ABSTRACT
Built environment restructuring can improve public health through increased opportunity for healthy behaviors. Behavioral science targets individual health behaviors within place, suggesting the potential to integrate these approaches. This scoping review was one of the first to summarise the impact built environment restructuring has on health outcomes and behaviors and integrate these findings with the Capability-Opportunity-Motivation-Behavior model and Theoretical Domains Framework of behavior change. Potential studies were identified from 12 academic databases in urban design, psychology and public health. Search parameters involved 50 environment types, for example green space or healthy cities, combined with both an intervention (e.g. green infrastructure, active transport) and a measurable health outcome (e.g. exercise, wellbeing). Searches were limited to North America, Europe, or Australia/New Zealand. Of 536 potential studies reviewed against defined inclusion/exclusion criteria, 23 contributed to the findings. Evidence supported the positive influence of restructuring on varied health outcomes, many of which were drivers and domains of health behavior. Most studies indicated a clear contribution to increased physical activity. Recommendations include the need for explicit communication of theories guiding restructuring project design, consideration of health outcomes beyond physical activity, and better investigation of unanticipated barriers to health behaviors arising from built environment restructuring projects.
KEYWORDS: Built environment, behavior change, COM-B, physical activity, public health, urban planning
Introduction
The built environment refers to ‘homes, schools, workplaces, parks/recreation areas, business areas and roads…. all buildings and spaces and products that are created or modified by people’ (Srinivasan et al. 2003, p. 1446). These places can influence population health (Barton and Grant 2006, 2013, Policy Connect 2017, World Health Organization (WHO) 2016, 2017), for example with effects on diabetes (Müeller-Riemenschneider et al. 2013), respiratory disease (Song et al. 2017), heart disease (Yitshak-Sade et al. 2017) and obesity (Mackenbach et al. 2014). The built environment also has an indirect influence on public health by providing or constraining opportunities for physical activity (Sallis et al. 2016), through food environments that encourage or discourage healthy diets (Lake and Townshend 2006, Townshend and Lake 2009, Algert et al. 2016, Townshend 2017), or by facilitating relaxation and recreation (Irvine et al. 2013, Völker and Kistermann 2015).
One approach to improve health outcomes is to provide more opportunity for healthy behaviors through built environment restructuring and urban planning (Barton and Grant 2006, Chriqui et al. 2016). In addition, behavioral science can be used to target individual health behaviors within these built environments (Davis et al. 2015, Glanz and Bishop 2010, Michie et al. 2013, Quigley 2013). However, the extent to which urban planning and behavioral science evidence intersect is unclear. This is possibly due to cross-disciplinary differences in methodology and targeted level of influence (Barton and Grant 2006, 2013, Tate et al. 2016). Recently, several studies suggested potential for the integration of these approaches; but were limited because there was no specific focus on built environment restructuring (Hollands et al. 2013) or the focus was on only one type of restructuring intervention (Arnott et al. 2014, Roberts et al. 2016). Building on this work, we conducted a scoping review of varied built environment restructuring projects for their impact on health outcomes and behaviors that are commonly targeted in behavioral science.
Behavioral science and behavior change theories cross disciplines such as psychology, economics, and marketing, highlighting a multitude of factors that influence individual behavior (Glanz and Bishop 2010, Matjasko et al. 2016); and research has implemented over 80 theories (Davis et al. 2015). Health psychologists and practitioners developed the Theoretical Domains Framework (TDF) to consolidate 33 of the most frequently used of these theories to identify 14 behaviour change domains, each ‘encompassing a set of similar theoretical constructs’ (Cane et al. 2012, p. 2). An example of a domain is a social influence, which includes a variety of constructs such as social support, group norms, or feedback. One model with increasing application within behaviour change research in recent years is the Capability-Opportunity-Motivation-Behavior model (COM-B), which suggests behaviour is the result of these three processes (Michie et al. 2011, 2014). Capability refers to necessary physical and psychological resources, opportunity to influences beyond the individual that facilitate or hinder behavior, and motivation to the varied influences on decision-making. An abridged overview of the COM-B and TDF is provided in Table 1; readers are encouraged to refer to the original articles for a full account of each.
Table 1.
Overview of the theory domain framework and capability-opportunity-motivation-behavior model of behavior change.
| Theoretical Domains Frameworka |
Capability-Opportunity-Motivation Modelb |
|---|---|
| TDF | COM-B |
| A framework of 14 domains (higher-order theoretical constructs) identified as being implemented across behavior change interventions in varied contexts including health. | Model consisting of three components for behavior change. The authors suggest capability and opportunity influence motivation. Behavior change is a bi-directional process by which all components influence the occurrence of the desired behavior; the occurence of the behavior can conversely contribute to perceptions of the components. |
| Knowledge (procedural, condition) | Capability (p.5) |
| ‘Actual capacity to engage in the behaviour.’ | |
| Skills (competence, development) | |
| Environmental context and resources (stressors, facilitators) | Opportunity (p. 5) |
| All factors external to the individual that make the behavior possible or prompt it.’ | |
| Social influence (social pressure, support) | |
| Intention (intrinsic motivation, commitment) | Motivation (p. 5) |
| “Brain processes that energize and direct | |
| Behavioural regulation (habits, monitoring) | Behaviour.” |
aCane et al. (2012). A subset of the 14 domains are listed here and examples of related constructs identified by Cane et al. are provided in (). For a full account of all domains, their constituent constructs, and how each domain corresponds to the COM-B model, refer to the original publication (pp. 8-10).
bMichie et al. (2011). Definitions of each model component are the original authors. For a full account of each component, refer to the original publication.
The COM-B and TDF were chosen as frameworks for this review because both highlight the important role of the environmental context, resources, and restructuring in changing health behaviors (Michie et al. 2011, Cane et al. 2012). The COM-B model was developed as a response to perceived limitations with existing models (Michie et al. 2011). Specifically, it encompasses varying levels of behavioral influence ranging from individual through to broader cultural, environmental and societal factors incorporated into a broader behavior change wheel to improve the design of behavior change interventions. The COM-B sits at the center of the wheel, contextualised by intervention function and policy typologies. In this regard, it was well suited to built environment restructuring initiatives that also vary in function and policy context. It was also integrated with the TDF framework to illustrate how the COM-B links explicitly to each theoretical domain. Additionally, the intention of the TDF was to provide a structured approach that would facilitate cross-disciplinary use of behavior change concepts by researchers from other professions (Cane et al. 2012).
In health behavior research, behavioral influences are often broadly categorized as micro or macro-level (Swinburn et al. 1999, Backholer et al. 2014). Macro-level factors include services or infrastructures across sectors such as public transportation systems; micro-level factors range from those in an immediate, specific location (e.g. within the home, the local doctor’s office) to neighbourhood or citywide initiatives like the introduction of cycle paths that operate at a larger spatial scale to impact daily activity (Swinburn et al. 1999, Hollands et al. 2013). The investigation of the complex interplay between human health and the built environment is well established in human geography, urban design/planning, and environmental psychology; and the micro and macro-level influences used in health behaviour research have clear parity with socio-ecological frameworks in these disciplines (Barton and Grant 2006, 2013, Sallis et al. 2006). However, explicit integration of behavioral science approaches typically operating at the individual level with the built environment approaches operating at higher micro- and macro-levels of influence has been limited to date.
Consequently, the aim of this scoping review was to determine whether the two approaches could be integrated. To achieve this aim, we focused on studies reporting built environment restructuring projects, which are considered interventions in TDF (Cane et al. 2012) and a type of behavior change technique (Michie et al. 2013). All studies also reported measurable outcomes relevant to behavior change; therefore, successfully achieving this aim would be evidenced, where possible, the findings could be integrated with the COM-B and TDF.
Varied methods are used to survey existing literature; and the manner by which information is reported and the degree of quality assessment in each varies (Garritty et al. 2016). The most rigorous is the systematic review, which typically focuses on the effectiveness clinical interventions, requires between 6–24 months to complete, implements very specific quantitative methods often including meta-analysis, and involves critical quality assessment of the evidence (Kanguara et al. 2012). Other rapid evidence assessment methods aim to balance the need for scientific rigor with the often time-limited requirements of the users of this information (Tricco et al. 2015). There is no agreed definition for rapid evidence assessments (Abou-Setta et al. 2016, Tricco et al. 2015). Generally they occur over a short time frame (3–6 months) using streamlined steps based on those for systematic reviews, for example by only searching one or limited numbers of academic databases, having one instead of two researchers extract data (Tricco et al. 2016), and/or excluding study quality assessment (Arksey and O’Malley 2005, Peters et al. 2015). A specific type of rapid evidence assessment is the scoping review, ‘a form of knowledge synthesis that addresses an exploratory research question aimed at mapping key concepts, types of evidence, and gaps in research related to a defined area or field by systematically searching, selecting, and synthesizing existing knowledge’ (Colquhoun et al. 2014, p. 1294). The scoping review was chosen because it was consistent with the aim of mapping concepts and evidence across disparate disciplines in an exploratory manner.
Methods
The review presented here was part of a wider literature review commissioned by the Public Health England Behavioural Insights Team to inform future research priorities. The methodology implemented five steps for scoping reviews: research question identification, identification of potential studies, inclusion/exclusion review, data charting, and findings/recommendations (e.g. Arksey and O’Malley 2005, Tricco et al. 2016). The funder specified the research question guiding the wider literature review: To what extent have built environment restructuring projects affected adult health outcomes and behaviors commonly used in behavioral science? Research inclusion/exclusion parameters and search terms were developed in conjunction with the funder. The authors independently generated the findings and recommendations.
To identify potential studies, the following databases were searched: Cochrane Library, Environmental Periodicals, PsycArticles, ProQuest, PubMed, SCOPUS, Social Sciences Index, SocINDEX, Thomson Reuters: Arts and Humanities Search, Urban Studies Abstracts, and Web of Science. During the search conducted between April–May 2017, three authors (A1, A2, A3) focused on the databases most relevant to their profession and implemented an iterative procedure with regular discussions to ensure consistent search methodology. The search included English-language studies with adult participants published between January 2000–March 2017. We chose 2000 as the starting point of our search because it allowed some time for the World Health Organization’s Healthy City Movement, initiated in the late 1980s/early 1990’s (Tsouros 1991), as well as the highlighted need for work linking built environments and public health at this time (e.g. Flynn 1996, Perdue et al. 2003) to be realised within both urban design and subsequent academic reporting. Searches were also limited to studies set in North American, Europe, or Australia/New Zealand as they have broadly similar urban design approaches to those in the UK, where the funder was based (Carmona et al. 2010).
Table 2 provides a summary of terms combined during the search process. This involved combining each lived environment search term with each intervention and each measurable outcome (e.g. urban AND active transport AND physical activity; urban AND active transport AND wellbeing). Built environment terms and project types included micro-level built projects beyond the immediate, specific spatial scale and macro-level projects (Swinburn et al. 1999, Backholer et al. 2014). Studies were excluded if they focused only on micro-level projects (e.g. within the home) or solely reported population-level trends associated with built environment characteristics. Measurable behaviours and outcomes were based on public health indicators such as obesity, physical activity and wellbeing (Department of Health 2015) and behavior change influences such as emotion, self-esteem, and social influence (Cane et al. 2012). Outcomes potentially related to capability and motivation and social opportunity aspects of the COM-B model were considered particularly important for searching based on the premise that built environment restructuring is intended to provide physical opportunity for health behaviors by default. Studies without measured behaviors or health outcomes were excluded (e.g. solely focused on subjective environment perceptions or social outcomes), as were studies conducted with child-only samples because adults often determine their experience in these settings.
Table 2.
Scoping review database search terms.
| Lived environments | Interventions | Measurable behaviours/outcomes linked to public health |
|---|---|---|
| Air quality Allotments Blue space* /City Cities, Towns Community gardens Country (nationality, not rural) Dene Dementia-friendly Districts /Eco- Eco-park Eco-town /Green Green field* Green space* Healthy cities /House Housing, Home, Housing plus Sheltered accommodation Inclusive design Lake* /Landscape Landscape planning Neighbour/neighbourhood New Urbanism Obesogenic Outdoor Park* Playing fields Promenade Public realm Region Responsive environments Resilient communities Salutogenic Seaside State Therapeutic landscape Town planning Townscape Transportation Urban Walkable /Water Waterfronts /Work Workplace, Worksite, Employment, Employer Occupational |
Behavio* insight Behavio* economics ‘Behavio* change’ ‘Behavior change technique taxonomy (BCCTv1)’ /COM-B Capability Motivation Opportunity Nudge theory Nudge Ability Accessibility /Active transport Paths/Footpaths Cycle lanes Trails Availability Competence Crime prevention /Environment* Ambient temperature Characteristics Noise Pollution Stressors Floorscaping Green infrastructure Healthy towns /Influenc* ‘Social influen*’ ‘Social norms’ Knowledge Landscaping Lighting Mobility Psycholog* ‘Psychosocial factors’ Reinforcement Rewards Skill Street furniture Tree planting Vegetation |
Alcohol Chronic conditions Diabetes Drug use Environmental attitude* Emotion Exercise Falls /Fatigue Tired* Injuries Health Health behaviour /Health-related quality of life Physical Mental /Medication Medication reduction /Mental health Anxiety, depression Mobility /Obesity Weight ‘Unhealthy adj4 weight’ ‘Healthy adj4 weight’ Pain management /Perception Attention, Memory Physical activity Physical inactivity Public health Restoration /Self- Care, Confidence, Efficacy, Esteem, Social isolation Sport Stress /Smoking Cessation, Tobacco use Water sports /Wellbeing Life satisfaction, Mood, Social cohesion, Social capital, Winter deaths |
After removing duplicates, 536 potential studies were identified using this search protocol. Before the abstract review, two researchers (A1, A3) randomly chose 20 titles and independently reviewed abstracts based on the inclusion/exclusion criteria. There was 100% agreement on which titles to include and which to exclude. One researcher (A1) conducted abstract reviews; 83 were retained. Five studies were randomly chosen by a second researcher (A3) and reviewed for inclusion/exclusion; again there was complete agreement.
Charting variables for full text review were consistent with recommendations (Arksey and O’Malley 2005). They included: authors/date/journal, location and type (e.g. intervention, natural experiment), theoretical framework, project type (e.g. vacant lot greening, cycleway installation), sample/methods, health outcomes, main findings, and recommendations.
Results
Included studies
Of the 83 studies identified from the abstract review for full text review, 57 were excluded using the stated criteria and three because full text could not be obtained. The included studies (N = 23, Figure 1) represented 19 independent built environment initiatives. Of these 19, three were quasi-experimental studies, 15 natural experiments, and one assessed the impact of built environment zoning (i.e. planning) targeted to improve health behavior using nationwide data (Chriqui et al. 2016). Two of these presented findings from multi-city natural experiments (Ward Thompson et al. 2012, Goodman et al. 2013). Based on U.K. Medical Research Council guidance (Craig et al. 2012), natural experiments were classified as initiatives or interventions were there was no random assignment or experimental manipulation either did not occur or was not feasible under the circumstances. Quasi-experimental studies were those where there was some experimental manipulation by the researcher when investigating the impact of built environment changes; none were randomised control trials.
Figure 1.
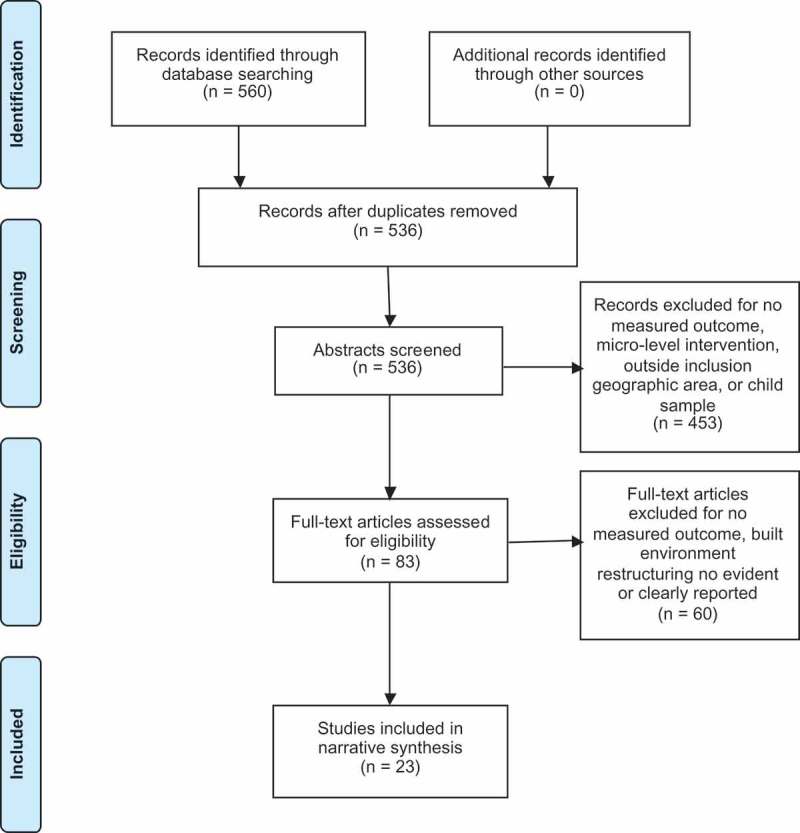
Flow diagram of extracted studies.
Studies were conducted in the USA (9), UK (5), Australia (3), Netherlands (1), and France (1). They were and reported in 17 journals, most of which were public health focused, although four were on urban design. Although the search timeframe was 17 years, the majority of studies (83%) were published in the last 5 years.
A summary of charted data for each study is provided in supplementary file 1. The narrative findings are presented by built environment project type, building development using New Urbanism design philosophy, health behaviours and outcomes affected, and methodologies used to assess the built environment. These findings are then integrated into the COM-B and TDF in the final sub-section of the results.
Built environment restructuring by type
World Health Organization Definitions of Physical Activity (2010; 2015)
Physical activity (PA) refers to movement classified in intensity based on ‘a ratio of working metabolic rate to resting metabolic rate’ (2015, p. 71).
Moderate physical activity requires motion between 3–6 times the intensity of an individual’s resting metabolic rate, or a 5–6 self-rating on a 0–10 scale of effort.
Vigorous physical activity typically refers to effort more than 6 times that resting rate, a self-rated effort of 7–8.
Recommended guidelines for healthy adults (18–64) are 150 minutes each week of moderate-to-vigorous physical activity (MVPA) accumulated from sessions of at least 10 minutes; 300 minutes is considered necessary for increased health benefits.
Active travel
Of the included studies, 61% reported environment restructuring with the aim to improve active travel and/or physical activity (PA). Six studies assessed transport infrastructure change on active travel and other PA; projects included a bus network and traffic-free walking/cycling route (Panter et al. 2016), a cycle lane/sidewalk/light rail project (Miller et al. 2015, Brown et al. 2016), cycle/sidewalk/pedestrian safety/aesthetics project with promotional programmes and signage specifying shortest/pleasant routes (Buscail et al. 2016), a multi-city initiative to improve urban greening/parking provision/pedestrian safety (Ward Thompson et al. 2012), and a traffic calming scheme (Morrison et al. 2004). There were clear links between usage of the new provisions and more active commuting (Miller et al. 2015, Panter et al. 2016), increased time spent in commute-related PA (Miller et al. 2015, Panter et al. 2016), increased walking (Morrison et al. 2004), and increased moderate-to-vigorous physical activity (MVPA) (Buscail et al. 2016). Benefits were best for those living closest to the new provision (Brown et al. 2016, Panter et al. 2016) or who were previously least active (Panter et al. 2016). Other outcomes affected included improved perceived safety and fewer unhealthy days by the elderly (Ward Thompson et al. 2012) and better quality of life (Morrison et al. 2004, Ward Thompson et al. 2012). However, barriers such as nuisances (e.g. groups of youths, dog fouling) increased; and decreased parking availability near the home was important to elderly PA levels (Ward Thompson et al. 2012). In the light rail extension project, some residents stopped using public transportation to result in decreased PA (Miller et al. 2015). The authors did not investigate why this occurred, missing an opportunity to explore potential barriers to public transportation usage. Finally, efforts to educate the public about PA opportunities did not translate into greater awareness of them (Buscail et al. 2016), suggesting message content and type of information campaign are also necessary considerations to effect health behavior change.
One nationwide US study provided comprehensive information on the impact of urban planning, specifically zoning code reforms, on active commuting using American Community Survey data (Chriqui et al. 2016). Zoning code reform to improve sidewalks, cycle-pedestrian connectivity/infrastructure, street connectivity, mixed-used development, and walkability were investigated for their impact on walking, cycling, public transportation use, or any active commuting. The most common zoning reforms were sidewalks/walkability/pedestrian infrastructure (> 70%), mixed-use development (58%) and shared cycle-pedestrian trails (57%). Overall, the rate of active commuting in nearly 4000 municipal jurisdictions across 48 US state was low, with only 6.25% engaging in any active travel. Residents in areas implementing pedestrian/transit-oriented reforms used public transit more; and in jurisdictions implementing eight or more reforms, walking, cycling and active travel levels were highest. Both walking and cycling to work were higher in areas with cycle parking, bike/pedestrian paths, walkability initiatives, and mixed-use development. This study was included because it illustrated the role urban planning plays in creating opportunity for behavior change in lived built environments based on its comprehensive review of behavioral differences resulting from zoning reform from approximately 4,000 US municipal jurisdictions covering 73% of the US population.
Three studies targeted cycling. These improved active transport and recreation-related PA in both cyclists and pedestrians (Goodman et al. 2013, Crane et al. 2016), increased numbers of new cyclists (Crane et al. 2016), and decreased car commuting (Goodman et al. 2013). Workplace initiatives to promote cycling collectively explained 33% of the variation between locations in cycling prevalence (Goodman et al. 2013). These workplace initiatives included cycle parking, travel planning, cycling training, and building ‘cycling culture’, all of which could be considered facilitators of health behavior in behavioral science (Thaler and Sunstein 2008). Seeing others cycle influenced activity (Crane et al. 2016) and paths improved perceived social connectedness and area aesthetics, suggesting social influences and beliefs/attitudes within TDF (Cane et al. 2012) were affected.
However, not all impact was positive. Barriers included feeling unable or ‘too old’ to cycle and cyclist-pedestrian conflict occurred due to insufficient ‘rules of the road’ information leading to safety concerns and perceived rudeness by cyclists towards non-cyclists (Crane et al. 2016). Additionally, Dill et al. (2014) reported new cycle boulevards had no impact on MVPA or minutes spent walking, and actually decreased bike trips. They noted positive attitudes towards the activity were important, reinforcing the potential for beliefs and attitudes to influence health behavior (McEachan et al. 2011).
Urban greenways
Urban greenways are ‘physical connectors between areas with green cover’ (Sharma 2015, p. 26), often to town centres or areas of mixed-land use, designed to improve both recreational and commuting PA. Although many initiatives have been reported, we found only four studies with measurable outcomes as defined here. Greenways resulted in higher PA in intervention locations compared to control streets (Fitzhugh et al. 2010, Gustat et al. 2012). Using health economics modelling, two studies explored the potential impact of new urban greenways on future health based on current resident PA (Dallat et al. 2014, Longo et al. 2015). Initial indications were 35% of males and 53% of females were not meeting MVPA guidelines prior to the project (Dallat et al. 2014). Perceived walkability also predicted behavior (Longo et al. 2015); residents who perceived ‘good’ availability of shops and facilities walked 37 minutes more per week. The authors estimated improved walkability combined with information programmes targeted at resident perceptions would increase MVPA in inactive residents by 39 minutes per week and potentially reduce mortality by 8%. Both study authors suggested these projects can be cost-effective in increasing PA (Fitzhugh et al. 2010) and improving quality-adjusted life years through reduced disease incidence (Dallat et al. 2014).
Urban green space
We only identified four studies of urban green space (UGS) projects that included any measurable outcomes of interest. An outdoor gym installation combined with behavior change facilitators such as marketing, instruction sessions and instructional guides attracted new elderly users, increased their confidence, and users indicated intentions for future use and recommendations to friends (Scott et al. 2014). In socio-economically disadvantaged areas, creating small parks on single plots of land had a positive effect. Self-reported (Branas et al. 2011) and observed PA/MVPA (Cohen et al. 2014) increased, perceived safety improved (Cohen et al. 2014), stress and crime/incivilities declined (Branas et al. 2011). Yet, other comprehensive restructuring initiatives within low socio-economic areas including UGS refurbishments, new parks, and improved neighbourhood ‘green character’ showed little impact on PA (Droomers et al. 2016). These authors noted substantial variation in initiatives meant combined analysis could have obscured the impact of specific interventions. They also speculated a lack of change in PA levels could have been the result of residents moving their PA to an improved local area, replacing PA in another location.
New Urbanism
The idea that built environments where people could live, work, and play support public health is a central tenet of New Urbanism (Day 2003). Features of these locations included mixed land usage, good walkability/active travel infrastructure, appropriate residential density, and parks/recreation space (Center for Active Design 2010). We included five studies describing three distinct New Urbanist locations that assessed measurable behavior change outcomes as specified by our criteria.
Across New Urbanist locations, residents engaged in more PA (Rodriguez et al. 2006, Calise et al. 2013, Christian et al. 2013, Zhu et al. 2013, Hooper et al. 2014) and more MVPA (Rodriguez et al. 2006, Zhu et al. 2013). Changes were most profound in those previously inactive or moving from less-walkable communities (Calise et al. 2013, Zhu et al. 2013). PA occurred within the neighbourhood more, suggesting design influenced where PA occurs (Rodriguez et al. 2006), as well as removing a barrier to PA (i.e. the need to travel) through better physical opportunity (Michie et al. 2011). Residents also reported better health after the move (Zhu et al. 2013), reduced social isolation, and reduced car journeys (Rodriguez et al. 2006, Zhu et al. 2013). New Urbanist design features varied in their impact (Hooper et al. 2014), with a neighbourhood centre complimented with higher-density housing increasing any walking and ≥ 60 minutes a week active transport; while better implementation of movement networks and land layout guidelines resulted in more recreational walking. Yet, across New Urbanist settings, the evidence supported their positive impact on PA, as well as the potential to increase social interaction and community cohesion, both important aspects of healthy cities (Swinburn et al. 1999, Barton and Grant 2006, 2013). Nonetheless, it is also important to explore the level of design implementation and the specific features associated with intended behavior change.
Health behaviors and other outcomes
Despite exhaustive searches for a range of other health outcomes and behaviors, all studies focused on PA as the primary or sole outcome; and the measures used to operationalize it varied. Fourteen studies relied on self-reported PA using established questionnaires (e.g. Neighbourhood Physical Activity Questionnaire or Recent Physical Activity Questionnaire). Some determined if this was MVPA (Rodriguez et al. 2006, Calise et al. 2013, Longo et al. 2015, Panter et al. 2016) or if recommended weekly PA guidelines were met (Rodriguez et al. 2006, Dallat et al. 2014). Only four measured PA with accelerometers or GPS (Ward Thompson et al. 2012, Dill et al. 2014, Miller et al. 2015, Brown et al. 2016) and four observed PA in the study area (Morrison et al. 2004, Fitzhugh et al. 2010, Gustat et al. 2012, Cohen et al. 2014).
Other public health outcomes such as psychological and social health may also be affected by the built environment (Schultz et al. 2016). Several studies included subjective measures of stress, quality of life (Ward Thompson et al. 2012), general health (Branas et al. 2011, Ward Thompson et al. 2012, Droomers et al. 2016) and health-related quality of life (Morrison et al. 2004, Ward Thompson et al. 2012, Longo et al. 2015). Wider determinants of public health (PHE 2016) were affected by built environments and those reported here included social isolation and community cohesion (Zhu et al. 2013).
Assessing built environments
The inclusion criteria required studies to include both built environment restructuring and measured outcomes/behaviors related to public health or behavior change. This requirement resulted in only a small number of studies being included. Of the 23 included, even fewer (5) included any assessment of the environment. Two studies implemented geographic information systems (GIS) technology to create indices of policy compliance with regional planning guidelines (Christian et al. 2013) and walkability (Hooper et al. 2014). Two others used walkability indices, one based on a formula combining land use mix, residential density, sidewalk density, and retail floor area (Longo et al. 2015) and the other on the Walkscore® method (Zhu et al. 2013), which is similar but uses proprietary software to calculate walkability.
Integration with COM-B and TDF
In this section, the summary narrative findings are integrated with the components of the COM-B and domains of the TDF, in order to identify where behavioral science can potentially strengthen the design and evaluation of future built environment restructuring projects. Each included study was mapped onto the TDF domains within each relevant source of behavior change from COM-B (see Table 3). All studies provided physical opportunity (COM-B behavior source) via environmental context/resources (TDF domain). This was to be expected given that change to the physical environment was necessary in order to meet inclusion criterion for the scoping review. In the COM-B model (Michie et al. 2011), there are other sources of behavior most relevant to built environment restructuring. Seven studies included outcomes relevant to social opportunity, all which were related to social influence (TDF domain). For example, a New Urbanist community provided social opportunity through increased resident social interaction (Zhu et al. 2013) and another study reported initiatives to build a ‘cycling culture’ to encourage cycling to work (Goodman et al. 2013). Automatic motivation was evident in five studies, primarily through environment restructuring projects’ impact on perceived safety and stress (TDF domain: emotion) but also via reinforcement with incentives (Goodman et al. 2013). Other COM-B behavior sources were found in seven studies. Scott et al. (2014) reported elderly outdoor gym participants felt their skills (a TDF domain) for engaging in physical activity (COM-B physical capability) were improved by instructor-led sessions and information leaflets on how to use the facilities improved their knowledge (COM-B psychological capability). These influenced reflective motivation through increased confidence (TDF domain: beliefs) and future plans to use the gym (TDF domain: intention). Future intention was included in a study after the introduction of new bicycle infrastructure (Crane et al. 2016) and attitude towards walking/cycling (TDF domain: beliefs) predicted cycle path usage in another (Dill et al. 2014). In summary, although not explicitly integrated into the studies included in this review, it appears behavioral science techniques have been used.
Table 3.
Integration of individual studies with TDF domains by COM-B behaviour source.
| COM-B model behaviour sourcesa associated with environmental restructuring |
Other COM-B model behaviour sourcesa |
|||||
|---|---|---|---|---|---|---|
| Author by built environment restructuring type | Automatic motivationb | Social opportunityb | Physical opportunityb | Psychological capabilityb | Physical capabilityb | Reflective motivationb |
| Active Travel | ||||||
| Brown et al. 2016 | Environmental Context/Resources | |||||
| Buscail et al. 2016 | Environmental Context/Resources | Knowledge | ||||
| Chriqui et al. 2016 | Environmental Context/Resources | |||||
| Crane et al. 2016 | Social Influences | Environmental Context/Resources | Intentions | |||
| Dill et al. 2014 | Environmental Context/Resources | Beliefs | ||||
| Goodman et al. 2013 | Reinforcement | Social Influences | Environmental Context/Resources | Behaviour Regulation; Knowledge | Skills | Goals |
| Miller et al. 2015 | Environmental Context/Resources | |||||
| Morrison et al. 2004 | Social Influences | Environmental Context/Resources | ||||
| Panter et al. 2016 | Environmental Context/Resources | |||||
| Ward Thompson et al. 2012 | Social Influences | Environmental Context/Resources | Beliefs | |||
| Urban Greenways | ||||||
| Dallat et al. 2014 | Environmental Context/Resources | |||||
| Fitzhugh et al. 2010 | Environmental Context/Resources | |||||
| Gustat et al. 2012 | Environmental Context/Resources | |||||
| Longo et al. 2015 | Emotion | Environmental Context/Resources | Beliefs | |||
| Urban Green Space | ||||||
| Branas et al. 2011 | Emotion | Environmental Context/Resources | ||||
| Cohen et al. 2014 | Emotion | Social Influences | Environmental Context/Resources | |||
| Droomers et al. 2016 | Environmental Context/Resources | |||||
| Scott et al. 2014 | Social Influences | Environmental Context/Resources | Knowledge | Skills | Beliefs; Intentions | |
| New Urbanism | ||||||
| Calise et al. 2013 | Environmental Context/Resources | |||||
| Christian et al. 2013 | Emotion | Environmental Context/Resources | ||||
| Hooper et al. 2014 | Environmental Context/Resources | |||||
| Rodriguez et al. 2006 | Environmental Context/Resources | |||||
| Zhu et al. 2013 | Social Influences | Environmental Context/Resources | ||||
aDefinitions of each COM-B behaviour source were obtained from http://www.behaviourchangewheel.com retrieved 21 July 2017.
b Each behaviour change source can include a range of TDF domains (Cane et al. 2012). For example, automatic motivation as a behaviour change source in the COM-B model includes social/professional identity, optimism, reinforcement, and emotion TDF domains.
Each TDF domain may then include up to 11 different concepts, therefore only the higher order TDF domains were mapped here.
Where other behaviour change sources of the COM-B model were observed, they were also included.
Discussion
The aim of this scoping review was to determine whether two common approaches for public health improvement, built environment restructuring and behavioral science, could or should be integrated. Our findings indicated built environment researchers were already using a number of behavioral science outcomes consistent with the COM-B and TDF, but not necessarily intentionally. The obvious reason for this was the projects reviewed here were developed prior to the initial publication of either COM-B or TDF. However, this cannot explain the lack of reports of the theories underpinning these built environment interventions. With the exception of one study based on the Theory of Planned Behavior (Crane et al. 2016), there was no evidence that behavioral science was intentionally integrated into project design; and only four other studies mentioned any theoretical framework. Three reports (Rodriguez et al. 2006, Ward Thompson et al. 2012, Zhu et al. 2013) were based on socio-ecological theory (McLeroy et al. 1988) and one on Broken Windows Theory (Branas et al. 2011). While we acknowledge reporting conventions vary across disciplines and, therefore, this information may not be required, we reiterate the need for theory development recently raised by others (Hassen and Kaufman 2016); and go further to suggest that the theory underpinning design should be explicitly communicated in all published accounts.
We would also recommend that built environment restructuring projects have health outcomes integrated from the initial design stage and based on clearly specified theoretical framework(s). A clear challenge in this respect is the need to include theories that bridge individual behavior through to macro-environment influences (Tate et al. 2016). The Health Map (Barton and Grant 2006, 2013) provides a useful framework to this aim but does not provide theoretical linkages. Based on the evidence presented in this review, we propose behavioral science frameworks such as the COM-B (Michie et al. 2011, 2014) and TDF (Cane et al. 2012) are useful at the individual-level; but that future cross-disciplinary collaboration is needed to synthesize theoretical approaches targeting different levels of influence into a multi-level, integrated theoretical model.
From a behavioral science perspective, built environment restructuring provides the physical opportunity for behavior change (Michie et al. 2011) through environmental context and resources (Cane et al. 2012). This review clearly indicated these physical opportunities typically translated into improved physical activity; but due to variability in methods used to measure physical activity, comparison across interventions was not possible. Reliance on self-report data is also particularly problematic in the behavioral science context, given self-reports often over-estimate PA (Troiano et al. 2014).
Being ‘healthy’ is based on multiple factors and built environment research should reflect a wider breadth of health outcomes and behaviors. In our review, we found evidence for the positive impact on stress, general/health-related quality of life and social isolation. Subjective environmental perceptions and attitudes can influence the use of urban settings, particularly green resources (Flowers et al. 2016) and should be reported in conjunction with physical activity. Other sources of behavior such as motivation, social opportunity, and beliefs about physical and psychological capabilities should also be acknowledged as important drivers to the health behavior these projects might intend to target.
Conversely, little research has focused on potential negative consequences resulting from built environment restructuring. Some evidence was presented indicating conflicts between user groups occur (Crane et al. 2016) and nuisances (e.g. dog fouling, groups of youths gathering) can arise (Ward Thompson et al. 2012). These findings reiterate the range of potential negative health and wellbeing outcomes associated with urban design factors such as noise, poor design quality, crowding and density, which have been summarized by other authors (Cooper 2014). Further research exploring these negative consequences has also been suggested by the WHO (2017); and, despite our focus in this review on measurable outcomes, we also argue for a balance between quantitative studies gathering self-report and observational behavior data with qualitative research exploring barriers and facilitators of healthy behavior in built environments.
In regards to the assessment of built environment characteristics, very few studies did so and there were potential limitations to the methods implemented. Walkscore® (Zhu et al. 2013), as a measure of walkability, only measures distance; however, multiple factors impact people’s propensity to walk. Other methods may also be potentially problematic. For example, a measure of land use mix may show as ‘mixed use’ based on a residential area with a drive-through restaurant and commercial warehousing but it will not necessarily support walking. The lack of consistency in measures of the built environment and the inability of them to be nuanced enough to be helpful is a criticism that has been made many times (Townshend and Lake 2009). There are also substantive problems with regard to ‘assessing’ the quality of green space within the urban context. GreenSpace Scotland (2008) defines quality greenspace as greenspace which is ‘fit for purpose’ – meaning it is in the right place, readily accessible, safe, inclusive, welcoming, well maintained, well managed and performing an identified function. Combining these complex variables would enhance usage. Therefore, it is essential to include measures of quality and quantity whilst attempting to avoid unwieldy research designs.
Finally, we suggest an approach to incorporate many of these recommendations. Built environment intervention project teams should agree the relevant theoretical frameworks from their respective disciplines in the initial planning stage. The manner by which these frameworks inform study design should then be explicitly summarised in a published study protocol. Study protocols are common in the public health, with examples of some that bridge with urban design (e.g. Chapman et al. 2014) and include how theory underpinned design (Razani et al. 2016). Published protocols should then be referred to in all subsequent published accounts, thus avoiding the need to fully summarise this information further. During the design stage, a variety of outcomes should be defined covering the breadth of both built environment and health evaluation needs. This could include assessing built environment characteristics and public perceptions of these settings, measuring health outcomes through objective means such as GPS tracking of physical activity, and capturing subjective health and wellbeing outcomes using both internationally-recognised measures (e.g. health-related quality of life, social isolation) and qualitative exploration of the users lived experience. The intention of our suggested approach is not to introduce unnecessary or unwieldy theoretical complexity to projects. Rather, our intention is to develop the ability to compare the effectiveness of interventions across settings or types of built environment interventions, as well as with other health behaviour change initiatives targeting the same health outcomes. The recommended approach also facilitates linkages between published accounts, each focused on a subset of discipline-specific results, to provide a full picture of both the positive and negative consequences of built environment interventions.
Study strengths and limitations
The primary strength of this scoping review was its attempt to integrate two disparate, yet common approaches to improving public health and health behaviors. Recent reports reiterate the potential for built environment and behavioral science approaches to facilitate our understanding of the varied, multi-level influences on health (Hollands et al. 2013, Arnott et al. 2014, Roberts et al. 2016); and our integration of the summary findings with two established behavioral science frameworks, the COM-B and TDF, further support the potential for synergy between them. It is important to acknowledge that scoping reviews are not without their limitations. As an evidence review method, the aim is to summarize evidence in a time-limited context. This required a decision to focus only on peer-reviewed studies, which meant potentially relevant sources such as government reports were absent. This is potentially problematic in two ways. First, design and evaluation phases of these types of interventions are not necessarily implemented by the same stakeholders. This may mean those who conduct these evaluations are inadvertently unaware of the theories underpinning original intervention design. The sole use of peer-reviewed published accounts and exclusion of grey literature such as government agency reports also means that potentially valuable lessons from implemented interventions were not included. Yet, we believe these concerns reinforce our recommendation that published protocols for interventions should become best practice. Even if later evaluations were only reported in the grey literature, the published protocols would facilitate compiling the relevant evidence for a specific project as the grey literature can cite the protocol. Overall, we believe the search parameters implemented in 12 academic databases across three disciplines minimised this limitation and provided the most thorough results possible.
Another limitation of this review was the decision to focus on studies only reporting measurable health outcomes and behaviors. In doing so, it was likely that informative studies reporting only subjective outcomes relevant to behavior change were excluded. Future reviews could focus on a single or limited number of similar built environment restructuring interventions and synthesise the range of behavioral science-relevant outcomes across published reports.
As with other health-related outcomes, it is also possible that detailed accounts of environment evaluations were presented in other published studies that did not meet the inclusion criterion for this scoping review. For example, studies would have been excluded because they focused on resident perceptions of the lived environment (but included no behavior) or were solely focused on evaluation of the design features. Therefore, we believe it is important for authors to either provide some account of this information in all studies or at the very least refer readers to other published studies in order to understand the full impact of these design initiatives.
Additionally, our initial search strategy was somewhat constrained by the requirements of the funder in respect of their wider remit to inform its future research priorities. As a result, the search was focused on studies from locations similar to the UK but did include a diverse number of countries. The funder, however, did not contribute to the current scoping review and encouraged us to disseminate any more specific, independent findings that resulted from the wider review.
Conclusion
The capacity for built environment restructuring to positively impact public health was clear in the studies reported in this scoping review; however the pathways for this impact remain unclear. In part, this is because existing evidence is too focused on physical health and there is a need to look at these pathways linking the individual, the environment, and their health, including mental health, more holistically. Nonetheless, good evidence is emerging that built environment interventions can facilitate improved public health, that these initiatives may be strengthened by integration with behavioral science.
Biographies
Dr. Stephanie Wilkie is an Environmental Psychologist with interests in the influence of urban green space and built environments on wellbeing, as well as expertise in research methods and statistics including large-scale studies for the US government. She is a Chartered Psychologists and associate member of FUSE, the Centre for Translational Research in Public Health.
Tim Townshend is Professor of Urban Design for Health at the School of Architecture, Planning and Landscape, Newcastle University, UK. His international research profile is focused on the relationship between built environments and human health/wellbeing. Tim has been part of multidisciplinary research projects exploring obesogenic environments, the benefits of urban parks, and mobility and ageing. His work is practice relevant as evidenced by his involvement with the ESRC ‘Reuniting Planning and Health’ seminar series, uniting practitioners and academics from health and planning disciplines. In 2016, his work on obesogenic environments was recognised by the Royal Society for Public Health, UK.
Dr. Emine Thompson is an independent researcher (previously at Northumbria University). Trained as a landscape architect, she has established wide-ranging expertise in areas related to digital urbanism, in particular to smart and future cities, virtual city modelling, city information modelling, virtual reality and augmented reality.
Jonathan Ling is a Professor of Public Health with interests across the breadth of public health and health sciences. A Fellow of the Royal Society of Public Health, the Higher Education Academy and a Chartered Psychologist, he is also a member of the NIHR Health Services and Delivery Research Specialty Group for the North East and North Cumbria, and the Regional Advisory Panel for the NIHR Research for Patient Benefit. Jonathan has been awarded national funding from the NIHR, Public Health England and the ESRC, as well as the NHS and other local organisations.
Funding Statement
This work was supported by the Public Health England Behavioural Insights Team (PHE BIT). Professor Jonathan Ling is a partially funded staff member of Fuse, the Centre for Translational Research in Public Health, a UKCRC Public Health Research Centre of Excellence. This article presents findings from independent research funded by the NIHR School for Public Health Research (SPHR). The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. Fuse is a UK Clinical Research Collaboration (UKCRC) Public Health Research Centre of Excellence. Funding for Fuse from the British Heart Foundation, Cancer Research UK, Economic and Social Research Council, Medical Research Council, the National Institute for Health Research, under the auspices of the UKCRC, is gratefully acknowledged.
Disclosure statement
No potential conflict of interest was reported by the authors.
Supplementary material
Supplementary data for this article can be accessed here.
References
- Abou-Setta A.M., et al, 2016. Methods for developing evidence reviews in short periods of time: a scoping review. PLOS One, 11 (12), e0165903. doi: 10.1371/journal.pone.0165903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Algert S., et al, 2016. Community and home gardens increase vegetable intake and food security of residents in San Jose, California. California Agriculture, 70 (2), 77–82. doi: 10.3733/ca.v070n02p77 [DOI] [Google Scholar]
- Arksey H. and O’Malley L., 2005. Scoping studies: towards a methodological framework. International Journal of Social Research Methodology, 8 (1), 19–32. doi: 10.1080/1364557032000119616 [DOI] [Google Scholar]
- Arnott B., et al, 2014. Efficacy of behavioural interventions for transport behaviour change: systematic review, meta-analysis and intervention coding. International Journal of Behavioural Nutrition and Physical Activity, 11, 133. doi: 10.1186/s12966-014-0133-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Backholer K., et al, 2014. A framework for evaluating the impact of obesity prevention strategies on socioeconomic inequalities in weight. American Journal of Public Health, 104 (10), e43–e50. doi: 10.2105/AJPH.2014.302066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barton H. and Grant M., 2006. A health map for the local human habitat. The Journal for the Royal Society for the Promotion of Health, 126 (6), 252–253. [DOI] [PubMed] [Google Scholar]
- Barton H. and Grant M., 2013. Urban planning for healthy cities. Journal of Urban Health, 90 (1), 129–141. doi: 10.1007/s11524-011-9649-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branas C., et al, 2011. A difference-in-differences analysis of health, safety, and greening vacant urban space. American Journal of Epidemiology, 174 (11), 1296–1306. doi: 10.1093/aje/kwr273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown B., et al, 2016. A Complete street intervention for walking to transit, nontransit walking, and bicycling: a quasi-experimental demonstration of increased use. Journal of Physical Activity and Health, 13 (11), 1210–1219. doi: 10.1123/jpah.2016-0066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buscail C., et al, 2016. Promoting physical activity in a low-income neighborhood of the Paris suburb of Saint-Denis: effects of a community-based intervention to increase physical activity. BMC Public Health, 16, 667. doi: 10.1186/s12889-016-3360-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calise T., et al, 2013. Do neighborhoods make people active, or do people make active neighborhoods? Evidence from a planned community in Austin, Texas. Preventing Chronic Disease, 10, E102. doi: 10.5888/pcd10.130016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cane J., O’Connor D., and Michie S., 2012. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implementation Science, 7, 1–17. doi: 10.1186/1748-5908-7-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmona M., et al, 2010. Public Places, Urban Spaces: the Dimensions of Urban Design. Abingdon: Routledge. [Google Scholar]
- Center for Active Design , 2010. Urban design checklist. Available from: https://centerforactivedesign.org/guidelines/[Accessed 22May 2017].
- Chapman R., et al, 2014. Increasing active travel: aims, methods and baseline measures of a quasi-experimental study. BMC Public Health, 14, 935. doi: 10.1186/1471-2458-14-935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chriqui J., et al, 2016. Communities on the move: pedestrian-oriented zoning as a facilitator of adult active travel to work in the United States. Frontiers in Public Health, 4, 71. doi: 10.3389/fpubh.2016.00071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christian H., et al, 2013. A new urban planning code’s impact on walking: the residential environments project. American Journal of Public Health, 103 (7), 1219–1228. doi: 10.2105/AJPH.2013.301230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen D.A., et al, 2014. The potential for pocket parks to increase physical activity. American Journal of Health Promotion, 28, S19–S26. doi: 10.4278/ajhp.130430-QUAN-213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colquhoun H.L., et al, 2014. Scoping reviews: time for clarity in definition, methods, and reporting. Journal of Clinical Epidemiology, 67, 1291–1294. doi: 10.1016/j.jclinepi.2014.03.013 [DOI] [PubMed] [Google Scholar]
- Cooper R., 2014. Wellbeing and the environment: an overview In: Cooper R., Burton E., and Cooper C., eds. Wellbeing: a complete reference guide (volume II): wellbeing and the environment. Chichester: Wiley Blackwell, 1–19. [Google Scholar]
- Craig P., et al, 2012. Using natural experiments to evaluate population health interventions: new MRC guidance. Journal of Epidemiology and Community Health, 66 (12), 1182–1186. doi: 10.1136/jech-2011-200375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crane M., et al, 2016. Neighbourhood expectations and engagement with new cycling infrastructure in Sydney, Australia: findings from a mixed method before-and-after study. Journal of Transport and Health, 3 (1), 48–60. doi: 10.1016/j.jth.2015.10.003 [DOI] [Google Scholar]
- Dallat M., et al, 2014. Urban greenways have the potential to increase physical activity levels cost-effectively. European Journal of Public Health, 24 (2), 190–195. doi: 10.1093/eurpub/ckt035 [DOI] [PubMed] [Google Scholar]
- Davis R., et al, 2015. Theories of behavior and behaviour change across the social and behavioural sciences: a Scoping Review. Health Psychology Review, 9 (3), 323–344. doi: 10.1080/17437199.2014.941722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Day K., 2003. New urbanism and the challenges of designing for diversity. Journal of Planning Education and research, 23 (1), 83–95. doi: 10.1177/0739456x03255424 [DOI] [Google Scholar]
- Department of Health , 2015. Government response to the consultation Refreshing the Public Health Outcomes Framework (2015). Available from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/520455/PHOF_cons_response.pdf[Accessed 28June 2016].
- Dill J., et al, 2014. Bicycle boulevards and changes in physical activity and active transportation: findings from a natural experiment. Preventive Medicine, 69, S74–S78. doi: 10.1016/j.ypmed.2014.10.006 [DOI] [PubMed] [Google Scholar]
- Droomers M., et al, 2016. The impact of intervening in green space in Dutch deprived neighbourhoods on physical activity and general health: results from the quasi-experimental URBAN40 study. Journal of Epidemiology and Community Health, 70, 147–154. doi: 10.1136/jech-2014-205210 [DOI] [PubMed] [Google Scholar]
- Fitzhugh E.C., Bassett D.R., and Evans M.F., 2010. Urban trails and physical activity: a natural experiment. American Journal of Preventive Medicine, 39 (3), 259–262. doi: 10.1016/j.amepre.2010.05.010 [DOI] [PubMed] [Google Scholar]
- Flowers E.P., et al, 2016. A cross-sectional study examining predictors of visit frequency to local green space and the impact this has on physical activity levels. BMC Public Health, 16, 420. doi: 10.1186/s12889-016-3050-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flynn B.C., 1996. Healthy cities: toward worldwide health promotion. Annual Review of Public Health, 17, 299–309. doi: 10.1146/annurev.pu.17.050196.001503 [DOI] [PubMed] [Google Scholar]
- Garritty C., et al, 2016. Cochrane rapid reviews methods group to play a leading role in guiding the production of informed, high-quality, timely research evidence syntheses. Systematic Reviews, 5, 184. doi: 10.1186/s13643-016-0360-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanz K. and Bishop D., 2010. The role of behavioral science theory in development and implementation of public health intervetions. Annual Review of Public Health, 31, 399–418. doi: 10.1146/annurev.publhealth.012809.103604 [DOI] [PubMed] [Google Scholar]
- Goodman A., et al, 2013. Effectiveness and equity impacts of town-wide cycling initiatives in England: a longitudinal, controlled natural experimental study. Social Science and Medicine, 97, 228–237. doi: 10.1016/j.socscimed.2013.08.030 [DOI] [PubMed] [Google Scholar]
- GreenSpace Scotland , 2008. Greenspace Quality-A guide to assessment, planning and strategic development. Available from: http://www.ukmaburbanforum.co.uk/documents/other/qualityguide.pdf[Accessed 16October 2017].
- Gustat J., et al, 2012. Effect of changes to the neighborhood built environment on physical activity in a low-income African American neighborhood. Preventing Chronic Disease, 9, E57. [PMC free article] [PubMed] [Google Scholar]
- Hassen N. and Kaufman P., 2016. Examining the role of urban street design in enhancing community engagement: a literature review. Health and Place, 41, 119–132. doi: 10.1016/j.healthplace.2016.08.005 [DOI] [PubMed] [Google Scholar]
- Hollands G.J., et al, 2013. Altering micro-environments to change population health behaviour: towards an evidence base for choice architecture interventions. BMC Public Health, 13, 1218–1223. doi: 10.1186/1471-2458-13-1218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooper P., Giles-Corti B., and Knuiman M., 2014. Evaluating the implementation and active living impacts of a state government planning policy designed to create walkable neighborhoods in Perth, Western Australia. American Journal of Health Promotion, 28, S5–S18. doi: 10.4278/ajhp.130503-QUAN-226 [DOI] [PubMed] [Google Scholar]
- Irvine K.N., et al, 2013. Understanding urban green space as a health resource: a qualitative comparison of visit motivation and derived effects among park users in Sheffield, UK. International Journal of Environmental Research and Public Health, 10 (1), 417–442. doi: 10.3390/ijerph10010417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khangura S., et al, 2012. Evidence summaries: the evolution of a rapid review approach. Systematic Reviews, 1, 10. doi: 10.1186/2046-4053-1-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lake A. and Townshend T., 2006. Obesogenic environments: exploring the built and food environments. The Journal of the Royal Society for the Promotion of Health, 126, 262–267. [DOI] [PubMed] [Google Scholar]
- Longo A., et al, 2015. Demand response to improved walking infrastructure: a study into the economics of walking and health behaviour change. Social Science and Medicine, 143, 107–116. doi: 10.1016/j.socscimed.2015.08.033 [DOI] [PubMed] [Google Scholar]
- Mackenbach J., et al, 2014. Obesogenic environments: a systematic review of the association between the physical environment and adult weight status, the SPOTLIGHT project. BMC Public Health, 14, 233. doi: 10.1186/1471-2458-14-233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matjasko J., et al, 2016. Applying behavioral economics to public health policy: illustrative examples and promising directions. American Journal of Preventive Medicine, 50 (5 Supp 1), S13–S19. doi: 10.1016/j.amepre.2016.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEachan R., et al, 2011. Prospective prediction of health-related behaviours with the theory of planned behaviour: a meta-analysis. Health Psychology Review, 5 (2), 97–144. doi: 10.1080/17437199.2010.521684 [DOI] [Google Scholar]
- McLeroy K.R., et al, 1988. An ecological perspective on health promotion programs. Health Education and Behavior, 15, 351–377. [DOI] [PubMed] [Google Scholar]
- Michie S., et al, 2013. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Annals of Behavioral Medicine, 46 (1), 81–95. doi: 10.1007/s12160-013-9486-6 [DOI] [PubMed] [Google Scholar]
- Michie S., Atkins L., and West R., 2014. The Behaviour Change Wheel: A Guide to Designing Interventions. 1st ed. London: Silverback Publishing. [Google Scholar]
- Michie S., van Stralen M., and West R., 2011. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implementation Science, 6, 42. doi: 10.1186/1748-5908-6-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller H., et al, 2015. Public transit generates new physical activity: evidence from individual GPS and accelerometer data before and after light rail construction in a neighborhood of Salt Lake City, Utah, USA. Health and Place, 36, 8–17. doi: 10.1016/j.healthplace.2015.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison D.S., Thomson H., and Petticrew M., 2004. Evaluation of the health effects of a neighbourhood traffic calming scheme. Journal of Epidemiology and Community Health, 58 (10), 837–840. doi: 10.1136/jech.2003.017509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Müeller-Riemenschneider F., et al, 2013. Neighborhood walkability and cardiometabolic risk factors in Australian adults: an observational study. BMC Public Health, 13, 755. doi: 10.1186/1471-2458-13-755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panter J., et al, 2016. Impact of new transport infrastructure on walking, cycling, and physical activity. American Journal of Preventive Medicine, 50 (2), e45–e53. doi: 10.1016/j.amepre.2015.09.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perdue W., Stone L., and Gostin L., 2003. The Built Environment and its relationship to the public’s health: the legal framework. American Journal of Public Health, 93 (9), 1390–1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters M., et al, 2015. Guidance for conducting systematic scoping reviews. International Journal of Evidence-based Healthcare, 13 (3), 141–146. doi: 10.1097/XEB.0000000000000050 [DOI] [PubMed] [Google Scholar]
- Policy Connect , 2017. People and place: design of the built environment and behaviour. London: Policy Connect. [Google Scholar]
- Public Health England , 2016. Active Transport. Available from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/523460/Working_Together_to_Promote_Active_Travel_A_briefing_for_local_authorities.pdf[Accessed 22May 2017].
- Quigley M., 2013. Nudging for health: on public policy and designing choice architecture. Medical Law Review, 21 (4), 588–621. doi: 10.1093/medlaw/fwt022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Razani N., et al, 2016. Design and evaluation of a park prescription program for stress reduction and health promotion in low-income families: the Stay Healthy in Nature Everyday (SHINE) study protocol. Contemporary Clinical Trials, 51, 8–14. doi: 10.1016/j.cct.2016.09.007 [DOI] [PubMed] [Google Scholar]
- Roberts H., et al, 2016. Identifying Effective Behavior Change Techniques in Built Environment Interventions to Increase Use of Green Space: a Systematic Review. Environment and Behavior, 50 (1), 28–55. doi: 10.1177/0013916516681391 [DOI] [Google Scholar]
- Rodriguez D.A., et al, 2006. Can new urbanism encourage physical activity? Comparing a new urbanist neighborhood with conventional suburbs. Journal of the American Planning Association, 72 (1), 43–54. doi: 10.1080/01944360608976723 [DOI] [Google Scholar]
- Sallis E., et al, 2016. Physical activity in relation to urban environments in 14 cities worldwide: a cross-sectional study. Lancet, 387 (10034), 2207–2217. doi: 10.1016/S0140-6736(15)01284-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallis J., et al, 2006. An ecological approach to creating active living communities. Annual Review of Public Health, 27, 297–322. doi: 10.1146/annurev.publhealth.27.021405.102100 [DOI] [PubMed] [Google Scholar]
- Schultz C., et al, 2016. Potential measures for linking park and trail systems to public health. Journal of Park and Recreation Administration, 34, 4–23. doi: 10.18666/JPRA-2016-V34-I1-7143 [DOI] [Google Scholar]
- Scott A., et al, 2014. Design and promotion of an outdoor gym for older adults: a collaborative project. Health Promotion Journal of Australia: Official Journal of Australian Association of Health Promotion Professionals, 25 (3), 212–214. doi: 10.1071/HE14037 [DOI] [PubMed] [Google Scholar]
- Sharma A., 2015. Urban greenways: operationalizing design syntax and integrating mathematics and science in design. Frontiers of Architectural Research, 4, 24–34. doi: 10.1016/j.foar.2014.11.002 [DOI] [Google Scholar]
- Song Q., et al, 2017. The global contribution of outdoor air pollution to the incidence, prevalence, mortality, and hospital admission for chronic obstructive pulmonary disease: a systematic review and meta-analysis. International Journal of Environmental Research and Public Health, 11 (11), 11822–11832. doi: 10.3390/ijerph111111822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srinivasan S., O’Fallon L., and Dearry A., 2003. Creating healthy communities, healthy homes, healthy people: initiating a research agenda on the built environment and public health. American Journal of Public Health, 93, 1446–1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swinburn B., Egger G., and Raza F., 1999. Dissecting obesogenic environments: the development and application of a framework for identifying and prioritizing environmental interventions for obesity. Preventive Medicine, 29 (6 Pt 1), 563–570. doi: 10.1006/pmed.1999.0585 [DOI] [PubMed] [Google Scholar]
- Tate D., et al, 2016. Deconstructing interventions: approaches to studying behavior change techniques across obesity interventions. Translational Behavioral Medicine, 6, 236–243. doi: 10.1007/s13142-015-0369-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thaler R. and Sunstein C., 2008. Nudge: improving decisions about health, wealth, and happiness. New Haven: Yale University Press. [Google Scholar]
- Townshend T., 2017. Toxic high streets. Journal of Urban Design, 22, 167–186. doi: 10.1080/13574809.2015.1106916 [DOI] [Google Scholar]
- Townshend T. and Lake A., 2009. Obesogenic urban form: theory, policy and practice. Health & Place, 15, 909–916. doi: 10.1016/j.healthplace.2008.12.002 [DOI] [PubMed] [Google Scholar]
- Tricco A., et al, 2016. A scoping review on the conduct and reporting of scoping reviews. BMC Medical Research Methodology, 16, 15. doi: 10.1186/s12874-016-0116-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tricco A.C., et al, 2015. A scoping review of rapid review methods. BMC Medicine, 13, 224. doi: 10.1186/s12916-015-0465-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troiano R., et al, 2014. Evolution of accelerometer methods for physical activity research. British Journal of Sports Medicine, 48 (13), 1019–1023. doi: 10.1136/bjsports-2014-093546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsouros A., 1991. World Health Organization Health Cities Project: a project becomes a movement. Review of progress 1987 to 1990. Available from: http://www.euro.who.int/en/health-topics/environment-and-health/urban-health/activities/healthy-cities/who-european-healthy-cities-network/phases-ivi-of-the-who-european-healthy-cities-network/phases-i-and-ii/who-healthy-cities-project-a-project-becomes-a-movement[Accessed 1April 2017].
- Völker S. and Kistermann T., 2015. Developing the urban blue: comparative health responses to blue and green urban open spaces in Germany. Health & Place, 35, 196–205. doi: 10.1016/j.healthplace.2014.10.015 [DOI] [PubMed] [Google Scholar]
- Ward Thompson C., et al, 2012. Do changes to the local street environment alter behaviour and quality of life of older adults? The ‘DIY Streets’ intervention. British Journal of Sports Medicine, 48, 1059–1065. doi: 10.1136/bjsports-2012-091718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization , 2010. Global Recommendations on Physical Activity for Health. Available from: http://apps.who.int/iris/bitstream/handle/10665/44399/9789241599979_eng.pdf?sequence=1[Accessed 26November 2017]. [PubMed]
- World Health Organization , 2015. 100 Core Health Indicators. Available from: http://apps.who.int/iris/bitstream/10665/173589/1/WHO_HIS_HSI_2015.3_eng.pdf?ua=1[Accessed 9August 2017].
- World Health Organization , 2016. Global report on urban health: equitable healthier cities for sustainable development. Available from: http://www.who.int/gender-equity-rights/knowledge/global-report-on-urban-health/en/[Accessed 3August 2017].
- World Health Organization , 2017. Urban green space interventions and health: a review of impacts and effectiveness. Available from: http://www.euro.who.int/en/health-topics/environment-and-health/urban-health/publications/2017/urban-green-space-interventions-and-health-a-review-of-impacts-and-effectiveness.-full-report-2017[Accessed 1June 2017].
- Yitshak-Sade M., Kloog I., and Novack V., 2017. Do air pollution and neighbourhood greenness exposures improve the predicted cardiovascular risk? Environment International, 107, 147–153. doi: 10.1016/j.envint.2017.07.011 [DOI] [PubMed] [Google Scholar]
- Zhu X., et al, 2013. A retrospective study on changes in residents’ physical activities, social interactions, and neighbourhood cohesion after moving to a walkable community. Preventative Medicine, 69 (Supp 1), 593–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


