Abstract
Background:
Sensory information gained through interoceptive awareness may play an important role in affective behavior and successful inhibition of drug use. This study examined the immediate pre-post effects of the mind-body intervention Mindful Awareness in Body-oriented Therapy (MABT) as an adjunct to women’s substance use disorder (SUD) treatment. MABT teaches interoceptive awareness skills to promote self-care and emotion regulation.
Methods:
Women in intensive outpatient treatment (IOP) for chemical dependency (N = 217) at 3 community clinics in the Pacific Northwest of the United States were recruited and randomly assigned to one of 3 study conditions: MABT + treatment as usual (TAU), women’s health education (WHE) + TAU (active control condition), and TAU only. At baseline and 3 months post-intervention, assessments were made of interoceptive awareness skills and mindfulness, emotion regulation (self-report and psychophysiological measures), symptomatic distress (depression and trauma-related symptoms), and substance use (days abstinent) and craving. Changes in outcomes across time were assessed using multilevel mixed-effects linear regression.
Results:
Findings based on an intent-to-treat approach demonstrated significant improvements in interoceptive awareness and mindfulness skills, emotion dysregulation (self-report and psychophysiology), and days abstinent for women who received MABT compared with the other study groups. Additional analyses based on participants who completed the major components of MABT (at least 75% of the intervention sessions) revealed these same improvements as well as reductions in depressive symptoms and substance craving.
Conclusions:
Findings that interoceptive training is associated with health outcomes for women in SUD treatment are consistent with emerging neurocognitive models that link interoception to emotion regulation and to related health outcomes, providing knowledge critical to supporting and improving SUD treatment.
Keywords: Complementary therapies, emotion regulation, interoception, mindfulness, substance use disorder, treatment, women
Introduction
For individuals seeking substance use disorder (SUD) treatment to address negative affect and stress, known primary precipitants to relapse,1–4 emotion regulation is likely to be critical treatment component.5–8 Emotion regulation involves the ability to monitor, understand, and accept emotions and to engage in goal-directed behavior.9 In contrast, emotion dysregulation is characterized by intense emotions, low stress tolerance, experiential avoidance, and lack of control.10 Importantly, emotion regulation difficulties are significantly greater among individuals in SUD treatment compared with the general population.5,6 Although few SUD treatment studies have utilized measures of emotion regulation, results from those that have suggest the importance of emotion regulation for positive treatment outcomes.11–13
Difficulty with emotion regulation is also common in clinical samples with co-occurring forms of psychopath-ology14,15 and is a primary clinical characteristic of individuals with a history of interpersonal trauma.16 The relevance of emotion dysregulation to SUD treatment is likely due to the high prevalence of co-occurring disorders in this population.17–19 Women compared with men have a higher prevalence of co-occurring mental health disorders, including interpersonal trauma.20,21 Dysregulated emotion is particularly evident among individuals with a history of childhood abuse, who are also at increased risk for SUD.22,23 Similarly, individuals in SUD treatment with, compared with those without, a history of childhood trauma and posttraumatic stress disorder (PTSD) have more emotion regulation difficulties.24 Thus, new and accumulating evidence highlights the importance of studying SUD interventions designed to promote skills in emotion regulation.
Dysregulated emotion in SUD has been linked to interoceptive dysfunction among individuals with SUD.25,26 Interoception is the processing of sensory input from inside the body.27,28 Sensory information gained through interoception may play an important role in affective behavior and relapse prevention among those in SUD treatment.29–31 Specifically, gaining interoceptive awareness (i.e., awareness of emotional and physical sensations) and learning to develop the capacity to attend to sensory cues may positively affect cognitive control and decision-making processes that underlie patterns of behavior associated with substance use.32
Interoceptive awareness is a fundamental aspect of mindfulness-based interventions, typically introduced through mindful attention to the sensation of inhaling and exhaling during respiration, and guided body scans, in a group context. Mindfulness-based SUD research shows reduced substance use and related health outcomes such as negative affect,33 depression,34 symptoms of posttraumatic stress,35 and craving.36,37 With interoception recognized as a possible mechanism underlying mindfulness-based approaches for SUD treatment,38,39 an identified gap in SUD research is the lack of large-sample SUD treatment studies that specifically target the development of interoceptive awareness skills.25,32,40
Mindful Awareness in Body-oriented Therapy (MABT) is a mindfulness-based approach uniquely designed to teach interoceptive awareness and related skills for self-care.41 This therapeutic approach was developed to facilitate the ability to access and develop interoceptive awareness skills, particularly important for individuals who face difficulties in attending to interoceptive signals, due to high stress, chronic pain, depression, or trauma. MABT provides an individualized protocol for scaffolding interoceptive awareness in the face of such difficulties, through a combination of psycho-educational and manual therapies that explicitly address difficulties with interoceptive processing. An initial feasibility study of MABT as an adjunct to women’s SUD treatment (N = 46) found several noteworthy results, including reduced substance use and symptoms of depression, perceived stress, physical symptoms of discomfort of pain, and bodily dissociation (an interoceptive awareness indicator) from baseline to 9-month follow-up.13 For individuals who received MABT, improvements in bodily dissociation contributed directly to reductions in trauma-related symptoms and indirectly to reductions in symptoms of emotion dysregulation.42 In addition, the results highlighted the ability to acquire and maintain interoceptive skills for self-care in response to MABT training.43 Although revealing promising results, the feasibility study sample was small and the design did not address the potential confounder of additional time and attention that MABT provided.
To address these shortcomings, we conducted a larger, pragmatic, randomized controlled trial of MABT, again within the context of outpatient SUD treatment for women. We also included an active control condition to test the efficacy of MABT as an adjunct to treatment as usual (TAU). This report describes the immediate pre-post results of this new research project. The primary outcomes are derived from the MABT explanatory model, which posits that interoceptive awareness underlies emotion regulation and related psychological outcomes. We hypothesized that MABT compared with TAU and women’s health education (WHE) would result in improved (a) interoceptive awareness and mindfulness skills (primary outcomes), (b) emotion regulation (self-report and psychophysiology), and (c) symptomatic distress (e.g., depression and trauma-related symptoms), and (d) substance use and craving.
Methods
Design
The focus of this paper is on the immediate pre- and post-intervention results from a longitudinal National Institute on Drug Abuse (NIDA)-funded study to examine the efficacy of MABT. The study design was a 3-group repeated-measures, randomized clinical trial. The longitudinal project was powered on several outcomes; for this study with interoceptive awareness as the primary outcome, the study was powered for a moderate effect (β=.40) based on pilot study results.13 The study procedures and consent forms, reviewed and approved by the institutional review board at a large university in the northwestern United States, were in accord with the Helskinki Declaration of 1975. The study was implemented in 3 community SUD outpatient treatment clinics. Women engaged in the clinic intensive outpatient program (IOP) were recruited for study participation. IOP served as the treatment as usual (TAU) condition; thus, this research examined the efficacy of MABT as an adjunct intervention to TAU. The “women’s health education” (WHE) group, designed to control for time and attention, involved educational sessions to provide women’s health information. Accordingly, participants were randomized to one of 3 possible study groups: MABT + TAU, WHE + TAU, or TAU only. Those assigned to MABT or WHE were offered an individually delivered intervention involving eight 90-minute sessions, delivered once weekly. All intervention sessions were provided by trained interventionists at the clinical site where the participant attended SUD treatment.
Clinical sites and study personnel
The 3 SUD clinics were located in a large urban area of the Pacific Northwest: one was a women’s only clinic and the other 2 clinics served men and women. The clinics were not-for-profit organizations, which served primarily individuals of low socioeconomic status (SES). The clinics offered outpatient, abstinent-based SUD programs, with IOP as well as less intensive (i.e., step-down) continuing care programs for individuals diagnosed with chemical dependency and seeking treatment. All 3 clinics collected random urine toxicology screens and maintained electronic health records.
There were 2 research coordinators, 2 WHE interventionists, and 3 MABT interventionists involved in the project. There was 1 MABT therapist assigned to each clinical site. One research coordinator and 1 WHE interventionist worked at the women’s only clinic, and the other research coordinator and WHE interventionist split their time between the other 2 facilities.
Recruitment and screening
Female patients enrolled in the 3 treatment facilities were recruited for study participation. Recruitment methods included posting of flyers in the clinics for self-referral, and presentation of the study in IOP groups by the research coordinator followed by a sign-up sheet for those interested in learning more. The research coordinator at each clinical site screened interested participants for study eligibility. Inclusion criteria were (1) female; (2) enrolled in IOP; (3) agreed to forgo (nonstudy) manual therapies (e.g., massage) and mind-body therapies (e.g., mindfulness meditation) for 3 months (baseline to post-test); (4) willing to sign release for access to electronic medical records; (5) fluent in English; and (6) able to attend MABT sessions. Exclusion criteria were (1) untreated psychotic diagnosis or symptoms;(2) unwilling or unable to remain in treatment for the duration of the trial (e.g., planned relocation, pending incarceration, upcoming surgical procedures); (3) cognitive impairment based on an informed consent assessment of demonstrated comprehension difficulty during consent; or (4) currently pregnant.
Enrollment and randomization
Patients eligible for study participation were administered the consent form and baseline measures by the research coordinator. After completing the study enrollment process, participants were randomly assigned to study treatment group using a block random group generator in STATA (StataCorp, College Station, TX) to distribute participants by clinic, such that equal distribution of cases to MABT, WHE, or TAU occurred for every block of 6 enrolled participants. Block randomization was used to facilitate the workload spacing for interventionists, as MABT and WHE sessions were offered only 1 day/week at each clinical site.
Treatment as usual
The intensive outpatient program at the 3 study site clinics complied with the specific requirements of the Washington State Code (WAC) that regulates chemical dependency IOP treatment, requiring a complete admission assessment, development of an individual treatment plan that involves group and individual counseling, education about alcohol and drug use, and participation in self-help groups (e.g., 12-step or equivalent) for SUD. IOP consisted of group sessions 2–3 times/week for 10–14 weeks and individual counseling sessions once per month at minimum. Psychoeducation was the primary approach used.
Mindful Awareness in Body-oriented Therapy (MABT)
MABT is a manualized protocol, developed by the first author (C.J.P.). The intervention involves 90-minute weekly sessions delivered individually over approximately 8–10 weeks. The protocol has 3 distinct stages for teaching interoceptive awareness and take-home skills. The stages provide an incremental approach to facilitate learning the interoceptive awareness components of Stage 1: identifying body sensations (body literacy); Stage 2: learning and developing strategies for interoceptive awareness; and Stage 3: developing the capacity to sustain interoceptive awareness as a mindful process to facilitate appraisal of interoceptive experiences (see Table 1). Touch is used to facilitate the participant’s ability to focus mindful attention to the body (vs. having attention wander, for example). These MABT stages align with the key aspects of interoceptive awareness27—specifically identifying, accessing, and appraisal—to promote the development of interoception and integration of related self-care skills to facilitate emotional awareness and regulation in daily life. Touch is used to facilitate the participant’s ability to focus mindful attention to the body (vs. having attention wander, for example). Participants learn to use their own hands (self-touch) to develop their capacity for and practice of interoceptive awareness skills in daily life. Three MABT pilot studies demonstrated the feasibility, acceptability, and safety of MABT for women in recovery from sexual trauma44–46 or chemical dependency.13 The Intake and Session Review aspects of the session are critical. Intake, taking approximately 30 minutes at the beginning of each session, is designed to gather information about the participant’s emotional and physical well-being, describe MABT processes, discuss use of take-home practice, and develop rapport. At the end of each session, approximately 15 minutes is reserved to review the interoceptive awareness training experience to promote cognitive integration and to guide the collaborative development of a take-home practice for the interim week.
Table 1.
Elements of MABT sessions.
| Stage 1 (Sessions 1–2) | Stage 2 (Sessions 3–4) | Stage 3 (Sessions 5–8) |
|---|---|---|
| Intake (30) | Intake (30) | Intake (30) |
| Body Literacy (45) | Body Literacy (15) | Body Literacy (15) |
| Interoceptive | Mindful Body | |
| Awareness Training (30) | Awareness Practice (30) | |
| Session Review (15) | Session Review (15) | Session Review (15) |
| Homework | Homework | Homework |
Note. Values in parentheses represent time spent in number of minutes in each session.
MABT, which integrates the use of touch, was delivered by licensed and experienced massage therapists who were trained to deliver the MABT protocol. The MABT approach involves a high level of client-therapist verbal interaction, with 45 minutes of each session used for the Session Intake and Session Review (see Table 1) as well during the interoceptive awareness training. Thus, all MABT therapists had considerable prior education and clinical experience, including advanced training in mind-body approaches or psychotherapy (certification programs or master’s degrees), a minimum of 10 years in practice, and significant clinical and/or research experience working with mental health concerns. They received direct training in the delivery of the MABT protocol. To monitor intervention fidelity and provide clinical supervision for therapists, all sessions were audio-recorded. Implementation fidelity of the MABT protocol was monitored by the principal investigator (C.J.P.), including twice-monthly review of audio-recorded sessions and process evaluation forms completed by the therapist after each session, and routine clinical supervision.
Women’s health education (WHE)
A manualized protocol for WHE was developed for this study, based on a similar attention-control intervention used in women’s SUD treatment studies.47,48 Delivered as a group curriculum in prior studies, the protocol for this project was developed for individual delivery involving eight 90-minute weekly sessions to match the time and attention of the MABT intervention. WHE contained a health curriculum focused on topics such as understanding the female body, reproductive health, cardiovascular health, and sexually transmitted diseases. It was designed to provide equivalent therapeutic attention, expectancy of benefit, and an issue-oriented focus, but without theory-driven techniques (i.e., of MABT or any explicit focus on mindfulness or body awareness). WHE health educators were college educated and had past work experience as research coordinators in behavioral health. They received direct training in the delivery of the health curriculum. To monitor intervention fidelity and provide clinical supervision for health educators, all sessions were audio-recorded. The fidelity to the WHE protocol was monitored by study co-investigator (C.H.) twice-monthly by review of audio-recorded sessions and process evaluation forms, completed by educators after each session, along with routine clinical supervision.
Procedures
Data were collected by research coordinators at 2 time points (baseline and at 3 months) and included (1) a calendar method interview and biochemical assay to collect alcohol or drug use information; (2) an online survey to collect self-reported health-related information using standardized questionnaires; and (3) a psychophysiological assessment to collect respiratory sinus arrhythmia (RSA).
RSA data collection
For RSA data collection, participants were asked to refrain from over-the-counter medications that could affect psychophysiological recordings and all participants completed approximately 1 hour of questionnaires prior to the psychophysiological assessment, which minimized other potential confounds (e.g., caffeine, tobacco intake, or strenuous exercise prior to assessment). Electrodes were placed on the participants’ torso using a standard spot configuration with one electrode placed on the right clavicle and the other on the left abdomen near the bottom of the ribcage.49 Tonic (i.e., resting-state) RSA was measured during a 5-minute baseline period, during which time participants were asked to sit quietly.
We examined phasic (i.e., task-based) RSA in response to 3 challenging tasks. The tasks were (1) watching a film clip that had been demonstrated to elicit sad emotions (Steel Magnolias) for 5.5 minutes50; (2) ruminating on a recent negative and unresolved event for 2.5 minutes, a well-tested rumination procedure51; and (3) engaging in an audio-recorded body awareness meditation for 2 minutes. Participants completed a 3-minute resting baseline between each of the tasks. The sad film task is a standard psychophysiological stress task designed to elicit a similar response from most participants. Rumination tasks are common in the psychophysiological literature and designed to elicit negative emotion in a more personal and variable way across participants. The body awareness task, created specifically for this study, was designed to elicit interoceptive awareness. The first 2 tasks were selected to elicit mild distress and emotion dysregulation, leading to phasic RSA decreases. The third task was designed to serve an emotion regulation function through mindful awareness of bodily sensations to prompt phasic RSA increases.
The same 3 tasks were used in data collection at baseline and 3-month follow-up. In this study, we examined change in response from baseline to the 3-month assessment, rather than individual participant’s responses to specific tasks. However, our prior research analyses indicate that these tasks functioned as hypothesized, with significant RSA decreases in response to the first 2 tasks and RSA increases during the third.52
Measures
Data were collected to assess interoceptive awareness and mindfulness skills, emotion regulation, psychological distress, and substance use outcomes. We also examined participant satisfaction and perceived benefits of the MABT and WHE interventions. Baseline measures were used to describe participant demographics, health history, and economic and legal status. To describe lifetime trauma exposure, we used the Traumatic Life Events Questionnaire (TLEQ).53
Primary outcomes: Interoceptive awareness and mindfulness skills
The Multidimensional Assessment of Interoceptive Awareness (MAIA), a 32-item scale on a 5-point scale, was used to assess interoceptive awareness.54 The MAIA has 8 distinct scales, all Likert-type scales that ask the frequency from “never” to “always” of practicing interoceptive skills. The scales are Noticing (awareness of body sensations), Not Distracting (tendency to not ignore or distract from sensations of discomfort), Not Worrying (tendency to not worry with sensations of discomfort), Attention Regulation (ability to sustain attention to body sensations), Emotional Awareness (aware of connection between physical and emotional states), Self-regulation (ability to regulate distress by attention to body sensations), Body Listening (active listening to body for insight), and Trusting (experience one’s body as safe and trustworthy). The internal consistency of MAIA scales ranged from .44 to .93 (total sale α = .95). The Freiburg Mindfulness Inventory (FMI) measures the practice of mindfulness on a 4-point Likert scale.55 Validated in a number of prior studies,56,57 Cronbach’s alpha for the FMI was .91.
Secondary outcomes
Emotion regulation.
Emotion regulation was examined using both self-report and psychophysiological measures. The self-report measure used was the Difficulties in Emotion Regulation Scale (DERS),58 a 36-item measure with total scores ranging from 36 to 180. Higher scores correspond to more difficulties in emotion regulation. Six subscales assess nonacceptance, goal-directed behavior, impulse control, awareness, regulation strategies, and emotional clarity.
To assess emotion regulation physiologically, we used measures of Respiratory Sinus Arrhythmia (RSA). A peripheral measure of parasympathetic-mediated cardiac output, RSA is measured via beat-to-beat fluctuations in heart rate across the respiratory cycle.59,60 Higher levels of RSA are protective, facilitating conservation of resources by allowing individuals to respond flexibly to environmental stressors. Lower RSA has been associated with poor emotion regulation across several clinical populations.61–63
To measure tonic (resting) RSA, the resting period at baseline RSA was scored in ten 30-second epochs (allowing maximum flexibility in analyses), then averaged across baseline epochs to produce a mean resting-state RSA value for each participant. Measures of phasic (task-based) RSA were collected during the 3 challenging tasks in 30-second epochs and averaged within each task.
RSA was collected with Biopac Acqknowledge software (Biopac Systems, Inc., Galeta, CA, USA) and scored using the MindWare HRV 3.0.10 software suite (Mindware Technologies Ltd., Gahanna, OH, USA). RSA is derived from the R-R time series, which is extracted from the electrocardiogram (ECG) waveform. MindWare computes RSA values by calculating spectral power in the high frequency range (>.15 Hz) using fast Fourier transformations.64 Consistent with standard RSA scoring processes, all data were normalized via log transformations within the MindWare algorithm. Cases with outlier data in any epoch or extreme values (<2 or >10 log[beats/min2/Hertz]) were reviewed by a co-investigator (S.E.C.). Movement artifacts resulted in unusable baseline ECG data for 5 participants.
Psychological distress.
Reliable and validated scales of psychological distress based on DSM-IV diagnostic criteria65 were used. To assess depression we used the Beck Depression Inventory-II (BDI-II), a 21-item questionnaire that measures severity of depressive symptoms.66 Scores range from 0 – 63; scores above 29 depict severe depression. BDI α was .92. To assess trauma-related symptoms, we used the PTSD Symptom Scale—Self Report (PSS-SR),67 a 17-item questionnaire that measures symptom frequency based on DSM-IV-TR (Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision) criteria.65 A score above 14 was used as the screening indicator of PTSD.68 Internal consistency reliability (Cronbach’s α) was .93.
Substance use and craving.
The Timeline FollowBack (TLFB) interview69 was used to assess all substance use (alcohol, illicit drugs, and nonprescribed medications). At baseline, participants were asked to report on substance use for 90 days prior to the last day of use and to identify the primary substance for which they were seeking treatment. For the post-intervention assessment, participants were asked to report on substance use since the previous assessment (approximately 90 days). Proportion of days used was calculated as the outcome variable. We also collected biological data (i.e., urine toxicology screens administered at assessments) and clinic electronic health records data to assess relapse. An exploratory measure of relapse (0 = no relapse, 1 = relapse) was calculated based on evidence of relapse across combined data from the TLFB, toxicology screen results, and electronic health records data. Substance use craving was measured using the 5-item Penn Alcohol Craving Scale (PACS)70 (α = .93), modified to address both alcohol and other drugs.
Intervention satisfaction.
Participant satisfaction with the MABT and WHE interventions were measured using a revised version of the Project Match participant satisfaction questionnaire71 and a written questionnaire that asked about intervention experience. The participant satisfaction questionnaire was composed of Likert-type response options specific to satisfaction with the intervention experience, including overall satisfaction with the therapist (MABT) or educator (WHE). The written questionnaire asked participants to describe what was most important about the intervention experience, what was learned, and if they perceived the intervention to have a positive influence on SUD treatment. These questionnaires were administered only to participants in MABT or WHE.
Data analyses
Preliminary analyses were used to examine the distributional properties of study measures, provide a detailed sample description by study group, and test for baseline equivalence among study groups. With one exception, no baseline differences were observed among study groups for the self-report measures or for RSA measures. There were, however, significant group differences in the baseline mean proportion of days abstinent (χ2 = 9.0, P = . 01), in the baseline mean proportion of days abstinent in past 90 days for MABT (mean = .78, SD = .26), WHE (mean = .74, SD = .28), and TAU (mean = .86, SD = .21). Thus, the analysis of proportion of Day abstinent, described below, were adjusted for baseline differences. We also examined pre-post outcomes including site in the mixed-level regression models; site did not alter the overall group intervention findings nor their interpretation. We did not adjust for therapist effects; our examination of MABT primary and secondary outcomes revealed no differences by therapist for the total scale scores. One RSA measure suggested possible therapist effect, but this uncommon finding was difficult to interpret, as the therapist’s workload was small (n = 8). A follow-up analysis of therapists whose workload included 20 or more participants revealed no significant therapist effects. In addition, ratings of participant satisfaction with the MABT therapist and intervention were consistently high and did not differ significantly by therapist.
Comparison of study group differences for continuous outcome variables, including RSA, were conducted using multilevel mixed-effects linear regression (Stata 15.1, Mixed procedure), which requires that the data be in long format. The analytic approach used in these analyses was based on unstructured residual covariance. Multilevel mixed-effects linear regression allows for unequal observations within subject and does not require the assumption of compound symmetry/exchangeable covariance structure. The approach can account for correlations that exist within subject in repeated measures across time. For the substance use outcome of proportion of days abstinent, the same analysis approach was used, but with multilevel mixed-effects tobit regression because the data were represented as proportions. Baseline values for the proportion of days abstinent were included as a covariate in the analyses to adjust for baseline group differences.
Study group assignment was incorporated as a fixed effect in all analyses. For analysis of RSA reactivity, we used the standard approach controlling for task baseline values32, and BMI and age. In other words, resting-state RSA, measured prior to each task, was statistically controlled in the analyses of RSA reactivity. For these tonic (resting) RSA analyses, we used mean resting-state RSA assessed at baseline and at 3 months, respectively, for preand post-intervention measures. For phasic (task-related) RSA analyses, we used the mean task score controlling for the physiological baseline prior to each task.
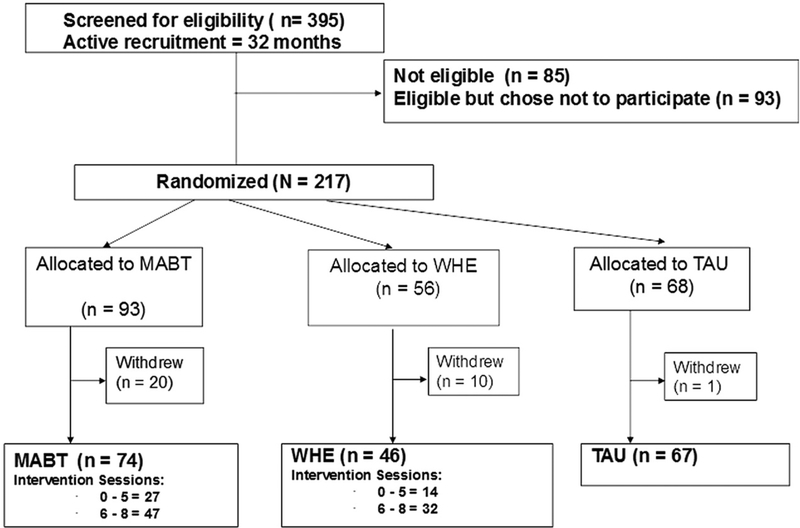
As detailed below, the pre-post outcomes were analyzed using the intent-to-treat (ITT) sample as well as the intervention-dose (ID) sample (see consort diagram, Figure 1). The intent-to-treat sample included all subjects for whom data were available pre- and/or post-intervention, whether they had engaged fully or partially in the MABT and WHE interventions. The intervention-dose sample, on the other hand, included study participants in MABT and WHE who had participated in 6 or more (≥75%) of the 8 intervention sessions and all participants in the TAU group. The Wald χ2 was used to test for group × time interaction effects to assess pre-post group differences for the primary and secondary outcomes. Statistical significance was set at P≤.05.
Figure 1.
Consort diagram.
Content analysis, with analytic tools focused on word use and phrasing from discourse analysis, was used to describe the qualitative responses on the written questionnaires. The initial step involved categorizing types of general response to the questions within MABT and WHE study groups, and the responses were then coded by theme for each question or set of participant responses following the strategy of Lincoln and Guba.72 To verify interpretation of meaning, word use and phrasing in response to questions were examined.
Results
Study enrollment, group assignment, and intervention attendance
Study recruitment was conducted over a course of 32 months to accommodate clinic routine as well as the demands of baseline data collection (Figure 1). Three hundred ninety-five women responded to study recruitment efforts and were screened for eligibility. Of these, 85 individuals did not meet the inclusion criteria primarily (62%) due to not being enrolled in IOP. Another 93 were initially screened as eligible but did not continue in the study enrollment process either because they did not have time to participate or because the invited individuals did not come to the initial enrollment appointment and were subsequently unreachable or if reachable, were no longer eligible for participation having completed IOP or dropped out of treatment. In all, 217 women were enrolled and randomly assigned to one of the 3 study groups. No one declined to continue in the study due to randomization assignment.
Approximately 20% of the enrolled participants assigned to MABT and WHE withdrew from study participation without attending MABT or WHE sessions. One TAU participant withdrew during the study period. For most of these individuals, we were unable to gather additional information regarding their withdrawal. For those who we were able to reach, reasons given for not participating were commonly related to scheduling concerns regarding transportation, employment (new job), or visitation with a child among those with child protective services (CPS) involvement. These findings are similar to prior MABT pilot study for women in SUD treatment in which relapse contributed to discontinuation of MABT sessions in 29% of sample.73 The final sample size was 187.
Participant baseline characteristics
Sample demographics and baseline health characteristics are summarized in Table 2 by study group. Most (75%) participants were Caucasian, 10% identified as mixed race, 8% as Hispanic, 5% as African American, and 4% as Native American. Participant ages ranged from 22 to 61 years; the median age was 35. Socioeconomic status was generally low; the majority (60%) had a high school education or less; 95% reported no monthly earnings; 86% received Medicaid or Medicare for health insurance; and 53% did not have permanent housing. The primary substances for which individuals had sought treatment included stimulants (45%), alcohol (39%), narcotics (24%), marijuana (8%), and other opiates or analgesics (6%); 22% reported using more than 1 primary drug. All participants were survivors of interpersonal trauma, typically characterized by multiple events and types. Correspondingly, 68% scored above the cutoff for PTSD. However, 50% of the study participants had received almost no prior mental health services. Most participants (68%) were mothers of children under 18 years; 56% had had court involvement related to their SUD treatment, most commonly linked to Child Protective Services.
Table 2.
Demographic and baseline characteristics.
| Category | MABT (n = 74) | WHE (n = 46) | TAU (n = 67) | Total (N = 187) |
|---|---|---|---|---|
| Age (median, range) | 35 (22–61) | 36 (20–59) | 35 (22–57) | 35 (20–61) |
| Race | ||||
| White | 56 (76) | 37 (80) | 47 (70) | 140 (75) |
| Mixed race | 7 (9) | 4 (9) | 8 (12) | 19 (10) |
| African American | 5 (7) | 0 | 4 (6) | 9 (5) |
| Other (filled in ethnicity) | 2 (3) | 1 (2) | 6 (9) | 9 (5) |
| Native American | 3 (4) | 3 (7) | 2 (3) | 8 (4) |
| Asian | 1 (1) | 1 (2) | 0 | 2 (1) |
| Ethnicity: Hispanic | 5 (7) | 2 (4) | 8 (12) | 15 (8) |
| Highest education level | ||||
| 11th grade or less | 16 (22) | 7 (15) | 12 (18) | 35 (19) |
| High school or GED | 28 (38) | 27 (59) | 22 (33) | 77 (41) |
| Two–year college/technical school | 24 (32) | 10 (22) | 24 (36) | 58 (31) |
| College degree (e.g., BA, BS) | 4 (5) | 2 (4) | 7 (10) | 13 (7) |
| Monthly income | ||||
| No monthly income | 42 (57) | 25 (54) | 28 (42) | 95 (51) |
| Less than $200 | 4 (5) | 7 (15) | 7 (10) | 18 (10) |
| Between $200 and $1000 | 18 (24) | 11 (24) | 22 (33) | 51 (27) |
| $1000 or more | 9 (12) | 3 (7) | 9 (13) | 21 (11) |
| Children under 18 years of age | 42 (57) | 31 (67) | 51 (76) | 124 (68) |
| Marital status | ||||
| Married | 3 (4) | 2 (4) | 6 (9) | 11 (6) |
| Single | 44 (59) | 18 (39) | 31 (46) | 93 (50) |
| Domestic partnership | 2 (3) | 5 (11) | 7 (10) | 14 (7) |
| Divorced | 15 (20) | 11 (24) | 15 (22) | 41 (22) |
| Separated | 7 (9) | 6 (13) | 6 (9) | 19 (10) |
| Other | 2 (3) | 4 (9) | 2 (8) | 8 (4) |
| Currently employed | 14 (19) | 4 (9) | 8 (12) | 26 (14) |
| Permanent housing | 39 (53) | 23 (50) | 37 (55) | 99 (53) |
| Health insurance | ||||
| Medicaid | 56 (56) | 32 (70) | 41 (61) | 129 (69) |
| Medicare | 9 (12) | 6 (13) | 16 (24) | 31 (17) |
| Private | 6 (8) | 4 (9) | 5 (7) | 15 (8) |
| None | 2 (3) | 2 (4) | 2 (3) | 6 (3) |
| Court involvement | 37 (50) | 27 (59) | 41 (61) | 105 (56) |
| Interpersonal trauma history | ||||
| Any reported traumatic event | 74(100) | 46(100) | 67(100) | 187(100) |
| Childhood sexual abuse | 42 (57) | 21 (46) | 27 (40) | 90 (48) |
| Childhood physical abuse | 29 (39) | 13 (18) | 28 (42) | 70 (37) |
| Adult physical assault (stranger) | 28 (38) | 18 (39) | 27 (40) | 73 (39) |
| Adult intimate partner violence | 62 (84) | 40 (87) | 52 (78) | 154 (82) |
| Adult sexual assault | 29 (39) | 23 (50) | 20 (30) | 72 (39) |
| Adult stalking | 44 (59) | 28 (61) | 33 (49) | 105 (56) |
| Lifetime mental health services | ||||
| None or <10 therapy sessions | 37 (50) | 24 (52) | 32 (48) | 93 (50) |
| 10–30 therapy sessions | 11 (15) | 12 (26) | 16 (24) | 39 (21) |
| >30 therapy sessions | 26 (35) | 10 (22) | 18 (27) | 54 (29) |
| Chronic health conditions | 32 (43) | 22 (48) | 22 (33) | 76 (41) |
Note. Values are number (percentage) unless otherwise indicated. All group comparisons P > .05 at baseline.
Primary outcomes
Primary and secondary study outcomes are described below and detailed in Tables 3 and 4. As described, the analyses were conducted using both an intent-to-treat (ITT) approach (Table 3) and an intervention-dose (ID) approach (Table 4). With a few exceptions, the patterns of findings based on these 2 analytic approaches were comparable. Consequently, the results described below are based on the ITT approach (Table 3), with differences in findings by the ID analysis (Table 4) noted in the text.
Table 3.
Means (SD) and group × time treatment effects for primary and secondary outcomes using the intent-to-treat sample.
| Construct (Scale) | MABT (n = 74) | WHE (n = 46) | TAU (n = 67) | Treatment × time interaction Wald χ2 | P value | |||
|---|---|---|---|---|---|---|---|---|
| Baseline | 3 Months | Baseline | 3 Months | Baseline | 3 Months | |||
| Mindfulness and interoception | ||||||||
| Mindfulness skills (FMI) | 35.2 (9.3) | 38.2 (8.9) | 37.0 (8.2) | 37.1 (10.9) | 35.6 (9.9) | 36.1 (10.3) | 3.41 | .18 |
| Interoceptive awareness (MAIA) | ||||||||
| Noticing | 3.0 (1.3) | 3.8 (1.2) | 3.1 (1.3) | 3.0 (1.3) | 2.9 (1.3) | 2.9 (1.2) | 13.51 | .002a,b |
| Not Distracting | 2.3 (1.2) | 2.4 (1.0) | 1.9 (1.2) | 2.4 (1.1) | 2.4 (1.0) | 2.5 (1.0) | 3.99 | .14 |
| Not Worrying | 2.6 (1.0) | 2.9 (1.0) | 2.7 (1.0) | 2.7 (1.0) | 2.8 (1.1) | 2.9 (1.0) | 3.32 | .19 |
| Attention Regulation | 2.1 (1.2) | 2.9 (1.2) | 2.3 (1.2) | 2.2 (1.1) | 2.1 (1.2) | 2.3 (1.3) | 16.67 | < .001a,b |
| Emotional Awareness | 3.1 (1.3) | 3.9 (1.1) | 3.4 (1.3) | 3.3 (1.3) | 3.0 (1.3) | 3.1 (1.3) | 12.46 | .002a,b |
| Self-regulation | 2.1 (1.2) | 3.2 (1.3) | 2.3 (1.4) | 2.6 (1.3) | 2.3(1.3) | 2.4 (1.4) | 14.75 | < .001a,b |
| Body Listening | 1.6 (1.3) | 2.7 (1.5) | 1.7 (1.5) | 1.8 (1.2) | 1.7 (1.4) | 1.9 (1.3) | 17.99 | < .001a,b |
| Trusting | 2.6 (1.5) | 3.5 (1.4) | 2.6 (1.6) | 3.1 (1.5) | 3.0 (1.5) | 2.9 (1.5) | 13.18 | .001a |
| Emotion and psychophysiological regulation | ||||||||
| Emotion dysregulation (DERS) | ||||||||
| Total | 87.3 (25.1) | 77.4 (24.2) | 88.2 (27.0) | 85.7 (28.0) | 83.8 (27.3) | 83.6 (27.5) | 6.38 | .04a |
| Nonacceptance | 13.1 (5.8) | 11.5 (5.2) | 13.8 (6.9) | 13.5 (6.7) | 12.2 (6.0) | 13.0 (6.6) | 5.71 | .06a |
| Goals | 14.9 (4.9) | 13.4 (4.9) | 15.8 (5.2) | 14.9 (5.4) | 14.3 (5.0) | 14.7 (5.4) | 5.82 | .05a |
| Impulse | 13.2 (5.4) | 11.4 (4.6) | 13.8 (5.6) | 12.5 (4.8) | 13.0 (5.4) | 12.0 (4.5) | 1.20 | .55 |
| Awareness | 16.7 (5.9) | 14.5 (5.3) | 15.7 (5.2) | 15.4 (5.5) | 15.8 (5.6) | 15.6 (5.9) | 6.48 | .04a,b |
| Strategies | 17.3 (6.3) | 15.7 (6.7) | 17.3 (7.0) | 17.9 (7.7) | 17.1 (7.0) | 17.7 (8.4) | 4.56 | .10a |
| Clarity | 12.0 (4.0) | 10.9 (3.9) | 12.0 (4.6) | 11.6 (4.2) | 11.3 (4.2) | 10.6 (3.7) | 0.95 | .62 |
| Respiratory sinus arrhythmia | ||||||||
| Tonic (resting) RSA | 5.6 (1.7) | 5.7 (1.4) | 5.7 (1.5) | 5.3 (1.4) | 5.6 (1.3) | 5.5 (1.4) | 5.73 | .06b |
| Film reactivitye | 5.5 (1.7) | 5.5 (1.6) | 5.6 (1.5) | 5.2 (1.6) | 5.4 (1.3) | 5.3 (1.5) | 13.81 | <.001a,b |
| Rumination reactivitye | 5.5 (1.7) | 5.7 (1.7) | 5.5 (1.6) | 5.1 (1.6) | 5.3 (1.4) | 5.3 (1.5) | 5.58 | .08b |
| Body awareness reactivitye | 6.2 (1.7) | 6.4 (1.6) | 6.4 (1.6) | 5.8 (1.9) | 6.2 (1.3) | 5.8 (1.6) | 13.51 | <.001a,b |
| Psychological distress | ||||||||
| Trauma (PSS-SR) | 20.0 (11.9) | 12.5 (11.2) | 20.0 (12.9) | 17.7 (13.1) | 18.5 (12.4) | 13.9 (11.8) | 3.90 | .14 |
| Depression (BDI-II) | 15.4 (10.5) | 12.1 (10.0) | 15.9 (10.8) | 14.8 (11.8) | 15.3 (10.5) | 13.9 (11.4) | 2.47 | .29 |
| Substance use and craving | ||||||||
| Proportion days abstinent | .78 (.26) | .92 (.22) | .74 (.28) | .92 (.18) | .86 (.21) | .91 (.20) | 8.62 | .01a,d |
| Craving (PENN Revised) | 13.6 (7.5) | 10.7 (7.9) | 13.3 (9.4) | 9.9 (8.6) | 10.7 (7.5) | 9.3 (8.1) | 3.24 | .20 |
Note. MABT=Mindful Awareness in Body-oriented Therapy; WHE=women’s health education; TAU=treatment as usual; PSS-SR=PTSD Symptom Scale—Self Report; EDE-Q=Eating Disorder Examination Questionnaire; BDI-II=Beck Depression Inventory-II; MDI=Multidimensional Dissociation Inventory; PHQ=Patient Health Questionnaire; PENN Revised=Penn Alcohol Craving Scale Revised; MQ Revised=Drinking Motives Questionnaire Revised; HRBS=HIV Risk Behavior Scale; DERS=Difficulties in Emotion Regulation Scale; FMI=Freiburg Mindfulness Inventory; MAIA=Multidimensional Assessment of Interceptive Awareness; scale of Body Connection. χ2 from Wald test with 2 d.f.
MABT improvement > TAU, P < .05.
MABT improvement > WHE, P < .05.
WHE improvement > MABT, P < .05.
WHE improvement > TAU, P < .05.
Predicted means (SE) from model with baseline value of measure, age and BMI as covariates.
Table 4.
Means (SD) and group by time treatment effects on primary and secondary outcomes using the intervention-dose sample.
| Construct (Scale) | MABT (n = 47) | WHE (n = 32) | TAU (n = 67) | Treatment × time interaction Wald χ2 | P value | |||
|---|---|---|---|---|---|---|---|---|
| Baseline | 3 Months | Baseline | 3 Months | Baseline | 3 Months | |||
| Primary outcomes | ||||||||
| Mindfulness skills (FMI) | 34.8 (9.5) | 39.8 (8.1) | 37.8 (8.9) | 35.5 (10.7) | 35.6 (9.9) | 36.1 (10.3) | 12.90 | .002a,b |
| Interoceptive awareness (MAIA) | ||||||||
| Noticing | 3.4 (1.3) | 4.1 (0.9) | 3.1 (1.3) | 2.8 (1.2) | 2.9 (1.3) | 2.9 (1.2) | 16.43 | <.001a,b |
| Not Distracting | 2.2 (1.3) | 2.4 (1.1) | 1.9 (1.2) | 2.4 (1.2) | 2.4 (1.0) | 2.5 (1.0) | 3.30 | .19 |
| Not Worrying | 2.6 (1.0) | 3.0 (1.1) | 2.6 (1.0) | 2.6 (1.1) | 2.8 (1.1) | 2.9 (1.0) | 6.55 | .04a,b |
| Attention Regulation | 2.3 (1.3) | 3.3 (1.1) | 2.5 (1.2) | 2.1 (1.2) | 2.1 (1.2) | 2.3 (1.3) | 29.84 | < .001a,b |
| Emotional Awareness | 3.3 (1.3) | 4.2 (0.9) | 3.5 (1.3) | 3.4 (1.3) | 3.0 (1.3) | 3.1 (1.3) | 13.26 | .002a,b |
| Self-regulation | 2.3 (1.2) | 3.6 (1.1) | 2.6 (1.4) | 2.5 (1.3) | 2.3(1.3) | 2.4 (1.4) | 26.51 | < .001a,b |
| Body Listening | 1.8 (1.4) | 3.1 (1.2) | 1.9 (1.5) | 1.8 (1.3) | 1.7 (1.4) | 1.9 (1.3) | 25.74 | < .001a,b |
| Trusting | 2.8 (1.6) | 3.8 (1.2) | 2.8 (1.6) | 3.0 (1.5) | 3.0 (1.5) | 2.9 (1.5) | 15.84 | .001a,b |
| Emotion and psychophysiological regulation | ||||||||
| Emotion dysregulation (DERS) | ||||||||
| Total | 88.1 (28.2) | 74.1 (23.8) | 90.7 (30.0) | 89.9 (27.6) | 83.8 (27.3) | 83.6 (27.5) | 11.70 | .01a,b |
| Nonacceptance | 13.6 (6.2) | 11.1 (4.9) | 14.9 (7.4) | 14.3(6.8) | 12.2 (6.0) | 13.0 (6.6) | 9.66 | .01a |
| Goals | 15.1 (5.1) | 13.0 (4.7) | 16.1 (5.6) | 15.5 (5.2) | 14.3 (5.0) | 14.7 (5.4) | 8.24 | .02a |
| Impulse | 13.5 (6.0) | 10.9 (4.8) | 14.3 (6.0) | 13.1 (4.8) | 13.0 (5.4) | 12.0 (4.5) | 3.10 | .21 |
| Awareness | 16.7 (6.3) | 13.5 (5.1) | 15.3 (5.5) | 16.0 (5.6) | 15.8 (5.6) | 15.6 (5.9) | 15.59 | <.001a,b |
| Strategies | 17.4 (7.1) | 14.9 (6.4) | 18.3 (7.5) | 18.9 (7.7) | 17.1 (7.0) | 17.7 (8.4) | 7.83 | .02a,b |
| Clarity | 11.7 (4.0) | 10.7 (3.8) | 12.3 (4.9) | 12.1 (4.2) | 11.3 (4.2) | 10.6 (3.7) | 0.99 | .61 |
| Respiratory sinus arrhythmia (RSA) | ||||||||
| Tonic (resting) RSA | 5.4 (1.9) | 5.7 (1.5) | 5.5 (1.6) | 5.4 (1.4) | 5.6 (1.3) | 5.5 (1.4) | 6.42 | <.04a |
| Film reactivitye | 5.3 (1.9) | 5.6 (1.6) | 5.4 (1.6) | 5.3 (1.6) | 5.4 (1.3) | 5.3 (1.5) | 8.08 | <.04a,b |
| Rumination reactivitye | 5.3 (1.9) | 5.7 (1.7) | 5.3 (1.8) | 5.3 (1.6) | 5.3 (1.4) | 5.3 (1.5) | 1.78 | .41 |
| Body awareness reactivitye | 5.9 (1.9) | 6.5 (1.6) | 6.2 (1.7) | 6.0 (1.8) | 6.2 (1.3) | 5.8 (1.6) | 18.66 | <.001a,b |
| Psychological distress | ||||||||
| Trauma (PSS–SR) | 20.6 (11.9) | 11.8 (11.0) | 20.8 (13.8) | 17.3 (13.2) | 18.5 (12.4) | 13.9 (11.8) | 3.99 | .14 |
| Depression (BDI–II) | 16.8 (11.1) | 11.2 (8.5) | 15.5 (11.8) | 15.3 (12.4) | 15.3 (10.5) | 13.9 (11.4) | 8.24 | .02a,b |
| Substance use and craving | ||||||||
| Proportion days abstinent | .78 (.27) | .94 (.19) | .69 (.26) | .95 (.10) | .86 (.21) | .91 (.20) | 14.72 | .0006a,d |
| Craving (PENN Revised) | 13.6 (8.0) | 9.4 (6.4) | 14.5 (9.2) | 11.1 (8.7) | 10.7 (7.5) | 9.3 (8.1) | 5.88 | .053a |
Note. MABT=Mindful Awareness in Body-oriented Therapy; WHE=women’s health education; TAU=treatment as usual; PSS-SR1/4PTSD Symptom Scale—Self Report; EDE-Q=Eating Disorder Examination Questionnaire; BDI-II=Beck Depression Inventory-II; MDI=Multidimensional Dissociation Inventory; PHQ=Patient Health Questionnaire; PENN Revised=Penn Alcohol Craving Scale Revised; MQ Revised=Drinking Motives Questionnaire Revised; HRBS=HIV Risk Behavior Scale; DERS=Difficulties in Emotion Regulation Scale. FMI=Freiburg Mindfulness Inventory; MAIA=Multidimensional Assessment of Interceptive Awareness; scale of Body Connection. χ2 from Wald test with 2 d.f.
MABT imrovment > TAU, P < .05.
MABT improvement > WHE, P < .05.
WHE improvement > MABT, P < .05.
WHE improvement > TAU, P < .05.
Predicted means and (standard errors) from model with baseline value of measure, age and BMI as covariates.
Mindfulness skills and interoceptive awareness
Although there were no statistically significant improvements in mindfulness skills based on the ITT analysis, results from the intervention-dose (ID) analysis (Table 4) showed statistically significant improvements (χ2 = 12.90, P = .002) for MABT compared with both WHE and TAU. MABT compared with the other study groups also showed significant improvements in interoceptive awareness for 6 of the 8 MAIA scales (Noticing: χ2 = 13.51, P = .002; Attention Regulation: χ2 = 16.67, P < .001; Emotional Awareness: χ2 = 12.46, P= .002; Self-regulation: χ2 = 14.75, P < .001; Body Listening: χ2 = 17.99, P < .001; and Trust: χ2 = 13.18, P = .001). There were no group differences for the MAIA Not Distracting and Not Worrying subscales in the ITT analysis. The MAIA intervention effect was, however, statistically significant for Not Worrying (χ2 = 6.55, P < .04) in the ID analysis.
Secondary outcomes
Emotion regulation
Overall, emotion regulation measured by the DERS revealed significant improvements for MABT compared with WHE and TAU (χ2 = 6.38, P = .04). Three of the 6 DERS subscales (Nonacceptance, Goals, and Awareness) improved for MABT compared with the other study groups; the Awareness subscale showed the greatest improvement (χ2 = 6.48, P = .04). In the ID analyses, in addition to a statistically significant total effect (χ2 = 11.70, P = .01), MABT showed significant improvements for the same 3 subscales (Nonacceptance: χ2 = 9.66, P = . 01; Goals: χ2 = 8.24, P = .02; and Awareness: χ2 = 15.59, P < .001) as well as for the Strategies (χ2 = 7.83, P = .02) subscale.
Respiratory sinus arrhythmia
We examined changes in RSA across resting-state measures and each of the 3 tasks. There were no baseline differences in RSA among the study groups. In general results from the ITT analyses, MABT showed a consistent pattern of increased RSA from pre to post on tonic (resting) measures, and in response to all 3 tasks. In contrast, the TAU and WHE study groups showed either no change or reduced RSA from pre to post (Table 3). MABT improved significantly on the film reactivity task (χ2 = 13.81, P < .001) compared with TAU and WHE study groups. RSA also improved significantly for MABT compared with TAU and WHE on the body awareness reactivity task (χ2 = 13.51, P < . 001). In the ID analysis, tonic (resting) RSA was also significantly improved for MABT compared to TAU (χ2 = 6.42, P = .04).
Trauma and depression symptoms
In terms of MABT intervention effects on improvement in psychological distress, no significant differences were observed among the 3 study groups based on the ITT analyses for either trauma-related symptoms or depression symptoms. On the other hand, the intervention-dose analysis revealed significant reductions in depression (χ2 = 5.24, P = .02)
Substance use and craving
Although substance use was generally low during the intervention period, participants in both MABT and WHE compared with TAU showed significantly greater improvement in the proportion of days abstinent in both the ITT (χ2 = 8.71, P = . 01) and the ID (χ2 = 14.20, P = . 0008) analyses. On the other hand, the relapse measure revealed no significant group differences in the proportion of participants who relapsed during the intervention period. However, the relapse pattern across the 3 groups was somewhat consistent with the proportion of days abstinent findings, in that relapse was lowest (30%) among MABT participants compared with WHE (47%) and TAU (43%). Significant improvements in substance craving by group was not observed in the ITT analysis (Table 3), but the ID analysis (Table 4) showed near significant improvement in craving for MABT compared with the other study groups (χ2 = 5.88, P = .053).
Intervention satisfaction
Participants responded to satisfaction questions with Likert-type response options in assessing their intervention experiences following completion of the intervention. Both MABT and WHE interventions were well received, with 94% of the participants in both groups indicating overall satisfaction. In response to the more specific question, “Overall, to what extent did the intervention meet your needs?” 72% of MABT and 63% of WHE participants endorsed highly positive ratings of “very much” or “extremely.” In addition, 25% of MABT and 20% of WHE participants endorsed moderate scale ratings of “somewhat” and “moderately.” The majority of MABT (83%) and WHE (77%) participants indicated interest in receiving the intervention again should they seek future treatment. There were no serious adverse events.
A primary theme that emerged from analysis of the written questionnaire responses was the importance of self-care. There were distinctly different themes within the intervention groups (WHE or MABT) related to what was learned in the intervention and how the intervention was important for their recovery. Women assigned to WHE learned health information (and appreciated topics new to them such as women’s cardiovascular health). They found learning about their health empowering and thus important for recovery; this experience prompted them to seek more health care services. Women assigned to MABT gained new physical and emotional awareness, as well as new or enhanced mind-body connection; these increases in awareness were recognized as critical for self-care. The ability to identify their emotional state was perceived to be critical for recovery, as it helped them to better cope with stressors and “triggers.” In addition, increased interoceptive awareness facilitated better physical symptom management, which was likewise identified as important for relapse prevention.
Discussion
The study pre-post findings demonstrate that interoceptive awareness, one of the primary outcomes, was significantly improved for participants in MABT when delivered as an adjunct to women’s SUD treatment. The significant changes for MABT compared with WHE and TAU on the majority of MAIA scales (P ≤ .002) indicates that the processes for learning interoceptive skills through MABT were highly effective for this population. This is notable given that this is a relatively brief intervention and that study participants tended to be highly distressed and had extensive interpersonal trauma histories. On the other hand, mindfulness skills showed improvement for MABT compared with WHE and TAU only in the intervention-dose but not ITT analysis. This observation is not surprising, as mindfulness skills are specifically taught and developed in the second half of the MABT intervention. Thus, many participants who did not complete the intervention but are included the ITT analysis were not actually exposed to this key aspect of MABT training.
Among the secondary health-related outcomes, participants in MABT compared with the other study groups showed significant improvement in both the self-report and physiological (RSA) measures of emotion regulation. For the self-report measure, the “awareness” aspect of emotion regulation improved most significantly, reflecting a primary focus of the MABT intervention. For RSA, each measure (resting and task reactivity) assessed a key aspect of regulatory capacity. For instance, resting-state RSA provides an index of overall regulatory capacity. Longitudinal research has demonstrated that resting RSA is highly stable over time and correlated with relatively enduring traits, such as positive emotionality.74,75 Thus, it is striking that MABT participants showed changes in resting-state RSA in response to an 8-week intervention. The film and rumination tasks were chosen to measure a capacity to regulate under the stress of negative emotional evocation, which is a significant risk factor for relapse. Thus, positive change in the MABT group on the film task compared with the other study groups provide further evidence of improved regulatory capacity under conditions of negative affect.
The response to the body awareness task resulted in an increase in RSA regardless of study group, an opposite pattern of physiological reactivity compared with the film and rumination tasks, indicating that participants experienced improved physiological regulation and reduced arousal during the body awareness task.52 Nonetheless, the results revealed highly significant RSA improvements among those in MABT compared with the other study groups. Given that this task requires skills that most closely mirror those learned in MABT, this finding strongly suggests that interoceptive awareness is a likely mechanism underlying improved regulatory capacity among those who received MABT.
Substance use, defined as the proportion days abstinent during the past 90 days, improved for both MABT and WHE compared with TAU. Notably, days abstinent from substance use was the only outcome that significantly improved for WHE compared with TAU, pointing to the potential positive effect of additional time and attention during early substance use disorder treatment.
The improvement in intervention group substance use results needs to be interpreted with caution. Observed baseline differences in substance use among the study groups suggest failure of the randomization process. Likewise, the overall substance use abstinence was relatively high during the 3-month study period, demonstrated by the mean proportion of days abstinent at 3 months across all study groups (Table 3). This high level of abstinence may be attributable to the fact that the majority of study participants had some form of court involvement (including CPS) and thus strong motivation to remain in compliance with the program abstinence requirements and to complete IOP. Craving for substances reduced significantly for MABT compared with TAU in the intervention-dose analysis. This finding is notable given that interoceptive dysfunction may be linked to craving.25,29 Although conceptualizations of craving vary,76 this result, along with the concomitant reductions in negative affect and improvements in emotion regulation capacity, suggests that interoceptive awareness training may reduce reactivity to drug cues and/or increase capacity to manage craving urges.
For psychological distress, all study groups showed some reductions in trauma-related symptoms and depression symptoms, although there were no significant between group differences in the ITT analysis. Participants in MABT showed the largest drop in trauma-related symptoms reflected in the proportion of women in MABT (44%) compared with WHE (29%) and TAU (39%) whose scores shifted from above to below the screening cutoff for PTSD.
Results from the intervention-dose analyses serve to underscore the importance of MABT based on intervention engagement. Among participants who received ≥75% of the MABT intervention, significant reductions were observed in depression symptoms for MABT compared with the other study groups and in craving compared with TAU. Depression symptoms are a primary indicator of reduced negative affect and a key factor associated with risk for relapse among individuals in SUD treatment.77 Thus, these findings point to the importance of interoceptive awareness training for longer-term treatment adherence and relapse prevention. In addition, the effect on reducing emotion regulation difficulties (self-reported) was stronger for MABT than for the other study groups, highlighting improved capacity to engage in emotion regulation strategies, a key MABT training focus. Thus, taken together, these results indicate the significance of receiving the full intervention, as MABT interoceptive and self-care skills are taught sequentially and incrementally over time.
Both the MABT and WHE interventions were highly acceptable to the study participants and had similar rates of attendance and completion. Likewise, both interventions were perceived to positively influence self-care, although in ways that reflected the distinct learning objectives of each intervention approach. The therapeutic elements of MABT, such as increased sensory (emotional and physical) awareness through interoception, mindfulness skills, and use of self-care strategies for emotion regulation practiced in daily life, appear to be key to improved outcomes. In contrast, each WHE session was a stand-alone information session, with no incremental skill-building components or personal growth orientation. Accordingly, the results showed that intervention dose was not a factor in WHE outcomes.
There are limitations to this study that need to be considered in interpreting the findings. This project was conducted with women only, so the findings may not generalize to men. Also, the SES of study participants was typically low and thus these findings may not generalize to women of higher SES, although a smaller MABT study with women across a more diverse education and economic spectrum showed similar results.13 The longer-term outcomes of MABT training were not examined in this study but will be forthcoming in future analyses of longitudinal data gathered at 6 and 12 months.
In conclusion, this study shows MABT training to be efficacious for immediate intervention improvements of interoceptive awareness, emotion regulation (self-report and psychophysiology), and substance use. In addition, the results also highlight the importance of MABT dose to reduce depression symptoms and substance use craving. Notably, this appears to be the first full-scale randomized controlled trial focused on interoceptive training as an adjunct to women’s SUD treatment. Interoception is thought to be critical for regulation, supporting healthy decisions and behavior change among individuals in SUD treatment. The significant improvements in interoceptive awareness and concomitant improvements in emotion regulation capacity are consistent with neurocognitive models that link interoception to emotion regulation for health outcomes important to SUD treatment. Current and evolving neurocognitive models highlight the importance of interoceptive awareness for the development of basic emotional awareness skills and the capacity for new emotion regulation appraisal and reappraisal processes that are critical for improved SUD treatment outcomes.32,78 Lastly, the overall findings are highly relevant to women’s recovery, providing evidence that interoceptive training improves health outcomes that are critical for supporting women’s SUD treatment. The high participant satisfaction, as well as clinical staff satisfaction as seen in our prior study of implementation feasibility,73 suggests that integrating MABT within the context of women’s SUD treatment is highly achievable. This population of highly distressed and traumatized women is very much in need of and likely to benefit from additional and targeted treatment options such as MABT.
Acknowledgments
The authors would like to gratefully acknowledge the women who participated in this study and the interventionists that worked with them: Elizabeth Chaison, Sarah Huntting, Lauren Oikle, Rebekah Ingalls, Christeine Terry, Anna Treadway, Lauren Oikle, and Carla Wiechman.
Funding
This study was funded by R01 DA033324 from the National Institute on Drug Abuse, National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funding organization had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
References
- [1].Lowman C, Allen J, Stout RL. Replication and extension of Marlatt’s taxonomy of relapse precipitants: overview of procedures and results. The Relapse Research Group. Addiction 1996;91:S51–S71. [PubMed] [Google Scholar]
- [2].Breese GR, Chu K, Dayas CV. Stress enhancement of craving during sobriety: a risk for relapse. Alcoholism, Clinical and Experimental Research. 2005;29(2):185–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Sinha R. The role of stress in addiction relapse. Curr Psychiatry Rep. 2007;9(5):388–395. [DOI] [PubMed] [Google Scholar]
- [4].McCabe SE, Cranford JA, Boyd CJ. Stressful events and other predictors of remission from drug dependence in the United States: longitudinal results from a national survey. J Subst Abuse Treat. 2016;71:41–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Fox HC, Axelrod SR, Paliwal P, Sleeper J, Sinha R. Difficulties in emotion regulation and impulse control during cocaine abstinence. Drug Alcohol Depend. 2007;89(2–3):298–301. [DOI] [PubMed] [Google Scholar]
- [6].Fox HC, Hong KA, Sinha R. Difficulties in emotion regulation and impulse control in recently abstinent alcoholics compared with social drinkers. Addict Behav. 2008;33(2):388–394. [DOI] [PubMed] [Google Scholar]
- [7].Moos RH. Theory-based active ingredients of effective treatments for substance use disorders. Drug Alcohol Depend. 2007;88(2–3):109–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Kopera M, Trucco EM, Jakubczyk A, et al. Interpersonal and intrapersonal emotional processes in individuals treated for alcohol use disorder and non-addicted healthy individuals. Addict Behav. 2018;79:8–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Gross JJ. (Ed.). Handbook of emotion regulation 2nd edn. Guildford Press; 2014:3–20. [Google Scholar]
- [10].Eftekhari A, Zoellner LA, Vigil SA. Patterns of emotion regulation and psychopathology. Anxiety Stress Coping. 2009;22(5):571–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Axelrod SR, Perepletchikova F, Holtzman K, Sinha R. Emotion regulation and substance use frequency in women with substance dependence and borderline personality disorder receiving dialectical behavior therapy. Am J Drug Alcohol Abuse. 2011;37(1):37–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Hoseiny H, Jadidi M, Habiballah Nataj L, Saberi-Zafarghandi MB. The effect of methadone-maintenance therapy with and without interactive treatment on improving emotion-regulation strategies and resilience among opiate-dependent clients. Int J High Risk Behav Addict. 2015;4(1):e23526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Price CJ, Wells EA, Donovan DM, Rue T. Mindful awareness in body-oriented therapy as an adjunct to women’s substance use disorder treatment: a pilot feasibility study. J Subst Abuse Treat. 2012;43(1):94–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Gross JJ, Munoz RF. Emotion regulation and mental-health. Clin Psychol-Sci Pr. 1995;2(2):151–164. [Google Scholar]
- [15].Vasilev CA, Crowell SE, Beauchaine TP, Mead HK, Gatzke-Kopp LM. Correspondence between physiological and self-report measures of emotion dysregulation: a longitudinal investigation of youth with and without psychopathology. J Child Psychol Psyc. 2009;50(11):1357–1364. [DOI] [PubMed] [Google Scholar]
- [16].Dvir Y, Ford JD, Hill M, Frazier JA. Childhood maltreatment, emotional dysregulation, and psychiatric comorbidities. Harv Rev Psychiatry. 2014;22(3):149–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Staiger PK, Melville F, Hides L, Kambouropoulos N, Lubman DI. Can emotion-focused coping help explain the link between posttraumatic stress disorder severity and triggers for substance use in young adults?. J Subst Abuse Treat. 2009;36(2):220–226. [DOI] [PubMed] [Google Scholar]
- [18].Bornovalova MA, Gratz KL, Daughters SB, et al. A multimodal assessment of the relationship between emotion dysregulation and borderline personality disorder among inner-city substance users in residential treatment. J Psychiatr Res. 2008;42(9):717–726. [DOI] [PubMed] [Google Scholar]
- [19].Bornovalova MA, Ouimette P, Crawford AV, Levy R. Testing gender effects on the mechanisms explaining the association between post-traumatic stress symptoms and substance use frequency. Addict Behav. 2009;34(8):685–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Greenfield SF, Brooks AJ, Gordon SM, et al. Substance abuse treatment entry, retention, and outcome in women: a review of the literature. Drug Alcohol Depend. 2007;86(1):1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Walitzer KS, Dearing RL. Gender differences in alcohol and substance use relapse. Clin Psychol Rev. 2006;26(2):128–148. [DOI] [PubMed] [Google Scholar]
- [22].Dube SR, Miller JW, Brown DW, et al. Adverse childhood experiences and the association with ever using alcohol and initiating alcohol use during adolescence. Adoles Health. 2006;38(4):444.e1–410. [DOI] [PubMed] [Google Scholar]
- [23].Strine TW, Dube SR, Edwards VJ, et al. Associations between adverse childhood experiences, psychological distress, and adult alcohol problems. AJHB. 2012;36(3):408–423. [DOI] [PubMed] [Google Scholar]
- [24].Weiss NH, Tull MT, Anestis MD, Gratz KL. The relative and unique contributions of emotion dysregulation and impulsivity to posttraumatic stress disorder among substance dependent inpatients. Drug Alcohol Depend. 2013;128(1–2):45–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Paulus MP, Stewart JL. Interoception and drug addiction. Neuropharmacology 2014;76 Pt B Pt B:342–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Sinha R, Li CS. Imaging stress- and cue-induced drug and alcohol craving: association with relapse and clinical implications. Drug Alcohol Rev. 2007;26(1):25–31. [DOI] [PubMed] [Google Scholar]
- [27].Cameron OG. Interoception: the inside story-a model for psychosomatic processes. Psychosom Med. 2001;63(5):697–710. [DOI] [PubMed] [Google Scholar]
- [28].McGlone F, Reilly D. The cutaneous sensory system. Neurosci Biobehav Rev. 2010;34(2):148–159. [DOI] [PubMed] [Google Scholar]
- [29].Gray MA, Critchley HD. Interoceptive basis to craving. Neuron 2007;54(2):183–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Naqvi NH, Bechara A. The insula and drug addiction: an interoceptive view of pleasure, urges, and decision-making. Brain Struct Funct. 2010;214(5–6):435–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Cisler JM, Elton A, Kennedy AP, et al. Altered functional connectivity of the insular cortex across prefrontal networks in cocaine addiction. Psychiatry Res. 2013;213(1):39–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Verdejo-Garcia A, Clark L, Dunn BD. The role of interoception in addiction: a critical review. Neurosci Biobehav Rev. 2012;36(8):1857–1869. [DOI] [PubMed] [Google Scholar]
- [33].Tang YY, Tang RX, Posner MI. Mindfulness meditation improves emotion regulation and reduces drug abuse. Drug Alcohol Depend. 2016;163:S13–S18. [DOI] [PubMed] [Google Scholar]
- [34].Witkiewitz K, Bowen S. Depression, craving, and substance use following a randomized trial of mindfulness-based relapse prevention. J Consult Clin Psychol. 2010;78(3):362–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Garland EL, Roberts-Lewis A, Tronnier CD, Graves R, Kelley K. Mindfulness-oriented recovery enhancement versus CBT for co-occurring substance dependence, traumatic stress, and psychiatric disorders: proximal outcomes from a pragmatic randomized trial. Behav Res Ther. 2016;77:7–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Bowen S, Chawla N, Collins SE, et al. Mindfulness-based relapse prevention for substance use disorders: a pilot efficacy trial. Subst Abuse. 2009;30(4):295–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Brewer JA, Mallik S, Babuscio TA, et al. Mindfulness training for smoking cessation: results from a randomized controlled trial. Drug Alcohol Depend. 2011;119(1–2):72–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Witkiewitz K, Lustyk MK, Bowen S. Retraining the addicted brain: a review of hypothesized neurobiological mechanisms of mindfulness-based relapse prevention. Psychol Addict Behav. 2013;27(2):351–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Garland EL. Restructuring reward processing with mindfulness-oriented recovery enhancement: novel therapeutic mechanisms to remediate hedonic dysregulation in addiction, stress, and pain. Ann N Y Acad Sci. 2016;1373(1):25–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Noel X, Brevers D, Bechara A. A neurocognitive approach to understanding the neurobiology of addiction. Curr Opin Neurobiol. 2013;23(4):632–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Price CJ, Hooven C. Interoceptive awareness skills for emotion regulation: theory and approach of mindful awareness in body-oriented therapy (MABT). Front Psychol. 2018;9:798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Price CJ, Herting JR. Changes in post traumatic stress symptoms among women in substance use disorder treatment: the mediating role of bodily dissociation and emotion regulation. Subst Abuse. 2013;7:SARTS12426–S153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Price C, Smith-DiJulio K. Interoceptive awareness is important for relapse prevention perceptions of women who received mindful body awareness. In substance use disorder treatment. J Addict Nurs. 2016;27(1):32–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Price CJ. Body-oriented therapy in recovery from child sexual abuse: an efficacy study. Alternative Therapies in Health and Medicine 2005;11(5):46–57. [PMC free article] [PubMed] [Google Scholar]
- [45].Price C. Body-oriented therapy in sexual abuse recovery: a pilot-test comparison. J Bodyw Mov Ther. 2006;10(1):58–64. [Google Scholar]
- [46].Price CJ, McBride B, Hyerle L, Kivlahan DR. Mindful awareness in body-oriented therapy for female veterans with post-traumatic stress disorder taking prescription analgesics for chronic pain: a feasibility study. Alternative Therapies in Health and Medicine 2007;13(6):32–40. [PMC free article] [PubMed] [Google Scholar]
- [47].Miller S, Pagan D, Tross S. Women’s health education. In peer activism for female partners of injection drug users. New York: Columbia University; 1998. [Google Scholar]
- [48].Hien DA, Wells EA, Jiang H, et al. Multisite randomized trial of behavioral interventions for women with co-occurring PTSD and substance use disorders. J Consult Clin Psychol. 2009;77(4):607–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Qu MH, Zhang YJ, Webster JG, Tompkins WJ. Motion artifact from spot and band electrodes during impedance cardiography. IEEE Trans Biomed Eng. 1986;33(11):1029–1036. [DOI] [PubMed] [Google Scholar]
- [50].Gross JJ, Levenson RW. Emotion elicitation using films. Cogn Emot. 1995;9(1):87–108. [Google Scholar]
- [51].Ottaviani C, Shapiro D, Davydov DM, Goldstein IB, Mills PJ. The autonomic phenotype of rumination. Int J Psychophysiol. 2009;72(3):267–275. [DOI] [PubMed] [Google Scholar]
- [52].Crowell SE, Price CJ, Puzia ME, Yaptangco M, Cheng SC. Emotion dysregulation and autonomic responses to film, rumination, and body awareness: extending psychophysiological research to a naturalistic clinical setting and a chemically dependent female sample. Psychophysiology 2017;54(5):713–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Kubany ES, Haynes SN, Leisen MB, et al. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: the traumatic life events questionnaire. Psychological Assessment. 2000;12(2):210–224. [DOI] [PubMed] [Google Scholar]
- [54].Mehling WE, Price C, Daubenmier JJ, Acree M, Bartmess E, Stewart A. The multidimensional assessment of interoceptive awareness (MAIA). PLoS One. 2012; 7(11):e48230. doi: 10.1371/journal.pone.0048230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Walach H, Buchheld N, Buttenmüller V, Kleinknecht N, Schmidt S. Measuring mindfulness—the Freiburg mindfulness inventory (FMI). Personality and Individual Differences. 2006;40(8):1543–1555. [Google Scholar]
- [56].Feicht T, Wittmann M, Jose G, Mock A, von Hirschhausen E, Esch T. Evaluation of a seven-week web-based happiness training to improve psychological well-being, reduce stress, and enhance mindfulness and flourishing: a randomized controlled occupational health study. Evidence-Based Complementary and Alternative Medicine. 2013;2013:1. doi: 10.1155/2013/676953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Sauer S, Walach H, Offenb€acher M, Lynch S, Kohls N. Measuring mindfulness: a Rasch analysis of the Freiburg mindfulness inventory. Religions 2011;2(4):693–706. [Google Scholar]
- [58].Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assessment. 2004;26(1):41–54. [Google Scholar]
- [59].Beauchaine T. Vagal tone, development, and Gray’s motivational theory: toward an integrated model of autonomic nervous system functioning in psychopathology. Develop Psychopathol. 2001;13(2):183–214. [DOI] [PubMed] [Google Scholar]
- [60].Porges SW. The polyvagal perspective. Biol Psychol. 2007;74(2):116–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Beauchaine TP, Gatzke-Kopp L, Mead HK. Polyvagal Theory and developmental psychopathology: emotion dysregulation and conduct problems from preschool to adolescence. Biol Psychol. 2007;74(2):174–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Crowell SE, Beauchaine TP, McCauley E, Smith CJ, Stevens AL, Sylvers P. Psychological, autonomic, and serotonergic correlates of parasuicide among adolescent girls. Develop Psychopathol. 2005;17(04):1105–1127. [DOI] [PubMed] [Google Scholar]
- [63].Thayer JF, Hansen AL, Saus-Rose E, Johnsen BH. Heart rate variability, prefrontal neural function, and cognitive performance: the neurovisceral integration perspective on self-regulation, adaptation, and health. Ann Behav Med. 2009;37(2):141–153. [DOI] [PubMed] [Google Scholar]
- [64].Hayano J, Sakakibara Y, Yamada A, et al. Accuracy of assessment of cardiac vagal tone by heart rate variability in normal subjects. Am J Cardiol. 1991;67(2):199–204. [DOI] [PubMed] [Google Scholar]
- [65].American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. 4th ed Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- [66].Beck AT, Steer RA, Brown GK. BDI-II, beck depression inventory: manual. 2nd ed San Antonio, Tex. Boston: Psychological Corp.; Harcourt Brace; 1996. [Google Scholar]
- [67].Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and Validity of a Brief Instrument for Assessing Posttraumatic-Stress-Disorder. J Traum Stress. 1993;6(4):459–473. [Google Scholar]
- [68].Coffey SF, Dansky BS, Falsetti SA, Saladin ME, Brady KT. Screening for PTSD in a substance abuse sample: psychometric properties of a modified version of the PTSD Symptom Scale Self-Report. J Traum Stress. 1998;11(2):393–399. [DOI] [PubMed] [Google Scholar]
- [69].Sobell L, Sobell M, Buchan G, Cleland P, Fedoroff I, Leo G. The reliability of the Timeline Followback method applied to drug, cigarette, and cannabis use. Paper presented at the The 30th Annual Meeting of the Association for Advancement of Behavior Therapy, New York; 1996. [Google Scholar]
- [70].Flannery B, Volpicelli J, Pettinati H. Psychometric properties of the Penn alcohol craving scale. Alcoholism Clin Exp Res. 1999;23(8):1289–1295. [PubMed] [Google Scholar]
- [71].Donovan DM, Kadden RM, DiClemente CC, Carroll KM. Client satisfaction with three therapies in the treatment of alcohol dependence: results from project MATCH. Am J Addict. 2002;11(4):291–307. [DOI] [PubMed] [Google Scholar]
- [72].Lincoln YS, Guba EG. Naturalistic Inquiry. Beverly Hills, CA: Sage; 1985. [Google Scholar]
- [73].Price CJ, Wells E, Donovan D, Brooks M. Implementation and acceptability of mindful awareness in body-oriented therapy in women’s substance use disorder treatment. J Altern Complement Med. 2012;18(5):454–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Oveis C, Gruber J, Haidt J, Cohen AB, Shiota MN, Keltner D. Resting respiratory sinus arrhythmia is associated with tonic positive emotionality. Emotion 2009;9(2):265–270. [DOI] [PubMed] [Google Scholar]
- [75].Yaptangco M, Crowell SE, Baucom BR, Bride DL, Hansen EJ. Examining the relation between respiratory sinus arrhythmia and depressive symptoms in emerging adults: a longitudinal study. Biol Psychol. 2015;110:34–41. [DOI] [PubMed] [Google Scholar]
- [76].Garland EL, Roberts-Lewis A, Kelley K, Tronnier C, Hanley A. Cognitive and affective mechanisms linking trait mindfulness to craving among individuals in addiction recovery. Subst Use Misuse. 2014;49(5):525–535. [DOI] [PubMed] [Google Scholar]
- [77].Abulseoud OA, Karpyak VM, Schneekloth T, et al. A retrospective study of gender differences in depressive symptoms and risk of relapse in patients with alcohol dependence. Am J Addict. 2013;22(5):437–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Garland EL, Farb NA, Goldin P, Fredrickson BL. Mindfulness broadens awareness and builds eudaimonic meaning: a process model of mindful positive emotion regulation. Psychol Inq. 2015;26(4):293–314. [DOI] [PMC free article] [PubMed] [Google Scholar]