Abstract
Background. Shift work is characterized by employees working outside the standard hours of 7:00 am to 6:00 pm. Because shift work includes night work, the normal sleep–wake cycle (circadian rhythm) is disrupted, with potential consequences for shift workers’ physical and mental health.
Objectives. To assess the pooled effects of shift work on mental health and to evaluate whether these differ in men and women.
Search Methods. We searched PubMed, Scopus, and Web of Science databases for peer-reviewed or government reports published up to August 2018
Selection Criteria. To be included, studies had to be longitudinal or case–control studies of shift work exposure associated with adverse mental health outcomes. For subanalyses, we grouped these outcomes as anxiety symptoms, depressive symptoms, or general poor mental health symptoms.
Data Collection and Analysis. We followed the Meta-Analysis of Observational Studies in Epidemiology Group guidelines. We extracted adjusted risk estimates for each study to calculate pooled effect sizes (ESs) using random effect models and metaregression analysis to explore sources of heterogeneity.
Main Results. We included 7 longitudinal studies, with 28 431 unique participants. Shift work was associated with increased overall risk of adverse mental health outcomes combined (ES = 1.28; 95% confidence interval [CI] = 1.02, 1.62; I2 = 70.6%) and specifically for depressive symptoms (ES = 1.33; 95% CI = 1.02, 1.74; I2 = 31.5%). Gender differences explained more than 90% of heterogeneity, with female shift workers more likely to experience depressive symptoms than female non–shift workers (odds ratio = 1.73; 95% CI = 1.39, 2.14).
Authors’ Conclusions. To our knowledge, this is the first meta-analysis to investigate the pooled effects of shift work on the risk of poor mental health, including subanalyses by type of poor mental health and gender. Shift workers, particularly women, are at increased risk for poor mental health, particularly depressive symptoms.
Public Health Implications. Depression accounts for 4.3% of the global burden of disease and incidence, with mental disorders worldwide predicted to cost US $16.3 million by 2030. With 1 in 5 people in the United States and Europe doing shift work, and the increased risk of poor mental health among shift workers, shift work industries are a priority context for reducing this burden. Workplace health promotion programs and policies are needed to minimize shift workers’ risk of poor mental health.
PLAIN-LANGUAGE SUMMARY
Many industries, such as transportation, health care, and hospitality, depend on employees working outside standard 7:00 am to 6:00 pm hours. Altering normal sleeping hours can affect shift workers’ physical and mental health. We analyzed data from 28 431 unique participants in studies that compared mental health outcomes in non–shift versus shift workers. Compared to non–shift workers, shift workers had a 30% higher risk of poor mental health and depression. Interestingly, women shift workers had a 70% higher risk of depression compared to women working day shifts. Poor mental health costs millions of dollars to health care systems and can affect people’s ability to work and have good quality of life. It is important to have programs and policies that can minimize shift workers’ risk of poor mental health.
Shift work is characterized by alternating and rotating morning, afternoon, and night shifts, with employees often working outside the standard hours of 7:00 am to 6:00 pm.1 About 20% of the working population in the United States, Australia, and Europe are engaged in this work pattern.2,3 Given service and production demands, industries in the transportation, hospitality, manufacturing, and health care sectors depend on shift work.3 Because shift work includes night work, the normal sleep–wake cycle (circadian rhythm) is disrupted, with potential consequences for shift workers’ physical and mental health.4,5
Altered sleep patterns owing to shift work have been associated with irritability, depressed mood, anxiety, and nervousness.6,7 Sleeping at odd times of the day together with shift schedules create challenges for maintaining healthy work–life balance in shift workers, as opportunities for family, social, and leisure activities are constrained.8,9 This may lead to social isolation and contribute to poor mental health in this occupational group.8 Mental disorders accounted for 14.4% of the total global burden of disease in 201710 and are estimated to cost the health system billions of dollars.11
Cross-sectional studies have suggested a positive association between shift work and poor mental health.12 In a large cohort study of Dutch employees, Driesen et al. reported that shift workers were twice as likely to report depressed mood as were those working day-only shifts (odds ratio [OR] = 2.05; 95% confidence interval [CI] = 1.52, 2.77).12 Similarly, Lee et al. found that Korean nurses who worked shifts had 1.5 times greater odds of experiencing higher severity of depressive symptoms than did non–shift workers (OR = 1.52; CI = 1.38, 1.67).13 Longitudinal studies have, however, provided conflicting results. Some studies have found increased risks of anxiety and depression in shift workers,14,15 whereas others found that shift workers had better psychological well-being and general mental health than did non–shift workers.16,17 The contradictory findings from these studies may be explained by differences in occupations, industry sectors, and the context of shift work in different countries.
Tolerance to shift work is defined as the ability to adapt to it without adverse health effects. This may explain individual differences in responses to shift work exposure,18 as well as gender differences. A recent systematic review of data from 60 studies of several occupations in 23 countries has shown that male shift workers had better sleep and less fatigue than did female shift workers.18 A prospective study of working conditions in the general Swedish population has shown that female shift workers had a higher risk of low psychological well-being than did male shift workers (risk ratio [RR] = 1.60; 95% CI = 1.00, 2.80).17 By contrast, Bara and Arber15 reported that male night workers in the United Kingdom had higher risks of poor mental health (OR = 2.58; 95% CI = 1.22, 5.48) and anxiety or depression (OR = 6.08; 95% CI = 2.06, 17.92) than did their female counterparts (OR = 1.06; 95% CI = 0.49, 2.27 and 1.69; 95% CI = 0.60, 4.76, respectively). Given these findings, the associations between shift work and the risk of poor mental health in men and women are unclear. Therefore, we assessed the pooled effects of shift work exposure on mental health and in specific outcomes and evaluated whether these differ in men and women.
METHODS
We followed the framework proposed by the Meta-Analysis of Observational Studies in Epidemiology group19 for design, research strategy, analysis, and reporting. We searched peer-reviewed publications in 3 major databases: PubMed, Scopus, and Web of Science. We performed all searches using title or abstract and keywords fields combining shift work and mental health terms, with publication up to August 2018. The search terms we used to identify studies with adverse mental health outcomes were based on a previous publication on optimal strategies to retrieve mental health content in MEDLINE20 and included truncated wildcard terms such as “depress*,” “anxi*,” “psychol*,” and “stress*” and other key words including “mental health,” “mental distress,” and “mental OR psychological well-being.” We used hierarchical MeSH (Medical Subject Headings) terms in the PubMed database to optimize inclusion of a range of adverse mental health outcomes (i.e., “mental health” [mh]; “emotions” [mh]; “mental disorders” [mh]). Shift work search terms were similar to those used in a previous systematic review on shift work and metabolic risk factors21: “shift work” OR “shiftwork” OR “irregular hours” OR “rotating shift” OR “rotating hours.” A complete list of all search term combinations used in each database is available on request. Reference lists of the included articles were also scanned for relevant studies and for systematic reviews on shift work and mental health.
Two authors (L. T. and T. L. K.-A.) scanned titles and abstracts independently to determine whether each article met the following inclusion criteria:
-
1.
was a prospective cohort or case–control study;
-
2.
included a measure of shift work defined as either night shift, irregular work, rotational work, or a combination of these;
-
3.
provided an estimate of risk of an adverse mental health outcome that was assessed via self-report using a validated scale score, reported as diagnosed by a professional as mental illness (e.g., anxiety, clinical depression), or both22;
-
4.
described shift work as the main exposure and had an independent referent group;
-
5.
was written in English; and
-
6.
was a peer-reviewed journal article or government report.
We excluded studies if shift work exposure was a secondary factor to insomnia, family or social conflict, or similar outcomes. For example, we excluded studies of job strain or relationships at work and similar exposures. We did not exclude any studies based on year of publication.
After selecting potentially eligible studies based on title or abstract, we performed a full-text scan. Disagreement on study inclusion arose for 2 studies, which analyzed data from the same cohort, but with different outcomes.7,23 These were resolved by consulting with a third reviewer to reach consensus, which was to include the study with the most recent analysis.7 After full-text review, 7 articles met all the selection criteria; their data were included in the meta-analysis.
Data Extraction
Two authors independently extracted data from each included study. This included information on author and year, study design, follow-up duration and years, sample size, participants’ age and gender, industry in which participants worked and cohort name (if ongoing cohort study), definition and assessment of shift work, duration of exposure to shift work (if reported), adverse mental health outcome, and variables used in the adjusted model for risk estimate. Risk estimates were extracted for both crude and adjusted models of OR, RR, or hazard ratio (HR). We included these in the analyses if they were measured using validated tools and were specific to the outcome reported (e.g., General Health Questionnaire used to identify poor mental health).
Risk of Bias Assessment
We used a tool from a previous meta-analysis on shift workers’ risk of poor physical health outcomes24 to assess the risk of bias in the included studies in our meta-analysis. Two authors (L. T. and T. L. K.-A.) independently assessed the following major domains of bias:
-
•
exposure definition,
-
•
exposure assessment,
-
•
reliability of assessments,
-
•
confounding, and
-
•
analysis methods (research-specific bias).
The tool also considered the following minor domains of bias:
-
•
blinding of assessors,
-
•
attrition,
-
•
selective reporting,
-
•
funding, and
-
•
conflict of interest.
We rated each criterion as high, low, or unclear risk of bias, as described in Appendix I. Based on these ratings, we classified studies as low (if all major domains and > 2 minor domains scored low risk), moderate (if 4 major domains and ≥ 2 minor domains scored low risk), or high risk (if < 4 major domains scored low risk) of bias.
Data Management and Statistical Analyses
We extracted ORs, RRs, and HRs from each study as a measure of risk estimates, including their respective SEs or 95% CIs. The reference group we used in all studies was non–shift workers, defined as those workers either not doing rotational shifts with night shift included or those who worked only day shifts (7:00 am–6:00 pm). For each study, we extracted those estimates with the highest level of adjustment for covariates. When studies calculated the risk estimates for men and women separately, we included 2 independent estimates in the meta-analysis. For studies with analyses of subgroups based on years of shift work, we included data from cumulative groups wherever possible. If a study included more than 1 type of work schedule (e.g., rotational shifts or permanent night shift), we extracted risk estimates for both groups. We created 4 groups of adverse mental health outcomes for the analyses. A combined group included all the outcomes (overall effect), and for the subanalyses we divided this into 3 mutually exclusive groups reflecting the type of outcome: depressive symptoms, anxiety symptoms, and general poor mental health symptoms.
We used risk estimates to calculate the pooled effect size (ES) using random effects models to assess the association between shift work and overall risk of adverse mental health outcomes combined (overall effect). We chose this approach because, unlike fixed-effect models, random effect models assume that the shift work effect might vary between studies as well as participants in each study.25 We first conducted an overall effect analysis, including all estimates in a nonexposure versus exposure meta-analysis, with shift work as the exposure group. We then conducted 2 subgroup analyses: (1) by type of adverse mental health outcomes (depressive symptoms, anxiety symptoms, general poor mental health symptoms), and (2) by gender to assess the risk of adverse mental health outcomes combined.
We used the I2 test to assess heterogeneity. To assess robustness of data and potential sources of heterogeneity, we conducted sensitivity analyses using univariate metaregression. Variables included in the sensitivity analyses were type of poor mental health outcome (depressive symptoms, anxiety symptoms, general poor mental health symptoms); gender; exposure definition (low or high risk of bias); industry or occupation (nursing, other); follow-up (≤ 1 year, > 1 year); risk of bias (moderate, high); average age of the cohort (≤ 35 vs > 35 years); sample size (< 1000, > 1000); and tool used to measure outcomes (General Health Questionnaire, other). We used funnel plots and the Egger test to evaluate publication bias. We conducted all analyses using Stata version 12.1 (StataCorp, College Station, TX).
RESULTS
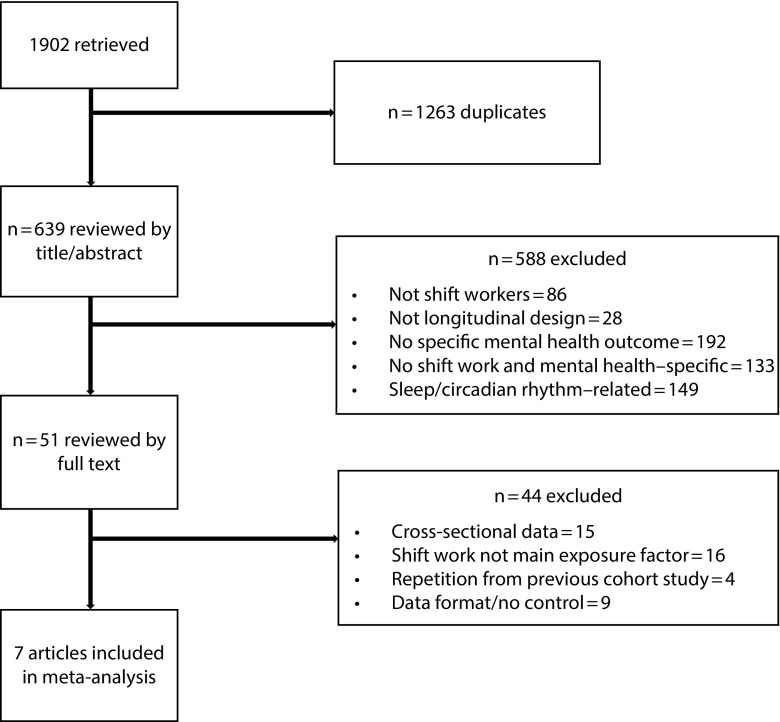
The results of the systematic review are shown in Figure 1. We retrieved 1902 articles and, after removing duplicates, reviewed 639 by title and abstract and 51 by full text. Of the eligible studies, we did not include 2 studies because of data format (continuous data),16,26 which resulted in 7 studies being included in the meta-analysis. These articles included 14 separate estimates of the association between shift work and adverse mental health outcomes.
FIGURE 1—
Flow Diagram of Literature Search and Selection of Studies: United States, 2018
Study Characteristics
Study characteristics are summarized in Table 1. All studies were prospective cohort studies, 3 had a follow-up of 1 year or less, and 4 had a follow-up of between 2 and 10 years. The latter studies had larger sample sizes than did those with 1 year or less follow-up (n = 37–1582 vs 420–9765, respectively).15,17,27,28 Most of the studies (n = 4) measured general poor mental health symptoms using the 12-question General Health Questionnaire.14,15,17,26 One study also used the Nottingham Life Quality Questionnaire, but to avoid duplication of estimates, we included only the general poor mental health symptoms estimate defined with the General Health Questionnaire.17 One study used the 28-item General Health Questionnaire and depression subscales to define cases of combined anxiety and depressive symptoms. The remaining studies used either the Hospital Anxiety and Depression scale to define cases of anxiety and depressive symptoms29 or a self-reported checklist from the Health and Work Productivity Questionnaire for cases of depressive symptoms.27 We excluded 1 risk estimate from the analysis because the authors measured symptoms of anxiety and depression together using a single self-reported question.13 The average age of participants in the studies was 39.7 years, with a range of 18 to 60 years.
TABLE 1—
Characteristics of the Studies Included in the Meta-Analysis of Effects of Shift Work Exposure on Mental Health and Male-Female Differences: United States, 2018
| Study | Design | Follow-Up | Type of Adverse Mental Health Outcome | Tool Used | Case Definition | Sample Size | Age, Yearsa | Gender | Occupational Group |
| Lin et al.14 | Cohort study | 1 y | General poor mental health symptoms | GHQ-12 | Score > 4 | 1360 | 29.9 (20–45) | Female | Nurses |
| Bara and Arber15 | Cohort study | 8 y | General poor mental health symptoms | GHQ-12 | Score > 4 | 9765 | 21–73 | Female and male | Not specified |
| Bildt and Michelsen17 | Cohort study | 4 y | General poor mental health symptoms | GHQ-12 | Score > 75th percentile | 420 | 46–63 | Female and male | Not specified |
| Driesen et al.27 | Cohort study | 10 y | Depressive symptoms | Self-report HPQ checklist | Current/past treatment of depressive disorder | 8178 | 40.1 (8.0) | Female and male | Not specified |
| De Raeve et al.28 | Cohort study | 2 y | General poor mental health symptoms | GHQ-12 | Score > 4 | 6828 | 41.72 (8.70) | Female and male | Not specified |
| Berthelsen et al.29 | Cohort study | 1 y | Anxiety and depressive symptoms | HADS-14 | Score > 8 in respective scales | 1582 | 30 (21–60) | Female and male | Nurses |
| Poole et al. 30 | Cohort study | 6 mo | Anxiety and depressive symptoms | GHQ-28 anxiety and depression scales | Score > 4 in respective scales | 298 | 35 (18–60) | Female and male | Factory employees |
Note. GHQ = General Health Questionnaire; HADS = Hospital Anxiety and Depression Scale; HPQ = Health and Work Performance Questionnaire.
Average age at baseline, or the highest mean when the study presented the population in stratified groups, with SD or range presented in parentheses.
Risk of Bias Assessment
The risk of bias was high in more than half the studies and moderate in the remaining studies (Table A, available as a supplement to the online version of this article at http://www.ajph.org). Exposure assessment (e.g., using self-report) and attrition (lost to follow-up > 20%) were the 2 domains with a high risk of bias in the majority of the studies. Three studies scored a high risk of bias for exposure definition. No studies reported on the blinding of assessors or researchers undertaking the studies. As this aspect is not relevant to the included studies’ design, we deemed the risk of bias unclear for this item.
Definition and Measure of Exposure to Shift Work
Six studies used self-report to measure shift work exposure, and 1 used company records.30 Studies defined shift work differently, with most using a work pattern consisting of rotations between morning, afternoon, and night shifts or between day and night shifts.14,27–30 Two studies considered working nights as shift work, but without a specific pattern definition (e.g., frequency of night shifts).15,17
Effect of Shift Work on Mental Health Outcomes
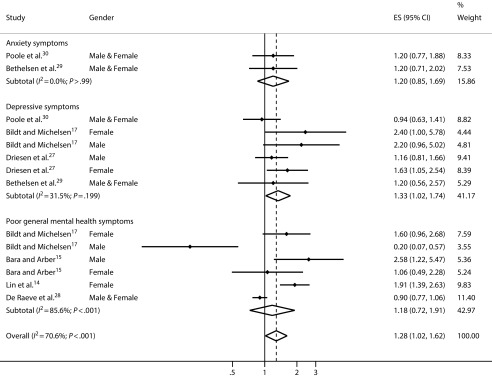
The results of the meta-analysis for the association between shift work and adverse mental health outcomes (combined and by type) are shown in Figure 2. The pooled ES shows shift workers had a higher risk of adverse mental health outcomes combined than those who did not do shift work (ES = 1.28; 95% CI = 1.02, 1.62). However, there was substantial heterogeneity among studies (I2 = 70.6%). In the subanalysis by type of adverse mental health outcome, shift work was associated with 33% higher risk of depressive symptoms (ES = 1.33; 95% CI = 1.02, 1.74). The risk of anxiety symptoms and general poor mental health symptoms was higher in shift workers than in non–shift workers; however, these associations were not statistically significant (ES = 1.20; 95% CI = 0.85, 1.69 and ES = 1.18; 95% CI = 0.72,1.91, respectively).
FIGURE 2—
Effect of Exposure to Shift Work by Adverse Mental Health Outcomes and Combined Outcomes (Overall Effect): United States, 2018
Note. ES = effect size.
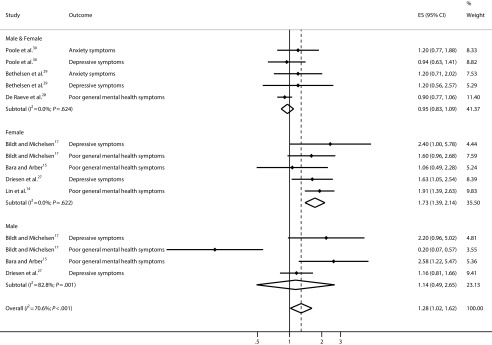
In the subgroup analysis in Figure 3, female shift workers were at higher risk for combined adverse mental health outcomes (ES = 1.78; 95% CI = 1.39, 2.14) than were female non–shift workers. However, this was not the case for male shift workers (ES = 1.14; 95% CI = 0.49, 2.65).
FIGURE 3—
Effect of Shift Work on Adverse Mental Health Outcomes (Overall Effect), by Gender: United States, 2018
Note. ES = effect size.
Sensitivity Analysis
Results of the sensitivity analysis are shown in Table B (available as a supplement to the online version of this article at http://www.ajph.org). The metaregression results show that gender and overall risk of bias could explain 90.00% and 0.61% of the heterogeneity of results. The rest of the factors measured resulted in a negative I2, which can be interpreted as zero.31 When the pooled effect size included estimates from women only, the effect of shift work was higher in female shift workers than in female non–shift workers (ES = 1.73; 95% CI = 1.39, 2.14). But this was not the case for male shift workers (ES = 1.25; 95% CI = 0.49, 2.65). The pooled effect sizes were significant for depressive symptoms, studies with low risk of bias in the exposure definition, studies of nurses, studies with large sample size (> 1000), and studies with moderate overall risk of bias.
DISCUSSION
To our knowledge, this is the first meta-analysis to investigate the pooled effects of shift work on the risk of poor mental health, including subanalyses by type of poor mental health and gender. The results show that shift work was associated with an increased overall risk of adverse mental health outcomes combined. Specifically, the risk of depressive symptoms was 33% higher in shift workers than in non–shift workers. Gender differences explained more than 90% of heterogeneity, with female shift workers more likely to experience depressive symptoms than female non–shift workers (OR = 1.73; 95% CI = 1.39, 2.14).
Our results are comparable with a previous meta-analysis that investigated depression risk in shift workers.32 Lee et al.32 reported a RR = 1.43 (95% CI = 1.24, 1.64), which is similar to our pooled estimate for depressive symptoms (ES = 1.33; 95% CI = 1.02, 1.74). Another review and meta-analysis of longitudinal studies found that most studies reported an increased risk of depression with night work, but the pooled effect size was not significant (ES = 1.42; 95% CI = 0.92, 2.19).33 Our study adds to previous literature by showing that shift workers’ risk is higher for adverse mental health outcomes combined, not just depression, and this risk might differ between men and women.
Although our study did not specifically assess positive mental health outcomes, our findings of an increased risk of symptoms related to depression and poor mental health outcomes seem to contrast with those of Nabe-Niesen et al.,16 who found that Danish shift workers had better mental health and vitality than did day workers. These differences might be because the study had a younger participant sample, the study had shorter follow-up and exposure to shift work, and the participants had more control over working times. Subgroup analysis in the other study showed that shift workers with low control of planning working hours scored the lowest on mental health (frequency of feeling nervous, blue, happy) and vitality scales (frequency of feeling energetic, worn out, tired).16
Although not assessed in our study, low job control has previously been demonstrated to have a negative effect on mental health.34,35 This suggests a mediating role for work-related factors in the shift work and mental health relationship. Two recent meta-analyses have reported that specific work-related factors such as job strain, low decision latitude, and low social support were associated with higher risk of poor mental health in the working population.36,37 These factors are common characteristics of shift work and could contribute to the risk of adverse mental health outcomes.38 Interestingly, one study showed that shift work was not associated with poor mental health after adjustment for psychosocial working conditions.27
Previous studies have shown that tolerance to different work stressors (e.g., job insecurity, life–work balance) differs by gender, with lower tolerance associated with higher incidence of major depressive disorders in women than in men.39 This might explain the higher pooled effect size observed for general poor mental health in women than in the overall effects in our subgroup analysis (ES = 1.73 vs 1.28). Our findings are comparable to other research reporting increased odds for depressive symptoms in female shift workers than in female non–shift workers (OR = 1.52; 95% CI = 1.38, 1.67).13 Cross-sectional analysis from a large Dutch cohort study also reported higher odds of depressed mood in female shift workers than in their day shift counterparts (OR = 5.96; 95% CI = 2.83, 12.56). This was higher than the odds reported for male shift compared with non–shift workers (OR = 2.05; 95% CI = 1.52, 2.77).12 Such findings suggest that female shift workers are at higher risk for adverse mental health outcomes than are male shift workers.
The higher risk of depression in female than male shift workers may be partly explained by the higher risk of depression among women than men in the general population.40 This increased vulnerability has been attributed to gender differences in physiological stress responses, biological load and hormones, interpersonal orientation, rumination and internalization of difficulties, and exposure to other adversity (e.g., relationship violence, discrimination).40 Future research on the effects of shift work on mental health outcomes could include measures of other relevant factors, such as alcohol abuse and aggression, that are more prevalent among men than women.
These results suggest that employers should consider strategies for reducing the mental health burden on shift workers, such as giving more control and flexibility over shift schedules, reducing job strain, and providing more social support at work. Workplace policies, programs, and practices could promote awareness of associated risks and protective factors and enable access to mental health services without stigmatization. Depression accounts for 4.3% of the global burden of disease and incidence,41 with mental disorders worldwide predicted to cost US $16.3 million by 2030.42 Untreated mental health conditions are costly to workplaces in terms of absenteeism, presenteeism, and compensation claims. With 1 in 5 people in the United States and Europe doing shift work,2,3 and the increased risk of poor mental health among shift workers, shift work industries are a priority context for reducing this burden.
Strengths and Limitations
The strengths of this study include our use of comprehensive search terms, with a combination of keywords that has previously been shown to be appropriate in maximizing retrieval of studies on shift work and poor mental health.20,43 We also used large databases, conducted by hand searches in reference lists of relevant articles, and contacted authors for data to optimize the data. The exclusion of 2 studies16,26 because of data format (continuous instead of categorical) remains a potential limitation; however, it is unlikely that this decision would have significantly changed our findings. One study26 had a very small sample size (n = 60) and reported similar findings to our study, whereas the other16 reported both negative and positive associations between shift work and mental health and vitality. The findings from these studies are similar to those reported in other included studies,17 and earlier in the discussion we explored possible reasons for the differences in associations.
We conducted sensitivity analyses on the effects of gender; however, we could not do this for other personality traits or job-related factors. This information was not available in the included studies. We conducted sensitivity analysis on participants’ occupation using a dichotomy of nursing versus other, but the lack of occupation information in most studies limited our ability to explore potential moderating effects of specific occupations. Given the large body of literature on these factors, these variables should be considered in future meta-analyses as mediators of overall pooled effect size. To enhance specificity, we grouped estimates into 3 types of adverse mental health outcomes (i.e., anxiety symptoms, depression symptoms, general poor mental health symptoms) and used a dichotomy of present versus not present.
We acknowledge that this could be perceived as a simplistic approach and that the measures used in the included studies were sometimes very basic (e.g., 1 question item to define clinical depression) and used cutoff scores to identify the presence or absence of adverse mental health outcomes. This approach would be insufficient for diagnostic purposes. We have, therefore, used language about “symptoms” rather than diagnoses and excluded estimates of anxiety and depression assessed with a single question.13 Future studies of the effects of shift work on adverse mental health outcomes could include subanalyses to assess the effects of gender differences in job-related factors.
Conclusions
Shift workers are at increased risk for poor mental health and, more specifically, symptoms related to depression; this is particularly true for female shift workers. Workplace health promotion programs and policies are needed to minimize shift workers’ risk of poor mental health.
ACKNOWLEDGMENTS
The authors would like to thank the following authors who kindly replied to our request for further data in an effort to include as many eligible studies as possible: I.J. Kant, Nicole W. H. Jansen, Amanda Cooklin, Ralph Mistlberger, Eirunn Thun, John Violanti, Sandra West, Margot Shields, and Marianna Virtanen.
CONFLICTS OF INTEREST
The authors declare no conflict of interests or financial conflicts.
HUMAN PARTICIPANT PROTECTION
No protocol approval was necessary because no human participants were involved in this study.
REFERENCES
- 1.Straif K, Baan R, Grosse Y et al. Carcinogenicity of shift-work, painting, and fire-fighting. Lancet Oncol. 2007;8(12):1065–1066. doi: 10.1016/S1470-2045(07)70373-X. [DOI] [PubMed] [Google Scholar]
- 2.Parent-Thirion A, Vermeylen G, Cabrita J . Sixth European Working Conditions Survey—Overview Report. Luxembourg City, Luxembourg: Publications Office of the European Union; 2016. [Google Scholar]
- 3.Alterman T, Luckhaupt S, Dahlhamer J, Ward B, Calvert G. Prevalence rates of work organization characteristics among workers in the US: data from the 2010 National Health Interview Survey. Am J Ind Med. 2013;56(6):647–659. doi: 10.1002/ajim.22108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wyse C, Celis Morales C, Graham N et al. Adverse metabolic and mental health outcomes associated with shiftwork in a population-based study of 277,168 workers in UK biobank. Ann Med. 2017;49(5):411–420. doi: 10.1080/07853890.2017.1292045. [DOI] [PubMed] [Google Scholar]
- 5.Torquati L, Mielke G, Brown W, Kolbe-Alexander T. Shift work and the risk of cardiovascular disease. A systematic review and meta-analysis including dose-response relationship. Scand J Work Environ Health. 2018;44(3):229–238. doi: 10.5271/sjweh.3700. [DOI] [PubMed] [Google Scholar]
- 6.Karatsoreos I. Effects of circadian disruption on mental and physical health. Curr Neurol Neurosci Rep. 2012;12(2):218–225. doi: 10.1007/s11910-012-0252-0. [DOI] [PubMed] [Google Scholar]
- 7.Berthelsen M, Pallesen S, Bjorvatn B, Knardahl S. Shift schedules, work factors, and mental health among onshore and offshore workers in the Norwegian petroleum industry. Ind Health. 2015;53(3):280–292. doi: 10.2486/indhealth.2014-0186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Drake CL, Wright KP., Jr . Shift work, shift-work disorder, and jet lag. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. 5th ed. St. Louis, MO: Saunders; 2011. pp. 784–798. [Google Scholar]
- 9.Cheung T, Yip P. Lifestyle and depression among Hong Kong Nurses. Int J Environ Res Public Health. 2016;13(1) doi: 10.3390/ijerph13010135. pii: E135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patel V, Saxena S, Lund C et al. The Lancet Commission on global mental health and sustainable development. Lancet. 2018;392(10157):1553–1598. doi: 10.1016/S0140-6736(18)31612-X. [DOI] [PubMed] [Google Scholar]
- 11.Australian Burden of Disease Study: Impact and Causes of Illness and Death in Australia 2011. Canberra, Australia: Australian Institute of Health and Welfare; 2016. [Google Scholar]
- 12.Driesen K, Jansen N, Kant I, Mohren D, van Amelsvoort L. Depressed mood in the working population: associations with work schedules and working hours. Chronobiol Int. 2010;27(5):1062–1079. doi: 10.3109/07420528.2010.489877. [DOI] [PubMed] [Google Scholar]
- 13.Lee H, Kim M, Kim O, Lee I, Kim H. Association between shift work and severity of depressive symptoms among female nurses: the Korea Nurses’ Health Study. J Nurs Manag. 2016;24(2):192–200. doi: 10.1111/jonm.12298. [DOI] [PubMed] [Google Scholar]
- 14.Lin P, Chen C, Pan S et al. Atypical work schedules are associated with poor sleep quality and mental health in Taiwan female nurses. Int Arch Occup Environ Health. 2012;85(8):877–884. doi: 10.1007/s00420-011-0730-8. [DOI] [PubMed] [Google Scholar]
- 15.Bara AC, Arber S. Working shifts and mental health—findings from the British Household Panel Survey (1995–2005) Scand J Work Environ Health. 2009;35(5):361–367. doi: 10.5271/sjweh.1344. [DOI] [PubMed] [Google Scholar]
- 16.Nabe-Nielsen K, Garde AH, Albertsen K, Diderichsen F. The moderating effect of work–time influence on the effect of shift work: a prospective cohort study. Int Arch Occup Environ Health. 2011;84(5):551–559. doi: 10.1007/s00420-010-0592-5. [DOI] [PubMed] [Google Scholar]
- 17.Bildt C, Michelsen H. Gender differences in the effects from working conditions on mental health: a 4-year follow-up. Int Arch Occup Environ Health. 2002;75(4):252–258. doi: 10.1007/s00420-001-0299-8. [DOI] [PubMed] [Google Scholar]
- 18.Saksvik IB, Bjorvatn B, Hetland H, Sandal GM, Pallesen S. Individual differences in tolerance to shift work—a systematic review. Sleep Med Rev. 2011;15(4):221–235. doi: 10.1016/j.smrv.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 19.Stroup DF, Berlin JA, Morton SC et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 20.Wilczynski NL, Haynes RB, Team H. Optimal search strategies for identifying mental health content in MEDLINE: an analytic survey. Ann Gen Psychiatry. 2006;5(1):4. doi: 10.1186/1744-859X-5-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Proper KI, van de Langenberg D, Rodenburg W et al. The relationship between shift work and metabolic risk factors: a systematic review of longitudinal studies. Am J Prev Med. 2016;50(5):e147–e157. doi: 10.1016/j.amepre.2015.11.013. [DOI] [PubMed] [Google Scholar]
- 22.American Psychiatric Association. What is mental illness? 2018. Available at: https://www.psychiatry.org/patients-families/what-is-mental-illness. Accessed August 5, 2018.
- 23.Thun E, Bjorvatn B, Torsheim T, Moen BE, Magerøy N, Pallesen S. Night work and symptoms of anxiety and depression among nurses: a longitudinal study. Work Stress. 2014;28(4):376–386. [Google Scholar]
- 24.Ijaz S, Verbeek J, Seidler A et al. Night-shift work and breast cancer—a systematic review and meta-analysis. Scand J Work Environ Health. 2013;39(5):431–447. doi: 10.5271/sjweh.3371. [DOI] [PubMed] [Google Scholar]
- 25.Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. BMJ. 2011;342:d549. doi: 10.1136/bmj.d549. [DOI] [PubMed] [Google Scholar]
- 26.Bohle P, Tilley AJ. The impact of night work on psychological well-being. Ergonomics. 1989;32(9):1089–1099. doi: 10.1080/00140138908966876. [DOI] [PubMed] [Google Scholar]
- 27.Driesen K, Jansen NWH, van Amelsvoort LGPM, Kant I. The mutual relationship between shift work and depressive complaints—a prospective cohort study. Scand J Work Environ Health. 2011;37(5):402–410. doi: 10.5271/sjweh.3158. [DOI] [PubMed] [Google Scholar]
- 28.De Raeve L, Kant I, Jansen NWH, Vasse RM, van den Brandt PA. Changes in mental health as a predictor of changes in working time arrangements and occupational mobility: results from a prospective cohort study. J Psychosom Res. 2009;66(2):137–145. doi: 10.1016/j.jpsychores.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 29.Berthelsen M, Pallesen S, Mageroy N et al. Effects of psychological and social factors in shiftwork on symptoms of anxiety and depression in nurses: a 1-year follow-up. J Occup Environ Med. 2015;57(10):1127–1137. doi: 10.1097/JOM.0000000000000532. [DOI] [PubMed] [Google Scholar]
- 30.Poole CJ, Evans GR, Spurgeon A, Bridges KW. Effects of a change in shift work on health. Occup Med (Lond). 1992;42(4):193–199. doi: 10.1093/occmed/42.4.193. [DOI] [PubMed] [Google Scholar]
- 31.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee A, Myung SK, Cho JJ, Jung YJ, Yoon JL, Kim MY. Night shift work and risk of depression: meta-analysis of observational studies. J Korean Med Sci. 2017;32(7):1091–1096. doi: 10.3346/jkms.2017.32.7.1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Angerer P, Schmook R, Elfantel I, Li J. Night work and the risk of depression: a systematic review. Dtsch Arztebl Int. 2017;114(24):404–411. doi: 10.3238/arztebl.2017.0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dalgard OS, Sorensen T, Sandanger I, Nygård JF, Svensson E, Reas DL. Job demands, job control, and mental health in an 11-year follow-up study: normal and reversed relationships. Work Stress. 2009;23(3):284–296. [Google Scholar]
- 35.Bentley RJ, Kavanagh A, Krnjacki L, LaMontagne AD. A longitudinal analysis of changes in job control and mental health. Am J Epidemiol. 2015;182(4):328–334. doi: 10.1093/aje/kwv046. [DOI] [PubMed] [Google Scholar]
- 36.Stansfeld S, Candy B. Psychosocial work environment and mental health—a meta-analytic review. Scand J Work Environ Health. 2006;32(6):443–462. doi: 10.5271/sjweh.1050. [DOI] [PubMed] [Google Scholar]
- 37.Theorell T, Hammarström A, Aronsson G et al. A systematic review including meta-analysis of work environment and depressive symptoms. BMC Public Health. 2015;15:738. doi: 10.1186/s12889-015-1954-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Åkerstedt T, Garefelt J, Richter A et al. Work and sleep—a prospective study of psychosocial work factors, physical work factors, and work scheduling. Sleep. 2015;38(7):1129–1136. doi: 10.5665/sleep.4828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang J, Patten SB, Currie S, Sareen J, Schmitz N. A population-based longitudinal study on work environmental factors and the risk of major depressive disorder. Am J Epidemiol. 2012;176(1):52–59. doi: 10.1093/aje/kwr473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kuehner C. Why is depression more common among women than among men? Lancet Psychiatry. 2017;4(2):146–158. doi: 10.1016/S2215-0366(16)30263-2. [DOI] [PubMed] [Google Scholar]
- 41.World Health Organization. Mental health action plan: 2013–2020. 2013. Available at: https://apps.who.int/iris/bitstream/handle/10665/89966/9789241506021_eng.pdf;jsessionid=F5991FA0FE45592A94946E5D25442844?sequence=1. Accessed August 30, 2019.
- 42.Bloom DE, Cafiero ET, Jané-Llopis E The global economic burden of noncommunicable diseases. 2011. Available at: https://ideas.repec.org/p/gdm/wpaper/8712.html. Accessed December 21, 2018.
- 43.Bekkers MB, Koppes LL, Rodenburg W, van Steeg H, Proper KI. Relationship of night and shift work with weight change and lifestyle behaviors. J Occup Environ Med. 2015;57(4):e37–e44. doi: 10.1097/JOM.0000000000000426. [DOI] [PubMed] [Google Scholar]