Abstract
Pain management for cancer patients should include pharmacologic and non-pharmacologic interventions. Integrative medicine therapies, such as mind-body practice, acupuncture, massage therapy, and music therapy, have been studied for their roles in pain management. Data from randomized controlled trials support the effect of hypnosis, acupuncture and music therapy in reduction of pain. Mindfulness meditation, yoga, qigong, and massage therapy, although may not reduce pain per se, can relieve anxiety and mood changes which are commonly associated with pain. In clinical practice, one should also consider burdens and risks to patients, patient preference, and the presence or absence of better alternatives when making decisions on whether an integrative medicine therapy is of clinical value.
Keywords: Pain, cancer pain, pain management, integrative medicine, mind-body therapies, hypnosis, mindfulness, acupuncture, massage therapy, music therapy
Pain Related to Cancer and Cancer Treatment
Pain is one of the most common, burdensome, and feared symptoms experienced by patients with cancer.1 A meta-analysis of 122 studies (N=4,199) showed that about 55% of patients experience pain during cancer treatment; 40% experience pain after curative treatment.1 Cancer patients can experience pain from the cancer itself (bone metastasis, cancer infiltrating soft tissues or pressing on nerves). They can also experience acute pain from cancer treatment-related effects, such as chemotherapy-induced mucositis,2 chemotherapy-induced musculoskeletal pain,3 post-operative wound pain,4 radiation-induced mucositis, dermatitis, or enteritis.5,6 For many cancer survivors, pain may become chronic as a long-term sequela of cancer treatment. In particular, taxanes, platins, vincristine and bortezomib can cause chemotherapy-induced peripheral neuropathy that manifests as pain in some patients;7 surgery can lead to phantom limb pain8 or pain from scar tissue contraction;9 and aromatase inhibitors can cause diffuse joint pain.10
Pain Management: Pharmacologic and Non-Pharmacologic Interventions
Pain management for cancer patients includes pharmacologic and non-pharmacologic interventions.11 Pharmacologic options include opioids (oxycodone, morphine, hydromorphone, fentanyl), the mainstay in managing somatic pain, and anti-convulsants (gabapentin, pregabalin) for neuropathic pain. However, lack of energy, drowsiness, constipation, nausea, and indigestion are common side effects.12 Acetaminophen and non-steroidal anti-inflammatory drugs (NSAIDs) are used for mild to moderate pain, but they are not favored during chemotherapy due to their potential for liver and kidney toxicity, or their ability to mask a fever that may be an early sign of infection. While antidepressants, anxiolytics, and steroids are sometimes used as adjuncts to enhance pain control, they are associated with their own side effects. Aversion to treatment side effects and fear of developing addiction or tolerance are cited as reasons that patients may be reluctant to take adequate pain medicine.13,14
Opioids are necessary and appropriate for patients with advanced cancer and intractable pain. However, they are not appropriate for most cancer survivors with no active cancer. Because of exposure to opioids during cancer treatment, cancer survivors have a higher risk for opioid misuse. A recent study using SEER and Medicare data of 46,789 older cancer survivors and 138,136 noncancer controls shows a significantly higher chronic opioid use in cancer survivors who had a higher pain burden during cancer treatment (colorectal cancer: odds ratio (OR) 1.34, 95% confidence interval (CI) 1.22 to 1.47; lung cancer: OR 2.55, 95% CI 2.34 to 2.77). It takes six years for opioid use to return to the level of controls.15 Other studies show that the exposure to opioids during treatment for acute pain is a strong risk factor for patients to become long-term opioid users even when the acute pain has subsided and opioids are no longer appropriate.16-19 The largest increments in probability of long-term opioid use were observed after the 5th and 31st days on short-term use.20 Unnecessary use of opioids presents problems beyond the medical field, such as effects on mental health, impact on family members, financial costs, and opioid misuse disorder, especially in light of the current opioid crisis. This is where non-pharmacologic interventions, including integrative medicine therapies, can help improve pain management and reduce unnecessary reliance on pharmacologic interventions.
The Joint Commission21 American College of Physicians (ACP),22,23 National Comprehensive Cancer Network (NCCN)24 and American Society of Clinical Oncology (ASCO)11 guidelines all recommend a combination of pharmacologic and non-pharmacologic modalities. Non-pharmacologic interventions are an important part of a comprehensive pain management plan. They include procedural and psychosocial interventions. Procedural interventions, such as radiation to bone metastasis, nerve block, and neurectomy, are effective but usually reserved for severe pain refractory to drugs. Psychosocial interventions, such as cognitive behavioral therapy, relaxation, and experiential interventions, are associated with fewer side effects and should be part of a multimodal approach to pain management.1,25,26
Integrative medicine therapies are other forms of non-pharmacologic interventions that historically have been used outside the domain of modern Western medicine yet shown to have benefits to patients in recent research. Once carefully incorporated to standard cancer care, these therapies can complement other treatments and enhance the quality of cancer care patients are receiving.27-29 Most of the current research data comes from studies of mind-body practice, acupuncture, massage therapy, and music therapy. Although a majority of the studies on these therapies were of uncontrolled design, a substantial number of randomized controlled trials (RCTs) have been conducted and reported. Here we summarize our current body of evidence from those studies.
Mind-Body Practices
Mind-body practices focus on interactions among the brain, mind, body and behavior, with the intent to use the mind to improve physical function and promote health. Some of these therapies, such as meditation, relaxation techniques, hypnosis, yoga, tai chi, and qigong have ancient roots, while others were developed more recently, such as guided imagery, biofeedback and music therapy. Their common goal is to reduce the impact of distressing problems such as anxiety, fear, phobia, anger, resentment, depression and pain, while promoting a sense of emotional, physical and spiritual well-being. Published studies of mind-body practices in general show benefit in anxiety, depression, fatigue and other emotional wellness, but not in pain per se, with the exception of hypnosis.
Hypnosis is a practice by which a therapist induces, or instructs the patient on how to self-induce, a mental state of focused attention or altered consciousness between wakefulness and sleep. In this state, distractions are blocked, allowing the patient to concentrate intently on a particular subject, memory, sensation, or problem. Patients may receive suggestions, or self-suggest, changes in perceptions toward sensations, thoughts, and behaviors.
In a systematic review of 21 studies (11 RCTs, 2 non-RCTs, and 8 case series), self-hypnosis provided pain relief in cancer patients and dying patients.30 Another systematic review of 27 reports (1 RCT, 24 case studies, and 2 other types of studies) concluded that the poor quality of studies evaluated, and the heterogeneity of study populations, limited further evaluation.31 A meta-analysis of 37 studies (N=4199) on psychosocial interventions, including hypnosis, concluded that these modalities have a significant medium-size effect on both pain severity and pain interference with functioning, and that quality-controlled psychosocial interventions should be considered in multimodal approaches to pain management for cancer patients.1 A systematic review of RCTS done in breast cancer patients showed that hypnosis positively influenced pain from diagnostic breast biopsy (3 RCTs), breast cancer surgery (1 RCT), radiotherapy (3 RCTs) and metastatic breast cancer (3 RCTs).32 Interestingly, patients who are highly hypnotizable reported greater benefits from hypnosis, used self-hypnosis more often outside of group therapy, and applied it to manage other symptoms in addition to pain (RCT, N=124), indicating selection of likely responders may be important in clinical practice.33
Meditation is a contemplative practice that invites heightened awareness and attention to one’s own sensations, surroundings, and/or inner mental processes. Most of the studies on meditation were conducted using a specific intervention - mindfulness-based stress reduction (MBSR). MBSR is a type of meditation practice taught through a well-defined, structured curriculum and aimed to create a nonjudgmental “mindful state” of conscious awareness of the moment. A systematic review and meta-analysis of 14 RCTs (N=1505) showed significant improvement in physiological function, cognitive function, fatigue, emotional wellbeing, anxiety, depression, stress, distress and mindfulness. Five trials included pain as an endpoint. There was a trend of reduction of pain (standardized mean difference (SMD) −0.46, 95% CI −1.05 to 0.12), which was not statistically significant.
Yoga and qigong are practices that combine physical movement, breath control and meditative components. Yoga has been found to significantly improve anxiety, depression, distress, and stress in a meta-analysis of 10 RCTs.34 RCTs evaluating pain as the primary endpoint in a cancer care setting are lacking. Similarly, a systematic review of qigong found promising data for stress reduction and improving quality of life, but not for pain.35
Mind-body practices are generally safe. A recent Cochrane review of studies involving breast cancer analyzed data from 10 RCTs (N=1571) reported no adverse events attributed to MBSR. Their effectiveness requires instructors skilled in conveying appropriate technique and regular practice by the patient. They are helpful complementary modalities that can be used as part of a multidisciplinary approach to reduce anxiety, mood disturbance, sleep disturbance, and improve quality of life in cancer patients, with the additional important component of empowering patients to do something for themselves. Research is underway to elucidate the mechanisms by which mental activity exerts control over physiologic function.
Acupuncture
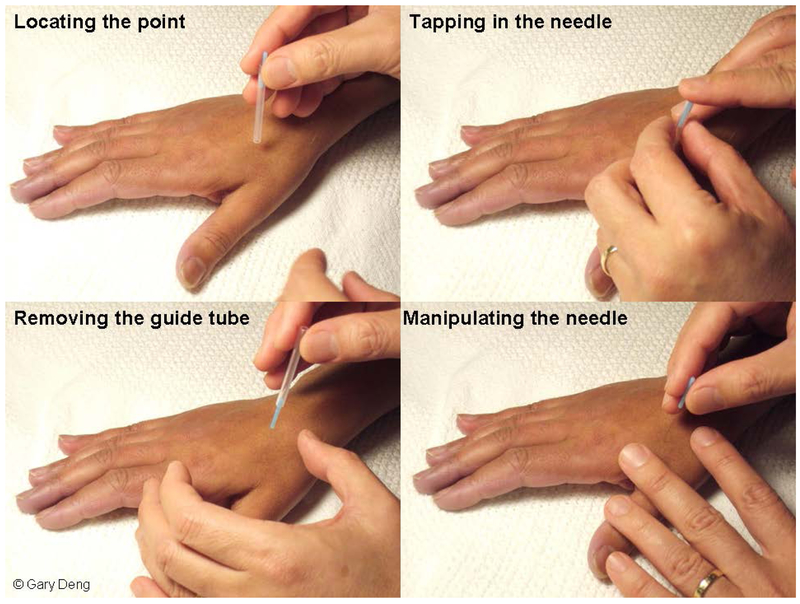
Acupuncture is a modality derived from Traditional Chinese Medicine (TCM). During acupuncture treatment, filiform needles are inserted into certain points on the body and stimulated with manual manipulation (twisting, pulling and pushing), heat, or electrical pulses (Figure 1). There is strong evidence supporting its analgesic effect on musculoskeletal pain.36-38 A systematic review of 17 trials (N= 2,027) showed that acupuncture reduced the intensity of acute and chronic low back pain more than sham acupuncture, leading ACP’s clinical practice guidelines to recommend acupuncture as a treatment option that should be considered.23 In a meta-analysis of 20,827 patients from 39 RCTs, the analgesic effect size of acupuncture was 0.5 SDs compared with no acupuncture control and close to 0.2 SDs compared with sham.38 According to neuroscience research, the mechanisms of action of acupuncture appear to be increased production of endogenous analgesic neurotransmitters, such as endorphins and adenosine, and modulation of neuronal matrix involved in pain perception.39-44
Figure 1.
Acupuncture procedure
In a Cochrane review of RCTs of acupuncture for treatment of cancer-related pain, five RCTs were identified(N=285).45 The five studies showed acupuncture was superior to sham acupuncture, or superior or equivalent to oral medications administrated according to the WHO analgesic scale.46-50 A recent systematic review and meta-analysis also included pain related to cancer treatments. A total of 29 RCTs yielding 36 effect sizes were included. The overall effect of acupuncture on cancer-related pain was SMD −0.45 (95% CI -0.63 to −0.26).51
Patients on hormone therapy regimens with aromatase inhibitors such as anastrozole, letrozole, or exemestane frequently report debilitating joint pain and discomfort. Some patients may have symptoms so severe that they stop aromatase inhibitor treatment, leading to higher risk of cancer recurrence. Several RCTs have been conducted to evaluate acupuncture’s effect on aromatase inhibitor-associated arthralgia and musculoskeletal symptoms (AIAA, AIMSS). A recent meta-analysis has identified three well-designed RCTs that support the use of acupuncture for these symptoms.51 In a 3-arm trial of 67 breast cancer patients, electroacupuncture led to clinically important and durable pain reduction at weeks 8 and 12 (P=.0004 and <.0001, respectively).52 In another study of 38 evaluable patients, manual acupuncture produced significant reductions in pain scores when compared to non-acupoint sham acupuncture (P<.001), as well as reductions in pain severity (P=.003) and pain-related interference (P=.002).53 A third study of 47 evaluable breast cancer patients showed pain improvements with no significant difference between manual acupuncture and sham acupuncture. Interestingly, there was a significant reduction in the proinflammatory cytokine IL-17, a cytokine implicated in AIMSS, in both groups at the end of the study (P≤.009).54 A recent multicenter trial funded by SWOG found long-term efficacy with acupuncture (N=110) compared to sham acupuncture (N=59) or waitlist control (N=57).29 After 6 weeks of twice weekly acupuncture followed by 6 weeks of once weekly acupuncture, Brief Pain Inventory Worst Pain (BPI-WP) scores were 0.92 point lower when acupuncture was compared to sham acupuncture (95% CI 0.20 to 1.65) and 0.96 point lower when compared to waitlist control (95% CI 0.24 to 1.67). This rigorously designed study generated important evidence in guiding the use of acupuncture for this difficult-to-treat clinical problem.
Acupuncture has a known safety record.55 According to data from 97,733 patients and more than 760,000 treatments, the most common adverse events (in around 7% treatments) were pain experienced during needling and loss of a drop of blood when the acupuncture needle was removed, all grade 1 and self-limiting. In clinical trial settings, serious adverse events are rare and found to be at a rate of around 0.005% of patients and 0.0008% of treatments.56 With the current level of evidence, clinical practice guidelines made a grade C recommendation for using acupuncture to treat pain in cancer patients.28
Massage Therapy
Therapeutic massage therapy refers to a modality that applies physical force to muscles, tendons and connective tissues to promote relaxation, reduce tension, relieve pain and improve circulation. “Swedish massage” is the most commonly used techniques in cancer care. It uses five types of strokes (gliding, kneading, tapping, friction and vibration). Other commonly available techniques include myofascial release, craniosacral technique, ayurvedic massage, tuina, shiatsu, reflexology, and deep tissue massage. The application of pressure, theoretical framework, education credential and regulatory environment vary for the different techniques.
Most non-randomized studies on massage therapy in cancer patients had small sample sizes. One example of large observational studies showed that massage improved pain scores by approximately 50% from baseline, with outpatients improved about 10% more than inpatients (N=1290). The benefits remained when reassessed 48-hour later.57
Results from RCTs are mixed. An early systematic review focusing on cancer patients found ten controlled trials.58 Control interventions in the studies included standard care, attention, or low-intensity bodywork. Significant reduction in anxiety was found. In three studies, pain was significantly reduced.59-61 The methodological quality of most included trials was poor. A more recent meta-analysis of 12 studies (N=559, 9 RCTs and 3 non-RCTs) on massage therapy and cancer pain was conducted.62 Pooled data from the 9 RCTs showed a significant reduction of pain scores when compared to usual care (−1.24, 95% CI −1.72 to −0.75). Significant reduction of pain was reported when pain was assessed at 1, 2 or 4 weeks of the studies. There was no significant publication bias based on funnel plot. A subsequent systematic review and meta-analysis of 16 RCTs (12 deemed of high quality) showed that massage therapy reduced pain more than either no treatment controls or active comparators, although the differences did not reach statistical significance.63 The effect sizes were −0.203 (95% CI, −0.99 to 0.59) and −0.545 (95% CI, −1.23 to 0.14) respectively. Active comparators included reading, healing touch, attention and usual care. In the same meta-analysis, massage was found to improve anxiety (−1.24, 95% CI −2.44 to −0.03) and sleep (−1.06, 95% CI −2.18 to 0.05). Methodological quality of the included trials was high, although the results were quite heterogenous.
In the cancer care setting, safety is an important factor when massage therapy is considered for a particular patient. Strong pressure should not be applied to soft tissues with underlying tumor or sites of bone metastasis. Nor should it be given to patients who are thrombocytopenic or on anticoagulants. For those patients, gentle light touch massage can still be used. Areas of open wounds, skin breakdown, venous thrombosis, implanted medical device (Mediport, hepatic artery infusion pump, or pacemaker), and areas with sensitive skin after radiation therapy or recent surgery should not be massaged. Thus, it is critical that the massage therapist be properly trained about safety precaution when treating cancer patients.
In summary, there is encouraging evidence suggesting massage therapy’s benefit, although the evidence is neither definitive nor strong. Given that massage therapy is recommended for anxiety (grade C evidence) and mood disturbance (grade B evidence), it can be considered in patients suffering from pain who also have anxiety and mood disturbance.28,29
Music Therapy
Music therapy is the use of music as a therapeutic intervention, provided by music therapists in the context of a therapist-patient relationship.64 It can be receptive – patients listening to recorded or live music selected by a music therapist, or active – patients participate in making music guided by a music therapist, either by singing or playing instruments. The therapist assesses the patient’s needs and conditions before designing and providing a tailored intervention regimen. Music can express and communicate in ways words cannot. Use of sound and music to elicit physical, emotional, spiritual, and social changes can be seen in almost all cultures in the world and can be traced to early stages of the development of human societies.65
Many randomized controlled studies of music therapy have been conducted to assess its effect on pain. In a meta-analysis of 97 trials, music therapy was shown to significantly reduce pain, emotional distress from pain, anesthetic use, and opioid intake in general populations.66 Regarding cancer patients, a Cochrane review of 52 music therapy trials with a total of 3731 patients identified 7 studies (N=528) with pain as an outcome.67 It showed that the mean pain score was 0.91 SMD less (95% CI −1.46 to −0.36) in the music therapy group than in the usual care control group. SMD of 0.91 is considered a more-than-moderate effect size. A recent systematic review and meta-analysis identified 25 RCTs, with 20 eligible for meta-analysis (N=1565).68 Music therapy was found to be effective in reducing pain (SMD −0.88, 95% CI −1.45 to −0.32), as well as reducing anxiety (SMD −0.80, 95% CI −1.35 to −0.25) and improving mood (SMD −0.55, 95% CI −0.98 to −0.13).
Music therapy is considered generally safe. It has little physical risk and in theory possible psychological risk as it may elicit strong emotions. However, music therapy has been studied in patients with psychosis and showed beneficial effects in psychosocial functioning without adverse events.69,70 Music therapists are trained to recognize clinical scenarios where referral to psychiatry is warranted.
In light of the current evidence base and the favorable benefit-risk ratio of music therapy, clinical practice guidelines recommend consideration of music therapy for the management of pain (grade C evidence).27-29
Summary
In short, current evidence for using integrative approaches to treat pain in cancer patients is encouraging. Overall evidence supports incorporation of hypnosis, acupuncture, and music therapy in a multidisciplinary pain management plan. For patients with accompanying psychological distress such as anxiety and depression, either as resulting from or independent of pain, MBSR and massage therapy can also be of benefit.
When considering various treatment options in clinical practice, we not only need to consider the presence or absence of evidence for a particular therapy, but also the strength (certainty) of the evidence, the effect size, and risks and burdens to patients. Evidence in favor of efficacy should be weighed against the risks and burdens, and any potential alternatives or the lack thereof.
Integrative medicine therapies present with low physical risks. They are generally safe when provided by properly trained practitioners. However, they may present financial burdens to patients. Acupuncture is increasingly being covered by commercial insurance plans, thanks to an increasing body of research evidence. Some mind-body techniques may be covered by some insurance plans under psychotherapy. Other than these two exceptions, integrative therapies often require self-pay by patients, support from hospital operational funds or philanthropy. Financial barriers may be partially overcome by operational adjustments. For example, patients can be taught to practice mind-body interventions themselves. Meditation, yoga and qigong classes can be given in group settings, lowering costs per patient. Acupuncture can be provided in a group setting too – called “community acupuncture”. Patients can be taught to do acupressure (application of pressure, usually with a finger, on acupuncture points) onto themselves, although the stimulation is not as strong as stimulation by needles. Family members or caregivers can be taught to safely give massages.
Pain causes not only physical suffering, but also mental suffering, influenced by the psycho-social-cultural context the patient is in. The origin of pain and complicating factors should be considered when we select treatments for pain. If the pain is augmented by anxiety, fear, depression or sleep disturbance, or if the pain exacerbates psychological distress— mind-body therapies and massage therapy should be considered. If opioid therapy creates undesirable effects, such as sedation, constipation, fatigue, nausea, and emesis, the addition of acupuncture has the potential of lowering the required dose of pain medications and hence their side effects.
Each patient’s personal preference, belief system and cultural background should be taken into consideration. Patients who have a strong spiritual need, who wish a more naturalistic approach to health, and patients who have experienced benefit from these therapies previously, are more open to integrative therapies and appreciate their availability. If a clinician partners with the patient and values their perspective in how to manage pain, she or he will find the therapeutic relationship between them enhanced. Only by considering what is truly important to a patient as an individual can we provide optimal patient-centered care, improve the quality of pain management, and comfort the patient to the best of our ability.
Acknowledgment:
This research was funded in part through the NIH/NCI Cancer Center Support Grant P30 CA008748.
References
- 1.Sheinfeld Gorin S, Krebs P, Badr H, et al. Meta-analysis of psychosocial interventions to reduce pain in patients with cancer. J Clin Oncol 2012;30:539–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lalla RV, Bowen J, Barasch A, et al. MASCC/ISOO clinical practice guidelines for the management of mucositis secondary to cancer therapy. Cancer 2014;120:1453–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saibil S, Fitzgerald B, Freedman OC, et al. Incidence of taxane-induced pain and distress in patients receiving chemotherapy for early-stage breast cancer: a retrospective, outcomes-based survey. Curr Oncol 2010;17:42–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fassoulaki A, Melemeni A, Staikou C, Triga A, Sarantopoulos C. Acute postoperative pain predicts chronic pain and long-term analgesic requirements after breast surgery for cancer. Acta Anaesthesiol Belg 2008;59:241–8. [PubMed] [Google Scholar]
- 5.Bray FN, Simmons BJ, Wolfson AH, Nouri K. Acute and Chronic Cutaneous Reactions to Ionizing Radiation Therapy. Dermatol Ther (Heidelb) 2016;6:185–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harb AH, Abou Fadel C, Sharara AI. Radiation enteritis. Curr Gastroenterol Rep 2014;16:383. [DOI] [PubMed] [Google Scholar]
- 7.Gewandter JS, Freeman R, Kitt RA, et al. Chemotherapy-induced peripheral neuropathy clinical trials: Review and recommendations. Neurology 2017;89:859–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wylde V, Dennis J, Beswick AD, et al. Systematic review of management of chronic pain after surgery. Br J Surg 2017;104:1293–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Couceiro TC, Menezes TC, Valenca MM. Post-mastectomy pain syndrome: the magnitude of the problem. Rev Bras Anestesiol 2009;59:358–65. [DOI] [PubMed] [Google Scholar]
- 10.Beckwee D, Leysen L, Meuwis K, Adriaenssens N. Prevalence of aromatase inhibitor-induced arthralgia in breast cancer: a systematic review and meta-analysis. Support Care Cancer 2017;25:1673–86. [DOI] [PubMed] [Google Scholar]
- 11.Paice JA, Portenoy R, Lacchetti C, et al. Management of Chronic Pain in Survivors of Adult Cancers: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol 2016;34:3325–45. [DOI] [PubMed] [Google Scholar]
- 12.Villars P, Dodd M, West C, et al. Differences in the prevalence and severity of side effects based on type of analgesic prescription in patients with chronic cancer pain. J Pain Symptom Manage 2007;33:67–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paice JA, Ferrell B. The management of cancer pain. CA Cancer J Clin 2011;61:157–82. [DOI] [PubMed] [Google Scholar]
- 14.Furlan AD, Sandoval JA, Mailis-Gagnon A, Tunks E. Opioids for chronic noncancer pain: a meta-analysis of effectiveness and side effects. CMAJ 2006;174:1589–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Salz T, Lavery JA, Lipitz-Snyderman AN, et al. Trends in Opioid Use Among Older Survivors of Colorectal, Lung, and Breast Cancers. J Clin Oncol 2019;37:1001–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barnett ML, Olenski AR, Jena AB. Opioid-Prescribing Patterns of Emergency Physicians and Risk of Long-Term Use. N Engl J Med 2017;376:663–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Edlund MJ, Martin BC, Russo JE, DeVries A, Braden JB, Sullivan MD. The role of opioid prescription in incident opioid abuse and dependence among individuals with chronic noncancer pain: the role of opioid prescription. Clin J Pain 2014;30:557–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harbaugh CM, Lee JS, Hu HM, et al. Persistent Opioid Use Among Pediatric Patients After Surgery. Pediatrics 2018;141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gil JA, Gunaseelan V, DeFroda SF, Brummett CM, Bedi A, Waljee JF. Risk of Prolonged Opioid Use Among Opioid-Naive Patients After Common Shoulder Arthroscopy Procedures. Am J Sports Med 2019;47:1043–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shah A, Hayes CJ, Martin BC. Characteristics of Initial Prescription Episodes and Likelihood of Long-Term Opioid Use - United States, 2006-2015. MMWR Morb Mortal Wkly Rep 2017;66:265–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baker DW. History of The Joint Commission’s Pain Standards: Lessons for Today’s Prescription Opioid Epidemic. JAMA 2017;317:1117–8. [DOI] [PubMed] [Google Scholar]
- 22.Qaseem A, Wilt TJ, McLean RM, Forciea MA, Clinical Guidelines Committee of the American College of P. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med 2017;166:514–30. [DOI] [PubMed] [Google Scholar]
- 23.Chou R, Deyo R, Friedly J, et al. Nonpharmacologic Therapies for Low Back Pain: A Systematic Review for an American College of Physicians Clinical Practice Guideline. Ann Intern Med 2017;166:493–505. [DOI] [PubMed] [Google Scholar]
- 24.Swarm RA, Abernethy AP, Anghelescu DL, et al. Adult cancer pain. J Natl Compr Canc Netw 2013;11:992–1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Syrjala KL, Donaldson GW, Davis MW, Kippes ME, Carr JE. Relaxation and imagery and cognitive-behavioral training reduce pain during cancer treatment: a controlled clinical trial. Pain 1995;63:189–98. [DOI] [PubMed] [Google Scholar]
- 26.Syrjala KL, Cummings C, Donaldson GW. Hypnosis or cognitive behavioral training for the reduction of pain and nausea during cancer treatment: a controlled clinical trial. Pain 1992;48:137–46. [DOI] [PubMed] [Google Scholar]
- 27.Lyman GH, Greenlee H, Bohlke K, et al. Integrative Therapies During and After Breast Cancer Treatment: ASCO Endorsement of the SIO Clinical Practice Guideline. J Clin Oncol 2018;36:2647–55. [DOI] [PubMed] [Google Scholar]
- 28.Greenlee H, DuPont-Reyes MJ, Balneaves LG, et al. Clinical practice guidelines on the evidence-based use of integrative therapies during and after breast cancer treatment. CA Cancer J Clin 2017;67:194–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Greenlee H, Balneaves LG, Carlson LE, et al. Clinical practice guidelines on the use of integrative therapies as supportive care in patients treated for breast cancer. J Natl Cancer Inst Monogr 2014;2014:346–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pan CX, Morrison RS, Ness J, Fugh-Berman A, Leipzig RM. Complementary and alternative medicine in the management of pain, dyspnea, and nausea and vomiting near the end of life. A systematic review. J Pain Symptom Manage 2000;20:374–87. [DOI] [PubMed] [Google Scholar]
- 31.Rajasekaran M, Edmonds PM, Higginson IL. Systematic review of hypnotherapy for treating symptoms in terminally ill adult cancer patients. Palliat Med 2005;19:418–26. [DOI] [PubMed] [Google Scholar]
- 32.Cramer H, Lauche R, Paul A, Langhorst J, Kummel S, Dobos GJ. Hypnosis in breast cancer care: a systematic review of randomized controlled trials. Integr Cancer Ther 2015;14:5–15. [DOI] [PubMed] [Google Scholar]
- 33.Butler LD, Koopman C, Neri E, et al. Effects of supportive-expressive group therapy on pain in women with metastatic breast cancer. Health Psychol 2009;28:579–87. [DOI] [PubMed] [Google Scholar]
- 34.Lin KY, Hu YT, Chang KJ, Lin HF, Tsauo JY. Effects of yoga on psychological health, quality of life, and physical health of patients with cancer: a meta-analysis. Evid Based Complement Alternat Med 2011;2011:659876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chan CL, Wang CW, Ho RT, et al. A systematic review of the effectiveness of qigong exercise in supportive cancer care. Support Care Cancer 2012;20:1121–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vickers AJ, Cronin AM, Maschino AC, et al. Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med 2012;172:1444–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vickers AJ, Linde K. Acupuncture for chronic pain. JAMA 2014;311:955–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vickers AJ, Vertosick EA, Lewith G, et al. Acupuncture for Chronic Pain: Update of an Individual Patient Data Meta-Analysis. J Pain 2018;19:455–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liao HY, Hsieh CL, Huang CP, Lin YW. Electroacupuncture Attenuates Induction of Inflammatory Pain by Regulating Opioid and Adenosine Pathways in Mice. Sci Rep 2017;7:15679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sawynok J Adenosine receptor targets for pain. Neuroscience 2016;338:1–18. [DOI] [PubMed] [Google Scholar]
- 41.Otti A, Noll-Hussong M. Acupuncture-induced pain relief and the human brain’s default mode network - an extended view of central effects of acupuncture analgesia. Forsch Komplementmed 2012;19:197–201. [DOI] [PubMed] [Google Scholar]
- 42.Wang SM, Kain ZN, White P. Acupuncture analgesia: I. The scientific basis. Anesth Analg 2008;106:602–10. [DOI] [PubMed] [Google Scholar]
- 43.Kaptchuk TJ. Acupuncture: theory, efficacy, and practice. Ann Intern Med 2002;136:374–83. [DOI] [PubMed] [Google Scholar]
- 44.Clement-Jones V, McLoughlin L, Tomlin S, Besser GM, Rees LH, Wen HL. Increased beta-endorphin but not met-enkephalin levels in human cerebrospinal fluid after acupuncture for recurrent pain. Lancet 1980;2:946–9. [DOI] [PubMed] [Google Scholar]
- 45.Paley CA, Johnson MI, Tashani OA, Bagnall AM. Acupuncture for cancer pain in adults. Cochrane Database Syst Rev 2015:CD007753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chen H, Liu TY, Kuai L, Zhu J, Wu CJ, Liu LM. Electroacupuncture treatment for pancreatic cancer pain: a randomized controlled trial. Pancreatology 2013;13:594–7. [DOI] [PubMed] [Google Scholar]
- 47.Lu W, Matulonis UA, Dunn JE, et al. The Feasibility and Effects of Acupuncture on Quality of Life Scores During Chemotherapy in Ovarian Cancer: Results from a Pilot, Randomized Sham-Controlled Trial. Med Acupunct 2012;24:233–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chen ZJ, Guo YP, Wu ZC. [Observation on the therapeutic effect of acupuncture at pain points on cancer pain]. Zhongguo Zhen Jiu 2008;28:251–3. [PubMed] [Google Scholar]
- 49.Alimi D, Rubino C, Pichard-Leandri E, Fermand-Brule S, Dubreuil-Lemaire ML, Hill C. Analgesic effect of auricular acupuncture for cancer pain: a randomized, blinded, controlled trial. J Clin Oncol 2003;21:4120–6. [DOI] [PubMed] [Google Scholar]
- 50.Dang W, Yang J. Clinical study on acupuncture treatment of stomach carcinoma pain. J Tradit Chin Med 1998;18:31–8. [PubMed] [Google Scholar]
- 51.Chiu HY, Hsieh YJ, Tsai PS. Systematic review and meta-analysis of acupuncture to reduce cancer-related pain. Eur J Cancer Care (Engl) 2017;26. [DOI] [PubMed] [Google Scholar]
- 52.Mao JJ, Xie SX, Farrar JT, et al. A randomised trial of electro-acupuncture for arthralgia related to aromatase inhibitor use. Eur J Cancer 2014;50:267–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Crew KD, Capodice JL, Greenlee H, et al. Randomized, blinded, sham-controlled trial of acupuncture for the management of aromatase inhibitor-associated joint symptoms in women with early-stage breast cancer. J Clin Oncol 2010;28:1154–60. [DOI] [PubMed] [Google Scholar]
- 54.Bao T, Cai L, Giles JT, et al. A dual-center randomized controlled double blind trial assessing the effect of acupuncture in reducing musculoskeletal symptoms in breast cancer patients taking aromatase inhibitors. Breast Cancer Res Treat 2013;138:167–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jindal V, Ge A, Mansky PJ. Safety and efficacy of acupuncture in children: a review of the evidence. J Pediatr Hematol Oncol 2008;30:431–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Melchart D, Weidenhammer W, Streng A, et al. Prospective investigation of adverse effects of acupuncture in 97 733 patients. Arch Intern Med 2004;164:104–5. [DOI] [PubMed] [Google Scholar]
- 57.Cassileth BR, Vickers AJ. Massage therapy for symptom control: outcome study at a major cancer center. J Pain Symptom Manage 2004;28:244–9. [DOI] [PubMed] [Google Scholar]
- 58.Wilkinson S, Barnes K, Storey L. Massage for symptom relief in patients with cancer: systematic review. J Adv Nurs 2008;63:430–9. [DOI] [PubMed] [Google Scholar]
- 59.Wilcock A, Manderson C, Weller R, et al. Does aromatherapy massage benefit patients with cancer attending a specialist palliative care day centre? Palliat Med 2004;18:287–90. [DOI] [PubMed] [Google Scholar]
- 60.Grealish L, Lomasney A, Whiteman B. Foot massage. A nursing intervention to modify the distressing symptoms of pain and nausea in patients hospitalized with cancer. Cancer Nurs 2000;23:237–43. [DOI] [PubMed] [Google Scholar]
- 61.Weinrich SP, Weinrich MC. The effect of massage on pain in cancer patients. Appl Nurs Res 1990;3:140–5. [DOI] [PubMed] [Google Scholar]
- 62.Lee SH, Kim JY, Yeo S, Kim SH, Lim S. Meta-Analysis of Massage Therapy on Cancer Pain. Integr Cancer Ther 2015;14:297–304. [DOI] [PubMed] [Google Scholar]
- 63.Boyd C, Crawford C, Paat CF, et al. The Impact of Massage Therapy on Function in Pain Populations-A Systematic Review and Meta-Analysis of Randomized Controlled Trials: Part II, Cancer Pain Populations. Pain Med 2016;17:1553–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gramaglia C, Gambaro E, Vecchi C, et al. Outcomes of music therapy interventions in cancer patients-A review of the literature. Crit Rev Oncol Hematol 2019;138:241–54. [DOI] [PubMed] [Google Scholar]
- 65.Thaut MH. Music as therapy in early history. Prog Brain Res 2015;217:143–58. [DOI] [PubMed] [Google Scholar]
- 66.Lee JH. The Effects of Music on Pain: A Meta-Analysis. J Music Ther 2016;53:430–77. [DOI] [PubMed] [Google Scholar]
- 67.Bradt J, Dileo C, Magill L, Teague A. Music interventions for improving psychological and physical outcomes in cancer patients. Cochrane Database Syst Rev 2016:CD006911. [DOI] [PubMed] [Google Scholar]
- 68.Bro ML, Jespersen KV, Hansen JB, et al. Kind of blue: A systematic review and meta-analysis of music interventions in cancer treatment. Psychooncology 2018;27:386–400. [DOI] [PubMed] [Google Scholar]
- 69.Volpe U, Gianoglio C, Autiero L, et al. Acute Effects of Music Therapy in Subjects With Psychosis During Inpatient Treatment. Psychiatry 2018;81:218–27. [DOI] [PubMed] [Google Scholar]
- 70.Helgason C, Sarris J. Mind-body medicine for schizophrenia and psychotic disorders: a review of the evidence. Clin Schizophr Relat Psychoses 2013;7:138–48. [DOI] [PubMed] [Google Scholar]