Abstract
Expectations and beliefs about complementary and integrative medicine (CIM) are the main predictors of its use in cancer patients. These expectations are rarely informed by consultation with a healthcare provider but are, rather, a result of family endorsement and information from nonmedical sources. As a rising number of cancer patients pursue integrative medicine, it is of increasing importance that healthcare providers understand their patients’ expectations and motivations. These can range from symptom management to unrealistic hopes for cure. CIM can be used to complement gold standard cancer care, but is sometimes dangerously touted as an alternative for it. Awareness of these nuances enables providers to initiate effective communication about CIM and to intervene when unrealistic expectations stand in the way of life-saving care. Refining patient-centered communication around integrative medicine is essential to avoid unsupervised, potentially harmful use, delays, or interruptions in cancer care, and ultimately, to maximize the benefits of integrative therapies during cancer treatment.
Keywords: Integrative Medicine, Integrative Oncology, Patient Expectations, CIM, CAM, Communication
Understanding Complementary and Integrative Medicine Use in the Cancer Population
The use of complementary and integrative medicine (CIM) is extensive in the cancer population, exceeding that of noncancer patients.1 Surveys reveal CIM use exceeds 65% among cancer survivors and 45% among patients in active treatment.2,3 This includes acupuncture, mind-body therapies such as meditation and yoga, and the use of natural products and supplements, as well as the unsubstantiated treatments often referred to as “alternative medicine”.
Integrative oncology is a patient-centered, evidence-informed field of comprehensive cancer care using nonpharmacologic interventions and lifestyle modifications alongside conventional cancer treatments.4 Integrative medicine prioritizes patient safety and formulates treatment goals that are supportive, preventive, personalized, and intended to complement conventional cancer care. In contrast to the practice of integrative oncology, “alternative medicine” can often involve the rejection of conventional cancer care and relies on unsubstantiated claims and anecdotal evidence. In addition, alternative therapies are often unrealistically touted to be curative, while its use in the cancer setting in lieu of conventional oncologic treatment has been associated with decreased survival.5
Existing studies find that up to 45–66% of cancer patients endorse the use of CIM during their treatment or thereafter, and the prevalence of this use is rising.6–8 Demand is thought to result from improved cancer survival and a growing survivorship population interested in managing symptoms associated with the disease and its treatment. As cancer mortality is declining, the number of patients facing lasting impact on their quality of life due to cancer-related fatigue, hot flashes, sleep-mood disturbance, and chronic pain is also rising steadily.9
While these symptoms are not life-threatening in themselves, they remain difficult to treat and often result in unmet needs and a quest for treatment options. These unmet needs paired with the heightened motivation to actively contribute to one’s health that often follows a cancer diagnosis, as well as the common preference for nonpharmacologic treatment options, drives patients towards integrative treatments and unsubstantiated alternatives.10,11
Motivations for choosing to use CIM in the cancer setting may range from inclination towards natural approaches and the need for personalized attention and psychological support to distrust in the pharmaceutical industry and medical establishment.10,11 While these motivations are important to consider, it is primarily expectations towards these treatments that determine CIM use in the cancer setting. A survey-based study in a mixed cancer population of almost 1000 patients revealed that patient-held beliefs, such as expectations of therapeutic benefits predicted the use of nonconventional therapies more than clinical or demographic factors.10
Risk Associated with Unrealistic Expectations of Integrative Treatments
Expectations with which cancer patients approach CIM vary broadly, from symptom improvement to expectations of improved outcomes and cure. It is these latter expectations that are important to understand and recognize as they can lead to delay, rejection, or noncompliance with indicated conventional care.12–14 Raising awareness among healthcare providers around the consequences of unrealistic expectations is essential, as patients who choose alternative medicine instead of conventional oncologic treatment compromise their outcomes and survival.5,15
The detriment of unrealistic expectations about integrative treatments is not limited to abandonment of conventional care. A recent European survey study found a high prevalence (45%) of complementary therapy use during the conventional cancer treatment.3 More than half of these patients believed that their concurrent use could positively reinforce their cancer treatments and did not believe in a possible negative impact. Of these concurrent users, 76% used biologically active products, including herbal teas, homeopathy, dietary supplements and herbal medicines, some of which have the potential to cause clinically significant herb-drug interactions [see Hou and Mao, this issue].16
Another study surveying 141 cancer patients in active treatment reported using CIM with various expectations: 18% hoped to increase their body’s ability to fight cancer by using CIM, 15% believed CIM to be part of their effort to do everything they could to fight the cancer, and 3% believed their CIM use could treat or cure their cancer.17 Among almost 700 breast cancer patients in a prospective cohort study, those that used dietary supplements or a higher number of nonconventional therapies, except for mind-body practices, were less likely to initiate indicated chemotherapy.18
Unrealistic expectations regarding integrative or alternative therapies have been further characterized as more common in younger patients. The belief that cancer can be cured by natural or alternative treatments alone is held by 4 in 10 Americans and more common among younger people.19 Additionally, there is an observed tendency in cancer patients younger than age 65 as well as those with a college education to expect greater benefits from integrative and alternative treamtents.10
Influencers and Predictors of CIM-Related Patient Expectations
Patients acquire information about integrative medicine from a diverse range of sources. Many nonconventional treatments go back to ancient and traditional healing methods that get passed along within cultural circles. Thus, family members play an important role in influencing the use of and enforcing beliefs and expectations about these therapies.
In a cross-sectional study of over 900 cancer patients, family endorsement of integrative and alternative therapies was associated with increased expectations of health benefits, including improved pain, stress, and immune function. However, this endorsement also led to expectations of increased longevity (61% vs 24% without endorsement) and cancer cure (37% vs 12%). This confirms findings from previous studies that decisions regarding the use of nonconventional treatments are highly influenced by a patient’s social network.10,20,21
Moreover, decisions on whether to use nonconventional therapies are often made without the knowledge of healthcare providers.22 Observational studies report that patients do not disclose their integrative medicine use for a variety of reasons, but perhaps one reason is most striking: When healthcare providers were perceived as uninformed or holding negative attitudes towards complementary therapies, breast cancer patients relied more on their social network to guide decisions about CAM use.23 Further evidence of this guiding principle for patients appeared in the 2010 AARP/NCCAM Survey of U.S. Adults, where 42% of participants reported that reasons for their nondisclosure on integrative and alternative therapies was their physician’s failure to ask about their use.24 Other reasons included patient unawareness that they should disclose their use, not enough time during their visit, and providers perceived lack of knowledge on the subject, and/or fear of dismissal.
Patients interested in CIM use can perceive their provider’s discouragement as a conflict between their own belief system and the standard of care.23 This not only strains the doctor-patient relationship, but also has significant consequences on treatment choices patients make when unsupervised CIM use and unrealistic expectations go unnoticed.25,26
For these reasons, it is pertinent to support provider-patient communications about integrative and alternative therapies (Table 1) and actively assess and address factors that influence a patient’s use and expectations about these treatments (Table 2).
Table 1.
Key Messages To Drive Front-Line Healthcare Provider-Patient Communications
|
Table 2.
Motivations Checklist for CIM/Nonconventional Therapies
| □ Symptoms have lasting impact on quality of life eg, fatigue, hot flashes, sleep-mood disturbance, and chronic pain |
| □ Other unmet needs including psychological, spiritual, and emotional |
| □ Heightened motivation to actively contribute to one’s health |
| □ Inclination towards natural approaches |
| □ Need for personalized attention and support |
| □ Distrust in the pharmaceutical industry and medical establishment |
| □ Expectations of therapeutic benefits from nonconventional therapies |
| □ Younger than age 65 and/or college-educated, who expect greater/unrealistic benefits |
| □ Familial and cultural ties to ancient and traditional healing methods |
| □ Influencer and/or family endorsement of integrative and alternative therapies |
| □ Expectations of improved outcomes and cure |
| □ Belief that concurrent use could benefit cancer treatments, without negative impact |
| □ Use of biologically active products, including teas, supplements, and herbal medicines |
| □ Use of supplements or nonconventional therapies before chemotherapy has begun |
| □ Unsaid decisions are being made on nonconventional therapies |
| □ Patient perception that the healthcare provider is uninformed |
| □ Patient perception that the healthcare provider is dismissive or holds negative attitudes about CIM or nonconventional therapies |
| □ Physician failure to ask patient about CIM and nonconventional therapies used |
| □ Provider discouragement at odds with personal belief system |
| □ Strained doctor-patient relationship |
| □ Patient unaware they should disclose CIM or nonconventional use |
| □ Inadequate visit time |
CIM, complementary and integrative medicine.
Leading forces that determine CIM use in the cancer setting.
Cautionary forces that can lead to delay, rejection, or noncompliance with indicated care, or compromised outcomes.
Best Practices in Assessing and Addressing Patient Expectations
Acknowledging the severe implications of lacking communication about nonconventional therapies in the cancer setting and the scarce availability of competent guidance for cancer patients interested in these treatments, there is a great need for education about integrative care in the cancer setting for both patients and healthcare providers. Indeed, many oncology providers are not comfortable discussing CIM use with their patients.27
Goals for healthcare provider-driven communications on CIM treatments (Table 1) align with the principles of patient-centered care. These include improved patient satisfaction, shared decision-making, improved patient adherence and compliance with indicated treatments, and avoidance of adverse effects, toxicities through herb-drug interactions, and unsupervised use. The most urgent indication to ramp up improvements in communication and education in this area, however, is the need for early identification of patients at risk of abandoning or compromising their care and survival due to unrealistic expectations of nonconventional therapies.
Frenkel and Cohen divided communication on integrative medicine in two different aspects: How and What.28 The How addresses topics related to clinician attitude toward CIM, and patients’ unmet needs and emotions. The What describes the content of CIM-related advice and recommendations.
A review of 36 publications on communication practices related to CIM use in the oncology setting summarized advice on how to pursue effective provider-patient communications about CIM: “(1) Elicit the person’s understanding of their situation; (2) Respect cultural and linguistic diversity and different epistemological frameworks; (3) Ask questions about CAM use at critical points in the illness trajectory; (4) Explore details and actively listen; (5) Respond to the person’s emotional state; (6) Discuss relevant concerns while respecting the person’s beliefs; (7) Provide balanced, evidence-based advice; (8) Summarize discussions; (9) Document the discussion; (10) Monitor and follow-up.”29
Delivering CIM-related content and information maybe optimally assisted by experienced integrative oncology specialists. But the How of actively addressing CIM topics and establishing a fundamental trust with patients lies in the hands of front-line oncology care providers.
QAER: A Model to Improve Front-Line Communications
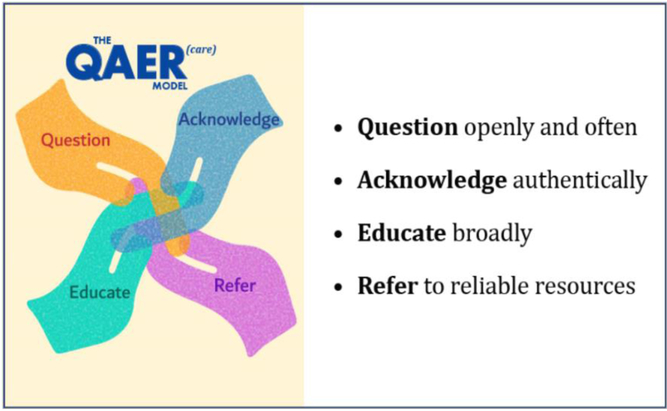
The QAER Model (pronounced care) may provide structure and guidance for clinicians seeking to improve CIM-related communications (Figure 1):
Question openly and often | Clinicians are encouraged to take initiative and ask directly about CAM use and the patient’s related expectations.29 Actively encouraging disclosure of CIM use may minimize unsupervised use, mitigate adverse outcomes related to the use, and unveil any unmet needs the patient may heave.
Acknowledge authentically | Active listening and affirmation of the patient’s wish to participate in their own care and incorporate their health philosophies and traditions may convey empathy and respect towards the patient’s preferences.
Educate broadly | Reviewing best available evidence and highlighting caveats of CIM use may address unrealistic expectations in a non-confrontational manner, improving compliance and minimizing risk.
Refer | Pointing patients towards reliable resources for CIM-related information may further encourage safe practices and patient empowerment.
Figure 1.
The QAER Model to improve front-line communications
CONCLUSIONS
Increased awareness about the driving motivations and expectations of patients for CIM use in the cancer setting may allow oncologists to identify patients at risk of nonadherence or rejection of life-saving care. The widespread unsupervised use of CIM demands that oncology providers actively encourage disclosure, destigmatize interests in integrative care and provide competent counseling in this area as an important prerequisite of patient-centered care.
Acknowledgments
The author thanks Ingrid Haviland, Assistant Editor at the MSK Integrative Medicine Service, for her editorial and graphic design assistance.
Funding
This work was supported by funding from the NIH/NCI Cancer Center Support Grant P30 CA008748 and the Laurance S. Rockefeller Fund at Memorial Sloan-Kettering Cancer Center.
Footnotes
Conflicts of Interest
The author has no conflicts of interest to report.
References
- 1.Mao JJ, Farrar JT, Xie SX, et al. Use of complementary and alternative medicine and prayer among a national sample of cancer survivors compared to other populations without cancer. Complement Ther Med. 2007;15:21–29. [DOI] [PubMed] [Google Scholar]
- 2.Mao JJ, Palmer CS, Healy KE, et al. Complementary and alternative medicine use among cancer survivors: a population-based study. J Cancer Surviv. 2011;5:8–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jermini M, Dubois J, Rodondi P- Y, et al. Complementary medicine use during cancer treatment and potential herb-drug interactions from a cross-sectional study in an academic centre. Sci Rep. 2019;9:5078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Witt CM, Balneaves LG, Cardoso MJ, et al. A Comprehensive Definition for Integrative Oncology. JNCI Monographs. 2017;2017. [DOI] [PubMed] [Google Scholar]
- 5.Johnson SB, Park HS, Gross CP, et al. Complementary Medicine, Refusal of Conventional Cancer Therapy, and Survival Among Patients With Curable Cancers. JAMA Oncol. 2018;4:1375–1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Horneber M, Bueschel G, Dennert G, et al. How many cancer patients use complementary and alternative medicine: a systematic review and metaanalysis. Integr Cancer Ther. 2012;11:187–203. [DOI] [PubMed] [Google Scholar]
- 7.Boon H, Stewart M, Kennard MA, et al. Use of complementary/alternative medicine by breast cancer survivors in Ontario: prevalence and perceptions. J Clin Oncol. 2000;18:2515–2521. [DOI] [PubMed] [Google Scholar]
- 8.Boon HS, Olatunde F, Zick SM. Trends in complementary/alternative medicine use by breast cancer survivors: comparing survey data from 1998 and 2005. BMC Womens Health. 2007;7:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Findley PA, Sambamoorthi U. Preventive health services and lifestyle practices in cancer survivors: a population health investigation. J Cancer Surviv. 2009;3:43–58. [DOI] [PubMed] [Google Scholar]
- 10.Bauml JM, Chokshi S, Schapira MM, et al. Do attitudes and beliefs regarding complementary and alternative medicine impact its use among patients with cancer? A cross-sectional survey. Cancer. 2015;121:2431–2438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mao JJ, Palmer SC, Straton JB, et al. Cancer survivors with unmet needs were more likely to use complementary and alternative medicine. J Cancer Surviv. 2008;2:116–124. [DOI] [PubMed] [Google Scholar]
- 12.Cassileth BR, Vickers AJ. High prevalence of complementary and alternative medicine use among cancer patients: implications for research and clinical care. J Clin Oncol. 2005;23:2590–2592. [DOI] [PubMed] [Google Scholar]
- 13.Hall JD, Bissonette EA, Boyd JC, et al. Motivations and influences on the use of complementary medicine in patients with localized prostate cancer treated with curative intent: results of a pilot study. BJU Int. 2003;91:603–607. [DOI] [PubMed] [Google Scholar]
- 14.Singh H, Maskarinec G, Shumay DM. Understanding the motivation for conventional and complementary/alternative medicine use among men with prostate cancer. Integr Cancer Ther. 2005;4:187–194. [DOI] [PubMed] [Google Scholar]
- 15.Verhoef MJ, White MA. Factors in making the decision to forgo conventional cancer treatment. Cancer Pract. 2002;10:201–207. [DOI] [PubMed] [Google Scholar]
- 16.Hou YN, Mao JJ. Practical application of “ABOUT HERBS” website: Herbs and dietary supplements use in oncology settings. Cancer J. 2019;May-Jun;26:XXX-XXX. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Buckner CA, Lafrenie RM, Dénommée JA, et al. Complementary and alternative medicine use in patients before and after a cancer diagnosis. Curr Oncol. 2018;25:e275–e281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Greenlee H, Neugut AI, Falci L, et al. Association Between Complementary and Alternative Medicine Use and Breast Cancer Chemotherapy Initiation: The Breast Cancer Quality of Care (BQUAL) Study. JAMA Oncol. 2016;2:1170–1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.ASCO National Cancer Opinion Survey, 2018; https://www.asco.org/sites/new-www.asco.org/files/content-files/research-and-progress/documents/2018-NCOS-Results.pdf; accessed 5/16/2019.
- 20.Boon H, Brown JB, Gavin A, et al. Breast cancer survivors’ perceptions of complementary/alternative medicine (CAM): making the decision to use or not to use. Qual Health Res. 1999;9:639–653. [DOI] [PubMed] [Google Scholar]
- 21.Naja F, Fadel RA, Alameddine M, et al. Complementary and alternative medicine use and its association with quality of life among Lebanese breast cancer patients: a cross-sectional study. BMC Complement Altern Med. 2015;15:444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tasaki K, Maskarinec G, Shumay DM, et al. Communication between physicians and cancer patients about complementary and alternative medicine: exploring patients’ perspectives. Psychooncology. 2002;11:212–220. [DOI] [PubMed] [Google Scholar]
- 23.Citrin DL, Bloom DL, Grutsch JF, et al. Beliefs and perceptions of women with newly diagnosed breast cancer who refused conventional treatment in favor of alternative therapies. Oncologist. 2012;17:607–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.AARP/NCCAM Survey of U.S. Adults 50+, 2010; https://nccih.nih.gov/sites/nccam.nih.gov/files/news/camstats/2010/NCCAM_aarp_survey.pdf, accessed in 05/16/2019.
- 25.Velicer CM, Ulrich CM. Vitamin and mineral supplement use among US adults after cancer diagnosis: a systematic review. J Clin Oncol. 2008;26:665–673. [DOI] [PubMed] [Google Scholar]
- 26.Shumay DM, Maskarinec G, Kakai H, et al. Why some cancer patients choose complementary and alternative medicine instead of conventional treatment. J Fam Pract. 2001;50:1067. [PubMed] [Google Scholar]
- 27.Roberts C, Benjamin H, Chen L, et al. Assessing communication between oncology professionals and their patients. J Cancer Educ. 2005;20:113–118. [DOI] [PubMed] [Google Scholar]
- 28.Frenkel M, Cohen L. Effective communication about the use of complementary and integrative medicine in cancer care. J Altern Complement Med. 2014;20:12–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schofield P, Diggens J, Charleson C, et al. Effectively discussing complementary and alternative medicine in a conventional oncology setting: communication recommendations for clinicians. Patient Educ Couns. 2010;79:143–151. [DOI] [PubMed] [Google Scholar]