Abstract
Background:
The meniscus is vital for load bearing, knee stabilization, and shock absorption, making a meniscal tear a well-recognized sport-related injury in children and young adults. An inverse relationship between the quality and value of orthopaedic care provided and the overall treatment cycle exists in which delayed meniscal tear treatment increases the likelihood of unfavorable outcomes. Although a majority of children and young adults have health insurance, many athletes within this demographic still face significant barriers in accessing orthopaedic services because of insurance type and household income.
Purpose:
To determine the impact of insurance status and socioeconomic markers on the time to orthopaedic evaluation and treatment as well as the rate of surgical interventions for meniscal tears in children and young adult athletes in the United States.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
We conducted a retrospective review of all patients ≤22 years of age who presented to our institution between 2008 and 2016 and who were diagnosed with meniscal tears. Patients were categorized based on insurance and socioeconomic status. Dates of injury, referral, evaluation by an orthopaedic surgeon, and surgery were also recorded. Chi-square and regression analyses were utilized to determine the significance and correlation between the influencing factors and time to referral, evaluation, and surgery.
Results:
Publicly insured, commercially insured, and uninsured patients comprised 49.4%, 26.6%, and 24.1%, respectively, of the 237 patients included in this study. Insurance status was predictive of time to orthopaedic referral, initial evaluation, and surgery (P < .01). Uninsured and publicly insured patients experienced significant delays during their orthopaedic care compared with commercially insured patients. However, no correlation was found between insurance status or household income and the rate of surgical interventions.
Conclusion:
Publicly insured and uninsured pediatric and college-aged patients faced significant barriers in accessing orthopaedic services, as demonstrated by substantially longer times between the initial injury and referral to an orthopaedic evaluation and surgery; however, these socioeconomic factors did not affect the rate of surgical management. Clinical competency regarding the effects of socioeconomic factors on the time to orthopaedic care and efforts to expedite care among underinsured and underserved children are vital for improving patient outcomes.
Keywords: meniscus, meniscal tear, sport injury, insurance status, socioeconomic factors, health care disparities
The incidence of traumatic meniscal injuries among youth is on the rise.14,26 Despite the increasing need for orthopaedic services among children, adolescents, and college-aged athletes in the United States, significant barriers remain in accessing these services. A nationwide survey in 2006 revealed that Medicaid-insured pediatric and adolescent patients have less access to orthopaedic surgeons compared to those with commercial insurance plans.19 In addition, pediatric and adolescent patients with noncommercial insurance plans often experience significant delays in anterior cruciate ligament (ACL) reconstruction, treatment of isolated fracture injuries, and spinal reconstructive surgery.2,4,6,11,17
Prompt management of traumatic meniscal tears is crucial. Delays in orthopaedic services often exacerbate these injuries at the time of clinical presentation and result in an increased indication for meniscectomy over repair.25 Meniscectomy often results in increased contact stresses and joint strain, contributing to early degenerative changes within the knee joint, and it is not a preferred modality for treating young patients.5,8 Furthermore, acutely repaired meniscal tears have demonstrated superior results compared with chronically repaired tears.23,25 Surgical treatment before the onset of progressive disease and meniscal degeneration decreases the likelihood of unfavorable subjective outcomes and radiographically detectable osteoarthritis.1,12,13,22 Although a specific timeline of repair has not been established, Sood et al21 demonstrated that patients with traumatic bucket-handle meniscal tears had a greater rate of successful repair when surgery was performed within 6 weeks of the injury.
Recently, health care discrepancies associated with socioeconomic factors have garnered increasing interest, as the health care community continues to recognize the importance of timely access to care on patient outcomes. The purpose of this study was to investigate the impact of insurance status and household income on rates of surgical management and time to evaluation and treatment of meniscal tears in patients ≤22 years of age.
Methods
Study Design and Patient Selection
After institutional review board approval, we conducted a retrospective chart review of all patients ≤22 years of age who were diagnosed with a meniscal tear between January 2008 and December 2016 within a single, large-volume academic health system. A query of medical records was performed using the appropriate International Classification of Diseases, Ninth and Tenth Revision (ICD-9 and -10, respectively) codes; only meniscal tears confirmed via magnetic resonance imaging and/or arthroscopic surgery were included. Excluded were patients referred to an orthopaedic surgeon outside of our health system, those receiving orthopaedic care through the juvenile detention system, patients with polytrauma and multiligamentous injuries (with the exception of concurrent isolated ACL injuries), and those without adequate data available for analysis.
Clinic notes and operative reports from the medical records were reviewed for each patient. Patients were divided into 3 groups based on their health insurance status: public, commercial, or uninsured/self-pay. Patients with public insurance included those covered by Medicaid, Medicare, or the Texas Children’s Health Insurance Program (CHIP). CHIP is a jointly funded program that provides low-cost medical coverage for children and pregnant women in families who cannot afford commercial insurance and do not qualify for Medicaid based on household income.
Patient characteristic data were recorded, including age, sex, self-reported race/ethnicity, zip code, type of meniscal tear (with respective ICD-9 or -10 code), type of elective surgery performed (meniscectomy vs repair), and postoperative complications. Patient ZIP code was used as a proxy for median household income, with values provided by the United States Census Bureau. Various time points during the health care cycle were recorded, including the dates of injury, referral to an orthopaedic service, initial evaluation by an orthopaedic surgeon, and surgery. Temporal relationships were analyzed between the time of referral and initial orthopaedic evaluation, orthopaedic evaluation and surgery, injury and orthopaedic evaluation, and injury and surgery. The impact of insurance status and household income on the rates of orthopaedic surgery was also explored.
Statistical Analysis
SAS software (SAS Institute) was used to analyze the rates of orthopaedic surgery and compare the time to evaluation and treatment for the public insurance, commercial insurance, and uninsured/self-pay groups. A negative binomial regression model was used to evaluate the association between insurance status and time to referral, clinic evaluation, and surgical management to account for overdispersion of the data. Logistic regression analysis was used to determine the socioeconomic factors predictive of delays in evaluation and treatment. A chi-square test was used to analyze the rates of surgical management among publicly insured, commercially insured, and uninsured patients and determine an association between surgical management and median household income. A P value ≤.05 was considered statistically significant.
Results
Patient Characteristics
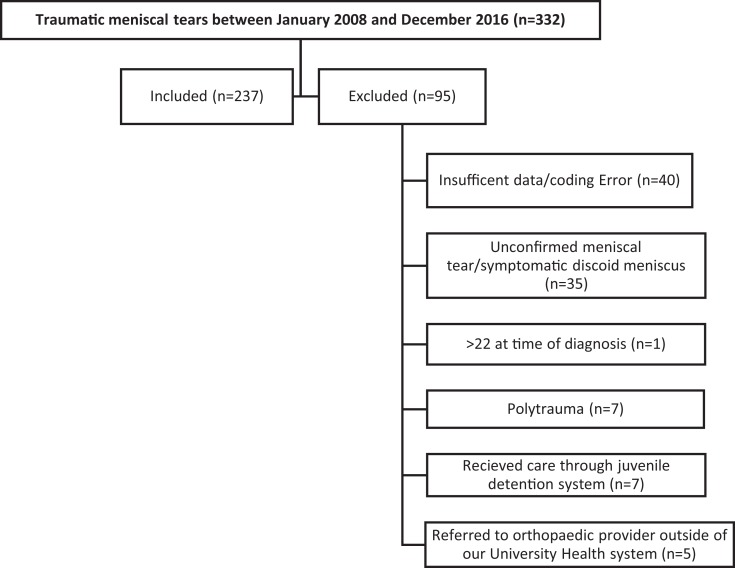
A total of 237 patients were included from the 332 patients diagnosed with a traumatic meniscal tear during the study period; a complete summary of patient enrollment is displayed in Figure 1, and patient characteristics are shown in Table 1. The study population consisted of 143 male (60.3%) and 94 female (39.7%) patients with a mean age at the time of diagnosis of 16.92 ± 2.72 years. A majority of patients in this study were white (89.5%) and Hispanic (73.8%). Furthermore, the majority of patients were covered by public insurance plans (n = 117, 49.4%), followed by commercial insurance plans (n = 63, 26.6%), and no insurance/self-pay (n = 57, 24.1%). The mean median household income of the study population was US$49,385 ± US$17,754. Surgery was the primary intervention and was performed in 83.9% of the patients; total or partial meniscectomy (56.1%) was performed more frequently than meniscal repair (38.9%) but with similar overall rates.
Figure 1.
Summary of patient enrollment.
TABLE 1.
Patient Characteristicsa
| Commercial Insurance | Public Insurance | Uninsured/Self-Pay | Total | |
|---|---|---|---|---|
| Overall | 63 (26.6) | 117 (49.4) | 57 (24.1) | 237 (100.0) |
| Sex | ||||
| Male | 38 (60.3) | 67 (57.3) | 38 (66.7) | 143 (60.3) |
| Female | 25 (39.7) | 50 (42.7) | 19 (33.3) | 94 (39.7) |
| Race | ||||
| Alaskan/Native American | 0 (0.0) | 1 (0.9) | 0 (0.0) | 1 (0.4) |
| Asian/Pacific Islander | 1 (1.6) | 0 (0.0) | 0 (0.0) | 1 (0.4) |
| Black | 7 (11.1) | 10 (8.6) | 4 (7.0) | 21 (8.9) |
| White | 55 (87.3) | 105 (89.7) | 52 (91.2) | 212 (89.5) |
| Other | 0 (0.0) | 1 (0.9) | 1 (1.8) | 2 (0.8) |
| Ethnicity | ||||
| Hispanic | 42 (66.7) | 86 (73.5) | 47 (82.5) | 175 (73.8) |
| Non-Hispanic | 21 (33.3) | 28 (23.9) | 9 (15.8) | 58 (24.5) |
| Unknown | 0 (0.0) | 3 (2.6) | 1 (1.7) | 4 (1.7) |
| Surgery | ||||
| Yes | 53 (85.5) | 97 (83.6) | 48 (82.7) | 198 (83.5) |
| No | 9 (14.5) | 18 (15.5) | 10 (17.3) | 37 (15.6) |
| Unknown | 0 (0.0) | 1 (0.9) | 0 (0.0) | 2 (0.8) |
| Type of surgery | ||||
| Total or partial meniscectomy | 29 (54.7) | 53 (54.6) | 29 (60.4) | 111 (56.1) |
| Meniscal repair | 20 (37.7) | 39 (40.2) | 18 (37.5) | 77 (38.9) |
| Trephination | 0 (0.0) | 2 (2.1) | 0 (0.0) | 2 (1.0) |
| Debridement only | 4 (7.6) | 3 (3.1) | 1 (2.1) | 8 (4.0) |
| Age at diagnosis, mean ± SD, y | 16.76 ± 2.77 | 16.05 ± 2.28 | 18.99 ± 2.55 | 16.92 ± 2.72 |
| Median household income, mean ± SD, US$ | 55,063 ± 22,949 | 46,648 ± 16,231 | 49,028 ± 12,671 | 49,385 ± 17,754 |
aData are shown as n (%) unless otherwise indicated.
Time to Referral and Orthopaedic Evaluation
The time from initial injury to orthopaedic referral by the primary care provider (PCP) or acute care provider was significantly prolonged for uninsured and publicly insured patients (χ2 = 19.145, P < .001) (Table 2). Those with commercial insurance plans obtained an orthopaedic referral within a mean of 9.11 ± 11.04 days after the meniscal injury. However, publicly insured and uninsured patients experienced a mean delay of 20.83 days (P < .001) and 68.00 days (P = .009), respectively, between the initial meniscal injury and referral to an orthopaedic surgeon.
TABLE 2.
Time to Referral, Evaluation, and Surgery Using Logistic Regression Analysisa
| Commercial Insurance | Public Insurance | Uninsured/Self-pay | P Value | |
|---|---|---|---|---|
| Injury to referral, d | 9.11 ± 11.04 | 20.83 ± 23.89 | 68.00 ± 115.92 | <.001 |
| Injury to evaluation, d | 13.71 ± 10.34 | 27.43 ± 27.01 | 64.71 ± 98.62 | <.0001 |
| Injury to surgery, d | 46.72 ± 26.76 | 67.97 ± 44.90 | 77.85 ± 102.29 | .05 |
| Referral to evaluation, d | 13.51 ± 15.30 | 17.64 ± 19.13 | 20.06 ± 27.45 | >.05 |
| Evaluation to surgery, d | 29.08 ± 21.87 | 50.95 ± 40.14 | 45.38 ± 127.00 | .0029 |
aData are shown as mean ± SD.
The mean time between referral and orthopaedic evaluation for all patients was 17.27 ± 20.90 days and ranged between 0 and 175 days. The mean time between referral and evaluation for patients with commercial insurance was 13.51 ± 15.30 days compared with 17.64 ± 19.13 days and 20.06 ± 27.45 days for publicly insured and uninsured patients, respectively. Although insurance status was not a significant predictor of time from referral to orthopaedic evaluation overall (P = .13), subgroup analysis revealed that uninsured patients demonstrated greater delays from referral to the orthopaedic evaluation compared to patients with commercial insurance (P = .04), although this difference was marginal. However, this same association was not found for patients with public insurance.
Insurance status was predictive of overall time from injury to orthopaedic evaluation (P < .0001), which ranged between 0 and 469 days and was a mean of 34.83 ± 59.31 days. The mean time between injury and orthopaedic evaluation for commercially insured, publicly insured, and uninsured patients was 13.71 ± 10.34, 27.43 ± 27.01, and 64.71 ± 98.62 days, respectively. The wait time between injury and evaluation for uninsured patients was 4.72-fold greater (95% CI, 2.62-8.51; P < .0001) than the wait time experienced by commercially insured patients. Similarly, patients with public insurance were found to have a 2.00-fold greater wait time to evaluation (95% CI, 1.16-3.44; P = .01) over patients with commercial insurance.
Time to Orthopaedic Surgery
Insurance status was also predictive of time from initial orthopaedic evaluation to orthopaedic surgery (χ2 = 11.72, P = .0029). The time between evaluation and surgery was 1.56-fold greater for uninsured patients (95% CI, 1.09-2.24; P = .01) and 1.75-fold greater for publicly insured patients (95% CI, 1.29-2.39; P < .001) compared with commercially insured patients. Furthermore, when examining the overall time between initial meniscal injury and orthopaedic surgery, we found that it was significantly higher for uninsured patients (odds ratio, 1.67 [95% CI, 1.10-2.53]; P = .01) versus patients with commercial insurance. However, we observed only a marginal difference for patients with public insurance versus patients with commercial insurance (odds ratio, 1.45 [95% CI, 0.00-0.75]; P = .04). Patients presented to surgery within a mean of 65.40 ± 63.59 days after the meniscal injury. Commercially insured, publicly insured, and uninsured patients presented to surgery at a mean of 46.72 ± 26.76, 67.97 ± 44.90, and 77.85 ± 102.29 days after the injury, respectively.
Although insurance status was a strong predictor of time to orthopaedic surgery, there was no evidence that electing to proceed with surgical management was associated with insurance status (P = .89). Of the 237 patients, 198 (83.5%) chose elective surgery. Of the 37 patients who decided not to proceed with surgical management, 48.6% were publicly insured (n = 18), 24.3% were commercially insured (n = 9), and 27.1% were uninsured (n = 10).
An association between median household income and the time to evaluation and treatment or the rate of surgical management was not established. Median household income data were available for 234 patients and were not found to be a significant factor in the time to referral, evaluation by an orthopaedic surgeon, or surgery (P > .05).
Discussion
The timely evaluation and treatment of meniscal tears among youth is essential to avoid the further exacerbation of knee injuries and restore knee stability.15 In this study, children, adolescents, and college-aged athletes experienced significant differences in time to orthopaedic evaluation after a meniscal injury depending on their medical insurance. Furthermore, publicly insured and uninsured patients experienced significant delays to orthopaedic surgery, although the decision to pursue elective surgery was ultimately not influenced by insurance type. Prior studies have demonstrated similar delays in young patients presenting with ACL tears; both Newman et al15 and Pierce et al17 demonstrated that adolescents with noncommercial insurance plans had longer wait times for ACL reconstruction. Similarly, Kocher et al10 demonstrated that Medicaid patients had a significantly longer median time from symptom onset to the diagnosis of slipped capital femoral epiphysis compared to patients with commercial insurance plans (12 weeks vs 7.5 weeks, respectively).
The time from injury to orthopaedic referral represents the earliest point during the treatment course, as the patient initially presents to the PCP, an acute care provider, or a hospital emergency department after a meniscal injury. In this study, the cause of timing delays experienced during this period appears to be multifactorial; underinsured patients are more likely to forego or alter a treatment course because of their inability to pay.24 Sabharwal et al18 found that pediatric patients with Medicaid were more likely to visit another health care facility for an orthopaedic condition before presenting to a university hospital’s emergency department. Additionally, in Texas, the requirement for Medicaid, Medicare, and CHIP patients to have a PCP referral to see an orthopaedic surgeon represents a potential barrier to care; underinsured patients are more likely to have limited resources for obtaining and attending medical appointments with their PCP and may not be able to obtain an orthopaedic referral. Furthermore, Wiznia et al27 found that the requirement for a PCP referral was more likely to be placed on Medicaid patients than on patients with commercial insurance.
Regarding the overall time from injury to orthopaedic evaluation, both uninsured and publicly insured patients experienced significant delays compared with commercially insured patients (P < .0001). A potential explanation for this delay includes patient-specific factors in addition to provider reluctance in providing care for patients with public insurance plans. In Texas, private orthopaedic practices frequently refuse to provide care for patients with Medicaid, Medicare, or CHIP, resulting in additional visits to orthopaedic offices before presentation to our university health system’s pediatric orthopaedics department. The reasons for low Medicaid and Medicare acceptance rates in private orthopaedic offices are multifaceted; low reimbursement rates, the increased complexity of cases, and the perceived hassle exhibited by cumbersome administrative duties have been cited as major factors contributing to provider reluctance and ultimately refusal.7,9,16,20
The fact that insurance status did not significantly affect the time from orthopaedic referral to the initial orthopaedic evaluation (P = .13) suggests that once patients were referred to an orthopaedic provider, they were able to be seen by an orthopaedic surgeon without significant delays related to insurance plans. This observation supports the conclusion that patient-specific circumstances—including but not limited to transportation, financial or work-related obligations, and perceived medical necessity of orthopaedic treatment—are vital factors contributing to the overall delay experienced from injury to surgery. These patients are taking longer to present to their PCP, acute care provider, or emergency department, ultimately delaying the process to obtain an orthopaedic referral.
The consequences of treatment delays for ligamentous knee injuries are known. Prior studies have demonstrated the association between the delayed surgical treatment of ACL tears among youth and an increased incidence of irreparable meniscal tears and chondral injuries at the time of reconstruction.3,6,25 Similarly, irreparable meniscal tears have been found to be more common in patients with public insurance.25 These findings are potentially related to the delays in care that underinsured pediatric and young adult patients often experience. Chronic meniscal tears are less amenable to repair and are more likely to require meniscal excision, ultimately predisposing young patients to early-onset knee osteoarthritis.1,5,12,21–23 The optimal timing for acute meniscal repair within the pediatric population has not yet been established; however, bucket-handle meniscal tears require time-sensitive surgery, with a higher success rate for patients who undergo surgery within 6 weeks after the injury.20 In adults, the 91% success rate for patients undergoing meniscal repair within 3 months reduces to 58% if undergoing surgery more than 3 months after the injury.23 Finally, despite the delays experienced by these patients, insurance status or household income was not correlated to the rate of surgical management.
Delayed access to orthopaedic services for various musculoskeletal injuries decreases the quality and value of the orthopaedic care provided.6 Several studies have demonstrated a delay in the treatment of orthopaedic injuries among youth covered by various forms of public insurance and have confirmed the unmet health care needs of underinsured patients. The results of this study add to the current knowledge regarding barriers faced by underinsured and uninsured pediatric and young adult patients in receiving proper health care, particularly with orthopaedic sport injuries.
The strengths of this study include the collection of data from a large population from a level I trauma center within a single university health system. This is the first study of its kind that we are aware of that strictly focuses on meniscal tears in American children, adolescents, and college-aged patients (≤22 years of age). The study was limited by its retrospective nature and was subject to possible selection bias, as all data were collected at a single academic institution. We were unable to ask patients and their families about specific factors representing barriers to care. Furthermore, because the majority of the patients in this study were of a single race (89.5% white) and ethnicity (73.8% Hispanic), the impact of additional socioeconomic factors on orthopaedic care within other underrepresented populations could not be determined. The generalization of insurance status into public, commercial, and uninsured/self-pay groups was also not ideal; further studies analyzing treatment timing based on a specific insurance type would be favorable. Furthermore, patient ZIP code was used as a proxy for median household income, which may not be considered an ideal method to measure socioeconomic status.
Despite these shortcomings, these data once again demonstrate the significant differences experienced by young patients in attaining access to orthopaedic care depending on their insurance type. Further studies examining the impact of insurance status and delays to care on clinical outcomes in young American patients with meniscal tears would be beneficial to elucidate the health disparities of this population. The next step for this study would be to determine if differences in intraoperative abnormalities are associated with insurance type and delays in the time to evaluation and treatment of acute meniscal injuries.
Footnotes
The authors have declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the University of Texas at San Antonio Institutional Review Board (protocol No. HSC20170432 H).
References
- 1. Aglietti P, Zaccherotti G, De Biase P, Taddei I. A comparison between medial meniscus repair, partial meniscectomy, and normal meniscus in anterior cruciate ligament reconstructed knees. Clin Orthop Relat Res. 1994;307:165–173. [PubMed] [Google Scholar]
- 2. Alosh H, Riley LH, 3rd, Skolasky RL. Insurance status, geography, race, and ethnicity as predictors of anterior cervical spine surgery rates and in-hospital mortality: an examination of United States trends from 1992 to 2005. Spine (Phila Pa 1976). 2009;34:1956–1962. [DOI] [PubMed] [Google Scholar]
- 3. Anderson AF, Anderson CN. Correlation of meniscal and articular cartilage injuries in children and adolescents with timing of anterior cruciate ligament reconstruction. Am J Sports Med. 2014;43(2):275–281. [DOI] [PubMed] [Google Scholar]
- 4. Archdeacon MT, Simon PM, Wyrick JD. The influence of insurance status on the transfer of femoral fracture patients to a level-I trauma center. J Bone Joint Surg Am. 2007;89:2625–2631. [DOI] [PubMed] [Google Scholar]
- 5. Baratz ME, Fu FH, Mengato R. Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee. A preliminary report Am J Sports Med. 1986;14:270–275. [DOI] [PubMed] [Google Scholar]
- 6. Dumont GD, Hogue GD, Padalecki JR, Okoro N, Wilson PL. Meniscal and chondral injuries associated with pediatric anterior cruciate ligament tears relationship of treatment time and patient-specific factors. Am J Sports Med. 2012;40:2128–2133. [DOI] [PubMed] [Google Scholar]
- 7. Friedman AB, Saloner B, Hsia RY. No place to call home: policies to reduce ED use in Medicaid. N Engl J Med. 2015;372:2382–2385. [DOI] [PubMed] [Google Scholar]
- 8. Fukubayashi T, Kurosawa H. The contact area and pressure distribution pattern of the knee: a study of normal and osteoarthrotic knee joints. Acta Orthop Scand. 1980;51:871–879. [DOI] [PubMed] [Google Scholar]
- 9. Hinman A, Bozic K. Impact of payer type on resource utilization, outcomes and access to care in total hip arthroplasty. J Arthroplasty. 2008;23(6 Suppl 1):9–14. [DOI] [PubMed] [Google Scholar]
- 10. Kocher MS, Bishop JA, Weed B, et al. Delay in diagnosis of slipped capital femoral epiphysis. Pediatrics. 2004;113(4):e322–e325. [DOI] [PubMed] [Google Scholar]
- 11. Lawrence JTR, Argawal N, Ganley TJ. Degeneration of the knee joint in skeletally immature patients with a diagnosis of an anterior cruciate ligament tear: is there harm in delay of treatment? Am J Sports Med. 2011;39:2582–2587. [DOI] [PubMed] [Google Scholar]
- 12. Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med. 2007;35:1756–1769. [DOI] [PubMed] [Google Scholar]
- 13. Manzione M, Pizzutillo PD, Peoples AB, Schweizer PA. Meniscectomy in children: a long-term follow-up study. Am J Sports Med. 1983;11:111–115. [DOI] [PubMed] [Google Scholar]
- 14. Mitchell J, Graham W, Best TM, et al. Epidemiology of meniscal injuries in US high school athletes between 2007 and 2013. Knee Surg Sports Traumatol Arthrosc. 2015;24(3):715–722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Newman JT, Carry PM, Terhune EB, et al. Delay to reconstruction of the adolescent anterior cruciate ligament: the socioeconomic impact on treatment. Orthop J Sports Med. 2014;2(8):2325967114548176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Perloff JD, Kletke P, Fossett JW. Which physicians limit their Medicaid participation, and why. Health Serv Res. 1995;30:7–26. [PMC free article] [PubMed] [Google Scholar]
- 17. Pierce TR, Mehlman CT, Tamai J, Skaggs DL. Access to care for the adolescent anterior cruciate ligament patient with Medicaid versus private insurance. J Pediatr Orthop. 2012;32:245–248. [DOI] [PubMed] [Google Scholar]
- 18. Sabharwal S, Zhao C, McClemens E, Kaufmann A. Pediatric orthopaedic patients presenting to a university emergency department after visiting another emergency department: demographics and health insurance status. J Pediatr Orthop. 2007;27:690–694. [DOI] [PubMed] [Google Scholar]
- 19. Skaggs DL, Clemens SM, Vitale MG, Femino JD, Kay RM. Access to orthopaedic care for children with Medicaid versus private insurance in California. Pediatrics. 2001;107(6):1405–1408. [DOI] [PubMed] [Google Scholar]
- 20. Sommers BD. Health care reform’s unfinished work: remaining barriers to coverage and access. N Engl J Med. 2015;373:2395–2397. [DOI] [PubMed] [Google Scholar]
- 21. Sood A, Gonzalez-Lomas G, Gehrmann R. Influence of health insurance status on the timing of surgery and treatment of bucket-handle meniscus tears. Orthop J Sports Med. 2015;3(5):2325967115584883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Stein T, Mehling AP, Welsch F, von Eisenhart-Rothe R, Jager A. Long-term outcome after arthroscopic meniscal repair versus arthroscopic partial meniscectomy for traumatic meniscal tears. Am J Sports Med. 2010;38:1542–1548. [DOI] [PubMed] [Google Scholar]
- 23. Venkatachalam S, Godsiff S, Harding M. Review of the clinical results of arthroscopic meniscal repair. Knee. 2001;8(2):129–133. [DOI] [PubMed] [Google Scholar]
- 24. Weiner S. “I can’t afford that!”: dilemmas in the care of the uninsured and underinsured. J Gen Intern Med. 2001;16(6):412–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Williams AA, Mancini NS, Solomito MJ, Nissen CW, Milewski MD. Chondral injuries and irreparable meniscal tears among adolescents with anterior cruciate ligament or meniscal tears are more common in patients with public insurance. Am J Sports Med. 2017;45(9):2111–2115. [DOI] [PubMed] [Google Scholar]
- 26. Wilson PL, Wyatt CW, Romero J, Sabatino MJ, Ellis HB. Incidence, presentation, and treatment of pediatric and adolescent meniscal root injuries. Orthop J Sports Med. 2018;6(11):2325967118803888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wiznia DH, Nwachuku E, Roth A, et al. The influence of medical insurance on patient access to orthopaedic surgery sports medicine appointments under the Affordable Care Act. Orthop J Sports Med. 2017;5(7):2325967117714140. [DOI] [PMC free article] [PubMed] [Google Scholar]