Abstract
Background
First-pass recanalization via mechanical thrombectomy (MT) has been associated with improved clinical outcome in patients with acute ischaemic stroke. The optimal approach to achieve first-pass effect (FPE) remains unclear. No study has evaluated angiographic features associated with the achievement of FPE. We aimed to determine the procedural approaches and angiographic signs that may predict FPE.
Methods
We performed a prospective, multi-centre, observational study of FPE in patients with anterior circulation stroke treated with MT between February and June 2017. MTs were performed using different devices, deployment manoeuvres (standard versus ‘Push and Fluff’ technique), proximal balloon guide catheter (PBGC), distal aspiration catheter (DAC) or both. The angiographic clot protrusion sign (ACPS) was recorded. Completed FPE (cFPE) was defined as a modified thrombolysis in cerebral infarction score of 2c–3. Associations were sought between cFPE and procedural approaches and angiographic signs.
Results
A total of 193 patients were included. cFPE was achieved in 74 (38.3%) patients. The use of the push and fluff technique (odds ratio (OR) 3.45, 95% confidence interval (CI): 1.28–9.29, p = 0.010), PBGC (OR 3.81, 95% CI: 1.41–10.22, p = 0.008) and ACPS (OR 4.71, 95% CI: 1.78–12.44, p = 0.002) were independently associated with cFPE. Concurrence of these three variables led to cFPE in 82 vs 35% of the remaining cases (p = 0.002).
Conclusions
The concurrence of the PBGC, the push and fluff technique, and the ACPS was associated with the highest rates of cFPE. Appropriate selection of the thrombectomy device and deployment technique may lead to better procedural outcomes. ACPS could be used to assess clot integration strategies in future trials.
Keywords: Stroke, mechanical thrombectomy, stent retriever, aspiration catheter, angiography
Introduction
Mechanical thrombectomy (MT) is considered standard care for patients with acute ischaemic stroke due to proximal artery occlusion.1 Several studies have demonstrated that achieving complete recanalization with the fewest number of passes is associated with improved clinical outcome.2–4 Currently, there is an ongoing debate on the importance of achieving a successful recanalization with a single pass. The first-pass effect (FPE) was recently proposed as a new success measure for stroke thrombectomy devices, defined as complete revascularization of the occluded artery and its downstream territory with a single pass.5 FPE has been associated with better clinical outcomes and lower mortality rates compared to non-FPE controls,5 which may be related to reduced procedural time and periprocedural complications such as arterial endothelial injury. Several approaches have been shown to improve revascularization and clinical outcomes, including the use of a balloon guide catheter5–7 or aspiration catheter.8–9 Additionally, the ‘push and fluff’ manoeuvre, a technique for maximum device deployment, has been associated with higher rates of successful FPE compared to standard unsheathing.10 The optimal procedural approach to increase the first-pass recanalization rate remains unclear, and no single study has ever evaluated angiographic imaging as a parameter to measure the achievement of successful first-pass recanalization. Therefore, we aimed to determine the procedural approaches and angiographic signs that may predict the achievement of FPE.
Methods
Patient selection
We performed a prospective, multi-centre, observational registry study of FPE in patients with large vessel occlusion of the anterior circulation treated with MT between February and June 2017. Five high-volume Comprehensive Stroke Centres in Spain participated in the study. Only data related to the first pass of MT were prospectively collected immediately after the procedure. Demographic and clinical parameters were recorded for all patients. The study protocol was approved by the local ethics committee.
Parameter definitions
The modified thrombolysis in cerebral infarction (mTICI) scale was used to characterize different levels of revascularization.11 mTICI 2c was defined as near-complete perfusion, except for slow flow in a few distal cortical vessels or the presence of small distal cortical emboli after MT. mTICI 3 was defined as complete revascularization. Complete FPE (cFPE) was defined as achieving mTICI 2c or 3 after the first MT pass. FPE was defined as achieving mTICI ≥ 2b–3; mTICI 2b was defined as restoration of blood flow in >50% of the affected territory after the first MT pass.
We elected to combine scores of mTICI 2c and 3 in the complete recanalization group, since it is well known that patients who achieve mTICI 2c scores have similar clinical outcomes as patients who achieve mTICI 3;17–18 however, since multiple clinical studies still define good procedural outcome as achieving mTICI 2b or higher, we concluded that it is useful to use these overlapping definitions of cFPE and FPE in order to enable comparisons with other studies. Moreover, this also facilitated separate assessment of procedural approaches and angiographic signs associated with the outcomes of cFPE and FPE.
The use of stent retrievers or primary direct aspiration technique was recorded as well as the name, the diameter and the length of the revascularization device. The device deployment manoeuvre (standard unsheathing or the push and fluff technique) was recorded in patients treated with stent retrievers. The push and fluff technique was defined as unsheathing the device by pulling the microcatheter, thereby leading to a passive stent opening. All interventionists had >2 years of experience performing the push and fluff technique. Solitaire TM was used in 92/193 (47.7%), TREVO in 36/193 (18.7%), direct aspiration first-pass technique (ADAPT) in 39/193 (20.2%) and other devices (Aperio, Capture, Catch, Embotrap, Eric and Stream) in 26/193 (13.4%) of cases. The Solitaire was compared against all the other stent retrievers used.
The use of proximal balloon guide catheter (PBGC), distal aspiration catheter (DAC) or both was recorded. In patients treated with PBGC but not DAC, the position of the catheter tip and partial blockage of aspiration during the procedure was recorded. For patients treated with a DAC, partial blockage of aspiration was also recorded.
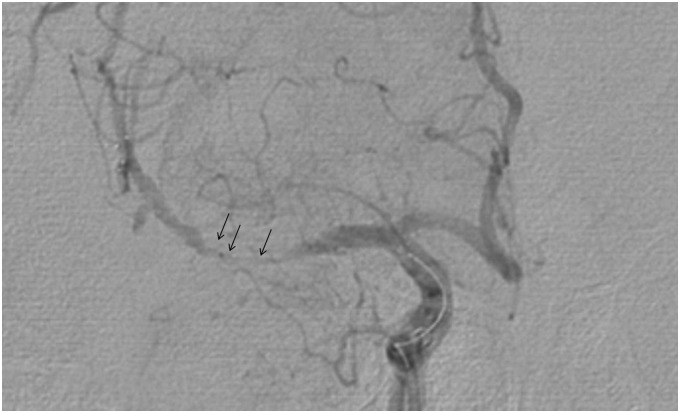
The angiographic clot protrusion sign (ACPS) was defined as the presence of irregular filling defects in the angiogram performed while the device was deployed due to the presence of a clot through the stentriever cells, as a sign of correct integration and internalization of the thrombus (Figure 1). The presence or absence of ACPS was recorded in 99/154 patients (55 missing data). ‘Bypass effect’ was defined as visualization of flow in the artery distal to the initial occlusion after deployment of the stentriever but before retrieval. The bypass effect was recorded in 124/154 patients. The positions of the thrombi were classified as proximal, central or distal in relation to the segment of the deployed device before retrieval, and recorded in 151/154 patients.
Figure 1.
Angiographic clot protrusion sign (ACPS). The dynamic subtracted angiography performed during the procedure shows the presence of irregular filling defects at the level of the right middle cerebral artery due to the presence of clots through stentriever cells.
Statistical analysis
Descriptive and frequency statistical analyses were obtained, and comparisons were made by use of the software IBM SPSS Statistics 22.0. Categorical variables were reported as frequencies (percentages), and continuous variables as mean ± SD or median (interquartile range), as appropriate. Statistical significance for intergroup differences was assessed by Pearson’s chi-square or Fisher’s exact test for categorical variables, the chi-square for linear trend for ordinal variables, and the Student’s t or Mann–Whitney U test for quantitative variables. Variables associated with p < 0.1 in the bivariate analysis were entered into forward stepwise multiple logistic regression models to identify factors independently associated with primary and secondary outcomes. p < 0.05 was considered statistically significant.
Data sharing
The data that support the findings of this study will be available from the corresponding author upon reasonable request.
Results
A total of 193 patients were included in the study, of which 97 (50%) were female; 36% were aged between 18–70, 32% were aged between 70–79 and 31% were aged >80 years. Median National Institutes of Health stroke score was 18 (interquartile range 16–21). The occlusion was localized in the internal carotid artery in 35 (18.1%) of patients, in the M1 segment of the medial cerebral artery in 132 (68.4%) and in the M2 segment of the medial cerebral artery in 24 (12.4%) of patients. Overall, cFPE was achieved in 74 (38.3%) patients and FPE was achieved in 97 (50.3%) patients. There was no difference in pre-procedural clinical characteristics between groups. Use of intravenous tissue-type plasminogen activator (tPA) was not associated with the achievement of first-pass recanalization.
There were no differences in FPE in patients treated with the stent retrievers compared to the ADAPT technique (Table 1). Additionally, no single device was associated with higher rates of cFPE or FPE.
Table 1.
Mechanical thrombectomy and support technical approaches associated with complete first-pass effect and first-pass effect.
| Complete first-pass effect |
First-pass effect |
||||||
|---|---|---|---|---|---|---|---|
| Overall | TICI 2c–3 | TICI 0–2b | p values | TICI 2b–3 | TICI 0–2a | p values | |
| 74 (38.3%) | 119 (61.7%) | 97 (50.3%) | 96 (49.7%) | ||||
| Mechanical thrombectomy technical approach | |||||||
| Stentriever technique | 154 (79.8%) | 61 (39.6%) | 93 (60.4%) | 0.471 | 80 (51.9%) | 74 (48.1%) | 0.351 |
| A direct aspiration first-pass technique | 39 (20.2%) | 13 (33.3%) | 26 (66.7%) | 17 (43.6%) | 22 (56.4%) | ||
| Stentriever radial diameter | 4 (4–6) | 4 (4–6) | 5 (4-6) | 0.738 | 4 (4–6) | 6 (4–6) | 0.031* |
| Stentriever total length | 30 (25–36) | 30 (25–40) | 30 (24.5-30) | 0.408 | 30 (25–40) | 30 (25–30) | 0.937 |
| Use of ‘push and fluff’ techniquea | 90 (60.8%) | 42 (47.2%) | 47 (52.8%) | 0.025 | 51 (56.7%) | 39 (43.3%) | 0.318 |
| Standard unsheathing techniquea | 58 (39.25) | 17 (29.3%) | 41 (70.7%) | 28 (48.3) | 30 (51.8) | ||
| Support technical approach | |||||||
| PBGC | 59 (38.8%) | 30 (50.8%) | 29 (49.2%) | 0.032 | 36 (61.0%) | 23 (39.0%) | 0.075 |
| DAC | 93 (61.2%) | 31 (33.3%) | 62 (66.7%) | 43 (46.3%) | 50 (53.8%) | ||
| Target of PBGC | |||||||
| ICA: petrous segment | 10 (16.7%) | 8 (80.0%) | 2 (20.0%) | 0.05 | 8 (80.0%) | 2 (20.0%) | 0.191 |
| CCA-ICA: cervical segment | 50 (83.3%) | 23 (46%) | 27 (54%) | 29 (58%) | 21 (42%) | ||
| Complications of PBGC | |||||||
| Aspiration through the PBGC was partially blocked | 13 (22%) | 4 (30.8%) | 9 (69.2%) | 0.101 | 4 (30.8%) | 9 (69.2%) | 0.011 |
| Aspiration through the PBGC was not partially blocked | 46 (78%) | 26 (56.5%) | 20 (43.5%) | 32 (69.6%) | 14 (30.4%) | ||
| Complications of DAC | |||||||
| Aspiration through the DAC was partially blocked | 60 (65.2%) | 21 (35.0%) | 39 (65.0%) | 0.717 | 27 (45.0%) | 33 (55.0%) | 0.647 |
| Aspiration through the DAC was not partially blocked | 32 (34.8%) | 10 (31.25%) | 22 (68.75%) | 16 (50.0%) | 16 (50.0%) | ||
CCA: common carotid artery; DAC: distal aspiration catheter; ICA: internal carotid artery; PBGC: proximal balloon guide catheter; TICI: thrombolysis in cerebral infarction.
Six had missing data. *This association failed if corrected for the location of the occlusion.
The Solitaire stent retriever was associated with higher rates of ACPS (75 vs 46.8%, p = 0.004).
A smaller stent diameter was associated with achievement of FPE (p = 0.031). This association failed if corrected for the location of the occlusion, as 4 mm stents were more likely to be used for middle cerebral artery (MCA) occlusion, in which a trend toward a better FPE was found (p = 0.090). No association was found between the length of the device and the achievement of cFPE or FPE.
The push and fluff technique was strongly associated with achievement of cFPE (47.2 vs 29.3%, p = 0.025), regardless of the device used. It was not associated with FPE (p = 0.318).
Direct comparison of PBGC vs DAC outcomes showed that PBGC was associated with the achievement of cFPE and FPE (50.8 vs 33.3%, p = 0.032 and 61 vs 46.3%, p = 0.075, respectively).
The target of PBGC at the level of the petrous segment of the internal carotid artery was significantly associated with cFPE (80 vs 46%, p = 0.05). Additionally, FPE was found to be lower when aspiration through the PBGC was partially blocked (30.8 vs 69.6%, p = 0.011). The ACPS was strongly associated with the achievement of a cFPE and FPE (50.8 vs 18.4%, p = 0.001 and 62.3 vs 34.2%, p = 0.007, respectively) (Table 2). In the presence of the bypass effect, a trend towards a better recanalization was found (p = 0.059 for cFPE and p = 0.074 for FPE). Multiple logistic regression indicated that using PBGC (odds ratio (OR) = 3.81; 95% confidence interval (CI): 1.41–10.22; p = 0.008), push and fluff (OR = 3.45; 95% CI: 1.28–9.29; p = 0.01) or APCS (OR = 4.71; 95% CI: 1.78–12.44; p = 0.002) was an independent predictor of cFPE. When the interventionalist decided to combine a PBGB and the push and fluff technique, cFPE was achieved in 64 vs 34% (p = 0.003) and FPE in 75 vs 46% (p = 0.005) of patients. When the combination concurred with APCS, higher incidence of cFPE (82 vs 35%; p = 0.002) and FPE (91 vs 47%; p = 0.005) was observed.
Table 2.
Angiographic signs associated with complete first-pass effect and first-pass effect in patients treated with stent retrievers.
| Complete first-pass effect |
First-pass effect |
||||||
|---|---|---|---|---|---|---|---|
| Overall | TICI 2c–3 | TICI 0–2b | p values | TICI 2b–3 | TICI 0–2a | p values | |
| 74 (38.3%) | 119 (61.7%) | 97 (50.3%) | 96 (49.7%) | ||||
| Angiographic clot protrusion signa | |||||||
| Presence | 61 | 31 (50.8%) | 30 (49.2%) | 0.001 | 38 (62.3%) | 23 (37.7%) | 0.007 |
| Absence | 38 | 7 (18.4%) | 31 (81.6%) | 13 (34.2%) | 25 (65.8%) | ||
| Bypass effectb | |||||||
| Presence | 84 | 38 (45.2%) | 46 (54.8%) | 0.059 | 48 (57.1%) | 36 (42.9%) | 0.074 |
| Absence | 40 | 11 (27.5%) | 29 (72.5%) | 16 (40.0%) | 24 (60.0%) | ||
| Position of thrombic | |||||||
| Proximal | 52 | 19 (36.5%) | 33 (63.5%) | 0.715 | 25 (48.1%) | 27 (51.9%) | 0.961 |
| Central | 88 | 37 (42.0%) | 51 (58.0%) | 49 (55.7%) | 39 (44.3%) | ||
| Distal | 11 | 4 (36.4%) | 7 (63.6%) | 4 (36.4%) | 7 (63.6%) | ||
TICI: thrombolysis in cerebral infarction.
Missing data for 55.
Missing data for 30.
Missing data for three.
Post hoc analyses demonstrated that frequency of use of the push and fluff technique, PBGC and DAC differed significantly between the five stroke centres that participated in the study, although the frequency of cFPE and FPE did not differ significantly between centres.
Discussion
The importance of achieving successful first-pass recanalization is increasingly recognized in endovascular therapy for acute ischaemic stroke. However, the optimal procedural approach and strategy to monitor the performance is unclear. We report that the use of PBGC, the push and fluff technique, and the ACPS are independent predictors of cFPE, and that the concurrence of these variables is associated with high rates of cFPE and FPE. All of these features concern the achievement of efficient and total thrombus integration into the device, with reduced distal embolization, to obtain a successful thrombectomy. Appropriate selection of the thrombectomy device and deployment technique may lead to better procedural outcomes.
Several recent studies have demonstrated aspiration as an equally effective strategy compared to stent retrievers for revascularization.12–14 ADAPT utilizes aspiration as the first approach for revascularization of the occluded vessel and, if this strategy fails, the aspiration catheter is used in conjunction with a stent retriever to achieve revascularization.13 This procedure has reported successful clot removal in ≤75% of cases, but may require multiple attempts.14
Balloon guide catheters are able to achieve efficient flow arrest and are consistently associated with positive angiographic outcomes.5,7 Chueh et al. found that the use of a balloon guide catheter during MT resulted in a significant reduction in large clot fragments.15 Additionally, the combination of a stentriever with PBGC has been previously reported as a feasible combinational approach, achieving first-pass recanalization in 110/170 (65%) of patients.16 Consistent with these findings, we found that the use of PBGC was strongly associated with cFPE (mTICI 2c–3). Our findings support the concept that mTICI 2c and 3 may be a homogeneous group of patients where no (or less) distal emboli were produced during MT.17 The class mTICI 2c grade has been recently been used to described cases of near-complete reperfusion, whose clinical outcomes are similar to those achieving mTICI 3.17–18
In our study, data were not correlated with patient clinical outcomes. However, the primary aim of this study was to find the best combination of device and technique to maximize the mTICI 2c-3 score, with a single device pass and without thrombus fragmentation.
Flow arrest achieved with the PBGS balloon, together with efficient thrombus entrapment (ACPS), may be sufficient to prevent thrombus fragmentation even in presence of non-continuous aspiration of the balloon catheter itself. It is important to note that continuous aspiration, which can be achieved by both PBGCs and DACs, does not necessary imply efficient flow arrest.15 In the case of continuous aspiration, the catheter contacts and fixes the proximal aspect of the clot, but the distal portion may still be exposed to the arterial flow. This may explain why, in cases with partially blocked aspiration of the PBGC, there was no significant reduction of FPE.
In our analysis, the use of DAC was associated with worse outcome, consistent with a previous study that reported higher rates of successful recanalization (91/102 (89.2%) and 55/81 (67.9%), respectively) and one-pass thrombectomy rates (65/102 (63.7%) and 29/81 (35.8%), respectively) with balloon guide catheters compared to non-balloon guided catheters.7 The decision to use a DAC is influenced by the characteristics of the patient; for example, it is used more prevalently in patients with complex anatomy of the vessels and the aortic arc.19 In these cases, cervical vascular tortuosity may be responsible for the limited success of the MT, representing a potential selection bias. Randomized controlled trials comparing PBGCs with DACs are lacking. Moreover, the adjunctive beneficial effect of combining the new generation of PBGCs with increased lumen diameter ratios compatible with DACs should be addressed in further studies.
In our analysis, the Push and Fluff technique was associated with cFPE, but not PFE, suggesting that, in addition to the devices used, the procedural approach can impact the amount of clot retrieved, which may be important in preventing distal embolus formation. The push and fluff manoeuvre leads to optimized wall apposition and increased thrombus/stentriever entanglement, leading to improved efficacy as compared to a standard unsheathing technique with use of the TREVO stentriever.10
Monitoring the achievement of ACPS during angiography allows real-time feedback of the amount of thrombus correctly integrated into the device. ACPS assessment allows for early modification of the strategy, which may increase the integration success rate of stentriever devices. In agreement with this finding, a recent study has proposed the use of post-deployment digital subtraction angiography as a method to confirm and increase thrombus integration.20 Possible strategies to improve efficient thrombus integration may be ‘waiting for a longer time’ and ‘mobilization of the device’, but the efficacy of these measures should be tested in future trials.
In this study, multiple types of stent retrievers and catheters were used, which may have introduced some heterogeneity into the results. The use of various devices, with different stent diameters, may also be responsible for the lack of correlation that we found between the length of the device used and successful first-pass recanalization, as previously reported.21 However, our study is highly representative of routine MT care in Comprehensive Stroke Centres and reflects the need to optimize the technique in order to obtain efficient thrombus integration. Finally, due to sample size, we were unable to compare outcomes between different occlusion locations (i.e., M1 and internal carotid artery bifurcation) and other essential baseline characteristics. However, it is noteworthy that we did not find significant differences according to previous intravenous tPA. This is in line with a previous study that suggested that outcomes after MT are not different if combined with previous intravenous treatment.22
We cannot rule out that the differences in achievement of FPE may be associated with intrinsic patient characteristics, such as clot density and vascular atheromatosis, that may distinguish whether successful recanalization may be achieved. In some patients, the impossibility of reaching a first-pass recanalization may reflect not being responsive to endovascular therapy, which highlights the need for better pre-procedural selection of patients. Future studies should aim to find the best combination of procedures according to patient and thrombus characteristics.
Conclusion
In our experience, the concurrence of the PBGC, the push and fluff technique, and the ACPS was associated with the highest rates of FPE and cFPE. Appropriate selection of the thrombectomy device and deployment technique may lead to better procedural outcomes. ACPS could be used to assess clot integration strategies in future trials.
Declaration of competing interests
The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding
The authors received no financial support for the research, authorship and/or publication of this article. None of the Comprehensive Stroke Centres received external funding.
References
- 1.Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2018; 49: e46–e110. [DOI] [PubMed] [Google Scholar]
- 2.Ozdemir O, Giray S, Arlier Z, et al. Predictors of a good outcome after endovascular stroke treatment with stent retrievers. ScientificWorldJournal 2015; 2015: 403726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Linfante I, Starosciak AK, Walker GR, et al. Predictors of poor outcome despite recanalization: A multiple regression analysis of the NASA registry. J Neurointerv Surg 2016; 8: 224–229. [DOI] [PubMed] [Google Scholar]
- 4.Rha JH, Saver JL. The impact of recanalization on ischemic stroke outcome: A meta-analysis. Stroke 2007; 38: 967–973. [DOI] [PubMed] [Google Scholar]
- 5.Zaidat OO, Castonguay AC, Linfante I, et al. First pass effect: A new measure for stroke thrombectomy devices. Stroke 2018; 49: 660–666. [DOI] [PubMed] [Google Scholar]
- 6.Nguyen TN, Malisch T, Castonguay AC, et al. Balloon guide catheter improves revascularization and clinical outcomes with the Solitaire device: Analysis of the North American Solitaire Acute Stroke Registry. Stroke 2014; 45: 141–145. [DOI] [PubMed] [Google Scholar]
- 7.Velasco A, Buerke B, Stracke CP, et al. Comparison of a balloon guide catheter and a non-balloon guide catheter for mechanical thrombectomy. Radiology 2016; 280: 169–176. [DOI] [PubMed] [Google Scholar]
- 8.Stampfl S, Kabbasch C, Müller M, et al. Initial experience with a new distal intermediate and aspiration catheter in the treatment of acute ischemic stroke: Clinical safety and efficacy. J Neurointerv Surg 2016; 8: 714–718. [DOI] [PubMed] [Google Scholar]
- 9.Sallustio F, Pampana E, Davoli A, et al. Mechanical thrombectomy of acute ischemic stroke with a new intermediate aspiration catheter: Preliminary results. J Neurointerv Surg 2018; 10: 975–977. [DOI] [PubMed] [Google Scholar]
- 10.Haussen DC, Rebello LC, Nogueira RG. Optimizating clot retrieval in acute stroke: The push and fluff technique for closed-cell stentrievers. Stroke 2015; 46: 2838–2842. [DOI] [PubMed] [Google Scholar]
- 11.Tung EL, McTaggart RA, Baird GL. Rethinking thrombolysis in cerebral infarction 2b: Which thrombolysis in cerebral infarction scales best define near complete recanalization in the modern thrombectomy era? Stroke 2017; 48: 2488–2493. [DOI] [PubMed] [Google Scholar]
- 12.Kabbasch C, Mohlenbruch M, Stampfl S, et al. First-line lesional aspiration in acute stroke thrombectomy using a novel intermediate catheter: Initial experiences with the SOFIA. Interv Neuroradiol 2016; 22: 333–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stapleton CJ, Leslie-Mazwi TM, Torok CM, et al. A direct aspiration first-pass technique vs stentriever thrombectomy in emergent large vessel intracranial occlusions. J Neurosurg 2018; 128: 567–574. [DOI] [PubMed] [Google Scholar]
- 14.Turk AS, Frei D, Fiorella D, et al. ADAPT FAST study: A direct aspiration first pass technique for acute stroke thrombectomy. J Neurointerv Surg 2014; 6: 260–264. [DOI] [PubMed] [Google Scholar]
- 15.Chueh JY, Kuhn AL, Puri AS, et al. Reduction in distal emboli with proximal flow control during mechanical thrombectomy: A quantitative in vitro study. Stroke 2013; 44: 1396–1401. [DOI] [PubMed] [Google Scholar]
- 16.Kammerer S, du Mesnil de Rochemont R, Wagner M, et al. Efficacy of mechanical thrombectomy using stent retriever and balloon-guiding catheter. Cardiovasc Intervent Radiol 2018; 41: 699–705. [DOI] [PubMed] [Google Scholar]
- 17.Dargazanli C, Fahed R, Blanc R, et al. Modified thrombolysis in cerebral infarction 2C/thrombolysis in cerebral infarction 3 reperfusion should be the aim of mechanical thrombectomy: Insights from the ASTER trial (contact aspiration versus stent retriever for successful revascularization). Stroke 2018; 49: 1189–1196. [DOI] [PubMed] [Google Scholar]
- 18.Almekhlafi MA, Mishra S, Desai JA, et al. Not all “successful” angiographic reperfusion patients are an equal validation of a modified TICI scoring system. Interv Neuroradiol 2014; 20: 21–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brinjikji W, Starke RM, Murad MH, et al. Impact of balloon guide catheter on technical and clinical outcomes: A systematic review and meta-analysis. J Neurointerv Surg 2018; 10: 335–339. [DOI] [PubMed] [Google Scholar]
- 20.Simon S, Langan S, Cooke J. Increasing efficacy of thrombectomy by using digital subtraction angiography to confirm stent retriever clot integration. Cureus 2016; 8: e559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Haussen DC, Al-Bayati AR, Grossberg JA, et al. Longer stent retrievers enhance thrombectomy performance in acute stroke. J Neurointerv Surg 2019; 11: 6–8. [DOI] [PubMed] [Google Scholar]
- 22.Abilleira S, Ribera A, Cardona P. Outcomes after direct thrombectomy or combined intravenous and endovascular treatment are not different. Stroke 2017; 48: 375–378. [DOI] [PubMed] [Google Scholar]