Key Points
Question
Is antidepressant use associated with adverse health outcomes, and how credible is the evidence behind this association in published meta-analyses of real-world data?
Findings
In this systematic umbrella review of 45 meta-analyses of observational studies, convincing evidence was found for the associations between antidepressant use and suicide attempt or completion among individuals younger than 19 years and between antidepressant use and autism risk among the offspring. However, none of these associations remained at the convincing evidence level after a sensitivity analysis that adjusted for confounding by indication.
Meaning
This study’s findings suggest that claimed adverse health outcomes associated with antidepressants may not be supported by strong evidence and may be exaggerated by confounding by indication; no absolute contraindication to the use of antidepressants was found to be currently supported by convincing evidence.
This umbrella review searches PubMed, Scopus, and PsycINFO to summarize and grade the strength of evidence of the associations between antidepressants and adverse outcomes reported in multiple meta-analyses.
Abstract
Importance
Antidepressant use is increasing worldwide. Yet, contrasting evidence on the safety of antidepressants is available from meta-analyses, and the credibility of these findings has not been quantified.
Objective
To grade the evidence from published meta-analyses of observational studies that assessed the association between antidepressant use or exposure and adverse health outcomes.
Data Sources
PubMed, Scopus, and PsycINFO were searched from database inception to April 5, 2019.
Evidence Review
Only meta-analyses of observational studies with a cohort or case-control study design were eligible. Two independent reviewers recorded the data and assessed the methodological quality of the included meta-analyses. Evidence of association was ranked according to established criteria as follows: convincing, highly suggestive, suggestive, weak, or not significant.
Results
Forty-five meta-analyses (17.9%) from 4471 studies identified and 252 full-text articles scrutinized were selected that described 120 associations, including data from 1012 individual effect size estimates. Seventy-four (61.7%) of the 120 associations were nominally statistically significant at P ≤ .05 using random-effects models. Fifty-two associations (43.4%) had large heterogeneity (I2 > 50%), whereas small-study effects were found for 17 associations (14.2%) and excess significance bias was found for 9 associations (7.5%). Convincing evidence emerged from both main and sensitivity analyses for the association between antidepressant use and risk of suicide attempt or completion among children and adolescents, autism spectrum disorders with antidepressant exposure before and during pregnancy, preterm birth, and low Apgar scores. None of these associations remained supported by convincing evidence after sensitivity analysis, which adjusted for confounding by indication.
Conclusions and Relevance
This study’s findings suggest that most putative adverse health outcomes associated with antidepressant use may not be supported by convincing evidence, and confounding by indication may alter the few associations with convincing evidence. Antidepressant use appears to be safe for the treatment of psychiatric disorders, but more studies matching for underlying disease are needed to clarify the degree of confounding by indication and other biases. No absolute contraindication to antidepressants emerged from this umbrella review.
Introduction
Accumulating evidence suggests a sharp growth in antidepressant use worldwide. Up to 8% to 10% of adults in the United States take at least 1 antidepressant drug, which is ranked third among prescribed and fourth among sold medications.1,2 Antidepressants are indicated and used for depressive disorders, anxiety disorders, posttraumatic stress disorder, premenstrual dysphoric disorder, obsessive-compulsive disorder, bulimia nervosa, and binge-eating disorder, among others.3,4,5
The safety profile of antidepressants is controversial. Since the US Food and Drug Administration introduced the black box warnings that associated selective serotonin reuptake inhibitor (SSRI) use with a higher risk of suicidal behavior in children and adolescents,6 the debate about the efficacy, acceptability, and safety profile of antidepressant medications has gradually increased.7,8,9,10,11 Evidence from randomized clinical trials (RCTs) of antidepressants’ efficacy and acceptability has been well documented in both meta-analyses and network meta-analyses,4,8,10,12,13 but safety assessment is inherently biased by certain methodological weaknesses of RCTs. These weaknesses include small and unrepresentative samples, rare and inconsistent reporting of adverse outcomes, and short duration of exposures.14,15
Observational studies complement RCTs by providing evidence with real-world data15 on a number of adverse health outcomes associated with antidepressants, which is not possible in RCTs.16 For example, observational studies can show medication safety because they include representatives of the overall target population, such as patients with comorbid disorders or suicidal thoughts who are often excluded from RCTs. In addition, observational studies typically have a longer follow-up duration compared with RCTs, providing data on the mid- or long-term consequences of antidepressants, such as poor bone status or gastrointestinal bleeding, that may not arise from short-term use.16
Several meta-analyses of observational studies have been published that assess antidepressant safety; however, to our knowledge, no attempt has been made to quantify the credibility of their findings. This quantification is crucial considering the uncertainty surrounding observational research results.17,18,19 Umbrella reviews make it feasible to summarize the evidence from multiple meta-analyses on the same topic20,21 and enable the ranking of evidence (as convincing, highly suggestive, suggestive, weak, or not significant) according to sample size, strength of the association, and assessment of presence of biases.22,23,24
In this umbrella review, we graded the evidence from published meta-analyses of observational studies. These studies tested the association between antidepressant use and risk of adverse health outcomes.
Methods
The protocol for this study was registered on PROSPERO (CRD42018103462). We followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline25 and the Meta-analysis of Observational Studies in Epidemiology (MOOSE) guidelines26 (eAppendix 1 in the Supplement).
Search Strategy and Selection Criteria
We searched PubMed, Scopus, and PsycINFO from database inception to April 5, 2019, to identify systematic reviews with meta-analysis of observational studies of the association between any adverse health outcome and exposure to antidepressants. Our search strategy used a combination of terms related to antidepressants (eg, antidepressants, selective serotonin reuptake inhibitors), to adverse health outcomes (eg, harms, suicide, bleeding, and autism), and to meta-analysis with no age, sex, population, and medical condition restrictions (eAppendix 2 in the Supplement). We also manually searched the cited references of the retrieved articles and reviews.
Two of us (E.D. and M.S.) independently searched titles or abstracts for eligibility and consulted a third reviewer (E.E.) when we could not reach a consensus. The full texts of potentially eligible articles were retrieved, and the same two of us (E.D. and M.S.) independently scrutinized each study for eligibility. Any discrepancies during this process were resolved by our third reviewer (E.E.).
We included only peer-reviewed systematic reviews with meta-analysis of observational studies with a cohort, case-control, or nested case-control study design measuring any association between antidepressant use and any adverse health outcome in any population of any age. Whenever multiple meta-analyses on the same adverse health outcome were performed (ie, overlapping meta-analyses with the same outcome, type of antidepressant used, and clinical or population setting), we assessed only the one that included the largest data set, as previously described.22,24,27 Details of the selection between overlapping meta-analyses are described in the eMethods in the Supplement. For each eligible meta-analysis, we considered the main analysis for all primary and secondary reported outcomes. The concordance between selected and nonselected meta-analyses was examined in a sensitivity analysis.27
We excluded (1) meta-analyses of studies with other study designs (eg, RCTs, cross-sectional) or that included both observational studies and RCTs in the same analysis; (2) meta-analyses published in languages other than English; (3) meta-analyses of individual patient or participant data, pooled analyses of a nonsystematic selection of observational studies, and nonsystematic reviews; (4) meta-analyses of St John’s wort (Hypericum perforatum) or tryptophan; and (5) meta-analyses that provided insufficient or inadequate data for quantitative synthesis.
Data Extraction
Two of us (E.D. and M.S.) independently performed data extraction, and disagreements were resolved by a consensus. Adverse health outcomes associated with exposure to antidepressants were extracted as defined by the original authors. For each meta-analysis, we recorded the standard identifier (PMID and DOI), first author, publication year, type of antidepressant, study design, age of participants, adverse health outcomes, exposure and nonexposure, illnesses examined (eg, depression), number of included studies, and total sample size.
For each primary study, we recorded first author; year of publication; study design (ie, cohort or case-control); number of cases and controls in case-control studies or total population in cohort studies; reported adjusted (or unadjusted) effect size (ie, relative risk, odds ratio, hazard ratio, and standardized mean difference), each with a 95% CI; and study location. We also captured the number and nature of adjustments, the length of follow-up, the study quality score, and whether the studies were controlled for a psychiatric condition (ie, confounding by indication).18,19
The methodological quality of each included meta-analysis was assessed by 2 of us (E.D. and M.S.) using the updated AMSTAR (A Measurement Tool to Assess Systematic Reviews) 2.28 AMSTAR 2 also accounts for the quality of studies included in the meta-analysis beyond a mere technical methodological assessment of the included meta-analysis (eMethods in the Supplement).16
Statistical Analysis
For each association, we extracted effect sizes of individual studies included in each meta-analysis, and we repeated the meta-analyses to calculate the pooled effect sizes and the 95% CIs using random-effects models to compare homogeneously analyzed results.29 We did not transform the initial effect sizes or modify the direction of associations presented by the original authors to compare the results we obtained with the reported results in the meta-analyses. Heterogeneity was assessed with the I2 statistic.30 In addition, we calculated the 95% prediction intervals for the summary random effect sizes, providing the possible range in which the effect sizes of future studies were expected to fall.31
Next, we tested whether smaller studies yielded larger effect sizes compared with larger studies, an indication of small-study effect bias.24,32,33,34 Small-study effect bias was indicated both by the Egger regression asymmetry test (P ≤ .10) and by the random-effects summary effect size being larger than that of the biggest study in each association.24,32,33,34
We then assessed the existence of excess significance bias by evaluating whether the observed number of studies with nominally statistically significant results (positive studies as indicated with a 1-sided P ≤ .05) was different from the expected number of studies with statistically significant results.34 The expected number of statistically significant studies per association was calculated by summing the statistical power estimates for each component study. The power estimates of each component study depend on the plausible effect size for the tested association, which we assumed to be the effect size of the largest study (ie, the smallest SE) per association.35 Excess significance bias was set at P ≤ .10. This test was designed to assess whether the published meta-analyses comprised an overrepresentation of false-positive findings.34 All analyses were conducted in Stata/MP, version 10.0 (StataCorp LLC).
Assessment of the Credibility of the Evidence
We assessed the credibility of the evidence per association provided in meta-analyses by applying several criteria in concordance with previously published umbrella reviews.22,23,32,33,36,37 In brief, associations that presented nominally significant random-effects summary effect sizes (ie, P ≤ .05) were ranked as convincing, highly suggestive, suggestive, or weak evidence according to sample size, strength of the association, and assessment of the presence of biases (Table 1 and eMethods in the Supplement). In addition, to provide an estimate of the epidemiologic implication of findings, we calculated the prevalence of outcomes of interest from cohort studies only (studies with case-control designs should not be considered for prevalence estimates).
Table 1. Criteria for Credibility-of-Evidence Classification in Observational Studies.
| Classification | Criteria |
|---|---|
| Convincing evidence (class I) |
|
| Highly suggestive evidence (class II) |
|
| Suggestive evidence (class III) |
|
| Weak evidence (class IV) |
|
| Nonsignificant association (NS) |
|
Sensitivity Analysis
We performed sensitivity analyses to assess whether the credibility of the evidence varied within both prospective and retrospective cohort studies, prospective cohort studies, studies adjusted for multiple covariates and for confounding by indication, high-quality primary studies, studies of antidepressant classes (SSRIs, tricyclic antidepressants [TCAs], and other or mixed antidepressants), and locations where studies were conducted (Europe, North America, or other regions). These analyses were performed only for the associations ranked as convincing evidence or highly suggestive evidence (ie, class I or II) in the main analysis.
Results
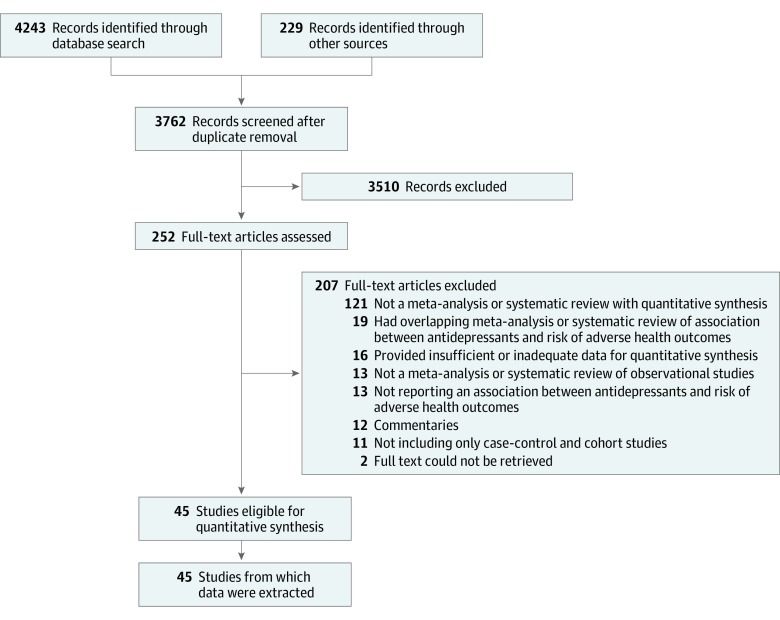
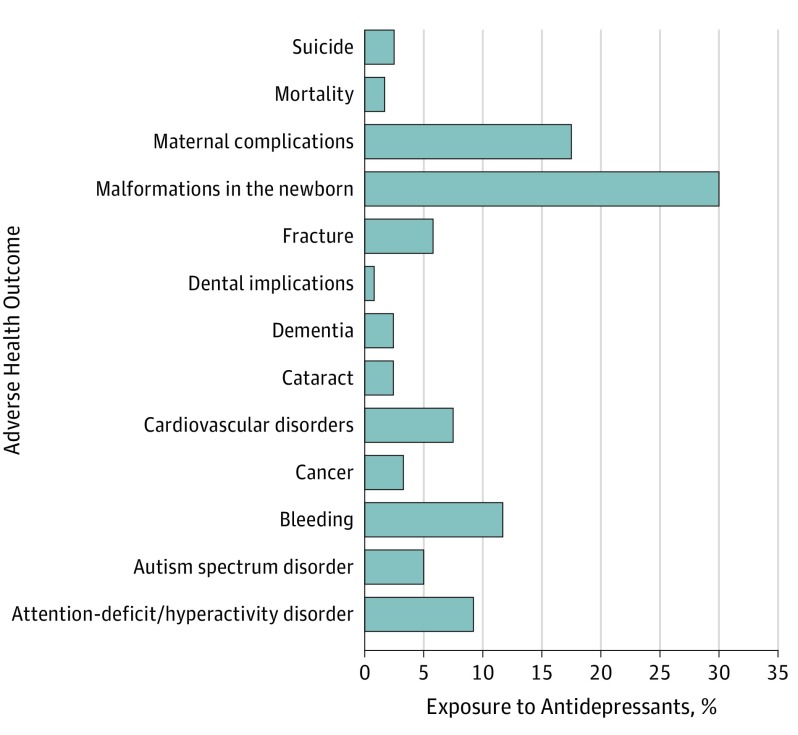
In total, we identified 4471 studies, scrutinized 252 full-text articles, and ultimately included 45 meta-analyses (17.9%) in this umbrella review38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83 (Figure 1), corresponding to 695 studies, 1012 study estimates, and 13 putative risks (Figure 2). The 207 excluded articles (82.1%) and the reasons for their exclusion are provided in eTable 1 in the Supplement.
Figure 1. Flowchart of the Literature Search and Evaluation Process for 45 Published Meta-analyses and Systematic Reviews.
Figure 2. Percentages of the Reported 13 Adverse Health Outcome Domains Associated With Antidepressant Exposure in 45 Published Meta-analyses.
Descriptive characteristics of the 45 eligible meta-analyses of observational studies can be found in eTable 2 in the Supplement. All meta-analyses had a control group that was not exposed to antidepressants except for 1 (2.2%), which compared the risk of gastrointestinal bleeding between mirtazapine and SSRIs.47 The median number of adjustments in the analyses was 7 (interquartile range [IQR], 4-11), and the median duration of follow-up was 4 (IQR, 2-5) years.
Thirty-three meta-analyses (73.4%) met the moderate-quality level according to the AMSTAR 2 evaluation, and 8 (17.8%) were of low quality. Two (4.4%) were high quality, whereas 2 others (4.4%) were of critically low quality. The 2 of us (E.D. and M.S.) reached a high level of agreement (91%) on the quality rating.
Description and Summary of Associations
Forty-five eligible meta-analyses described 120 associations, including 1012 individual study estimates of adverse health outcomes associated with exposure to antidepressants (Table 2 and eTables 2-5 in the Supplement), with a median (IQR) number of estimates per association of 6 (4-12). Seventy-four (61.7%) of the associations concerned maternal and pregnancy-related adverse health outcomes (Figure 2). Most associations (80 [66.7%]) concerned SSRIs or serotonin-norepinephrine reuptake inhibitors, 9 (7.5%) TCAs, and 31 (25.8%) mixed or other antidepressants.
Table 2. Class I or II Evidence in Meta-analyses of the Association Between Antidepressant Use and Risk of Adverse Health Outcomes.
| Source | Adverse Health Outcome | Exposed/ Unexposed |
Prevalence Based on Cohort Studies, % | No. of Included Studies per Association | Random-Effects Measure, ES (95% CI) | Result | Criteria for Level-of-Evidence Classification | AMSTAR 2 Quality | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of Cases/ Total Population |
P Value for Random Effects | Heterogeneity, I2 (P Value) |
PI, 95% CI |
SSE/ESB | LS | CE | ||||||||
| Morales et al,51 2018 | Autism spectrum disorders (prepregnancy maternal exposure) | Any AD users/ no AD users |
0.8 | 7 | RR: 1.48 (1.29 to 1.71) | Increased risk for AD | 22 877/ 2 400 720 |
6.8 × 10−8 | 24 (.24) | 1.09 to 2.02 | No/NP | Yes | I | Moderate |
| Andalib et al,52 2017 | Autism spectrum disorders (pregnancy maternal exposure; unadjusted estimates only) | SSRI/ non-SSRI users |
0.9 | 7 | OR: 1.84 (1.60 to 2.11) | Increased risk for SSRI | 58 178/ 5 868 692 |
1.2 × 10−17 | 0 (.73) | 1.53 to 2.20 | No/NP | Yes | I | Moderate |
| Barbui et al,80 2009 | Suicide attempt and completion in children and adolescents | SSRI/ non-SSRI users |
9.4 | 5 | OR: 1.92 (1.51 to 2.44) | Increased risk for SSRI | 6531/ 61 522 |
1.0 × 10−7 | 0 (.47) | 1.30 to 2.84 | No/NP | Yes | I | High |
| Khanassov et al,42 2018 | Osteoporotic fractures | SSRI/ non-SSRI users |
6.5 | 24 | RR:1.67 (1.56 to 1.80) | Increased risk for SSRI | 136 449/ 1 546 913 |
1.3 × 10−44 | 88 (<.001) | 1.23 to 2.27 | No/NP | Yes | II | Moderate |
| Man et al,48 2018 | ADHD in children | Prenatal exposure to AD/ no AD users |
2.4 | 7 | RR: 1.39 (1.21 to 1.61) | Increased risk for AD | 57 552/ 2 886 904 |
5.1 × 10−6 | 79 (<.001) | 0.90 to 2.15 | No/NP | Yes | II | Moderate |
| Fu et al,49 2018 | Cataract development | TCA/nonusers or no users of any other AD |
NA | 3 | OR: 1.19 (1.11 to 1.28) | Increased risk for TCA | 215 298/ 431 171 |
2.0 × 10−6 | 58 (.09) | 0.50 to 2.52 | No/NP | Yes | II | Moderate |
| Laporte et al,55 2017 | Severe bleeding at any site | SSRI + SNRI/ non-users or no users of any other AD |
2.4 | 44 | OR: 1.41 (1.27 to 1.57) | Increased risk for SSRI + SNRI | 75 215/ 1 443 029 |
2.2 × 10−10 | 90 (<.001) | 0.77 to 2.59 | No/no | Yes | II | Low |
| Jiang et al,58 2016 | Postpartum hemorrhage | Any AD users/non-AD users | 6.8 | 17 | RR: 1.32 (1.17 to 1.48) | Increased risk for AD | 49 155/ 651 715 |
3.3 × 10−6 | 85 (<.001) | 0.84 to 2.07 | No/NP | Yes | II | Low |
| Jiang et al,64 2015 | Upper GI bleeding | SSRI + other non-AD/ no SSRI use only + other non-AD |
0.7 | 22 | OR: 1.55 (1.35 to 1.78) | Increased risk for SSRI | 56 182/ 592 508 |
9.2 × 10−12 | 89 (<.001) | 0.83 to 2.91 | No/no | Yes | II | Moderate |
| Huang et al,66 2014 | Preterm birth | Any AD users/ no AD users |
0.8 | 28 | RR: 1.68 (1.52 to 1.86) | Increased risk for AD | 24 669/ 3 063 709 |
3.6 × 10−23 | 44 (.008) | 1.23 to 2.30 | Yes/NP | Yes | II | Moderate |
| Wu et al,70 2013 | Osteoporotic fractures | TCA users/ non-TCA users |
1.4 | 12 | RR: 1.45 (1.31 to 1.60) | Increased risk for TCA | 178 237/ 831 912 |
6.2 × 10−13 | 76 (<.001) | 1.04 to 2.01 | Yes/no | Yes | II | Moderate |
| Ross et al,71 2013 | Apgar score at 5 min | Any AD users/ no AD users |
2.1 | 15 | SMD: −0.33 (−0.47 to −0.20) | Increased risk for AD | 1473/ 71 828 |
7.5 × 10−7 | 58 (.003) | −1.02 to 0.36 | No/no | Yes | II | Moderate |
| Oderda et al,76 2012 | Hip fracture | TCA and/or SSRI users/no AD users |
7.4 | 18 | OR: 1.78 (1.53 to 2.07) | Increased risk for TCA or SSRI | 49 276/ 210 577 |
5.2 × 10−14 | 89 (<.001) | 1.00 to 3.19 | Yes/yes | Yes | II | Critically low |
| Barbui et al,80 2009 | Suicide attempt and completion in adults | SSRI/ non-SSRI users |
4.5 | 7 | OR: 0.59 (0.48 to 0.72) | Decreased risk for SSRI | 7164/ 147 383 |
5.2 × 10−7 | 59 (.02) | 0.33 to 1.05 | No/NP | Yes | II | High |
Abbreviations: AD, antidepressant; ADHD, attention-deficit/hyperactivity disorder; Apgar score, appearance (skin color), pulse (heart rate), grimace (reflex irritability), activity (muscle tone), and respiration; AMSTAR, A Measurement Tool to Assess Systematic Reviews; CE, class of evidence; ES, effect size; ESB, excess significance bias; GI, gastrointestinal; LS, largest study with significant effect; NA, not applicable; NP, not pertinent because of fewer-than-expected number of observed studies; OR, odds ratio; PI, prediction interval; RR, relative risk; SMD, standardized mean difference; SNRI, serotonin-norepinephrine reuptake inhibitor; SSE, small-study effect; SSRI, selective serotonin reuptake inhibitor; TCA, tricyclic antidepressant.
The median (IQR) number of the total population per association was 1 056 374 (152 180-2 215 969). The median (IQR) number of cases (adverse health outcomes) per association was 12 097 (2585-56 272), and the number of cases was greater than 1000 for 87 associations (72.5%).
A summary of all 120 associations is presented in Table 2 and Table 3 and eTables 3-5 in the Supplement. Seventy-four of the 120 examined associations (61.7%) were nominally statistically significant at P ≤ .05 based on random-effects models, and only 22 (18.3%) reached a P ≤ 1 × 10−6. Almost all statistically significant associations indicated an increased risk for antidepressants and adverse health outcomes except for 2 associations (2.7%) showing the protective property of SSRIs against suicide attempt or completion in adults and in older adults.80
Table 3. Sensitivity Analysis of Class I or II Evidence in Meta-analyses of the Association Between Antidepressants and Risk of Adverse Health Outcomesa.
| Source | Adverse Health Outcome | Exposed/ Unexposed |
Prevalence Based on Cohort Studies, % | No. of Included Studies per Association | Random Effects Measure to ES (95% CI) | Criteria for Level-of-Evidence Classification | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of Cases/ Total Population |
P Value Random Effects | Heterogeneity, I2 (P Value) | PI, 95% CI | SSE/ESB | LS | CE | CES/ AMSTAR 2 |
||||||
| Retrospective and Prospective Cohort Studies | |||||||||||||
| Andalib et al,52 2017 | Autism spectrum disorders (pregnancy maternal exposure; unadjusted estimates only) | SSRI/ non-SSRI users |
0.9 | 3 | OR: 1.65 (1.37 to 2.00) | 50 494/ 5 790 186 |
2.2 × 10−7 | 0 (.69) | 0.48 to 5.68 | No/no | Yes | I | II/Moderate |
| Khanassov et al,42 2018 | Osteoporotic fractures | SSRI/ non-SSRI users |
6.5 | 16 | RR: 1.63 (1.49 to 1.79) | 56 397/ 859 611 |
8.9 × 10−27 | 85 (<.001) | 1.20 to 2.22 | No/NP | Yes | II | II/Moderate |
| Huang et al,66 2014 | Preterm birth | Any AD users/ no AD users |
0.8 | 24 | RR: 1.67 (1.51 to 1.86) | 24 378/ 3 063 012 |
6.5 × 10−22 | 49 (.004) | 1.21 to 2.33 | Yes/no | Yes | II | II/Moderate |
| Ross et al,71 2013 | Apgar score at 5 min | Any AD users/ no AD users |
2.1 | 15 | SMD: −0.33 (−0.47 to −0.20) | 1473/ 71 828 |
7.5 × 10−7 | 58 (.003) | 1.02 to 0.36 | No/no | Yes | II | II/Moderate |
| Barbui et al,80 2009 | Suicide attempt and completion in children and adolescents | SSRI/ non-SSRI users |
9.4 | 3 | OR: 1.89 (1.46 to 2.43) | 5647/ 59 971 |
1.8 × 10−7 | 0 (.46) | 0.36 to 9.85 | No/NP | Yes | I | II/High |
| Barbui et al,80 2009 | Suicide attempt and completion in adults | SSRI/ non-SSRI users |
4.5 | 5 | OR: 2.53 (0.43 to 0.66) | 6458/ 143 340 |
5.2 × 10−7 | 55 (.06) | 0.27 to 1.04 | No/NP | Yes | II | II/High |
| Prospective Cohort Studies | |||||||||||||
| Andalib et al,52 2017 | Autism spectrum disorders (pregnancy maternal exposure; unadjusted estimates only) | SSRI/ non-SSRI users |
0.9 | 3 | OR: 1.65 (1.37 to 2.00) | 50 494/ 5 790 186 |
2.2 × 10−7 | 0 (.69) | 0.48 to 5.68 | No/no | Yes | I | II/Moderate |
| Huang et al,66 2014 | Preterm birth | Any AD users/ no AD users |
0.4 | 11 | RR: 1.87 (1.52 to 2.30) | 2540/ 690 121 |
3.4 × 10−9 | 31 (.15) | 1.17 to 3.00 | No/NP | Yes | II | I/Moderate |
| Studies Adjusted for Multiple Covariates | |||||||||||||
| Morales et al,51 2018 | Autism spectrum disorders (prepregnancy maternal exposure) | Any AD users/ no AD users |
0.8 | 7 | RR: 1.48 (1.29 to 1.71) | 22 877/ 2 400 720 |
6.8 × 10−8 | 24 (.24) | 1.09 to 2.02 | No/NP | Yes | I | I/Moderate |
| Barbui et al,80 2009 | Suicide attempt and completion in children and adolescents | SSRI/ non-SSRI users |
9.4 | 5 | OR: 1.92 (1.51 to 2.44) | 6531/ 61 522/ |
1.0 × 10−7 | 0 (.47) | 1.30 to 2.84 | No/NP | Yes | I | I/High |
| Khanassov et al,42 2018 | Osteoporotic fractures | SSRI/ non-SSRI users |
6.5 | 22 | RR: 1.67 (1.53 to 1.82) | 96 353/ 929 936 |
6.6 × 10−33 | 88 (<.001) | 1.17 to 2.38 | No/NP | Yes | II | II/Moderate |
| Man et al,48 2018 | ADHD in children | Prenatal exposure to AD/ no AD users |
2.4 | 7 | RR: 1.39 (1.21 to 1.61) | 57 552/ 2 886 904 |
5.1 × 10−6 | 79 (<.001) | 0.90 to 2.15 | No/NP | Yes | II | II/Moderate |
| Jiang et al,64 2015 | Upper GI bleeding | SSRI + other non-AD/ no SSRI use only + other non-AD |
1.3 | 15 | RR: 1.48 (1.32 to 1.67) | 43 571/ 08 060 |
1.3 × 10−10 | 61 (.001) | 1.00 to 2.20 | No/NP | Yes | II | II/Moderate |
| Wu et al,70 2013 | Osteoporotic fractures | TCA users/ non-TCA users |
NA | 11 | RR: 1.43 (1.29 to 1.58) | 178 237/ 740 768 |
1.9 × 10−12 | 77 (<.001) | 1.04 to 1.97 | Yes/no | Yes | II | II/Moderate |
| Oderda et al76 2012 | Hip fracture | TCA and/or SSRI users/no AD users |
NA | 14 | OR: 1.76 (1.49 to 2.08) | 47 762/ 198 820 |
1.9 × 10−11 | 92 (<.001) | 0.96 to 3.24 | Yes/no | Yes | II | II/Critically low |
| Studies Adjusted for Confounding by Indication | |||||||||||||
| Morales et al,51 2018 | Autism spectrum disorders (prepregnancy maternal exposure) | Any AD users/ no AD users |
1.1 | 3 | RR: 1.69 (1.39 to 2.05) | 3016/ 667 431 |
1.0 × 10−7 | 0 (.74) | 0.48 to 5.94 | No/no | Yes | I | II/Moderate |
| Barbui et al,80 2009 | Suicide attempt and completion in children and adolescents | SSRI/ non-SSRI users |
9.7 | 4 | OR: 2.04 (1.23 to 3 to 41) | 5522/ 55 124 |
0.006 | 16 (.31) | 0.47 to 8.81 | Yes/NP | No | I | IV/High |
| Khanassov et al,42 2018 | Osteoporotic fractures | SSRI/ non-SSRI users |
6.3 | 11 | RR: 1.61 (1.43 to 1.82) | 54 023/ 645 463 |
1.0 × 10−14 | 88 (<.001) | 1.08 to 2.41 | No/NP | Yes | II | II/Moderate |
| Wu et al,70 2013 | Osteoporotic fractures | TCA users/ non-TCA users |
NA | 7 | RR: 1.47 (1.23 to 1.69) | 156 374/ 659 389 |
5.0 × 10−8 | 62 (.02) | 0.98 to 2.22 | No/no | Yes | II | II/Moderate |
| High-Quality Primary Studies | |||||||||||||
| Morales et al,51 2018 | Autism spectrum disorders (prepregnancy maternal exposure) | Any AD users/ no AD users |
0. 8 | 7 | RR: 1.48 (1.29 to 1.71) | 22 877/ 2 400 720 |
6.8 × 10−8 | 24 (.24) | 1.09 to 2.02 | No/NP | Yes | I | I/Moderate |
| Andalib et al,52 2017 | Autism spectrum disorders (pregnancy maternal exposure; unadjusted estimates only) | SSRI/ non-SSRI users |
0.9 | 7 | OR: 1.84 (1.60 to 2.11) | 58 178/ 5 868 692 |
1.2 × 10−17 | 0 (.73) | 1.53 to 2.20 | No/NP | Yes | I | I/Moderate |
| Barbui et al,80 2009 | Suicide attempt and completion in children and adolescents | SSRI/ non-SSRI users |
3.6 | 4 | OR: 1.88 (1.47 to 2.40) | 5961/ 30 343 |
3.5 × 10−7 | 0 (.50) | 1.10 to 3.21 | No/NP | Yes | I | I/High |
| Khanassov et al,42 2018 | Osteoporotic fractures | SSRI/ non-SSRI users |
6.6 | 20 | RR: 1.70 (1.57 to 1.85) | 117 567/ 1 053 697 |
9.6 × 10−37 | 88 (<.001) | 1.23 to 2.35 | No/NP | Yes | II | II/Moderate |
| Man et al,48 2018 | ADHD in children | Prenatal exposure to AD/no AD users | 2.4 | 7 | RR: 1.39 (1.21 to 1.61) | 57 552/ 2 886 904 |
5.1 × 10−6 | 79 (<.001) | 0.90 to 2.15 | No/NP | Yes | II | II/Moderate |
| Jiang et al,58 2016 | Postpartum hemorrhage | Any AD users/ no AD users |
6.8 | 16 | RR: 1.32 (1.17 to 1.48) | 49 142/ 651 439 |
3.7 × 10−6 | 86 (<.001) | 0.84 to 2.08 | No/NP | Yes | II | II/Low |
| Huang et al,66 2014 | Preterm birth | Any AD users/ no AD users |
0.3 | 19 | RR: 1.86 (1.59 to 2.19) | 5116/ 1 658 666 |
5.3 × 10−14 | 52 (.004) | 1.16 to 3.00 | Yes/no | Yes | II | II/Moderate |
| Wu et al,70 2013 | Osteoporotic fractures | TCA users/ non-TCA users |
NA | 9 | RR: 1.46 (1.30 to 1.65) | 36 865/ 247 078 |
6.0 × 10−10 | 82 (<.001) | 0.99 to 2.15 | Yes/NP | Yes | II | II/Moderate |
| Oderda et al,76 2012 | Hip fracture | TCA and/or SSRI users/no AD users |
NA | 6 | OR: 1.59 (1.31 to 1.92) | 41 227/ 159 831 |
2.5 × 10−7 | 91 (<.001) | 0.82 to 3.07 | Yes/no | Yes | II | II/Critically low |
| Barbui et al,80 2009 | Suicide attempt and completion in adults | SSRI/ non-SSRI users |
4.5 | 7 | OR: 0.59 (0.48 to 0.72) | 7164/ 147 383 |
5.2 × 10−7 | 59 (.02) | 0.33 to 1.05 | No/NP | Yes | II | II/High |
| SSRI Studies | |||||||||||||
| Andalib et al,52 2017 | Autism spectrum disorders (pregnancy maternal exposure; unadjusted estimates only) | SSRI/ non-SSRI users |
0.9 | 7 | OR: 1.84 (1.60 to 2.11) | 58 178/ 5 868 692 |
1.2 × 10−17 | 0 (.73) | 1.53 to 2.20 | No/NP | Yes | I | I/Moderate |
| Barbui et al,80 2009 | Suicide attempt and completion in children and adolescents | SSRI/ non-SSRI users |
9.4 | 5 | OR: 1.92 (1.51 to 2.44) | 6531/ 61 522 |
1.0 × 10−7 | 0 (.47) | 1.30 to 2.84 | No/NP | Yes | I | I/High |
| Ross et al,71 2013 | Apgar score at 5 min | SSRI/ non-SSRI users |
5.7 | 13 | SMD: −0.27 (−0.37 to −0.16) | 1127/ 19 695 |
2.1 × 10−7 | 35 (.10) | 0.53 to 0.01 | No/no | Yes | II | I/Moderate |
| Khanassov et al,42 2018 | Osteoporotic fractures | SSRI/ non-SSRI users |
6.5 | 24 | RR: 1.67 (1.56 to 1.80) | 136 449/ 1 546 913 |
1.3 × 10−44 | 88 (<.001) | 1.23 to 2.27 | No/NP | Yes | II | II/Moderate |
| Huang et al,66 2014 | Preterm birth | SSRI/ non-SSRI users |
9.7 | 20 | RR: 1.73 (1.53 to 1.96) | 21 163/ 2 153 680 |
3.6 × 10−23 | 48 (.009) | 1.22 to 2.46 | Yes/NP | Yes | II | II/Moderate |
| Barbui et al,80 2009 | Suicide attempt and completion in adults | SSRI/ non-SSRI users |
3.5 | 7 | OR: 0.59 (0.48 to 0.72) | 7164/ 147 383 |
5.2 × 10−7 | 59 (.02) | 0.33 to 1.05 | No/NP | Yes | II | II/High |
| TCA Studies | |||||||||||||
| Fu et al,49 2018 | Cataract development | TCA/non-users or no users of any other AD | NA | 3 | OR: 1.19 (1.11 to 1.28) | 215 298/ 431 171 |
2.0 × 10−6 | 58 (.09) | 0.56 to 2.52 | No/NP | Yes | II | II/moderate |
| Wu et al,70 2013 | Osteoporotic fractures | TCA users/ non-TCA users |
1.4 | 12 | RR: 1.45 (1.31 to 1.60) | 178 237/ 831 912 |
6.2 × 10−13 | 76 (<.001) | 1.04 to 2.01 | Yes/no | Yes | II | II/Moderate |
| Other or Mixed AD Studies | |||||||||||||
| Morales et al,51 2018 | Autism spectrum disorders (prepregnancy maternal exposure) | Other or mixed/ no AD users |
0.8 | 7 | RR: 1.48 (1.29 to 1.71) | 22 877/ 2 400 720 |
6.8 × 10−8 | 24 (.24) | 1.09 to 2.02 | No/NP | Yes | I | I/Moderate |
| Huang et al,66 2014 | Preterm birth | Other or mixed/ no AD users |
0.4 | 8 | RR: 1.59 (1.31 to 1.93) | 3506/ 910 029 |
3.4 × 10−7 | 35 (.15) | 1.02 to 2.47 | No/NP | Yes | II | I/Moderate |
| Laporte et al,55 2017 | Severe bleeding at any site | Other or mixed/ no AD users |
6.8 | 44 | OR: 1.41 (1.27 to 1.57) | 190 016/ 1 512 411 |
2.2 × 10−10 | 90 (<.001) | 0.77 to 2.59 | No/no | Yes | II | II/Low |
| Jiang et al,58 2016 | Postpartum hemorrhage | Other or mixed/ no AD users |
6.8 | 17 | RR: 1.32 (1.17 to 1.48) | 49 155/ 651 715 |
3.3 × 10−6 | 85 (<.001) | 0.84 to 2.07 | No/NP | Yes | II | II/Low |
| Jiang et al,64 2015 | Upper GI bleeding | Other or mixed/no AD users |
0.7 | 22 | OR: 1.55 (1.35 to 1.78) | 56 182/ 592 508 |
9.2 × 10−12 | 89 (<.001) | 0.83 to 2.91 | No/no | Yes | II | II/Moderate |
| European Studies | |||||||||||||
| Andalib et al,52 2017 | Autism spectrum disorders (pregnancy maternal exposure; unadjusted estimates only) | SSRI/ non-SSRI users |
0.1 | 4 | OR: 1.80 (1.54 to 2.10) | 6394/ 5 741 029 |
1.1 × 10−13 | 0 (.39) | 1.28 to 2.53 | No/no | Yes | I | I/Moderate |
| Khanassov et al,42 2018 | Osteoporotic fractures | SSRI/ non-SSRI users |
6.5 | 12 | RR: 1.76 (1.68 to 1.87) | 92 760/ 1 228 807 |
2.3 × 10−86 | 67 (<.001) | 1.50 to 2.07 | No/no | Yes | II | II/Moderate |
| Jiang et al,64 2015 | Upper GI bleeding | SSRIs + other non-AD/ no SSRI use only + other no AD users |
0.4 | 14 | OR: 1.60 (1.33 to 1.93) | 46 594/ 236 085 |
4.8 × 10−7 | 86 (<.001) | 0.80 to 3.91 | No/NP | Yes | II | II/Moderate |
| Huang et al,66 2014 | Preterm birth | Any AD users/ no AD users |
0.9 | 7 | RR: 1.61 (1.36 to 1.92) | 17 518/ 1 984 543 |
5.6 × 10−8 | 56 (.03) | 1.02 to 2.55 | No/NP | Yes | II | II/Moderate |
| Wu et al,70 2013 | Osteoporotic fractures | TCA users/ non-TCA users |
NA | 6 | RR: 1.37 (1.19 to 1.56) | 164 476/ 724 914 |
6.6 × 10−6 | 69 (.007) | 0.91 to 2.05 | No/NP | Yes | II | II/Moderate |
| Oderda et al,76 2012 | Hip fracture | TCA and/or SSRI users/no AD users |
2.1 | 8 | OR: 1.74 (1.39 to 2.17) | 40 196/ 159 706 |
1.1 × 10−6 | 89 (<.001) | 0.88 to 3.42 | Yes/no | Yes | II | II/Critically low |
| North American Studies | |||||||||||||
| Khanassov et al,42 2018 | Osteoporotic fractures | SSRI/ non-SSRI users |
5.2 | 10 | RR: 1.56 (1.33 to 1.84) | 31 683/ 249 808 |
1.0 × 10−7 | 87 (<.001) | 0.91 to 2.70 | No/NP | Yes | II | II/Moderate |
| Huang et al,66 2014 | Preterm birth | Any AD users/ no AD users |
0.6 | 17 | RR: 1.70 (1.44 to 1.99) | 6129/ 928 528 |
1.2 × 10−10 | 29 (.12) | 1.17 to 2.45 | Yes/NP | Yes | II | II/Moderate |
| Wu et al,70 2013 | Osteoporotic fractures | TCA users/ non-TCA users |
NA | 6 | RR: 1.54 (1.32 to 1.81) | 13 761/ 84 583 |
7.3 × 10−8 | 76 (.001) | 0.95 to 2.51 | No/No | Yes | II | II/Moderate |
| Oderda et al,76 2012 | Hip fracture | TCA and/or SSRI users/no AD users |
2.5 | 8 | OR: 1.81 (1.51 to 2.18) | 8654/ 49 024 |
2.8 × 10−10 | 82 (<.001) | 1.01 to 3.27 | No/NP | Yes | II | II/Critically low |
Abbreviations: See Table 2. CES, class of evidence after sensitivity analysis.
Sensitivity analysis of studies located in other regions showed no associations supported by class I and II evidence.
Fifty-two associations (43.3%) had large heterogeneity (I2 > 50%), and the 95% prediction intervals excluded the null value for only 24 associations (20.0%). In 63 associations (52.5%), the effect sizes of the largest study were nominally statistically significant at P ≤ .05. Small-study effects were found for 17 associations (14.2%), and excess significance bias was observed for 9 associations (7.5%).
Main Analysis Grading
Convincing Evidence
Among the 120 associations, 3 (2.5%) were supported by convincing evidence, namely, the association between SSRI use and increased risk of suicide attempt or completion in children and adolescents80 as well as the association between exposure to any antidepressant before pregnancy and SSRIs during pregnancy and autism spectrum disorder51,52 (Table 2). The association with suicide risk reached the high-quality level based on AMSTAR 2, whereas the 2 associations with autism spectrum disorder reached moderate quality.
Highly Suggestive Evidence
Eleven associations (9.2%) had highly suggestive evidence of the association between any antidepressant use and increased risk of adverse health outcomes (Table 2). The adverse outcomes were attention-deficit/hyperactivity disorder in children, cataract development (associated with TCAs), severe bleeding at any site, upper gastrointestinal tract bleeding, postpartum hemorrhage, preterm birth, lower Apgar score at 5 minutes, osteoporotic fractures (1 associated with TCAs and 1 with SSRIs), and risk of hip fracture. Seven of these associations reached the moderate-quality level based on AMSTAR 2 (Table 2). One association with highly suggestive evidence, however, showed a decreased risk (ie, protective association) of suicide attempt or completion in adults,80 meeting a high-quality level based on AMSTAR 2. The effect sizes of those adverse outcomes supported by convincing and highly suggestive evidence were small and the prevalence was on average low (range, 0.1%-9.7%) as well (Tables 2 and 3).
Suggestive, Weak, and No Evidence
Suggestive evidence was found for 21 additional associations (17.5%) between antidepressant use and increased risk of adverse health outcomes (eTable 3 in the Supplement). For the remaining associations, either weak evidence (n = 39 [32.5%]) or no evidence (n = 46 [38.3%] was found (ie, all associations with P > .05) (eTables 4 and 5 in the Supplement).
Sensitivity Analyses
A sensitivity analysis limited to cohort studies, prospective cohort studies, studies controlled for confounding by indication, and North American studies showed that none of the associations within convincing evidence (class I) retained the same rank (Table 3). The most important change was within prospective cohort studies, with 1 association being upgraded to having convincing evidence (preterm birth associated with the use of any antidepressant).
Another association was upgraded to having convincing evidence (lower Apgar scores at 5 minutes) when the sensitivity analysis was limited to SSRIs. The association between antidepressant use and preterm birth was also upgraded to being supported by convincing evidence when the analysis was limited to other or mixed antidepressants (Table 3).
Findings from another sensitivity analysis, limited to excluded meta-analyses owing to overlap, agreed with the results of the main analysis (eResults and eTable 6 in the Supplement). The results of each sensitivity analysis are presented in the eResults in the Supplement, with the full list of covariates in eTable 7 in the Supplement.
Discussion
We reviewed 45 meta-analyses of observational studies and found that only a few of the 74 statistically significant associations between antidepressants and adverse health outcomes were supported by convincing evidence in the main and sensitivity analyses, namely, the association between antidepressant use and increased suicide attempt or completion in individuals younger than 19 years (SSRI studies),80 autism risk in the offspring,51,52 preterm birth,66 and neonatal adaptation.71 However, the few with convincing evidence associations did not reflect causality, and none of them remained at the convincing evidence level after accounting for confounding by indication. Overall, the results showed that the association between antidepressant use and adverse health outcomes was not supported by robust evidence and that the underlying disease likely inflated the findings in a relevant way.39,44
To our knowledge, this study is the first umbrella review that systematically assessed the potential risk of adverse health outcomes associated with antidepressant use across a large spectrum of published meta-analyses of observational studies, grading the evidence by using well-recognized criteria of credibility.22,23,32,33,36,37 The umbrella review approach has been applied to assess the associations between adverse health outcomes and other medical variables, such as dietary fiber consumption,37 serum uric acid level,23 and vitamin D concentration.22 This approach fits in a research field that is undeniably complex and uncertain, as conveyed here.22,23,32,33,36,37 The large median number of participants and cases per association allowed for robust classifications; the number of cases was greater than 1000 for 87 of the 120 associations. Quality ratings of the included meta-analyses with AMSTAR 2 also allowed for the confident interpretation of the results. Sensitivity analyses provided additional evidence from the cohort studies, high-quality studies, and studies controlled for a psychiatric condition, thus further increasing the reliability of the results.
These results need to be considered when contemplating the use of antidepressants in children and adolescents or integrated with efficacy data from RCTs. A network meta-analysis of RCTs in children and adolescents showed that no antidepressant medication was superior to placebo apart from fluoxetine, that several antidepressants had higher discontinuation rates compared with placebo, and that venlafaxine increased the risk of suicidality even in the short-term duration of an RCT.13 However, although 1 single antidepressant, venlafaxin (odds ratio, 7.7), was associated with an increased risk of suicidality compared with placebo, none of the other SSRIs or antidepressants had an association. Not only did placebo have a substantially reduced risk of suicidality (87% lower) compared with venlafaxine, but the same was true (and with a similar degree) for 5 antidepressants (duloxetine, escitalopram, fluoxetine, imipramine, and paroxetine), with an 81% to 86% reduced risk compared with venlafaxine; according to the network meta-analysis, these antidepressants were safe with regard to suicidality as an adverse effect.13 Moreover, antidepressants’ lack of superiority over placebo,12 especially in children, was associated with a high placebo response, which has been an increasing problem in RCTs in psychiatry. In addition, the increased suicidality in children and adolescents who use antidepressants may be associated with the unsuccessful reduction of depressive symptoms in suicidal individuals rather than a direct result of antidepressant use. Furthermore, the results showed that confounding by indication probably contributes to the safety concerns of using these drugs in children and adolescents. Besides, the risk-benefit evaluation in children and adolescents is different for antidepressants (predominantly SSRIs) when used for psychiatric conditions, such as anxiety disorders and obsessive-compulsive disorder.3,4,5,12
Conversely, we found highly suggestive evidence supporting the protective role of antidepressants against suicidality in adults,80 which is consistent with results of a network meta-analysis of RCTs in adults that showed all antidepressants were superior to placebo in reducing depressive symptoms.10 Similarly, meta-analyses support the efficacy of antidepressant use for anxiety disorders5 and obsessive-compulsive disorder3 in adults. In adults, the risk-benefit ratio must account for clear efficacy of antidepressants and protection against suicide, which should be balanced with other safety concerns that emerged from the present umbrella review. Overall, several adverse outcomes associated with antidepressant use supported by highly suggestive evidence (ie, poor bone status, gastrointestinal tract bleeding) can be prevented medically, as previously reported.82 Hence, the advantages of antidepressant use in adults and older adults may well trump preventable safety issues given their efficacy in treating various psychiatric disorders.3,4,5,12 Moreover, the association between antidepressant use and certain adverse health outcomes varied within specific age groups. For instance, increased risk of fractures applied predominantly to an older population (>65 years) already prone to poor bone status and multimorbidity84 and not to people aged 20 to 40 years.
Convincing evidence, before accounting for confounding by indication, that supported the association between antidepressant use and autism, as well as other offspring adverse health outcomes, may call for the restriction of antidepressant use during pregnancy among women with a high risk of relapse and severe clinical presentations. Warnings to avoid prescribing medications in early pregnancy have been issued.85 However, autism remains a rare event, with a prevalence from cohort studies of less than 1% according to data pooled in this study. The convincing evidence level was not confirmed when confounding by indication was considered, suggesting that the association between antidepressant use and autism as well as suicidality in youth and other outcomes may be due to the underlying disease rather than to the use of antidepressants,39,43,44,50 as shown in a recent umbrella review on risk factors for autism.86
Comparing 2 depression-matched groups with or without antidepressant exposure may be more methodologically accurate than adjusting analyses statistically. Several adverse outcomes had small effect sizes in addition to low prevalence and no proof of a causal relationship between antidepressants and adverse health outcomes.
Hence, given that a depressive episode itself can impair adolescents and both maternal and fetal health, individualized and shared clinical decisions about the risk-benefit ratio of antidepressant use during adolescence and pregnancy should be implemented, but adolescence and pregnancy should not be considered absolute contraindications to the use of antidepressants.
Further research in RCTs and with real-world samples matched for underlying disease is needed to confirm a possible causal association between antidepressants and adverse outcomes. Such research should consider dose-effect response; mechanistic processes; and patient-specific data such as age, clinical diagnoses, and severity of clinical condition. No absolute contraindication against the use of antidepressants is currently supported by convincing evidence.
Limitations
This study had several limitations. First, we did not grade the evidence from meta-analyses of RCTs, instead focusing on a portion of available evidence. However, evidence from RCTs was limited by the selection of healthier patients and frequent short-term follow-up, among other factors.16 Many severe adverse outcomes cannot be addressed in RCTs, and observational research is the most feasible method for low-frequency and long-term health risks.17 Nevertheless, observational studies are not free from bias, either.18,87 Their results yield associations, which do not imply causality. Second, results from main analyses were affected by various confounders owing to lack of randomization, potential channeling bias, and confounding by indication.17,18,80 Specifically, the nature of the control groups was only insufficiently characterized; according to the evidence, risk differences, when matched (and not adjusted) for the underlying psychiatric disorder, become smaller or nonsignificant.43,44,51 Thus, the association with suicidality may be contributed to by the antidepressants’ limited efficacy in suicidal children and adolescents, according to results from RCTs,19 rather than by antidepressant use increasing suicidality. The association between autism spectrum disorder and SSRI use during pregnancy52 included studies that were not adjusted for confounders, in contrast with weak evidence of an association between any antidepressant use during pregnancy and autism spectrum disorder when adjusted for confounders50 (eTable 4 in the Supplement). Third, no inference can be made about newer antidepressants (eg, vortioxetine hydrobromide) that have not been assessed in any of the included meta-analyses. Fourth, the data on cardiometabolic outcomes were insufficient, which is an emerging concern regarding the increased prescribing rates of antidepressants and is a crucial area for future research.88 Fifth, we used a grading system that can provide only warnings of the potential presence of systematic biases but cannot provide evidence of the nature and extent of these biases,16,32,33 just as umbrella reviews cannot supply any comparative ranking as in network meta-analyses.
Conclusions
The findings of this umbrella review are important in the context of increased antidepressant use worlwide.1,2 Convincing evidence was found for the association between antidepressant use and a few adverse health outcomes, yet the prevalence of those outcomes was low in general, and no association was supported by convincing evidence after confounding by indication. Future research is needed to identify whether a causal association exists between antidepressant use and adverse outcomes.
eAppendix 1. ePRISMA Checklist and MOOSE Checklist
eAppendix 2. Search Strings for PubMed
eTable 1. Articles Excluded After Full-Text Revision, With Reasons
eTable 2. Characteristics of Meta-analyses of Observational Studies Studying the Association Between Antidepressants and Risk of Any adverse Health Outcome
eTable 3. Suggestive Evidence (Class III) for the Association of Antidepressant Use and Risk of Adverse Health Outcomes in Meta-analyses of Observational Studies
eTable 4. Weak Evidence (Class IV) for the Association of Antidepressant Use and Risk of Adverse Health Outcomes in Meta-analyses of Observational Studies
eTable 5. No Evidence (Nonsignificant Associations, P > 0.05) for the Association of Antidepressant Use and Risk of Adverse Health Outcomes in Meta-analyses of Observational Studies
eTable 6. Sensitivity Analysis Results of Nonselected Meta-analyses Due to Overlap
eTable 7. List of Covariates Used for the Sensitivity Analysis Limited to Studies Adjusted for Covariates
eMethods. Supplementary Methods
eResults. Supplementary Results
References
- 1.Pratt LA, Brody DJ, Gu Q. Antidepressant use in persons aged 12 and over: United States, 2005-2008. NCHS Data Brief. 2011;(76):1-8. [PubMed] [Google Scholar]
- 2.Davey CG, Chanen AM. The unfulfilled promise of the antidepressant medications. Med J Aust. 2016;204(9):348-350. doi: 10.5694/mja16.00194 [DOI] [PubMed] [Google Scholar]
- 3.Skapinakis P, Caldwell DM, Hollingworth W, et al. . Pharmacological and psychotherapeutic interventions for management of obsessive-compulsive disorder in adults: a systematic review and network meta-analysis. Lancet Psychiatry. 2016;3(8):730-739. doi: 10.1016/S2215-0366(16)30069-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Locher C, Koechlin H, Zion SR, et al. . Efficacy and safety of selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors, and placebo for common psychiatric disorders among children and adolescents: a systematic review and meta-analysis. JAMA Psychiatry. 2017;74(10):1011-1020. doi: 10.1001/jamapsychiatry.2017.2432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bighelli I, Castellazzi M, Cipriani A, et al. . Antidepressants versus placebo for panic disorder in adults. Cochrane Database Syst Rev. 2018;4:CD010676. doi: 10.1002/14651858.CD010676.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leon AC. The revised warning for antidepressants and suicidality: unveiling the black box of statistical analyses. Am J Psychiatry. 2007;164(12):1786-1789. doi: 10.1176/appi.ajp.2007.07050775 [DOI] [PubMed] [Google Scholar]
- 7.Hammad TA, Laughren T, Racoosin J. Suicidality in pediatric patients treated with antidepressant drugs. Arch Gen Psychiatry. 2006;63(3):332-339. doi: 10.1001/archpsyc.63.3.332 [DOI] [PubMed] [Google Scholar]
- 8.Gibbons RD, Brown CH, Hur K, Davis J, Mann JJ. Suicidal thoughts and behavior with antidepressant treatment: reanalysis of the randomized placebo-controlled studies of fluoxetine and venlafaxine. Arch Gen Psychiatry. 2012;69(6):580-587. doi: 10.1001/archgenpsychiatry.2011.2048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carvalho AF, Sharma MS, Brunoni AR, Vieta E, Fava GA. The safety, tolerability and risks associated with the use of newer generation antidepressant drugs: a critical review of the literature. Psychother Psychosom. 2016;85(5):270-288. doi: 10.1159/000447034 [DOI] [PubMed] [Google Scholar]
- 10.Cipriani A, Furukawa TA, Salanti G, et al. . Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. Lancet. 2018;391(10128):1357-1366. doi: 10.1016/S0140-6736(17)32802-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gartlehner G, Gaynes BN, Amick HR, et al. . Comparative benefits and harms of antidepressant, psychological, complementary, and exercise treatments for major depression: an evidence report for a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016;164(5):331-341. doi: 10.7326/M15-1813 [DOI] [PubMed] [Google Scholar]
- 12.Bridge JA, Iyengar S, Salary CB, et al. . Clinical response and risk for reported suicidal ideation and suicide attempts in pediatric antidepressant treatment: a meta-analysis of randomized controlled trials. JAMA. 2007;297(15):1683-1696. doi: 10.1001/jama.297.15.1683 [DOI] [PubMed] [Google Scholar]
- 13.Cipriani A, Zhou X, Del Giovane C, et al. . Comparative efficacy and tolerability of antidepressants for major depressive disorder in children and adolescents: a network meta-analysis. Lancet. 2016;388(10047):881-890. doi: 10.1016/S0140-6736(16)30385-3 [DOI] [PubMed] [Google Scholar]
- 14.Moret C, Isaac M, Briley M. Problems associated with long-term treatment with selective serotonin reuptake inhibitors. J Psychopharmacol. 2009;23(8):967-974. doi: 10.1177/0269881108093582 [DOI] [PubMed] [Google Scholar]
- 15.Corrigan-Curay J, Sacks L, Woodcock J. Real-world evidence and real-world data for evaluating drug safety and effectiveness. JAMA. 2018;320(9):867-868. doi: 10.1001/jama.2018.10136 [DOI] [PubMed] [Google Scholar]
- 16.Solmi M, Correll CU, Carvalho AF, Ioannidis JPA. The role of meta-analyses and umbrella reviews in assessing the harms of psychotropic medications: beyond qualitative synthesis. Epidemiol Psychiatr Sci. 2018;27(6):537-542. doi: 10.1017/S204579601800032X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Benson K, Hartz AJ. A comparison of observational studies and randomized, controlled trials. N Engl J Med. 2000;342(25):1878-1886. doi: 10.1056/NEJM200006223422506 [DOI] [PubMed] [Google Scholar]
- 18.Kyriacou DN, Lewis RJ. Confounding by indication in clinical research. JAMA. 2016;316(17):1818-1819. doi: 10.1001/jama.2016.16435 [DOI] [PubMed] [Google Scholar]
- 19.Cipriani A, Barbui C, Geddes JR. Suicide, depression, and antidepressants. BMJ. 2005;330(7488):373-374. doi: 10.1136/bmj.330.7488.373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ioannidis JP. Integration of evidence from multiple meta-analyses: a primer on umbrella reviews, treatment networks and multiple treatments meta-analyses. CMAJ. 2009;181(8):488-493. doi: 10.1503/cmaj.081086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ioannidis J. Next-generation systematic reviews: prospective meta-analysis, individual-level data, networks and umbrella reviews. Br J Sports Med. 2017;51(20):1456-1458. doi: 10.1136/bjsports-2017-097621 [DOI] [PubMed] [Google Scholar]
- 22.Theodoratou E, Tzoulaki I, Zgaga L, Ioannidis JP. Vitamin D and multiple health outcomes: umbrella review of systematic reviews and meta-analyses of observational studies and randomised trials. BMJ. 2014;348:g2035. doi: 10.1136/bmj.g2035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li X, Meng X, Timofeeva M, et al. . Serum uric acid levels and multiple health outcomes: umbrella review of evidence from observational studies, randomised controlled trials, and Mendelian randomisation studies. BMJ. 2017;357:j2376. doi: 10.1136/bmj.j2376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Radua J, Ramella-Cravaro V, Ioannidis JPA, et al. . What causes psychosis? an umbrella review of risk and protective factors. World Psychiatry. 2018;17(1):49-66. doi: 10.1002/wps.20490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group . Preferred Reporting Items for Systematic Reviews and Meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stroup DF, Berlin JA, Morton SC, et al. ; Meta-analysis of Observational Studies in Epidemiology (MOOSE) Group . Meta-analysis of Observational Studies in Epidemiology: a proposal for reporting. JAMA. 2000;283(15):2008-2012. doi: 10.1001/jama.283.15.2008 [DOI] [PubMed] [Google Scholar]
- 27.Raglan O, Kalliala I, Markozannes G, et al. . Risk factors for endometrial cancer: an umbrella review of the literature. Int J Cancer. 2019;145(7):1719-1730. doi: 10.1002/ijc.31961 [DOI] [PubMed] [Google Scholar]
- 28.Shea BJ, Reeves BC, Wells G, et al. . AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. doi: 10.1136/bmj.j4008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177-188. doi: 10.1016/0197-2456(86)90046-2 [DOI] [PubMed] [Google Scholar]
- 30.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557-560. doi: 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. BMJ. 2011;342:d549. doi: 10.1136/bmj.d549 [DOI] [PubMed] [Google Scholar]
- 32.Bortolato B, Köhler CA, Evangelou E, et al. . Systematic assessment of environmental risk factors for bipolar disorder: an umbrella review of systematic reviews and meta-analyses. Bipolar Disord. 2017;19(2):84-96. doi: 10.1111/bdi.12490 [DOI] [PubMed] [Google Scholar]
- 33.Dragioti E, Evangelou E, Larsson B, Gerdle B. Effectiveness of multidisciplinary programmes for clinical pain conditions: an umbrella review. J Rehabil Med. 2018;50(9):779-791. doi: 10.2340/16501977-2377 [DOI] [PubMed] [Google Scholar]
- 34.Ioannidis JP, Trikalinos TA. An exploratory test for an excess of significant findings. Clin Trials. 2007;4(3):245-253. doi: 10.1177/1740774507079441 [DOI] [PubMed] [Google Scholar]
- 35.Ioannidis JPA. Clarifications on the application and interpretation of the test for excess significance and its extensions. J Math Psychol. 2013;57(5):184-187. doi: 10.1016/j.jmp.2013.03.002 [DOI] [Google Scholar]
- 36.Dragioti E, Karathanos V, Gerdle B, Evangelou E. Does psychotherapy work? an umbrella review of meta-analyses of randomized controlled trials. Acta Psychiatr Scand. 2017;136(3):236-246. doi: 10.1111/acps.12713 [DOI] [PubMed] [Google Scholar]
- 37.Veronese N, Solmi M, Caruso MG, et al. . Dietary fiber and health outcomes: an umbrella review of systematic reviews and meta-analyses. Am J Clin Nutr. 2018;107(3):436-444. doi: 10.1093/ajcn/nqx082 [DOI] [PubMed] [Google Scholar]
- 38.Masarwa R, Bar-Oz B, Gorelik E, Reif S, Perlman A, Matok I. Prenatal exposure to selective serotonin reuptake inhibitors and serotonin norepinephrine reuptake inhibitors and risk for persistent pulmonary hypertension of the newborn: a systematic review, meta-analysis, and network meta-analysis. Am J Obstet Gynecol. 2019;220(1):57.e1-57.e13. doi: 10.1016/j.ajog.2018.08.030 [DOI] [PubMed] [Google Scholar]
- 39.Halvorsen A, Hesel B, Ostergaard SD, Danielsen AA. In utero exposure to SSRIs and development of mental disorders: a systematic review and meta-analysis. Acta Psychiatr Scand. 2019;139(6):493-507. doi: 10.1111/acps.13030 [DOI] [PubMed] [Google Scholar]
- 40.Wang YC, Tai PA, Poly TN, et al. . Increased risk of dementia in patients with antidepressants: a meta-analysis of observational studies. Behav Neurol. 2018;2018:5315098. doi: 10.1155/2018/5315098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schweiger JU, Schweiger U, Hüppe M, et al. . The use of antidepressive agents and bone mineral density in women: a meta-analysis. Int J Environ Res Public Health. 2018;15(7):E1373. doi: 10.3390/ijerph15071373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Khanassov V, Hu J, Reeves D, van Marwijk H. Selective serotonin reuptake inhibitor and selective serotonin and norepinephrine reuptake inhibitor use and risk of fractures in adults: a systematic review and meta-analysis. Int J Geriatr Psychiatry. 2018;33(12):1688-1708. doi: 10.1002/gps.4974 [DOI] [PubMed] [Google Scholar]
- 43.Jiang HY, Peng CT, Zhang X, Ruan B. Antidepressant use during pregnancy and the risk of attention-deficit/hyperactivity disorder in the children: a meta-analysis of cohort studies. BJOG. 2018;125(9):1077-1084. doi: 10.1111/1471-0528.15059 [DOI] [PubMed] [Google Scholar]
- 44.Gao SY, Wu QJ, Sun C, et al. . Selective serotonin reuptake inhibitor use during early pregnancy and congenital malformations: a systematic review and meta-analysis of cohort studies of more than 9 million births. BMC Med. 2018;16(1):205. doi: 10.1186/s12916-018-1193-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Guan HB, Wei Y, Wang LL, Qiao C, Liu CX. Prenatal selective serotonin reuptake inhibitor use and associated risk for gestational hypertension and preeclampsia: a meta-analysis of cohort studies. J Womens Health (Larchmt). 2018;27(6):791-800. doi: 10.1089/jwh.2017.6642 [DOI] [PubMed] [Google Scholar]
- 46.Chappuis V, Avila-Ortiz G, Araújo MG, Monje A. Medication-related dental implant failure: systematic review and meta-analysis. Clin Oral Implants Res. 2018;29(suppl 16):55-68. doi: 10.1111/clr.13137 [DOI] [PubMed] [Google Scholar]
- 47.Na KS, Jung HY, Cho SJ, Cho SE. Can we recommend mirtazapine and bupropion for patients at risk for bleeding?: a systematic review and meta-analysis. J Affect Disord. 2018;225:221-226. doi: 10.1016/j.jad.2017.08.002 [DOI] [PubMed] [Google Scholar]
- 48.Man KKC, Chan EW, Ip P, et al. . Prenatal antidepressant exposure and the risk of attention-deficit hyperactivity disorder in children: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2018;86:1-11. doi: 10.1016/j.neubiorev.2017.12.007 [DOI] [PubMed] [Google Scholar]
- 49.Fu Y, Dai Q, Zhu L, Wu S. Antidepressants use and risk of cataract development: a systematic review and meta-analysis. BMC Ophthalmol. 2018;18(1):31. doi: 10.1186/s12886-018-0699-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhou XH, Li YJ, Ou JJ, Li YM. Association between maternal antidepressant use during pregnancy and autism spectrum disorder: an updated meta-analysis. Mol Autism. 2018;9:21. doi: 10.1186/s13229-018-0207-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Morales DR, Slattery J, Evans S, Kurz X. Antidepressant use during pregnancy and risk of autism spectrum disorder and attention deficit hyperactivity disorder: systematic review of observational studies and methodological considerations. BMC Med. 2018;16(1):6. doi: 10.1186/s12916-017-0993-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Andalib S, Emamhadi MR, Yousefzadeh-Chabok S, et al. . Maternal SSRI exposure increases the risk of autistic offspring: a meta-analysis and systematic review. Eur Psychiatry. 2017;45:161-166. doi: 10.1016/j.eurpsy.2017.06.001 [DOI] [PubMed] [Google Scholar]
- 53.Zhang TN, Gao SY, Shen ZQ, et al. . Use of selective serotonin-reuptake inhibitors in the first trimester and risk of cardiovascular-related malformations: a meta-analysis of cohort studies. Sci Rep. 2017;7:43085. doi: 10.1038/srep43085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Shen ZQ, Gao SY, Li SX, et al. . Sertraline use in the first trimester and risk of congenital anomalies: a systemic review and meta-analysis of cohort studies. Br J Clin Pharmacol. 2017;83(4):909-922. doi: 10.1111/bcp.13161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Laporte S, Chapelle C, Caillet P, et al. . Bleeding risk under selective serotonin reuptake inhibitor (SSRI) antidepressants: a meta-analysis of observational studies. Pharmacol Res. 2017;118:19-32. doi: 10.1016/j.phrs.2016.08.017 [DOI] [PubMed] [Google Scholar]
- 56.Gao SY, Wu QJ, Zhang TN, et al. . Fluoxetine and congenital malformations: a systematic review and meta-analysis of cohort studies. Br J Clin Pharmacol. 2017;83(10):2134-2147. doi: 10.1111/bcp.13321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Biffi A, Scotti L, Corrao G. Use of antidepressants and the risk of cardiovascular and cerebrovascular disease: a meta-analysis of observational studies. Eur J Clin Pharmacol. 2017;73(4):487-497. doi: 10.1007/s00228-016-2187-x [DOI] [PubMed] [Google Scholar]
- 58.Jiang HY, Xu LL, Li YC, Deng M, Peng CT, Ruan B. Antidepressant use during pregnancy and risk of postpartum hemorrhage: a systematic review and meta-analysis. J Psychiatr Res. 2016;83:160-167. doi: 10.1016/j.jpsychires.2016.09.001 [DOI] [PubMed] [Google Scholar]
- 59.Healy D, Le Noury J, Mangin D. Links between serotonin reuptake inhibition during pregnancy and neurodevelopmental delay/spectrum disorders: a systematic review of epidemiological and physiological evidence. Int J Risk Saf Med. 2016;28(3):125-141. doi: 10.3233/JRS-160726 [DOI] [PubMed] [Google Scholar]
- 60.Eke AC, Saccone G, Berghella V. Selective serotonin reuptake inhibitor (SSRI) use during pregnancy and risk of preterm birth: a systematic review and meta-analysis. BJOG. 2016;123(12):1900-1907. doi: 10.1111/1471-0528.14144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bérard A, Iessa N, Chaabane S, Muanda FT, Boukhris T, Zhao JP. The risk of major cardiac malformations associated with paroxetine use during the first trimester of pregnancy: a systematic review and meta-analysis. Br J Clin Pharmacol. 2016;81(4):589-604. doi: 10.1111/bcp.12849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Undela K, Parthasarathi G, John SS. Impact of antidepressants use on risk of myocardial infarction: a systematic review and meta-analysis. Indian J Pharmacol. 2015;47(3):256-262. doi: 10.4103/0253-7613.157112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Singh I, Achuthan S, Chakrabarti A, Rajagopalan S, Srinivasan A, Hota D. Influence of pre-operative use of serotonergic antidepressants (SADs) on the risk of bleeding in patients undergoing different surgical interventions: a meta-analysis. Pharmacoepidemiol Drug Saf. 2015;24(3):237-245. doi: 10.1002/pds.3632 [DOI] [PubMed] [Google Scholar]
- 64.Jiang HY, Chen HZ, Hu XJ, et al. . Use of selective serotonin reuptake inhibitors and risk of upper gastrointestinal bleeding: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2015;13(1):42-50.e3. doi: 10.1016/j.cgh.2014.06.021 [DOI] [PubMed] [Google Scholar]
- 65.Shin D, Oh YH, Eom CS, Park SM. Use of selective serotonin reuptake inhibitors and risk of stroke: a systematic review and meta-analysis. J Neurol. 2014;261(4):686-695. doi: 10.1007/s00415-014-7251-9 [DOI] [PubMed] [Google Scholar]
- 66.Huang H, Coleman S, Bridge JA, Yonkers K, Katon W. A meta-analysis of the relationship between antidepressant use in pregnancy and the risk of preterm birth and low birth weight. Gen Hosp Psychiatry. 2014;36(1):13-18. doi: 10.1016/j.genhosppsych.2013.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Huybrechts KF, Sanghani RS, Avorn J, Urato AC. Preterm birth and antidepressant medication use during pregnancy: a systematic review and meta-analysis. PLoS One. 2014;9(3):e92778. doi: 10.1371/journal.pone.0092778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Grigoriadis S, Vonderporten EH, Mamisashvili L, et al. . Prenatal exposure to antidepressants and persistent pulmonary hypertension of the newborn: systematic review and meta-analysis. BMJ. 2014;348:f6932. doi: 10.1136/bmj.f6932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Oh SW, Kim J, Myung SK, Hwang SS, Yoon DH. Antidepressant use and risk of coronary heart disease: meta-analysis of observational studies. Br J Clin Pharmacol. 2014;78(4):727-737. doi: 10.1111/bcp.12383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wu Q, Qu W, Crowell MD, Hentz JG, Frey KA. Tricyclic antidepressant use and risk of fractures: a meta-analysis of cohort and case-control studies. J Bone Miner Res. 2013;28(4):753-763. doi: 10.1002/jbmr.1813 [DOI] [PubMed] [Google Scholar]
- 71.Ross LE, Grigoriadis S, Mamisashvili L, et al. . Selected pregnancy and delivery outcomes after exposure to antidepressant medication: a systematic review and meta-analysis. JAMA Psychiatry. 2013;70(4):436-443. doi: 10.1001/jamapsychiatry.2013.684 [DOI] [PubMed] [Google Scholar]
- 72.Riggin L, Frankel Z, Moretti M, Pupco A, Koren G. The fetal safety of fluoxetine: a systematic review and meta-analysis. J Obstet Gynaecol Can. 2013;35(4):362-369. doi: 10.1016/S1701-2163(15)30965-8 [DOI] [PubMed] [Google Scholar]
- 73.Grigoriadis S, VonderPorten EH, Mamisashvili L, et al. . The effect of prenatal antidepressant exposure on neonatal adaptation: a systematic review and meta-analysis. J Clin Psychiatry. 2013;74(4):e309-e320. doi: 10.4088/JCP.12r07967 [DOI] [PubMed] [Google Scholar]
- 74.Myles N, Newall H, Ward H, Large M. Systematic meta-analysis of individual selective serotonin reuptake inhibitor medications and congenital malformations. Aust N Z J Psychiatry. 2013;47(11):1002-1012. doi: 10.1177/0004867413492219 [DOI] [PubMed] [Google Scholar]
- 75.Nikfar S, Rahimi R, Hendoiee N, Abdollahi M. Increasing the risk of spontaneous abortion and major malformations in newborns following use of serotonin reuptake inhibitors during pregnancy: a systematic review and updated meta-analysis. Daru. 2012;20(1):75. doi: 10.1186/2008-2231-20-75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Oderda LH, Young JR, Asche CV, Pepper GA. Psychotropic-related hip fractures: meta-analysis of first-generation and second-generation antidepressant and antipsychotic drugs. Ann Pharmacother. 2012;46(7-8):917-928. doi: 10.1345/aph.1Q589 [DOI] [PubMed] [Google Scholar]
- 77.Eom CS, Park SM, Cho KH. Use of antidepressants and the risk of breast cancer: a meta-analysis. Breast Cancer Res Treat. 2012;136(3):635-645. doi: 10.1007/s10549-012-2307-y [DOI] [PubMed] [Google Scholar]
- 78.Lee HK, Eom CS, Kwon YM, Ahn JS, Kim S, Park SM. Meta-analysis: selective serotonin reuptake inhibitors and colon cancer. Eur J Gastroenterol Hepatol. 2012;24(10):1153-1157. doi: 10.1097/MEG.0b013e328355e289 [DOI] [PubMed] [Google Scholar]
- 79.Cosgrove L, Shi L, Creasey DE, Anaya-McKivergan M, Myers JA, Huybrechts KF. Antidepressants and breast and ovarian cancer risk: a review of the literature and researchers’ financial associations with industry. PLoS One. 2011;6(4):e18210. doi: 10.1371/journal.pone.0018210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Barbui C, Esposito E, Cipriani A. Selective serotonin reuptake inhibitors and risk of suicide: a systematic review of observational studies. CMAJ. 2009;180(3):291-297. doi: 10.1503/cmaj.081514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hemels ME, Einarson A, Koren G, Lanctôt KL, Einarson TR. Antidepressant use during pregnancy and the rates of spontaneous abortions: a meta-analysis. Ann Pharmacother. 2005;39(5):803-809. doi: 10.1345/aph.1E547 [DOI] [PubMed] [Google Scholar]
- 82.National Institute for Health and Care Excellence Depression in adults. Clinical guideline (CG 90). http://www.nice.org.uk/. Published October 2009. Accessed November 2018.
- 83.Eckersley MJ, Sepehripour AH, Casula R, Punjabi P, Athanasiou T. Do selective serotonin reuptake inhibitors increase the risk of bleeding or mortality following coronary artery bypass graft surgery? a meta-analysis of observational studies. Perfusion. 2018;33(6):415-422. doi: 10.1177/0267659118765933 [DOI] [PubMed] [Google Scholar]
- 84.Brännström J, Lövheim H, Gustafson Y, Nordström P. Association between antidepressant drug use and hip fracture in older people before and after treatment initiation. JAMA Psychiatry. 2019;76(2):172-179. doi: 10.1001/jamapsychiatry.2018.3679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.British Medical Association; Royal Pharmaceutical Society . British National Formulary 57. London, UK: BMJ Group & RPS Publishing; 2009. [Google Scholar]
- 86.Kim JY, Son MJ, Son CY, et al. . Environmental risk factors and biomarkers for autism spectrum disorder: an umbrella review of the evidence. Lancet Psychiatry. 2019;6(7):590-600. doi: 10.1016/S2215-0366(19)30181-6 [DOI] [PubMed] [Google Scholar]
- 87.Howland RH. Antidepressant medication and pregnancy: time for randomized controlled trials. J Psychosoc Nurs Ment Health Serv. 2013;51(2):11-14. doi: 10.3928/02793695-20130109-01 [DOI] [PubMed] [Google Scholar]
- 88.Firth J, Siddiqi N, Koyanagi A, et al. . The Lancet Psychiatry Commission: a blueprint for protecting physical health in people with mental illness. Lancet Psychiatry. 2019;6(8):675-712. doi: 10.1016/S2215-0366(19)30132-4 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix 1. ePRISMA Checklist and MOOSE Checklist
eAppendix 2. Search Strings for PubMed
eTable 1. Articles Excluded After Full-Text Revision, With Reasons
eTable 2. Characteristics of Meta-analyses of Observational Studies Studying the Association Between Antidepressants and Risk of Any adverse Health Outcome
eTable 3. Suggestive Evidence (Class III) for the Association of Antidepressant Use and Risk of Adverse Health Outcomes in Meta-analyses of Observational Studies
eTable 4. Weak Evidence (Class IV) for the Association of Antidepressant Use and Risk of Adverse Health Outcomes in Meta-analyses of Observational Studies
eTable 5. No Evidence (Nonsignificant Associations, P > 0.05) for the Association of Antidepressant Use and Risk of Adverse Health Outcomes in Meta-analyses of Observational Studies
eTable 6. Sensitivity Analysis Results of Nonselected Meta-analyses Due to Overlap
eTable 7. List of Covariates Used for the Sensitivity Analysis Limited to Studies Adjusted for Covariates
eMethods. Supplementary Methods
eResults. Supplementary Results