Denver Aerosol Sources and Health (DASH) Study: Overview and Early Findings. Atmospheric Environ Oxf Engl 1994 20094391666–1673.doi:10.1016/j.atmosenv.2008.12.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.US Environmental Protection Agency [US EPA] 8-Hour Ozone (2008) Designated Area/State Information with Design Values. Green Book. https://www3.epa.gov/airquality/greenbook/hbtcw.html. Published May 31, 2018. Accessed June 26, 2018.
- 29.Batterman S, Chambliss S, Isakov V. Spatial resolution requirements for traffic-related air pollutant exposure evaluations. Atmos Environ 201494518–528.doi:10.1016/j.atmosenv.2014.05.065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Office of Environmental Health Hazard Assessment. CalEnviroScreen 3.0. OEHHA. https://oehha.ca.gov/calenviroscreen/report/calenviroscreen-30. Published December 29, 2016. Accessed November 28, 2017.
- 31.van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate Imputation by Chained Equations in R. J Stat Softw 20112531–67.https://www.jstatsoft.org/article/view/v045i03. Accessed February 6, 2017 [Google Scholar]
- 32.US Environmental Protection Agency [US EPA] AQS Data Mart. https://aqs.epa.gov/api. Published 2016. Accessed July 30, 2016.
- 33.Multi-Resolution Land Characteristics Consortium. National Land Cover Database. https://www.mrlc.gov/. Published November 1, 2017. Accessed November 17, 2017.
- 34.US Environmental Protection Agency [US EPA] TRI Data and Tools. US EPA. https://www.epa.gov/toxics-release-inventory-tri-program/tri-data-and-tools. Published March 3, 2013. Accessed August 27, 2018.
- 35.US Department of Transportation [US DOT] Highway Performance Monitoring System. https://www.fhwa.dot.gov/policyinformation/hpms.cfm. Published 2018. Accessed July 23, 2018.
- 36.Colorado Department of Public Health and Environment [CDPHE] Maps and GIS for health and environment. https://www.colorado.gov/pacific/cdphe/maps-and-spatial-data. Published 2018. Accessed July 23, 2018.
- 37.US Environmental Protection Agency [US EPA] National Emissions Inventory. http://www.epa.gov/ttn/chief/net/2005inventory.html#inventorydata. Published 2012. Accessed March 10, 2015.
- 38.Colorado Oil and Gas Conservation Commission [COGCC] Colorado Oil and Gas Information System. https://cogcc.state.co.us/data.html#/cogis. Published 2018. Accessed July 23, 2018.
- 39.Inter-university Consortium for Political and Social Research [ICPSR] Uniform Crime Reporting Program Data Series. https://www.icpsr.umich.edu/icpsrweb/ICPSR/series/57. Published 2018. Accessed July 23, 2018.
- 40.US Census Bureau. 2010–2014 American Community Survey (ACS) 5-year Estimates. https://www.census.gov/programs-surveys/acs/. Published 2014. Accessed October 6, 2016.
- 41.Clark LP, Millet DB, Marshall JD. National Patterns in Environmental Injustice and Inequality: Outdoor NO2 Air Pollution in the United States. Plos One 201494e94431.doi:10.1371/journal.pone.0094431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dominguez-Cortinas G, Cifuentes E, Rico Escobar E, Diaz-Barriga Martinez F. Assessment of Environmental Health Children’s Population Living in Environmental Injustice Scenarios. J Community Health 20123761199–1207.doi:10.1007/s10900-012-9555-y [DOI] [PubMed] [Google Scholar]
- 43.Cheng TL, Goodman E; Research TC on P Race, Ethnicity, and Socioeconomic Status in Research on Child Health. Pediatrics 20151351e225–e237.doi:10.1542/peds.2014–3109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Starling AP, Brinton JT, Glueck DH, et al. Associations of maternal BMI and gestational weight gain with neonatal adiposity in the Healthy Start study. Am J Clin Nutr 20151012302–309.doi:10.3945/ajcn.114.094946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Moore BF, Sauder KA, Starling AP, Ringham BM, Glueck DH, Dabelea D. Exposure to secondhand smoke, exclusive breastfeeding and infant adiposity at age 5 months in the Healthy Start study. Pediatr Obes 201712Suppl 1111–119.doi:10.1111/ijpo.12233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.World Health Organization [WHO] Geneva: 2006. WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development. [Google Scholar]
- 47.Cushing L, Faust J, August LM, Cendak R, Wieland W, Alexeeff G. Racial/Ethnic Disparities in Cumulative Environmental Health Impacts in California: Evidence From a Statewide Environmental Justice Screening Tool (CalEnviroScreen 1.1). Am J Public Health 2015105112341–2348.doi:10.2105/AJPH.2015.302643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shmool JLC, Bobb JF, Ito K, et al. Area-level socioeconomic deprivation, nitrogen dioxide exposure, and term birth weight in New York City. Environ Res 2015142624–632.doi:10.1016/j.envres.2015.08.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kuhn M, Wing J, Weston S, et al. Caret: Classification and Regression Training. R Package Version 6.0–80 2018https://CRAN.R-project.org/package=caret. Accessed 30 July 2018
- 50.R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2018. http://www.R-project.org/. Accessed 30 July 2018. [Google Scholar]
- 51.Garnier S. Viridis: Default Color Maps from “matplotlib’’. R Package Version 0.5.1.” 2018https://CRAN.R-project.org/package=viridis. Accessed 30 July 2018 [Google Scholar]
- 52.Kahle D, Wickham H. ggmap: Spatial Visualization with ggplot2. R J 201351144–161. [Google Scholar]
- 53.Pebsema E. Sf: Simple Features for R. R Package Version 0.6–3 2018https://CRAN.R-project.org/package=sf [Google Scholar]
- 54.Wickham H. Ggplot2: Elegant Graphics for Data Analysis 2016New York: Springer-Verlag [Google Scholar]
- 55.Burris HH, Hacker MR. Birth outcome racial disparities: A result of intersecting social and environmental factors. Semin Perinatol 2017416360–366.doi:10.1053/j.semperi.2017.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Morello-Frosch R, Zuk M, Jerrett M, Shamasunder B, Kyle AD. Understanding The Cumulative Impacts Of Inequalities In Environmental Health: Implications For Policy. Health Aff (Millwood) 2011305879–887.doi:10.1377/hlthaff.2011.0153 [DOI] [PubMed] [Google Scholar]
- 57.Sadd JL, Pastor M, Morello-Frosch R, Scoggins J, Jesdale B. Playing it safe: assessing cumulative impact and social vulnerability through an environmental justice screening method in the South Coast Air Basin, California. Int J Environ Res Public Health 2011851441–1459.doi:10.3390/ijerph8051441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Su JG, Morello-Frosch R, Jesdale BM, Kyle AD, Shamasunder B, Jerrett M. An Index for Assessing Demographic Inequalities in Cumulative Environmental Hazards with Application to Los Angeles, California. Environ Sci Technol 200943207626–7634.doi:10.1021/es901041p [DOI] [PubMed] [Google Scholar]
- 59.Su JG, Jerrett M, Morello-Frosch R, Jesdale BM, Kyle AD. Inequalities in cumulative environmental burdens among three urbanized counties in California. Environ Int 20124079–87.doi:10.1016/j.envint.2011.11.003 [DOI] [PubMed] [Google Scholar]
- 60.Savitz DA, Bobb JF, Carr JL, et al. Ambient Fine Particulate Matter, Nitrogen Dioxide, and Term Birth Weight in New York, New York. Am J Epidemiol 20141794457–466.doi:10.1093/aje/kwt268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Perng W, Ringham BM, Glueck DH, et al. An observational cohort study of weight- and length-derived anthropometric indicators with body composition at birth and 5 mo: the Healthy Start study. Am J Clin Nutr 20171062559–567.doi:10.3945/ajcn.116.149617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Starling AP, Adgate JL, Hamman RF, et al. Perfluoroalkyl Substances during Pregnancy and Offspring Weight and Adiposity at Birth: Examining Mediation by Maternal Fasting Glucose in the Healthy Start Study. Environ Health Perspect 20171256067016.doi:10.1289/EHP641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Starling AP, Shapiro ALB, Sauder KA, et al. Blood pressure during pregnancy, neonatal size and altered body composition: the Healthy Start study. J Perinatol 2017375502–506.doi:10.1038/jp.2016.261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Braun JM, Gennings C, Hauser R, Webster TF. What Can Epidemiological Studies Tell Us about the Impact of Chemical Mixtures on Human Health? Environ Health Perspect 20161241A6–A9.doi:10.1289/ehp.1510569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Davalos AD, Luben TJ, Herring AH, Sacks JD. Current approaches used in epidemiologic studies to examine short-term multipollutant air pollution exposures. Ann Epidemiol 2017272145–153.e1.doi:10.1016/j.annepidem.2016.11.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Boardman JD. Stress and physical health: the role of neighborhoods as mediating and moderating mechanisms. Soc Sci Med 200458122473–2483.doi:10.1016/j.socscimed.2003.09.029 [DOI] [PubMed] [Google Scholar]
- 67.Dole N, Savitz DA, Hertz-Picciotto I, Siega-Riz AM, McMahon MJ, Buekens P. Maternal Stress and Preterm Birth. Am J Epidemiol 2003157114–24.doi:10.1093/aje/kwf176 [DOI] [PubMed] [Google Scholar]
- 68.Hobel CJ, Goldstein A, Barrett ES. Psychosocial Stress and Pregnancy Outcome. Clin Obstet Gynecol 2008512333.doi:10.1097/GRF.0b013e31816f2709 [DOI] [PubMed] [Google Scholar]
- 69.Nkansah-Amankra S, Luchok KJ, Hussey JR, Watkins K, Liu X. Effects of Maternal Stress on Low Birth Weight and Preterm Birth Outcomes Across Neighborhoods of South Carolina, 2000–2003. Matern Child Health J 2010142215–226.doi:10.1007/s10995-009-0447-4 [DOI] [PubMed] [Google Scholar]
- 70.Cohen S, Kamarck T, Mermelstein R. A Global Measure of Perceived Stress. J Health Soc Behav 1983244385–396.doi:10.2307/2136404 [PubMed] [Google Scholar]
- 71.Messer LC, Jagai JS, Rappazzo KM, Lobdell DT. Construction of an environmental quality index for public health research. Environ Health 20141339.doi:10.1186/1476-069X-13–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Messer LC, Laraia BA, Kaufman JS, et al. The development of a standardized neighborhood deprivation index. J Urban Health Bull N Y Acad Med 20068361041–1062.doi:10.1007/s11524-006-9094-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ebisu K, Bell ML. Airborne PM2.5 Chemical Components and Low Birth Weight in the Northeastern and Mid-Atlantic Regions of the United States. Environ Health Perspect 2012120121746–1752.doi:10.1289/ehp.1104763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Khreis H, Nieuwenhuijsen MJ. Traffic-Related Air Pollution and Childhood Asthma: Recent Advances and Remaining Gaps in the Exposure Assessment Methods. Int J Environ Res Public Health 20171431–19.doi:10.3390/ijerph14030312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.U.S. Census Bureau. Understanding and Using American Community Survey Data: What All Data Users Need to Know. 2018 https://www.census.gov/content/dam/Census/library/publications/2018/acs/acs_general_handbook_2018.pdf. Accessed 1 January 2019.


