Abstract
Introduction:
Opioid-related overdoses have been steadily increasing over the past decade in the United States. Naloxone is used by first responders to revive overdose victims, but results may be improved by increasing access to and usage of naloxone by bystanders. Automated External Defibrillators (AEDs) are pervasive, recognizable and publicly accessible. Co-locating naloxone kits with AEDs could increase public naloxone access and usage. However, the impact of co-locating naloxone kits with AEDs is not known.
Objectives:
We sought to evaluate the impact of co-locating naloxone kits with AEDs in a simulation study centered on Allegheny County, Pennsylvania.
Methods:
Naloxone administration frequency (N = 3650) at the zip-code level from March 2016-March 2017 was provided by the Allegheny County Health Department. AED point locations (N=1653) were obtained from the University of Pittsburgh’s Resuscitation Logistics and Informatics Venture. Zip-code level geospatial analyses were conducted using QGIS and STATA to determine the correlation between AED count and naloxone administrations. AED naloxone kit (N-AED) coverage, based on a maximum “walking-distance” radius of 200m, was estimated at a zip-code level using the QGIS buffer tool and a custom MATLAB script. Potential impact of N-AEDs was estimated assuming uniform spatial distribution of naloxone administrations.
Results:
The median(IQR) AED coverage based on a 200m access radius per zip code was 4%(0–7). The median(IQR) number of naloxone administrations per zip code was 27(7–55). A total of 82 zip codes had data for both AED locations and naloxone administrations. The correlation between number of AEDs and naloxone administrations per zip code was 0.2. Overall, 16% of naloxone administrations were estimated to be covered by an N-AED.
Conclusion:
Using these limited methods, co-locating naloxone with AEDs is not likely to have a standalone impact on preventing overdose fatalities.
Introduction
Opioid-related overdoses have been steadily increasing over the past decade.1 An opioid overdose causes respiratory distress, potentially leading to cardiac arrest and death. Naloxone is an opioid receptor antagonist which, when given shortly after an overdose, can reverse the event.2 Delays in administration may increase the probability of death or morbidity.3 While naloxone has historically been administered by EMS, the opioid crisis has led to increased accessibility to laypeople. For example, the Commonwealth of Pennsylvania has made naloxone available for over-the-counter purchase and added a statewide opioid overdose-specific “Good Samaritan” law to protect those who contact emergency services from legal repurcussions.4 Widespread bystander naloxone access could potentially expedite treatment of public overdoses before the arrival of EMS personnel and impact outcomes.
There is precedent in other areas of prehospital emergency care for bystander medical interventions facilitated by publicly available medical resources. Automatic External Defibrillators (AEDs) are emergency medical devices designed to deliver electricity to the heart during cardiac arrest, featuring a simple user interface and audio prompting suitable for use by laypeople with minimal training. As part of public access defibrillation programs, AEDs are often stationed in public locations and buildings to facilitate rapid access by bystanders during cardiac emergencies; this approach has been proven to increase out-of-hospital cardiac arrest survival, including cardiac arrest due to overdose in which standard resuscitation applies.5 Physical AED locations are frequently marked with highly visible signage which make them easy to find in an emergency, and locations of publicly accessible AEDs are increasingly being integrated into electronic databases that enable wide and rapid dissemination.6 Furthermore, AEDs are broadly distributed across cities in a wide variety of location and building types, owing to the spontaneous nature of out-of-hospital cardiac arrest.7 Geographically, public overdoses have been shown to occur most frequently in urban locations, leading to potential overlap in AED placement and overdose incidence.8 Such diversity of locations in public areas, along with an existing maintenance infrastructure, and potential utility for treating overdose-related cardiac arrest suggest that AEDs may be a logical location for publicly accessible naloxone kits.
To our knowledge, there are no studies investigating the potential impact or utility of co-locating naloxone kits with AEDs. We sought to begin investigating the potential of this strategy by simulating co-location of naloxone kits with known publicly accessible AEDs in Allegheny County, Pennsylvania. We hypothesized that AED locations would overlap with historical naloxone administrations by public safety and afford rapid accessibility to naloxone throughout the County.
Methods
This simulation study was performed using publicly available, de-identified data and did not constitute human subjects research.
Data Collection
Zip code level naloxone administration data was provided by the Allegheny County Health Department for the period spanning March 10, 2016 to March 10, 2017. Naloxone administration events were determined from public safety records, including police, fire and emergency medical services (EMS) agencies (N=2536). In Allegheny County, there are 107 independent municipalities, many with their own public safety agencies, emergency response procedures, and approaches to naloxone administration, so providing a uniform set of determinants for naloxone administration among all of these events is not possible. In the Commonwealth of Pennsylvania, naloxone administration by public safety professionals is governed by Standing Order DOH-001–2016 and the 2017 Pennsylvania Statewide Basic Life Support Protocols.9 We therefore assumed that naloxone administration occurred in accordance with these two statutes and followed identification of suspected opioid overdose (symptoms of unresponsiveness, decreased respiratory effort, pinpoint pupils, history of narcotic ingestion, or fentanyl patches on skin).10 Lastly, for this analysis, we considered each event requiring an administration, not the number of administrations (i.e., doses) per event. Thus, the unit level of analysis is a unique patient encounter.
AED point locations (N=1653) in Allegheny County were obtained from the University of Pittsburgh’s Resuscitation Logistics and Informatics Venture (ReLIVe) in latitude /longitude coordinates. ReLIVe determines AED locations through a combination of active and passive device surveillance, confirming device locations with direct follow-up. For this study, buildings with more than one AED were consolidated into a single geospatial point. We then determined the count, the spatial density (AED/mi2), and the per capita density of AEDs per zip code area.
Demographic data were obtained from the US Census Bureau’s American FactFinder tool.11 These included population count, population density, median household income, median age, and proportion of the population over the age of 65.
Analysis
AED-naloxone kit (N-AED) spatial coverage was estimated at a zip code level using the QGIS buffer tool and a custom MATLAB script. The ability of 9-1-1 dispatchers to disseminate N-AED location information to bystanders was assumed to expand the radius in which the caller could locate and retrieve the device for use. Coverage was based on a maximum “walking-distance” radius of 200m which assumes a responder’s ability to retrieve naloxone and return to the patient within 3 minutes, assuming a travel speed of 5MPH (see Map 3). To calculate the spatial coverage, we superimposed the N-AED accessibility buffers (i.e., radii) on each zip code polygon, and used an image analysis algorithm to determine the proportion of the zip code area covered.
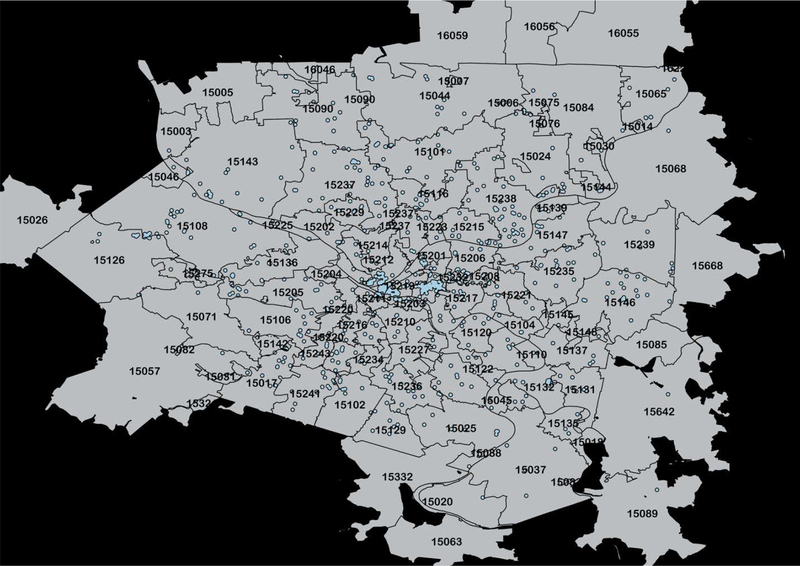
Map 3. AED Coverage in Allegheny County.
–Geospatial AED coverage is shown over the zip-codes of Allegheny County. The blue area is the area with an AED accessible within a 200m walking distance.
N-AED event coverage was estimated assuming uniform spatial distribution of naloxone events, a constraint that we shall acknowledge in the limitations below. Therefore, if the 200m accessibility radius of all AEDs in a zip code covered 90% of the land area within a zip code, our estimation method assumed that 90% of naloxone administration events occurred within range of an AED, i.e. 90% event coverage. Event coverage was reported at the zip code level as well as in aggregate for Allegheny County and separately the City of Pittsburgh, which is the largest urban area in the County.
Frequency, minimum, maximum, and median (IQR) AEDs and naloxone administration events per zip code were calculated. To determine if AEDs tend to be located where naloxone is most needed, we initially calculated a Pearson correlation coefficient for the number of AEDs and the number of naloxone administrations at the zip code level. To investigate how this relationship might be confounded by demographic factors, we conducted multivariable regression analysis, adjusting for the factors listed above. All statistical analyses were conducted in Stata (Version 14, Stata Corp., College Station, TX).
Results
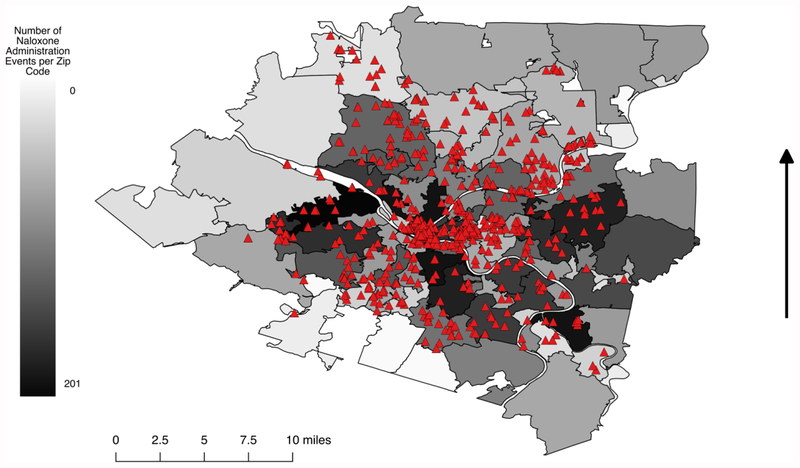
Naloxone administration counts with AED locations superimposed are shown in Map 1. AED location and naloxone administration data were available in total of 82 of 97 zip codes in Allegheny County: 21 (22%) of zip codes had no AEDs, 15 (15%) had no naloxone administrations, 15 (15%) had neither, and 76 (78%) had both. The median(IQR) number of naloxone administrations per zip code in the County was 27(7–55) and in the City was 42(28–64). The median(IQR) number of AEDs per zip code in the County was 9(3–17) and in the City was 11(4.75–19.5). The majority of AEDs were clustered in the urban centers of the City of Pittsburgh, with the rest diffusely distributed across the County. Naloxone administrations tended to be clustered in the City of Pittsburgh and the nearest surrounding zip codes, with the southwest and northeast portions of the County experiencing the least number of naloxone administration events.
Map 1. AED Locations and Naloxone Administration Events in Allegheny County.
AED locations are represented by the red triangles. Naloxone administration events per zip code are shaded from white to black, with increasingly dark shades of gray representing increasing frequency of naloxone administration events.
The Pearson correlation between naloxone administrations and AED count (0.20), naloxone administrations and AEDs per capita (0.10), and naloxone administrations and AED density (−0.03) were calculated. In a multivariate regression model, both total population (.002, p<0.000) and median household income (−0.0008, p<0.001) were associated with naloxone administrations when controlling for other demographic factors. However, there was no significant association between naloxone administrations and number of AEDs, AED density, or AED coverage.
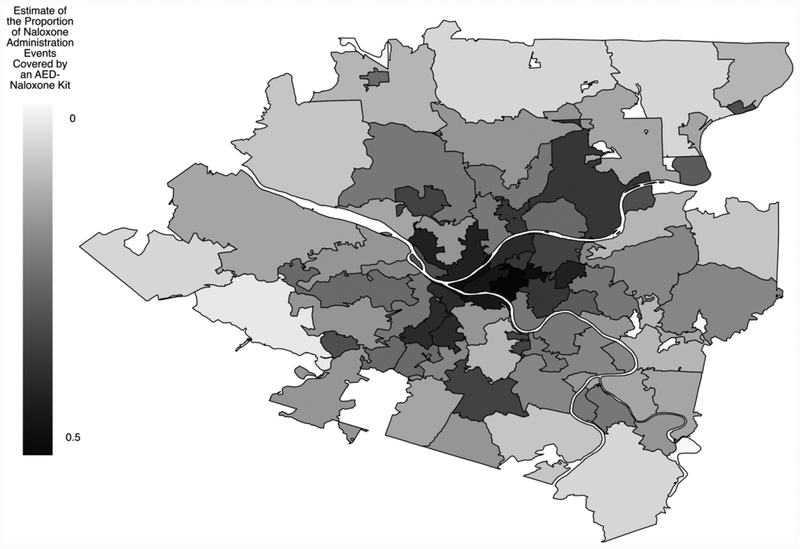
Map 2 shows the distribution of event coverage across the County. The median(IQR) AED coverage per zip code in the County was 4%(0–7) and in the City was 11%(7–22), with two zip codes within the City reaching 100% coverage. Overall, event coverage by N-AEDs was estimated to be 16%, or 288 events, in the County as a whole and 23%, or 189 events, in the City of Pittsburgh. Event coverage was moderately correlated with median age (−0.55), and weakly correlated with population density (0.20), proportion of the population over 65 (−0.20), total population (0.14), median household income (−0.11), total number of events (0.12), and spatial area (−0.01).
Map 2. Distribution of Event Coverage Across Allegheny County.
Proportion of events estimated to be covered by an AED-naloxone kit per zip code are shaded from white to black, with increasingly dark shades of gray representing increasing frequency of naloxone administration events covered by an AED-naloxone kit.
Discussion
If naloxone kits were co-located with AEDs, they might provide life-saving treatment to overdose patients near these locations. However, our study shows a weak correlation between AED locations and naloxone administrations. Only 16% of naloxone administrations were estimated to be covered by AED-naloxone kits, assuming even spatial distribution of naloxone administrations within zip codes. This may indicate that AED-naloxone placement would not be sufficient by itself, and would best be implemented in consort with other interventions, such as targeted distribution of naloxone in affected areas.
Bystander naloxone administration has been shown to improve outcomes of overdose patients.3 Providing laypeople with naloxone kits, rather than laypeople seeking out kits at pharmacies, could increase the likelihood that it is used when it is needed. Organizations across the country have already begun naloxone distribution programs to laypeople.12 However, these programs are limited. Public naloxone kits would not depend on an individual’s participation in a naloxone distribution program, and could be closer to the actual overdose event, both temporally and spatially.
The strategy of co-locating naloxone with AEDs carries several important requirements, constraints and potential consequences. To be effective under emergency circumstances, N-AED locations would have to be communicated to the public, either through 911 or another real-time information source. Dissemination of AED location data has been facilitated by the development of smartphone applications and web services integrated with electronic AED databases. The same data infrastructure could theoretically be utilized to enable rapid location of naloxone in an overdose emergency. Availability is also a function of distribution and maintenance; naloxone kits would have to be placed and regularly verified or replaced as they expire or are retrieved for use. Layers of infrastructure exist for replacing AED components, and likely the same infrastructure could be employed to replace naloxone kits. This includes regularly scheduled maintenance by responsible personnel, contact-if-used information paired with the supplies, and alarmed AED cabinets that audibly signal materials have been accessed. More technologically advanced solutions are available as well, including 911-connected AED cabinets and the FDA-sponsored HeartMap Challenge, which places QR-coded labels on publicly accessible AEDs, enabling real-time tracking of usage.6,13
Some of the potential barriers to N-AED placement are the same barriers encountered for general AED placement. Although in principle accessible to the public, some AEDs are on private property and can be affected by changes in security procedures, operating hours, or building management. Even AEDs that are always physically accessible to the public may be difficult to find, limiting their practical utility. From a deployment perspective, costs associated with maintaining either type of AED may limit their acceptance. Research on PADs has shown that they are utilized at very low rates, with some areas reporting successful PAD use as low as 1.7%.14 These rates may serve as counter-evidence to the value of maintaining AEDs in a given building.
Placing naloxone in a public location may inadvertently create demand if the public utilizes AEDs as a source of prophylactic naloxone. Depending on the breadth of dissemination of N-AEDs, this may cause a substantial cost and labor burden for system maintenance. Importantly, alarmed AED cabinets could deter users from accessing naloxone in an overdose situation, though non-using bystanders would not encounter this barrier. Furthermore, it is conceivable that building owners may object to storing naloxone on site due to perceived liability. It may be difficult to overcome the stigmas associated with drug use and subsequent overdose that are inextricably connected with this intervention, as well as the perception that locating reversal agents in a building will attract drug users and increase drug use therein.
Co-locating life-saving resources with AEDs is not unprecedented. For instance, the federal “Stop the Bleed” campaign aims to co-locate trauma kits with AEDs.15 In this scheme, bystanders with minimal training can theoretically prevent death by hemorrhage by applying publicly accessible tourniquets or hemostatic bandages before EMS arrives. Co-location of bleed kits with AEDs simplifies localization of these resources in an emergency, because bystanders need only recall a single location that serves as a multi-condition emergency medical supply station. Inclusion of naloxone is a natural extension of this strategy, reinforced by the increasingly high incidence of opioid overdose. It is difficult to directly compare the relative impacts of naloxone co-location and bleed kit co-location, in part because the epidemiological characterization of prehospital conditions that would specifically qualify for treatment with a bleed kit is very limited. However, it seems intuitive that their relative impacts would vary at least geographically with variation in the underlying incidence of either type of condition. Our group is actively investigating these considerations in on-going work. Other potential extensions of this strategy are conceivable, including publicly accessible albuterol and epinephrine, all of which would address acute prehospital conditions largely resolvable with a simple intervention, although each carries important practical and regulatory constraints for deployment beyond the scope of this study.
There are several limitations to our study. First, we only had access to naloxone administration data at the zip code level, limiting the resolution of our analyses and preventing direct ascertainment of the spatial relationship between N-AEDs and individual events. To compensate for this, we assessed coverage in terms of a fixed radius around each device. However, this radius does not account for street navigation distance, and it is likely that the radius will not always provide the optimal response time to meet the needs of every patient. More importantly, our analysis methodology could not account for event clustering tendencies, if present, below the zip code level. Vertical distance to N-AEDs in buildings with multiple floors was not considered as part of our coverage analysis. We also did not consider the cost of an N-AED intervention. It is convenient to simulate the dissemination of naloxone to 1,000 or more locations across a broad geographic area, but the costs of doing so could make this prohibitive in practice. Finally, our approach did not consider temporal factors associated with emergency demand for naloxone. Our data set did not include the day or time of naloxone administration events, and therefore could not be compared with real AED accessibility hours. It is likely that both would have a significant impact on true spatiotemporal coverage and therefore effectiveness of such an intervention.
Conclusion
Using these limited methods, co-locating naloxone with AEDs is not likely to have a standalone impact on preventing overdose fatalities.
Acknowledgments
We would like to thank Dr. LuAnn Brink and Steven Forest for providing us the naloxone administration data.
Jessica Salerno’s salary was supported during the study period by grants from the Henry L. Hillman Foundation, which also supports the Resuscitation Logistics and Informatics Venture. Dr. Salcido’s effort for this project was supported by a grant from the National Heart, Lung, and Blood Institute (1R21HL135369).
Footnotes
Declaration of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- 1.Centers for Disease Control and Prevention. (2016. December 16). Retrieved from https://www.cdc.gov/drugoverdose/epidemic/index.html
- 2.Volkow ND, Collins FS. The Role of Science in Addressing the Opioid Crisis. N Engl J Med. 2017. July 27;377(4):391–394. Epub 2017 May 31. [DOI] [PubMed] [Google Scholar]
- 3.Giglio RE, Li G, DiMaggio CJ. Effectiveness of bystander naloxone administration and overdose education programs: a meta-analysis. Inj Epidemiol. 2015. December;2(1):10 Epub 2015 May 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wolf T, Smith J. 2017. Opioid/Heroin Reversal (Naloxone). Retrieved from http://www.ddap.pa.gov/overdose/pages/naloxone_reversal.aspx
- 5.Bækgaard J, Viereck S, Møller T, Ersbøll A, Lippert F, Folke F. The Effects of Public Access Defibrillation on Survival After Out-of-Hospital Cardiac Arrest: A Systematic Review of Observational Studies. Circulation. (2017. July 7). pii: CIRCULATIONAHA.117.029067. doi: 10.1161/CIRCULATIONAHA.117.029067. [DOI] [PubMed] [Google Scholar]
- 6.Elrod JB, Merchant R, Daya M, Youngquist S, Salcido D, Valenzuela T, Nichol G. Public health surveillance of automated external defibrillators in the USA: protocol for the dynamic automated external defibrillator registry study. BMJ Open. 2017. March 29;7(3):e014902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chrisinger BW, Grossestreuer AV, Laguna MC, Griffis HM, Branas CC, Wiebe DJ, Merchant RM. Characteristics of automated external defibrillator coverage in Philadelphia, PA, based on land use and estimated risk. Resuscitation. 2016. December;109:9–15. doi: 10.1016/j.resuscitation.2016.09.021. Epub 2016 Oct 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meiman J, Tomasallo C, Paulozzi L. Trends and characteristics of heroin overdoses in Wisconsin, 2003–2012. Drug Alcohol Depend. 2015. July 1;152:177–84. [DOI] [PubMed] [Google Scholar]
- 9.Pennsylvania Department of Health. STANDING ORDER DOH-002–2017 Naloxone Prescription for Overdose Prevention. By Dr. Levine Rachel. Retrieved from http://www.health.pa.gov/My%20Health/Diseases%20and%20Conditions/M-P/opioids/Documents/Standing%20Order_Public_002-2017.pdf
- 10.Pennsylvania Department of Health Bureau of Emergency Medical Services. Pennsylvania Statewide Basic Life Support Protocols. By Barishansky Raphael M. and Dr. Kupas Douglas F.. Retrived from http://www.health.pa.gov/My%20Health/Emergency%20Medical%20Services/EMS%20Statewide%20Protocol/Documents/FINAL%202017%20BLS%20PROTOCOL.pdf
- 11.United States Census Bureau. (2015). Pennsylvania Zip Code Tabulation Area. Retrieved from https://factfinder.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh=t
- 12.Wheeler E, Jones TS, Gilbert MK, Davidson PJ; Centers for Disease Control and Prevention (CDC). Opioid Overdose Prevention Programs Providing Naloxone to Laypersons - United States, 2014. MMWR Morb Mortal Wkly Rep. 2015. June [PMC free article] [PubMed] [Google Scholar]
- 13.Hankins MS (2011). U.S. Patent Application No. 13/135,368 19;64(23):631–5. [Google Scholar]
- 14.Deakin CD, Shewry E, Gray HH. Public access defibrillation remains out of reach for most victims of out-of-hospital sudden cardiac arrest. Heart. 2014. April;100(8):619–23. [DOI] [PubMed] [Google Scholar]
- 15.Levy M (2016). Public Access Bleeding Control: Enhancing Local Resilience. Prehospital and Disaster Medicine,31(3), 235–236. [DOI] [PubMed] [Google Scholar]