Abstract
Aims:
Compare the incidence and costs of urgent and low acuity ED presentations of people with opioid use disorder (OUD) while in and out of opioid agonist treatment (OAT).
Design:
Retrospective cohort study using linked administrative health data.
Setting:
New South Wales (NSW), Australia.
Participants:
24,875 people receiving OAT between 1st January 2012 and 30th September 2014.
Measurements:
Urgent and low acuity ED incidence and associated costs were calculated for periods in and out of OAT. GEE models estimated the adjusted incidence rate ratio (IRR) for ED presentations. Average costs per person-day were calculated with 95% bootstrap confidence intervals. Interactions with geographical remoteness were examined.
Findings:
Incidence of urgent presentations was lower in OAT compared to out of OAT [IRR (95%CI): 0.65 (0.61–0.69)]. In major cities, low acuity presentations were less frequent during OAT compared to time out of OAT [IRR (95%CI): 0.82 (0.70–0.96)], but in regional/remote areas, low acuity presentations were more common during OAT compared to out of OAT [IRR (95%CI): 2.65 (1.66–4.21)]. In major cities, average costs for low acuity presentations in OAT were 28% lower than out of OAT at A$0.50 (95%CI: A$0.48-A$0.52) and A$0.69 (95%CI: A$0.66-A$0.71), respectively, but 103% higher in regional/remote NSW, at A$2.12 (95%CI: A$1.91-A$2.34) in OAT and A$1.04 (95%CI: A$0.91-A$1.16) out of OAT.
Conclusion:
OAT was associated with reductions in urgent ED presentations and associated costs among people with OUD. Geographical variation was evident for low acuity ED presentations, highlighting the need to increase access to OAT in regional/remote areas of NSW.
Keywords: Opiate substitution treatment, Emergency medical services, Health services geographic accessibility, methadone, buprenorphine
INTRODUCTION
Emergency department (ED) presentations in Australia are increasing at rates greater than population growth [1, 2]. Low acuity presentations (i.e. those that are triaged as semi-urgent or non-urgent based on the Australasian Triage Scale), have been examined for their impact on ED presentation rates, overcrowding, and functioning. Although these presentations do not appear to impact on overcrowding or ED waiting times [3], low acuity presentations among vulnerable populations are associated with significant costs to public health systems and may indicate poor access to primary care, particularly in regional areas [4–6].
People with opioid use disorder (OUD) have higher rates of emergency department (ED) presentation than the general population [7, 8]. Data on reasons for ED presentation by people with OUD are scarce, but among people who use and inject drugs (commonly opioids), the most frequent reasons for ED presentation are drug-related, including overdose and skin and soft-tissue infections [9, 10]. In one cohort of people who inject drugs (72% of whom injected opioids), almost half of all ED presentations were triaged as semi-urgent or non-urgent [8]. Although this is similar to the proportion of semi-urgent and non-urgent presentations nationally [11], given their higher overall presentation rates, reducing low acuity presentations among people with OUD may provide particular benefits.
Opioid agonist treatment (OAT) with methadone or buprenorphine is an effective treatment for OUD that reduces extra-medical opioid use, leading to a range of positive clinical outcomes including reduced injecting drug use, overdose and all-cause mortality [12]. Reductions in ED use have been shown during periods of OAT compared to periods out of OAT or compared to people with OUD receiving non-pharmacological treatments [13]. It is not known if this reduction occurs across both urgent and low acuity presentations, or in rural areas where access to health care services may be limited relative to urban areas. Understanding the extent to which urgent and low acuity ED presentations are separately affected by OAT can provide important insights into the health care needs of people with OUD. Declines in urgent ED presentations during OAT could suggest reductions in acute, life-threatening events such as overdose, while ongoing urgent ED presentations while in OAT may indicate poor management of OUD. Ongoing low acuity ED presentations in OAT may suggest limited access to primary care. We aimed to examine the association between receipt of OAT and both urgent and low acuity ED presentations. Specifically, we compared the incidence and associated costs of urgent and low acuity ED presentations during OAT to those during time out of OAT.
METHODS
This was a retrospective cohort study using state-wide linked administrative health data in New South Wales, Australia.
Ethical review
Approval for this study was obtained from the New South Wales (NSW) Population & Health Services Research Ethics Committee and the Australian Institute of Health and Welfare.
Setting and data sources
NSW is the most populous state in Australia and provides care for around 40% of all people receiving OAT [14]. In NSW, methadone and buprenorphine for the treatment of OUD are prescribed in various settings, including public and private outpatient clinics and primary care, and dispensed in outpatient clinics, pharmacies, and hospitals, as well as through the correctional system. The most common model of OAT care is prescribing of treatment in primary care, with medicine dispensed in a community pharmacy [14]. All OAT prescriptions require an authority from the Pharmaceutical Services Branch (PSB) of the NSW Ministry of Health. A prescriber must request an authority from the PSB for a patient and report to the PSB when a patient exits the program.
Opioid agonist treatment data: The Pharmaceutical Drugs of Addiction System
All authorities and exits from OAT are recorded in the Pharmaceutical Drugs of Addiction System (PHDAS), which is a complete record of OAT in NSW. The PHDAS was implemented in 1985 and includes details on all clients participating in the NSW Opioid Treatment Program including full name, date of birth, gender, and postcode of residence. Identifiers are considered reliable because proof of identity must be shown to the prescribing doctor before a prescription can be issued.
Emergency presentation data: Emergency Department Data Collection
The Emergency Department Data collection (EDDC) is maintained by the NSW Ministry of Health and provides information about presentations to EDs of public hospitals in NSW. The data items included are demographic information, triage category, primary diagnosis, and other clinical information. Records date from January 2005, but not all EDs reported to the EDDC from this time. The impact of this on the linkage and analysis is discussed further below.
Death data: National Death Index
The National Death Index (NDI) is administered by the Australian Institute of Health and Welfare and records deaths in Australia since 1980. In this study, mortality data were used only for calculation of person days of observation.
Data linkage and cohort definition
Linkage of the PHDAS cohort to the EDDC was completed by the Centre for Health Record Linkage (CHeReL). The CHeReL uses best practice privacy preserving record linkage procedures, such that no health information is used in the linkage process, and only de-identified data are released to researchers. Probabilistic linkage was completed using ChoiceMaker software to match records from each database using names, gender, date of birth and state of residence. Linkage between the PHDAS and EDDC was completed for 2005–2014 (the years for which ED data were available).
Deaths within the cohort were identified through linkage of the PHDAS to the NDI. Linkage was undertaken by the Australian Institute of Health and Welfare using similar protocols as described above, and was based on full name, gender, date of birth and state of residence.
The planned analyses were to use data from 2005–2014 inclusive, including all people receiving OAT during that time frame. However, during the preliminary analyses the number of presentations reported annually from the EDDC increased between 2005 and 2012. Between 2010 and 2012 there was a 19% increase in ED episodes reported in major cities, however a 115% increase in regional\remote NSW, (Supplementary Material, Figure S1). This trend stabilised from 2012 onwards, suggesting stable EDDC coverage in urban and regional/remote areas; as such, the cohort was limited to all people with an eligible episode of OAT between 2012 and 2014.
Definitions and data analysis
In keeping with previous studies, a new OAT episode was defined as one commencing seven or more days after the end date of a prior treatment episode. The same definition was used for defining the end of programme, treating the 6 days following the programme as part of the programme when allocating ED presentations to time in OAT or out of OAT [15]. Ineligible OAT episodes included participants on temporary programmes (usually interstate visitors) or withdrawal programs. Participants aged less than 18 years were excluded.
ED presentations were considered urgent if the triage category assigned to the presentation was resuscitation, emergency or urgent. Presentations with a triage scale of semi-urgent or non-urgent were categorised as low acuity [8].
Person-days (PD) of observation for the calculation of urgent and low acuity incidence rates began at the 1st January 2012 for participants on OAT prior to 2012 or the date of first entry to OAT episode (for dates greater than or equal to 1st January 2012), and ceased accruing at the earliest of death, 24 months post the last OAT episode end date, or 31 September 2014. Person-days were allocated to time in OAT or out of OAT per the definitions above.
Poisson regression models estimated the adjusted incidence rate ratio (IRR) for ED presentations per 100 person-years (PY), using a generalised estimating equation (GEE) approach to account for multiple observations per participant.
Previous studies have shown that age, gender and accessibility/remoteness are important covariates when examining people with OUD [15–17]. Age was categorised as: <30, 30–39, 40–49, and 50+ years. Remoteness area (major cities vs regional/remote) was included as a covariate by matching each participant’s postcode of residence with the postcode in the Accessibility/Remoteness Index of Australia Plus (ARIA+) 2016 [18]. Postcode was carried forward to time out of OAT. Due to the varying number of EDs providing data each year, the year of presentation was adjusted for in the GEE.
Unadjusted and adjusted incidence rates were calculated for time in and out of OAT; marginal estimates were used to adjust for the covariates already discussed. The two-way interactions considered were OAT status with gender, age and remoteness areas. Non-significant interactions were removed using a backward stepwise approach. Tukey-Kramer adjustment for multiple comparison testing was used to hold the experimentwise error rate at 5% when comparing incidence rates for interaction terms.
To compare the ED utilisation costs between OAT periods, each episode was assigned an associated cost. All presentations were processed using the cost weights from 2014–2015. Costs were based on a combination of triage category and mode of separation. Presentations were assigned an average cost in Australian dollars (AUD) by either using the Urgency Related Group (URG) description from the “16 URG table” of the National Hospital Cost Data Collection, Cost Weights for URG Version.4.3, Round 19 (2014–15) [19], or an average of the mode of separation (for admitted & non-admitted presentations) by triage category costings. A summary of cost group assignment and methodology can be found in the supplementary materials (Tables S1–S4). Confidence intervals were calculated using bootstrapping. Analyses were conducted in SAS V9.4 (SAS Institute Inc. Cary, NC, USA). All reported p-values are two-sided and considered significant at p < 0.05.
RESULTS
There were 55,468 participants in the PHDAS database from 1985 onwards; after data cleaning and application of exclusion criteria, there were 24,875 participants who received OAT between 1st Jan 2012 and 31st Sep 2014 (Figure S2). Two-thirds of the cohort was male (67%; n=16,682), the median age at the beginning of 2012 was 38 years, and 73% (n=18,213) resided in major cities.
Initial analyses identified participants with high frequency presentations, sometimes daily, with a diagnosis code that repeated for many months. Most of these participants resided in regional/remote NSW and most of the presentations occurred while in OAT (Supplementary materials, Figure S3). Discussion with OAT prescribers identified that EDs in these areas may provide a dispensing service for OAT. To explore this possibility, we examined diagnosis codes associated with high-frequency, low acuity presentations. No specific code for OAT dispensing exists, but multiple codes suggestive of this activity were identified (e.g. “Issue of repeat prescriptions”). Supplementary table S4 provides a complete list of codes explored for this purpose and codes used to define suspected OAT dosing episodes. High-frequency low acuity presentations with these codes were flagged as suspected dosing episodes and a sensitivity analysis was undertaken excluding all presentations with these diagnosis codes. The incident rates of all low acuity presentations were compared with the incident rates excluding suspected dosing presentations.
Between 1st January 2012 and 30th September 2014, there were 92,987 ED presentations. Only 0.3% (n=284) presentations were missing a triage category. These were excluded from the incidence rate analysis as urgency could not be defined but included in the overall cost analysis. Of the presentations with a triage category, 68.2% (n=63,432) were classified as low acuity (Table 1). However, when considering remoteness area, 52.8% of presentations in major cities were low acuity compared with 85.5% in regional/remote NSW.
Table 1:
Participant characteristics and characteristics of included ED presentations (2012–14)
| Participants (n=24,875) | |
|---|---|
| Gender | N (%) |
| Male | 16,682 (67.1%) |
| Female | 8,193 (32.9%) |
| Geographic remoteness | |
| Major Cities NSW | 18,214 (73.2%) |
| Regional/Remote NSW | 6,200 (24.9%) |
| Other | 461 (1.9%) |
| Median age in years (IQR) at cohort entry | 38 (31–46) |
| Number of presentations | N (%) |
| None | 10,022 (40.3%) |
| 1–2 | 7,732 (31.1%) |
| 3–4 | 2,959 (11.9%) |
| 5–10 | 2,882 (11.6%) |
| 11–1333 | 1,280 (5.1%) |
| ED Participants (n=14,853) | |
| Gender | N (%) |
| Male | 9,746 (65.6%) |
| Female | 5,107 (34.4%) |
| Geographic remoteness | |
| Major Cities NSW | 10,735 (72.3%) |
| Regional/Remote NSW | 3,828 (25.8%) |
| Other | 290 (2.0%) |
| Median age in years (IQR) at cohort entry | 38 (31–45) |
| ED Presentations (n=92,987) | |
| Triage category | N (%) |
| Urgent | 29,271 (31.5%) |
| Low acuity | 63,432 (68.2%) |
| Other | 284 (0.3%) |
| Major Cities NSW - ED Triage Scale | |
| Urgent | 22,180 (46.9%) |
| Low acuity | 24,944 (52.8%) |
| Other | 128 (0.3%) |
| Regional/Remote NSW - ED Triage Scale | |
| Urgent | 6,229 (14.3%) |
| Low acuity | 37,090 (85.3%) |
| Other | 144 (0.3%) |
| Unknown - ED Triage Scale | |
| Urgent | 862 (37.9%) |
| Low acuity | 1,398 (61.5%) |
| Other | 12 (0.5%) |
There were 461 (1.9%) participants missing a remoteness area value, which led to 2,272 presentations in total (2.4%) being excluded from the analysis.
Incidence of urgent presentations
There were 28,409 urgent ED presentations in 61,031 person-years (PY). The adjusted incidence rate of urgent presentations per 100 PY was significantly lower during OAT compared to not in OAT: [IRR (95%CI): 0.65 (0.61, 0.69)] (Table 2). There was no evidence of significant interaction terms.
Table 2:
Rates of Urgent ED presentations per 100 person-years in and out of OAT (2012–14)
| Urgent presentations | n | PY | IR | IRR (95% CI) | Adjusted IRa (95% CI) | Adjusted IRRa (95% CI) | Effect P value |
|---|---|---|---|---|---|---|---|
| OAT Status | P < 0.001 | ||||||
| In OAT | 20,040 | 48,014 | 41.7 (40.4, 43.1) | 0.65 (0.61, 0.69) | 41.6 (40.2, 42.9) | 0.65 (0.61, 0.69) | |
| Out of OAT | 8,369 | 13,017 | 64.3 (61.2, 67.6) | Ref. | 64.1 (60.9, 67.4) | Ref. | |
| Age in Years | P = 0.02 | ||||||
| 18–29 yrs | 5,369 | 10,070 | 53.3 (50.1, 56.8) | Ref. | 50.8 (47.7, 54.1) | Ref. | |
| 30–39 yrs | 10,349 | 22,784 | 45.4 (43.4, 47.5) | 0.85 (0.79, 0.92) | 44.9 (43.0, 47.0) | 0.88 (0.82, 0.95) | |
| 40–49 yrs | 8,075 | 17,997 | 44.9 (42.5, 47.4) | 0.84 (0.77, 0.91) | 45.9 (43.5, 48.5) | 0.90 (0.83, 0.98) | |
| 50+ yrs | 4,616 | 10,179 | 45.3 (41.4, 49.7) | 0.85 (0.76, 0.95) | 47.4 (43.2, 51.9) | 0.93 (0.83, 1.04) | |
| Area of Residence | P < 0.001 | ||||||
| Major Cities of NSW | 22,180 | 46,038 | 48.2 (46.5, 49.9) | 1.16 (1.09, 1.23) | 48.5 (46.9, 50.2) | 1.17 (1.10, 1.25) | |
| Regional/Remote NSW | 6,229 | 14,993 | 41.5 (39.5, 43.7) | Ref. | 41.4 (39.3, 43.6) | Ref. | |
| Gender | P < 0.001 | ||||||
| Female | 10,106 | 20,254 | 49.9 (47.5, 52.4) | 1.11 (1.05, 1.18) | 50.8 (48.4, 53.3) | 1.13 (1.07, 1.20) | |
| Male | 18,303 | 40,778 | 44.9 (43.2, 46.6) | Ref. | 44.8 (43.2, 46.4) | Ref. | |
| Year | P = 0.05 | ||||||
| 2012 | 9,702 | 21,501 | 45.1 (43.4, 46.9) | Ref. | 45.4 (43.8, 47.2) | Ref. | |
| 2013 | 10,717 | 22,485 | 47.7 (45.9, 49.4) | 1.06 (1.02, 1.10) | 47.6 (46.0, 49.4) | 1.05 (1.01, 1.09) | |
| 2014 | 7,990 | 17,045 | 46.9 (45.1, 48.7) | 1.04 (0.99, 1.09) | 46.9 (45.1, 48.7) | 1.03 (0.99, 1.08) |
Adjusted for all other variables shown. PY: person-years of observation. IR: incidence rate. CI: confidence interval. IRR: incidence rate ratio. OAT: opioid agonist therapy.
Incidence of low acuity presentations
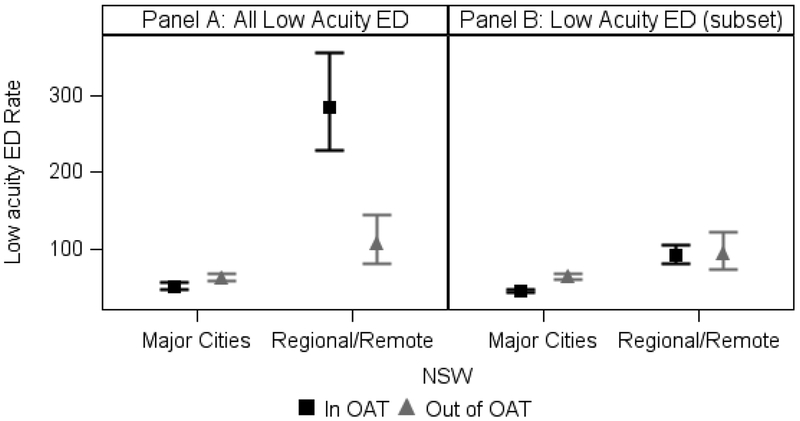
There were 62,034 low acuity ED presentations in 61,031 person-years (PY). The main effects for OAT status and remoteness area were not reported due to a significant interaction, (P < 0.001). Figure 1, panel A, and Table 3 illustrates the difference in incidence of low acuity presentations while in OAT and out of OAT by remoteness areas. The adjusted incidence of low acuity presentations in OAT in major cities of NSW was 51 per 100 PY compared to 285 per 100 PY for regional/remote NSW. The corresponding rates not in OAT were 62 per 100 PY and 107 per 100 PY, respectively. There was a significantly higher incidence of low acuity presentations in OAT in regional/remote NSW compared to out of OAT [IRR (95%CI): 2.65 (1.66–4.21)], but significantly lower incidence in the major cities [IRR (95%CI): 0.82 (0.70–0.96)].
Figure 1.
Average low acuity incidence rate per 100 person-years for treatment status by remoteness area (2012–2014)
Table 3:
Rates of All low acuity ED presentations per 100 person-years in and out of OAT (2012–14)
| Low acuity presentations | n | PY | IR | IRR (95% CI) | Adjusted IRa (95% CI) | Adjusted IRRa (95% CI) | Effect P value |
|---|---|---|---|---|---|---|---|
| OAT Status | P < 0.001 | ||||||
| In OAT | 51,752 | 48,014 | 107.8 (92.9, 125.1) | 1.36 (1.14, 1.63) | N/A | N/A | |
| Out of OAT | 10,282 | 13,017 | 79.0 (70.5, 88.5) | Ref. | N/A | N/A | |
| Age in Years | P < 0.001 | ||||||
| 18–29 yrs | 13,282 | 10,070 | 131.9 (101.8, 170.9) | Ref. | 101.3 (79.7, 128.7) | Ref. | |
| 30–39 yrs | 25,432 | 22,784 | 111.6 (89.9, 138.6) | 0.85 (0.60, 1.19) | 86.1 (72.3, 102.4) | 0.85 (0.61, 1.19) | |
| 40–49 yrs | 16,666 | 17,997 | 92.6 (73.0, 117.5) | 0.70 (0.49, 1.00) | 67.9 (54.4, 84.7) | 0.67 (0.47, 0.95) | |
| 50+ yrs | 6,654 | 10,179 | 65.4 (48.6, 88.0) | 0.50 (0.33, 0.73) | 48.5 (36.0, 65.3) | 0.48 (0.32, 0.71) | |
| Area of Residence | P < 0.001 | ||||||
| Major Cities of NSW | 24,944 | 46,038 | 54.2 (50.3, 58.3) | 0.22 (0.18, 0.27) | N/A | N/A | |
| Regional/Remote NSW | 37,090 | 14,993 | 247.4 (201.4, 303.9) | Ref. | N/A | N/A | |
| Gender | P = 0.86 | ||||||
| Female | 21,774 | 20,254 | 107.5 (86.3, 134.0) | 1.09 (0.83, 1.43) | 77.3 (64.5, 92.6) | 1.02 (0.78, 1.34) | |
| Male | 40,260 | 40,778 | 98.7 (84.5, 115.3) | Ref. | 75.5 (66.7, 85.4) | Ref. | |
| Year | P = 0.66 | ||||||
| 2012 | 22,207 | 21,501 | 103.3 (88.4, 120.7) | Ref. | 78.7 (70.7, 87.7) | Ref. | |
| 2013 | 22,728 | 22,485 | 101.1 (88.5, 115.4) | 0.98 (0.89, 1.08) | 75.6 (69.5, 82.3) | 0.96 (0.87, 1.06) | |
| 2014 | 17,099 | 17,045 | 100.3 (87.4, 115.1) | 0.97 (0.84, 1.12) | 73.9 (66.8, 81.8) | 0.94 (0.82, 1.08) | |
| Area*OAT | P < 0.001 | ||||||
| Major Cities of NSW*In OAT | 18,481 | 36,329 | 50.9 (46.2, 56.0) | 0.76 (0.68, 0.86) | 51.0 (46.2, 56.2) | 0.82 (0.70, 0.96) | |
| Major Cities of NSW*Out of OAT | 6,463 | 9,710 | 66.6 (62.4, 71.0) | Ref. | 62.1 (57.4, 67.3) | Ref. | |
| Regional/Remote NSW*In OAT | 33,271 | 11,685 | 284.7 (227.5, 356.4) | 2.47 (1.74, 3.50) | 284.9 (228.5, 355.3) | 2.65 (1.66, 4.21) | |
| Regional/Remote NSW*Out of OAT | 3,819 | 3,307 | 115.5 (86.8, 153.6) | Ref. | 107.6 (80.6, 143.6) | Ref. |
Adjusted for all other variables shown. PY: person- years of observation. IR: incidence rate. CI: confidence interval. IRR: incidence rate ratio. OAT: opioid agonist therapy.
The sensitivity analysis, fitting a GEE model with suspected OAT dosing presentations excluded, revealed a significantly lower incidence of low acuity presentations in the major cities, corroborating the previous analysis, [IRR (95%CI): 0.71 (0.64–0.79)]. However, as shown in Table 4 and Figure 1, panel B, there was no evidence of a significant difference in regional/remote NSW, [IRR (95%CI): 0.97 (0.68–1.39)].
Table 4:
Rates of low acuity ED presentations, excluding OAT dosing episodes, per 100 person-years in and out of OAT (2012–14)
| Low acuity presentations | n | PY | IR | IRR (95% CI) | Adjusted IRa (95% CI) | Adjusted IRRa (95% CI) | Effect P value |
|---|---|---|---|---|---|---|---|
| OAT Status | P < 0.001 | ||||||
| In OAT | 26,938 | 48,014 | 56.1 (52.9, 59.6) | 0.77 (0.69, 0.85) | N/A | N/A | |
| Out of OAT | 9,534 | 13,017 | 73.2 (66.4, 80.8) | Ref. | N/A | N/A | |
| Age in Years | P < 0.001 | ||||||
| 18–29 yrs | 6,863 | 10,070 | 68.2 (62.9, 73.8) | Ref. | 63.9 (58.9, 69.4) | Ref. | |
| 30–39 yrs | 15,039 | 22,784 | 66.0 (59.4, 73.4) | 0.97 (0.85, 1.11) | 63.9 (58.1, 70.3) | 1.00 (0.87, 1.15) | |
| 40–49 yrs | 9,930 | 17,997 | 55.2 (50.2, 60.6) | 0.81 (0.72, 0.92) | 53.7 (49.0, 58.7) | 0.84 (0.74, 0.95) | |
| 50+ yrs | 4,640 | 10,179 | 45.6 (41.3, 50.4) | 0.67 (0.59, 0.76) | 45.2 (40.8, 50.0) | 0.71 (0.62, 0.80) | |
| Area of Residence | P < 0.001 | ||||||
| Major Cities of NSW | 22,620 | 46,038 | 49.1 (47.3, 51.1) | 0.53 (0.47, 0.61) | N/A | N/A | |
| Regional/Remote NSW | 13,852 | 14,993 | 92.4 (81.3, 105.0) | Ref. | N/A | N/A | |
| Gender | P = 0.38 | ||||||
| Female | 12,466 | 20,254 | 61.5 (56.3, 67.3) | 1.05 (0.93, 1.17) | 59.0 (54.4, 64.0) | 1.03 (0.92, 1.15) | |
| Male | 24,006 | 40,778 | 58.9 (55.0, 63.0) | Ref. | 57.1 (53.8, 60.6) | Ref. | |
| Year | P = 0.10 | ||||||
| 2012 | 13,116 | 21,501 | 61.0 (56.6, 65.7) | Ref. | 59.4 (55.8, 63.2) | Ref. | |
| 2013 | 12,843 | 22,485 | 57.1 (54.2, 60.2) | 0.94 (0.87, 1.01) | 55.0 (52.3, 57.7) | 0.93 (0.86, 1.00) | |
| 2014 | 10,513 | 17,045 | 61.7 (56.6, 67.2) | 1.01 (0.92, 1.11) | 59.0 (54.7, 63.6) | 0.99 (0.91, 1.09) | |
| Area*OAT | P = 0.002 | ||||||
| Major Cities of NSW*In OAT | 16,288 | 36,329 | 44.8 (42.9, 46.9) | 0.69 (0.64, 0.74) | 45.2 (43.2, 47.3) | 0.71 (0.64, 0.79) | |
| Major Cities of NSW*Out of OAT | 6,332 | 9,710 | 65.2 (61.1, 69.6) | Ref. | 63.5 (59.3, 67.9) | Ref. | |
| Regional/Remote NSW*In OAT | 10,650 | 11,685 | 91.1 (79.7, 104.2) | 0.94 (0.72, 1.24) | 91.9 (80.5, 104.9) | 0.98 (0.68, 1.39) | |
| Regional/Remote NSW*Out of OAT | 3,202 | 3,307 | 96.8 (74.4, 125.9) | Ref. | 94.2 (72.5, 122.4) | Ref. |
Adjusted for all other variables shown. PY: person- years of observation. IR: incidence rate. CI: confidence interval. IRR: incidence rate ratio. OAT: opioid agonist therapy.
Cost comparison
The average cost per PD for urgent presentations was 34% lower in OAT at A$0.95 (95%CI: A$0.93-A$0.97) than out of OAT at A$1.45 (95%CI: A$1.41-A$1.49). The average cost per PD for low acuity presentations in major cities of NSW was 28% lower at A$0.50 (95%CI: A$0.48-A$0.52) during OAT compared to out of OAT at A$0.69 (95%CI: A$0.66-A$0.71). The reverse was true for remote/regional NSW where the average cost per PD was 103% higher at A$2.12 (95%CI: A$1.91-A$2.34) during OAT compared to out of OAT at A$1.04 (95%CI: A$0.91-A$1.16). Table 5 provides the average cost per PD and 95% confidence intervals in and out of OAT, for all presentations and by acuity.
Table 5:
Average Cost (AUD)^ of ED presentations per person-day by acuity (2012–14)
| ED Acuity | Costs in OAT (95% CI) | Costs out of OAT (95% CI) | % change in cost from in OAT |
|---|---|---|---|
| Accessibility | |||
| Low acuity ED presentation | |||
| Major cities of NSW | $0.45 ($0.44–$0.47) | $0.68 ($0.65–$0.70) | −33% |
| Regional/Remote NSW | $0.80 ($0.74–$0.85) | $0.92 ($0.81–$1.00) | −13% |
| Total | $0.54 ($0.53–$0.56) | $0.74 ($0.71–$0.77) | −26% |
| Low acuity ED presentation | |||
| Major cities of NSW | $0.50 ($0.48–$0.52) | $0.69 ($0.66–$0.71) | −28% |
| Regional/Remote NSW | $2.12 ($1.91–$2.34) | $1.04 ($0.91–$1.16) | +103% |
| Total | $0.90 ($0.84–$0.95) | $0.78 ($0.74–$0.81) | +16% |
| Urgent ED presentation | |||
| Major cities of NSW | $0.98 ($1.45–$1.49) | $1.51 ($2.17–$2.22) | −35% |
| Regional/Remote NSW | $0.83 ($2.74–$3.17) | $1.23 ($2.14–$2.39) | −32% |
| Total | $0.95 ($0.93–$0.97) | $1.45 ($1.41–$1.49) | −34% |
| All ED presentation | |||
| Major cities of NSW | $1.47 ($1.44–$1.51) | $2.20 ($2.13–$2.27) | −33% |
| Regional/Remote NSW | $2.96 ($2.74–$3.18) | $2.28 ($2.12–$2.43) | +30% |
| Total | $1.86 ($1.80–$1.91) | $2.23 ($2.17–$2.29) | −17% |
Based on 2014–2015 cost weights.
Suspected OAT dosing presentations have been excluded
DISCUSSION
Using linked administrative data on OAT and ED presentations, this study has identified that among people with OUD, urgent ED presentations and associated costs are reduced during periods of OAT relative to periods out of OAT. This difference was seen regardless of geographical remoteness and suggests that life-threatening events (e.g. overdose) are reduced in frequency while in OAT. This likely also provides a population health benefit in releasing emergency healthcare resources.
A more complex picture was identified in relation to low acuity ED presentations. Two-thirds of all ED presentations in this cohort were low acuity, compared to 49% of ED presentations among the Australian population [11]. For OAT clients in major cities, low acuity presentations were significantly less frequent during periods of treatment compared to time out of treatment. This was not the case in regional/remote areas. Examination of diagnosis codes identified repeated ED presentations that were likely made for the purpose of receiving OAT. Hence, we attribute the higher incidence of low acuity presentations in regional/remote areas during OAT to the practice of OAT dosing in ED. When these presentations were removed from the analysis, there was no difference in incidence of low acuity ED presentations in regional/remote areas by OAT status.
These findings likely reflect difficulties in accessing OAT, and possibly primary care more broadly, in regional/remote NSW. Most OAT in NSW is prescribed in primary care, with dispensing of methadone or buprenorphine in community pharmacies [14], but people living outside major cities may have difficulties accessing a community-based general practitioner who prescribes OAT. A study of OAT in one geographically large but sparsely populated area in NSW found that OAT prescribers travel to clinics where local general practitioners are limited or not available, but caseloads are high and there may be a wait of 2–3 weeks for an appointment [20]. Similar issues are apparent in relation to dosing points. In 2017, nearly two-thirds of NSW dosing sites were in major cities [14]. OAT clients and prescribers in regional and remote areas have identified extensive travel times, and the impact that this has on employment opportunities, as important barriers to accessing treatment [21, 22]. There may be as few as 1.7 pharmacies providing OAT dosing per 10,000 km2 outside of major cities in NSW (see supplementary materials for details), making accessing OAT-dosing pharmacies outside of major cities a significant challenge.
A lack of primary care-based prescribers and difficulty in accessing dosing sites has been reported to create ‘bottlenecks’ in specialist services in regional/remote areas, such that clients remain in specialist services such as those located in hospitals in these areas [20]. Our findings suggest that OAT clients are using ED for treatment dispensing in regional/remote NSW. This analysis alludes that there is still a need to increase accessibility of OAT in regional/remote areas of NSW, and Australia, through greater numbers of prescribers in primary care settings and flexible dosing in community settings, including but not limited to pharmacies and community health centres. Consideration of models of care that permit unobserved home induction of buprenorphine, as are used in several countries, is warranted [23].
These findings contribute to the growing body of evidence documenting reductions in health service use and associated costs among people with OUD while prescribed OAT. Such studies have largely been undertaken in the United States, using state-based Medicaid data or insurance claims databases [12, 13]. Our study suggests these benefits are obtained in a setting with universal health care, while identifying that benefits may not translate to geographical areas with limited access to OAT.
Limitations
This study was based on linked, administrative datasets. We are confident in the quality of linkage; the identifiers in PHDAS are considered to be reliable as patients are required to show identification to receive a prescription, and patients are typically required to show their identification (Medicare card) when presenting at an ED.
Person days of observation was not adjusted for time in custody, during which people may be somewhat protected from common causes of urgent ED presentation (e.g. overdose) and are unlikely to be transported to ED for low acuity issues. Person days were also not adjusted for hospitalisations. We endeavoured to identify OAT dosing episodes within ED settings and exclude these from our sensitivity analysis, but it is unclear if all dosing episodes were excluded as a range of diagnostic codes for this service were entered at the point of care. As such, the incidence of non-OAT related low acuity presentations in OAT in regional/remote areas may be over-estimated.
Conclusions
OAT is beneficial in reducing urgent ED presentations and costs among people with opioid use disorders. Low acuity ED presentations are reduced during OAT in major cities, but the association between OAT and low acuity ED presentations in regional/remote NSW is less clear due to difficulties in identifying OAT dosing episodes in ED. These findings highlight the need to improve access to OAT in regional and remote areas of NSW.
Supplementary Material
Acknowledgements
The authors wish to acknowledge all data custodians for providing access to the datasets used in this study: the NSW Ministry of Health (PHDAS, EDDC, & APDC dataset), the Australian Institute of Health and Welfare (NDI dataset).
Funding
This study was funded by NHMRC Centre of Research Excellence in Injecting Drug Use and NIDA R01DA1104470. LD and SL are supported by NHMRC Research Fellowships (GNT1135991, GNT1140938) and NIDA R01DA1104470. NG and SL are supported by UNSW Scientia Fellowships. The National Drug and Alcohol Research Centre at UNSW Australia is supported by funding from the Australian Government Department of Health under the Drug and Alcohol Program.
Footnotes
Ethics committee approval
This study was approved by the Population and Health Services Research Ethics Committee and the Australian Institute of Health and Welfare Research Ethics Committee.
Declaration of interests
SL has received untied education funding from Indivior. LD has received untied educational funding from Indivior, Mundipharma, and Seqirus. MM has received untied educational funding from Pfizer and AbbVie.
References
- 1.Dinh MM, Berendsen Russell S, Bein KJ, Chalkley D, Muscatello D, Paoloni R, et al. Understanding drivers of demand for emergency service trends in years 2010–2014 in New South Wales: An initial overview of the DESTINY project. Emerg Med Australas. 2016;28:179–86. [DOI] [PubMed] [Google Scholar]
- 2.Lowthian JA, Curtis AJ, Jolley DJ, Stoelwinder JU, McNeil JJ, Cameron PA. Demand at the emergency department front door: 10-year trends in presentations. Medical J Australia. 2012;196(2):128–32. [DOI] [PubMed] [Google Scholar]
- 3.Nagree Y, Camarda VJ, Fatovich DM, Cameron PA, Dey I, Gosbell AD, et al. Quantifying the proportion of general practice and low-acuity patients in the emergency department. Medical J Australia. 2013;198:612–5. [DOI] [PubMed] [Google Scholar]
- 4.Allen P, Cheek C, Foster S, Ruigrok M, Wilson D, Shires L. Low acuity and general practice-type presentations to emergency departments: a rural perspective. Emerg Med Australas. 2015;27:113–8. [DOI] [PubMed] [Google Scholar]
- 5.Stephens AS, Broome RA. Patterns of low acuity patient presentations to emergency departments in New South Wales, Australia. Emerg Med Australas. 2017;29:283–90. [DOI] [PubMed] [Google Scholar]
- 6.Islam MM, Topp L, Day CA, Dawson A, Conigrave KM. The accessibility, acceptability, health impact and cost implications of primary healthcare outlets that target injecting drug users: a narrative synthesis of literature. Int J Drug Policy. 2012;23(2):94–102. [DOI] [PubMed] [Google Scholar]
- 7.O’Toole J, Hambly R, Cox AM, O’Shea B, Darker C. Methadone-maintained patients in primary care have higher rates of chronic disease and multimorbidity, and use health services more intensively than matched controls. Eur J Gen Pract. 2014;20(4):275–80. [DOI] [PubMed] [Google Scholar]
- 8.Nambiar D, Spelman T, Stoové M, Dietze P. Are People Who Inject Drugs Frequent Users of Emergency Department Services? A Cohort Study (2008–2013). Subst Use Misuse. 2018;53(3):457–65. [DOI] [PubMed] [Google Scholar]
- 9.Aitken C, Kerr T, Hickman M, Stoové M, Higgs P, Dietze P. A cross-sectional study of emergency department visits by people who inject drugs. Emerg Med J. 2012;30:421–2. [DOI] [PubMed] [Google Scholar]
- 10.Nambiar D, Stoové M, Dietze P. Frequent emergency department presentations among people who inject drugs: A record linkage study. Int J Drug Policy. 2017;44:115–20. [DOI] [PubMed] [Google Scholar]
- 11.AIHW. Emergency department care 2017–18: Australian hospital statistics [Internet]. Canberra: Australian Institute of Health and Welfare; 2018. [Google Scholar]
- 12.Schwarz R, Zelenev A, Bruce RD, Altice FL. Retention on buprenorphine treatment reduces emergency department utilization, but not hospitalization, among treatment-seeking patients with opioid dependence. J Subst Abuse Treat. 2012;43(4):451–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mohlman MK, Tanzman B, Finison K, Pinette M, Jones C. Impact of Medication-Assisted Treatment for Opioid Addiction on Medicaid Expenditures and Health Services Utilization Rates in Vermont. J Subst Abuse Treat. 2016;67:9–14. [DOI] [PubMed] [Google Scholar]
- 14.AIHW. National opioid pharmacotherapy statistics (NOPSAD) [Internet]. Web Page. Canberra: Australian Institute of Health and Welfare; 2017. 2017. [Google Scholar]
- 15.Degenhardt L, Randall D, Hall W, Law M, Butler T, Burns L. Mortality among clients of a state-wide opioid pharmacotherapy program over 20 years: risk factors and lives saved. Drug Alcohol Depend. 2009;105(1–2):9–15. [DOI] [PubMed] [Google Scholar]
- 16.Larney S, Grebely J, Falster M, Swart A, Amin J, Degenhardt L, et al. Opioid substitution therapy is associated with increased detection of hepatitis C virus infection: a 15-year observational cohort study. Drug Alcohol Depend. 2015;148:213–6. [DOI] [PubMed] [Google Scholar]
- 17.Iversen J, Dertadian G, Geddes L, Maher L. High risk injecting behaviour among people who inject pharmaceutical opioids in Australia. Int J Drug Policy. 2017;42:1–6. [DOI] [PubMed] [Google Scholar]
- 18.Australian Bureau of Statistics. The Australian Standard Geographical Classification (ASGC) Remoteness Structure [cited 2019 11th March]. Available from: https://www.abs.gov.au/ausstats/abs@.nsf/mf/1270.0.55.005.
- 19.Independent Hospital Pricing Authority (IHPA). National Hospital Cost Data Collection Australian Public Hospitals Report, Round 19 (2014–15) [Internet]. Australia: Independent Hospital Pricing Authority; 2015. [Google Scholar]
- 20.Berends L, Larner A, Lubman DI. Delivering opioid maintenance treatment in rural and remote settings. Aust J Rural Health. 2015;23(4):201–6. [DOI] [PubMed] [Google Scholar]
- 21.Wood P, Opie C, Tucci J, Franklin R, Anderson K. “A lot of people call it liquid handcuffs” – barriers and enablers to opioid replacement therapy in a rural area. J Subst Use. 2019;24(2):150–5. [Google Scholar]
- 22.Peterson GM, Northeast S, Jackson SL, Fitzmaurice KD. Harm minimization strategies: opinions of health professionals in rural and remote Australia. J Clin Pharm Ther. 2007;32(5):497–504. [DOI] [PubMed] [Google Scholar]
- 23.Lee JD, Vocci F, Fiellin DA. Unobserved “home” induction onto buprenorphine. J Addict Med. 2014;8(299–308). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.