Abstract
Ancient Greece was the cradle of the Mediterranean food tradition, characterized by the Mediterranean “eternal trinity” wheat - olive oil - wine, the very essence of the country’s traditional agricultural and dietary regime, enriched by a culture of sharing and commensality. This food model, subsequently adopted and spread by the Romans, was rediscovered at the end of the Second World War by two American researchers, Leland Allbaugh and Ancel Keys. With the famous Seven Countries Study, Keys demonstrated for the first time that populations practicing a Mediterranean diet - such as the Greeks and southern Italians - showed low mortality rates from ischemic heart disease compared to the peoples of Northern Europe and North America. Since then, numerous subsequent epidemiological studies and randomized clinical trials have confirmed the beneficial effects of the Mediterranean diet both in primary and secondary prevention of cardiovascular diseases. This review will focus on the origins of the Mediterranean diet from its roots and its relationship to cardiovascular disease, with a brief overview of the nutritional mechanisms that influence atherosclerosis.
Keywords: mediterranean diet, cardiovascular disease, medical history
Introduction
The traditional “Mediterranean diet” (MeD) is a legacy of millennia of contacts between cultures, traditions and dietary patterns typical of several countries of the Mediterranean basin, essentially based on the rural and agricultural habits of those populations.1 Today the MeD is considered the healthiest among diets, with evidence of increased longevity and protection against cardiovascular disease, cancer, Alzheimer’s and Parkinson’s diseases, as well as other chronic and inflammatory diseases.2,3 Although recognized as an Intangible Cultural Heritage of Humanity by UNESCO in 2010,4 the classic MeD is losing share, since the growing globalization has also affected the typical local eating habits, conforming them to unbalanced Western-style dietary patterns.
The MeD is an expression of the different agri-food cultures of the peoples living in the Mediterranean region, representing the heterogeneous historical and environmental context of this area. Consequently, there is no single well-defined MeD, but rather a series of variations on a common theme, that reflect a mosaic of food habits, cultural traditions, religions and lifestyles of the different Mediterranean regions: therefore, the term Mediterranean diet would be a misnomer.
Nevertheless - despite several variations - the “classic” MeD is largely plant- centered, with a high intake of legumes, fruit, nuts, whole-grains cereals and olive oil, but a low intake of saturated lipids, a moderately high consumption of fish, low-to-moderate intake of dairy products, a low intake of meat, poultry and sweets, and often a rather moderate drinking of red wine, generally with meals.5
The protective role of the MeD came to scientific attention with the Seven Countries Study conducted by Ancel Keys (1904–2004) (Figure 1). He demonstrated a correlation between dietary habits in the 1960s in Crete and low incidence of ischemic heart disease and other morbid conditions.6
Figure 1.
Ancel keys with Paul Dudley White and Flaminio Fidanza. Press conference in Gioia Tauro, Italy, 1960. Reproduced from: https://it.wikipedia.org/wiki/File:Ancel_Keys_-_Paul_Dudley_White_-_Flaminio_Fidanza_-_press_conference_in_Gioia_Tauro_-1960.JPG.
This historical and narrative review examines the origins of the MeD and its relationship with atherosclerosis, succinctly revising the current knowledge on nutritional mechanisms involved in cardiovascular disease.
Ancient Mediterranean Diet: Historical Context
Ancient Greece was the cradle of the Mediterranean food tradition, characterized by the Mediterranean “eternal trinity” wheat - olive oil - wine, the very essence of the country’s traditional agricultural and dietary regime, enriched by a culture of sharing and commensality.7
Written records and archaeological finds testify to the importance of food in the organization of the ancient Greek society, with frugal and simple meals; the shared meal was an act of good citizenship.
This dietary pattern was also adopted by the Romans, who spread it across a significant portion of their Empire.7
The nutritional choices were based on the availability of the products of agriculture, pastoralism and fishing, present in the Mediterranean bioregion. The typical diet of ordinary people in Greece and Rome was rather poor and based mainly on vegetables and bread, olive oil, legumes, fruit, milk, cheese, with only occasional meat and fish consumption.7 These were probably the ordinary foods of most of the population, not just the wealthy classes.
These products, mentioned in the writings of Homer and other classical authors, confirmed by archaeological findings, provide strong evidence that the aforementioned foods did exist in the period from about 750 BC to the classic period including. The same Homeric texts narrate that the Hellenic heroes - unlike the common people - ate mainly meat, accompanied by abundant quantities of bread and wine, since fruit and vegetables were not considered foods worthy of gods and heroes.8
The Greek playwright Antiphanes (circa 404–330 BC) nicknamed the Greeks “leaf chewers”, to emphasize their very rich diet in vegetables. According to the Orphic and Pythagorean teachings, meat was rarely consumed (also because it was expensive), while fish was more popular than meat.9
The ancient Greeks paid special attention to nutrition, believing that a correct diet was a prerequisite for the physical and mental health. It was thought that several diseases depended on incorrect diets, so different nutritional approaches were used to treat various disorders.9
Epicurean philosophy developed the theory of the pleasure of eating, in opposition to behavioural excesses and greed; the meal not only had to nourish, but also stimulate the spirit.
Hippocrates (460 BC – 370 BC), the father of Western Medicine, in work “On diet” expounded his nutritional theory, emphasizing the importance of diet in the treatment of diseases. One of the features of Hippocratic medicine was precisely the development of dietetics, in addition to traditional pharmacology. His famous aphorism “ Let food be thy medicine and medicine thy food”, highlighted the importance he attached to food in maintaining good health. The Hippocratic diet was not a restrictive diet for therapeutic purposes, but rather a wise and balanced lifestyle that allowed maintaining a status of wellbeing.10 The concept of diet included, together with food and drinks, also physical exercise, just as contemplated by the current guidelines.
Later, also Herophilus and Erasistratus (3rd century BC), founders of the great medical school of Alexandria, Celsus (1st century AD), and Galen (130–200 AD) wrote essays on the role of the diet in the treatment of diseases.7
Plato (428 BC - 348 BC) discussed the diet in his famous dialogues: his philosophical conception based on moderation is also found in the vision of the dietary style. According to Plato, a balanced and healthy dietary pattern is based on cereals, legumes, fish, fruit, milk and honey; while meat, sweets and wine should be consumed only in limited quantities. Food abuse was not permitted, since it caused disturbances. Plato recommended a balanced diet, with consumption of all types of nutrients in moderate quantities: one should note that he considered obesity as a disease, correlating it with a lower life expectancy.11 For ancient physicians, food was only part of the lifestyle, that was to be evaluated in order to maintain or restore good health. It is remarkable that the food style proposed by Plato and by physicians and philosophers of classical antiquity is surprisingly similar to the modern Mediterranean diet, currently considered healthier than the diets of the rich western societies.
The Greek food model - adopted by Rome and widespread throughout Europe with its achievements - remained the reference for medicine throughout the Middle Ages and the Renaissance, although revised according to the “four humours” theory. In the Middle Ages, the Hippocratic teachings were preserved and disseminated at the Salerno School of Medicine, which reached its peak during the 12th century, especially in the study of nutrition.
Only in 1614, the Italian Giacomo Castelvetro (1546–1616) - a preceptor, diplomat, teacher of Italian, exiled from Modena and rescued from the Inquisition in Venice by the British ambassador - spread and promoted the salient features of the Italian diet, rich in fruit and vegetables, foods rarely consumed in England. Castelvetro was shocked by the large amount of meat and sweets consumed by the British. So, he tried to convince the British to change their incorrect eating habits diet, adopting the balanced, diversified and virtuous Italian food model, based on plant foods.12 His exhortation, however, remained a dead letter.
Then, during the 1950s Ancel Keys with the Seven Country Study showed, as we shall see, the existence of a clear relationship between the MeD and low mortality rates due to coronary heart disease.6
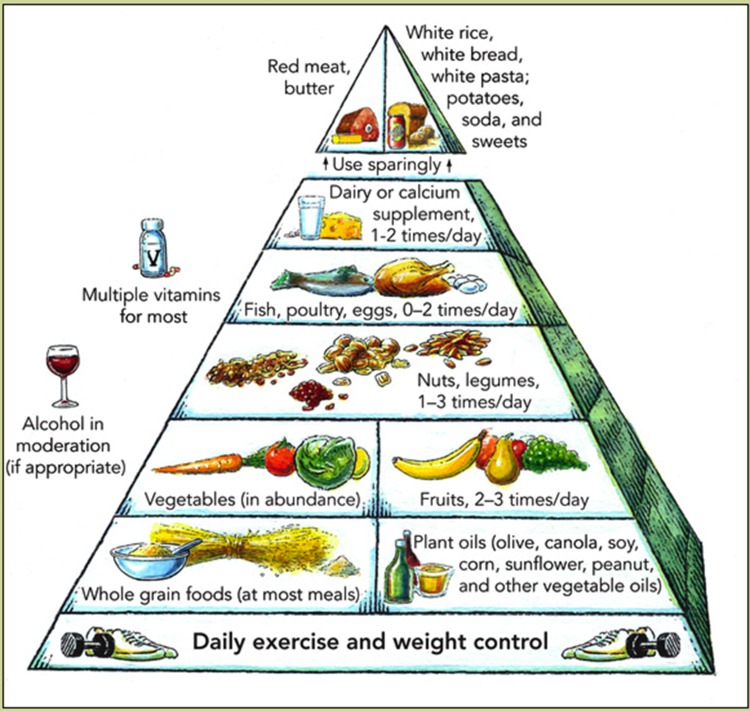
Finally, in 1993 the Harvard School of Public Health presented the first Mediterranean Diet Pyramid produced by the Oldway’s Preservation and Exchange Trust, indicating the recommendations for a healthy diet, according to the rules of the Mediterranean diet.1 The pyramid (Figure 2) has undergone several changes over the years, but the basic concept is substantially unchanged.
Figure 2.
Mediterranean diet pyramid. Reproduced from: https://commons.wikimedia.org/wiki/File:Harvard_food_pyramid.png.
The Main Epidemiological Evidence
The beginning of the history on the prevention of coronary heart disease in humans can be traced back to the well-known Framingham study wich showed a clear and significant relationship between plasma cholesterol level in the apparently healthy people and the consequent probability of developing coronary disease.13
Subsequent works showed that dietary cholesterol was closely associated with both serum cholesterol levels and mortality rates for atherosclerosis in humans,14 leading to the classical diet-heart hypothesis. This theory suggested that a high dietary intake of saturated fats and cholesterol played a crucial role in causing coronary atherosclerosis in humans.15
The Early Epidemiological Studies
The first research on dietary intake and food styles in the Mediterranean area dates back to the period after World War II. In 1948, the Greek government commissioned the Rockefeller foundation to study the population of the island of Crete. Cretan Greeks - despite living in backward socio-economic conditions - had good health, minimal incidence of coronary heart disease and exceptional longevity.
From the questionnaires administered by the epidemiologist Leland Allbaugh (1896–1991) it has emerged that the population practiced a “poor” diet based on cereals, legumes, vegetables and fruit, with limited consumption of meat; these were meals simply prepared and “floated” in olive oil.16 This important fact was not adequately evaluated and only thanks to the results of the subsequent Seven Countries Study it was possible to demonstrate a scientific link between the abundant use of olive oil and the incidence of cardiovascular diseases. Anyway, the Rockfeller Foundation’s study allowed to understand how food choices could affect people’s health.
Further support to the Mediterranean diet’s cardioprotection came precisely from studies on the ecological correlations between diet and coronary heart disease rates in different countries. The Seven Countries Study was designed in the 1950s by Ancel Keys (1904–2004) et al mainly to verify a possible link between diet, lifestyle and ischemic heart disease.17 Keys enrolled 16 population cohorts in eight nations of seven Mediterranean and non-Mediterranean countries for a total of 12,763 middle-aged men, obtaining follow-up data for over 50 years. This study demonstrated for the first time that the Mediterranean populations - such as Greeks (especially the farmers of Crete) and southern Italians - showed low mortality rates from ischemic heart disease compared to the peoples of Northern Europe and North America. The diet, without caloric restrictions, did not select specific foods, but was characterized by an abundant consumption of vegetables, a great use of olive oil as the main source of fats, a daily intake fresh fruit, a low intake of red meat, moderate consumption of wine, fish and poultry, limited dairy products. The differences across countries in coronary artery disease rates were closely related to different intakes of saturated fats and average levels of serum cholesterol. The MeD was associated with a lower incidence and mortality from coronary heart disease, with the lowest mortality rates and the highest survival rates. This pioneering large ecological investigation - despite its limitations - is still internationally recognized as the seminal study in this area.
Another study conducted by the EURATOM (European Atomic Energy Commission) from 1963 to 1965 provided comparative data on food intake in the Mediterranean and other European regions.18
The Commission examined domestic food consumption in 3725 families in 11 regions of 6 European countries to identify commonly consumed foods, probably contaminated by radioactive substances. The study revealed significant differences in dietary style, particularly among the Italian regions. Diets in the Mediterranean areas were characterized by a higher consumption of cereals, vegetables, fruit and fish and a low intake of potatoes, meat, dairy products, eggs and sweets. The levels of fat intake also showed differences: the consumption of butter and margarine was much higher in northern regions, whilst in the south the main fat was olive oil and margarine was not used at all. The data from this study provide additional evidence that the MeD in the mid-60s was essentially based on plant foods and olive oil was the main fat.
Findings From Randomized Clinical Trials
Below, we review some major randomized clinical trials that evaluated the effects of MeD on blood lipoproteins and heart disease.
Early randomized trials (Wadsworth Hospital and Veterans Administration Center in Los Angeles,19 The Oslo Diet-Heart Study,20 Finnish Mental Hospital Study21) investigated the effectiveness of low-cholesterol diets, enriched in polyunsaturated fatty acids. These studies showed a 25 to 50 percent reduction in coronary heart disease endpoints over 5 to 12 years, with a 13 to 15 percent reduction in blood cholesterol levels.
Another important study was the DART (Diet and Reinfarction trial) a secondary prevention trial after myocardial infarction.22 2033 men were randomly allocated to three different dietary patterns independently: a reduction in fat intake and an increase in the ratio of polyunsaturated to saturated fat, an increase in fatty fish intake, and an increase in cereal fibre intake. Those subjects advised to eat fatty fish had a 29% reduction of all-cause mortality in a 2 year period compared with those that had not been advised. These results demonstrated that a modest intake of fatty fish could reduce medium and long-term mortality in men after myocardial infarction.
The effect of the MeD on coronary death after myocardial infarction was also studied in the famous Lyon Diet Heart Study. In 1999, de Lorgeril et al published the final report of this randomized secondary prevention trial. 605 French men with a first myocardial infarction were randomized to the MeD vs American Heart Association Step 1 control diet. After a mean follow-up of 27 months, the study was early interrupted because the MeD group had a significant 70% reduction in all-cause mortality due to a 73% reduction in coronary heart disease mortality and analogous major reductions in non fatal complications.23 This benefit emerged only a few months after starting, probably due to the antithrombotic, antioxidants anti-inflammatory and antiarrhythmic pathways, related to the increased intake of omega-3 fatty acids, monounsaturated fats, vitamins and fiber.
In another randomized clinical trial, Singh et al tested a “Indo-Mediterranean diet,” in 1,000 Indian patients at high risk or with existing coronary heart disease (Indo-Mediterranean Diet Heart Study). As compared with the control diet, the intervention diet - rich in whole grains, fruits, vegetables, walnuts, almonds, mustard, or soybean oil - reduced the rate of nonfatal myocardial infarction by about 50% and the rate of sudden death from cardiac causes by about 60%.24
The Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto Miocardico in 1999 published a typical secondary prevention study, the GISSI-Prevenzione trial. The study was designed to test the benefits of vitamin E and n-3 polyunsaturated fatty acid supplementation in 11,324 patients surviving recent myocardial infarction. Patients were randomly assigned as follows: supplements of n-3 PUFA (1 g daily), vitamin E (300 mg daily), both, or none (control) for 3.5 years. Treatment with n-3 PUFA, but not vitamin E, significantly lowered the overall risk of death and of coronary death from 6.8% to 4.8% (−2%).25
Similarly, the Jelis study showed that eicosapentaenoic acid was a promising approach for the prevention of major coronary events, in Japanese hypercholesterolemic individuals.26
Although meta-analysis of observational studies has supported the intake of larger amounts of fish in high-risk patients, a recent extensive Cochrane Systematic Review showed that increasing polyunsaturated fatty acids (PUFA) intake has little or no effect on all-cause mortality or cardiovascular deaths, probably slightly reducing the risk of coronary heart disease and cardiovascular disease events, the risk of coronary heart disease death and stroke. Furthermore, it slightly reduces total cholesterol and probably triglycerides, with little or no effect on high‐density lipoprotein.27
The risk reduction would be related to reduced inflammation and angiogenesis, favorable effects on lipid metabolism and thrombogenesis, and to the physiological antiarrhythmic properties of omega-3 fatty acids, as already detailed in several researches.28
Some randomized studies testing the efficacy of various antioxidants, vitamins and supplements have instead reported insignificant evidence on the role of individual Mediterranean nutrients in preventing heart disease and mortality. This indicates a complex relationship between diet and heart disease, suggesting that the beneficial effects of the MeD are related to the synergy between its various cardio-protective foods, and not to individual nutrients or artificial dietary supplements and addictives.29,30
A Primary Prevention Study
The PREDIMED study (PREvención con DIetaMEDiterránea) was the first randomized clinical trial designed to evaluate the beneficial effects of MeD on the primary prevention of cardiovascular diseases, performed in Spain from 2003 to 2011. 7447 participants (55 to 80 years, 57% women) at high cardiovascular risk, but without cardiovascular disease were randomly assigned to three diet groups as follows: 1) The MeD supplemented with extra-virgin olive oil; 2) The MeD supplemented with nuts; and 3) a control diet (advice to reduce fat).
The assignment to an unrestricted MeD supplemented with either extra virgin olive oil or nuts was associated with a lower risk of major cardiovascular events over a period of 5 years compared to assignment to a control (low fat) diet, with a relative difference of 30% and an absolute difference of 1.7 to 2.1 percentage points.31,32
Subsequently, a series of sub-studies of PREDIMED concerning other chronic conditions were published. The incidence of the metabolic syndrome,33 diabetes,34 hypertension,35 breast cancer36 was significantly reduced in individuals randomized to the MeD, while it did not result in lower heart failure incidence.37 Diet have also shown beneficial effects in the treatment of obesity38 and decreased inflammatory biomarkers related to atherosclerosis.39
Although the mechanisms involved are not fully understood, the abundance of this dietary pattern in antioxidants and anti-inflammatory molecules is likely to be remarkable. The protection observed in the PREDIMED study is linked to improvement of various cardiovascular risk factors, as well as to a significant anti-inflammatory and immunomodulatory effect, in the short- and long-terms.
Diet And Atherosclerosis
Historically, diet has always been considered a crucial element for cardiovascular health, since correct eating habits positively influence other cardiovascular risk factors.2,40 The MeD has a protective effect against atherosclerosis, commonly considered a disease of the contemporary age associated with advanced modern lifestyles and diets.
However, atherosclerosis is certainly ancient disease, according to indications of paleopathology. Autopsy studies and computed tomographic findings of ancient mummies have clearly shown that atherosclerosis has been present in humans for more than 5,000 years. The Horus study of four ancient populations showed that atherosclerosis - evidenced by arterial calcifications found on whole-body CT scan of the mummies - was common in preindustrial civilizations including preagricultural hunter-gatherers.41–43 A study compared patterns and demographic characteristics of atherosclerosis among Egyptians from ancient and modern times, showing that the extent and severity of atherosclerotic vascular disease were strongly related to aging in both modern and ancient Egyptians, regardless of gender.44 Nevertheless, the ancient elite classes were more affected by atherosclerosis than the less well-off ones, likely due to the high intake of very atherogenic foods (fatty meats, such as goose and pork; abundant consumption of sugar and honey) in their diet, as well as for a greater tendency to overweight and diabetes.45 Probable unconventional cardiovascular risk factors related to atherosclerotis could be identified in a chronic microbial and parasitic inflammatory burden widespread in ancient peoples, lacking adequate hygiene and antimicrobial agents. Also domestic smoke inhalation used by ancient civilizations for daily cooking and lighting would be another potential pro-atherogenic inflammatory cause, as well as other unknown risk factors.46
This confirms that the interaction between aging, genetic and environmental factors is crucial in atherogenesis.
High Fat Diet And Atherosclerosis
The relationship between diet, lipoprotein metabolism, inflammation and atherosclerosis has been the subject of intense studies for about a century and the explanation of the role of the cholesterol-rich diet in the pathogenesis of atherosclerosis is often considered one of the most important discoveries of the 20th century.47 In the early 1900s, several researchers thoroughly studied the pathophysiological aspects of atherosclerotic plaque. Russian scientists developed an interesting experimental animal model of atherosclerosis, using rabbits fed on a diet high in cholesterol and fat. In particular, Nikolai N. Anichkov (1885–1964) first demonstrated that it was cholesterol only that caused atherosclerotic changes in the rabbit arterial intima (Figure 3). He fed these animals with foods high in cholesterol and fat, and observed that such diet caused - in association with greatly elevated blood cholesterol - arterial lesions that closely resembled those of human atherosclerosis.48,49 Anichkov was the first to describe the “cholesterinesterphagozyten”, nowadays called foam cells, originating from macrophages, and identified the cell types involved in atherosclerotic lesion, i.e. smooth muscle cells, macrophages and lymphocytes.
Figure 3.

Nikolaj Anitschkow. Reproduced from: https://it.m.wikipedia.org/wiki/File:Anichkov,_Nikolay_Nikolayevich.jpg.
In 1958 William Dock - reviewing the first fifty years of atherosclerosis research - likened Anichkov’s discovery to the discovery of the tubercle bacillus by Robert Koch;50 his theory of coronary atherosclerosis, published in Circulation, inaugurated a new era in research on this disease.51
After many years of epidemiological and clinical studies, the importance of the diet on cardiovascular diseases was widely accepted, confirming that the increase in blood cholesterol was an important independent risk factor for coronary artery disease (the diet-heart hypothesis).15,52
Inflammation And Atherosclerosis: The Current Interpretation Of An Ancient Hypothesis
Until relatively recently, most clinical and epidemiological studies have been influenced by classical diet-heart hypothesis. However, today we know that the aforementioned theory is too simplistic. The traditional interpretation of atherosclerosis as lipid storage pathology failed in the face of large and increased evidence that inflammation and the immune system played a key role in all phases of the disease, from its onset to the end-stage thrombotic events.53,54
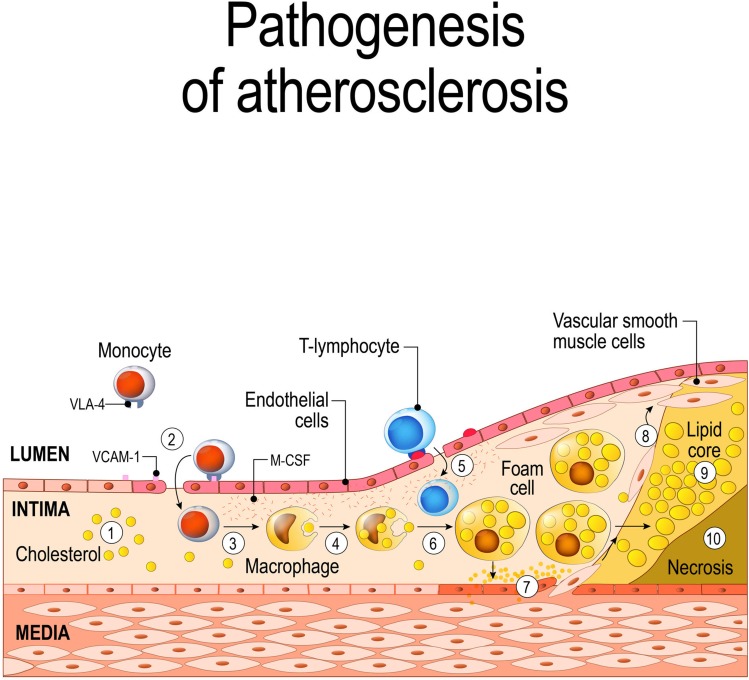
The chronic inflammatory process that affects the endothelium and causes the complications of the disease can be initiated by atherogenic triggers, such as modified or oxidized LDL, advanced glycation end products (in diabetes), free radicals, infectious agents, or other factors. These factors trigger atherogenesis, promoting the expression of adhesion molecules, in particular vascular cell adhesion molecule 1 (VCAM-1) by endothelial cells that allow the attachment of monocytes to the vascular endothelium. Subsequently, other signal molecules, such as monocyte chemoattractant protein-1, (MCP-1,) various cytokines and growth factors, including macrophage colony-stimulating factor (M-CSF), interferon γ, CD40 ligand (CD154), tumor necrosis factor α (TNF-α) interleukin 1 (IL-1) and IL-6, allow diapedesis into the intima of T lymphocytes and monocytes. The latter mature into macrophages and - incorporating modified lipoproteins - become lipid-rich foam cells, that are characteristic of fatty streaks, the first stage of atherosclerosis.53,54 The same signal molecules are also involved in plaque progression and eventual rupture. Inflammatory mediators, such as matrix-degrading metalloproteinase and gelatinases can weaken the atherosclerotic plaque’s fibrous cap, facilitating its rupture and subsequent thrombosis, responsible for the acute complications of atherosclerosis.53–55 Resident macrophages proliferate, release growth factors and cytokines, maintaining and increasing local inflammation, thus predisposing plaque fissuring. (Figure 4)
Figure 4.
Schematic of atherogenesis. Explanation in the text. ©[designua]/123RF.COM.
Nowadays, research have demonstrated that adherence to the MeD is associated with antiatherogenic effects such as: reduced blood pressure and lipemic levels;35 decreased oxidative stress, endothelial dysfunction and vascular inflammation.39 In truth, we must remember that Rudolf Virchow (1821–1902), in 1856, first attributed inflammation to a primary role in the atherosclerotic disease (“endo-arteritis chronica deformans”), considering it an initiating factor of atherogenesis.56
In the twentieth century - between the 60s and 70s - cytological studies on atherogenesis focused on the migration and proliferation of smooth muscle cells in atherosclerotic plaques,57,58 while in recent years several elegant experimental works have tried to clarify the molecular mechanisms involved in the pathogenesis of this disease.
Around the 90s, Polly Matzinger overcame the concept that the immune system’s primary objective was to discriminate between self and non-self, suggesting that its primary role was to detect danger signals, released from damaged tissues or cells, and not only by pathogens.59 Today we know that innate and adaptive immunity participate in atherothrombosis, as pathways linking classic risk factors to the altered arterial function.60 Danger signals are recognized by pattern recognition receptors (PRRs) that can identify two different molecular patterns: pathogen-associated molecular patterns (PAMPs) and damage/danger-associated molecular patterns (DAMPs). Among these PPRs groups, in particular NLRP3 (NOD-like receptor family, pyrin domain-containing protein 3) recognizes various DAMPs to form an NLRP3 inflammasome molecular complex in the cytoplasm and causes inflammatory responses. Recent research showed that NLRP3 inflammasome activation takes part in the pathogenesis of atherosclerosis.61 Various danger signals, such as cholesterol crystals, calcium crystals, and oxidized low-density lipoprotein, activate NLRP3 inflammasome to initiate inflammatory responses that leads to caspase-1-dependent programmed cell death, defined as pyroptosis.60,61
Current studies have focused on the therapeutic potential of NLRP 3 inflammasoma inhibitor (such as arglabine) in mice fed with a high-fat Western-type diet, observing a marked reduction of atherosclerotic lesions. These results, besides opening new interesting therapeutic scenarios, support an important link between diet and inflammation.62,63
Conclusions
From the ancient Greeks to the present day the MeD is considered as one of the healthiest dietary patterns. There is remarkable, strong and consistent evidence to support the benefits of the MeD in heart disease, and no other dietary pattern has been so widely and thoroughly studied in this area. So, today has become the gold standard for healthy eating.
The adherence to a Mediterranean-type dietary pattern is associated with a lower cardiovascular risk, a lower rate of mortality and incidence of cardiovascular disease.64 Its health benefits have also been demonstrated in primary31,32 and secondary cardiovascular prevention,23,25 and in prevention of major chronic degenerative diseases such as cancer.3,40 The beneficial effects of the MeD seem related to the synergy between its various cardio-protective nutrients. The modulation of vascular inflammation, the long-term immunomodulatory properties, the increased nitric oxide bioavailability, as well as the antioxidant effects are very likely the main mechanisms by which nutrients exert cardioprotective action.
In sum, the MeD can influence multiple modifiable cardiovascular risk factors, offering surprising possibilities for heart disease prevention. Improving inadequate eating habits remains a crucial goal to reach, as already appropriately recommended by ancient physicians.
Acknowledgment
We would like to thank Dr. Sergio Minelli (Department of Cardiology, Local Health Unit Lecce, Lecce, Italy) for his valuable support in reviewing the article.
Abbreviation
MeD, Mediterranean diet.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Willett WC, Sacks F, Trichopoulou A, et al. Mediterranean diet pyramid: a cultural model for healthy eating. Am J Clin Nutr. 1995;61(6):1402S–1406S. doi: 10.1093/ajcn/61.6.1402 [DOI] [PubMed] [Google Scholar]
- 2.Sofi F, Abbate R, Gensini GF, Casini A. Accruing evidence on benefits of adherence to the mediterranean diet on health: an updated systematic review and meta-analysis. Am J Clin Nutr. 2010;92:1189–1196. doi: 10.3945/ajcn.2010.29673 [DOI] [PubMed] [Google Scholar]
- 3.Schwingshackl L, Schwedhelm C, Galbete C, Hoffmann G. Adherence to mediterranean diet and risk of cancer: an updated systematic review and meta-analysis. Nutrients. 2017;9(10):1063 Published 2017 Sep 26. doi: 10.3390/nu9101063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Davis C, Bryan J, Hodgson J, Murphy K. Definition of the mediterranean diet; a literature review. Nutrients. 2015;7(11):9139–9153. Published 2015 Nov 5. doi: 10.3390/nu7115459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Available from: https://ich.unesco.org/en/RL/mediterranean-diet-00884. Accessed September11, 2019.[webpage on the Internet].
- 6.Keys A, Blackburn H, Menotti A, et al. Coronary heart disease in seven countries. Circulation. 1970;41(suppl 1):1–211. [DOI] [PubMed] [Google Scholar]
- 7.Garnsey P. Food and Society in Classical Antiquity. Cambridge University Press; 1999. [Google Scholar]
- 8.Seymour TD. Life in Homeric Age. The MacMillan Co; 1907:208–234. [Google Scholar]
- 9.Waterlow JC. Diet of the classical period of Greece and Rome. Eur J Clin Nutr. 1989;43(Suppl.2):3–12. [PubMed] [Google Scholar]
- 10.Craik E. Hippokratic diaita In: Wilkins J, Harvey D, Dobson M, editors. Food in Antiquity. Exeter, UK: University of Exeter Press; 1995:343–358. [Google Scholar]
- 11.Skiadas PK, Lascaratos JG. Dietetics in ancient Greek philosophy: plato’s concepts of healthy diet. Eur J Clin Nutr. 2001;55(7):532–537. doi: 10.1038/sj.ejcn.1601179 [DOI] [PubMed] [Google Scholar]
- 12.Castelvetro G. The Fruit, Herbs & Vegetables of Italy. London: Viking; 1989. [Google Scholar]
- 13.Kannel WB, Castelli WP, Gordon T, McNamara PM. Serum cholesterol, lipoproteins, and the risk of coronary heart disease: the framingham study. Ann Intern Med. 1971;74:1–12. doi: 10.7326/0003-4819-74-1-1 [DOI] [PubMed] [Google Scholar]
- 14.McGill HC. The relationship of dietary cholesterol to serum cholesterol concentration and to atherosclerosis in man. Am J Clin Nutr. 1979;32:2664–2702.05. doi: 10.1093/ajcn/32.12.2664 [DOI] [PubMed] [Google Scholar]
- 15.Gordon T. The diet-heart idea: outline of a history. Am J Epidemiol. 1988;127:220–225. doi: 10.1093/oxfordjournals.aje.a114798 [DOI] [PubMed] [Google Scholar]
- 16.Allbaugh LG. Crete — A Case Study of an Underdeveloped Area. Princeton, NJ: Princeton University Press; 1953. [Google Scholar]
- 17.Keys A, Menotti A, Karvonen MJ, et al. The diet and 15-year death rate in the seven countries study. Am J Epidemiol. 1986;124(6):903–915. doi: 10.1093/oxfordjournals.aje.a114480 [DOI] [PubMed] [Google Scholar]
- 18.Cresta M, Ledermann S, Garnier A, Lombardo E, Lacouply G. Etude des Consommations alimentaires des Populations de onze Régions de la Communauté Européenne en vue de la Détermination des Niveaux de Contamination radioactive. Rapport EUR 4218f (1969). Available from: http://aei.pitt.edu/91957/1/4218_f.pdf. Accessed September 11, 2019. [Google Scholar]
- 19.Dayton S, Pearce ML, Hashimoto S, Dixon WJ, Tomiyasu U. A controlled clinical trial of a diet high in unsaturated fat in preventing complications of atherosclerosis. Circulation. 1969;40(suppl II):II-1–II-63. doi: 10.1161/01.CIR.40.1S2.II-1 [DOI] [Google Scholar]
- 20.Leren P. The oslo diet-heart study. eleven-year report. Circulation. 1970;42:935–942. doi: 10.1161/01.cir.42.4.625 [DOI] [PubMed] [Google Scholar]
- 21.Turpeinen O, Karvonen MJ, Pekkarinen M, Miettinen M, Elosuo R, Paavilainen E. Dietary prevention of coronary heart disease: the finnish mental hospital study. Int J Epidemiol. 1979;8:99–118. doi: 10.1093/ije/8.2.99 [DOI] [PubMed] [Google Scholar]
- 22.Burr M, Fehily AM, Gilbert JF, et al. Effects of changes in fat, fish and fibre intakes on death and reinfarction: diet and reinfarction trial (DART). Lancet. 1989;2(8666):757–761. doi: 10.1016/s0140-6736(89)92010-2 [DOI] [PubMed] [Google Scholar]
- 23.de Lorgeril M, Salen P, Martin JL, Monjaud I, Delaye J, Mamelle N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: final report of the lyon diet heart study. Circulation. 1999;99(6):779–785. doi: 10.1161/01.cir.99.6.779 [DOI] [PubMed] [Google Scholar]
- 24.Singh RB, Dubnov G, Niaz MA, et al. Effect of an Indo-mediterranean diet on progression of coronary artery disease in high risk patients (Indo-mediterranean diet heart study): a randomised single-blind trial. Lancet. 2002;360:1455–1461. doi: 10.1016/S0140-6736(02)11472-3 [DOI] [PubMed] [Google Scholar]
- 25.GISSI-Prevenzione Investigators. Dietary supplementation with n-3 polyunsaturated fatty acids and vitamin E after myocardial infarction: results of the GISSI-prevenzione trial. Lancet. 1999;354:447–455. doi: 10.1016/S0140-6736(99)00434-1 [DOI] [PubMed] [Google Scholar]
- 26.Yokoyama M, Origasa H, Matsuzaki M, et al. Japan EPA lipid intervention study (JELIS) investigators. Effects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients (jelis): a randomised open-label, blinded endpoint analysis. Lancet. 2007;369:1090–1098. doi: 10.1016/S0140-6736(07)60527-3 [DOI] [PubMed] [Google Scholar]
- 27.Abdelhamid AS, Martin N, Bridges C, et al. Polyunsaturated fatty acids for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2018;7:CD012345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Massaro M, Scoditti E, Carluccio MA, Montinari MR, De Caterina R. Omega–3 fatty acids, inflammation and angiogenesis: nutrigenomic effects as an explanation for anti-atherogenic and anti-inflammatory effects of fish and fish oils. J Nutrigenet Nutrigenomics. 2008;1:4–23. doi: 10.1159/000109871 [DOI] [PubMed] [Google Scholar]
- 29.Brown BG, Zhao X-Q, Chait A, et al. Simvastatin and niacin, antioxidant vitamins, or the combination for the prevention of coronary disease. N Engl J Med. 2001;345:1583–1592. doi: 10.1056/NEJMoa011090 [DOI] [PubMed] [Google Scholar]
- 30.Meade T, Sleight P, Collins R, et al.MRC/BHF heart protection study of cholesterol-lowering therapy and of antioxidant vitamin supplementation in a wide range of patients at increased risk of coronary heart disease death: early safety and efficacy experience. Eur Heart J. 1999;20(10):725–741. doi: 10.1053/euhj.1998.1350 [DOI] [PubMed] [Google Scholar]
- 31.Estruch R, Ros E, Salas-Salvadó J, et al. Primary prevention of cardiovascular disease with a mediterranean diet. N Engl J Med. 2013;368:1279–1290. doi: 10.1056/NEJMoa1200303 [DOI] [PubMed] [Google Scholar]
- 32.Estruch R, Ros E, Salas-Salvadó J, et al. Primary prevention of cardiovascular disease with a mediterranean diet supplemented with extra-virgin olive oil or nuts. N Engl J Med. 2018;378(25):e34. doi: 10.1056/NEJMc1711583 [DOI] [PubMed] [Google Scholar]
- 33.Babio N, Toledo E, Estruch R, et al. Mediterranean diets and metabolic syndrome status in the PREDIMED randomized trial. Cmaj. 2014;186:E649–E657. doi: 10.1503/cmaj.140764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Salas-Salvadó J, Bulló M, Babio N, et al. Reduction in the incidence of type 2 diabetes with the mediterranean diet: results of the PREDIMED-reus nutrition intervention randomized trial [published correction appears in diabetes care. 2018 Oct;41(10):2259-2260]. Diabetes Care. 2010;34(1):14–19. doi: 10.2337/dc10-1288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Doménech M, Roman P, Lapetra J, et al. Mediterranean diet reduces 24 hr ambulatory blood pressure, blood glucose, and lipids: one-year randomized, clinical trial. Hypertension. 2014;64:69–76. doi: 10.1161/HYPERTENSIONAHA.113.03353 [DOI] [PubMed] [Google Scholar]
- 36.Toledo E, Salas-Salvadó J, Donat-Vargas C, et al. Mediterranean diet and invasive breast cancer risk among women at high cardiovascular risk in the PREDIMED trial: a randomized clinical trial. JAMA Intern Med. 2015;175:1752–1760. doi: 10.1001/jamainternmed.2015.4838 [DOI] [PubMed] [Google Scholar]
- 37.Papadaki A, Martínez-González MÁ, Alonso-Gómez A, et al. Mediterranean diet and risk of heart failure: results from the PREDIMED randomized controlled trial. Eur J Heart Fail. 2017;19:1179–1185. doi: 10.1002/ejhf.750 [DOI] [PubMed] [Google Scholar]
- 38.Ruiz-Canela M, Zazpe I, Shivappa N, et al. Dietary inflammatory index and anthropometric measures of obesity in a population sample at high cardiovascular risk from the PREDIMED (PREvención con DIeta MEDiterránea) trial. Br J Nutr. 2015;113:984–995. doi: 10.1017/S0007114514004401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Medina-Remón A, Casas R, Tressserra-Rimbau A, et al. Polyphenol intake from a mediterranean diet decreases inflammatory biomarkers related to atherosclerosis: a substudy of the PREDIMED trial. Br J Clin Pharmacol. 2016;83(1):114–128. doi: 10.1111/bcp.12986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dinu M, Pagliai G, Casini A, Sofi F. Mediterranean diet and multiple health outcomes: an umbrella review of meta-analyses of observational studies and randomised trials. Eur J Clin Nutr. 2018;72(1):30–43. Epub 2017 May 10. doi: 10.1038/ejcn.2017.58 [DOI] [PubMed] [Google Scholar]
- 41.Thompson RC, Allam AH, Lombardi GP, et al. Atherosclerosis across 4000 years of human history: the horus study of four ancient populations. Lancet. 2013;381:1211–1222. doi: 10.1016/S0140-6736(13)60598-X [DOI] [PubMed] [Google Scholar]
- 42.Allam AH, Thompson RC, Wann LS, et al. Atherosclerosis in ancient Egyptian mummies: the horus study. JACC Cardiovasc Imaging. 2011;4:315–327. doi: 10.1016/j.jcmg.2011.02.002 [DOI] [PubMed] [Google Scholar]
- 43.Thompson RC, Allam AH, Zink AR, et al. Computed tomographic evidence of atherosclerosis in the mummified remains of humans from around the world. Glob Heart. 2014;9(2):187–196. ISSN 2211-8160. doi: 10.1016/j.gheart.2014.03.2455 [DOI] [PubMed] [Google Scholar]
- 44.Allam AH, Mandour Ali MA, Wann LS, et al. Atherosclerosis in ancient and modern Egyptians: the horus study. Glob Heart. 2014;9(2):197–202. doi: 10.1016/j.gheart.2014.03.2454 [DOI] [PubMed] [Google Scholar]
- 45.David AR, Kershaw A, Heagerty A. Atherosclerosis and diet in ancient Egypt. The Lancet. 2010;375(9716):718–719. doi: 10.1016/S0140-6736(10)60294-2 [DOI] [PubMed] [Google Scholar]
- 46.Thomas GS, Wann LS, Allam AH, et al. Why did ancient people have atherosclerosis? From autopsies to computed tomography to potential causes. Glob Heart. 2014;9(2):229–237. ISSN 2211-8160. doi: 10.1016/j.gheart.2014.04.002 [DOI] [PubMed] [Google Scholar]
- 47.Friedman M, Friedland GW. Medicine’s 10 Greatest Discoveries. New Haven (CT): Yale University Press; 1998. [Google Scholar]
- 48.Anichkov NN. Experimental arteriosclerosis in animals In: Cowdry EV, editor. Arteriosclerosis: A Survey of the Problem. New York: MacMillan Publishing; 1933:271–322. [Google Scholar]
- 49.Anichkov NN. A history of experimentation on arterial atherosclerosis in animals In: Blumenthal HT, editor. Cowdry’s Arteriosclerosis: A Survey of the Problem. 2nd ed. Springfield, (IL): Charles C. Thomas Publishing; 1967:21–46. [Google Scholar]
- 50.Dock W. Research in arteriosclerosis; the first fifty years. Ann Intern Med. 1958;49:699–707. doi: 10.7326/0003-4819-49-3-699 [DOI] [PubMed] [Google Scholar]
- 51.Anitschkow NN, Wolkoff KG, Kikaion EE, Pozharisski KM. Compensatory adjustments in the structure of coronary arteries of the heart with stenotic atherosclerosis. Circulation. 1964;29:447–455. doi: 10.1161/01.cir.29.1.4 [DOI] [PubMed] [Google Scholar]
- 52.Ross R, Harker L. Hyperlipidemia and atherosclerosis. Science. 1976;193:1094–1100. doi: 10.1126/science.822515 [DOI] [PubMed] [Google Scholar]
- 53.Libby P, Ridker PM, Maseri A. Inflammation and atherosclerosis. Circulation. 2002;105:1135–1143. doi: 10.1161/hc0902.104353 [DOI] [PubMed] [Google Scholar]
- 54.Libby P. Inflammation in atherosclerosis. Nature. 2002;420:868–874. doi: 10.1038/nature01131 [DOI] [PubMed] [Google Scholar]
- 55.Libby P. The molecular mechanisms of the thrombotic complications of atherosclerosis. J Intern Med. 2008;263:517–527. doi: 10.1111/j.1365-2796.2008.01965.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Virchow R. Cellular Pathology. London, United Kingdom: John Churchill; 1858. [Google Scholar]
- 57.Ross R, Glomset JA. The pathogenesis of atherosclerosis I. N Engl J Med. 1976;295(7):369–377. doi: 10.1056/NEJM197608122950707 [DOI] [PubMed] [Google Scholar]
- 58.Ross R, Glomset JA. The pathogenesis of atherosclerosis II. N Engl J Med. 1976;295(8):420–425. doi: 10.1056/NEJM197608192950805 [DOI] [PubMed] [Google Scholar]
- 59.Matzinger P. Tolerance, danger, and the extended family. Annu Rev Immunol. 1994;12:991–1045. doi: 10.1146/annurev.iy.12.040194.005015 [DOI] [PubMed] [Google Scholar]
- 60.Libby P, Lichtman AH, Hansson GK. Immune effector mechanisms implicated in atherosclerosis: from mice to humans. Immunity. 2013;38(6):1092–1104. doi: 10.1016/j.immuni.2013.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Liu D, Zeng X, Li X, Mehta JL, Wang X. Role of NLRP3 inflammasome in the pathogenesis of cardiovascular diseases. Basic Res Cardiol. 2018;113:5. doi: 10.1007/s00395-017-0663-9 [DOI] [PubMed] [Google Scholar]
- 62.Abderrazak A, Couchie D, Mahmood DF, et al. Anti-inflammatory and antiatherogenic effects of the NLRP3 inflammasome inhibitor arglabin in ApoE2. Ki mice fed a high-fat diet. Circulation. 2015;131(12):1061–1070. doi: 10.1161/CIRCULATIONAHA.114.013730 [DOI] [PubMed] [Google Scholar]
- 63.Libby P, Brendan M. Everett novel antiatherosclerotic therapies. Arterioscler Thromb Vasc Biol. 2019;39:538–545. doi: 10.1161/ATVBAHA.118.310958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lopez-Garcia E, Rodriguez-Artalejo F, Li TY, et al. The mediterranean-style dietary pattern and mortality among men and women with cardiovascular disease. Am J Clin Nutr. 2014;99(1):172–180. doi: 10.3945/ajcn.113.068106 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Available from: https://ich.unesco.org/en/RL/mediterranean-diet-00884. Accessed September11, 2019.[webpage on the Internet].