Abstract
Objectives
Late-life disability is highly dynamic but within-person short-term fluctuations have not been assessed previously. We analyze how substantial such late-life disability fluctuations are and whether they are associated with time-to-death, long-term disability trajectories, frailty, and sociodemographics.
Methods
Monthly survey data (Precipitating Events Project Study) on activities of daily living/instrumental activities of daily living (ADL/IADL) disability (0–9) in the last years of life from 642 deceased respondents providing 56,308 observations were analyzed with a two-step approach. Observation-level residuals extracted from a Poisson mixed regression model (first step), which depict vertical short-term fluctuations from individual long-term trajectories, were analyzed with a linear mixed regression model (second step).
Results
Short-term disability fluctuations amounted to about one ADL/IADL limitation, increased in the last 4 years of life, and were closely associated with disability increases. Associations with frailty or sociodemographics characteristics were absent except for living alone.
Discussion
Short-term disability fluctuations in late life were substantial, were linked to mortality-related processes, and represent a concomitant feature of disability increases in late life.
Keywords: Disability, Health disparities, Intraindividual variability, Longitudinal methods, Short-term fluctuations
Disability, defined as the need for personal assistance with daily activities essential for self-care and independent living (Fried, Ferrucci, Darer, Williamson, & Anderson, 2004), increases with age and thus represents a concern against the background of population aging. In contrast to the notion of old-age disability as a one-way progressive condition, it has been shown that late-life disability is highly dynamic (Boyd et al., 2009; Gill, Gahbauer, Han, & Allore, 2010; Gill, Hardy, & Williams, 2002; Verbrugge, Reoma, & Gruber-Baldini, 1994). Results from the Precipitating Events Project (PEP Study), for example, showed that a majority of disability episodes were brief (1–2 months), followed by recovery to independence, and often recurrent (Gill et al., 2002; Hardy, Dubin, Holford, & Gill, 2005; Hardy & Gill, 2004). Disability dynamics are often analyzed based on discrete transitions between a limited number of predefined categorical states (eg, none/light/severe disability) using multistate models (Hardy et al., 2005). This approach, however, ignores more gradual dynamics within broad categories, renders analyses complex as the number of states and transitions increases, and does not quantify the amplitude of disability dynamics. The principal alternative to evaluating disability dynamics is analyzing trajectories based on continuous disability measures with mixed models (Gill, Gahbauer, Han, & Allore, 2010; Taylor, 2010). Such analyses, however, focus on (groups of) long-term disability trajectories whereas short-term disability dynamics within individuals are smoothed over and relegated to the sphere of residual error and statistical noise.
Recently, Lin and Kelley-Moore (2017) found that intraindividual variability in functional limitations—which are antecedents of disability (Verbrugge & Jette, 1994)—increases with age and exhibits a social patterning: women, ethnic minorities and those with low socioeconomic status reported not only lower but also more unstable functioning. However, this study was based on biannual data and thus likely missed a considerable amount of short-term dynamics (Gill et al., 2002).
In this analysis, we were interested in short-term disability fluctuations, that is, the sum of reversible vertical ups and downs fluctuating around a person’s long-term disability trajectory (Figure 1). Such fluctuations may occur in the setting of illnesses or injuries leading to hospitalizations or restricted activity with subsequent recoveries and resolutions (Gill, Allore, Gahbauer, & Murphy, 2010) or could reflect frailty-related “unstable disability” (Campbell & Buchner, 1997). Time-unstructured (Ram & Gerstorf, 2009) short-term disability fluctuations—a hitherto neglected aspect of health dynamics—could add to our understanding of late-life disability and act as an indicator of future health deterioration. Furthermore, unrecognized substantial short-term fluctuations may render disability measurements with long intervals unreliable (Gill et al., 2002) and may lead to inflated estimates of late-life interindividual heterogeneity (Lin & Kelley-Moore, 2017). However, it is currently unclear how substantial late-life disability fluctuations are, and whether they represent mostly measurement error and random noise, or whether they are associated with time-to-death, long-term disability trajectories, frailty, and sociodemographic conditions related to disability (Fried et al., 2004; Taylor, 2010). To address these questions, we model monthly disability measurements during the last years of life to assess the amplitude of short-term disability fluctuations as well as its determinants.
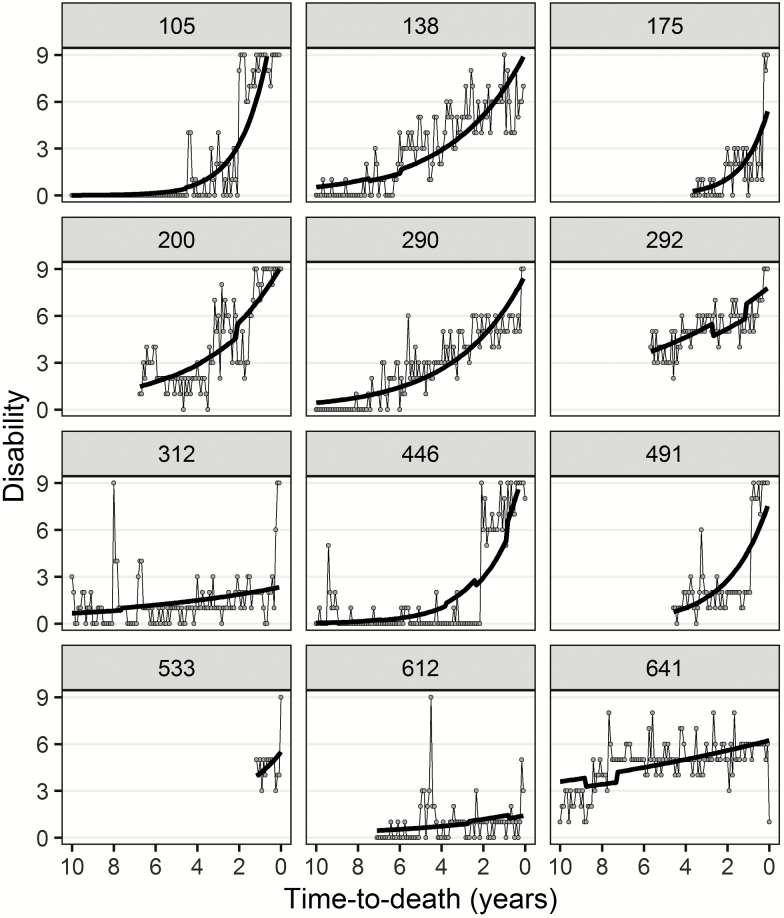
Figure 1.
Long-term disability trajectories and short-term fluctuations in disability in the last 10 years of life for 12 random respondents. Disability is scored as 0–9 based on need for personal assistance (no/yes) in four activities of daily living (ADLs) and five instrumental activities of daily living (IADLs). Thick lines show fitted disability values (fixed and random effects) from model 1 (Poisson mixed model), dots represent actual observations, which are connected by thin lines. The vertical difference between actual observations and subject-specific long-term disability trajectories reflects observation-level residuals. Breaks in the fitted disability trajectories are due to frailty and living alone, which are time-varying predictor variables. Numbers in the header refer to respondent’s ID. Depending on how many observations respondents provided before death (minimum = 6), time-to-death varies up to a maximum of 10 years before death.
Method
Data
The PEP Study provides monthly disability assessments by telephone and home-based assessments at 18-months intervals for 754 health plan members 70+ in greater New Haven, Connecticut. For more details, see Gill (2014) and the Supplementary File. As of November 2018, 677 (91.2%) respondents had died, as determined from local obituaries and informants (100% completion rate). We used disability measurements from the last (up to 10) years of life from decedents, who did not withdraw permanently from the study before death and who provided at least six monthly observations. This amounted to a total of 642 deceased participants and 56,308 monthly observations. When respondents were unable to answer, highly concordant proxy-respondents (Gill et al., 2002), which accounted for 20.9% of the total observations, provided information.
Variables
Disability (range = 0–9) was measured with an ADL/IADL aggregate index (Spector & Fleishman, 1998) based on the need for personal assistance (no = 0, yes = 1) in four activities of daily living (ADLs: bathing, dressing, walking inside the house, transferring from a chair) and five instrumental activities of daily living (IADLs: shopping, housework, meal preparation, taking medications, managing finances).
Predictor variables included time-to-death in years (0–10), sociodemographics (men/women, <12/≥12 years of education, white/non-white ethnicity, living not alone/alone), and physical frailty (no/yes, for details see Gill, Gahbauer, Allore, and Han (2006)). Control variables included age at death (<80/80–89/90+ years) and the number of monthly interviews (6–121).
Statistical Analysis
In a first step, we assessed long-term disability trajectories with a Poisson mixed regression model. We used time-to-death as metric as this avoids implicit imputation after death (Kurland, Johnson, Egleston, & Diehr, 2009) and provides a better characterization of late-life health decline than age (Gerstorf, Ram, Lindenberger, & Smith, 2013). In a second step, we extracted observation-level residuals (Lin & Kelley-Moore, 2017), which represent the vertical deviations from the individual-specific trajectories comprised of random intercept and slope (time-to-death) effects. To assess short-term disability fluctuations, the absolute values of observation-level residuals were evaluated with a linear mixed regression model using the log-link function due to skewness. Estimates of individual-level random intercept and slope from the first model were used as additional predictors in the second model. We used a Bayesian estimation procedure via package brms (Bürkner, 2017), a front-end for Stan (Stan Development Team, 2018) in R: A language and environment for statistical computing (R Core Team, 2018).
Results
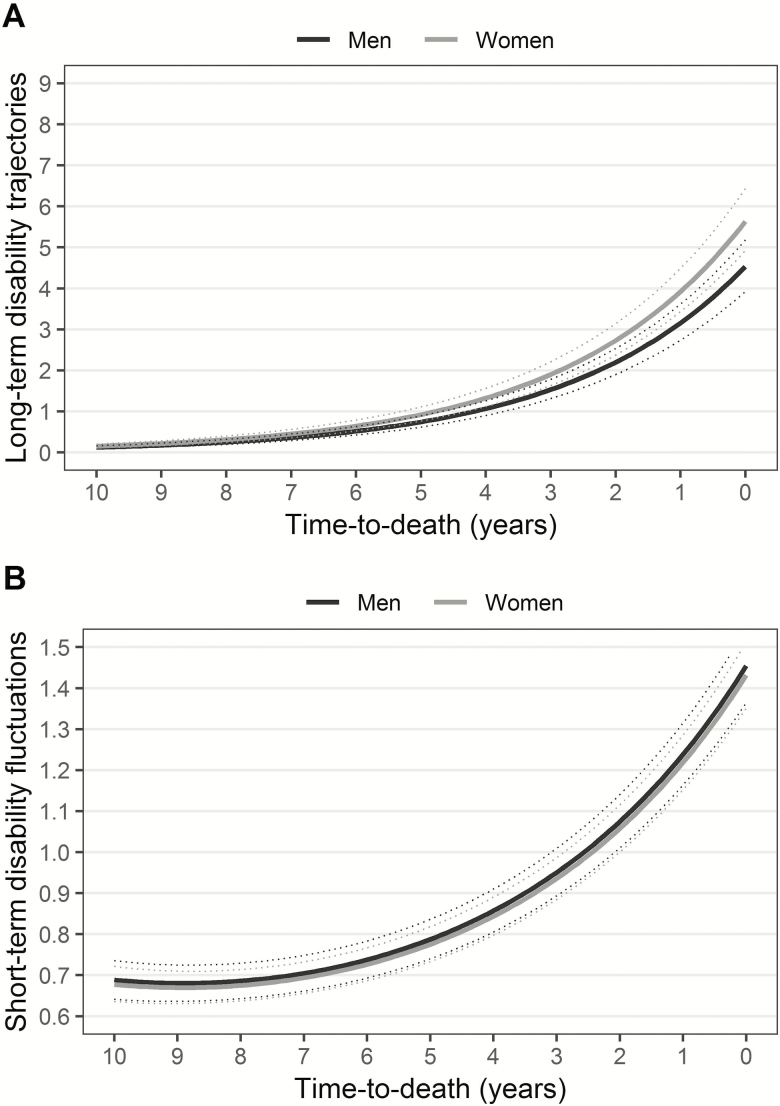
63.1% of the respondents were women and mean age at baseline was 78.8 years (SD = 5.2, range = 70–96). Average age at death was 86.5 for men and 87.1 for women. Figure 1 shows fitted individual long-term disability trajectories and actual observations for randomly selected respondents, which illustrates short-term disability fluctuations. Figure 2A shows the average long-term disability trajectory, indicating a notable increase in the last 4 years of life, with a steeper increase in women than men. Predictor variables showed the expected associations with disability levels (left panel, Table 1) and were able to explain 30% of the variance. Absolute values of observation-level residuals were sizeable (M = 1.0, SD = 1.0, skew = 2.1) with 12.8% >2 ADLs/IADLs. Parallel to disability levels, the amplitude of disability fluctuations increased in the last 4 years of life (Figure 2B). Those with higher mean disability levels (+1SD = 47%) and steeper long-term disability trajectories (+1SD=+361%) showed considerably more short-term fluctuations (right panel, Table 1). No effects were found for frailty or sociodemographics, but those who lived alone had higher fluctuations (+22%). Predictors accounted for 10% of the variance in short-term disability fluctuations.
Figure 2.
Mean long-term disability trajectories (A) and mean amplitude of short-term fluctuations (B) in the last 10 years of life for men and women. Thick lines show fitted disability values based on the fixed effects only, thin lines represent 95% credible intervals.
Table 1.
Predictors of Long-Term Disability Trajectories and Short-Term Disability Fluctuations in the Last 10 Years of Life
| Long-term disability trajectories log(b (95 CI)) | Short-term disability fluctuations log(b (95 CI)) | |
|---|---|---|
| Population-level (fixed) effects | ||
| Intercept | 0.07 (–0.07, 0.23) | –0.18 (–0.23, –0.13) |
| Time-to-death (years) | 0.36 (0.34, 0.39) | 0.09 (0.08, 0.09) |
| Time-to-death2 (years) | — | 0.01 (0.01, 0.01) |
| Female | 0.22 (0.09, 0.34) | –0.02 (–0.07, 0.04) |
| Low education | 0.15 (0.02, 0.27) | –0.00 (–0.06, 0.06) |
| Non-white ethnicity | 0.07 (–0.13, 0.27) | 0.03 (–0.12, 0.06) |
| Living alone | 0.01 (–0.04, 0.01) | 0.20 (0.17, 0.22) |
| Frailty | 0.16 (0.14, 0.18) | –0.00 (–0.03, 0.02) |
| Long-term mean disability level | — | 0.39 (0.35, 0.43) |
| Long-term disability increase | — | 1.28 (1.10, 1.46) |
| Individual-level (random) effects | ||
| SD Intercept | 1.57 (1.45, 1.71) | 0.31 (0.29, 0.33) |
| SD time-to-death | 0.34 (0.31, 0.37) | — |
| COR | –0.88 (–0.90, –0.85) | — |
| Model fit | ||
| WAIC | 213,580.8 | 183,219.2 |
| R 2 | 0.30 (0.27, 0.33) | 0.10 (0.09, 0.11) |
Note. PEP Study, N-observations = 56,308, N-individuals = 642, unweighted data. Reported effects (b) are unstandardized and on the log scale. Models adjusted for age at death and number of interviews. Quadratic growth curves were tested but improved model fit only for the model of short-term disability fluctuations. Inference is based on a Hamiltonian Monte Carlo (HMC) sampler with a no-U-turn sampler (NUTS). Convergence of four chains with each 5,000 iterations (1,000 iterations warm-up) under weakly information priors was confirmed by inspection of trace-plots and Rˆ < 1.1 for all parameters. Neffective> 100 for all parameters. Abbreviations: 95 CI = 95% credible intervals, SD = standard deviation, COR = correlation between random effects, WAIC = Watanabe Akaike information criterion, R2 = explained variance based on fixed effects.
Discussion
In this study, we found short-term fluctuations in late-life disability of about one ADL/IADL limitation on average (on nine-point scale), which is substantial relative to mean long-term disability trajectories and the sex difference therein. Given the size, the nature of these fluctuations requires closer inspection.
Observation-level residuals could foremost reflect measurement error. For example, differences in the self-reported disability level based on monthly telephone interviews could be due to variation in the interpretation of the meaning of “do you need help” based on day-to-day variations in affective well-being or gradual activity modification, that is, variation in the “how,”, “how long,” and “how often” of an activity and the details of what “help” entails. However, we consider it unlikely that random measurement error is the main source of the found short-term fluctuations because (a) fluctuations were not constant but increased over time; (b) the retest reliability of the disability measure was substantial (Gill et al., 2002); and (c) ADL/IADL measures have been shown to reflect objective measures of functioning well (Bravell, Zarit, & Johansson, 2011).
Thus, we consider the measured short-term fluctuations to be depictions of actual ADL/IADL limitations reflecting the highly dynamic within-person characteristic that is late-life disability (Boyd et al., 2009; Gill, 2014; Gill et al., 2002; Hardy et al., 2005; Hardy & Gill, 2004; Verbrugge et al., 1994). The question then is whether these fluctuations show predictable systematic patterns. We found that time-to-death, disability level and increases therein were predictors of short-term disability fluctuations, which is likely a consequence of age-related but particularly mortality-related processes in late life. These processes result in progressive physiological instability in the setting of intervention efforts (Verbrugge et al., 1994) leading to temporary recoveries and resolutions. Physiological instability may manifest in repeated spells of activity restrictions at the end of life, for example, due to fatigue, pain, and infections (Chaudhry et al., 2013), but also in an increased likelihood for serious illnesses or injuries leading to hospitalization, which again increases the likelihood of increased disability levels (Gill, Murphy, Gahbauer, & Allore, 2013) and short-term disability fluctuations (Verbrugge et al., 1994). The strong impact of long-term increases in disability on short-term disability fluctuations implies that older adults do not lose the ability to perform ADLs/IADLs in a gradual manner, but that this process is accompanied by increasing performance fluctuations, a little-recognized facet of late-life vulnerability. This implies that disability measurement in late life for both research and clinical purposes should be based on short-time intervals to capture disability levels accurately (Gill et al., 2002).
Our results of increasing ADL/IADL disability fluctuations in late life are in line with the age- and mortality-related increases in intraindividual variability in functional limitations reported by Lin and Kelley-Moore (2017). It is unclear though whether fluctuations in functional limitations and disability are directly related as implied by the disablement process (Verbrugge & Jette, 1994). A study on weekly fluctuations in physical functioning and ADL-disability showed only a weak association between these constructs (Mendes de Leon, Guralnik, & Bandeen-Roche, 2002). In contrast to Lin and Kelley-Moore (2017), we found no support for sociodemographic predictors (gender, education, ethnicity) of short-term disability fluctuations, which could be due to the different data sets used, specifically with regard to the outcomes (functional limitations vs disability), representativity (national vs regional sample), and temporal resolution (biannual vs monthly assessments). Finally, increased disability fluctuations among those who lived alone could reflect more unstable health due to the lack of compensating comprehensive daily care provided by cohabiting family members, which might both aid in the prevention of and recovery from illnesses and injuries.
This is the first analysis of both short-term disability fluctuations and long-term disability trajectories. Further strengths of this analysis include a low rate of missing data and loss-to-follow-up, high proxy-respondent reliability, and monthly assessments. However, relevant disability fluctuations might occur on an even shorter time-scale, that is, as day-to-day or week-to-week fluctuations. To measure both long- and short-term changes in disability, future studies could make use of measurement-burst designs (Ram & Gerstorf, 2009). Finally, future research should also rely on objective rather than subjective measures to minimize measurement error as the potential source of fluctuations and should assess the relevance of short-term disability fluctuations as a prognostic factor with regard to long-term disability trajectories, institutionalization, and mortality.
Conclusion
In conclusion, we have shown that short-term disability fluctuations in late life are neither small nor exclusively random. These fluctuations increase toward the end of life in parallel with increases in disability severity. Further research is required to assess the relevance of short-term disability fluctuations.
Funding
This work was supported by a grant from the National Institute on Aging (R01AG17560). Dr. Gill is the recipient of an Academic Leadership Award (K07AG043587) from the National Institute on Aging and is supported by the Yale Claude D. Pepper Older Americans Independence Center (P30AG21342).
Supplementary Material
Acknowledgments
E.S. planned the study, performed all statistical analysis, and wrote the article. T.G. contributed to the planning of the study, provided access to the data, and critically reviewed the manuscript. H.M. contributed to the methodological approach and critically reviewed the manuscript. W.F. supervised the analysis, contributed to the planning of the study and critically reviewed the article. We thank Denise Shepard, Andrea Benjamin, Barbara Foster, and Amy Shelton for assistance with data collection; Wanda Carr, Geraldine Hawthorne, and Evelyne A. Gahbauer for assistance with data entry and data management; Peter Charpentier for design and development of the study database and participant tracking system; and Joanne McGloin for leadership and advice as the Project Director.
Conflict of Interest
The authors declare that there is no conflict of interest.
References
- Boyd C. M., Ricks M., Fried L. P., Guralnik J. M., Xue Q. L., Xia J., & Bandeen-Roche K (2009). Functional decline and recovery of activities of daily living in hospitalized, disabled older women: The Women’s Health and Aging study I. Journal of the American Geriatrics Society, 57, 1757–1766. doi: 10.1111/j.1532-5415.2009.02455.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bravell M. E., Zarit S. H., & Johansson B (2011). Self-reported activities of daily living and performance-based functional ability: A study of congruence among the oldest old. European Journal of Ageing, 8, 199–209. doi: 10.1007/s10433-011-0192-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bürkner P-C. (2017). Brms: An R package for Bayesian multilevel models using stan (Version 2.6.0). Journal of Statistical Software 80, 1–28. doi: 10.18637/jss.v080.i01 [DOI] [Google Scholar]
- Campbell A. J., & Buchner D. M (1997). Unstable disability and the fluctuations of frailty. Age and Ageing, 26, 315–318. doi: 10.1093/ageing/26.4.315 [DOI] [PubMed] [Google Scholar]
- Chaudhry S. I., Murphy T. E., Gahbauer E., Sussman L. S., Allore H. G., & Gill T (2013). Restricting symptoms in the last year of life: A prospective cohort study. JAMA Internal Medicine, 173, 1534–1540. doi: 10.1001/jamainternmed.2013.8732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried L. P., Ferrucci L., Darer J., Williamson J. D., & Anderson G (2004). Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 59, 255–263. doi: 10.1093/gerona/59.3.m255 [DOI] [PubMed] [Google Scholar]
- Gerstorf D., Ram N., Lindenberger U., & Smith J (2013). Age and time-to-death trajectories of change in indicators of cognitive, sensory, physical, health, social, and self-related functions. Developmental Psychology, 49, 1805–1821. doi: 10.1037/a0031340 [DOI] [PubMed] [Google Scholar]
- Gill T. (2014). Disentangling the disabling process: Insights from the precipitating events project. The Gerontologist, 54, 533–549. doi: 10.1093/geront/gnu067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gill T., Allore H. G., Gahbauer E. A., & Murphy T. E (2010). Change in disability after hospitalization or restricted activity in older persons. JAMA, 304, 1919–1928. doi: 10.1001/jama.2010.1568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gill T. M., Gahbauer E. A., Allore H. G., & Han L (2006). Transitions between frailty states among community-living older persons. Archives of Internal Medicine, 166, 418–423. doi: 10.1001/archinte.166.4.418 [DOI] [PubMed] [Google Scholar]
- Gill T. M., Gahbauer E. A., Han L., & Allore H. G (2010). Trajectories of disability in the last year of life. New England Journal of Medicine, 362, 1173–1180. doi: 10.1056/NEJMoa0909087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gill T. M., Hardy S. E., & Williams C. S (2002). Underestimation of disability in community-living older persons. Journal of the American Geriatrics Society, 50, 1492–1497. doi: 10.1046/j.1532-5415.2002.50403.x [DOI] [PubMed] [Google Scholar]
- Gill T. M., Murphy T. E., Gahbauer E. A., & Allore H. G (2013). Association of injurious falls with disability outcomes and nursing home admissions in community-living older persons. American Journal of Epidemiology, 178, 418–425. doi: 10.1093/aje/kws554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardy S. E., Dubin J. A., Holford T. R., & Gill T. M (2005). Transitions between states of disability and independence among older persons. American Journal of Epidemiology, 161, 575–584. doi: 10.1093/aje/kwi083 [DOI] [PubMed] [Google Scholar]
- Hardy S. E., & Gill T. M (2004). Recovery from disability among community-dwelling older persons. JAMA, 291, 1596–1602. doi: 10.1001/jama.291.13.1596 [DOI] [PubMed] [Google Scholar]
- Kurland B. F., Johnson L. L., Egleston B. L., & Diehr P. H (2009). Longitudinal data with follow-up truncated by death: match the analysis method to research aims. Statistical Science: A Review Journal of the Institute of Mathematical Statistics, 24, 211. doi: 10.1214/09-STS293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin J., & Kelley-Moore J. A (2017). From noise to signal: the age and social patterning of intra-individual variability in late-life health. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 72, 168–179. doi: 10.1093/geronb/gbv081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendes de Leon C. F., Guralnik J. M., & Bandeen-Roche K (2002). Short-term change in physical function and disability: The Women’s Health and Aging study. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 57, S355–365. doi: 10.1093/geronb/57.6.S355 [DOI] [PubMed] [Google Scholar]
- Ram N., & Gerstorf D (2009). Time-structured and net intraindividual variability: tools for examining the development of dynamic characteristics and processes. Psychology and Aging, 24, 778–791. doi: 10.1037/a0017915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team (2018). R: A language and environment for statistical computing (Version 3.5.1). Vienna, Austria: R Foundation for Statistical Computing. [Google Scholar]
- Spector W. D., & Fleishman J. A (1998). Combining activities of daily living with instrumental activities of daily living to measure functional disability. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 53, S46–S57. doi: 10.1093/geronb/53b.1.s46 [DOI] [PubMed] [Google Scholar]
- Stan Development Team (2018). RStan: The R interface to Stan (Version2.18.2) Retrieved from https://mc-stan.org/users/citations/. [Google Scholar]
- Taylor M. G. (2010). Capturing transitions and trajectories: The role of socioeconomic status in later life disability. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 65, 733–743. doi: 10.1093/geronb/gbq018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbrugge L. M., & Jette A. M (1994). The disablement process. Social Science & Medicine (1982), 38, 1–14. doi: 10.1016/0277-9536(94)90294-1 [DOI] [PubMed] [Google Scholar]
- Verbrugge L. M., Reoma J. M., & Gruber-Baldini A. L (1994). Short-term dynamics of disability and well-being. Journal of Health and Social Behavior, 35, 97–117. doi: 10.2307/2137359 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.