Abstract
Introduction: Preexposure prophylaxis (PrEP) is an effective biomedical intervention that has the potential to dramatically decrease the incidence of HIV but remains an underutilized method of HIV prevention. The Philadelphia Department of Public Health administered an online survey to health care providers in the Philadelphia area with the aim of characterizing PrEP attitudes, knowledge, and prescribing practices. Methods: Online surveys were distributed to 1000 providers who were recruited through distribution lists of Philadelphia medical providers between September and December 2017. A Likert-type response scale was utilized to analyze participant self-reported responses. Participant practice settings included HIV/ID, family and internal medicine, women’s health, and pediatric/adolescent clinics. Results and Discussion: The response rate of the survey was 9%. Of 81 complete responses, 75% (N = 61) felt comfortable providing PrEP and 77% (N = 62) had ever written a PrEP prescription. Compared with primary care providers, HIV care providers were significantly more knowledgeable about required laboratory testing for prescribing PrEP (P = .03) and were more likely to have prescribed PrEP to more than 10 patients (P = .006). Women’s health and pediatric providers reported feeling less comfortable providing PrEP to their patients (P = .0003). Conclusion: The majority of health care providers in the Philadelphia area who responded to the survey reported experience with providing PrEP to their patients. In the present study, HIV care providers were significantly more comfortable and knowledgeable about prescribing PrEP compared with providers in primary care, women’s health, and/or adolescent/pediatric medicine. Results were limited by sampling bias, as providers who responded to the survey may have prior experience with PrEP. Future Health Department educational trainings need to target primary and preventive care providers, providers who have never prescribed PrEP, and providers who see few patients living with HIV.
Keywords: preexposure prophylaxis, HIV care providers, primary care, HIV prevention
Introduction
HIV preexposure prophylaxis (PrEP) was first approved by the Food and Drug Administration (FDA) in 2012 and is effective in preventing HIV in individuals who are vulnerable to HIV transmission. Despite the fact that multiple clinical trials have demonstrated PrEP efficacy in preventing HIV transmission when taken daily as prescribed, with relatively few side effects, PrEP is an underutilized method of HIV prevention in the United States.1 The Centers for Disease Control and Prevention (CDC) estimates that 1.2 million individuals are eligible for PrEP based on sexual and/or drug use behaviors, yet the total number of people using PrEP in the United States is approximately 225 000.2 A multicity survey (Philadelphia, Houston, Detroit, Atlanta, and Washington, DC) conducted in 2014 found that Philadelphia had one of the lowest PrEP usage rates (0.5%) among persons facing the greatest risk: black men and transgender women who have sex with men.3 PrEP has shown significant effectiveness in reducing HIV transmission and holds great promise for increasing community-level protection, particularly in cities like Philadelphia where the prevalence of HIV is high at 1.2%.4
Success of the scale up and adoption of PrEP requires that health care providers are aware of PrEP, knowledgeable to discuss it with their patients, and comfortable prescribing it. Previous studies examining PrEP prescriber comfort have found that common perceived barriers are the assumed time-consuming process of prescribing PrEP,5 insufficient clinical capacity,6 and insurance concerns and potential cost to patients.7 Providers have reported concerns prescribing PrEP to patients who report low medication adherence and the potential for drug resistance.8,9 Additionally, provider discomfort with taking a comprehensive sexual history or difficulty determining PrEP patient eligibility are limitations that prevent adoption of PrEP.10,11 Provider discomfort prescribing PrEP presents a major barrier to PrEP access.
Primary care providers (PCPs) are uniquely positioned to identify patients who are eligible for PrEP as they may serve HIV uninfected patients who are vulnerable to HIV acquisition.12 Because of a lack of awareness of PrEP and a low prevalence of PrEP prescriptions written by these medical providers, there are missed opportunities for engaging persons vulnerable to HIV along the PrEP continuum.13,14 Our study sought to examine Philadelphia health care providers’ knowledge and attitudes, prescribing practices, and self-reported comfort level with PrEP in order to identify potential areas of training and capacity building.
Methods
Respondents and Procedures
The survey was administered by the Philadelphia Department of Public Health (PDPH) AIDS Activities Coordinating Office (AACO) and was conducted through an online platform from September to December 2017. One email reminder was sent 2 months after initial survey; no compensation was provided. Survey participants were recruited through the Philadelphia County Medical Society distribution list and a PDPH HIV provider listserv. Both lists included HIV/ID specialists, family medicine, internal medicine, women’s health, and pediatric/adolescent providers, who were mainly physicians, and also included nurse practitioners and physician assistants. Recruitment emails included a brief description of the survey and were sent to 1000 providers. Study questions characterized the sample through identifying health care setting type, number of patients with HIV cared for, and knowledge of PrEP eligibility criteria. Questions asked respondents to rate their comfort level discussing HIV risk factors and prescribing PrEP (Figure 1).
Figure 1.
Questions assessing preexposure prophylaxis (PrEP) prescribing comfort and experience.
Statistical Analysis
Respondents were anonymous and results were analyzed based on aggregate data. The analysis focused on the respondents answer to the question “Do you feel comfortable prescribing PrEP to your patients?” on a Likert-type scale of “Strongly Disagree” to “Strongly Agree.” For the purpose of this assessment, respondents who had answered “Strongly Disagree,” “Disagree,” or “No Opinion or Uncertain” were considered to feel “Not Comfortable” and respondents who had answered “Agree” or “Strongly Agree” were considered to feel “Comfortable” prescribing PrEP.
The analysis was done using χ2 tests to describe differences in sample demographics between providers who were and were not comfortable prescribing PrEP. Similarly, χ2 tests were used to identify differences along the PrEP continuum between HIV care providers and non-HIV care providers. All statistical tests were completed using SAS 9.4.
Ethics Statement
The study received institutional review board approval from the Philadelphia Department of Public Health.
Results and Discussion
Characteristics of the Study Population
Of 1000 potential respondents, there was a 9% response rate. Of the 87 respondents, 6 were excluded based on incomplete or missing survey responses leaving a total of 81 eligible participants. The majority of participants were family/internal medicine physicians (48%) and HIV/infectious disease specialist (31%). Respondents included 8 nurse practitioners and physician assistants. The sample was evenly distributed in terms of age, gender, and years practicing; 53% (n = 43) were female, 63% (n = 51) were younger than 50 years, and 60% (n = 49) had been practicing medicine for over 10 years. Demographics, including professional and clinical practice type, are shown in Table 1.
Table 1.
Participant Demographics.
| Total |
||
|---|---|---|
| n | Column % | |
| Total (81) | 81 | 100 |
| Gender | ||
| Female | 43 | 53 |
| Male | 38 | 47 |
| Age group (years) | ||
| 25-34 | 25 | 31 |
| 35-50 | 26 | 32 |
| 51+ | 30 | 37 |
| Years practicing (n = 79) | ||
| <5 | 14 | 17 |
| 5-9 | 16 | 20 |
| ≥10 | 49 | 60 |
| Provider type | ||
| Physician | 73 | 90 |
| Physician assistant/nurse practitioner | 8 | 10 |
| Practice type | ||
| Family/internal medicine | 39 | 48 |
| HIV/infectious specialist disease | 25 | 31 |
| Pediatrician/adolescent medicine | 9 | 11 |
| Women’s health | 5 | 6 |
| Other | 3 | 4 |
| HIV/infectious disease specialist | ||
| Yes | 25 | 31 |
| No | 56 | 69 |
Provider Comfort of Prescribing PrEP
The majority of providers (76%) felt comfortable prescribing PrEP to their patients. There were no significant differences in the providers who were comfortable and those who were not comfortable prescribing PrEP in terms of gender, age, and years practicing medicine (Table 2). More than half of the providers (58%, n = 47) had cared for more than 50 HIV patients ever, and those providers who had cared for more than 50 HIV patients were significantly more likely to feel comfortable in prescribing PrEP (P = .0003).
Table 2.
Preexposure Prophylaxis (PrEP) Prescribing Indicators by Provider Comfort Level.
| Not Comfortable |
Comfortable |
Total |
||||
|---|---|---|---|---|---|---|
| n | Row % | n | Row % | n | Column % | |
| Total (81) | 20 | 25 | 61 | 75 | 81 | 100 |
| Practice typea (P = .0003) | ||||||
| Family/internal medicine | 6 | 15 | 33 | 85 | 39 | 48 |
| HIV/infectious disease specialist | 3 | 12 | 22 | 88 | 25 | 31 |
| Pediatrician/adolescent medicine | 7 | 78 | 2 | 22 | 9 | 11 |
| Women’s health | 3 | 60 | 2 | 40 | 5 | 6 |
| Other | 1 | 33 | 2 | 67 | 3 | 4 |
| Number of HIV patients evera (P = .0003) | ||||||
| 1-50 | 16 | 44 | 18 | 56 | 34 | 42 |
| ≥50 | 4 | 9 | 43 | 91 | 47 | 58 |
| Provider initiated PrEP discussiona (P < .0001) | ||||||
| No | 9 | 69 | 4 | 31 | 13 | 16 |
| Yes | 11 | 16 | 57 | 84 | 68 | 84 |
| Ever prescribed PrEPa (P < .0001) (n = 77) | ||||||
| I have prescribed and/or currently prescribe PrEP for HIV prevention | 4 | 7 | 55 | 93 | 59 | 77 |
| I refer patients to other providers who prescribe PrEP | 5 | 56 | 4 | 44 | 9 | 12 |
| I will not prescribe PrEP to my patients | 1 | 100 | 0 | 0 | 1 | 1 |
| With more education and training, I would prescribe PrEP | 6 | 75 | 2 | 25 | 8 | 10 |
| Number of PrEP prescriptionsa (P < .0001) | ||||||
| 0 | 14 | 74 | 5 | 26 | 19 | 23 |
| 1-5 | 4 | 20 | 16 | 80 | 20 | 25 |
| 6-20 | 2 | 7 | 27 | 93 | 29 | 36 |
| >20 | 0 | 0 | 13 | 100 | 13 | 16 |
Chi-square P value <.05.
Providers from family/internal medicine and HIV/infectious disease specialist were more likely to feel comfortable prescribing PrEP than providers who were in pediatrics/adolescent medicine or women’s health (P = .0003). Those providers who were comfortable providing PrEP were more likely to have their patients ask them about PrEP (P < .0001), more likely to have initiated a PrEP discussion with their patients (P < .0001), and were more likely to have prescribed PrEP (P < .0001). Of those uncomfortable prescribing PrEP, 30% (n = 6) were family/internal medicine, 35% (n = 7) were pediatric/adolescent medicine, and 15% (n = 3) were women’s health providers.
PrEP Prescribing Continuum
Providers were asked about their familiarity and comfort with PrEP prescribing indicators and clinical protocols. The questions were asked using a Likert-type scale of “Strongly Disagree” to “Strongly Agree.”
Provider responses based on comfort were used to create the PrEP prescribing continuum (Figure 2). For the purpose of the PrEP prescribing continuum, the categories of pediatric/adolescent medicine, women’s health, and family/internal medicine were collapsed into the category of “Non-HIV Provider” There was a significant difference between HIV/infectious disease specialist and Non-HIV Providers in the categories of being knowledgeable about required labs (P = .03) and of a history of prescribing PrEP to more than 10 patients (P = .006).
Figure 2.
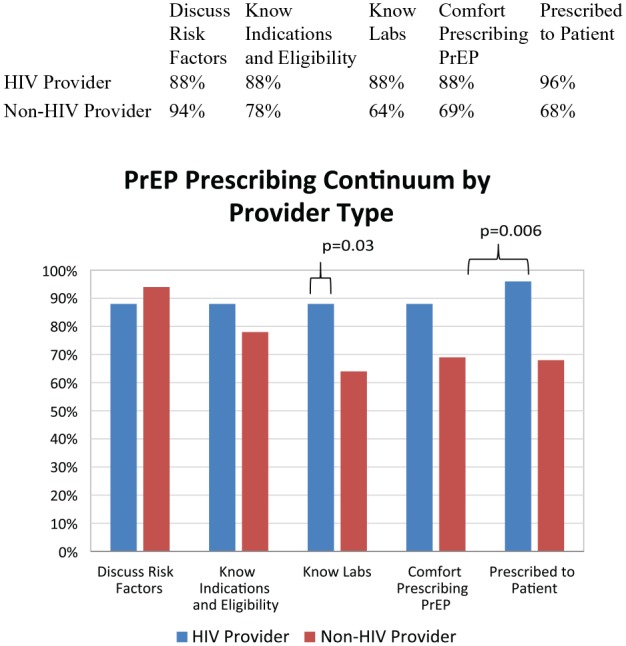
Preexposure (PrEP) prophylaxis prescribing continuum, by provider type.
Consistent with previous studies, we found that HIV providers who cared for more than 50 persons living with HIV were more likely than non-HIV providers to be comfortable in prescribing PrEP to their patients.1,15 The PrEP prescribing continuum illustrates that a significantly higher proportion of HIV specialists had prescribed PrEP to their patients and were knowledgeable about required labs compared with non-HIV providers. These providers may be more aware of and able to identify HIV risk factors in HIV-negative patients.
When the provider types were disaggregated, results of PrEP comfort varied by practice type. Over three-fourths (77%) of pediatric/adolescent medicine providers felt uncomfortable prescribing PrEP to their patients, which was consistent with previous surveys in which providers felt less comfortable prescribing PrEP to adolescents due to concerns about confidentiality, legality of prescriptions without parental consent, and high costs of PrEP medication.16,17 Similarly, 60% of surveyed women’s health providers felt uncomfortable prescribing PrEP. Family planning and women’s health providers have an opportunity to discuss HIV/sexually transmitted infection prevention and screening with their patients, yet only 4% of family planning/women’s health providers surveyed in other studies had ever prescribed PrEP to their patients.18 With an estimated 624,000 heterosexual persons having risks of acquiring HIV consistent with indicators for PrEP,19 it would be beneficial to include family planning and women’s health providers in future PrEP educational programs.
There are limitations to this study. Recruitment for the survey was a convenience sample and inherently biased, as providers who see HIV patients and have preexisting knowledge about PrEP may be more willing to respond to a survey on PrEP. The survey attained a low response rate and we were unable to compare characteristics of surveyed providers with nonresponders to assess response bias. Although we received a lower response rate from adolescent medicine and women’s health providers than HIV care providers and primary care providers, we were able to characterize potential PrEP prescribers, which will help inform future opportunities for training and education that build on PrEP prescribing comfort.
Reducing the rate of new HIV transmissions will require a broad and diverse dissemination of PrEP. Addressing provider concerns and perceived barriers through educational efforts is a critical component to increasing PrEP prescribing comfort amongst a diverse set of providers.
Conclusions
In summary, this study found there is variation in comfort and experience in prescribing PrEP across provider types. Of those surveyed, HIV care providers were significantly more likely to report experience and knowledge in prescribing PrEP compared with providers in primary care, women’s health, and/or adolescent/pediatric medicine. It would be beneficial to include family planning and women’s health providers in future PrEP educational programs, as this is a population whose risks for HIV may be unrecognized.19 In order to grow broad and diverse dissemination of PrEP, non-HIV providers must be aware of the efficacy of PrEP and be prepared to integrate conversations about sexual health, HIV prevention, and PrEP into routine preventive health care to raise awareness among patients about PrEP availability.
Acknowledgments
We thank the Philadelphia Department of Public Health for their assistance. We thank the Philadelphia County Medical Society for their contribution of a county medical provider listserv. We thank the Arizona Department of Health Services for their permission to adapt their questions from PrEP provider attitude survey.
Footnotes
Author Contributions: EA designed the study. MC and EA were involved in data collection. TN and KAB conducted the analysis. All authors contributed to the writing of the manuscript. All authors have read and approved the manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Erika Aaron  https://orcid.org/0000-0003-0757-2338
https://orcid.org/0000-0003-0757-2338
References
- 1. Petroll AE, Walsh JL, Owczarzak JL, McAuliffe TL, Bogart LM, Kelly JA. PrEP awareness, familiarity, comfort, and prescribing experience among US Primary Care Providers and HIV Specialists. AIDS Behav. 2017;21:1256-1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fitch L, Clancy J, Donaldson E, Gardiner E, Warren M. Tracking global oral PrEP provision: the who, what and where of oral PrEP. Paper presented at: HIV Research for Prevention Conference (HIVR4P 2018); October 23, 2018, Madrid, Spain. [Google Scholar]
- 3. Eaton LA, Matthews DD, Driffin DD, Bukowski L, Wilson PA, Stall RD; POWER Study Team. A multi-US city assessment of awareness and uptake of pre-exposure prophylaxis (PrEP) for HIV prevention among black men and transgender women who have sex with men. Prev Sci. 2017;18:505-516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nnomulu C, Brady K, Miller M, Nassau T. AIDS Activities Coordinating Office Surveillance Report: HIV in Philadelphia 2016. Philadelphia, PA: Philadelphia Department of Public Health; 2017. https://www.phila.gov/health/pdfs/aaco/HIV%20Surveillance%20Report-2016web.pdf. Accessed September 9, 2019. [Google Scholar]
- 5. Karris MY, Beekmann SE, Mehta SR, Anderson CM, Polgreen PM. Are we prepped for preexposure prophylaxis (PrEP)? Provider opinions on the real-world use of PrEP in the United States and Canada. Clin Infect Dis. 2014;58:704-712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Arnold EA, Hazelton P, Lane T, et al. A qualitative study of provider thoughts on implementing pre-exposure prophylaxis (PrEP) in clinical settings to prevent HIV infection. PLoS One. 2012;7:e40603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wood BR, McMahan VM, Naismith K, Stockton JB, Delaney LA, Stekler JD. Knowledge, practices, and barriers to HIV pre-exposure prophylaxis (PrEP) prescribing among Washington State Medical Providers. Sex Transm Dis. 2018;45:452-458. [DOI] [PubMed] [Google Scholar]
- 8. Blumenthal J, Jain S, Krakower D; The CCTG 598 Team, , et al. Knowledge is Power! Increased provider knowledge scores regarding pre-exposure prophylaxis (PrEP) are associated with higher rates of PrEP prescription and future intent to prescribe PrEP. AIDS Behav. 2015;19:802-810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Castel AD, Feaster DJ, Tang W, et al. Understanding HIV care provider attitudes regarding intentions to prescribe PrEP. J Acquir Immune Defic Syndr. 2015;70:520-528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bartram L, Chiosi J, Varley C, Halperin J. Let’s talk about sex: improving the adoption of pre-exposure prophylaxis by internal medicine resident physicians in New Orleans. Open Forum Infect Dis. 2017;4(suppl 1):S446. [Google Scholar]
- 11. Calabrese SK, Magnus M, Mayer KH, et al. Putting PrEP into practice: lessons learned from early-adopting US providers’ firsthand experiences providing HIV pre-exposure prophylaxis and associated care. PLoS One. 2016;11:e0157324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Silapaswan A, Krakower D, Mayer KH. Pre-exposure prophylaxis: a narrative review of provider behavior and interventions to increase PrEP implementation in primary care. J Gen Intern Med. 2017;32:192-198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Smith DK, Mendoza MC, Stryker JE, Rose CE. PrEP awareness and attitudes in a National Survey of Primary Care Clinicians in the United States, 2009-2015. PLoS One. 2016;11:e0156592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tellalian D, Maznavi K, Bredeek UF, Hardy WD. Pre-exposure prophylaxis (PrEP) for HIV infection: results of a survey of HIV healthcare providers evaluating their knowledge, attitudes, and prescribing practices. AIDS Patient Care STDs. 2013;27:553-559. [DOI] [PubMed] [Google Scholar]
- 15. Blackstock OJ, Moore BA, Berkenblit GV, et al. A cross-sectional online survey of HIV pre-exposure prophylaxis adoption among primary care physicians. J Gen Intern Med. 2017;32:62-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mullins TL, Zimet G, Lally M, Kahn JA. Adolescent human immunodeficiency virus care providers’ attitudes toward the use of oral pre-exposure prophylaxis in youth. AIDS Patient Care STDs. 2016;30:339-348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mullins TL, Zimet G, Lally M, Xu J, Thornton S, Kahn JA. HIV care providers’ intentions to prescribe and actual prescription of pre-exposure prophylaxis to at-risk adolescents and adults. AIDS Patient Care STDs. 2017;31:504-516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Seidman D, Carlson K, Weber S, Witt J, Kelly PJ. United States family planning providers’ knowledge of and attitudes towards preexposure prophylaxis for HIV prevention: a national survey. Contraception. 2016;93:463-469. [DOI] [PubMed] [Google Scholar]
- 19. Smith DK, van Handel M, Wolitski RJ, Stryker JE, Hall HI, Prejean J, et al. Vital signs: estimated percentages and numbers of adults with indications for preexposure prophylaxis to prevent HIV acquisition—United States, 2015. MMWR Morb Mortal Wkly Rep. 2015;64:1291-1295. [DOI] [PubMed] [Google Scholar]