Abstract
This study examines trends in aggregate use and expenditures for diabetes mellitus therapies among US Medicare Part D beneficiaries.
There are now 12 classes of antihyperglycemic medications available for patients with type 2 diabetes mellitus (DM). With an estimated 30 million patients in the United States living with DM1 and increasing complexity and financial burden of DM care, the relative distribution of expenditures across DM therapeutic classes needs to be reexamined. We evaluated trends in aggregate use and expenditures for all DM therapies among US Medicare Part D beneficiaries from 2012 to 2017.
Methods
We analyzed 2012 to 2017 Medicare Part D Prescription Drug Event data. All classes of antihyperglycemic therapies, defined by the American Diabetes Association, were identified.2 Bromocriptine and colesevelam were excluded given overlapping indications and infrequent use. Total spending (both Medicare Part D and beneficiary payments) were adjusted for inflation and presented in 2017 US dollars. Annual spending, number of claims, and spending per claim were extracted. Descriptive computations were performed using STATA statistical software (version 14.1, StataCorp). Because these deidentified data were publicly available and did not contain detailed patient characteristics, institutional review board approval was waived by the institutional review board of Partners HealthCare.
Results
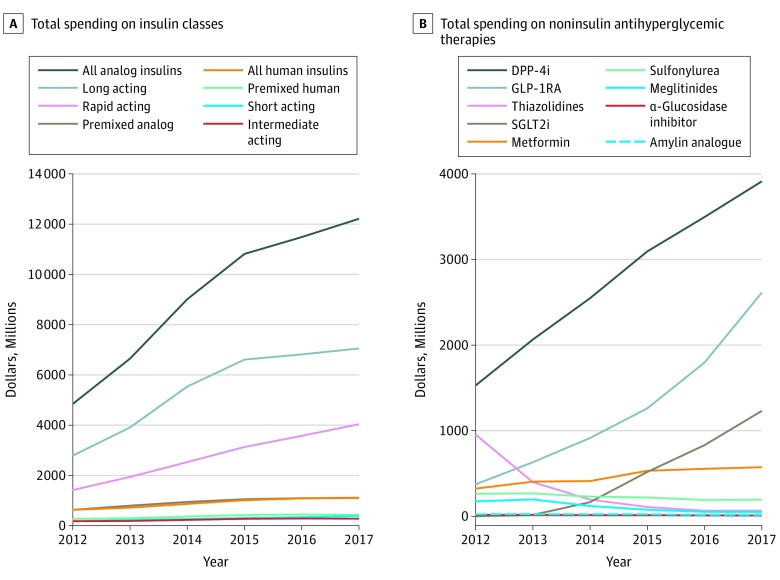
In 2017, Medicare Part D spent $22 billion on all DM therapies (144% increase from 2012). Medicare spent $94 billion on DM therapies from 2012 to 2017, including $60 billion on insulin ($55 billion on analog, $5 billion on human) (Figure 1A). Medicare filled 36% more analog insulins prescriptions but 17% fewer human insulin prescriptions over this timeframe (Figure 2A). Since 2015, spending increases for analog insulin have slowed, driven by plateauing in per-claim spending for long-acting insulins (Figure 1B).
Figure 1. US Medicare Part D Total Spending Trends.
A, Total spending on insulin classes. B, Total spending on noninsulin antihyperglycemic therapies. DPP-4i indicates dipeptidyl peptidase-4 inhibitors; GLP-1RA, glucagon-like peptide-1 receptor agonists; SGLT2i, sodium-glucose cotransporter-2 inhibitors.
Figure 2. US Medicare Part D Trends in Claims and Per-Claim Spending on Antihyperglycemic Therapies Between 2012 and 2017.
A, Claims. B, Per-claim spending. DPP-4i indicates dipeptidyl peptidase-4 inhibitors; GLP-1RA, glucagon-like peptide-1 receptor agonists; SGLT2i, sodium-glucose cotransporter-2 inhibitors.
Noninsulin therapies accounted for $3.7 billion in 2012 and $8.7 billion in 2017 (135% increase) (Figure 1B). The costliest noninsulin therapies were dipeptidyl peptidase-4 inhibitors (DPP-4i), which increased from $1.5 billion to $3.9 billion (156% increase). The next 2 costliest noninsulin therapies were the glucagon-like peptide-1 receptor agonists (GLP-1RA) and the sodium-glucose cotransporter-2 inhibitors (SGLT2i). Total spending on GLP-1RA increased from $374 million on 753 855 prescriptions in 2012 to $2.6 billion on 2.7 million prescriptions in 2017. In 2014, Medicare Part D spent $165 million on 381 093 SGLT2i prescriptions, which increased to $1.2 billion on 2 million SGLT2i prescriptions in 2017.
Between 2012 and 2017, the most commonly prescribed antihyperglycemic therapy was metformin (163 million prescriptions at $17/prescription). Similarly, Medicare spent $14 per prescription on 95 million prescriptions on sulfonylureas. Amylin analogues were the least commonly prescribed antihyperglycemic therapy, but had the highest per-claim cost. Driven by decreasing per-claim cost, overall spending for thiazolidinediones decreased by 93% (from $956 million to $65 million). Spending (not included in the above estimates) from 2012 to 2017 on combination products was $5 billion on 15.6 million claims.
Discussion
Spending for DM-related therapies is rising rapidly among Medicare beneficiaries in the US. Although insulins, primarily analog insulins, remain the primary drivers of cost,3 overall insulin expenditure growth appears to be slowing. In contrast, spending on newer antihyperglycemic therapies is increasing, driven by not only greater uptake, but also longitudinal increases in per-claim costs of DPP-4i, GLP-1RA, and SGLT2i. The DPP-4i class remains the most costly noninsulin therapy despite lack of established cardiovascular benefits and only modest glycemic efficacy.
Increased aggregate spending has not been accompanied by apparent improvements in population-level glycemic control.4 However, it is uncertain whether greater use of SGLT2i and GLP-1RA, classes with proven cardiovascular benefits, may still advance value by averting downstream complications and health care expenditures.
Our data do not account for patient-level characteristics (including cardiovascular risk) and thus do not inform appropriateness of spending changes. We also could not differentiate expenditures related to types of DM, distinguish new vs existing prescriptions, or account for manufacturer rebates or discounts.
Conclusions
As DM prevalence in the United States is projected to remain high, costs of DM therapeutics may pose barriers to affordability and adherence. Further work is needed to capture health system costs of DM care to potentially redistribute current expenditures to high-value care practices.
References
- 1.Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2017: Estimates of Diabetes and Its Burden in the United States. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf. Accessed August 28, 2019.
- 2.American Diabetes Association 9. Pharmacologic approaches to glycemic treatment: Standards of Medical Care in Diabetes-2019. Diabetes Care. 2019;42(suppl 1):S90-S102. doi: 10.2337/dc19-S009 [DOI] [PubMed] [Google Scholar]
- 3.Hernandez I, Good CB, Shrank WH, Gellad WF. Trends in Medicaid prices, market share, and spending on long-acting insulins, 2006-2018. JAMA. 2019;321(16):1627-1629. doi: 10.1001/jama.2019.2990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dennis JM, Henley WE, McGovern AP, et al. ; MASTERMIND consortium . Time trends in prescribing of type 2 diabetes drugs, glycaemic response and risk factors: a retrospective analysis of primary care data, 2010-2017. Diabetes Obes Metab. 2019;21(7):1576-1584. [DOI] [PMC free article] [PubMed] [Google Scholar]