Abstract
Mechanical loading is essential for the maintenance of musculoskeletal homeostasis. Cartilage has been demonstrated to be highly mechanoresponsive, but the mechanisms by which chondrocytes respond to mechanical stimuli are not clearly understood. The goal of the study was to determine how LRP4, LRP5, and LRP6 within canonical Wnt-signaling are regulated in simulated microgravity and cyclic hydrostatic pressure, and to investigate the potential role of LRP 4/5/6 in cartilage degeneration. Rat chondrosacroma cell (RCS) pellets were stimulated using either cyclic hydrostatic pressure (1Hz, 7.5 MPa, 4hr/day) or simulated microgravity in a rotating wall vessel (RWV) bioreactor (11RPM, 24hr/day). LRP4/5/6 mRNA expression was assessed by RT-qPCR and LRP5 protein expression was determined by fluorescent immunostaining. To further evaluate our in vitro findings in vivo, mice were subjected to hindlimb suspension for 14 days and the femoral heads stained for LRP5 expression. We found that, in vitro, LRP4/5/6 mRNA expression is modulated in a time-dependent manner by mechanical stimulation. Additionally, LRP5 protein expression is upregulated in response to both simulated microgravity and cyclic hydrostatic pressure. LRP5 is also upregulated in vivo in the articular cartilage of hindlimb suspended mice. This is the first study to examine how LRP4/5/6, critical receptors within musculoskeletal biology, respond to mechanical stimulation. Further elucidation of this mechanism could provide significant clinical benefit for the identification of pharmaceutical targets for the maintenance of cartilage health.
Introduction
Mechanical loading is essential for the maintenance of musculoskeletal homeostasis. It is well known that mechanical loading stimulates bone formation but the absence of loading, such as in patients on prolonged bed-rest or astronauts on long-term space missions, leads to loss of bone mass [1–3] and skeletal muscle [4,5]. Cartilage has also been demonstrated to be highly mechanoresponsive. Similar to bone, insufficient loading can lead to cartilage degeneration. Patients on bed-rest experience loss of cartilage thickness after only 14 days [6]; and, muscle weakness has been associated with the progression of osteoarthritis [7,8]. However, excessive repetitive loading has been associated with chondrocyte death and cartilage degeneration [9,10]. Obesity is recognized as a major risk factor for osteoarthritis, in part due to increased axial loading patterns on the hip and knee joints [11]. Other studies suggest that moderate loading patterns from normal daily activities such as walking promote cartilage health [12–14]. The responses and the mechanisms by which chondrocytes respond to mechanical stimuli remains an active area of investigation.
The effects of mechanical loading and unloading on cartilage biology have been studied via hydrostatic pressure [15–18] and simulated microgravity [19–22], respectively. Cyclic hydrostatic pressure within physiologic magnitudes (<10 MPa) has been demonstrated to promote cartilage matrix deposition [15] and chondrogenesis in human bone-marrow derived mesenchymal stem cells [23–26] and human adipose-derived stem cells [22,27–29]. Cyclic hydrostatic pressure mimics physiologic loading patterns, which are necessary to prevent cartilage degeneration from disuse [12]. Simulated microgravity has been used to study chondrocytes and chondrogenesis in unloaded conditions [19–22]. Simulated microgravity can be produced by rotating wall vessel (RWV) bioreactors developed by NASA, which rotate at a constant speed to maintain pellets in free-fall resulting in a randomized gravitational vector [30]. The forces generated by this vessel produce vector-averaged forces comparable with that of near-earth free fall orbit [30,31]. Currently, however, it is unclear whether simulated microgravity promotes [19] or inhibits [20,22] cartilage matrix synthesis. In vivo, the hindlimb suspension rodent model was developed to mimic the microgravity environment experienced during space flight [32]. This model allows for preliminary studies to be carried out on Earth without taxing the limited resources available for spaceflight experimentation. While hindlimb suspension studies have primarily focused on bone-related research, recently hindlimb suspension was demonstrated to protect against articular cartilage degeneration in a rat osteoarthritis model [33]. Current literature clearly demonstrates that mechanical stimulation modulates cartilage biology, however the mechanisms by which cyclic hydrostatic pressure and simulated microgravity modulate chondrocytes need to be further elucidated.
Cartilage and bone are developmentally linked through processes such as endochondral ossification and share common signaling pathways including canonical Wnt-signaling. In active Wnt-signaling, Wnts bind to the frizzled and low-density lipoprotein receptor-related protein (LRP) co-receptors. This activates a signaling cascade, preventing β-catenin from degrading within the cytoplasm, thus allowing β-catenin to translocate and accumulate within the nucleus [34]. Nuclear β-catenin initiates the transcription of many genes responsible for bone and cartilage homeostasis [34–36]. LRP receptors are well known to be major mediators of musculoskeletal homeostasis. LRP5 and LRP6, specifically, are critical for transduction of canonical Wnt-signaling [35]. In bone, LRP5/6 receptors have been shown to be essential for maintaining balance between bone formation and resorption [3]. LRP receptors are also important for signaling in cartilage and, as in bone, have been indicated to transduce Wnt signaling and induce nuclear β-catenin localization. LRP5 has been found to be upregulated in osteoarthritis [37]. However, LRP6 loss-of-function mutation has been associated with an increased progression of osteoarthritis [38]. LRP4 has been implicated in regulation of Wnt-signaling, and has been reported to induce extracellular matrix production in cartilage [39]. However, the exact mechanism by which LRP4 acts within cartilage biology remains elusive, as it appears to have a role distinct from LRP5/6. In the context of mechanobiology, it has been demonstrated that tensile strain and Wnt3a act synergistically to activate Wnt signaling and trigger genes associated with cartilage catabolism [40]. Chondrocyte response to mechanical loading has been shown to be dependent on Wnt-signaling [41]. Furthermore, Wnt-signaling has been demonstrated to be activated following mechanical injury of cartilage [42]. However, it is currently unclear how LRP receptors respond to mechanical stimulation.
The goal of this study was to determine if, and to what extent, LRP receptors are regulated in simulated microgravity and cyclic hydrostatic pressure in order to elucidate the mechanisms by which mechanical stimulation regulates cartilage homeostasis. Since canonical Wnt-signaling and LRPs are involved in the maintenance of bone homeostasis and LRPs have been associated with cartilage pathologies, we hypothesized that LRP expression is responsive to these mechanical stimuli.
Materials and methods
Rat chondrosarcoma cell culture
Rat chondrosarcoma cells (RCS), which are a cell line derived from Swarm rat chondrosarcoma [43] were sent to us from collaborators at Boise State University who specialize in RCS culture (see acknowledgements). This cell type has been used extensively to study cartilage and cartilage matrix biology [44–46] and has been used to study chondrocyte response to mechanical stimulation [47]. RCS were cultured in Dulbecco's Modified Eagle Medium (DMEM) supplemented with 10% v/v fetal bovine serum, 100 units/ml penicillin, and 100 μg/ml streptomycin (RCS media). When pellet culture was utilized, RCS were resuspended at a density of 250,000 cells per pellet in 15 ml conical tubes. The RCS were centrifuged at 300 g for 5 min to form a pellet, and incubated for 2 days with loose tube caps in order for the cell pellets to coalesce.
Stimulation in simulated microgravity and cyclic hydrostatic pressure
Pellets were subjected to either simulated microgravity or cyclic hydrostatic pressure and compared to control pellets, which were continuously incubated at 37°C, 5% CO2 without mechanical stimulation. The intent of using cyclic hydrostatic pressure in this experiment was to mimic physiological loading on the chondrocytes. Simulated microgravity was achieved by culturing cell pellets in a RWV bioreactor. The RWV bioreactor was set to a speed of 11RPM and kept in a standard 37°C, 5% CO2 incubator for the full 14 days. Any air bubbles that accumulated within the vessel were removed daily.
For cyclic hydrostatic pressure stimulation, the pellets were placed in sterile heat-sealed bags with 10 ml of RCS media and loaded in a custom cyclic hydrostatic pressure system designed by our lab, as described previously [28,48]. Briefly, the heat-sealed bags were placed in a stainless steel pressure vessel (Parr Instruments, Moline, Illinois) filled with mineral oil. The pressure vessel was connected via high-pressure stainless steel tubing to a hydraulic cylinder mounted to an MTS 858 Mini Bionix II load frame. Loading operations were controlled using a MTS TestStar control program (MTS System Corp, Eden Prairie, MN). Loading was applied at a magnitude of 7.5 MPa and frequency of 1Hz, 4 hours per day for up to 14 days. After daily loading, the heat-sealed bags were removed from the apparatus and maintained in a standard incubator at 37°C. Pellets were transferred to new bags with fresh media every 3–4 days.
Mouse hindlimb suspension procedures
In order to further examine the effect of unloading in vivo, hindlimb suspension was used to unload the synovial joints of male C57BL/6J mice (Jackson Laboratories, Bar Harbor, ME) for 14 days. The protocol was performed in collaboration with the Penn State College of Medicine. All procedures were approved by the Penn State Institutional Animal Care and Use Committee (Protocol #2013–033) and were performed according to institutional guidelines. All mice in the study were randomly assigned to experimental groups. All the samples were analyzed blind; that is none of the investigators knew which experimental group a particular sample came from. All mice used were approximately 18 weeks old ± 5 days and thus skeletally mature on day 0 (start of experiment). WT mice weighed 30.7±0.2 grams and Sost KO weighed 31.0±0.3 grams at the start of experiment. There were four experimental groups and 8–9 mice per group for a total of 32–36 mice. The numbers were based on previous experiments demonstrating that 8 mice per group were sufficient to detect significant differences in micro architectural features at p<0.05. All mice in the study were randomly assigned to experimental groups. The order that the animals were treated and assessed was random and blinded. Sclerostin deficient male C57BL/6J mice (Sost-/-) were generated using a LacZ replacement of the sclerostin gene as described previously [49]. Mice were housed in standard enclosures modified for hindlimb suspension (2 mice/cage), with the room temperature at 25°C and on a 12-hour light/dark cycle. Corn cobb bedding with a wire floor above was used. The heath of the mice was assessed by Penn State Hershey veterinary staff prior to the study. During the study the health of the mice was assessed twice daily by Donahue Lab staff and daily by the veterinary staff at Penn State Hershey. Any health issues were immediately reported to the PI Dr. Donahue. Standard rodent 2018 Tekland Global 18% protein rodent diet (Harlan Laboratories Inc., Indianapolis, IN, USA) was provided ad libitum throughout the study. Mice were acclimated to the room used for hindlimb suspension for 1 week prior to study commencement. Hindlimb suspension mice were anesthetized and tape strips were secured to the tails. The tape allowed the animal to be attached to tethers that ran along the top of the cage. The tethers were adjusted to support the mouse at 30° of elevation. Ground control mice were kept in identical housing units without the tethers. After 14 days, mice were anesthetized with isoflurane (3% + oxygen) during final tissue collection, and then euthanized with isoflurane overdose (greater than 5% isoflurane concertation until 1 minute after breathing stops); confirmation of euthanasia was done via bilateral thoracotomy.
Immunofluorescence
After 14 days of culture, RCS pellets were fixed in 10% buffered formalin for 1 hour (n = 4 simulated microgravity, n = 3 control, n = 3 cyclic hydrostatic pressure). After fixation, gross pellet morphology was imaged on an EZ4D histology microscope (Leica, Wetzlar, Germany). In addition, mouse femoral heads from control and hindlimb suspension mice (n = 3 or greater for all groups) were fixed in formalin for 36 hours and decalcified in a solution of 2.5% EDTA in 0.2 M phosphate-buffer, pH 6.0, as described previously [50]. Fixed pellets and femoral heads were paraffin embedded and sectioned at the North Carolina State University College of Veterinary Medicine histology facilities. Sections were taken at a thickness of 10 μm from pellets and mouse femoral heads for immunofluorescent staining. Both pellet and femoral head sections were deparaffinized in SafeClear II (Thermo Fisher, Waltham, MA), hydrated in ethanol series, and treated with Antigen Retrieval Reagent-Universal (R&D Systems, Minneapolis, MN) following manufacturer’s protocol. The samples were then blocked with a 0.2% v/v Triton X-100/5.0% v/v BSA stock solution for 40 minutes.
Primary antibody dilutions were prepared in a PBS solution containing 0.2% v/v Triton X-100, and 0.5% v/v BSA. Pellets were incubated in goat polyclonal antibody to LRP5 (1:500 dilution, Abcam, Cambridge, United Kingdom) and mouse monoclonal antibody to active β-catenin (1:300 dilution, Millipore, Billerica, MA). The mouse femoral head sections were incubated in a goat polyclonal antibody to LRP5 solution (1:500 dilution). Sections were incubated overnight at 4°C in the primary antibody solution and then rinsed three times in PBS. Secondary antibody solutions were prepared using chicken anti-mouse Alexa Fluor 488 (1:1000 dilution, Molecular Probes, Eugene, Oregon), donkey anti-goat 594 (1:1000 dilution, Molecular Probes), and DAPI (1:1000, Molecular Probes, Eugene, Oregon). The samples were incubated in secondary antibody solutions for one hour at room temperature followed by three more PBS washes. Prolong Gold Mounting Media (Molecular Probes, Eugene, Oregon) was used to mount coverslips on the slides. The slides were dried in the dark for 24 hours and imaged on a Leica DM5500B Fluorescent Microscope using the compatible LAS-AF software.
Application of Wnt-regulating treatments
In order to determine if sclerostin levels alter LRP expression in RCS cells, RCS cells were cultured in RCS medium supplemented with recombinant sclerostin protein (R&D Systems, Minneapolis, MN). RCS were seeded at a density of 375,000 cells per well in standard six well plates and were incubated for 24 hours in RCS media. Media formulations were then switched to contain 25ng/ml, 100ng/ml, or 250ng/ml sclerostin protein and cultured for an additional 48 hours (n = 3 per condition).
Total RNA extraction and RT-PCR
PCR was used to evaluate LRP expression after 3, 7, 10, and 14 days of exposure to simulated microgravity, cyclic hydrostatic pressure, or six-well plate control and after sclerostin stimulation experiments described above (n = 3 per condition). RNA extraction was carried out using a Trizol (Invitrogen, Carlsbad, CA) extraction method following the manufacturer’s protocol. RNA concentration and quality were assessed using a NanoDrop spectrophotometer (Thermo Scientific, Wilmington, DE). RNA was reverse-transcribed using Marligen’s First-strand cDNA Synthesis System (Origene, Rockville, MD). RT-PCR was performed with an ABI Prism 7000 system (Applied Biosystems, Carlsbad, CA) using SYBR Green (Life Technologies, Grand Island, NY) for fluorescent detection. Primers were designed using the Integrated DNA Technologies (Coralville, IA) website. RT-PCR data were analyzed using the 2-ΔΔCT method [51] and 18s was used as the housekeeping control. Primer sequences used were: 18s 5’AAGACGAACCAGAGCGAAAG3’, 3’TCTATGGCAGCATCAAGGCT5’; LRP4 5’GCAGCAAGAGGAAGGTACTAAT3’, 3’TCATAGGTTTCACGACTGGC5’; LRP5 5’CCATACAGGCCCTACATCATTC3’, 3’GATGGACCTGAACTTAAGCCTG5’; LRP6 5’GGGAGAAGTGCCAAAGATAGAA3’, 3’CTAATACTCCTCGCCTTCGAA5’.
Statistical analyses
All gene expression data sets were analyzed in Statistical Package for the Social Science (IBM SPSS Statistics, North Castle, NY). Data were analyzed using Tukey test with p-values less than 0.05 considered statistically significant. All data are presented as averages with error bars representing standard error of the mean. All experiments were carried out with n = 3 or greater. A connecting letters report was used to denote statistical significance, and in each graph, levels not connected by the same letter are significantly different (p<0.05).
Results
Pellet growth was modulated by mechanical stimulation
Gross examination of the pellets showed that pellets in simulated microgravity grew larger than those in control and cyclic hydrostatic pressure conditions after 14 days in culture (Fig 1). In addition, pellets stimulated via cyclic hydrostatic pressure and simulated microgravity developed into circular disks, but the control pellets were more irregular in shape.
Fig 1. Gross morphology of pellets.
Rat chondrosarcoma (RCS) pellets at day 14 in (A) simulated microgravity (11RPM, 24hrs/day) (B) control (six well plate, 37C, 5% CO2) and (C) cyclic hydrostatic pressure conditions (7.5 MPa, 1 Hz, 4 hrs/day) (Scale bars = 1mm).
LRP expression patterns are modulated by simulated microgravity and cyclic hydrostatic pressure
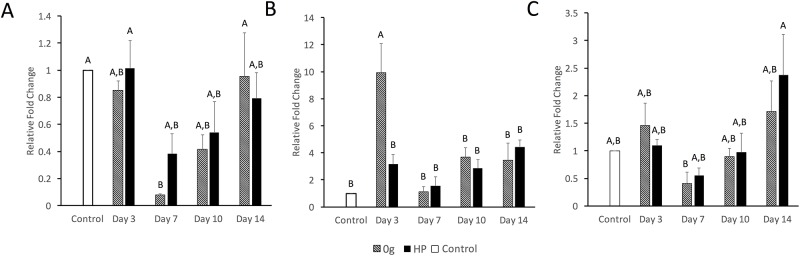
Expressions of LRP4, LRP5, and LRP6 in response to simulated microgravity or cyclic hydrostatic pressure were evaluated at days 3, 7, 10, and 14 via quantitative RT-PCR (Fig 2) relative to control pellets. LRP4 mRNA expression was significantly reduced at the day 7 in simulated microgravity. LRP6 mRNA exhibited a 2.4 fold expression elevation in cyclic hydrostatic pressure at day 14 relative to controls. LRP5 mRNA expression was significantly upregulated in simulated microgravity at day 3 (9.9 fold). In all cases, LRP4/5/6 expression was lower at 7 than at day 3.
Fig 2. Gene expression of LRP4/5/6 in response to mechanical stimuli.
Expression changes of (A) LRP4, (B) LRP5, and (C) LRP6 in response to simulated microgravity or cyclic hydrostatic pressure relative to unstimulated controls at days 3, 7, 10, and 14. All data was normalized to day 0 control data represented by the dashed line. Levels not connected by the same letter are significantly different (p<0.05).
Since LRP5 was the most highly upregulated LRP within our RT-PCR data and has been demonstrated to be the LRP receptor most responsible for Wnt-mediated osteoarthritic cartilage destruction [52], we next evaluated LRP5 protein-level changes within the Wnt-signaling pathway in response to cyclic hydrostatic pressure and simulated microgravity. 14-day RCS pellets were stained for LRP5 and β-catenin with an antibody that recognizes the active form of β-catenin dephosphorylated on Ser37 or Thr41 (Fig 3). Congruent with our mRNA results, LRP5 protein expression in RCS cells was elevated in response to both simulated microgravity and cyclic hydrostatic pressure when compared to the unstimulated controls. LRP5 expression was greater in response to cyclic hydrostatic pressure than simulated microgravity. Active β-catenin followed the same trend as LRP5 protein expression with highest expression in RCS cells exposed to cyclic hydrostatic pressure and lowest expression in the unstimulated controls. All RCS cells stained for LRP5 and active β-catenin to some extent, although the intensity was greater in the cells that had been subjected to mechanical stimulation. It should also be noted that cells that were stimulated via mechanical stimulation were larger in size than the unstimulated controls, which enhanced the overall appearance of LRP5 and active β-catenin expression.
Fig 3. Immunofluorescence of LRP5 and β-catenin in response to mechanical stimuli.
LRP5 and active β-catenin after 14 days of culture in simulated microgravity, unstimulated control (6-well plate, no loading) or cyclic hydrostatic pressure. All scale bars = 50 μm.
Because of the high LRP5 upregulation observed in both our RT-PCR and in vitro immunostaining assays, we tested whether LRP5 was also modulated in vivo. WT mice weighed 30.7±0.2 grams and Sost KO weighed 31.0±0.3 grams at the start of experiment. After two weeks of no hind limb suspension (HLS) control or HLS, WT control lost 1±0.2 grams body weight; WT HLS lost 4±0.2 grams; Sost KO lost 2.5±0.2 grams; and Sost KO HLS lost 6.7±1.0 grams. Microbiological status was not assessed. Mice did not receive drug treatment. There were no adverse events and there were no modifications to the experimental protocols made to reduce adverse events. For qualitative data, the staining was carried out in at least triplicate. We stained for LRP5 expression in the femoral heads of mice subjected to either normal loading or hindlimb suspension in both wild type mice and Sost-/- mice (Fig 4). In both wild type mice and Sost-/- mice LRP5 expression was elevated within the articular cartilage of mice subjected to hindlimb suspension relative to cartilage of the ground controls. No perceptible differences in LRP5 expression were observed between wild type and Sost-/- mice.
Fig 4. Immunofluorescence of LRP5 in response to hindlimb suspension.
LRP5 expression in the articular cartilage of mouse femoral heads after 14 days of hindlimb suspension. All scale bars = 100 μm.
Sclerostin modulates expression of LRP4 in a dose-dependent manner
To determine the effect of sclerostin on LRP expression, RCS pellets were cultured in the presence of 25ng/ml, 100ng/ml, or 250ng/ml of recombinant sclerostin. Interestingly, a dose-dependent effect was observed (Fig 5). Of the three LRPs tested, LRP4 was most responsive to sclerostin addition and exhibited a reduction (0.47 fold) in expression with the addition of 25ng/ml sclerostin (p<0.05). Higher LRP4 levels were observed when sclerostin concentrations were increased to 100ng/ml and 250ng/ml, with statistical significance observed between 25ng/ml and 250ng/ml (p<0.05). LRP5 and LRP6 were not significantly affected.
Fig 5. Gene expression of LRP4/5/6 in response to sclerostin.
Expression of (A) LRP4, (B) LRP5, and (C) LRP6 after 48 hours of exogenous sclerostin. All data were normalized to the control 0 ng/ml sclerostin data represented by the dashed line. Levels not connected by the same letter are significantly different (p<0.05).
Discussion
The objective of this study was to investigate how simulated microgravity and cyclic hydrostatic pressure modulate chondrocyte homeostasis, specifically focusing on the effects of these mechanical stimuli on LRP4/5/6 expression. The Wnt-signaling pathway has been previously demonstrated to be an important regulator of musculoskeletal mechanobiology. We hypothesized that LRP4/5/6 expression is modulated via mechanical stimuli in the form of cyclic hydrostatic pressure and simulated microgravity. Our in vitro data demonstrated that LRP4/5/6 are regulated by the mechanical stimuli evaluated in this study. A deeper proteomic look at LRP5 confirmed that LRP5 is upregulated in both simulated microgravity and cyclic hydrostatic pressure. In addition, LRP5 immunohistological staining intensity was greater in the articular cartilage of hindlimb suspended mice relative to articular cartilage of the ground controls in vivo. This is the first study to demonstrate the response of LRPs to mechanical stimulation in chondrocytes.
Varying pellet sizes were observed in response to the mechanical stimuli. Pellets maintained in simulated microgravity grew larger than pellets maintained in control or cyclic hydrostatic pressure conditions. This is consistent with previous studies that observed larger cartilage pellets or aggregates cultured in RWV bioreactors when compared to static controls, likely due to the dynamic laminar flow in rotating bioreactors and increased nutrient diffusion [53–55]. However, we previously tested the gene expression of human adipose derived stem cells cultured in microgravity, static culture or cyclic hydrostatic pressure, and found that aggrecan, sox9 and collagen II mRNA expression was upregulated in cyclic hydrostatic pressure, suggesting that simulated microgravity decreased chondrogenesis when compared to pellets cultured under cyclic hydrostatic pressure conditions [22]. These historic findings suggest that cells may divide more rapidly in rotating bioreactors, the chemical and mechanical properties of the end-product reflect native cartilage tissue more when cultured under hydrostatic pressure conditions.
LRP5 is necessary for skeletal mechanotransduction [56]. The trabecular bone of LRP5 knockout mice has greater sensitivity to disuse [57]. Previous reports on LRP5 mRNA expression in response to mechanical loading have been contradictory. Lau et al. demonstrated an upregulation of LRP5 mRNA in vitro in osteoblasts subjected to fluid shear and an upregulation of LRP5 mRNA in vivo in the tibia of mice subjected to a four-point bending exercise regimen [58]. However, Robinson et al. reported no change in LRP5 or LRP6 mRNA expression in vivo when mice were loaded using the same method [2]. To our knowledge, this study and our findings are the first to suggest that LRP5 is involved in cartilage mechanobiology. The role of LRP5 within cartilage has been controversial. LRP5 deletion has been found to increase cartilage degeneration in osteoarthritic mouse models [59]. However, activated Wnt signaling has been reported to have a catabolic effect on cartilage tissue and inhibition of Wnt signaling through sclerostin has been found to be chondroprotective [60]. Hence, it is expected that excessive LRP5 expression would lead to cartilage degeneration. Within this study, LRP5 expression was elevated in response to both cyclic hydrostatic pressure and simulated microgravity conditions. LRP6, a protein that has been reported to have at least a partially redundant role to LRP5 [61], followed the same trend. In vivo, a similar mechano-response was observed in our hindlimb suspension model. Suspended mice displayed an increase in articular cartilage LRP5 expression, which suggests that unloading conditions enhance Wnt-signaling transduction in cartilage.
In this study we also observed changes in LRP4 of RCS pellets when exposed to either two weeks of cyclic hydrostatic pressure or simulated microgravity. LRP4 expression decreased at day 7 and day 10 relative to the 0-day control and 3-day time point. While LRP4’s role within the Canonical Wnt-signaling pathway has yet to be fully elucidated, studies have implicated that LRP4 may act as a sink for Wnt antagonists such as sclerostin and Wise [62,63]. The observed repression of LRP4 at day 7 might be a protective response initiated by the cell to release more sclerostin and counteract the large spike in LRP5 expression observed at day 3. Further investigation is needed to fully elucidate LRP4’s role within cartilage mechanobiology.
In this study, we did not observe nuclear translocation of β-catenin in response to mechanical stimulation, but this is consistent with previous literature. Normal human chondrocytes demonstrated cytoplasmic localization after 3 hrs of cyclic hydrostatic pressure, and the nuclear localization of β-catenin in OA chondrocytes was reduced after cyclic hydrostatic pressure [64]. In a study that examined the synergistic effect of tensile strain and Wnt3a signaling on nuclear translocation of β-catenin it was reported that tensile strain did not trigger complete nuclear translocation of β-catenin, but Wnt3a did stimulate nuclear translocation of β-catenin [40]. When chondrocytes were stimulated with both tensile strain and Wnt3a only partial nuclear translocation of β-catenin was observed immediately following loading period. Once the chondrocytes stimulated with both tensile strain and Wnt3a were allowed to recover for four hours, many of the cells did exhibit nuclear translocation of β-catenin [40]. In the ATDC5 cell line it was demonstrated that the number of cells positive for nuclear β-catenin was dependent on the duration of stretch loading [65]. Taken together, the literature suggests there is likely a complex, time-dependent relationship between nuclear translocation of β-catenin and mechanical stimulation that is not fully understood and should be studied in further depth in future studies.
The observed changes in LRP expression could be caused directly by mechanical stimulation, indirectly by stimulation through another mechanoresponsive protein, or a combination of both. Here we examined how sclerostin, an antagonist of Wnt signaling, regulates LRP4/5/6 expression in cartilage. Sclerostin appears to be a major regulator of bone’s response to mechanical loading [66]. It acts by binding to the LRP5/6 receptors, effectively blocking the Wnt signaling from transducing intracellularly [66]. It has been shown that serum levels of sclerostin and DKK1, another Wnt-inhibitor, are elevated in patients on bed-rest [67,68]. Mechanical loading has been shown to reduce sclerostin expression, while unloading increases sclerostin expression in bone [69]. and the down regulation of sclerostin has been shown to be necessary for increased bone formation in response to mechanical loading [70]. Sclerostin has also been demonstrated to be upregulated in simulated microgravity in osteocytes and this upregulation has been shown to be cell autonomous in osteocytes and hence independent of endocrine or paracrine factors [71]. This is consistent with studies that have shown that mechanical unloading of bone increases sclerostin expression [72]. Additionally, sclerostin inhibition has been reported to prevent loss of bone due to unloading [72,73]. While sclerostin is unfavorable to bone density maintenance, it appears to act as a defense mechanism to modulate Wnt signaling and prevent excessive cartilage degradation [60].
In this study, we found that the addition of exogenous sclerostin to chondrocytes modulated LRP4 expression, but the modulation of LRP5/6 expression was not statistically significant. While lower concentrations of sclerostin were found to repress LRP4 expression, higher concentrations of sclerostin restored LRP4 expression patterns to non-treated levels, likely due to saturation. Sclerostin has been previously reported to repress LRP5 and LRP6 expression in ovine chondrocytes using the same range of sclerostin concentrations [60]. The discrepancy could potentially be because chondrocytes were used from different animal models, which may have different physiologic concentrations of sclerostin. Additionally, it has been well documented that rats and other small animal models have a greater intrinsic capacity to cartilage regeneration than large animal models [74,75], which suggests that altered mechanism may be observed between ovine and murine models. While small animal models, such as the hindlimb suspension model, may be useful for identifying mechanisms of interest, these data must be verified in large animal studies before the development of human pharmaceuticals can arise. In the current study, we also compared LRP5 staining between Sost-/- mice and wild type mice and observed similar staining patterns, which supports the modest changes in LRP5 expression observed with the addition of exogenous sclerostin in vitro. Nevertheless, results from this study suggest that sclerostin modulates LRP4 expression and, in conjunction with previous research showing that mechanical loading regulates sclerostin expression [67–69,71], changes in sclerostin expression in response to mechanical stimuli may still partially contribute to observed LRP expression patterns. Hence, sclerostin should be further evaluated as a pharmaceutical target for osteoarthritis treatment in the case of abnormal loading patterns experienced by patients on long-term bed rest or astronauts on long-term space missions.
A limitation of the present study is that the in vivo studies only examine two conditions: ground control and hindlimb suspension. Future studies should examine how supra-physiological loading regulates LRP receptors in vivo through the use of methods such as in vivo tibial compression. Another aspect that would be of interest to future studies would be further investigating if the observed changes in expression of LRP receptors lead to downstream effects within the Wnt-signaling pathway. Since LRP4/5/6 are receptors in the Wnt-signaling pathway [63,76], it is expected that the elevated LRP expression patterns observed here would correspond to upregulation of Lef1, c-fos, MMPs, and other Wnt targets. Furthermore, it would be of great interest to study how LRP4/5/6 knockout models respond to mechanical stimuli in terms of matrix gene expression and matrix deposition. Although these studies were outside the scope of the present work, they should be explored in future studies.
This is the first study to show that LRP4/5/6 expression is modulated via mechanical stimulation. Specifically, we have demonstrated that RCS pellet growth was modulated by mechanical stimulation. LRP4/5/6 expression is affected in chondrocytes exposed to either cyclic hydrostatic pressure or simulated microgravity. Both simulated microgravity and cyclic hydrostatic pressure increase LRP5 expression. LRP5 expression is also increased in an in vivo mouse hindlimb suspension model. Finally, we have shown that exogenous sclerostin modulates the expression of LRP4. Further elucidation of the role that mechanical stimulation modulates the Wnt-signaling pathway could lead to development of effective countermeasures against cartilage degeneration due to overuse or disuse. However, it should be noted that while active Wnt-signaling may have adverse side effects in cartilage [60], it is known to be beneficial to bone development and remodeling [77]. This research warns of the potential side effects that current SOST-targeting osteoporosis treatments may have on the neighboring cartilage. Better understanding mechano-modulation of the Wnt-signaling pathway will be critical to determining if and how the Wnt-signaling pathway should be modulated pharmaceutically to best promote both bone and cartilage health.
Acknowledgments
We thank Dr. Julia Oxford for sending us the RCS cells used for the study.
Data Availability
All relevant data are within the Figshare repository at https://doi.org/10.6084/m9.figshare.9899195.v1.
Funding Statement
This study was funded by an NC Space Grant Graduate Research Fellowship (RCN), UNC Summer Research Fellowship (RCN), the National Space Biomedical Research Institute through NASA NCC9-58 (LFM), NIH/NIBIB 1R03EB008790 (EGL), NIH/CTSA 550KR71418 (EGL), NIH/CTSA 550KR61325 (EGL), and NSF/CBET 1133427 and 1702841 (EGL), and the William R. Kenan Institute for Engineering, Technology and Science (EGL). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Robling AG, Turner CH. Mechanical signaling for bone modeling and remodeling. Crit Rev Eukaryot Gene Expr. 2009;19: 319–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Robinson JA, Chatterjee-Kishore M, Yaworsky PJ, Cullen DM, Zhao W, Li C, et al. Wnt/beta-catenin signaling is a normal physiological response to mechanical loading in bone. J Biol Chem. 2006;281: 31720–31728. 10.1074/jbc.M602308200 [DOI] [PubMed] [Google Scholar]
- 3.Kang KS, Robling AG. New Insights into Wnt-Lrp5/6-beta-Catenin Signaling in Mechanotransduction. Front Endocrinol (Lausanne). 2015;5: 246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.LeBlanc A, Schneider V, Shackelford L, West S, Oganov V, Bakulin A, et al. Bone mineral and lean tissue loss after long duration space flight. J Musculoskelet Neuronal Interact. 2000;1: 157–160. [PubMed] [Google Scholar]
- 5.LeBlanc A, Lin C, Shackelford L, Sinitsyn V, Evans H, Belichenko O, et al. Muscle volume, MRI relaxation times (T2), and body composition after spaceflight. J Appl Physiol (1985). 2000;89: 2158–2164. [DOI] [PubMed] [Google Scholar]
- 6.Liphardt AM, Mundermann A, Koo S, Backer N, Andriacchi TP, Zange J, et al. Vibration training intervention to maintain cartilage thickness and serum concentrations of cartilage oligometric matrix protein (COMP) during immobilization. Osteoarthritis Cartilage. 2009;17: 1598–1603. 10.1016/j.joca.2009.07.007 [DOI] [PubMed] [Google Scholar]
- 7.Roos EM, Herzog W, Block JA, Bennell KL. Muscle weakness, afferent sensory dysfunction and exercise in knee osteoarthritis. Nat Rev Rheumatol. 2011;7: 57–63. 10.1038/nrrheum.2010.195 [DOI] [PubMed] [Google Scholar]
- 8.Rehan Youssef A, Longino D, Seerattan R, Leonard T, Herzog W. Muscle weakness causes joint degeneration in rabbits. Osteoarthritis Cartilage. 2009;17: 1228–1235. 10.1016/j.joca.2009.03.017 [DOI] [PubMed] [Google Scholar]
- 9.Clements KM, Bee ZC, Crossingham GV, Adams MA, Sharif M. How severe must repetitive loading be to kill chondrocytes in articular cartilage? Osteoarthritis Cartilage. 2001;9: 499–507. 10.1053/joca.2000.0417 [DOI] [PubMed] [Google Scholar]
- 10.Horisberger M, Fortuna R, Valderrabano V, Herzog W. Long-term repetitive mechanical loading of the knee joint by in vivo muscle stimulation accelerates cartilage degeneration and increases chondrocyte death in a rabbit model. Clin Biomech (Bristol, Avon). 2013;28: 536–543. 10.1016/j.clinbiomech.2013.04.009 [DOI] [PubMed] [Google Scholar]
- 11.Sharma L, Chang A. Overweight: advancing our understanding of its impact on the knee and the hip. Ann Rheum Dis. 2007;66: 141–142. 10.1136/ard.2006.059931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bader DL, Salter DM, Chowdhury TT. Biomechanical influence of cartilage homeostasis in health and disease. Arthritis. 2011;2011: 979032 10.1155/2011/979032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roddy E, Zhang W, Doherty M. Aerobic walking or strengthening exercise for osteoarthritis of the knee? A systematic review. Ann Rheum Dis. 2005;64: 544–548. 10.1136/ard.2004.028746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Manninen P, Riihimaki H, Heliovaara M, Suomalainen O. Physical exercise and risk of severe knee osteoarthritis requiring arthroplasty. Rheumatology (Oxford). 2001;40: 432–437. [DOI] [PubMed] [Google Scholar]
- 15.Elder BD, Athanasiou KA. Hydrostatic pressure in articular cartilage tissue engineering: from chondrocytes to tissue regeneration. Tissue Eng Part B Rev. 2009;15: 43–53. 10.1089/ten.teb.2008.0435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fioravanti A, Moretti E, Scapigliati G, Cervone R, Galeazzi M, Collodel G. Morphological, immunocytochemical and biochemical studies in human osteoarthritic chondrocytes exposed to IL-1b and cyclical hydrostatic pressure. Clin Exp Rheumatol. 2007;25: 690–695. [PubMed] [Google Scholar]
- 17.Fioravanti A, Collodel G, Petraglia A, Nerucci F, Moretti E, Galeazzi M. Effect of hydrostatic pressure of various magnitudes on osteoarthritic chondrocytes exposed to IL-1beta. Indian J Med Res. 2010;132: 209–217. [PubMed] [Google Scholar]
- 18.Karamesinis K, Spyropoulou A, Dalagiorgou G, Katsianou MA, Nokhbehsaim M, Memmert S, et al. Continuous hydrostatic pressure induces differentiation phenomena in chondrocytes mediated by changes in polycystins, SOX9, and RUNX2. J Orofac Orthop. 2017;78: 21–31. 10.1007/s00056-016-0061-1 [DOI] [PubMed] [Google Scholar]
- 19.Yu B, Yu D, Cao L, Zhao X, Long T, Liu G, et al. Simulated microgravity using a rotary cell culture system promotes chondrogenesis of human adipose-derived mesenchymal stem cells via the p38 MAPK pathway. Biochem Biophys Res Commun. 2011;414: 412–418. 10.1016/j.bbrc.2011.09.103 [DOI] [PubMed] [Google Scholar]
- 20.Mayer-Wagner S, Hammerschmid F, Redeker JI, Schmitt B, Holzapfel BM, Jansson V, et al. Simulated microgravity affects chondrogenesis and hypertrophy of human mesenchymal stem cells. Int Orthop. 2014;38: 2615–2621. 10.1007/s00264-014-2454-3 [DOI] [PubMed] [Google Scholar]
- 21.Emin N, Koc A, Durkut S, Elcin AE, Elcin YM. Engineering of rat articular cartilage on porous sponges: effects of tgf-beta 1 and microgravity bioreactor culture. Artif Cells Blood Substit Immobil Biotechnol. 2008;36: 123–137. 10.1080/10731190801932116 [DOI] [PubMed] [Google Scholar]
- 22.Mellor LF, Steward AJ, Nordberg RC, Taylor MA, Loboa EG. Comparison of Simulated Microgravity and Hydrostatic Pressure for Chondrogenesis of hASC. Aerosp Med Hum Perform. 2017;88: 377–384. 10.3357/AMHP.4743.2017 [DOI] [PubMed] [Google Scholar]
- 23.Angele P, Yoo JU, Smith C, Mansour J, Jepsen KJ, Nerlich M, et al. Cyclic hydrostatic pressure enhances the chondrogenic phenotype of human mesenchymal progenitor cells differentiated in vitro. J Orthop Res. 2003;21: 451–457. 10.1016/S0736-0266(02)00230-9 [DOI] [PubMed] [Google Scholar]
- 24.Miyanishi K, Trindade MC, Lindsey DP, Beaupre GS, Carter DR, Goodman SB, et al. Effects of hydrostatic pressure and transforming growth factor-beta 3 on adult human mesenchymal stem cell chondrogenesis in vitro. Tissue Eng. 2006;12: 1419–1428. 10.1089/ten.2006.12.1419 [DOI] [PubMed] [Google Scholar]
- 25.Miyanishi K, Trindade MC, Lindsey DP, Beaupre GS, Carter DR, Goodman SB, et al. Dose- and time-dependent effects of cyclic hydrostatic pressure on transforming growth factor-beta3-induced chondrogenesis by adult human mesenchymal stem cells in vitro. Tissue Eng. 2006;12: 2253–2262. 10.1089/ten.2006.12.2253 [DOI] [PubMed] [Google Scholar]
- 26.Finger AR, Sargent CY, Dulaney KO, Bernacki SH, Loboa EG. Differential effects on messenger ribonucleic acid expression by bone marrow-derived human mesenchymal stem cells seeded in agarose constructs due to ramped and steady applications of cyclic hydrostatic pressure. Tissue Eng. 2007;13: 1151–1158. 10.1089/ten.2006.0290 [DOI] [PubMed] [Google Scholar]
- 27.Ogawa R, Mizuno S, Murphy GF, Orgill DP. The effect of hydrostatic pressure on three-dimensional chondroinduction of human adipose-derived stem cells. Tissue Eng Part A. 2009;15: 2937–2945. 10.1089/ten.TEA.2008.0672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Puetzer J, Williams J, Gillies A, Bernacki S, Loboa EG. The effects of cyclic hydrostatic pressure on chondrogenesis and viability of human adipose- and bone marrow-derived mesenchymal stem cells in three-dimensional agarose constructs. Tissue Eng Part A. 2013;19: 299–306. 10.1089/ten.TEA.2012.0015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ogawa R Md P, Orgill DP, Murphy GF, Mizuno S. Gene Expression Profile on Hydrostatic Pressure-Driven Three-Dimensional Cartilage Induction using Human Adipose-Derived Stem Cells and Collagen Gels. Tissue Eng Part A. 2014. [DOI] [PubMed]
- 30.Jin L, Feng G, Reames DL, Shimer AL, Shen FH, Li X. The effects of simulated microgravity on intervertebral disc degeneration. Spine J. 2013;13: 235–242. 10.1016/j.spinee.2012.01.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mellor LF, Baker TL, Brown RJ, Catlin LW, Oxford JT. Optimal 3D culture of primary articular chondrocytes for use in the rotating wall vessel bioreactor. Aviat Space Environ Med. 2014;85: 798–804. 10.3357/ASEM.3905.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Milstead JR, Simske SJ, Bateman TA. Spaceflight and hindlimb suspension disuse models in mice. Biomed Sci Instrum. 2004;40: 105–110. [PubMed] [Google Scholar]
- 33.Takahashi I, Matsuzaki T, Kuroki H, Hoso M. Joint unloading inhibits articular cartilage degeneration in knee joints of a monosodium iodoacetate-induced rat model of osteoarthritis. Osteoarthritis Cartilage. 2019;27: 1084–1093. 10.1016/j.joca.2019.03.001 [DOI] [PubMed] [Google Scholar]
- 34.Chun JS, Oh H, Yang S, Park M. Wnt signaling in cartilage development and degeneration. BMB Rep. 2008;41: 485–494. 10.5483/bmbrep.2008.41.7.485 [DOI] [PubMed] [Google Scholar]
- 35.Usami Y, Gunawardena AT, Iwamoto M, Enomoto-Iwamoto M. Wnt signaling in cartilage development and diseases: lessons from animal studies. Lab Invest. 2016;96: 186–196. 10.1038/labinvest.2015.142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bonewald LF, Johnson ML. Osteocytes, mechanosensing and Wnt signaling. Bone. 2008;42: 606–615. 10.1016/j.bone.2007.12.224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Papathanasiou I, Malizos KN, Tsezou A. Low-density lipoprotein receptor-related protein 5 (LRP5) expression in human osteoarthritic chondrocytes. J Orthop Res. 2010;28: 348–353. 10.1002/jor.20993 [DOI] [PubMed] [Google Scholar]
- 38.Joiner DM, Less KD, Van Wieren EM, Hess D, Williams BO. Heterozygosity for an inactivating mutation in low-density lipoprotein-related receptor 6 (Lrp6) increases osteoarthritis severity in mice after ligament and meniscus injury. Osteoarthritis Cartilage. 2013;21: 1576–1585. 10.1016/j.joca.2013.05.019 [DOI] [PubMed] [Google Scholar]
- 39.Asai N, Ohkawara B, Ito M, Masuda A, Ishiguro N, Ohno K. LRP4 induces extracellular matrix productions and facilitates chondrocyte differentiation. Biochem Biophys Res Commun. 2014. [DOI] [PubMed] [Google Scholar]
- 40.Thomas RS, Clarke AR, Duance VC, Blain EJ. Effects of Wnt3A and mechanical load on cartilage chondrocyte homeostasis. Arthritis Res Ther. 2011;13: R203 10.1186/ar3536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Praxenthaler H, Kramer E, Weisser M, Hecht N, Fischer J, Grossner T, et al. Extracellular matrix content and WNT/beta-catenin levels of cartilage determine the chondrocyte response to compressive load. Biochim Biophys Acta Mol Basis Dis. 2018;1864: 851–859. 10.1016/j.bbadis.2017.12.024 [DOI] [PubMed] [Google Scholar]
- 42.Dell'Accio F, De Bari C, El Tawil NM, Barone F, Mitsiadis TA, O'Dowd J, et al. Activation of WNT and BMP signaling in adult human articular cartilage following mechanical injury. Arthritis Res Ther. 2006;8: R139 10.1186/ar2029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yingst S, Bloxham K, Warner LR, Brown RJ, Cole J, Kenoyer L, et al. Characterization of collagenous matrix assembly in a chondrocyte model system. J Biomed Mater Res A. 2009;90: 247–255. 10.1002/jbm.a.32078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stevens JW. Swarm chondrosarcoma: a continued resource for chondroblastic-like extracellular matrix and chondrosarcoma biology research. Connect Tissue Res. 2013;54: 252–259. 10.3109/03008207.2013.806913 [DOI] [PubMed] [Google Scholar]
- 45.Brown RJ, Mallory C, McDougal OM, Oxford JT. Proteomic analysis of Col11a1-associated protein complexes. Proteomics. 2011;11: 4660–4676. 10.1002/pmic.201100058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chen Y, Sumiyoshi H, Oxford JT, Yoshioka H, Ramirez F, Morris NP. Cis-acting elements regulate alternative splicing of exons 6A, 6B and 8 of the alpha1(XI) collagen gene and contribute to the regional diversification of collagen XI matrices. Matrix Biol. 2001;20: 589–599. [DOI] [PubMed] [Google Scholar]
- 47.Freeman PM, Natarajan RN, Kimura JH, Andriacchi TP. Chondrocyte cells respond mechanically to compressive loads. J Orthop Res. 1994;12: 311–320. 10.1002/jor.1100120303 [DOI] [PubMed] [Google Scholar]
- 48.Hanson AD, Marvel SW, Bernacki SH, Banes AJ, van Aalst J, Loboa EG. Osteogenic effects of rest inserted and continuous cyclic tensile strain on hASC lines with disparate osteodifferentiation capabilities. Ann Biomed Eng. 2009;37: 955–965. 10.1007/s10439-009-9648-7 [DOI] [PubMed] [Google Scholar]
- 49.Collette NM, Genetos DC, Murugesh D, Harland RM, Loots GG. Genetic evidence that SOST inhibits WNT signaling in the limb. Dev Biol. 2010;342: 169–179. 10.1016/j.ydbio.2010.03.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Parkinson IH, Parsons MA, Moore RJ. The Histochemical Localization of Osteoclasts in EDTA Decalcified Bone. Journal of Histotechnology. 1990;13. [Google Scholar]
- 51.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001;25: 402–408. 10.1006/meth.2001.1262 [DOI] [PubMed] [Google Scholar]
- 52.Shin Y, Huh YH, Kim K, Kim S, Park KH, Koh JT, et al. Low-density lipoprotein receptor-related protein 5 governs Wnt-mediated osteoarthritic cartilage destruction. Arthritis Res Ther. 2014;16: R37 10.1186/ar4466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sakai S, Mishima H, Ishii T, Akaogi H, Yoshioka T, Ohyabu Y, et al. Rotating three-dimensional dynamic culture of adult human bone marrow-derived cells for tissue engineering of hyaline cartilage. J Orthop Res. 2009;27: 517–521. 10.1002/jor.20566 [DOI] [PubMed] [Google Scholar]
- 54.Vunjak-Novakovic G, Obradovic B, Martin I, Freed LE. Bioreactor studies of native and tissue engineered cartilage. Biorheology. 2002;39: 259–268. [PubMed] [Google Scholar]
- 55.Baker TL, Goodwin TJ. Three-dimensional culture of bovine chondrocytes in rotating-wall vessels. In Vitro Cell Dev Biol Anim. 1997;33: 358–365. 10.1007/s11626-997-0006-5 [DOI] [PubMed] [Google Scholar]
- 56.Sawakami K, Robling AG, Ai M, Pitner ND, Liu D, Warden SJ, et al. The Wnt co-receptor LRP5 is essential for skeletal mechanotransduction but not for the anabolic bone response to parathyroid hormone treatment. J Biol Chem. 2006;281: 23698–23711. 10.1074/jbc.M601000200 [DOI] [PubMed] [Google Scholar]
- 57.Akhter MP, Alvarez GK, Cullen DM, Recker RR. Disuse-related decline in trabecular bone structure. Biomech Model Mechanobiol. 2011;10: 423–429. 10.1007/s10237-010-0244-4 [DOI] [PubMed] [Google Scholar]
- 58.Lau KH, Kapur S, Kesavan C, Baylink DJ. Up-regulation of the Wnt, estrogen receptor, insulin-like growth factor-I, and bone morphogenetic protein pathways in C57BL/6J osteoblasts as opposed to C3H/HeJ osteoblasts in part contributes to the differential anabolic response to fluid shear. J Biol Chem. 2006;281: 9576–9588. 10.1074/jbc.M509205200 [DOI] [PubMed] [Google Scholar]
- 59.Lodewyckx L, Luyten FP, Lories RJ. Genetic deletion of low-density lipoprotein receptor-related protein 5 increases cartilage degradation in instability-induced osteoarthritis. Rheumatology (Oxford). 2012;51: 1973–1978. 10.1093/rheumatology/kes178 [DOI] [PubMed] [Google Scholar]
- 60.Chan BY, Fuller ES, Russell AK, Smith SM, Smith MM, Jackson MT, et al. Increased chondrocyte sclerostin may protect against cartilage degradation in osteoarthritis. Osteoarthritis Cartilage. 2011;19: 874–885. 10.1016/j.joca.2011.04.014 [DOI] [PubMed] [Google Scholar]
- 61.Holmen SL, Giambernardi TA, Zylstra CR, Buckner-Berghuis BD, Resau JH, Hess JF, et al. Decreased BMD and limb deformities in mice carrying mutations in both Lrp5 and Lrp6. J Bone Miner Res. 2004;19: 2033–2040. 10.1359/JBMR.040907 [DOI] [PubMed] [Google Scholar]
- 62.Choi HY, Dieckmann M, Herz J, Niemeier A. Lrp4, a novel receptor for Dickkopf 1 and sclerostin, is expressed by osteoblasts and regulates bone growth and turnover in vivo. PLoS One. 2009;4: e7930 10.1371/journal.pone.0007930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ahn Y, Sims C, Murray MJ, Kuhlmann PK, Fuentes-Antras J, Weatherbee SD, et al. Multiple modes of Lrp4 function in modulation of Wnt/beta-catenin signaling during tooth development. Development. 2017;144: 2824–2836. 10.1242/dev.150680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cheleschi S, De Palma A, Pecorelli A, Pascarelli NA, Valacchi G, Belmonte G, et al. Hydrostatic Pressure Regulates MicroRNA Expression Levels in Osteoarthritic Chondrocyte Cultures via the Wnt/beta-Catenin Pathway. Int J Mol Sci. 2017;18: 10.3390/ijms18010133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Niu Q, Li F, Zhang L, Xu X, Liu Y, Gao J, et al. Role of the Wnt/beta-catenin signaling pathway in the response of chondrocytes to mechanical loading. Int J Mol Med. 2016;37: 755–762. 10.3892/ijmm.2016.2463 [DOI] [PubMed] [Google Scholar]
- 66.Semenov M, Tamai K, He X. SOST is a ligand for LRP5/LRP6 and a Wnt signaling inhibitor. J Biol Chem. 2005;280: 26770–26775. 10.1074/jbc.M504308200 [DOI] [PubMed] [Google Scholar]
- 67.Frings-Meuthen P, Boehme G, Liphardt AM, Baecker N, Heer M, Rittweger J. Sclerostin and DKK1 levels during 14 and 21 days of bed rest in healthy young men. J Musculoskelet Neuronal Interact. 2013;13: 45–52. [PubMed] [Google Scholar]
- 68.Spatz JM, Fields EE, Yu EW, Divieti Pajevic P, Bouxsein ML, Sibonga JD, et al. Serum sclerostin increases in healthy adult men during bed rest. J Clin Endocrinol Metab. 2012;97: E1736–40. 10.1210/jc.2012-1579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Robling AG, Niziolek PJ, Baldridge LA, Condon KW, Allen MR, Alam I, et al. Mechanical stimulation of bone in vivo reduces osteocyte expression of Sost/sclerostin. J Biol Chem. 2008;283: 5866–5875. 10.1074/jbc.M705092200 [DOI] [PubMed] [Google Scholar]
- 70.Tu X, Rhee Y, Condon KW, Bivi N, Allen MR, Dwyer D, et al. Sost downregulation and local Wnt signaling are required for the osteogenic response to mechanical loading. Bone. 2012;50: 209–217. 10.1016/j.bone.2011.10.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Spatz JM, Wein MN, Gooi JH, Qu Y, Garr JL, Liu S, et al. The Wnt Inhibitor Sclerostin Is Up-regulated by Mechanical Unloading in Osteocytes in Vitro. J Biol Chem. 2015;290: 16744–16758. 10.1074/jbc.M114.628313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lin C, Jiang X, Dai Z, Guo X, Weng T, Wang J, et al. Sclerostin mediates bone response to mechanical unloading through antagonizing Wnt/beta-catenin signaling. J Bone Miner Res. 2009;24: 1651–1661. 10.1359/jbmr.090411 [DOI] [PubMed] [Google Scholar]
- 73.Spatz JM, Ellman R, Cloutier AM, Louis L, van Vliet M, Suva LJ, et al. Sclerostin antibody inhibits skeletal deterioration due to reduced mechanical loading. J Bone Miner Res. 2013;28: 865–874. 10.1002/jbmr.1807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Chu CR, Szczodry M, Bruno S. Animal models for cartilage regeneration and repair. Tissue Eng Part B Rev. 2010;16: 105–115. 10.1089/ten.TEB.2009.0452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Moran CJ, Ramesh A, Brama PA, O'Byrne JM, O'Brien FJ, Levingstone TJ. The benefits and limitations of animal models for translational research in cartilage repair. J Exp Orthop. 2016;3: 1-015-0037-x. Epub 2016 Jan 6. 10.1186/s40634-015-0037-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.MacDonald BT, Semenov MV, Huang H, He X. Dissecting molecular differences between Wnt coreceptors LRP5 and LRP6. PLoS One. 2011;6: e23537 10.1371/journal.pone.0023537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Krishnan V, Bryant HU, Macdougald OA. Regulation of bone mass by Wnt signaling. J Clin Invest. 2006;116: 1202–1209. 10.1172/JCI28551 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the Figshare repository at https://doi.org/10.6084/m9.figshare.9899195.v1.