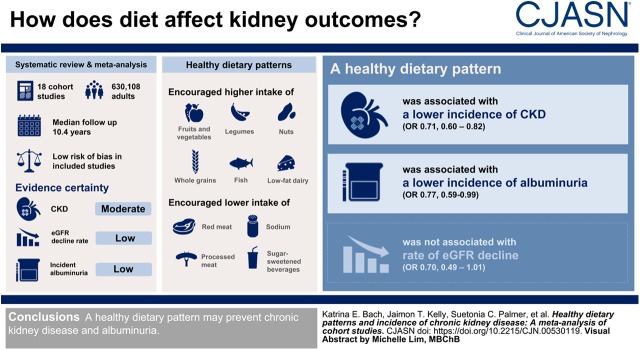
Visual Abstract
Keywords: Diet, dietary patterns, Mediterranean, DASH, chronic kidney disease, systematic review, adult, child, human, vegetables, glomerular filtration rate, fruit, albuminuria, whole grains, nuts, incidence, sweetening agents, fabaceae, sodium, sugars, prospective studies, retrospective studies, follow-up studies, chronic renal insufficiency, diet, fat-restricted
Abstract
Background and objectives
Whether a healthy dietary pattern may prevent the incidence of developing CKD is unknown. This study evaluated the associations between dietary patterns and the incidence of CKD in adults and children.
Design, setting, participants, & measurements
This systematic review and meta-analysis identified potential studies through a systematic search of MEDLINE, Embase and references from eligible studies from database inception to February 2019. Eligible studies were prospective and retrospective cohort studies including adults and children without CKD, where the primary exposure was dietary patterns. To be eligible, studies had to report on the primary outcome, incidence of CKD (eGFR<60 ml/min per 1.73 m2). Two authors independently extracted data, assessed risk of bias and evidence certainty using the Newcastle–Ottawa scale and GRADE.
Results
Eighteen prospective cohort studies involving 630,108 adults (no children) with a mean follow-up of 10.4±7.4 years were eligible for analysis. Included studies had an overall low risk of bias. The evidence certainty was moderate for CKD incidence and low for eGFR decline (percentage drop from baseline or reduced by at least 3 ml/min per 1.73 m2 per year) and incident albuminuria. Healthy dietary patterns typically encouraged higher intakes of vegetables, fruit, legumes, nuts, whole grains, fish and low-fat dairy, and lower intakes of red and processed meats, sodium, and sugar-sweetened beverages. A healthy dietary pattern was associated with a lower incidence of CKD (odds ratio [OR] 0.70 (95% confidence interval [95% CI], 0.60 to 0.82); I2=51%; eight studies), and incidence of albuminuria (OR 0.77, [95% CI, 0.59 to 0.99]; I2=37%); four studies). There appeared to be no significant association between healthy dietary patterns and eGFR decline (OR 0.70 [95% CI, 0.49 to 1.01], I2=49%; four studies).
Conclusions
A healthy dietary pattern may prevent CKD and albuminuria.
Introduction
CKD is a growing public health concern because of the increasing prevalence worldwide (1), substantially increased risk of death from cardiovascular disease (2), and costs from treating ESKD. Dietary modification is considered one of the key modifiable risk factors for the progression of CKD (3). However, whether a healthy diet is protective against the incidence of CKD is not fully understood (4). The potential to prevent the incidence of CKD may assist in reducing the significant individual burden of disease, with over 497 million adults worldwide with CKD stages 1–5 (5).
Dietary patterns are defined as the consumption of foods that reflect habitual dietary intake. For this reason, a dietary pattern can be classified as “healthy” or “unhealthy.” Examples of healthy dietary patterns include approaches like the Mediterranean diet, the Dietary Approach to Stop Hypertension (DASH), vegetarian diets, dietary guidelines, and any approach to dietary intake that focuses on the overall pattern of eating as opposed to approaches targeting individual (or multiple) nutrients (6). Although dietary patterns can differ in their advocated servings of food and beverages, a healthy dietary pattern share similar characteristics, typically involving a higher consumption of whole grains, fruits, vegetables, and healthy fats and the consequential intake of fiber, vitamin C, vitamin E, and carotenoids, and lower consumption of saturated fats, salt, and processed foods, and lower dietary acid load. As these healthy dietary patterns share similar characteristics, it is reasonable to assess dietary patterns collectively, recognizing the importance of the synergy of food groups and nutrients working concurrently for health outcomes. The associations of dietary patterns on health outcomes, including cardiovascular disease, have been linked to reduced inflammation from higher consumption of whole grains (7), reduced oxidative stress through increased consumption of fruits and vegetables (8), decreased circulating concentrations of inflammatory markers through a higher consumption of unsaturated fats including nuts and seeds (9), and a reduced dietary acid load associated with CKD progression (10). In contrast, examples of unhealthy dietary patterns include Western diets and high fat and meat diets (11). It is thought that diets high in refined starches, saturated fats, trans-fatty acids, and sodium, and lower in whole grains, fruit, vegetables, omega-3 fatty acids, and fiber may heighten the inflammatory response (12). As elevations in inflammatory markers have been suggested as a biomarker for the incidence of CKD (13), a dietary approach which lowers inflammatory markers and dietary acid load may be important for reducing the incidence of CKD.
Observational evidence supports the association between healthy dietary patterns and the primary prevention of major health conditions, including type 2 diabetes (14), cardiovascular disease, hypertension, and metabolic syndrome (15); however, it is unclear whether a healthy dietary pattern may prevent CKD. Therefore, the aim of this systematic review was to evaluate the association between healthy dietary patterns and the incidence of CKD and other kidney outcomes in adults and children.
Materials and Methods
Data Sources and Searches
This systematic review and meta-analysis was conducted according to the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) checklist for observational studies (16) and was prospectively registered in the International Prospective Register of Systematic Reviews (PROSPERO; identifier CRD42017080881). MEDLINE and Embase were searched (from database inception to February 2019) without date or language restriction. Search strategies were developed by the research team with assistance from an information specialist (Supplemental Table 1). Two investigators (K.E.B. and J.T.K.) manually searched the reference lists of eligible studies, clinical practice guidelines, reviews, and other relevant studies. All citations were uploaded into an electronic reference management system. Non-English papers were translated by a native speaker of the language, and where this was not possible, these papers were electronically translated using Google Translate before assessment and data extraction.
Study Selection
Two investigators independently reviewed the studies for inclusion. The first round of study selection involved screening of title and abstracts conducted by at least two investigators (K.E.B. and J.T.K.). Potentially eligible studies were reviewed in full text primarily by one investigator (K.E.B.) and checked for accuracy by a second reviewer (K.L.C.). Methodological queries regarding study inclusion were discussed among two investigators (K.E.B. and J.T.K.). Discussion with a third investigator (K.L.C.) was used to achieve consensus.
Studies with participants without established CKD (eGFR<60 ml/min2) at baseline were eligible (17). Studies were eligible if they reported a subgroup of the studied population with data specifically relating to participants without evidence of CKD. We included prospective and retrospective longitudinal cohort studies in which participants were grouped according to exposure to a healthy dietary pattern. A healthy dietary pattern was defined as the overall habitual dietary intake of individuals on the basis of the consumption of whole foods, of more than one food group, and therefore each study had to report a dietary pattern exposure that encompassed multiple food and beverage groups. We excluded studies if they reported associations of isolated food groups or nutrients. Studies were eligible if they reported the association between healthy dietary patterns and at least one of the following kidney outcomes: (1) incidence of CKD, (2) ESKD, (3) eGFR decline, (4) progression of albuminuria, (5) eGFR or creatinine clearance at end of study follow-up, (6) serum creatinine, or (7) AKI. Studies had to report on at least one kidney outcome to be included in the review.
Data Extraction and Quality Assessment
Two authors (K.E.B. and S.K.) independently extracted data from studies using standardized data extraction forms. The same two authors applied the Newcastle–Ottawa Quality Assessment Scale (18) to assess the methodological quality of the included studies. Three domains were evaluated: selection (or representativeness) of cohorts, comparability of cohorts (because of design or analysis), and outcomes (assessment and follow-up). Included studies were rated as low, unclear, or high risk of bias for each criterion and then subsequently assigned an overall score. For each kidney outcome, confidence in the evidence (risk of bias, consistency, directness, and precision) was assessed using the Grading of Recommendations Assessment, Development and Evaluation methodology (GRADE) (19). Because of the observational cohort study design, all GRADE ratings started at low. Evidence certainty could be upgraded if there was evidence of a large and strong association, evidence of a dose response, or adjustment for plausible confounding factors. Publication bias was assessed by visual inspection of funnel plots symmetry for analyses with more than five studies included in the analysis.
Outcomes
The primary outcome was the incidence of CKD (defined as eGFR<60 ml/min per 1.73 m2). The secondary outcomes were (1) ESKD (requiring dialysis or kidney transplantation or eGFR<15 ml/min per 1.73 m2), (2) eGFR decline (as defined by study authors), (3) progression of albuminuria (normal or mildly increased to moderately or severely increased), (4) eGFR or creatinine clearance at the end of study follow-up, and (5) doubling of serum creatinine. The most adjusted risk estimate was extracted.
Data Synthesis and Analysis
Extracted data were entered into RevMan 5.3 for analysis. Data were summarized as hazard ratio, odds ratio (OR), or risk ratios. A random-effects inverse variance meta-analysis model was used to calculate the comparisons between the lowest and highest levels of adherence to dietary patterns. If the association compared low dietary pattern adherence with the outcome, the ratio methods were inverted and then combined into the meta-analysis. For studies reporting associations from the same cohort dataset, we included results from the cohort representing the highest number of participants.
The association between healthy dietary patterns and outcomes was expressed as OR together with 95% confidence interval (95% CI) for binary outcomes (incidence of CKD, ESKD, eGFR decline, and progression of albuminuria). For continuous outcomes (change in serum creatinine and eGFR at the end of the study), the mean and SD were extracted. The association of healthy dietary patterns with continuous outcomes was expressed as mean difference with 95% CI. Heterogeneity was assessed using the chi-squared test and I2 statistic. Heterogeneity was rated according to I2 statistic values as low (<25%), moderate (25%–75%), or high (>75%) (20). Funnel plots were visually inspected for the evidence of small study effects in analyses of more than five studies.
To explore the sources of heterogeneity, a priori subgroup analyses were conducted exploring the type of ratio reported (risk ratio, OR, or hazard ratio) and the type of dietary patterns (Mediterranean diet, DASH diet, or dietary guidelines) included in each outcome. We explored other potential sources of heterogeneity using sensitivity analysis to repeat each analysis excluding studies at high risk of bias, involving ≤100 participants, with short-term follow-up (<6 months), possessing a high attrition rate (>20%), and any source of industry funding. We also conducted a study-by-study sensitivity analysis substituting included studies that reported associations from the same cohort dataset, where one study cohort is removed and another study reporting an association from the same cohort added in, with the process repeated until all studies from the same cohort dataset have been rotated through the meta-analysis once.
Results
Study Selection
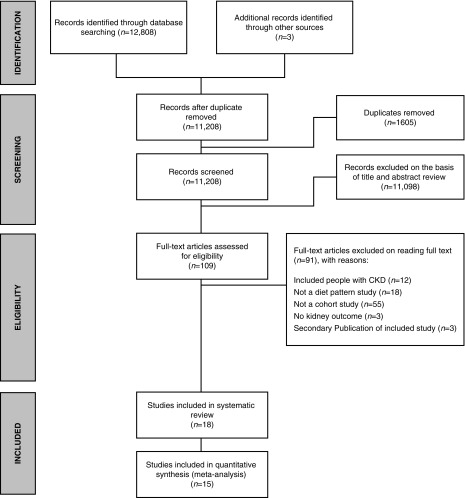
Electronic searching retrieved 12,810 records (Figure 1). Eighteen cohort studies involving 630,108 participants were eligible (Table 1), and 15 studies (85,473 participants) provided extractable data for meta-analysis.
Figure 1.
PRISMA flow diagram showing the selection of studies.
Table 1.
Characteristics of the included studies
| Study | Dietary Pattern | Country | No. of Participants | Follow-up (yr) | Age (yr) | Sex | Comorbidity | Ethnicity | Baseline eGFR (ml/min per 1.73 m2) |
|---|---|---|---|---|---|---|---|---|---|
| Asghari, et al. (31) | Mediterranean diet | Iran | 1212 | 6 | 30–70 (43.5) | 51% male | 6% diabetes 22% hypertension | NA | 73.5 |
| Asghari, et al. (22) | DASH | Iran | 1630 | 6 | >27 (42) | 51.5% male | NA | NA | 74.3 |
| Asghari, et al. | Lacto-vegetarian | Iran | 1630 | 6.1 | >27 (43.4) | 50.8% male | 6.1% diabetes 14.5% hypertension | NA | 73.7 |
| Dunkler, et al. (30) | MAHEI | 40 Countries | 6916 | 5.5 | 61–71 (66) | 68% male | 100% diabetes | NA | 71.5 (67% no CKD and 33% CKD) |
| Foster, et al. (28) | DGAS | United States | 1802 | 6.6 | 59 (±9) | 45.2% male | 7.7% diabetes 38.4% hypertension | NA | NA |
| Khatri, et al. (32) | Mediterranean diet | United States | 900 | 6.9 | >40 | 41% male | 18% diabetes 69% hypertension | 65% Hispanic | 83.1 |
| Liu, et al. (23) | DASH | United States | 1534 | 5 | 30–64 | 42% male | 15% diabetes 42% hypertension | 58% black | 95.5 |
| Rebholz, et al. (33) | American Heart Association: Life’s Simple Seven Healthy Diet | United States | 14,832 | 22 | 45–65 | 43% male | 11.5% diabetes 32.5% hypertension | 24% black | 103.5 |
| Rebholz, et al. (34) | Dietary acid load | United States | 15,055 | 21 | 45–64 | 45% male | 11.4% diabetes 34% hypertension | 26% black | 103.1 |
| Rebholz, et al. (24) | DASH | United States | 14,882 | 23 | 45–64 | 44% male | 11.5% diabetes 34% hypertension | 25% black | 103.1 |
| Haring, et al. (35) | Vegetable protein | United States | 11,952 | 23 | 45–64 | 43% male | 30.7% hypertension | 22.8% black | 103.1 |
| Chang, et al. (25) | DASH | United States | 2354 | 15 | 18–30 (34.8) | 47% male | 7.2% hypertension 1.5% diabetes | 50% black | 101.5 |
| Smyth, et al. (26) | AHEI; HEI; Mediterranean diet score; RFS; DASH | United States | 544,635 | 14.3 | 62.2 | 59% male | 9.2% diabetes 43.5% hypertension | 92.7% white | NA |
| Lin, et al. (21) | DASH | United States | 3121 | 11 | 67 | 100% female | 54% hypertension 23% diabetes 26.4 BMI | 97% white | 76 |
| Chung, et al. (36) | Fish and vegetables | Taiwan | 838 | 2 | 59.5 | 47.5% male | 100% diabetes | NA | 87.5 |
| Ma, et al. (29) | DGAS | United States | 1822 | 7 | 59.4 | 43.6% male | 7.7% diabetes 48.8% hypertension 28 BMI | NA | 86.8 |
| Naderinejad, et al. (37) | Healthy diet | Iran | 1521 | 3.7 | <27 (46.2) | 58% male | 10.5% diabetes >120 mm Hg systolic BP >80 mm Hg diastolic BP | NA | NA |
| Yuzbashian, et al. | DASH | Iran | 3472 | 3.1 | ≤30 | 55% male | hypertension (n=2,089) dyslipidemia (n=2,715) dysglycemia (n=1,100) | NA | NA |
NA, not applicable; DASH, Dietary Approaches to Stop Hypertension; MAHEI, Modified Alternate Healthy Eating Index; DGAS, Dietary Guidelines Adherence Score; AHEI, Alternate Healthy Eating Index; HEI, Healthy Eating Index; RFS, Recommended Food Score; BMI, body mass index.
Study Characteristics
The average study baseline eGFR was 87.2±13 ml/min per 1.73 m2 (range, 72–104). The range of participant ages ranged from 27 to 71 years. No studies were identified in children. Studies were published between 2011 and 2018. All studies included men and women, except one study (21), in which the participants were all women. The follow-up time was 10.4±7.4 years on average (range, 2–23). The healthy dietary patterns reported in these studies included the DASH diet (n=7) (21–27), dietary guidelines (n=4) (26,28–30), Mediterranean diet (n=3) (26,31,32), and other dietary patterns (n=5) (33–38) (Supplemental Table 2). Overall, the characteristics of the healthy dietary patterns reported across the included studies encouraged higher intakes of vegetables, fruit, legumes, nuts, whole grains, fish, and low-fat dairy, and lower intakes of red and processed meats, sodium, and sugar-sweetened beverages.
Outcomes
Risk of bias and quality of evidence.
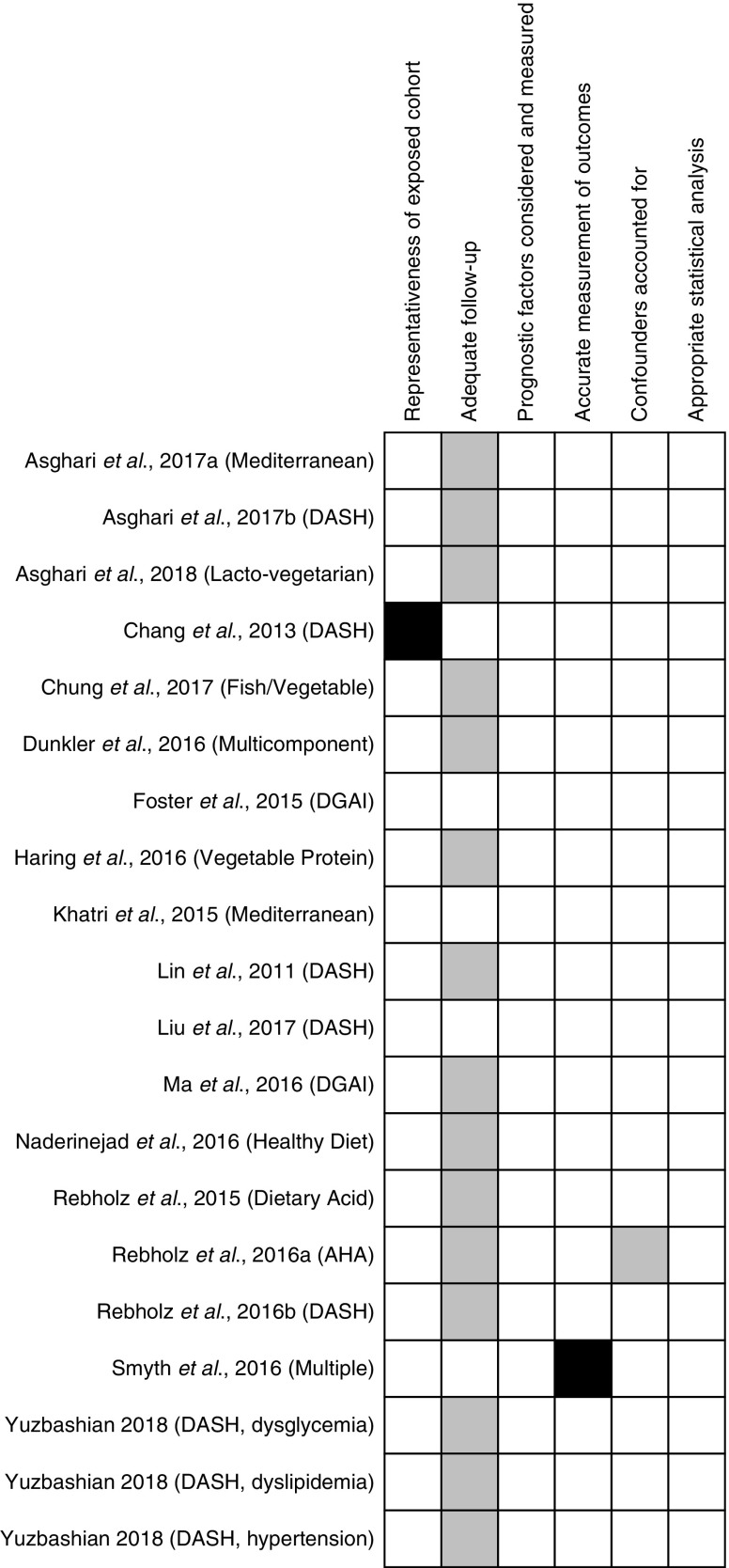
The overall risk of bias for the included studies was considered low across the studies (Figure 2). Two studies had high risk of bias for two components, a possible nonrepresentative sample as a result of a younger population (25), and subjective outcome measures due to dialysis being self-reported (Supplemental Table 3) (26). The overall GRADE for CKD incidence was considered to be moderate because of the large association size. It was low for eGFR decline and incidence of albuminuria (Table 2).
Figure 2.
Study risk of bias. Each color represents a level of risk of bias: white boxes, low risk of bias; grey boxes, unclear risk of bias; black boxes, high risk of bias. Key: Newcastle–Ottawa Scale. 1. Was there a representative and well defined sample? 2. Was the follow-up of participants sufficiently long and completed? 3. Were important prognostic factors considered and measured for? 4. Were the outcomes measured accurately? 5. Were important potential confounders accounted for? 6. Was the statistical analysis appropriate for the design of the study? AHA, American Heart Association; DASH, Dietary Approach to Stop Hypertension; DGAI, Dietary Guidelines Adherence Index.
Table 2.
Summary of assessment of certainty of evidence (GRADE) for different outcomes
| Outcome | No. of Studies | No. of Participants | 95% CI | I2 | Quality of Evidence (GRADE)a |
|---|---|---|---|---|---|
| Incident CKD | 8 | 31,410 | 0.60 to 0.82 | 51% | Moderateb |
| eGFR decline | 4 | 7377 | 0.49 to 1.01 | 59% | Lowc |
| Albuminuria | 4 | 8135 | 0.59 to 0.99 | 37% | Lowc |
| ESKDd | 1 | 544,635 | NA | NA | NA |
| Serum creatinined | 0 | 0 | NA | NA | NA |
| Creatinine clearanced | 0 | 0 | NA | NA | NA |
Low certainty: the confidence in the estimate is limited and the true association may be different from the estimate of association (19). GRADE, Grading of Recommendations Assessment, Development and Evaluation methodology; 95% CI, 95% confidence interval; NA, not applicable.
Moderate certainty: we are moderately confident in the association estimate and the true estimate is likely to be close to the estimate of the association; however, there is the possibility it could be different (19).
Evidence certainty upgraded to moderate because of the large association size.
Evidence quality downgraded to low because of the nonrandomized nature of the studies.
GRADE not possible because of the lack of data.
CKD incidence.
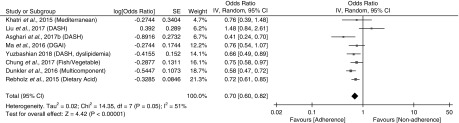
Fifteen studies (79,998 participants) reported incident CKD (22–24,27–38) across eight datasets (22,23,27,29,30,32,34,36). Four studies reported data from the Tehran Lipid and Glucose Study 2006–2008 (22,31,37,38), one study reported three different analyses from the Tehran Lipid and Glucose Study 2009–2011 (27), four studies reported data from the Atherosclerosis Risk in Communities study (24,33,34,39), and two studies reported data from the Framingham Offspring Cohort (28,29). In a meta-analysis including eight studies from the eight eligible cohort datasets (31,410 participants; mean, 7.1 years follow-up), adherence to a healthy dietary pattern was associated with lower odds of incident CKD (OR, 0.70; 95% CI, 0.60 to 0.82; I2=51%) with moderate certainty of evidence (Figure 3). This finding was consistent across different dietary subtypes (P value for interaction =0.65). In a sensitivity analysis, repeating the analysis by rotating each study reporting associations to incident CKD from the same cohort of data one by one, there was no change to the primary finding (Supplemental Table 4).
Figure 3.
Incident CKD associated with adherence to healthy dietary patterns. DASH, Dietary Approach to Stop Hypertension; IV, inverse variance.
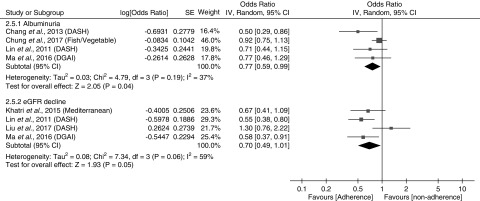
Five studies (9179 participants) reported the outcome of eGFR decline (Figure 4) (23,28,29,32,40) across four datasets, with two studies reported data from the Framingham Offspring Cohort (28,29). The definitions of eGFR decline in eligible studies were reduction from baseline ≥2.5 ml/min per 1.73 m2 per year (32), ≥3.0 ml/min per 1.73 m2 per year (21,23,28,29), ≥25% (23), or ≥30% (21). In a meta-analysis of four studies from four eligible datasets (7377 participants; mean, 7.5 years follow-up), a healthy dietary pattern was nonsignificantly associated with lower odds of eGFR decline (OR, 0.70; 95% CI, 0.49 to 1.01; I2=59%). This finding was consistent across dietary subtypes (P value for subgroup interaction =0.57). In a sensitivity analysis, repeating the analysis by rotating each study reporting associations to eGFR decline from the same cohort of data one by one, there was no change to the primary finding (Supplemental Table 4).
Figure 4.
Risk of albuminuria and eGFR decline associated with adherence to healthy dietary patterns. DASH, Dietary Approach to Stop Hypertension; DGAI, Dietary Guidelines Adherence Index.
Albuminuria.
Four studies (8135 participants; mean, 8.8±5.6 years follow-up) reported incidence of albuminuria (21,25,29,36). A healthy dietary pattern was associated with reduced odds of albuminuria (OR, 0.77; 95% CI, 0.59 to 0.99; I2=37%) (Figure 4).
ESKD, creatinine clearance, or serum creatinine levels.
There were insufficient data to conduct a meta-analysis for ESKD or serum creatinine levels as this was only reported in one study (26). None of the included studies reported results on the outcome creatinine clearance or serum creatinine.
Publication bias.
Publication bias was difficult to assess because of the small number of included studies. Within the included studies there was no evidence of publication bias or small study effects (Supplemental Figure 1).
Subgroup analyses.
The series of planned subgroup analyses are presented in Supplemental Table 5. Mediterranean diets and dietary patterns consistent with dietary guidelines were consistently associated with incident CKD, whereas DASH dietary patterns were not (Supplemental Table 5). Analysis according to the type of risk estimate reported demonstrated significant associations to incident CKD in six studies reporting the OR but not the two studies reporting the hazard ratio. Association estimates by cohort location demonstrated no significant associations in two studies using United States cohorts; however, four cohorts in other geographic locations did demonstrate significant associations to incident CKD. There was no evidence that results in the meta-analysis for incident CKD were different on the basis of duration of follow up time or sample size (Supplemental Table 5).
Discussion
This systematic review and meta-analysis evaluated the association between adherence to dietary patterns and incident CKD in adults without kidney impairment. With moderate certainty of evidence, the primary analysis demonstrated that adherence to a dietary pattern rich in whole grains, vegetables, fruit, legumes, nuts, and fish, and lower intake of red and processed meats, sodium, and sugar sweetened beverages was associated with lower odds of incident CKD, and albuminuria over an average of 10.4 years of follow-up. Across the included studies the overall risk of bias was low.
These results add to the accumulating evidence base supporting the benefits of adherence to healthy dietary patterns for chronic conditions, including those which are considered to be risk factors for the development of kidney disease such as type 2 diabetes, hypertension, cardiovascular, and increased weight (41). A systematic review of randomized controlled trials demonstrated a positive association between adhering to a Mediterranean diet and glycemic control, weight loss, and cardiovascular risk factors in individuals with type 2 diabetes (14). In a large Greek cohort study (n=3042), high Mediterranean diet adherence was associated with a 60% reduced 10-year incidence risk of type 2 diabetes (42). Likewise, higher adherence to the DASH diet has shown significant reductions in both systolic and diastolic BP and reductions in the incidence of cardiovascular disease, coronary heart disease, stroke, and heart failure (43). Previous findings of a meta-analysis have also supported the role of healthy dietary patterns in the prevention of CKD progression (3). Our results add to this evidence base and suggest that following healthy dietary patterns may play a protective role in the primary prevention of CKD. However, it remains unclear what type of “healthy” dietary pattern may be more beneficial, given the high heterogeneity across the studies. When a subgroup analysis of the different dietary patterns was performed, the heterogeneity was almost entirely explained by studies reporting associations to the DASH diet. Analyzing studies reporting DASH dietary pattern exposures separately in a subgroup analysis was not statistically significant, whereas studies reporting associations to the Mediterranean diet and dietary guidelines remained aligned with the primary finding of the review. It is worth noting that only two types of dietary pattern were represented in three separate studies, whereas all others were isolated to one or two investigations. Future research is needed into the potential associations of other dietary patterns, such as vegetarian and Mediterranean diets to kidney outcomes.
This meta-analysis showed reduced odds of incident albuminuria when adhering to a healthy dietary pattern. Albuminuria is regarded as one of the early indicators of kidney damage (44) and an independent risk factor for CKD progression, cardiovascular disease, and all-cause mortality (45). The US National Health and Nutrition Examination Survey showed that the presence of microalbuminuria was the single diagnostic factor for 90% of people with stage 1 CKD (44). The results of this meta-analysis are in agreement with current literature. For example, in two cross-sectional studies, one with multiethnic United States adult participants (n=6814) (11) and the other conducted in Greek adolescent participants (46), showed that plant-based and Mediterranean dietary patterns were inversely associated with microalbuminuria. Moreover, a Western-style dietary pattern high in refined grains, high-fat dairy foods, meat, beans, and tomatoes was positively associated with albumin-to-creatinine ratio (11).
Only one of the included studies reported the risk of ESKD. Given the participants in these studies were free of CKD at baseline, this is not surprising as this is a rare outcome even among patients with established CKD. Specifically, of the 10% of the population that currently live with CKD, a much smaller proportion will progress to ESKD (47). The findings of a recent Australian CKD cohort study showed that adherence to a dietary pattern rich in fruit and vegetables reduced the risk of the composite end point of mortality, doubling of serum creatinine, and ESKD (48), although there was no association with the individual components of the composite end point (48).
This systematic review had a rigorous and extensive search of the literature, utilization of two independent reviewers for each stage of the review and adhered to the PRISMA reporting guidelines. However, there are important limitations worth noting. First, there was a lack of standardization of dietary pattern reporting across the included studies. Generally, whole grains, fruit, and vegetables were consistently considered to be key components to a healthy dietary pattern; however, meat and milk products varied between desirable (healthy) and undesirable (unhealthy) categories. In addition, some studies included alcohol as one of their components, whereas others either did not report or did not include this component. The misclassification of dietary reporting is also important to acknowledge, particularly long-term diet intake behavior quantified using a single food frequency questionnaire measurement, which was the predominant method utilized across the included studies. Second, there was variation in measurement reporting of some outcomes, including incident CKD, albuminuria, and eGFR decline (Supplemental Table 3). Third, the results may not be generalizable to other populations around the world, as 14 of the 16 included studies were conducted in either the United States or Iran, and none of the studies were conducted in children. Finally, as this meta-analysis was on the basis of cohort studies and not randomized trials, the findings do not imply causality. The conclusions generated by this review are hypothesis-generating and indicate the need for large long-term, randomized trials.
In conclusion, this systematic review and meta-analysis indicates that adhering to a healthy dietary pattern rich in, vegetables, fruit, legumes, nuts, whole grains, fish, and low-fat dairy, and lower intakes of red and processed meats, sodium, and sugar-sweetened beverages, is associated with reduced incidence of CKD and albuminuria. On the basis of the findings from this review, a healthy dietary pattern (possibly the Mediterranean diet) and/or interventions testing the effectiveness of dietary guidelines need to be studies in randomized, controlled trials.
Disclosures
Mrs. Bach, Dr. Campbell, Dr. Kelly, Dr. Khalesi, Dr. Palmer, and Dr. Strippoli have nothing to disclose.
Supplementary Material
Acknowledgments
Dr. Kelly, Dr. Campbell, and Dr. Palmer contributed to the study conception. Mrs. Bach and Dr. Kelly conducted the literature search and data analysis. Dr. Bach and Dr. Khalesi extracted data and appraised risk of bias. Mrs. Bach was responsible for writing the first draft of the manuscript. Dr. Kelly and Dr. Campbell reviewed the first draft of the manuscript. All authors read and approved the final version of the manuscript.
We would like to acknowledge the contribution of David Honeymann, a Bond University Librarian, with assistance in the development of the search strategy.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
Supplemental Material
This article contains the following supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.00530119/-/DCSupplemental.
Supplemental Table 1. List of search terms.
Supplemental Table 2. Characteristics of the dietary patterns reported in the included studies.
Supplemental Table 3. Measurement of outcomes.
Supplemental Table 4. Results from sensitivity analysis substituting data from secondary publications of the same cohort dataset. The shaded rows represent the study citation included in the primary analysis.
Supplemental Table 5. Subgroup analysis for incident CKD.
Supplemental Figure 1. Funnel plot for risk of incidence of CKD associated with adherence to healthy dietary patterns.
References
- 1.Eknoyan G, Lameire N, Barsoum R, Eckardt KU, Levin A, Levin N, Locatelli F, MacLeod A, Vanholder R, Walker R, Wang H: The burden of kidney disease: Improving global outcomes. Kidney Int 66: 1310–1314, 2004 [DOI] [PubMed] [Google Scholar]
- 2.Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY: Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 351: 1296–1305, 2004 [DOI] [PubMed] [Google Scholar]
- 3.Kelly JT, Palmer SC, Wai SN, Ruospo M, Carrero JJ, Campbell KL, Strippoli GF: Healthy dietary patterns and risk of mortality and ESRD in CKD: A meta-analysis of cohort studies. Clin J Am Soc Nephrol 12: 272–279, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kelly JT, Rossi M, Johnson DW, Campbell KL: Beyond sodium, phosphate and potassium: Potential dietary interventions in kidney disease. Semin Dial 30: 197–202, 2017 [DOI] [PubMed] [Google Scholar]
- 5.Mills KT, Xu Y, Zhang W, Bundy JD, Chen CS, Kelly TN, Chen J, He J: A systematic analysis of worldwide population-based data on the global burden of chronic kidney disease in 2010. Kidney Int 88: 950–957, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leech RM, Worsley A, Timperio A, McNaughton SA: Understanding meal patterns: Definitions, methodology and impact on nutrient intake and diet quality. Nutr Res Rev 28: 1–21, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Salas-Salvadó J, Garcia-Arellano A, Estruch R, Marquez-Sandoval F, Corella D, Fiol M, Gómez-Gracia E, Viñoles E, Arós F, Herrera C, Lahoz C, Lapetra J, Perona JS, Muñoz-Aguado D, Martínez-González MA, Ros E; PREDIMED Investigators : Components of the Mediterranean-type food pattern and serum inflammatory markers among patients at high risk for cardiovascular disease. Eur J Clin Nutr 62: 651–659, 2008 [DOI] [PubMed] [Google Scholar]
- 8.Hermsdorff HH, Barbosa KB, Volp AC, Puchau B, Bressan J, Zulet MÁ, Martínez JA: Vitamin C and fibre consumption from fruits and vegetables improves oxidative stress markers in healthy young adults. Br J Nutr 107: 1119–1127, 2012 [DOI] [PubMed] [Google Scholar]
- 9.Jiang R, Jacobs DR Jr., Mayer-Davis E, Szklo M, Herrington D, Jenny NS, Kronmal R, Barr RG: Nut and seed consumption and inflammatory markers in the multi-ethnic study of atherosclerosis. Am J Epidemiol 163: 222–231, 2006 [DOI] [PubMed] [Google Scholar]
- 10.Banerjee T, Tucker K, Griswold M, Wyatt SB, Harman J, Young B, Taylor H, Powe NR: Dietary potential renal acid load and risk of albuminuria and reduced kidney function in the Jackson heart study. J Ren Nutr 28: 251–258, 2018 [DOI] [PubMed] [Google Scholar]
- 11.Nettleton JA, Steffen LM, Palmas W, Burke GL, Jacobs DR Jr.: Associations between microalbuminuria and animal foods, plant foods, and dietary patterns in the Multiethnic Study of Atherosclerosis. Am J Clin Nutr 87: 1825–1836, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Casas R, Estruch R: Dietary patterns, foods, nutrients and chronic inflammatory disorders. Immunome Res 12: 122, 2016 [Google Scholar]
- 13.Fried L, Solomon C, Shlipak M, Seliger S, Stehman-Breen C, Bleyer AJ, Chaves P, Furberg C, Kuller L, Newman A: Inflammatory and prothrombotic markers and the progression of renal disease in elderly individuals. J Am Soc Nephrol 15: 3184–3191, 2004 [DOI] [PubMed] [Google Scholar]
- 14.Huo R, Du T, Xu Y, Xu W, Chen X, Sun K, Yu X: Effects of Mediterranean-style diet on glycemic control, weight loss and cardiovascular risk factors among type 2 diabetes individuals: A meta-analysis. Eur J Clin Nutr 69: 1200–1208, 2015 [DOI] [PubMed] [Google Scholar]
- 15.Panagiotakos DB, Pitsavos C, Arvaniti F, Stefanadis C: Adherence to the Mediterranean food pattern predicts the prevalence of hypertension, hypercholesterolemia, diabetes and obesity, among healthy adults; the accuracy of the MedDietScore. Prev Med 44: 335–340, 2007 [DOI] [PubMed] [Google Scholar]
- 16.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group : Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med 6: e1000097, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group : KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl 3: 1–163, 2013 [Google Scholar]
- 18.Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P: The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2014
- 19.Guyatt GH, Oxman AD, Schünemann HJ, Tugwell P, Knottnerus A: GRADE guidelines: A new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol 64: 380–382, 2011 [DOI] [PubMed] [Google Scholar]
- 20.Higgins JPT, Green S, editor: Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011], London, UK, The Cochrane Collaboration, 2011 [Google Scholar]
- 21.Lin J, Fung TT, Hu FB, Curhan GC: Association of dietary patterns with albuminuria and kidney function decline in older white women: A subgroup analysis from the Nurses’ Health Study. Am J Kidney Dis 57: 245–254, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Asghari G, Yuzbashian E, Mirmiran P, Azizi F: The association between Dietary Approaches to Stop Hypertension and incidence of chronic kidney disease in adults: The Tehran Lipid and Glucose Study. Nephrol Dial Transplant 32[suppl_2]: ii224–ii230, 2017 [DOI] [PubMed] [Google Scholar]
- 23.Liu Y, Kuczmarski MF, Miller ER 3rd, Nava MB, Zonderman AB, Evans MK, Powe NR, Crews DC: Dietary habits and risk of kidney function decline in an urban population. J Ren Nutr 27: 16–25, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rebholz CM, Crews DC, Grams ME, Steffen LM, Levey AS, Miller ER 3rd, Appel LJ, Coresh J: DASH (Dietary Approaches to Stop Hypertension) diet and risk of subsequent kidney disease. Am J Kidney Dis 68: 853–861, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chang A, Van Horn L, Jacobs DR Jr., Liu K, Muntner P, Newsome B, Shoham DA, Durazo-Arvizu R, Bibbins-Domingo K, Reis J, Kramer H: Lifestyle-related factors, obesity, and incident microalbuminuria: The CARDIA (Coronary Artery Risk Development in Young Adults) study. Am J Kidney Dis 62: 267–275, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Smyth A, Griffin M, Yusuf S, Mann JF, Reddan D, Canavan M, Newell J, O’Donnell M: Diet and major renal outcomes: A prospective cohort study. The NIH-AARP diet and health study. J Ren Nutr 26: 288–298, 2016 [DOI] [PubMed] [Google Scholar]
- 27.Yuzbashian E, Asghari G, Mirmiran P, Amouzegar-Bahambari P, Azizi F: Adherence to low-sodium Dietary Approaches to Stop Hypertension-style diet may decrease the risk of incident chronic kidney disease among high-risk patients: A secondary prevention in prospective cohort study. Nephrol Dial Transplant 33: 1159–1168, 2018 [DOI] [PubMed] [Google Scholar]
- 28.Foster MC, Hwang SJ, Massaro JM, Jacques PF, Fox CS, Chu AY: Lifestyle factors and indices of kidney function in the Framingham Heart Study. Am J Nephrol 41: 267–274, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ma J, Jacques PF, Hwang SJ, Troy LM, McKeown NM, Chu AY, Fox CS: Dietary guideline adherence index and kidney measures in the Framingham heart study. Am J Kidney Dis 68: 703–715, 2016 [DOI] [PubMed] [Google Scholar]
- 30.Dunkler D, Kohl M, Teo KK, Heinze G, Dehghan M, Clase CM, Gao P, Yusuf S, Mann JF, Oberbauer R; ONTARGET Investigators : Population-attributable fractions of modifiable lifestyle factors for CKD and mortality in individuals with type 2 diabetes: A cohort study. Am J Kidney Dis 68: 29–40, 2016 [DOI] [PubMed] [Google Scholar]
- 31.Asghari G, Farhadnejad H, Mirmiran P, Dizavi A, Yuzbashian E, Azizi F: Adherence to the Mediterranean diet is associated with reduced risk of incident chronic kidney diseases among Tehranian adults. Hypertens Res 40: 96–102, 2017 [DOI] [PubMed] [Google Scholar]
- 32.Khatri M, Moon YP, Scarmeas N, Gu Y, Gardener H, Cheung K, Wright CB, Sacco RL, Nickolas TL, Elkind MS: The association between a Mediterranean-style diet and kidney function in the Northern Manhattan Study cohort. Clin J Am Soc Nephrol 9: 1868–1875, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rebholz CM, Anderson CA, Grams ME, Bazzano LA, Crews DC, Chang AR, Coresh J, Appel LJ: Relationship of the American Heart Association’s impact goals (Life’s Simple 7) with risk of chronic kidney disease: Results from the Atherosclerosis Risk in Communities (ARIC) cohort study. J Am Heart Assoc 5: e003192, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rebholz CM, Coresh J, Grams ME, Steffen LM, Anderson CAM, Appel LJ, Crews DC: Dietary acid load and incident chronic kidney disease: Results from the ARIC study. Am J Nephrol 42: 427–435, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Haring B, Selvin E, Liang M, Coresh J, Grams ME, Petruski-Ivleva N, Steffen LM, Rebholz CM: Dietary protein sources and risk for incident chronic kidney disease: Results from the Atherosclerosis Risk in Communities (ARIC) study. J Ren Nutr 27: 233–242, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chung HF, Hsu CC, Mamun AA, Long KZ, Huang YF, Shin SJ, Hwang SJ, Huang MC: Dietary patterns, dietary biomarkers, and kidney disease in patients with type 2 diabetes: A repeated-measure study in Taiwan. Asia Pac J Clin Nutr 27: 366–374, 2018 [DOI] [PubMed] [Google Scholar]
- 37.Naderinejad N, Ejtahed HS, Asghari G, Mirmiran P, Azizi F: Association between dietary patterns and incidence of chronic kidney disease in adults with high blood pressure: Tehran Lipid and Glucose study. Majallah-i Ghudad-i Darun/Riz va Mitabulism-i Iran 18: 231–242, 2016 [Google Scholar]
- 38.Asghari G, Momenan M, Yuzbashian E, Mirmiran P, Azizi F: Dietary pattern and incidence of chronic kidney disease among adults: A population-based study. Nutr Metab (Lond) 15: 88, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Haring B, Selvin E, Liang M, Coresh J, Grams ME, Petruski-Ivleva N, Steffen LM, Rebholz CM: Dietary protein sources and risk for incident chronic kidney disease: Results from the Atherosclerosis Risk in Communities (ARIC) study. J Ren Nutr 27: 233–242, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lin J, Hu FB, Curhan GC: Associations of diet with albuminuria and kidney function decline. Clin J Am Soc Nephrol 5: 836–843, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kazancioğlu R: Risk factors for chronic kidney disease: An update. Kidney Int Suppl (2011) 3: 368–371, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Koloverou E, Panagiotakos DB, Pitsavos C, Chrysohoou C, Georgousopoulou EN, Grekas A, Christou A, Chatzigeorgiou M, Skoumas I, Tousoulis D, Stefanadis C; ATTICA Study Group : Adherence to Mediterranean diet and 10-year incidence (2002-2012) of diabetes: Correlations with inflammatory and oxidative stress biomarkers in the ATTICA cohort study. Diabetes Metab Res Rev 32: 73–81, 2016 [DOI] [PubMed] [Google Scholar]
- 43.Salehi-Abargouei A, Maghsoudi Z, Shirani F, Azadbakht L: Effects of Dietary Approaches to Stop Hypertension (DASH)-style diet on fatal or nonfatal cardiovascular diseases--incidence: A systematic review and meta-analysis on observational prospective studies. Nutrition 29: 611–618, 2013 [DOI] [PubMed] [Google Scholar]
- 44.Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, Van Lente F, Levey AS: Prevalence of chronic kidney disease in the United States. JAMA 298: 2038–2047, 2007 [DOI] [PubMed] [Google Scholar]
- 45.Ninomiya T, Perkovic V, de Galan BE, Zoungas S, Pillai A, Jardine M, Patel A, Cass A, Neal B, Poulter N, Mogensen CE, Cooper M, Marre M, Williams B, Hamet P, Mancia G, Woodward M, Macmahon S, Chalmers J; ADVANCE Collaborative Group : Albuminuria and kidney function independently predict cardiovascular and renal outcomes in diabetes. J Am Soc Nephrol 20: 1813–1821, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mazaraki A, Tsioufis C, Dimitriadis K, Tsiachris D, Stefanadi E, Zampelas A, Richter D, Mariolis A, Panagiotakos D, Tousoulis D, Stefanadis C: Adherence to the Mediterranean diet and albuminuria levels in Greek adolescents: Data from the Leontio Lyceum ALbuminuria (3L study). Eur J Clin Nutr 65: 219–225, 2011 [DOI] [PubMed] [Google Scholar]
- 47.Meguid El Nahas A, Bello AK: Chronic kidney disease: The global challenge. Lancet 365: 331–340, 2005 [DOI] [PubMed] [Google Scholar]
- 48.Wai SN, Kelly JT, Johnson DW, Campbell KL: Dietary patterns and clinical outcomes in chronic kidney disease: The CKD.QLD nutrition study. J Ren Nutr 27: 175–182, 2017 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.