Summary:
To increase self-examination for syphilis among men who have sex with men (MSM), we developed educational materials to increase knowledge of primary and secondary syphilis manifestations. Materials were piloted in five cities’ infectious disease or MSM clinics. Self- and partner-examination behaviour was assessed with an anonymous questionnaire. Of 1459 participants, 914 men had had sex with a man in the previous three months; the 171 MSM who reported having read the materials were significantly more likely to examine themselves (anus, adjusted prevalence ratio [aPR] 1.3, 95% confidence interval [CI] 1.15–1.52), mouth, penis and skin, and their partners’ anus (aPR 1.3, 95% CI 1.03–1.73) and mouth (aPR 1.6, 95% CI 1.1–2.26). Further research is needed to determine whether educational materials affect early detection and treatment of primary and secondary syphilis and reduce transmission.
Keywords: sexually transmitted infections, syphilis, Treponema pallidum, men who have sex with men, MSM, behavioural change, self-examination, health promotion
BACKGROUND
Rates of primary and secondary syphilis among men who have sex with men (MSM) in the USA continue to rise.1,2 In 2009, 62% of reported primary and secondary syphilis cases in the USA were among MSM.2 Efforts to reduce transmission of syphilis among MSM have typically focused on promoting routine syphilis screening at least annually (or more frequently in high-risk MSM), partner notification and symptom recognition by providers.3–5 These interventions have not had a demonstrable effect on the continued sexual transmission of syphilis, which often occurs through a painless, but highly infectious, ulcer (chancre) present during the primary stage of syphilis or from skin and mucosal lesions/rash that appear during the secondary stage of syphilis. Because they are painless, these lesions are often undetected when located in less visible areas, which in men include the rectum, anus or mouth. A proportion of primary and secondary syphilis is asymptomatic, and can only be detected through serology. In 2009, 76% of primary and secondary syphilis cases among MSM were secondary and only 24% were primary syphilis. Furthermore, 68% of all syphilis reported was diagnosed during the latent stages that follow primary and secondary infection, suggesting missed opportunities for early detection.2
Interventions to reduce syphilis incidence among MSM have emphasized screening by providers, behavioural change such as partner reduction and condom use. Only one has described self- and partner-examination for primary syphilis as a means to detect and treat syphilis early and reduce its transmission.4 Therefore, we evaluated whether educational materials about syphilis lesion recognition could increase self- and partner-examination behaviours among MSM.
METHODS
To increase awareness of syphilis signs, transmission and prevention, two types of printed materials were developed by the company palladian consultants under a contract with Centers for Disease Control and Prevention (CDC). The first materials developed were posters that encourage MSM to examine themselves and their partners for syphilis; the second was a brochure that describes syphilis stages, signs, transmission and prevention, including reducing number of partners, condom use and where to examine yourself and your partner. These materials were developed and focus-group tested in three large metropolitan cities (Baltimore, Philadelphia and Dallas) among six focus groups of sexually active MSM by palladian consultants. A total of 49 men were recruited based on their age, race and ethnicity, income, education and regular attendance at gay venues, use of the Internet for finding sexual partners, and HIV status; a broad representation of each category was sought as much as possible. Feedback from the focus groups was used to select and revise materials that were acceptable to heterogeneous groups of MSM and to improve the clarity of messages incorporated in these materials.
From 2009 to 2011, a convenience sample of five general infectious disease or sexually transmitted disease (STD) clinics primarily serving MSM populations were invited to participate in this evaluation. Clinics were located in Phoenix, Arizona (MSM clinic); Washington, DC (MSM clinic); Ft Lauderdale, FL (STD clinic); Miami, FL (MSM clinic) and Atlanta, GA (Infectious Disease clinic). All patients arriving at these clinics were asked to participate in this short evaluation. If they agreed to participate, they were given a one-page, anonymous survey to complete in the clinic exam room while waiting for a health-care provider. The survey included questions about age group, reason(s) for clinic visit, number of recent sexual partners (previous 3 months or since last clinic visit), knowledge about syphilis transmission and self- and partner-examination behaviours. Participants placed completed surveys in a closed box to maintain confidentiality. Patients were given the informational brochure about syphilis at the end of their clinic visit. Informational posters were hung in clinical encounter rooms. At a subsequent visit to the same clinic, patients could fill out the form again, but they were asked not to fill it out more than twice. Among the patients who completed an anonymous survey, only the men who reported having sex with a man in the last three months or since their last clinic visit were included in this evaluation. Women, men who only had sex with women and MSM who reported no partners since their last clinic visit or in the last three months were excluded from the analysis.
Men were classified into unexposed and exposed groups based on their responses to the following question, ‘before this (clinic) visit, had you read the Syphilis and Men Who Have Sex With Men information brochure provided by this clinic?’ Men who responded to this question by checking ‘No’ were classified as having not read the brochure before and men who responded by checking ‘Yes’ were classified as having read the brochure. We needed 112 surveys from MSM who had not read the brochure and 112 surveys from MSM who had read the brochure to detect an increase in daily self-examination from 10% to 25%, at a power of 80%. Because fewer surveys were completed by MSM who had read the brochure, we pooled the surveys across clinics to reach the required 112 MSM who had read the brochure.
Data were analysed using SAS v. 9.2 (SAS Institute, Cary, NC, USA). Demographic comparisons between participant groups were made using chi-squared tests. The variables ‘site’ and ‘number of sexual partners’ were associated with both brochure status and examination behaviours; therefore, we controlled for these two variables in our binomial regression models that examined the effect of having seen a brochure on examination behaviours. For all comparisons, significance was determined at P < 0.05.
Since the surveys were anonymous, of minimal risk to participants, and evaluated a programmatic intervention, this evaluation was determined by the CDC IRB-designated Human Subjects Contact as not being subject to Institutional Review Board (IRB) review for human subjects’ protection and received a non-research determination from the IRBs at each of the clinics.
RESULTS
From September 2009 to March 2011, a total of 1459 surveys were collected from all sites. After applying the selection criteria, we analysed 735 surveys from men who had not read the brochure and 171 surveys from men who had read the brochure. Men who had not read the brochure varied significantly from men who had read the brochure by site and number of sexual partners (Table 1). The highest percentage of men who had not read the brochure was from Washington, DC (27%) and the highest percentage of men who had read the brochure was from Phoenix (35%). Men who had not read the brochure reported having more sexual partners than those who had read the brochure. Age did not vary significantly between groups; most were aged 18–39 years (Table 1).
Table 1.
Participant characteristics by exposure to brochure status
| Had not read brochure (n = 735) | Had not read brochure (n = 171) | P value (Chi-square) | |
|---|---|---|---|
| Sites | % | % | |
| Phoenix, AZ | 17 | 35 | <0.0001* |
| Washington, DC | 27 | 15 | |
| Ft. Lauderdale, FL | 21 | 25 | |
| Miami, FL | 17 | 11 | |
| Atlanta, GA | 18 | 14 | |
| Number of sexual partners | |||
| 1 | 34 | 47 | 0.01* |
| 2–3 | 31 | 26 | |
| 4–10 | 28 | 23 | |
| >10 | 7 | 4 | |
| Age (years) | |||
| 18–39 | 59 | 66 | 0.09 |
| ≥40 | 41 | 34 | |
Compared with men who had not read the brochure before, men who had read the brochure from a previous visit reported more frequent self-examination of their anus, mouth, penis and skin at least once per week (Figure 1); prevalence ratios for all body parts were significantly higher (Table 2). A similar trend was noted for examination of partners’ bodies at least once per week (Figure 2). Participants who had read the brochure from a previous visit reported examining their partners’ bodies more frequently; prevalence ratios for examining partners’ anus and mouth were significantly higher (Table 2). Overall, participants reported examining their partners’ bodies less frequently than their own bodies.
Figure 1.
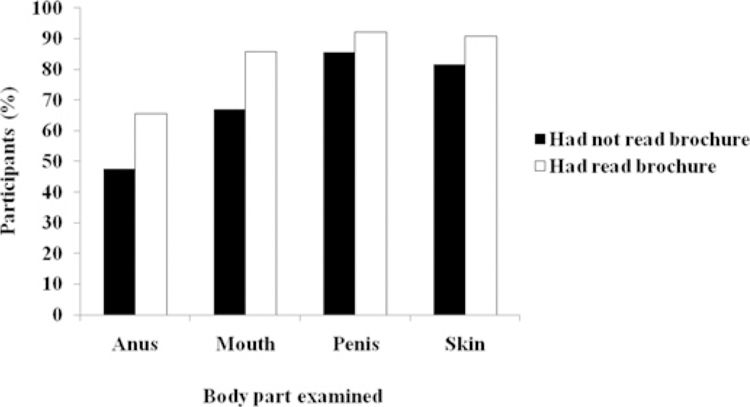
Proportion of participants reporting self-examination at least once a week by exposure to brochure status
Table 2.
Adjusted prevalence ratios for self- and partner-examination of various body parts at least once a week, comparing MSM who had read the brochure to MSM who had not read the brochure
| Self-examination |
Partner-examination |
|||
|---|---|---|---|---|
| Body part examined | aPR | 95% CI | aPR | 95% CI |
| Anus | 1.3 | 1.15–1.52* | 1.3 | 1.03–1.73* |
| Mouth | 1.2 | 1.14–1.36* | 1.6 | 1.10–2.26* |
| Penis | 1.1 | 1.01–1.14* | 1.1 | 0.94–1.38 |
| Skin | 1.2 | 1.05–1.19* | 1.1 | 0.95–1.39 |
MSM=who have sex with men; P = chi-squared; aPR = adjusted prevalence ratio; CI = confidence interval
P < 0.05 after adjusting for site and number of sexual partners
Figure 2.
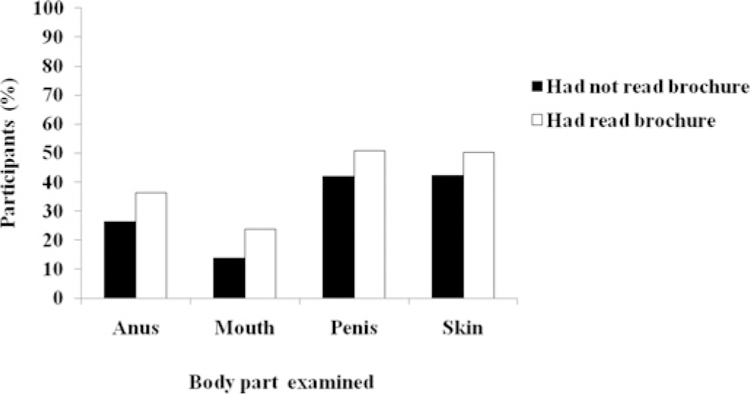
Proportion of participants reporting partner-examination at least once a week by exposure to brochure status
CONCLUSION
MSM in this assessment who reported having read a brochure on syphilis reported examining themselves and their partners more frequently than MSM who had not read the brochure. These results support findings from a previous evaluation of self-examination behaviours among HIV-infected MSM at two clinics in Phoenix.4 That study found that HIV-infected MSM who received provider counselling on syphilis prevention during their quarterly HIV clinic visits increased self-examination of oral and rectal areas from 60% to 80% between the first and second visits.4 Our evaluation differed from that study in that we did not collect identifying information from individuals to be able to compare ‘before’ and ‘after’ in the same individuals; we compared group responses for before and after exposure to the brochure (and posters). Our evaluation also differed in that we relied on participants reading the materials rather than providers giving counseling. Both evaluations suggest that low cost interventions can increase self- and partner-examination, although it remains unclear whether these behaviours will result in earlier detection and treatment of syphilis and reduction of transmission.
There were several limitations to this evaluation. First, misclassification of exposure to the brochure might have occurred because exposure to the brochure was determined by participants’ response to a survey question. Memory of having read the brochure could be erroneous, biasing results towards the null. Second, selection bias for health-conscious behaviour might have occurred among participants who had read the brochure or who were coming for a second visit, biasing results towards demonstrating an effect because, by definition, these participants had to have returned to the clinic. We did not collect detailed demographic information such as exact age, or race, ethnic group, or socioeconomic status. Lastly, due to social desirability bias, reports of self- and partner-examination behaviours might be overestimated.
Despite these limitations, the results of this evaluation suggest that low-cost educational materials on syphilis signs, examination sites and prevention messages could enhance existing syphilis prevention strategies for MSM. Given the effect of the brochure seen in this evaluation and the acceptability of educational materials on syphilis lesion recognition among MSM,6 broader dissemination of these materials could be considered alongside further research on whether such materials also affect early detection and treatment of primary syphilis and reduce its transmission in high-risk communities.
ACKNOWLEDGEMENTS
The authors thank the following people for their contributions to this project: Stuart Berman, Jim Braxton, Beverley Campbell, Justin Goforth, Kim Honer, Jamie Krashin, Edward Lake, Manya Magnus, John Marangio, Rachel Robitz, Tom Peterman and James Vellequette.
Disclosures: The CDC Experience is a one-year fellowship in applied epidemiology at CDC made possible by a public/ private partnership supported by a grant to the CDC Foundation from External Medical Affairs, Pfizer Inc.
Footnotes
Conflicts of interest: None declared.
REFERENCES
- 1.Peterman TA, Heffelfinger JD, Swint EB, Groseclose SL. The changing epidemiology of syphilis. Sex Trans Dis 2005;32:S4–S10 [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Sexually Transmitted Diseases Surveillance 2009. Atlanta: US Department of Health and Human Services, 2010 [Google Scholar]
- 3.Centers for Disease Control and Prevention. Sexually Transmitted Diseases Treatment Guidelines, 2010. MMWR 2010;59(No. RR–12):12. [PubMed] [Google Scholar]
- 4.Taylor MM, Peterson B, Post J, Williams C, Vanig T, Winscott M. Self-examination behaviors for syphilis symptoms among HIV-infected men. J Acquir Immune Defic Syndr 2010;55:284–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vega MY, Roland EL. Social marketing techniques for public health communication: a review of syphilis awareness campaigns in 8 US cities. Sex Transm Dis 2005;32(Suppl. 10):S30–6 [DOI] [PubMed] [Google Scholar]
- 6.Peterman TA. Promoting syphilis ulcer recognition among men who have sex with men (MSM); Focus groups to explore feasibility. Presented at National STD Prevention Conference. Oral presentation A1B 2008. March 10–13 Chicago, IL, 2008 [Google Scholar]


