Key Points
Question
Do the outcomes of bioresorbable scaffolds in patients with coronary artery disease vary during the course of their bioresorption?
Findings
In this individual patient data pooled analysis and summary-level meta-analysis of 4 randomized clinical trials of a polymeric bioresorbable scaffold and a contemporary metallic drug-eluting stent in 3884 patients, scaffold-related adverse events increased within 3 years of implantation but not thereafter.
Meaning
If new scaffolds are shown to have improved early results, bioresorbable scaffolds may be an acceptable alternative for many patients with coronary artery disease.
Abstract
Importance
Bioresorbable scaffolds were designed to provide clinical benefits after their complete bioresorption. Prior studies demonstrated early risks with the Absorb polymeric bioresorbable vascular scaffold (BVS). Whether this risk profile changes over time during the course of its bioresorption is unknown.
Objective
To examine outcomes of the first-generation BVS before and after 3 years, the point of its complete bioresorption in animals.
Data Sources
We searched MEDLINE and the Cochrane database, conference proceedings, and public websites for relevant studies.
Study Selection
Eligible studies were randomized clinical trials of BVS vs metallic drug-eluting stents in patients with coronary artery disease with at least 5-year follow-up. Four trials of BVS vs everolimus-eluting stents (EES) with 3384 patients met criteria.
Data Extraction and Synthesis
Individual patient data from the 4 trials were pooled, and summary-level meta-analysis was performed.
Main Outcomes and Measures
The major effectiveness and safety measures were target lesion failure (TLF; cardiac death, target vessel–related myocardial infarction, or ischemia-driven target lesion revascularization) and device thrombosis. Outcomes were examined through 5-year follow-up and between 0 to 3 and 3 to 5 years.
Results
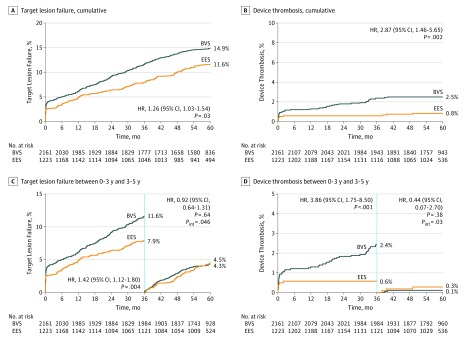
Mean age for the 3384 patients was 62.8 years; 2452 patients were men (72.5%), and diabetes was present in 1020 patients (30.2%). Through 5-year follow-up, treatment with BVS compared with EES was associated with higher rates of TLF (14.9% vs 11.6%; HR, 1.26; 95% CI, 1.03-1.54; P = .03) and device thrombosis (2.5% vs 0.8%; HR, 2.87; 95% CI, 1.46-5.65; P = .002). Target lesion failure occurred in 11.6% of BVS-treated patients vs 7.9% of EES-treated patients between 0 to 3 years (HR, 1.42; 95% CI, 1.12-1.80), and 4.3% of BVS-treated patients vs 4.5% of EES-treated patients between 3 to 5 years (HR, 0.92; 95% CI, 0.64-1.31) (P for interaction = .046). Device thrombosis occurred in 2.4% of BVS-treated patients vs 0.6% of EES-treated patients between 0 to 3 years (HR, 3.86; 95% CI, 1.75-8.50) and 0.1% of BVS-treated patients vs 0.3% of EES-treated patients between 3 to 5 years (HR, 0.44; 95% CI, 0.07-2.70) (P for interaction = .03). These results were consistent by spline analysis and after multiple imputation and multivariable analysis.
Conclusions and Relevance
The period of excess risk for the first-generation Absorb BVS ends at 3 years. These data provide mechanistic insights into the timing of adverse events after BVS and identify the hurdles to be overcome for bioresorbable technology to be accepted as a valid alternative for patients with coronary artery disease.
Trial Registration
ClinicalTrials.gov identifiers: NCT01751906, NCT01844284, NCT01923740, and NCT01425281
This individual patient data pooled analysis and meta-analysis examines the outcomes of first-generation bioresorbable vascular scaffolds in patients with coronary artery disease before and after 3 years.
Introduction
Although event-free survival for patients with coronary artery disease treated with metallic stents has improved with enhancements in technology and implantation technique, long-term studies have demonstrated an ongoing risk of restenosis or thrombosis arising from the implant site, which persists for at least 20 years, whether the stent was bare metal or drug eluting and regardless of the type of polymer or antiproliferative agent.1,2,3 These adverse events, which occur after the first year at a rate of approximately 2% to 3% per year, may be attributed to strut fractures, loss of vessel compliance, vasomotion, and the capability for vascular adaptive remodeling, coverage of side branches, and the development of late neoatherosclerosis.4,5,6,7 A permanent implant may also impede noninvasive imaging (eg, computed tomographic angiography owing to blooming artifacts), may eliminate suitable bypass graft targets, and is suboptimal for treatment of stent failure owing to its obligate space-occupying effects. In addition, for cultural or religious reasons, many patients would prefer not to have a permanent implant. Drug-eluting bioresorbable scaffolds were designed to overcome many of these very late limitations of metallic drug-eluting stents (DES) by providing temporary mechanical support and antiproliferative effects similar to metallic DES but then completely resorbing within several years, normalizing vascular function and potentially improving late outcomes.8
The most widely studied bioresorbable scaffold is the poly-l-lactic acid (PLLA)–based everolimus-eluting Absorb bioresorbable vascular scaffold (BVS) (Abbott Vascular), which, in a porcine model, completely resorbs in approximately 3 years.9,10 Numerous randomized clinical trials of BVS compared with contemporary cobalt-chromium fluoropolymer-based everolimus-eluting stents (EES) demonstrated that within the first 3 years, BVS resulted in higher adverse event rates than EES, which has been attributed largely to the relatively thick struts and suboptimal mechanical characteristics of this first-generation design, as well as suboptimal implantation technique.8,11,12 While these limitations may be potentially overcome with device design and implantation technique enhancements, to our knowledge, whether BVS is as safe as or more safe and effective than metallic DES beyond 3 years has not been reported. We therefore performed a systematic meta-analysis and individual patient data (IPD) pooled analysis of completed randomized clinical trials of the Absorb BVS to examine its relative outcomes before and after 3 years, the established point of its complete bioresorption in animal models.
Methods
Trials
For inclusion in this meta-analysis, we identified all randomized clinical trials of the Absorb BVS vs metallic DES in which at least 5-year clinical follow-up has been reported. This systematic meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for aggregate-level data and IPD (eTable 1 in the Supplement).13,14 Eligible studies were identified by searching MEDLINE and the Cochrane database, http://www.tctmd.com, http://www.clinicaltrials.gov, http://www.pcronline.com, http://www.clinicaltrialresults.org, and https://www.acc.org using the keywords “randomized trial,” “drug-eluting stent,” “everolimus-eluting stent,” “Xience,” “bioabsorbable scaffold,” “bioresorbable scaffold,” “bioabsorbable stent,” and “bioresorbable stent” through July 21, 2019, in duplicate. The primary exclusion criteria were observational or nonrandomized study design, less than 5 years of follow-up data, lack of interval data between 0 to 3 years and 3 to 5 years, non-Absorb BVS, metallic DES with bioabsorbable polymers, editorials, letters, expert opinions, case reports/series, studies with duplicated data, and nonhuman studies. Two reviewers (Z.A.A. and G.W.S.) abstracted and reviewed the trials. Five-year data were available from 4 trials meeting these criteria in which patients with noncomplex coronary artery disease were randomized to BVS vs EES (Abbott Vascular) (eFigure 1 in the Supplement). The 5-year outcomes from the ABSORB II trial (n = 501) have been publicly reported.15,16 Three other qualifying trials have reached their 5-year end point, their databases have been locked, and the results will be reported in September 2019: ABSORB Japan (n = 400),17 ABSORB China (n = 480),18 and ABSORB III (n = 2008).19,20 The sponsor of the 4 ABSORB trials (Abbott Vascular) and the principal investigators of each study have provided the data from these 4 trials for this IPD and aggregate summary-level analyses. The 5-year data from 1 other trial, Comparison of Everolimus- and Biolimus-Eluting Stents With Everolimus-Eluting Bioresorbable Vascular Scaffold Stents II (EVERBIO II), in which 238 patients were randomized 1:2 to BVS vs DES,21 have not been reported and were not available for this report. The current version of the Cochrane tool (RoB 2) was used to evaluate selection bias for each trial.22 The risk of bias was low in the 4 trials other than some concerns because of missing data (eTable 2 in the Supplement). Each study was approved by the institutional review board or ethics committee at each participating center, and all patients signed informed, written consent prior to randomization.
End Points and Definitions
Consistent with the prespecified secondary end points of the ABSORB III and ABSORB IV trials, we hypothesized that the relative hazard for adverse events after BVS compared with DES would vary before and after 3 years following its implantation.19,20,23 The primary effectiveness outcome measure for this study was the device-oriented composite end point of target lesion failure (TLF; cardiac mortality, target vessel–related myocardial infarction [TV-MI], or ischemia-driven target lesion revascularization [ID-TLR]). The primary safety outcome measure was definite or probable device thrombosis according to the Academic Research Consortium criteria.24 Secondary end points included the patient-oriented composite end point (POCE; all-cause mortality, all MI, or all revascularization), all-cause mortality and its subcategorization as cardiac vs noncardiac mortality, all MI and its subcategorization as TV-MI vs non–TV-MI, all revascularization, ID-TLR and ischemia-driven target vessel revascularization (ID-TVR), and device thrombosis subcategorized as definite or probable. The definitions used in each trial for all the end points were identical except for periprocedural MI, which for uniformity was converted from each trial to the ABSORB III definition using original source data.
Statistical Analysis
All data were analyzed in the intention-to-treat population, consisting of all patients in their randomized groups regardless of treatment received. All outcomes were examined between 0 days to 5 years and between 0 days to 3 years and 3 years to 5 years, with the 3-year landmark, representing the established approximate point of complete scaffold bioresorption in animals.8,9,10 For the main IPD analysis, patients with nonfatal events before 3 years were included in the landmark analysis between 3 to 5 years. A sensitivity analysis was performed in which patients with nonfatal events before 3 years were excluded from the 3-year to 5-year analysis. Time to first event curves are displayed using Kaplan-Meier estimates, with between-group differences tested using the log-rank test, stratified by study. Hazard ratios (HR) with 95% confidence intervals were determined using a study-stratified Cox proportional hazards regression model with no other covariates. The factors independently associated with TLF in the 3 periods were determined by multivariable Cox regression, stratified by study, with the variables for each model chosen according to their historical relationship to TLF. The consistency of the treatment effect on selected end points in relevant subgroups was examined with formal interaction testing. To further examine the change in HR during the 5-year follow-up period, a flexible parametric survival model was used to estimate the HR and 95% confidence interval for TLF over time. An interaction term between treatment and a natural spline of the log of time was included in the model.
Study-level treatment outcomes were examined using both a Mantel-Haenszel fixed-effect model and a DerSimonian and Laird random-effect model. Summary statistics are relative risks (RR) with 95% confidence intervals. Heterogeneity between trials was evaluated with the Cochran Q test and the I2statistic (with <25%, 25%-50%, and >50% indicating low, moderate, and high heterogeneity, respectively).
Baseline characteristics are summarized using means and standard deviations for continuous variables and as numbers and percentages for categorical variables. Continuous data were compared by t test, and binary data were compared by Pearson χ2 test or Fisher exact test. A sensitivity analysis using multiple imputation to account for missing follow-up data was performed on the IPD pooled data set.25 Meta-analysis was performed using the meta package (version 4.9-2) in R, version 3.5.1 (the R Foundation). All other statistical analyses were performed with SAS, version 9.4 (SAS Institute).
Results
Patients and Procedures
The 4 ABSORB trials enrolled 3389 patients at 301 centers in North America, Europe, and Asia (Table 1)26; 2164 and 1225 patients were randomly assigned to BVS and EES, respectively. Three patients randomized to BVS and 2 patients randomized to EES in the ABSORB China trial withdrew consent immediately after enrollment and were deregistered. Thus, the study population consists of 3884 patients (2161 BVS-treated and 1223 EES-treated). Three-year and 5-year follow-up data were available in 2054 patients (95.1%) and 1892 patients (87.6%) treated with BVS and in 1160 patients (94.9%) and 1084 patients (88.6%) treated with EES, respectively. The baseline characteristics of the patients enrolled from each study have been previously reported.27 Baseline clinical features and angiographic data for the pooled analysis are shown in eTables 3 and 4 in the Supplement and were well matched between groups. Procedural and angiographic results for the randomized groups are shown in eTable 5 in the Supplement. Device length was marginally less for BVS compared with EES, despite similar lesion length. Postdilatation and intravascular imaging guidance were more frequent with BVS. The final minimal lumen diameter was smaller and the in-device percent diameter stenosis was greater with BVS than EES. Dual antiplatelet therapy was used slightly more frequently with BVS than EES from 2 years and beyond (eTable 6 in the Supplement).
Table 1. Major Characteristics of the 4 Randomized ABSORB Trials.
| Characteristic | ABSORB II | ABSORB | ABSORB III | |
|---|---|---|---|---|
| Japan | China | |||
| ClinicalTrials.gov identifier | NCT01425281 | NCT01844284 | NCT01923740 | NCT01751906 |
| Masking | Single blind | Single blind | Open label | Single blind |
| No. of centers | 46 | 38 | 24 | 193 |
| No. of randomized patients | 501 | 400 | 480a | 2008 |
| Assigned to BVS | 335 | 266 | 241 | 1322 |
| Assigned to EES | 166 | 134 | 239 | 686 |
| No. of study lesions allowed | 2 | 2 | 2 | 2 |
| No. of study vessels allowedb | 2 | 2 | 2 | 2 |
| Target lesion reference vessel diameter | Maximum lumen diameter 2.25 to 3.8 mm by online QCA | ≥2.5 to ≤3.75 mm by online QCA or visual assessment | ≥2.5 to ≤3.75 mm by online QCA or visual assessment | ≥2.5 to ≤3.75 mm by visual assessment (QCA or imaging allowed) |
| Target lesion length, mm | ≤48 | ≤24 | ≤24 | ≤24 |
| Device overlap allowed | Yes | For bailout only | For bailout only | For bailout only |
| Routine angiographic follow-up | At 3 y | At 13 mo | At 1 y | No |
| Primary end point | Angiographic vasomotion at 3 y | TLF at 1 y | Angiographic in-segment late loss at 1 y | TLF at 1 y |
| Clinical follow-up complete, No. (%)c | ||||
| 3 y | 481 (96.0) | 383 (95.8) | 471 (99.2) | 1879 (93.6) |
| 5 y | 401 (80.0) | 375 (93.8) | 458 (96.4) | 1742 (86.7) |
| Total duration of follow-up, y | 5 | 5 | 5 | 5 |
Abbreviations: BVS, bioresorbable vascular scaffolds; EES, everolimus-eluting stents; QCA, quantitative coronary angiography; TLF, target lesion failure.
A total of 5 patients (3 randomized to BVS and 2 randomized to EES) withdrew consent immediately after enrollment and were deregistered. These patients are not included in the study population.
Maximum 1 lesion per vessel.
Follow-up is defined as complete for that time if there is follow-up data within 28 days or a prior TLF event or death. Modified from Stone et al.26
Individual Patient Data Outcomes
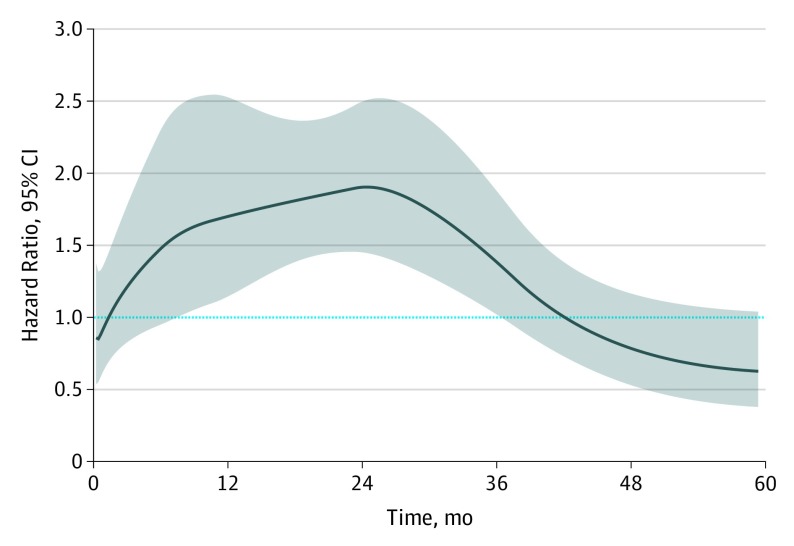
Study level–stratified IPD pooled estimates for adverse events occurring through 5 years after randomization in the 4 ABSORB trials appear in Table 2 and Figure 1A and B. The cumulative 5-year rates of TLF, POCE, all MI, TV-MI, ID-TLR, and device thrombosis were greater with BVS than EES. There were no significant differences in all-cause death or cardiac death between the groups. Outcomes between 0 to 3 years and 3 to 5 years appear in Table 3 and Figure 1C and D. Between 0 and 3 years, TLF occurred in 11.6% of 2161 BVS-treated patients vs 7.9% of 1223 EES-treated patients (HR, 1.42; 95% CI, 1.12-1.80), whereas between 3 and 5 years, TLF occurred in 4.3% of 1984 at-risk BVS-treated patients vs 4.5% of 1121 at-risk EES-treated patients (HR, 0.92; 95% CI, 0.64-1.31) (P for interaction = .046). By spline analysis, the HR for the risk of BVS compared with EES for TLF was relatively constant at 1.5 to 2.0 between 6 and 30 months and then progressively declined. The lower bound of the 95% CI of the HR was less than 1.0 at 36 months and the HR was less than 1.0 at 42 months (Figure 2). Between 0 and 3 years, device thrombosis occurred in 2.4% of 2161 BVS-treated patients vs 0.6% of 1223 EES-treated patients (HR, 3.86; 95% CI, 1.75-8.50), whereas between 3 and 5 years, device thrombosis occurred in 0.1% of 1984 at-risk BVS-treated patients vs 0.3% of 1121 at-risk EES-treated patients (HR, 0.44; 95% CI, 0.07-2.70) (P for interaction = .03). The increased risks of POCE, all MI, TV-MI, and ID-TLR present with BVS compared with EES between 0 and 3 years were also not evident between 3 and 5 years. The results were similar after multiple imputation to account for missing data (eTable 7 in the Supplement).
Table 2. Adverse Event Rates Cumulative Through 5 Years.
| Adverse Event | Events, No. (%)a | HR (95% CI) | P Value | |
|---|---|---|---|---|
| BVS (n = 2161) | EES (n = 1223) | |||
| TLF | 308 (14.9) | 135 (11.6) | 1.26 (1.03-1.54) | .03 |
| POCE | 550 (26.4) | 267 (22.7) | 1.15 (0.99-1.33) | .07 |
| All-cause mortality | 119 (5.9) | 64 (5.6) | 1.02 (0.75-1.38) | .92 |
| Cardiac | 44 (2.2) | 31 (2.8) | 0.79 (0.50-1.25) | .31 |
| Noncardiacb | 75 (3.8) | 33 (2.9) | 1.23 (0.81-1.85) | .33 |
| All MI | 221 (10.7) | 92 (7.9) | 1.30 (1.02-1.66) | .03 |
| TV-MI | 184 (8.8) | 64 (5.5) | 1.55 (1.16-2.06) | .003 |
| Non-TV-MI | 51 (2.5) | 35 (3.1) | 0.78 (0.51-1.20) | .26 |
| All revascularization | 378 (18.4) | 189 (16.3) | 1.10 (0.92-1.31) | .28 |
| ID-TLR | 172 (8.4) | 67 (5.8) | 1.41 (1.06-1.87) | .02 |
| ID-TVR | 268 (13.1) | 112 (9.8) | 1.32 (1.06-1.65) | .01 |
| Device thrombosis, definite/probable | 53 (2.5) | 10 (0.8) | 2.87 (1.46-5.65) | .002 |
| Definite | 48 (2.3) | 8 (0.7) | 3.14 (1.48-6.64) | .003 |
| Probable | 5 (0.2) | 2 (0.2) | 1.73 (0.33-9.09) | .52 |
Abbreviations: BVS, bioresorbable vascular scaffold; EES, everolimus-eluting stents; HR, hazard ratio; ID-TLR, ischemia-driven target lesion revascularization; ID-TVR, ischemia-driven target vessel revascularization; MI, myocardial infarction; POCE, patient-oriented composite end point (all death, all MI, or all revascularization); TLF, target lesion failure (cardiac death, TV-MI, or ID-TLR); TV-MI, target vessel–related MI.
Event rates are Kaplan-Meier time to first event estimates.
Includes noncardiac vascular deaths.
Figure 1. Study-Level Stratified Individual Patient Data Pooled Event Rates for 3884 Patients Randomized to Bioresorbable Vascular Scaffolds (BVS) vs Everolimus-Eluting Stents (EES) in 4 Randomized Clinical Trials.
A, Target lesion failure cumulative through 5 years. B, Device thrombosis (definite or probable) cumulative through 5 years. C, Target lesion failure between 0 to 3 years and 3 to 5 years. D, Device thrombosis (definite or probable) between 0 to 3 years and 3 to 5 years. The P value for interaction (Pint) represents the likelihood of interaction between the periods and the relative treatment effect. HR indicates hazard ratio.
Table 3. Adverse Event Rates Occurring Within the First 3 Years and Between 3 Years and 5 Yearsa.
| Event | From Randomization to 3 y | From 3 y to 5 y | P Value for Interaction | ||||
|---|---|---|---|---|---|---|---|
| No. (%) | HR (95% CI) | No. (%) | HR (95% CI) | ||||
| BVS (n = 2161) | EES (n = 1223) | BVS (n = 1984) | EES (n = 1121) | ||||
| TLF | 245 (11.6) | 95 (7.9) | 1.42 (1.12-1.80) | 82 (4.3) | 48 (4.5) | 0.92 (0.64-1.31) | .046 |
| POCE | 422 (19.9) | 190 (15.8) | 1.23 (1.04-1.46) | 180 (9.4) | 100 (9.3) | 0.97 (0.76-1.24) | .10 |
| All-cause mortality | 54 (2.6) | 35 (3.0) | 0.84 (0.55-1.29) | 65 (3.4) | 29 (2.7) | 1.22 (0.79-1.90) | .23 |
| Cardiac | 22 (1.1) | 13 (1.1) | 0.94 (0.47-1.88) | 22 (1.2) | 18 (1.7) | 0.68 (0.36-1.26) | .48 |
| Noncardiacb | 32 (1.5) | 22 (1.9) | 0.79 (0.46-1.35) | 43 (2.3) | 11 (1.0) | 2.11 (1.09-4.10) | .02 |
| All MI | 190 (9.0) | 66 (5.5) | 1.56 (1.18-2.06) | 38 (2.0) | 28 (2.6) | 0.71 (0.44-1.16) | .004 |
| TV-MI | 161 (7.6) | 49 (4.1) | 1.76 (1.28-2.43) | 27 (1.4) | 15 (1.4) | 0.96 (0.51-1.81) | .05 |
| Non–TV-MI | 39 (1.9) | 21 (1.8) | 1.01 (0.59-1.73) | 12 (0.7) | 14 (1.3) | 0.44 (0.20-0.95) | .08 |
| All revascularization | 299 (14.3) | 138 (11.6) | 1.20 (0.98-1.47) | 108 (5.7) | 67 (6.3) | 0.86 (0.63-1.17) | .08 |
| ID-TLR | 137 (6.6) | 51 (4.3) | 1.48 (1.07-2.04) | 43 (2.3) | 19 (1.8) | 1.20 (0.70-2.06) | .52 |
| Device thrombosis, definite/probable | 51 (2.4) | 7 (0.6) | 3.86 (1.75-8.50) | 2 (0.1) | 3 (0.3) | 0.44 (0.07-2.70) | .03 |
Abbreviations: BVS, bioresorbable vascular scaffold; EES, everolimus-eluting stents; HR, hazard ratio; ID-TLR, ischemia-driven target lesion revascularization; MI, myocardial infarction; POCE, patient-oriented composite end point (all death, all MI, or all revascularization); TLF, target lesion failure (cardiac death, TV-MI or ID-TLR); TV-MI, target vessel–related MI.
Event rates are Kaplan-Meier time to first event estimates expressed as event, number (percentage). Denominators are patients known to be alive and with valid follow-up at the beginning of the interval. Event rates are nonhierarchical. The 3-year to 5-year landmark period includes all randomized patients at 3 years except those who died before 3 years (day 1095). Thus, there may be some patients with a nonfatal event within 3 years who have a second event between 3 years and 5 years. The results were similar when patients with nonfatal events within the first 3 years were excluded from the 3-year to 5-year landmark analysis period (eTable 12 in the Supplement).
Includes noncardiac vascular deaths.
Figure 2. Spline Analysis Demonstrating the Association of the Hazard for Target Lesion Failure After Treatment With Bioresorbable Vascular Scaffolds (BVS) vs Everolimus-Eluting Stents (EES) During the 5-Year Follow-up Period.
The solid black line represents the hazard ratio while the gray shadow represents the 95% confidence interval. There were not enough events to perform a similar analysis for device thrombosis.
Multivariable factors associated with TLF are shown in eTable 8 in the Supplement. Treatment with BVS vs EES was a strong independent factor associated with TLF between 0 to 5 years and 0 to 3 years, but not between 3 and 5 years. In this latter period, only diabetes and hypertension were associated with TLF. The treatment effect of BVS vs EES was also consistent across 11 baseline subgroups for the TLF end point through 5 years and between 3 to 5 years (eFigure 2 in the Supplement).
Aggregate Outcomes
Individual study-level and summary-level estimates for adverse events from the 4 trials occurring from randomization through 5 years and between 0 to 3 years and 3 to 5 years appear in eTables 9-11 and eFigures 3-5 in the Supplement. A similar time-dependent heterogeneity of treatment effect was observed in the aggregate study meta-analysis as in the IPD pooled analysis. Treatment with BVS compared with EES cumulative through 3 years and 5 years resulted in greater rates of composite TLF and POCE, owing to increased rates of all MI, TV-MI, ID-TLR, and definite device thrombosis, with similar rates of death. In contrast, between 3 and 5 years the rates of all ischemic end points were not significantly different between BVS and EES. These results were similar in the random-effect and fixed-effect models. No significant heterogeneity was present between the 4 studies for any of the evaluated end points in the 3 periods.
Discussion
The major findings from this systematic meta-analysis and IPD pooled analysis of 4 randomized trials of Absorb BVS vs metallic EES in 3884 patients with follow-up through 5 years are as follows: (1) BVS use was associated with higher 5-year rates of the device-oriented composite end point of TLF and the POCE owing to increased rates of TV-MI, all MI, ID-TLR, and device thrombosis within the first 3 years after implantation; (2) in contrast to the first 3 years, the absolute and relative rates of adverse events with BVS were markedly less between 3 and 5 years after implantation, such that there were no significant differences in any adverse outcomes between BVS and EES in this interval; and (3) these results were confirmed by spline analysis, in multivariable analysis, and after multiple imputations to account for missing follow-up data and were consistent in 11 examined subgroups and across the 4 randomized trials.
The increased risk of the polymeric Absorb BVS within 3 years of its implantation has been previously reported.8,11,12 Many of these adverse events have been attributed to the relatively thick struts of this first-generation device (150 μm), which was required for adequate radial strength, suboptimal mechanical properties including a risk of fracture with overexpansion, device implantation technique not optimized for these characteristics, and a unique failure mode during its bioresorption by bulk erosion, namely intraluminal scaffold dismantling.8,28,29 These issues may in part be overcome by improvements in device design and construction and deployment technique. Scaffolds nearly as thin as metallic DES with favorable expansion properties and minimal recoil have been developed, and improved 3-year results with a 100-μm PLLA-based bioresorbable scaffold have been reported.30 Use of BVS-specific implantation techniques have been associated with substantially reduced early and late event rates.23,31,32 However, what has not previously been described, to our knowledge, is whether the safety and effectiveness profile of BVS changes after 3 years, the point of its complete bioresorption in animal models. In this regard, neoatherosclerosis has been reported to occur at the prior BVS implant site beyond 3 years.33
This study demonstrates a marked difference in the absolute and relative hazards of BVS after 3 years compared with before 3 years, the point after which PLLA is no longer detectable by high-pressure liquid chromatography in animals and at which imaging studies demonstrate the absence of an organized scaffold frame (although ghost shadows of prior strut cross-sections without PLLA material after its replacement by proteoglycans may still be visible for some time by optical coherence tomography).9,10 Serial optical coherence tomography imaging has demonstrated similar changes in the structure of the BVS scaffold over time in humans as in pigs.34 Significant time-treatment interactions were present for both TLF and device thrombosis before vs after 3 years. Before 3 years, adverse event rates were clearly increased with BVS compared with EES, many of which have been attributed to the greater risk of scaffold thrombosis.8,11 However, after 3 years, the point estimates slightly favored BVS, although the confidence intervals were wide and the differences not significant, reflecting the fact that these trials (and even this meta-analysis) were not powered to show a difference in event rates between the devices in this interval. Nonetheless, given the major excess in device thrombosis with BVS compared with EES before 3 years, the fact that between 3 and 5 years, device thrombosis occurred in 0.1% BVS-treated patients vs 0.3% EES-treated patients (HR, 0.44; 95% CI, 0.07-2.70) is notable.
Limitations
Additional limitations of this study deserve mention. First, the 3-year cutoff was prespecified as the point of approximate complete BVS bioresorption, consistent with the chromatographic findings from porcine studies demonstrating absence of polymer at this time and the comparable serial imaging findings from porcine and human studies.9,10,34 However, the exact point of the complete bioresorption of PLLA in humans is unknown. While the degradation and resorption rate for any given PLLA formulation is species independent and depends principally on water content and temperature, the resulting structures and geometries that ensue are variable and depend on implantation technique and acute results and on the biologic makeup of the tissue that replaces the scaffold (eg, proportion of cellular content vs extracellular matrix). Nonetheless, the marked change in absolute and relative clinical risk with BVS observed at and beyond 3 years (especially for device thrombosis) is consistent with this landmark representing the point of clinical stabilization after scaffold resorption in humans. However, the conversion from excess BVS risk to stabilization may in truth be more gradual. Spline modeling suggested that the peak point for BVS risk for TLF was at 2 years, after which the relative hazard of BVS gradually fell, with a similar or lower risk observed with BVS compared with EES between 3 and 5 years.
Second, 3 of the Absorb trials were single blind and 1 (Absorb China) was open label. The risk of bias by the Cochrane tool was judged as low for all 4 trials except for some concerns from missing data. This issue was addressed by performing multiple imputation, which demonstrated results consistent with the primary analysis. Third, many high-risk patients and complex lesions were excluded from the 4 ABSORB randomized trials, including in-stent restenosis lesions, true bifurcations, chronic total occlusions, and acute MIs. Long-term outcomes in large randomized clinical trials are required to examine the late performance of bioresorbable technology in these settings. In addition, this systematic review included only those trials that had reached 5-year follow-up with available data. The study results should be confirmed as additional studies reach this landmark. Fourth, the ABSORB trials were performed before the recognition of the importance of optimized scaffold-specific technique. While improved scaffold deployment has been associated with improved BVS outcomes within the first several years of implantation,23,31,32 whether it would affect very late outcomes after complete scaffold bioresorption is unknown. This question may be answered in part by the 5-year follow-up from the large-scale ABSORB IV trial in which improved technique was used.23 Fifth, dual antiplatelet therapy was used in approximately 4% to 5% more BVS-treated patients than EES-treated patients between 2 and 5 years. Given this constant difference, it is unlikely that dual antiplatelet therapy use affected the relative change in event rate trajectory before and after 3 years. However, 40% of BVS-treated patients (n = 701 of 1762) and 36% of EES-treated patients (n = 364 of 1017) were still receiving dual antiplatelet therapy at 5 years. Whether the absolute or relative differences in device thrombosis between years 3 and 5 would have varied with greater or lesser dual antiplatelet therapy use in this very late period is unknown. Sixth, noncardiac death was increased in BVS-treated patients between 3 and 5 years, a finding that should be interpreted cautiously given the similar total mortality between the devices in this period, the absence of a likely mechanism, and the lack of adjustment of the numerous secondary end points reported for multiplicity. Seventh, while it might be conjectured that the results from this study are fundamental and therefore translatable to all bioresorbable scaffolds once they have completely resorbed, long-term data from large-scale studies of other polymeric and metal-based resorbable coronary implants are required before reaching this conclusion. Finally, follow-up from the ABSORB trials has concluded at 5 years, and even our large-scale pooled analysis was not adequately powered to determine whether event rates between the devices differ between 3-year and 5-year follow-up. Whether BVS are noninferior or superior to EES or other contemporary metallic DES would likely require follow-up for 10 years or more in very large trials, a not unreasonable requirement given the millions of patients treated with DES every year worldwide.
Conclusions
In conclusion, this IPD pooled analysis and summary-level meta-analysis from 4 randomized trials of the PLLA-based everolimus-eluting BVS vs cobalt-chromium fluoropolymer-based EES in 3884 patients demonstrates that although the rates of adverse ischemic events cumulative through 5 years were increased with the first-generation BVS compared with EES, the period of excess risk ended at 3 years. These data provide mechanistic insights into the timing of adverse events after BVS and identify the hurdles that need to be overcome for BVS technology to provide enhanced patient benefit. Specifically, if new-generation bioresorbable scaffolds are demonstrated to have comparable results with metallic DES during their active bioresorption phase, this study suggests that BVS technology might be an acceptable alternative to metallic DES for many patients with coronary artery disease.
eTable 1. PRISMA checklist
eTable 2. Risk of bias in the 4 ABSORB trials
eTable 3. Baseline clinical features and antiplatelet medications
eTable 4. Baseline angiographic features (core laboratory)
eTable 5. Procedural and angiographic results (core laboratory)
eTable 6. Antiplatelet agent use during follow-up
eTable 7. Adverse event rates occurring within 5 years, within 3 years and between 3 years and 5 years after multiple imputation to account for missing follow-up data
eTable 8. Independent predictors of target lesion failure by Cox regression between 0 to 5 years, 0 to 3 years and 3 to 5 years
eTable 9. Aggregate level treatment effects from 0 through 5 years
eTable 10. Aggregate level treatment effects from 0 through 3 years
eTable 11. Aggregate level treatment effects between 3 years and 5 years
eTable 12. Adverse event rates occurring within the first 3 years and between 3 years and 5 years, with events before 3 years censored at the landmark period
eFigure 1. Search strategy diagram
eFigure 2. Subgroup outcomes for target lesion failure between 0 to 5 and 3 to 5 years
eFigure 3. Aggregate level meta-analysis, cumulative outcomes through 5 years
eFigure 4. Aggregate level meta-analysis, cumulative outcomes through 3 years
eFigure 5. Aggregate level meta-analysis, cumulative outcomes between 3 and 5 years
References
- 1.Yamaji K, Räber L, Zanchin T, et al. . Ten-year clinical outcomes of first-generation drug-eluting stents: the Sirolimus-Eluting vs. Paclitaxel-Eluting Stents for Coronary Revascularization (SIRTAX) VERY LATE trial. Eur Heart J. 2016;37(45):3386-3395. doi: 10.1093/eurheartj/ehw343 [DOI] [PubMed] [Google Scholar]
- 2.Gada H, Kirtane AJ, Newman W, et al. . 5-Year results of a randomized comparison of XIENCE V everolimus-eluting and TAXUS paclitaxel-eluting stents: final results from the SPIRIT III trial (clinical evaluation of the XIENCE V everolimus eluting coronary stent system in the treatment of patients with de novo native coronary artery lesions). JACC Cardiovasc Interv. 2013;6(12):1263-1266. doi: 10.1016/j.jcin.2013.07.009 [DOI] [PubMed] [Google Scholar]
- 3.Yamaji K, Kimura T, Morimoto T, et al. . Very long-term (15 to 20 years) clinical and angiographic outcome after coronary bare metal stent implantation. Circ Cardiovasc Interv. 2010;3(5):468-475. doi: 10.1161/CIRCINTERVENTIONS.110.958249 [DOI] [PubMed] [Google Scholar]
- 4.Kuramitsu S, Jinnouchi H, Shinozaki T, et al. . Incidence and long-term clinical impact of late-acquired stent fracture after sirolimus-eluting stent implantation in narrowed coronary arteries. Am J Cardiol. 2017;120(1):55-62. doi: 10.1016/j.amjcard.2017.03.259 [DOI] [PubMed] [Google Scholar]
- 5.Kuramitsu S, Hiromasa T, Enomoto S, et al. . Incidence and clinical impact of stent fracture after PROMUS element platinum chromium everolimus-eluting stent implantation. JACC Cardiovasc Interv. 2015;8(9):1180-1188. doi: 10.1016/j.jcin.2015.02.029 [DOI] [PubMed] [Google Scholar]
- 6.Otsuka F, Byrne RA, Yahagi K, et al. . Neoatherosclerosis: overview of histopathologic findings and implications for intravascular imaging assessment. Eur Heart J. 2015;36(32):2147-2159. doi: 10.1093/eurheartj/ehv205 [DOI] [PubMed] [Google Scholar]
- 7.Ali ZA, Roleder T, Narula J, et al. . Increased thin-cap neoatheroma and periprocedural myocardial infarction in drug-eluting stent restenosis: multimodality intravascular imaging of drug-eluting and bare-metal stents. Circ Cardiovasc Interv. 2013;6(5):507-517. doi: 10.1161/CIRCINTERVENTIONS.112.000248 [DOI] [PubMed] [Google Scholar]
- 8.Kereiakes DJ, Onuma Y, Serruys PW, Stone GW. Bioresorbable vascular scaffolds for coronary revascularization. Circulation. 2016;134(2):168-182. doi: 10.1161/CIRCULATIONAHA.116.021539 [DOI] [PubMed] [Google Scholar]
- 9.Otsuka F, Pacheco E, Perkins LE, et al. . Long-term safety of an everolimus-eluting bioresorbable vascular scaffold and the cobalt-chromium XIENCE V stent in a porcine coronary artery model. Circ Cardiovasc Interv. 2014;7(3):330-342. doi: 10.1161/CIRCINTERVENTIONS.113.000990 [DOI] [PubMed] [Google Scholar]
- 10.Onuma Y, Serruys PW, Perkins LE, et al. . Intracoronary optical coherence tomography and histology at 1 month and 2, 3, and 4 years after implantation of everolimus-eluting bioresorbable vascular scaffolds in a porcine coronary artery model: an attempt to decipher the human optical coherence tomography images in the ABSORB trial. Circulation. 2010;122(22):2288-2300. doi: 10.1161/CIRCULATIONAHA.109.921528 [DOI] [PubMed] [Google Scholar]
- 11.Ali ZA, Gao R, Kimura T, et al. . Three-year outcomes with the absorb bioresorbable scaffold: individual-patient-data meta-analysis from the ABSORB randomized trials. Circulation. 2018;137(5):464-479. doi: 10.1161/CIRCULATIONAHA.117.031843 [DOI] [PubMed] [Google Scholar]
- 12.Cassese S, Byrne RA, Jüni P, et al. . Midterm clinical outcomes with everolimus-eluting bioresorbable scaffolds versus everolimus-eluting metallic stents for percutaneous coronary interventions: a meta-analysis of randomised trials. EuroIntervention. 2018;13(13):1565-1573. doi: 10.4244/EIJ-D-17-00492 [DOI] [PubMed] [Google Scholar]
- 13.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stewart LA, Clarke M, Rovers M, et al. ; PRISMA-IPD Development Group . Preferred reporting items for systematic review and meta-analyses of individual participant data: the PRISMA-IPD statement. JAMA. 2015;313(16):1657-1665. doi: 10.1001/jama.2015.3656 [DOI] [PubMed] [Google Scholar]
- 15.Serruys PW, Chevalier B, Dudek D, et al. . A bioresorbable everolimus-eluting scaffold versus a metallic everolimus-eluting stent for ischaemic heart disease caused by de-novo native coronary artery lesions (ABSORB II): an interim 1-year analysis of clinical and procedural secondary outcomes from a randomised controlled trial. Lancet. 2015;385(9962):43-54. doi: 10.1016/S0140-6736(14)61455-0 [DOI] [PubMed] [Google Scholar]
- 16.Serruys PW, Chevalier B; the ABSORB II Investigators. The 5-year clinical outcomes of the ABSORB II trial: first randomized comparison between the Absorb everolimus eluting bioresorbable vascular scaffold and the XIENCE everolimus eluting stent. https://www.tctmd.com/slide/absorb-beyond-3-years-absorb-ii-5-year-data. Accessed July 22, 2019.
- 17.Kimura T, Kozuma K, Tanabe K, et al. ; ABSORB Japan Investigators . A randomized trial evaluating everolimus-eluting Absorb bioresorbable scaffolds vs. everolimus-eluting metallic stents in patients with coronary artery disease: ABSORB Japan. Eur Heart J. 2015;36(47):3332-3342. doi: 10.1093/eurheartj/ehv435 [DOI] [PubMed] [Google Scholar]
- 18.Gao R, Yang Y, Han Y, et al. ; ABSORB China Investigators . Bioresorbable vascular scaffolds versus metallic stents in patients with coronary artery disease: ABSORB China trial. J Am Coll Cardiol. 2015;66(21):2298-2309. doi: 10.1016/j.jacc.2015.09.054 [DOI] [PubMed] [Google Scholar]
- 19.Ellis SG, Kereiakes DJ, Metzger DC, et al. ; ABSORB III Investigators . Everolimus-eluting bioresorbable scaffolds for coronary artery disease. N Engl J Med. 2015;373(20):1905-1915. doi: 10.1056/NEJMoa1509038 [DOI] [PubMed] [Google Scholar]
- 20.Kereiakes DJ, Ellis SG, Metzger C, et al. ; ABSORB III Investigators . 3-Year clinical outcomes with everolimus-eluting bioresorbable coronary scaffolds: the ABSORB III trial. J Am Coll Cardiol. 2017;70(23):2852-2862. doi: 10.1016/j.jacc.2017.10.010 [DOI] [PubMed] [Google Scholar]
- 21.Puricel S, Arroyo D, Corpataux N, et al. . Comparison of everolimus- and biolimus-eluting coronary stents with everolimus-eluting bioresorbable vascular scaffolds. J Am Coll Cardiol. 2015;65(8):791-801. doi: 10.1016/j.jacc.2014.12.017 [DOI] [PubMed] [Google Scholar]
- 22.Sterne JAC, Savović J, Page MJ, et al. . RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 23.Stone GW, Ellis SG, Gori T, et al. ; ABSORB IV Investigators . Blinded outcomes and angina assessment of coronary bioresorbable scaffolds: 30-day and 1-year results from the ABSORB IV randomised trial. Lancet. 2018;392(10157):1530-1540. doi: 10.1016/S0140-6736(18)32283-9 [DOI] [PubMed] [Google Scholar]
- 24.Garcia-Garcia HM, McFadden EP, Farb A, et al. ; Academic Research Consortium . Standardized end point definitions for coronary intervention trials: the Academic Research Consortium-2 Consensus Document. Circulation. 2018;137(24):2635-2650. doi: 10.1161/CIRCULATIONAHA.117.029289 [DOI] [PubMed] [Google Scholar]
- 25.Little RJ, D’Agostino R, Cohen ML, et al. . The prevention and treatment of missing data in clinical trials. N Engl J Med. 2012;367(14):1355-1360. doi: 10.1056/NEJMsr1203730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stone GW, Gao R, Kimura T, et al. . 1-year outcomes with the Absorb bioresorbable scaffold in patients with coronary artery disease: a patient-level, pooled meta-analysis. Lancet. 2016;387(10025):1277-1289. [DOI] [PubMed] [Google Scholar]
- 27.Ali ZA, Serruys PW, Kimura T, et al. . 2-Year outcomes with the Absorb bioresorbable scaffold for treatment of coronary artery disease: a systematic review and meta-analysis of seven randomised trials with an individual patient data substudy. Lancet. 2017;390(10096):760-772. doi: 10.1016/S0140-6736(17)31470-8 [DOI] [PubMed] [Google Scholar]
- 28.Stone GW, Abizaid A, Onuma Y, et al. . Effect of technique on outcomes following bioresorbable vascular scaffold implantation: analysis from the ABSORB trials. J Am Coll Cardiol. 2017;70(23):2863-2874. doi: 10.1016/j.jacc.2017.09.1106 [DOI] [PubMed] [Google Scholar]
- 29.Stone GW, Granada JF. Very late thrombosis after bioresorbable scaffolds: cause for concern? J Am Coll Cardiol. 2015;66(17):1915-1917. doi: 10.1016/j.jacc.2015.08.863 [DOI] [PubMed] [Google Scholar]
- 30.Seth A, Onuma Y, Chandra P, et al. . Three-year clinical and two-year multimodality imaging outcomes of a thin-strut sirolimus-eluting bioresorbable vascular scaffold: MeRes-1 trial. EuroIntervention. 2019:EIJ-D-19-00324. doi: 10.4244/EIJ-D-19-00324 [DOI] [PubMed] [Google Scholar]
- 31.Puricel S, Cuculi F, Weissner M, et al. . Bioresorbable coronary scaffold thrombosis: multicenter comprehensive analysis of clinical presentation, mechanisms, and predictors. J Am Coll Cardiol. 2016;67(8):921-931. doi: 10.1016/j.jacc.2015.12.019 [DOI] [PubMed] [Google Scholar]
- 32.Tanaka A, Latib A, Kawamoto H, et al. . Clinical outcomes of a real-world cohort following bioresorbable vascular scaffold implantation utilising an optimised implantation strategy. EuroIntervention. 2017;12(14):1730-1737. doi: 10.4244/EIJ-D-16-00247 [DOI] [PubMed] [Google Scholar]
- 33.Moriyama N, Shishido K, Tanaka Y, et al. . Neoatherosclerosis 5 years after bioresorbable vascular scaffold implantation. J Am Coll Cardiol. 2018;71(17):1882-1893. doi: 10.1016/j.jacc.2018.02.051 [DOI] [PubMed] [Google Scholar]
- 34.Serruys PW, Ormiston J, van Geuns RJ, et al. . A Polylactide bioresorbable scaffold eluting everolimus for treatment of coronary stenosis: 5-year follow-up. J Am Coll Cardiol. 2016;67(7):766-776. doi: 10.1016/j.jacc.2015.11.060 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. PRISMA checklist
eTable 2. Risk of bias in the 4 ABSORB trials
eTable 3. Baseline clinical features and antiplatelet medications
eTable 4. Baseline angiographic features (core laboratory)
eTable 5. Procedural and angiographic results (core laboratory)
eTable 6. Antiplatelet agent use during follow-up
eTable 7. Adverse event rates occurring within 5 years, within 3 years and between 3 years and 5 years after multiple imputation to account for missing follow-up data
eTable 8. Independent predictors of target lesion failure by Cox regression between 0 to 5 years, 0 to 3 years and 3 to 5 years
eTable 9. Aggregate level treatment effects from 0 through 5 years
eTable 10. Aggregate level treatment effects from 0 through 3 years
eTable 11. Aggregate level treatment effects between 3 years and 5 years
eTable 12. Adverse event rates occurring within the first 3 years and between 3 years and 5 years, with events before 3 years censored at the landmark period
eFigure 1. Search strategy diagram
eFigure 2. Subgroup outcomes for target lesion failure between 0 to 5 and 3 to 5 years
eFigure 3. Aggregate level meta-analysis, cumulative outcomes through 5 years
eFigure 4. Aggregate level meta-analysis, cumulative outcomes through 3 years
eFigure 5. Aggregate level meta-analysis, cumulative outcomes between 3 and 5 years