Key Points
Question
How does the number needed to treat to prevent 1 atherosclerotic cardiovascular disease event compare among 5 major statin guidelines for primary prevention?
Findings
In this cohort study, statin eligibility, sensitivity, and specificity differed markedly between the guidelines. However, although the Canadian Cardiovascular Society, American College of Cardiology/American Heart Association, and National Institute for Health and Care Excellence guidelines would target statin therapy to more people than the US Preventive Services Task Force and the European Society of Cardiology/European Atherosclerosis Society, the number needed to treat to prevent 1 event was similar between guidelines.
Meaning
The Canadian Cardiovascular Society, American College of Cardiology/American Heart Association, and National Institute for Health and Care Excellence guidelines may prevent more atherosclerotic cardiovascular disease events despite having a similar number needed to treat to prevent 1 event as the US Preventive Services Task Force and the European Society of Cardiology/European Atherosclerosis Society guidelines.
Abstract
Importance
Five major guidelines on statin use for primary prevention of atherosclerotic cardiovascular disease (ASCVD) have been published since 2014: the National Institute for Health and Care Excellence (NICE; 2014), US Preventive Services Task Force (USPSTF; 2016), Canadian Cardiovascular Society (CCS; 2016), European Society of Cardiology/European Atherosclerosis Society (ESC/EAS; 2016), and American College of Cardiology/American Heart Association (ACC/AHA; 2018).
Objective
To compare the sensitivity, specificity, and estimated number needed to treat (NNT10) to prevent 1 ASCVD event in 10 years according to statin criteria from the 5 guidelines.
Design, Setting, and Participants
Population-based contemporary cohort study. Analyses were performed in the Copenhagen General Population Study, with a mean follow-up time of 10.9 years. We included 45 750 individuals aged 40 to 75 years. The participants were enrolled between 2003 and 2009 and were all free of ASCVD at baseline. Data were analyzed between January 1, 2019, and August 4, 2019.
Exposures
Statin treatment according to guideline criteria. We assumed a 25% relative reduction of ASCVD events per 38 mg/dL (to convert to millimoles per liter, multiply by 0.0259) reduction in low-density lipoprotein cholesterol.
Main Outcomes and Measures
Sensitivity and specificity for ASCVD events and the NNT10 to prevent 1 ASCVD event according to guideline criteria.
Results
Median age at baseline examination was 56 years, and 43% of participants were men (n = 19 870 of 45 750). During follow-up, we observed 4156 ASCVD events. Overall, 44% of individuals in Copenhagen General Population Study were statin eligible with CCS (n = 19 953 of 45 750), 42% with ACC/AHA (n = 19 400 of 45 750), 40% with NICE (n = 19 400 of 45 750), 31% with USPSTF (n = 13 966 of 45 750), and 15% with ESC/EAS (n = 6870 of 45 750). Sensitivity and specificity for ASCVD events were 68% (n = 2815 of 4156) and 59% (n = 24 456 of 41 594) for CCS, 70% (n = 2889 of 4156) and 60% (n = 25 083 of 41 594) for ACC/AHA, 68% (n = 2815 of 4156) and 63% (n = 26 213 of 41 594) for NICE, 57% (n = 2377 of 4156) and 72% (n = 30 005 of 41 594) for USPSTF, and 24% (n = 1001 of 4156) and 86% (n = 35 725 of 41 594) for ESC/EAS. The NNT10 to prevent 1 ASCVD using moderate-intensity and high-intensity statin therapy, respectively, was 32 and 21 for CCS criteria, 30 and 20 for ACC/AHA criteria, 30 and 20 for NICE criteria, 27 and 18 for USPSTF criteria, and 29 and 20 for ESC/EAS criteria.
Conclusions and Relevance
With similar NNT10 to prevent 1 event, the CCS, ACC/AHA, and NICE guidelines correctly assign statin therapy to many more of the individuals who later develop ASCVD compared with the USPSTF and ESC/EAS guidelines. Our results therefore suggest that the CCS, ACC/AHA, or NICE guidelines may be preferred for primary prevention.
This study compares the sensitivity, specificity, and estimated number needed to treat to prevent 1 atherosclerotic cardiovascular disease event in 10 years according to statin criteria from 5 major guidelines.
Introduction
Since 2014, 5 major guidelines/statements on statin use for primary prevention of atherosclerotic cardiovascular disease (ASCVD) have been published: the UK National Institute for Health and Care Excellence (NICE; 2014),1 US Preventive Services Task Force statement (USPSTF; 2016, named a statement but referred to as a guideline in the rest of this article),2 Canadian Cardiovascular Society (CCS; 2016),3 European Society of Cardiology/European Atherosclerosis Society (ESC/EAS; 2016),4 and American College of Cardiology/American Heart Association (ACC/AHA; 2018).5
Although these guidelines are founded on the same evidence originating predominantly from multiple randomized clinical trials (RCTs) of statin therapy for primary prevention of ASCVD, their recommendations for who should be treated with statins differ markedly.6,7,8,9 Specifically, the guidelines recommend using different prediction models for ASCVD risk assessment as well as different risk thresholds and low-density lipoprotein cholesterol (LDL-C) criteria for prescription of statin therapy. We have previously7 compared the guidelines regarding their potential for overall ASCVD prevention in the general population, showing that the guidelines that recommend more individuals to use statins for primary prevention will prevent more events than the guidelines recommending statin use by fewer individuals.7 However, to our knowledge, the ability of the guidelines to correctly assign statin therapy has not been compared. Theoretically, it could be that the higher preventive potential with the more statin-liberal guidelines come with the downside of treating many people at low ASCVD risk, giving rise to higher numbers needed to treat (NNT) to prevent 1 ASCVD event compared with the more statin-conservative guidelines.
In this study, we therefore performed a comparison of the 5 major guidelines regarding their ability to correctly assign statin therapy, that is, the sensitivity and specificity for ASCVD events as well as the NNT to prevent 1 ASCVD event according to statin eligibility criteria with each guideline. We used both the risk scores and the applied treatment thresholds to examine the performance of the overall guideline. This is how the guidelines are intended for use, and this approach provides a clear view of their potential effectiveness.
Methods
Copenhagen General Population Study
The Copehnagen General Population Study (CGPS) is an ongoing prospective cohort study of the Danish general population.10,11,12 Enrollment began in November 2003, and participants are randomly selected through the Danish Civil Registration system to reflect the adult Danish general population. The CGPS covers selected regions of Copenhagen, including surrounding countryside, and both from low-income and high-income areas. All individuals 40 years and older in these regions were invited along with a random selection of 25% of individuals aged 20 to 39 years. For this study, we included individuals of Danish descent aged 40 to 75 years (individuals younger than 40 years and older than 75 years were excluded to comply with guidelines), enrolled consecutively from 2003 to 2009. We excluded individuals with preexisting ASCVD, statin use, or with missing information at baseline examination. The study was approved by Herlev and Gentofte Hospital and by the Danish National Committee on Health Research Ethics. Written informed consent was obtained from all individuals.
Recommendations for Statin Therapy by the 5 Guidelines
The treatment criteria for primary prevention with statins according to the 5 guidelines are summarized in Table 1 and described in detail in the eMethods in the Supplement. These criteria are strong or class A recommendations.
Table 1. Statin Eligibility Criteria According to 5 Major ASCVD Primary Prevention Guidelines.
| Criteria | NICE | USPSTF | CCS | ESC/EAS | ACC/AHA |
|---|---|---|---|---|---|
| Lipid-based | |||||
| Cholesterol level | LDL-C >190mg/dL or TC >290 mg/dL | NA | LDL-C ≥193 mg/dL | LDL-C >232 mg/dL or TC >309 mg/dL | LDL-C ≥190 mg/dL |
| Risk-based | |||||
| Age range, y | 40-75 | 40-75 | 40-75 | 40-65 | 40-7 |
| Eligibility | QRISK2 ≥ 10% predicted 10-y risk of any ASCVD or nondialysis–dependent CKD | PCE ≥10% predicted 10-y risk of any ASCV plus ≥1 CVD risk factora | FRS ≥20% predicted 10-y risk of any ASCVD or age 40-75 y; FRS≥10% to <20% predicted 10-y risk of any ASCVD; LDL-C ≥135 mg/dLb or diabetes or CKD (age ≥50 y) and eGFR level <60 mL/min/1.73m2 | LDL-C level ≥155 mg/dL; SCORE 5% to <10% predicted 10-y risk of fatal ASCVD or age 40-65 y; LDL-C ≥97 mg/dL; SCORE ≥10% predicted 10-y risk of fatal ASCVD or diabetes; or nondialysis–dependent CKD and eGFR level <60 mL/min/1.73m2 | PCE ≥7.5% predicted 10-y risk of any ASCVD; LDL-C 70-189 mg/dL or diabetes (plus LDL-C level ≥70 mg/dL); risk-enhancersc: family history of ASCVD, persistently elevated LDL-C levels ≥160 mg/dL, CKD, metabolic syndrome, persistently elevated triglycerides ≥175 mg/dL, hs-CRP levels ≥2.0 mg/dL; Lp(a) levels >50mg/dL, apoB levels ≥130mg/dL, and ankle-brachial index <0.9 |
Abbreviations: ACC, American College of Cardiology; ASCVD, atherosclerotic cardiovascular disease; AHA, American Heart Association; apoB, apolipoprotein B; CCS, Canadian Cardiovascular Society; CKD, chronic kidney disease; CVD, cardiovascular disease; ESC, European Society of Cardiology; EAS, European Atherosclerosis Society; eGFR, estimated glomerular filtration rate; FRS, Framingham Risk Score; LDL-C, low-density lipoprotein cholesterol; Hs-CRP, high-sensitivity C-reactive protein; Lp(a), Lipoprotein(a); NICE, National Institute for Health and Care Excellence; PCE, pooled cohorts equations; TC, total cholesterol; USPSTF, US Preventive Services Task Force.
SI conversion factor: To convert apoB to grams per liter, multiply by 0.01; cholesterol levels to millimoles per liter, multiply by 0.0259; Lp(a) to micromoles per liter, multiply by 0.0357; triglycerides to millimoles per liter, multiply by 0.0113.
USPSTF CVD risk factors include dyslipidemia (LDL-C levels >130 mg/dL or high-density lipoprotein cholesterol levels <40 mg/dL), diabetes, hypertension, and smoking.
Or non–high-density lipoprotein cholesterol levels at least 166 mg/dL or men 50 years and older and women 60 years and older with LDL-C levels less than 135 mg/dL but with a CVD risk factor.
Risk-enhancing factors to help guide class IIb statin allocation in the ACC/AHA guidelines. Chronic inflammatory conditions, history of premature menopause, and preeclampsia are also ACC/AHA defined risk enhancers, but information on these variables were not available for this study.
Because the USPSTF, ESC/EAS, and ACC/AHA guidelines also provide weaker class IIa (ESC/EAS), C (USPSTF), or IIb (ACC/AHA) recommendations for statin therapy, we assessed the performance of these criteria in sensitivity analyses. The USPSTF C recommendation lowers the pooled cohort equations (PCE) threshold to 7.5%. The ESC/EAS class IIa recommendation lowers the LDL-C–based threshold to at least 70 mg/dL (to convert to millimoles per liter, multiply by 0.0259) for individuals with a Systematic Coronary Risk Evaluation (SCORE) risk of at least 10% and to at least 97 mg/dL for individuals with a SCORE risk of at least 5% and less than 10%.4 Further, although the ESC/EAS guidelines discourage uncritical use of statins in adults older than 60 years even if SCORE risk is very high (≥10%) because “their age-specific risk is normally around these levels, even when other cardiovascular risk factor levels are ‘normal,’”4 the ESC/EAS guidelines do provide Class IIa recommendation for older persons (>65 years) in the presence of hypertension, smoking, dyslipidemia, or diabetes. Finally, the ACC/AHA class IIb recommendation lowers the PCE threshold from 7.5% to 5% (borderline risk) if risk-enhancing factors are present (Table 1 and eTable 1 in the Supplement).5 Of the ACC/AHA risk-enhancing factors, information on premature menopause, preeclampsia, and chronic inflammatory conditions were not available for this study.
Atherosclerotic Cardiovascular Disease Events
We defined any ASCVD events as nonfatal myocardial infarction (MI), fatal coronary heart disease (CHD), and stroke. These outcomes were identified by linkage to the national Danish Patient Registry covering all Danish hospitals and to the national Danish Cause of Death Registry using the following International Statistical Classification of Diseases and Related Health Problems, Tenth Revision codes: I21-I22 for nonfatal MI and I20-I25 for fatal CHD. Possible stroke events (among hospitalized patients) were identified with the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision codes I60, I61, I63, I64, and G45 and subsequently individually validated using the World Health Organization definition of stroke, ie, an acute disturbance of focal or global cerebral function with symptoms lasting longer than 24 hours or leading to death, with presumably no other reasons than of vascular origin.13
All individuals in Denmark are assigned a personal identification number at birth or immigration by which they can be traced in the national registries; therefore, follow-up is without losses. Thus, we followed up each individual from the time of participation in the population study until 1 of the following events occurred: ASCVD (n = 2320), death (n = 1800), emigration (n = 169), or end of follow-up (December 7, 2018).
Statistical Analyses
Analyses were performed using Stata, version 13.1 SE (StataCorp LP). Baseline characteristics are presented as proportions for categorical variables and as medians (interquartile range) for continuous variables. The P value level of significance was .05, and all P values were 2-sided.
First, we calculated 10-year risk ASCVD events for each individual using the guideline-recommended prediction models, that is, PCE for ACC/AHA and USPSTF, Framingham Risk Score for CCS, QRISK2 for NICE, and SCORE for ESC/EAS (fatal ASCVD only). Then, the proportion of individuals eligible for statin therapy by the ACC/AHA, NICE, USPSTF, CCS, and ESC/EAS guidelines was calculated using class I recommendations or strong recommendations from each guideline (Table 1).
Second, to compare the clinical performance of the 5 guidelines, we calculated sensitivity and specificity overall and across 5-year age groups for ASCVD events occurring during follow-up in those respectively with and without statin eligibility. Third, we estimated the NNT in 10 years (NNT10) to prevent 1 ASCVD event through statin assignment according to each guideline. For these analyses, we first determined the total number of events among all individuals aged 40 years to 75 years as well as among individuals eligible for statin therapy by each guideline using 10-year Kaplan-Meier estimates. For estimation of the absolute risk reduction achieved by following each guideline, we assumed a 25% relative risk/event reduction per 38.7-mg/dL reduction in LDL-C among individuals free of ASCVD.14 In this analysis, high-intensity and moderate-intensity statin therapy was expected to reduce LDL-C by approximately 50% and approximately 30%, respectively.15 The calculations of relative risk reductions with LDL-C lowering was appropriately scaled on the natural logarithm scale:
| Relative Risk Reduction = (1 − 0.75[LDL-C lowering in mg/dL]/38.7) |
The NNT10 to prevent 1 ASCVD event was then calculated as the reciprocal of the absolute risk differences in 10-year event rates.16 We also estimated the number of additional diabetes cases by assuming 100 and 200 additional cases in 10 years per 10 000 individuals treated with moderate-intensity and high-intensity statins.17
Results
Baseline characteristics of the 45 750 individuals aged 40 to 75 years included in this study are presented in Table 2 and for men and women separately in eTables 2 and 3 in the Supplement. All were free of statin use and ASCVD at baseline. During a mean follow-up of 10.9 years, we observed 4156 ASCVD events.
Table 2. Baseline Characteristics of All Individuals From the Copenhagen General Population Study and of Those Eligible for Statin Therapy According to 5 Major Statin Guidelines for Primary Prevention of Atherosclerotic Cardiovascular Disease.
| Characteristics | All Individuals | Statin Eligibility According to Guidelines | ||||
|---|---|---|---|---|---|---|
| CCS | ACC/AHA | NICE | USPSTF | ESC/EAS | ||
| Individuals, No. | 45 750 | 19 953 | 19 400 | 18 196 | 13 966 | 6870 |
| Male, No. (%) | 19 870 (43) | 11 431 (57) | 11 785 (61) | 9947 (55) | 9200 (66) | 2547 (37) |
| Age, median (IQR), y | 56 (48-64) | 62 (56-68) | 64 (58-70) | 65 (60-70) | 66 (61-70) | 63 (58-68) |
| Blood pressure, median (IQR), mm Hg | ||||||
| Systolic | 139 (125-152) | 150 (135-163) | 148 (135-162) | 148 (135-162) | 152 (140-166) | 148 (133-164) |
| Diastolic | 84 (77-90) | 88 (80-95) | 87 (80-95) | 85 (80-94) | 88 (80-95) | 86 (80-95) |
| Plasma cholesterol, median (IQR), mg/dL | ||||||
| Total cholesterol, mg/dL | 220 (197-247) | 244 (220-267) | 236 (213-267) | 236 (209-263) | 236 (209-263) | 252 (224-286) |
| HDL cholesterol, mg/dL | 61 (49-76) | 55 (46-68) | 56 (45-71) | 56 (45-71) | 55 (43-70) | 62 (50-77) |
| LDL cholesterol, mg/dL | 128 (108-155) | 147 (131-170) | 143 (120-170) | 139 (116-162) | 143 (120-166) | 155 (128-182) |
| Current smoker, No. (%) | 9907 (21) | 5981 (30) | 6140 (32) | 5497 (30) | 4987 (36) | 1942 (28) |
| Diabetes, No. (%) | 861 (2) | 861 (4) | 795 (4) | 817 (4) | 631 (5) | 861 (13) |
| 10-y PCE risk, median (IQR), % | 5.4 (1.9-12.6) | 13.3 (7.6-20.9) | 14.2 (9.9-21.2) | 15.0 (10.5-22.0) | 17.6 (13.2-24.4) | 13.7 (6.2-21.8 |
Abbreviations: ACC, American College of Cardiology; AHA, American Heart Association; ASCVD, atherosclerotic cardiovascular disease; CCS, Canadian Cardiovascular Society; ESC, European Society of Cardiology; EAS, European Atherosclerosis Society; HDL, high-density lipoprotein; IQR, interquartile range; LDL, low-density lipoprotein; NICE, National Institute for Health and Care Excellence; PCE, pooled cohort equations; USPSTF, US Preventive Services Task Force.
SI conversion factor: To convert cholesterol levels to millimoles per liter, multiply by 0.0259.
Statin Eligibility
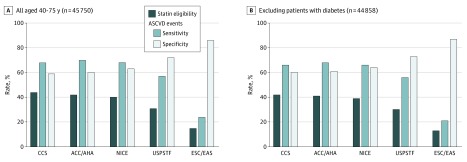
Statin eligibility was found for 44% of individuals according to CCS (n = 19 953 of 45 750), for 42% according to ACC/AHA (n = 19 400 of 45 750), for 40% according to NICE (n = 19 400 of 45 750), for 31% according to USPSTF (n = 13 966 of 45 750), and for 15% according to ESC/EAS (n = 6870 of 45 750) (Figure 1A). Similar results were obtained after excluding individuals with diabetes (Figure 1B) and in men and women separately (eFigure 1 in the Supplement). The overlap in statin eligibility between guidelines are visualized in Venn diagrams in eFigure 2 in the Supplement.
Figure 1. Clinical Performance of 5 Major Guidelines on Cholesterol Treatment for Primary Prevention of Atherosclerotic Cardiovascular Disease (ASCVD): Statin Eligibility, Sensitivity, and Specificity.
ASCVD events were defined as nonfatal myocardial infarction, fatal coronary heart disease, and stroke. ACC indicates American College of Cardiology; AHA, American Heart Association; CCS, Canadian Cardiovascular Society; ESC, European Society of Cardiology; EAS, European Atherosclerosis Society; NICE, National Institute for Health and Care Excellence; USPSTF, US Preventive Services Task Force.
Sensitivity and Specificity for ASCVD Events
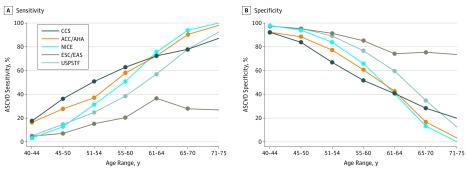
Sensitivity and specificity for future ASCVD events by the 5 guidelines were inversely correlated. Overall sensitivity and specificity for ASCVD events in those respectively with and without statin eligibility were 68% (n = 2815 of 4156) and 59% (n = 24 456 of 41 594) for CCS, 70% (n = 2889 of 4156) and 60% (n = 25 083 of 41 594) for ACC/AHA, 68% (n = 2815 of 4156) and 63% (n = 26 213 of 41 594) for NICE, 57% (n = 2377 of 4156) and 72% (n = 30 005 of 41 594) for USPSTF, and 24% (n = 1001 of 4156) and 86% (n = 35 725 of 41 594) for ESC/EAS (Figure 1). In younger individuals, CCS and ACC/AHA guidelines had the highest sensitivity (and lowest specificity), while ACC/AHA and NICE guidelines had the highest sensitivity (and lowest specificity) among elderly individuals (Figure 2). Similar relative differences between the guidelines were observed in men and women separately, although guidelines generally had higher sensitivity (and lower specificity) in men (eFigures 3 and 4 in the Supplement). As shown in eTable 4 in the Supplement, positive predictive values ranged from 14% (CCS) to 17% (USPSTF) while negative predictive values ranged from 92% (ESC/EAS) to 95% (CCS, ACC/AHA, and NICE).
Figure 2. Sensitivity and Specificity for Primary Prevention of Atherosclerotic Cardiovascular Disease (ASCVD) According to 5 Major Guidelines Stratified by 5-Year Age Groups.
ACC indicates American College of Cardiology; AHA, American Heart Association; CCS, Canadian Cardiovascular Society; ESC, European Society of Cardiology; EAS, European Atherosclerosis Society; NICE, National Institute for Health and Care Excellence; USPSTF, US Preventive Services Task Force.
Event Rates and NNT to Prevent 1 Event
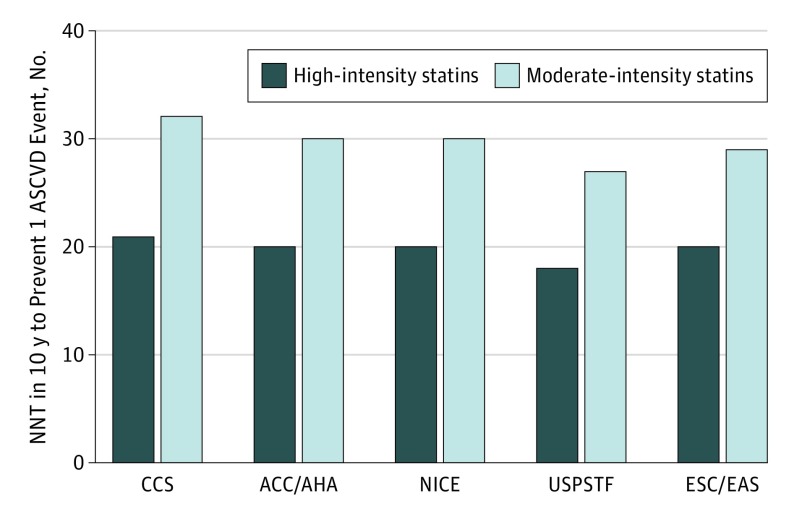
We next assessed event rates in statin-eligible individuals as well as the NNT10 to prevent 1 ASCVD event during 10 years. Overall, there was no major difference in event rates in individuals eligible for statin therapy with different guidelines (eTable 5 in the Supplement). Consistently, the NNT10 to prevent 1 ASCVD event was similar between guidelines. Using high-intensity statins, the NNT10 varied from 18 with the USPSTF guideline to 21 with the CCS guideline. The corresponding numbers for the moderate-intensity statins were 27 and 32, respectively (Figure 3 and eTable 6 in the Supplement). Importantly, the estimated number of prevented ASCVD events was several times higher than the expected additional diabetes cases with all guidelines (eFigure 5 in the Supplement).
Figure 3. Number Needed to Treat (NNT) to Prevent 1 Atherosclerotic Cardiovascular Disease (ASCVD) Event With the 5 Major Guidelines on Statin Use for Primary Prevention.
ACC indicates American College of Cardiology; AHA, American Heart Association; CCS, Canadian Cardiovascular Society; ESC, European Society of Cardiology; EAS, European Atherosclerosis Society; LDL-C, low-density lipoprotein cholesterol; NICE, National Institute for Health and Care Excellence; RRR, relative risk reduction; USPSTF, US Preventive Services Task Force.
Sensitivity Analysis
Because the ACC/AHA guidelines are somewhat vague regarding the need of risk-enhancers for class I statin eligibility when PCE risk is 7.5% to 20%, we recalculated the results for class I statin therapy assuming that such individuals should have at least 1 risk enhancer to be statin eligible. As shown in eFigure 6 in the Supplement, statin eligibility fell to 33% (−9%), sensitivity fell to 60% (−10%), and specificity increased to 69% (10%), while the NNTs remained similar to the main analyses.
In another sensitivity analysis, we also included class IIa and IIb recommendations for statin eligibility with the ESC/EAS and ACC/AHA guidelines and C recommendation with the USPSTF guideline. As shown in eFigure 7 in the Supplement, statin eligibility increased to 50% (+8%) of the population with ACC/AHA, to 38% (+7%) with USPSTF, and to 29% (+14%) with ESC/EAS guidelines. However, the NNTs remained similar to the main analyses (eFigure 8 in the Supplement).
Finally, we performed the analyses in 2 different age groups: individuals aged 40 years to 65 years (to comply with the age range of the ESC/EAS SCORE calculator) and individuals aged 66 years to 75 years. As seen in eTables 7 and 8 in the Supplement and eFigures 9 to 11 in the Supplement, the NNTs were generally higher in those aged 40 years to 65 years than in those aged 66 years to 75 years, but no major difference between guidelines was found.
Discussion
To our knowledge, this is the first study to compare the ability of the 5 major statin guidelines to correctly assign statin therapy for primary prevention of cardiovascular disease; that is, the 2014 NICE, 2016 USPSTF, 2016 CCS, 2016 ESC/EAS, and the 2018 ACC/AHA guidelines.1,2,3,4,5 Our data show that although statin eligibility and sensitivity for ASCVD events differ markedly, the estimated NNT10 to prevent 1 event in 10 years is nearly identical for the 5 guidelines. These results are important for clinical practice because they demonstrate that the greater potential for reducing ASCVD burden in the population with the more statin-liberal guidelines is not counteracted by higher NNTs to prevent ASCVD events, as compared with the more statin-conservative guidelines.
The purpose of preventive statin guidelines is to reduce the burden of ASCVD in the population. Guidelines should therefore provide recommendations that target treatment to as many individuals as possible who are destined to develop ASCVD. In all 5 guidelines, treatment decisions are based on the predicted absolute ASCVD risk and/or on the presence of high-risk markers such as diabetes.1,2,3,4,5 Owing to the growing evidence base, documented long-term safety, and available cheap generics, most guidelines have lowered the treatment threshold since 2013. Although based on trial evidence, the expanded indication for statins may result in treatment of many lower-risk individuals, theoretically giving rise to high NNTs to prevent 1 ASCVD event (the inverse of absolute risk reduction) compared with more statin-conservative guidelines. We here show that this is not the case.
The NNT to prevent 1 event is a metric of treatment benefit that encompasses both absolute and relative risk reductions, and it is commonly used to compare treatment strategies. Although the NNT have previously been reported for some of the guidelines, they have never been compared in a head-to-head fashion in the same general population cohort. Indeed, care must be taken to specify the population under study as well as the end points and time frames of interest when comparing NNT from study to study. Perhaps the most revealing results from our analyses is that, while the CCS, ACC/AHA, and NICE guidelines would treat many more people than the USPSTF and ESC/EAS guidelines, the CCS, ACC/AHA, and NICE strategies would also target statin therapy to many more of the individuals who develop ASCVD. As a result, more ASCVD events are prevented by the CCS, ACC/AHA, and NICE guidelines, resulting somewhat surprisingly in NNT10 that is nearly identical to those achieved by the USPSTF and ESC/EAS guidelines. Thus, assuming negligible harm from statin therapy and low cost for the drugs, the CCS, ACC/AHA, and NICE strategies seem to be the superior guidelines for clinical practice for primary prevention of ASCVD.
The estimated NNT10 using high-intensity statins was 18 to 21 across the 5 guidelines in our study. These NNTs are lower than those reported in primary-prevention RCTs of statin therapy. For example, the 5-year NNTs in The West of Scotland Coronary Prevention Study (WOSCOPS), Air Force/Texas Coronary Atherosclerosis Prevention Study (AFCAPS/TexCAPS), and Heart Outcomes Prevention Evaluation-3 (HOPE-3) were 63, 44, and 100, respectively.18,19,20,21 There are likely several reasons for the favorable NNTs in our study. First, many individuals enrolled in RCTs are low-risk individuals who do not meet guideline treatment criteria. Indeed, using both the Multi-Ethnic Study of Atherosclerosis (MESA) and the CGPS, we have previously shown that 23% to 28% of participants from these cohorts met inclusion criteria from at least 1 RCT without being eligible for statins by the ACC/AHA guidelines because of low ASCVD risk.11,22 Second, the NNTs from RCTs are based on intention-to-treat analyses irrespective of whether participants are adherent to treatment.17 Third, primary prevention studies have mostly used low-intensity to intermediate-intensity statins, with less effect on ASCVD prevention than high-intensity statins.
Notably, our estimates for the NNT with statin guidelines are lower than the NNT to prevent 1 event for aspirin or antihypertensive therapy generally reported in primary-prevention RCTs.16,23 The A Study of Cardiovascular Events in Diabetes (ASCEND) and Aspirin in Reducing Events in the Elderly (ASPREE) studies have questioned the net benefit of aspirin in primary-prevention patients.24,25,26 Although antihypertensive therapy has been clearly shown to reduce ASCVD risk among patients with known ASCVD, the benefits of blood pressure lowering in primary-prevention individuals with mild hypertension are less clear because, to our knowledge, only 1 RCT (HOPE-3) has been performed in this population.27 However, HOPE-3 did not show benefit of blood pressure treatment, but this may be caused by the weak blood pressure–lowering effect in the treatment arm (6 mm Hg lower in treatment vs placebo arm).28,29 In a meta-analysis30 of earlier RCTs treating uncomplicated hypertension in higher-risk middle-aged individuals, a 5-year NNT of 86 was found. The NNTs in our strictly primary-prevention cohort are similar to those estimated in an analysis31 investigating the effect of the new 2018 ACC/AHA blood pressure guideline among individuals older than 45 years with much higher ASCVD risk (combined primary and secondary prevention).
We have previously shown that the potential reduction of ASCVD events in the population is highest for the CCS, ACC/AHA, and NICE guidelines, where 32% to 34% of all ASCVD events would be prevented compared with 18% to 27% for ESC/EAS and USPSTF guidelines.7 Our completely new analyses demonstrate that this is achieved with NNTs that are similar to those achieved by assigning statins according to the more statin-conservative guidelines. Thus, when taking the guidelines as a whole, what seems to work best is the combination of an appropriately calibrated risk score that addresses an end point of interest (ie, ASCVD events, not just CVD death as in the ESC/EAS SCORE calculator) together with evidence-based and risk/benefit-based treatment thresholds.
Limitations and Strengths
A limitation of our study is that we only studied white European individuals living in a high-income country, and extrapolation of our results to individuals living in low-income and middle-income countries and to other ethnicities should be done cautiously because their risk factor level may differ. However, we are not aware of data to suggest that this result should not apply to people of other races/ethnicities living in a high-income country. Compared with MESA and Reasons for Geographic and Racial Differences in Stroke (REGARS) participants, the CGPS participants had slightly higher blood pressure and cholesterol levels (eTable 9 in the Supplement). However, importantly, the PCE calculator has been shown to be fairly well calibrated in both the REGARDS and the CGPS populations, indicating that event rates are comparable in individuals with similar risk factor levels.10,11,32
Further, we were not able to adjust for change in prescription of medication during follow-up (including dropin of statin use), which might have reduced the number of ASCVD events observed during follow-up and potentially differentially between guidelines. However, although generic simvastatin and atorvastatin became available in Denmark in 2002 and 2012, respectively, which might have increased their use, the endorsed 2013 ESC/EAS guidelines significantly restricted the indication for primary prevention with statins by reclassifying Denmark from a high-risk to low-risk country and recommending the use of the low-risk SCORE calculator.
A major strength of our study is that the results originate from a contemporary, population-based large cohort, with no participants lost to follow-up. Also, ASCVD events were appropriately identified, which is essential for the assessment of potential effect on its prevention and NNT.
Conclusions
Sensitivity and specificity for ASCVD events by assigning statin therapy according to the 5 major guidelines differ markedly. Compared with the USPSTF and ESC/EAS guidelines, the CCS, ACC/AHA, and NICE guidelines assign statin therapy to many more of the individuals who later develop ASCVD. Nevertheless, the estimated NNT to prevent 1 ASCVD event is nearly identical between the 5 major guidelines. Taken together, our results therefore suggest that the CCS, ACC/AHA, or NICE guidelines should be preferred in clinical practice for primary prevention because they will prevent more ASCVD events at NNTs that are similar to those achieved by more statin-conservative guidelines with less effect on ASCVD prevention.
eMethods.
eTable 1. Atherosclerotic cardiovascular disease risk enhancers according to the 2018 ACC/AHA cholesterol guidelines
eTable 2. Baseline characteristics of all men from the Copenhagen General Population Study
eTable 3. Baseline characteristics of all women from the Copenhagen General Population Study
eTable 4. Positive and negative predictive values for statin allocation according to 5 guidelines
eTable 5. Event rates per 1000 person-years for atherosclerotic cardiovascular disease in individuals eligible for statin therapy for primary prevention according to 5 guidelines
eTable 6. Calculations of the number needed to treat to prevent one ASCVD event in 10 years among individuals aged 40-75
eTable 7. Calculations of the number needed to treat to prevent one ASCVD event in 10 years among individuals aged 40-65
eTable 8. Calculations of the number needed to treat to prevent one ASCVD event in 10 years among individuals aged 66-75
eTable 9. Baseline characteristics of individuals without known atherosclerotic cardiovascular disease or statin use at baseline from the Copenhagen General Population Study
eFigure 1. Clinical performance of 5 major guidelines on cholesterol treatment for primary prevention of ASCVD stratified by gender in the Copenhagen General Population Study
eFigure 2. Area-proportional Venn diagrams demonstrating overlap in statin eligibility by 5 major guidelines on statin use for primary prevention
eFigure 3. Statin eligibility, ASCVD sensitivity and specificity of five major guidelines for primary prevention of ASCVD stratified by 5-year age groups in men in the Copenhagen General Population Study
eFigure 4. Statin eligibility, ASCVD sensitivity and specificity for primary prevention of ASCVD of five major guidelines stratified by 5-year age groups in women in the Copenhagen General Population Study
eFigure 5. Total number of ASCVD events prevented vs total number of additional diabetes diagnoses per 100.000 Copenhagen General Population participants by following the 5 major statin guidelines
eFigure 6. Clinical performance of two different interpretations of ACC/AHA class I recommendations
eFigure 7. Clinical performance of 5 major guidelines on cholesterol treatment for primary prevention of ASCVD among individuals aged 40 to 75 also including the weaker class IIa (for ESC/EAS), IIb (for ACC/AHA) and C recommendation (for USPSTF) in the Copenhagen General Population Study
eFigure 8. The number needed to treat to prevent one ASCVD event in primary prevention in individuals aged 40-75 also including the weaker class IIa (ESC/EAS), IIb (ACC/AHA) and C recommendation (for USPSTF)
eFigure 9. Clinical performance of 5 major guidelines on cholesterol treatment for primary prevention of ASCVD among individuals aged 40 to 65 in the Copenhagen General Population Study
eFigure 10. The number needed to treat (NNT) to prevent one ASCVD event in primary prevention in individuals aged 40-65
eFigure 11. The number needed to treat (NNT) to prevent one ASCVD event in primary prevention in individuals aged 66-75.
References
- 1.National Clinical Guideline Centre. National Institute for Health and Care Excellence (NICE) clinical guideline CG181: lipid modification, cardiovascular risk assessment and the modification of blood lipids for the primary and secondary prevention of cardiovascular disease. https://www.nice.org.uk/guidance/cg181. Published July 2014. Accessed August 28, 2019. [PubMed]
- 2.Bibbins-Domingo K, Grossman DC, Curry SJ, et al. ; US Preventive Services Task Force . Statin use for the primary prevention of cardiovascular disease in adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2016;316(19):1997-2007. doi: 10.1001/jama.2016.15450 [DOI] [PubMed] [Google Scholar]
- 3.Anderson TJ, Grégoire J, Pearson GJ, et al. . 2016 Canadian Cardiovascular Society guidelines for the management of dyslipidemia for the prevention of cardiovascular disease in the adult. Can J Cardiol. 2016;32(11):1263-1282. doi: 10.1016/j.cjca.2016.07.510 [DOI] [PubMed] [Google Scholar]
- 4.Piepoli MF, Hoes AW, Agewall S, et al. ; ESC Scientific Document Group . 2016 European Guidelines on cardiovascular disease prevention in clinical practice: the Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2016;37(29):2315-2381. doi: 10.1093/eurheartj/ehw106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grundy SM, Stone NJ, Bailey AL, et al. . AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;73(24):3168. doi: 10.1016/j.jacc.2018.11.002 [DOI] [PubMed] [Google Scholar]
- 6.Mortensen MB, Falk E. Primary prevention with statins in the elderly. J Am Coll Cardiol. 2018;71(1):85-94. doi: 10.1016/j.jacc.2017.10.080 [DOI] [PubMed] [Google Scholar]
- 7.Mortensen MB, Nordestgaard BG. Comparison of five major guidelines for statin use in primary prevention in a contemporary general population. Ann Intern Med. 2018;168(2):85-92. doi: 10.7326/M17-0681 [DOI] [PubMed] [Google Scholar]
- 8.Pagidipati NJ, Navar AM, Mulder H, Sniderman AD, Peterson ED, Pencina MJ. Comparison of recommended eligibility for primary prevention statin therapy based on the US Preventive Services Task Force recommendations vs the ACC/AHA guidelines. JAMA. 2017;317(15):1563-1567. doi: 10.1001/jama.2017.3416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nayor M, Vasan RS. Recent update to the US cholesterol treatment guidelines: a comparison with international guidelines. Circulation. 2016;133(18):1795-1806. doi: 10.1161/CIRCULATIONAHA.116.021407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mortensen MB, Nordestgaard BG, Afzal S, Falk E. ACC/AHA guidelines superior to ESC/EAS guidelines for primary prevention with statins in non-diabetic Europeans: the Copenhagen General Population Study. Eur Heart J. 2017;38(8):586-594. doi: 10.1093/eurheartj/ehw426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mortensen MB, Afzal S, Nordestgaard BG, Falk E. Primary prevention with statins: ACC/AHA risk-based approach versus trial-based approaches to guide statin therapy. J Am Coll Cardiol. 2015;66(24):2699-2709. doi: 10.1016/j.jacc.2015.09.089 [DOI] [PubMed] [Google Scholar]
- 12.Mortensen MB, Afzal S, Nordestgaard BG, Falk E. The high-density lipoprotein-adjusted SCORE model worsens SCORE-based risk classification in a contemporary population of 30,824 Europeans: the Copenhagen General Population Study. Eur Heart J. 2015;36(36):2446-2453. doi: 10.1093/eurheartj/ehv251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brøndum-Jacobsen P, Nordestgaard BG, Schnohr P, Benn M. 25-hydroxyvitamin D and symptomatic ischemic stroke: an original study and meta-analysis. Ann Neurol. 2013;73(1):38-47. doi: 10.1002/ana.23738 [DOI] [PubMed] [Google Scholar]
- 14.Mihaylova B, Emberson J, Blackwell L, et al. ; Cholesterol Treatment Trialists’ (CTT) Collaborators . The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012;380(9841):581-590. doi: 10.1016/S0140-6736(12)60367-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Law MR, Wald NJ, Rudnicka AR. Quantifying effect of statins on low density lipoprotein cholesterol, ischaemic heart disease, and stroke: systematic review and meta-analysis. BMJ. 2003;326(7404):1423. doi: 10.1136/bmj.326.7404.1423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ridker PM, MacFadyen JG, Fonseca FAH, et al. ; JUPITER Study Group . Number needed to treat with rosuvastatin to prevent first cardiovascular events and death among men and women with low low-density lipoprotein cholesterol and elevated high-sensitivity C-reactive protein: justification for the use of statins in prevention: an intervention trial evaluating rosuvastatin (JUPITER). Circ Cardiovasc Qual Outcomes. 2009;2(6):616-623. doi: 10.1161/CIRCOUTCOMES.109.848473 [DOI] [PubMed] [Google Scholar]
- 17.Collins R, Reith C, Emberson J, et al. . Interpretation of the evidence for the efficacy and safety of statin therapy. Lancet. 2016;388(10059):2532-2561. doi: 10.1016/S0140-6736(16)31357-5 [DOI] [PubMed] [Google Scholar]
- 18.Shepherd J, Cobbe SM, Ford I, et al. ; West of Scotland Coronary Prevention Study Group . Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. N Engl J Med. 1995;333(20):1301-1307. doi: 10.1056/NEJM199511163332001 [DOI] [PubMed] [Google Scholar]
- 19.Downs JR, Clearfield M, Weis S, et al. . Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/TexCAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study. JAMA. 1998;279(20):1615-1622. doi: 10.1001/jama.279.20.1615 [DOI] [PubMed] [Google Scholar]
- 20.Ridker PM, Danielson E, Fonseca FAH, et al. ; JUPITER Study Group . Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008;359(21):2195-2207. doi: 10.1056/NEJMoa0807646 [DOI] [PubMed] [Google Scholar]
- 21.Yusuf S, Bosch J, Dagenais G, et al. ; HOPE-3 Investigators . Cholesterol lowering in intermediate-risk persons without cardiovascular disease. N Engl J Med. 2016;374(21):2021-2031. doi: 10.1056/NEJMoa1600176 [DOI] [PubMed] [Google Scholar]
- 22.Mortensen MB, Budoff MJ, Li D, et al. . High quality statin trials support the 2013 ACC/AHA cholesterol guidelines after HOPE-3: the multi-ethnic study of atherosclerosis. Circulation. 2017;136(19):1863-1865. doi: 10.1161/CIRCULATIONAHA.117.029381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ridker PM. The JUPITER trial: results, controversies, and implications for prevention. Circ Cardiovasc Qual Outcomes. 2009;2(3):279-285. doi: 10.1161/CIRCOUTCOMES.109.868299 [DOI] [PubMed] [Google Scholar]
- 24.Bowman L, Mafham M, Wallendszus K, et al. ; ASCEND Study Collaborative Group . Effects of aspirin for primary prevention in persons with diabetes mellitus. N Engl J Med. 2018;379(16):1529-1539. doi: 10.1056/NEJMoa1804988 [DOI] [PubMed] [Google Scholar]
- 25.McNeil JJ, Wolfe R, Woods RL, et al. ; ASPREE Investigator Group . Effect of aspirin on cardiovascular events and bleeding in the healthy elderly. N Engl J Med. 2018;379(16):1509-1518. doi: 10.1056/NEJMoa1805819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McNeil JJ, Nelson MR, Woods RL, et al. ; ASPREE Investigator Group . Effect of aspirin on all-cause mortality in the healthy elderly. N Engl J Med. 2018;379(16):1519-1528. doi: 10.1056/NEJMoa1803955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Viera AJ, Hawes EM. Management of mild hypertension in adults. BMJ. 2016;355:i5719. doi: 10.1136/bmj.i5719 [DOI] [PubMed] [Google Scholar]
- 28.Lonn EM, Bosch J, López-Jaramillo P, et al. ; HOPE-3 Investigators . Blood-pressure lowering in intermediate-risk persons without cardiovascular disease. N Engl J Med. 2016;374(21):2009-2020. doi: 10.1056/NEJMoa1600175 [DOI] [PubMed] [Google Scholar]
- 29.Yusuf S, Lonn E, Pais P, et al. ; HOPE-3 Investigators . Blood-pressure and cholesterol lowering in persons without cardiovascular disease. N Engl J Med. 2016;374(21):2032-2043. doi: 10.1056/NEJMoa1600177 [DOI] [PubMed] [Google Scholar]
- 30.Pearce KA, Furberg CD, Psaty BM, Kirk J. Cost-minimization and the number needed to treat in uncomplicated hypertension. Am J Hypertens. 1998;11(5):618-629. doi: 10.1016/S0895-7061(97)00488-3 [DOI] [PubMed] [Google Scholar]
- 31.Bress AP, Colantonio LD, Cooper R, et al. . Potential cardiovascular disease events prevented with adoption of the 2017 American College of Cardiology/American Heart Association blood pressure guideline. Circulation. 2019;139(1):24-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Muntner P, Colantonio LD, Cushman M, et al. . Validation of the atherosclerotic cardiovascular disease pooled cohort risk equations. JAMA. 2014;311(14):1406-1415. doi: 10.1001/jama.2014.2630 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods.
eTable 1. Atherosclerotic cardiovascular disease risk enhancers according to the 2018 ACC/AHA cholesterol guidelines
eTable 2. Baseline characteristics of all men from the Copenhagen General Population Study
eTable 3. Baseline characteristics of all women from the Copenhagen General Population Study
eTable 4. Positive and negative predictive values for statin allocation according to 5 guidelines
eTable 5. Event rates per 1000 person-years for atherosclerotic cardiovascular disease in individuals eligible for statin therapy for primary prevention according to 5 guidelines
eTable 6. Calculations of the number needed to treat to prevent one ASCVD event in 10 years among individuals aged 40-75
eTable 7. Calculations of the number needed to treat to prevent one ASCVD event in 10 years among individuals aged 40-65
eTable 8. Calculations of the number needed to treat to prevent one ASCVD event in 10 years among individuals aged 66-75
eTable 9. Baseline characteristics of individuals without known atherosclerotic cardiovascular disease or statin use at baseline from the Copenhagen General Population Study
eFigure 1. Clinical performance of 5 major guidelines on cholesterol treatment for primary prevention of ASCVD stratified by gender in the Copenhagen General Population Study
eFigure 2. Area-proportional Venn diagrams demonstrating overlap in statin eligibility by 5 major guidelines on statin use for primary prevention
eFigure 3. Statin eligibility, ASCVD sensitivity and specificity of five major guidelines for primary prevention of ASCVD stratified by 5-year age groups in men in the Copenhagen General Population Study
eFigure 4. Statin eligibility, ASCVD sensitivity and specificity for primary prevention of ASCVD of five major guidelines stratified by 5-year age groups in women in the Copenhagen General Population Study
eFigure 5. Total number of ASCVD events prevented vs total number of additional diabetes diagnoses per 100.000 Copenhagen General Population participants by following the 5 major statin guidelines
eFigure 6. Clinical performance of two different interpretations of ACC/AHA class I recommendations
eFigure 7. Clinical performance of 5 major guidelines on cholesterol treatment for primary prevention of ASCVD among individuals aged 40 to 75 also including the weaker class IIa (for ESC/EAS), IIb (for ACC/AHA) and C recommendation (for USPSTF) in the Copenhagen General Population Study
eFigure 8. The number needed to treat to prevent one ASCVD event in primary prevention in individuals aged 40-75 also including the weaker class IIa (ESC/EAS), IIb (ACC/AHA) and C recommendation (for USPSTF)
eFigure 9. Clinical performance of 5 major guidelines on cholesterol treatment for primary prevention of ASCVD among individuals aged 40 to 65 in the Copenhagen General Population Study
eFigure 10. The number needed to treat (NNT) to prevent one ASCVD event in primary prevention in individuals aged 40-65
eFigure 11. The number needed to treat (NNT) to prevent one ASCVD event in primary prevention in individuals aged 66-75.