This cohort study evaluates whether stroke incidence declined among older adults from 1987 to 2011 vs 2011 to 2017 in the Atherosclerosis Risk in Communities study.
Key Points
Question
Have stroke incidence rates among adults aged 65 years and older continued to decline in recent years?
Findings
In this study of the Atherosclerosis Risk in Communities cohort study data including 1340 incident strokes occurring from 1987 to 2017, adjusted stroke incidence rates decreased by 32% per 10 years in participants 65 years and older. Findings were consistent in men and women as well as in white and black individuals.
Meaning
Validated stroke incidence rates in adults 65 years and older decreased over the last 30 years in the Atherosclerosis Risk in Communities cohort; the decrease in rates previously reported for 1987 to 2011 has extended to 2017.
Abstract
Importance
Determining whether the previously reported decreased stroke incidence rates from 1987 to 2011 among US adults 65 years and older in the Atherosclerosis Risk in Communities (ARIC) study continued to decrease subsequently can help guide policy and planning efforts.
Objective
To evaluate whether stroke incidence declines among older adults in the ARIC study continued after 2011.
Design, Setting, and Participants
ARIC is a community-based prospective cohort study including 15 792 individuals aged 45 to 64 years at baseline (1987-1989), selected by probability sampling from residents of Forsyth County, North Carolina; Jackson, Mississippi (black individuals only); the northwestern suburbs of Minneapolis, Minneapolis; and Washington County, Maryland (ie, center). The present study included ARIC participants free of stroke at baseline, followed up through December 31, 2017. Data were collected through personal interviews and physical examinations during study visits, annual/semiannual telephone interviews, and active surveillance of discharges from local hospitals. Stroke events were adjudicated by study-physicians reviewers. Analysis began September 2018.
Main Outcomes and Measures
The main outcome was stroke incidence rates, which were computed with 95% CIs stratifying the analysis by age and calendar time. Trends in adjusted incidence rates were assessed using Poisson regression incidence rate ratios. Models included calendar time, age, sex, race/center, and time-varying risk factors (hypertension, diabetes, coronary heart disease, cholesterol-lowering medication use, and smoking).
Results
Of 14 357 ARIC participants with 326 654 person-years of follow-up, the mean (SD) age at baseline was 54.1 (5.8) years and 7955 (55.4%) were women. From 1987 to 2017, a total of 1340 incident strokes occurred among ARIC participants, and among them, 1028 (76.7%) occurred in participants 65 years and older. Crude incidence rates of stroke for participants 65 years and older decreased progressively from 1987 to 2017. Incidence rates, adjusted for age, sex, race/center, and time-varying risk factors, decreased by 32% (95% CI, 23%-40%) per 10 years in participants 65 years and older. Findings were consistent across decades, sex, and race.
Conclusions and Relevance
Validated total stroke incidence rates in adults 65 years and older decreased over the last 30 years in the ARIC cohort. The decrease in rates previously reported for 1987 to 2011 extends for the subsequent 6 years in men and women as well as in white and black individuals.
Introduction
Global data show that stroke incidence rates in high-income countries decreased from 1990 to 2010 by 13% (95% CI, 6%-18%) for ischemic stroke and by 19% (95% CI, 5%-30%) for hemorrhagic stroke.1 In the United States, declines in stroke incidence have been reported in participants of the Framingham Heart Study up to 2004,2 the Greater Cincinnati/Northern Kentucky Stroke Study3,4 up to 2010, and the BASIC Project5 also up to 2010; however, these studies did not include data from 2010 to the present. Using validated stroke data in the Atherosclerosis Risk in Communities (ARIC) cohort study, we have shown decreasing stroke incidence rates from 1987 to 2011 among people 65 years and older, while no significant changes were evident in younger ARIC participants.6 In the present study, we evaluated whether the decline in stroke incidence rates in older adults continued in the subsequent 6 years, from 2011 to 2017.
Methods
Study Population
The ARIC cohort study has been previously described.7 Briefly, at baseline (1987-1989), ARIC included 15 792 individuals aged 45 to 64 years, selected by probability sampling from residents of 4 communities in the United States (Forsyth County, North Carolina; Jackson, Mississippi [black individuals only]; the northwestern suburbs of Minneapolis, Minneapolis; and Washington County, Maryland). All ARIC participants provided written informed consent, and the study was approved by institutional review boards of all collaborating centers. At ARIC visits (baseline and follow-up in 1990-1992, 1993-1995, 1996-1998, 2011-2013, and 2016-2017), data were collected through personal interviews and physical examinations. In addition, annual/semiannual telephone interviews and active surveillance of discharges from local hospitals were conducted. For the present study, we included black and white individuals with no prevalent stroke at baseline and with complete data on covariates.
Ascertainment of Stroke Events
All stroke hospitalizations and deaths from January 1, 1987, to December, 31, 2017, were identified. Methods for ascertainment of stroke events were detailed elsewhere.7,8 Hospital records for possible stroke-related hospitalizations were obtained (International Classification of Diseases, Ninth Revision [ICD-9] codes: 430-438 until 1997; ICD-9 codes 430-436 and ICD-10 codes G45.X, I60.X, I61.X, I62.X, I63.X, I65.X, I66.X, and I67.X afterward) and information on fatal stroke was collected through linkage with the National Death Index. Strokes were identified by a computer algorithm and adjudicated by physician reviewers.6,8The present study includes 1340 incident strokes occurring from baseline to December 31, 2017, defined as a first definite or probable stroke in a participant with no self-report of physician-diagnosed stroke at baseline.
Statistical Analysis
We studied the characteristics of participants at baseline (ARIC visit 1, 1987-1989) for all 14 357 participants included in the present study and at 2 follow-up visits (visit 4, 1996-1998 and visit 5, 2011-2013) for participants 65 years and older, as the study focuses on this age group. Incidence rates and 95% confidence intervals of definite or probable stroke per 1000 person-years (PY) were calculated and modeled with Poisson regression, stratifying age by 5-year groups and calendar time by 3-year groups (4-year for the most recent period, 2014-2017). Temporal trends were estimated using Poisson regression incidence rate ratios.
Crude incidence rates per 1000 PY and adjusted incidence rate ratios per 10-year calendar time and age are presented. Incidence rate ratios were adjusted for age and calendar time (model 1) and additionally adjusted for sex, race/center, and time-varying risk factors (hypertension, diabetes, coronary heart disease, cholesterol-lowering medications use, and smoking) (model 2). Interactions between calendar time and race, sex, and age group were assessed. Analysis by race, sex, and age group was also performed. Stata version 14 (Stata Corp) was used for data analysis. All tests were 2 sided, and P less than .05 was considered statistically significant. Analysis began in September 2018.
Results
At baseline, 7955 of 14 357 participants (55.4%) were women, and the mean (SD) age of all participants was 54.1 (5.8) years. Participants were followed up for 326 654 PY. Among ARIC participants aged 65 to 74 years, the distribution of risk factors changed from 1996-1998 (visit 4) to 2011-2013 (visit 5) (Table 1). Adjusted for age, sex, and race/center, the prevalence of diabetes and hypertension increased, while the use of antihypertensive and cholesterol-lowering medications increased, and blood pressure, lipids levels, and current smoking decreased.
Table 1. Characteristics of ARIC Participants at Baseline and Aged 65-74 Years at Visits 4 and 5.
| Characteristic | No. (%)a | ||
|---|---|---|---|
| Overall | Age 65-74 yb | ||
| 1987-1989 (Visit 1) | 1996-1998 (Visit 4) | 2011-2013 (Visit 5) | |
| Total No. | 14 357 | 4218 | 2843 |
| Age, mean (SD), y | 54.1 (5.8) | 68.8 (2.6) | 71.1 (1.9) |
| Female | 7955 (55.4) | 2204 (52.3) | 1716 (60.4) |
| Race/center | |||
| White/Minneapolis, MN | 3844 (26.8) | 1190 (28.2) | 848 (29.8) |
| White/Washington County, MD | 3382 (23.6) | 1172 (27.8) | 651 (22.9) |
| Forsyth County, NC | |||
| White | 3331 (23.2) | 1079 (25.6) | 596 (21.0) |
| Black | 442 (3.1) | 105 (2.5) | 54 (1.9) |
| Black/Jackson, MS | 3358 (23.4) | 672 (15.9) | 694 (24.4) |
| Smoking statusc | |||
| Current | 3711 (25.9) | 485 (11.6) | 210 (7.7) |
| Former | 4651 (32.4) | 1946 (46.6) | 1316 (48.0) |
| Never | 5995 (41.8) | 1747 (41.8) | 1214 (44.3) |
| Hypertensionc | 4886 (34.0) | 2327 (55.5) | 2000 (70.9) |
| Blood pressure, median (range), mm Hgc | |||
| Systolic | 119 (108-131) | 130 (118-144) | 127 (117-139) |
| Diastolic | 73 (66-80) | 69 (62-76) | 68 (61-75) |
| Hypertension medicationc | 4241 (29.5) | 2129 (50.5) | 2.030 (71.6) |
| Diabetesc | 1662 (11.6) | 782 (18.7) | 1066 (38.1) |
| Coronary heart disease | 649 (4.5) | 476 (11.3) | 322 (11.3) |
| Total cholesterol, median (range), mg/dLc | 212 (186-239) | 198 (176-222) | 182 (156-211) |
| Cholesterol-lowering medicationc | 404 (2.8) | 742 (17.7) | 1526 (54.0) |
Abbreviation: ARIC, Atherosclerosis Risk in Communities.
SI conversion factor: To convert cholesterol to mmol/L, multiply by 0.0259.
Missing data rate was <2.5% for all variables.
Rates among participants aged 65 to 74 years in 1996-1998 (visit 4) and 2011-2013 (visit 5) were adjusted for age, sex, and race/center.
P < .001 for the comparison between participants aged 65 to 74 years in 1996-1998 (visit 4) and in 2011-2013 (visit 5).
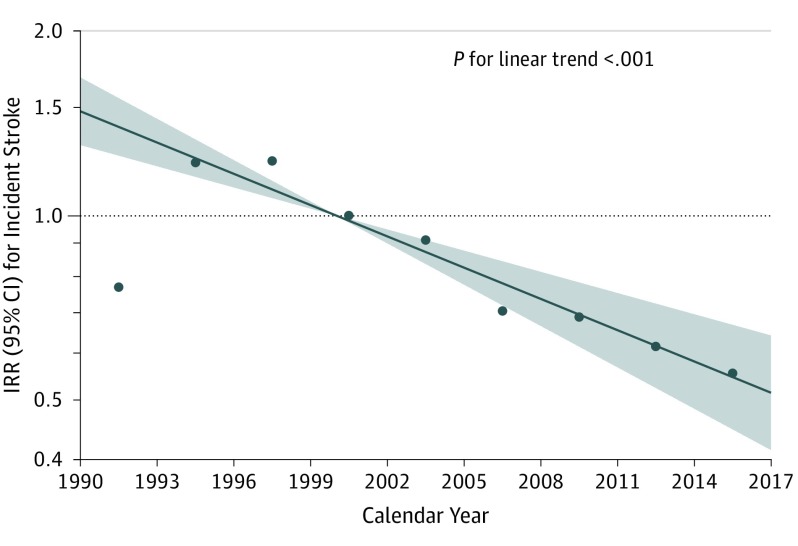
Overall, 1028 incident strokes occurred among individuals 65 years and older during 184 343 PY in this age group. Crude incidence rates of stroke for individuals 65 years and older decreased from 1987 to 2017, while no significant changes in rates were observed among those younger than 65 years (eTable in the Supplement). Incidence rates adjusted for age, sex, race/center, time-varying hypertension, diabetes, coronary heart disease, smoking, and use of cholesterol-lowering medications decreased by 28% per 10 years (95% CI, 20%-36%) overall. Decreases were similar in men and women as well as in white and black individuals (Table 2), and there was no significant interaction by these demographics or follow-up decade, although power is limited. Analysis by age group showed a 32% (95% CI, 23%-40%) decrease in adjusted rates among individuals 65 years and older from 1987 to 2017 (Table 2). A significant decreasing linear trend with continuous calendar time over the last 30 years was observed in stroke incidence rates for older adults in ARIC (Figure).
Table 2. Total Stroke Incidence Rates and Incidence Rate Ratios per 10-Year Calendar Time and Age, Overall and Stratified by Race, Sex, and Age Group, 1987-2017.
| Variable | Overall | Race | Sex | Age Group | |||
|---|---|---|---|---|---|---|---|
| White | Black | Men | Women | <65 y | ≥65 y | ||
| No. of events/No. of person-years | 1340/326 654 | 834/245 931 | 506/80 823 | 635/138 336 | 705/188 318 | 312/142 312 | 1028/184 343 |
| Total crude IRs (95% CI) per 1000 person-years | 4.10 (3.89-4.33) | 3.39 (3.17-3.63) | 6.26 (5.74-6.83) | 4.59 (4.25-4.96) | 3.74 (3.48-4.03) | 2.19 (1.96-2.45) | 5.58 (5.25-5.93) |
| Model 1: Calendar Year and Age, IRR (95% CI) | |||||||
| Calendar time per 10 y | 0.77 (0.69-0.85) | 0.75 (0.65-0.86) | 0.73 (0.61-0.87) | 0.75 (0.64-0.87) | 0.80 (0.69-0.93) | 0.98 (0.76-1.26) | 0.73 (0.64-0.82)a |
| Age per 10 y | 2.10 (1.91-2.31) | 2.51 (2.21-2.84) | 1.81 (1.56-2.10)a | 2.02 (1.76-2.32) | 2.14 (1.88-2.44) | 1.98 (1.48-2.64) | 2.05 (1.80-2.33) |
| Model 2: Calendar Year, Age, Sex, Time-Varying Risk Factors, and Race/Center, IRR (95% CI) | |||||||
| Calendar time per 10 y | 0.72 (0.64-0.80) | 0.71 (0.62-0.82) | 0.74 (0.62-0.88) | 0.70 (0.60-0.82) | 0.74 (0.63-0.86) | 0.94 (0.73-1.21) | 0.68 (0.60-0.77)a |
| Age per 10 y | 2.03 (1.84-2.24) | 2.36 (2.08-2.68) | 1.61 (1.38-1.88)a | 1.98 (1.72-2.28) | 2.07 (1.81-2.37) | 1.63 (1.21-2.18) | 2.04 (1.79-2.33) |
| Sex | |||||||
| Women | 1 [Reference] | 1 [Reference] | 1 [Reference] | NA | NA | 1 [Reference] | 1 [Reference] |
| Men | 1.18 (1.05-1.32) | 1.20 (1.04-1.39) | 1.18 (0.98-1.43) | NA | NA | 1.29 (1.02-1.64) | 1.14 (1.00-1.30) |
| Time-varying risk factorsb | |||||||
| Hypertension | 1.80 (1.58-2.05) | 1.59 (1.36-1.85) | 2.38 (1.85-3.07)a | 1.89 (1.57-2.27) | 1.72 (1.43-2.07) | 2.36 (1.83-3.05) | 1.59 (1.37-1.85)a |
| Diabetes | 1.62 (1.44-1.83) | 1.44 (1.23-1.68) | 1.96 (1.63-2.35)a | 1.46 (1.22-1.73) | 1.77 (1.51-2.08) | 2.77 (2.18-3.52) | 1.40 (1.22-1.60)a |
| Coronary heart disease | 1.69 (1.48-1.94) | 1.61 (1.36-1.91) | 1.84 (1.46-2.33) | 1.49 (1.24-1.78) | 2.07 (1.69-2.53)a | 2.72 (2.03-3.65) | 1.53 (1.31-1.78)a |
| Smoking status | |||||||
| Never smoker | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Former smoker | 1.05 (0.93-1.19) | 1.02 (0.88-1.20) | 1.14 (0.92-1.40) | 0.97 (0.81-1.17) | 1.12 (0.95-1.34) | 1.20 (0.90-1.60) | 1.01 (0.88-1.17) |
| Current smoker | 1.81 (1.56-2.10) | 1.90 (1.56-2.32) | 1.69 (1.34-2.12) | 1.70 (1.35-2.13) | 1.86 (1.52-2.28) | 2.07 (1.57-2.73) | 1.73 (1.44-2.07) |
| Cholesterol-lowering medication | 1.00 (0.87-1.15) | 1.06 (0.90-1.25) | 0.89 (0.68-1.16) | 0.95 (0.77-1.16) | 1.05 (0.87-1.26) | 0.83 (0.56-1.25) | 1.05 (0.90-1.22) |
Abbreviations: IR, incidence rate; IRRs, incidence rate ratio; NA, not applicable.
P < .05 for interaction in a model containing both groups and interaction terms for all variables.
Prevalence at baseline as reference.
Figure. Adjusted Stroke Incidence Rate Ratios vs Calendar Time in Atherosclerosis Risk in Communities Participants 65 Years and Older.
Dots represent adjusted incidence rate ratio point estimates from a model run using a categorical calendar time variable, plotted at midpoint of each 3-year calendar time category (4 years for the last period 2014-2017), with 1999-2001 as the reference category. The solid line represents the linear trend in adjusted incidence rate ratios (IRRs), and the shaded area represents the 95% CI with 2000 as the reference point. Rates were adjusted for age, sex, race/center, and time-varying risk factors (hypertension, diabetes, coronary heart disease, cholesterol-lowering medications use, and smoking status).
Discussion
We found that the decrease in stroke incidence rates previously observed in the ARIC cohort participants6 continued into the recent years. The decrease in rates over the last 30 years was observed in men and women as well as in black and white individuals 65 years and older. After 2011, all ARIC participants were 65 years and older; therefore, the present update does not show new data for the younger group.
Limited data are available on stroke incidence rates for the most recent years. Declines in stroke incidence in older adults during recent years have been reported in 3 recent studies. A Canadian study9 reported declining incidence of stroke from 2002-2003 to 2013-2014 among individuals 80 years and older. Similar to our findings, rates of first-ever stroke in Sweden decreased by 33% from 2001-2002 to 2015-2016 in older adults, while no change was found in those younger than 65 years.10 In the United Kingdom, age-adjusted incidence of ischemic stroke decreased by 43% from 2000-2003 to 2012-2015. Yet, different from ours and other studies findings, the decreasing trends in the United Kingdom were observed both in younger (age <55 years) and older (age ≥55 years) groups.11 We are now reporting updated rates and trends in stroke incidence in the United States using data on validated stroke events in the ARIC cohort study. Availability of detailed information collected in the ARIC biracial cohort during the last 3 decades, including time-varying data on important risk factors for stroke, and complete adjudication of all stroke events in ARIC, are the main strengths in our study. Although smoking, systolic blood pressure, and cholesterol levels have decreased over time in ARIC participants, measured risk factors did not explain the decline in stroke incidence.
Limitations
A limitation of the present study is the small number of hemorrhagic strokes, which does not allow for analysis by stroke type. In addition, the ARIC population includes only white and black individuals and the cohort ages with time; therefore, no new information for individuals younger than 65 years is available on this age group for the most recent years. The decline observed in rates of incident stroke among individuals 65 years and older is reassuring; nevertheless, as result of the aging of the population, stroke continues to pose an important global burden.
Conclusions
Validated total stroke incidence rates among individuals 65 years and older decreased over the last 30 years in the ARIC cohort. The decrease in rates previously reported for 1987-2011 extends for the subsequent 6 years (2011-2017) in men and women as well as in white and black individuals.
eTable. Crude total stroke incidence rates (per 1,000 person-years) stratified by 5-year age group and 3-year calendar period of follow-up
References
- 1.Krishnamurthi RV, Feigin VL, Forouzanfar MH, et al. ; Global Burden of Diseases, Injuries, Risk Factors Study 2010 (GBD 2010); GBD Stroke Experts Group . Global and regional burden of first-ever ischaemic and haemorrhagic stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet Glob Health. 2013;1(5):e259-e281. doi: 10.1016/S2214-109X(13)70089-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carandang R, Seshadri S, Beiser A, et al. Trends in incidence, lifetime risk, severity, and 30-day mortality of stroke over the past 50 years. JAMA. 2006;296(24):2939-2946. doi: 10.1001/jama.296.24.2939 [DOI] [PubMed] [Google Scholar]
- 3.Kleindorfer DO, Khoury J, Moomaw CJ, et al. Stroke incidence is decreasing in whites but not in blacks: a population-based estimate of temporal trends in stroke incidence from the Greater Cincinnati/Northern Kentucky Stroke Study. Stroke. 2010;41(7):1326-1331. doi: 10.1161/STROKEAHA.109.575043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Madsen TE, Khoury J, Alwell K, et al. Sex-specific stroke incidence over time in the Greater Cincinnati/Northern Kentucky Stroke Study. Neurology. 2017;89(10):990-996. doi: 10.1212/WNL.0000000000004325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morgenstern LB, Smith MA, Sánchez BN, et al. Persistent ischemic stroke disparities despite declining incidence in Mexican Americans. Ann Neurol. 2013;74(6):778-785. doi: 10.1002/ana.23972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Koton S, Schneider AL, Rosamond WD, et al. Stroke incidence and mortality trends in US communities, 1987 to 2011. JAMA. 2014;312(3):259-268. doi: 10.1001/jama.2014.7692 [DOI] [PubMed] [Google Scholar]
- 7.The ARIC investigators The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. Am J Epidemiol. 1989;129(4):687-702. doi: 10.1093/oxfordjournals.aje.a115184 [DOI] [PubMed] [Google Scholar]
- 8.Rosamond WD, Folsom AR, Chambless LE, et al. Stroke incidence and survival among middle-aged adults: 9-year follow-up of the Atherosclerosis Risk in Communities (ARIC) cohort. Stroke. 1999;30(4):736-743. doi: 10.1161/01.STR.30.4.736 [DOI] [PubMed] [Google Scholar]
- 9.Cerasuolo JO, Azarpazhooh MR, Kapral MK, Cipriano LE, Hachinski V. Evidence of concomitantly increasing stroke and dementia prevalence among those 80 years and older in Ontario, Canada, 2003-04 to 2012-13. Can J Neurol Sci. 2019;46(1):105-107. doi: 10.1017/cjn.2018.347 [DOI] [PubMed] [Google Scholar]
- 10.Aked J, Delavaran H, Norrving B, Lindgren A. Temporal Trends of Stroke Epidemiology in Southern Sweden: a population-based study on stroke incidence and early case-fatality. Neuroepidemiology. 2018;50(3-4):174-182. doi: 10.1159/000487948 [DOI] [PubMed] [Google Scholar]
- 11.Wafa HA, Wolfe CDA, Rudd A, Wang Y. Long-term trends in incidence and risk factors for ischaemic stroke subtypes: prospective population study of the South London Stroke Register. PLoS Med. 2018;15(10):e1002669. doi: 10.1371/journal.pmed.1002669 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Crude total stroke incidence rates (per 1,000 person-years) stratified by 5-year age group and 3-year calendar period of follow-up