Abstract
Background
Many people with type 2 diabetes do not take their treatment as prescribed. Brief messages to support medication use could reach large numbers of people at a very low cost per person, but current interventions using brief messages rarely adequately describe the content of the messages, nor base these messages on explicit behavior change principles. This study reports the views of people with type 2 diabetes concerning the acceptability of 1) a messaging system and 2) proposed messages based on behavior change techniques (BCTs) and beliefs and concerns around taking medication.
Methods
The proposed system and brief messages were discussed in focus groups of people with type 2 diabetes recruited through general practices in England. Transcripts were analyzed thematically.
Participants
Twenty-three participants took part in one of five focus group discussions. All participants were over 18 years, were taking tablet medication for their diabetes, and had access to a mobile phone. Key exclusion criteria were recent hospitalization for hyper- or hypoglycemia or diagnosis with a terminal illness.
Results
Four themes were identified as relating to the acceptability of the messaging system: “opportunities and limitations of technology”, “us and them (who is the system for?)”, “responsibility for adherence”, and “diabetes management beyond medication”. Participants recognized the benefit of using technology. Those with high confidence in their ability to adhere were keen to make a distinction between themselves and those who did not adhere; participants were more comfortable taking responsibility for medication than diet and exercise. Acceptability of the messages hinged on avoiding “preaching to the converted”.
Conclusions
These findings show that brief messaging could be acceptable to the target population for a range of diabetes-related behaviors but highlight the need for such a system to be perceived as personally relevant. Acceptable messages would need to maintain novelty for the target population.
Keywords: diabetes, mHealth, health psychology, behavior change, qualitative, focus groups
Introduction
Diabetes affects 422 million people worldwide, and the majority of these are affected by type 2 diabetes.1 People with type 2 diabetes are commonly prescribed oral antidiabetic medications. If taken as intended, these medications can be effective in lowering HbA1c (a measure of blood glucose concentration). However, people do not always use their medication as intended, often termed nonadherence. Only half the expected reduction in HbA1c can result from taking <80% of the recommended dose.2 Poorly controlled HbA1c can lead to both macro- and microvascular complications, with eye and foot problems being the most common. Reported levels of patient adherence to oral antidiabetic medications vary from 36% to 93%.3
Current interventions to support medication taking both in diabetes and in other long-term conditions have had limited success and can be complex and poorly described.4 A Cochrane review of the area found that there is a “lack of convincing evidence” [p. 1] of effectiveness with many poorly designed studies and an absence of effect in well-designed studies. The authors concluded that alternative approaches should be explored.4 Brief messages may provide a low-cost solution with a wide reach and have been found to be a potentially effective way to deliver health-related interventions, for example in smoking cessation,5 increasing physical activity,6 and increasing adherence to antiretroviral therapy.7
Text messages, a form of brief messaging that can be used to support medication adherence in type 2 diabetes, were identified as being promising in a recent systematic review.8 However, the review found that there were limitations with the interventions that were evaluated. Only 5 of the 15 interventions reviewed were based on a stated theoretical framework, and the authors concluded that there is often inadequate detail in publications related to i) how the text messages were developed and ii) what the content of the text messages is.8 In the UK, recent National Institute for Health and Care Excellence evidence standards recommend that digital health technologies that aim to change behavior should identify the specific behavior change techniques (BCTs) used.9 This would enable us to understand more about what may work to change behavior and refine medication adherence interventions accordingly.
In recent years, there has been growing interest in using BCTs to develop and describe interventions that aim to influence behavior such as taking medication. BCTs are defined as the smallest active components of an intervention;10 examples include “self-monitoring of behavior” or “self-reward”. Identifying the active components of an intervention allows researchers to develop a working model of how any intervention is proposed to change behavior and to describe the intervention in a way that can be replicated by others. In 2013, a taxonomy that defined and described 93 BCTs organized into a hierarchical structure was published.11 However, thus far, where described, text message interventions for diabetes include a relatively limited range of BCTs from the 93 available. In a review of text messages targeting a range of diabetes management behaviors in people with poorly controlled blood glucose (type 1 or type 2 diabetes), 8 BCTs were identified across the 7 included studies,12 and in a review of eHealth interventions for people with poorly controlled type 2 diabetes, 16 distinct BCTs were identified over the 6 studies that used text messages as a mode of delivery.13
To inform the current study, a rapid systematic review of medication adherence literature was conducted.14 The purpose of this review was to identify as many BCTs as possible for which there was some evidence of efficacy to improve adherence. It also aimed to identify the specific beliefs and concerns people with type 2 diabetes have about their medication, as these could be promising targets for brief message interventions. Text messages based on these BCTs, or that aimed to address the identified beliefs and concerns, were then developed by a group of 21 behavior change experts and health care professionals (HCPs) involved in care for people with type 2 diabetes. The BCTs were organized into strategies according to the hierarchical structure of the 2013 taxonomy (eg, the strategy “Goals and Planning” contained the individual BCTs “Problem solving” and “Action Planning”).11 This resulted in 15 strategies, with 31 linked BCTs and beliefs and concerns (see Table 1).
Table 1.
Categories, category descriptions, and component behavior change techniques (BCTs) with example text messages
| Taxonomy category | Strategy title (if different from taxonomy category): Description given to participants | Component BCTs | Example text message |
|---|---|---|---|
| 1. Goals and planning* | Planning and problem-solving: Messages that support and encourage you to plan to take your medication as intended, along with messages that encourage you to solve problems to help you achieve those goals | 1.2 Problem solving 1.4 Action planning |
Plan when, where, and how you are going to take your medication |
| 2. Feedback and monitoring* | Self-monitoring: Messages that suggest monitoring how often you take your medication | 2.3 Self-monitoring of behavior | Make a note of when you take your medication so you know that you have not forgotten |
| 3. Social support* | Messages that encourage and support you to get help from friends, relatives, or services around you. This could be in terms of practical help such as taking you to the pharmacist, or emotional help such as supporting you when you feel fed up | 3.1 Social support (unspecified) 3.2 Social support (practical) 3.3 Social support (emotional) |
Struggling with medication? Can your friends and family help? You’re welcome to bring someone with you to your practice team appointments |
| 4. Shaping knowledge* | Messages that help you to understand how to take your medication and what might affect you taking your medication | 4.1 Instruction on how to perform behavior 4.2 Information about antecedents |
Are you out and about today? Remember that you still need to take your medication as prescribed in order to control your blood sugar |
| 5. Natural consequences* | Messages that either provide or remind you of information about what may happen if you do not take your medication, in terms of your health, feelings, and the effect on society and the people around you | 5.1 Information about health consequences 5.3 Information about social and environmental consequences 5.5 Anticipated regret 5.6 Information about emotional consequences |
Even when you are not experiencing diabetes symptoms, your tablets are still needed to maintain your health |
| 6. Comparison of behavior | Messages that encourage you to think about your medication taking in the context of others around you, for example by comparing it with others or considering what others think of your medication taking | 6.2 Social comparison 6.3 Information about others’ approval |
Compare yourself to other people who are taking diabetes medication. Are you more or less likely than them to take your meds as prescribed? |
| 7. Associations* presented together with 12. Antecedents* | Prompting: Messages that prompt you to take your medication or encourage you to place things around you that may prompt you to take your medication | 7.1 Prompts/cues 12.1 Restructuring the physical environment |
Why not set a reminder on your phone to prompt you to take your medication? |
| 8. Repetition and substitution* | Habits: Messages that help you to make good habits around medication taking | 8.3 Habit formation | Why not take your meds at the same time as something you do every day? For example, when you are brushing your teeth or after a meal |
| 9. Comparison of outcomes | Thinking about the pros and cons of taking medication regularly and comparing what may happen if you do, or do not. Where does the information for these decisions come from? | 9.1 Credible source 9.2 Pros and cons 9.3 Comparative imaginings of future outcomes |
List the benefits of taking your medication as prescribed against the reasons for not wanting to take it |
| 10. Reward and threat | Reward: Messages that congratulate you when you take medication as intended | 10.5 Social reward | |
| 11. Regulation | Managing negative emotions: Messages that help you manage any worries you may have around taking your diabetes medication as intended | 11.2 Reduce negative emotions | Give yourself one less thing to worry about. Take your diabetes medications as prescribed and take control |
| 13. Identity* | Messages that help you to think about how your health and medication fit with your sense of who you are | 13.5 Identity associated with changed behavior | Make successfully managing your medication part of who you are |
| 15. Self-belief | Messages that help to improve your confidence in your ability to take your medication as intended | 15.1 Verbal persuasion about capability 15.2 Mental rehearsal of successful performance 15.4 Self-talk |
If you are struggling with your diabetes meds, then don’t worry you will be able to master it in time. You will get on top of it |
| Dealing with side effects* | Messages that help you address the side effects of taking diabetes medication | NA | Some diabetes medication can give you an upset stomach, if this doesn’t settle speak to your Dr or nurse |
| Concerns with health care system and medications* | Messages that address concerns people have around the health care system and taking medications generally | 4.1 Instruction on how to perform a behavior | Questions about your diabetes medications? Make the most of your next appointment by writing down the questions you want to ask |
Note: *Indicates a category that was introduced spontaneously by participants, eg, before the moderator had introduced it and shown example messages.
The above process ensured the messages developed were based on a wide range of explicitly identified BCTs. However, to meet relevant evidence standards for digital health technologies, acceptability to the intended users of the intervention is essential.9 Although often measured and reported,15,16 acceptability has been relatively poorly defined as a concept. To overcome this, a systematic review of existing literature related to acceptability of health care interventions defined acceptability as a
multi-faceted construct that reflects the extent to which people delivering or receiving a healthcare intervention consider it to be appropriate, based on anticipated or experienced cognitive and emotional responses to the intervention [p. 1].17
Previous studies have explored the experienced acceptability of text message interventions sent to people with type 2 diabetes. However, often the messaging intervention incorporates only a small number of BCTs.18,19 If novel approaches are needed to address medication adherence in this population,4 then including a wider range of BCTs might be preferable. To our knowledge, the present study is the first to explore the perceived acceptability of a message system with messages based on a wide range of BCTs.
This study aims to establish the acceptability of 1) a brief message-based system for medication adherence and 2) the proposed content of the messages sent by this system to people with type 2 diabetes.
Methods
Participants
Participants were recruited through general practices (GPs) in the Greater Manchester and Thames Valley areas of England. Participants were eligible if they i) were aged 18 or above, ii) were diagnosed with type 2 diabetes, iii) were taking oral medication to control their diabetes, and iv) either used or had access to a mobile phone and were able to send and receive text messages (including shared access to a phone). Participants were excluded if they i) had been hospitalized for hyper- or hypoglycemia within the last 3 months or ii) were pregnant or within 3 months postpartum or iii) had been diagnosed with a terminal medical condition.
Study design
Focus groups were selected to enable interaction between participants with shared experiences and to explore similarities and differences of opinions. Through listening to the interaction between participants, researchers can gain a deeper understanding of the topics discussed than with one-to-one interviews.20 As recommended, introductory questions were used to provide a context for the discussion before more detailed discussion.21 Further information about the content of the group is provided in the procedure section.
Procedure
The study received ethical approval from the NHS North West – Greater Manchester West Research Ethics Committee (17/NW/02/24). In collaboration with Clinical Research Networks, practices were contacted and invited to take part. Five practices agreed. Invitation letters with the information sheet, reply slips, and questionnaires were sent to eligible patients by the GP in batches of 50 with freepost return envelopes. Interested individuals returned the reply slip and the questionnaire in separate envelopes and were contacted by the research team to arrange attendance at a focus group. Groups were held at either a university or a community location. Written consent was collected before the group began. Participants were shown a short presentation outlining the background of the project and some information about what the proposed system might look like.
Introductory questions were asked about initial impressions of the system. In four of the five groups, strategies (clusters of BCTs) were then introduced and discussed in turn. For each strategy, an overall summary was shown with example brief messages. Between four and seven strategies were discussed per group. Further details about the strategies, BCTs, and example messages are provided in Table 1. Finally, opinions toward the system specifications were given, for example thoughts related to interactivity, personalizing, and tailoring. There was no reimbursement for participants, but refreshments were provided and travel expenses paid.
Analysis
The recordings of the focus groups were transcribed verbatim and analyzed using thematic analysis. The first four transcripts were coded by hand with a combination of data-driven and a priori codes. The data-driven codes were generated from the data alone without reference to other sources. The a priori codes were based on the BCT taxonomy where each BCT is given a number and a title, eg, “8.3 Habit Formation”.11 Hence, this a priori code was used either when example messages related to this BCT were discussed or when the participants spontaneously mentioned forming habits at other points in the group. Codes were summarized into initial categories and NVivo 1122 was used to code the transcripts into these categories. The content of each category was then explored for overarching themes that provided understanding across categories. The identified themes contained elements of the transcript that had been coded with a priori and data-driven codes. The themes were discussed between two authors, and both of these authors applied the draft themes independently to a fifth transcript before final themes were agreed on.
Results
Sample
Participants (n=23) were recruited from 5 GPs (see Table 2 for demographic information); each participant took part in one of five focus groups. Cross-referencing individual postcodes with the Index of Multiple Deprivation, those recruited spanned from the top 10% to the bottom 20% most deprived areas in the UK.23
Table 2.
Participant demographics and time since diagnosis with type 2 diabetes
| N (%)/Mean (SD)a | |
|---|---|
| Age | 68.11 (7.25) |
| Female | 3 (16.7%) |
| Years since diabetes diagnosis | 10.78 (5.94) |
| Ethnicity White British | 15 (83.3%) |
Note: an=18. Attendees at 1 of the 5 groups did not complete the questionnaire.
Overview of results
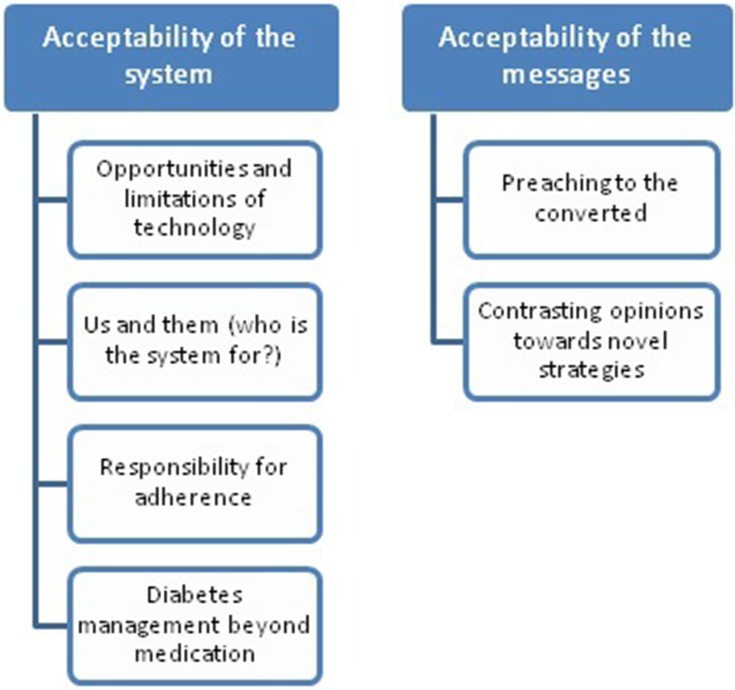
Themes were identified related to 1) the messaging system and 2) the proposed messages based on BCTs and beliefs and concerns around medication taking. Four themes were identified related to the acceptability of the system overall: “opportunities and limitations of technology”, “us and them (who is the system for?)”, “responsibility for adherence”, and “diabetes management beyond medication”. Two themes were also identified that related to the acceptability of the proposed messages “preaching to the converted” and “contrasting opinions toward novel strategies” (see Figure 1). Ten of the 15 behavioral strategies were brought up spontaneously by participants during discussions (eg, outside of the strategy being presented with example messages) and the beliefs and concerns related to medication were familiar to participants.
Figure 1.
Themes identified related to the proposed system and the proposed messages.
Acceptability of a text message system to support medication adherence
Opportunities and limitations of technology
The opportunities presented by technology were acknowledged in terms of the potential for greater connection between systems such as those used by the GP and the pharmacy. However, limitations were also acknowledged in terms of the potential cost of such a system, in terms of both monetary cost and the time taken by HCPs.
“Where the cost is coming from, who’s going to be behind the cost of it all, because texts do cost money.” Male, aged 61
There was discussion around whether delivery by text message would be appropriate in principle. For example, there were concerns that some people may be excluded if they did not use mobile phones, and that some of the content, such as information about side effects and forming habits to take diabetes tablets, would be more suitable for delivery by an HCP than by a mobile phone.
“I think [messages based on habit formation] are precisely the sort of messages the diabetic nurse should give you when you first have things prescribed. “ Male aged 73
The opportunities and limitations were discussed in the light of participants’ experiences of current technologies related to self-management. For example, while the idea of using technology such as automatic pill dispensers or automated reminders for appointments or medication refills was supported, there was frustration when technology did not work as intended.
“The pharmacy sends me a text message to tell me that the prescription is ready for picking up, except they only do it about three-quarters of the time … which is really annoying.” Male, aged 69
Us and them (who is the system for?)
Although many participants reported taking their medication as prescribed, all participants described instances of forgetting to take their medication or making changes to their regimen to fit around their lifestyle. Despite this, participants who were confident in their own skills to manage their medication seemed keen to draw a distinction between themselves and those who did not take their medication (and thus would need a system such as this). People who did not take their medication were perceived to have “chaotic lifestyles” or were unable to “cope with life”. Differences between “us and them” were highlighted in terms of perceived socioeconomic status, cognitive functioning, and health as well as attitude toward the self and others. The portrayal of people who did not take their medication was more sympathetic if it was perceived that health issues prevented them from doing it:
“It’s about self-worth, isn’t it? You know, really, do you want to keep yourself alive … or are you going to let go of your family and friends, and die?” Female, aged 72
“It could be useful for maybe older people who [‘re] not quite as sort of coherent on these sorts of things, taking medications and all that.” Male, aged 65
The exception to this differentiation between themselves and people who need this type of system was a single participant who described themselves as having less confidence in their ability to self-manage and also experiencing some memory problems:
“I’m trying to be independent, you know. I hope [the proposed system] might be useful for me” Female, aged 68
Responsibility for adherence
Opinion of the system as a whole was influenced by the perception of whose responsibility taking medication as intended was thought to be, with some individuals stating strongly that to assist by sending brief messages was tantamount to a “nanny state”.
“As far as I’m concerned … text messages would be an irritation and moving onto the wider picture how much further do we want to get down to our nanny state?” Male, aged 64
In contrast, some participants viewed it as welcome support, especially for those who had recently been prescribed the medication.
“I don’t think we forget to take the medicine … But the new people who are initially diagnosed [with] diabetes, I think these type of things [eg messages are] more beneficial to them.” Male, aged 56
Largely, participants thought that the responsibility to take medication lay with the individual unless poor health prevented it.
“It’s like the cigarette packets, if you want lung cancer, try smoking; if you want to lose your limbs, don’t take your medicine. It’s down to you.” Male, aged 71
“There are a lot of people in this stage of life who cannot remember, they’re not aware of their whereabouts … those kind of people need support like that.” Male, aged 75
However, where opportunities arose for participants to share the responsibility of their own medication self-management with the health care services (eg, through pharmacy alert systems) or with friends and family, participants made use of this shared responsibility:
“My pharmacist always phones me to tell me my medication’s ready so I don’t have to worry.” Male, aged 75
“I’ve got the family, they remind me.” Female, aged 68
This acknowledges the fact that most participants proactively managed their condition, making use of both public and private services, and that this would be difficult to maintain without support and sharing responsibility with others.
Diabetes management beyond medication
The majority of the participants had confidence in their own medication management, and therefore seemed comfortable that the responsibility lay mostly with them (as long as they were able). However, this differed when the focus was changed to diabetes management that did not involve medication. There was less certainty around aspects such as diet and exercise, and there was less comfort with the idea that individuals were wholly responsible, and more of a sense that people with diabetes would benefit from more support. In some cases, there seemed to be genuine fear related to dietary management and an acknowledgment that even information from seemingly credible sources could be contradictory.
“I know I don’t forget to take my medication, very rare if I do. It’s what you do prior to that, what you eat and balance everything out. That can be a bit of a struggle, with the eating side.” Male, aged 72
I’m so scared that I can’t eat, I just don’t eat any carbohydrate. I stopped eating that at all because I … hate the needle so much … and I said, okay if I eat then it will go worse and I’ll end up with the needle. [referring to becoming insulin dependent] Female, aged 68
“Over the years, asking my GPs about dietary practice, they seemed to change their minds and be very confused about what one should eat and what one shouldn’t eat.” Male, aged 83
Acceptability of the proposed content of the messages to change behavior
Ten of the 15 behavior change strategies and beliefs and concerns were brought up spontaneously by groups either prior to being presented or at groups where a particular strategy was not presented. The five strategies that were only discussed when introduced by the moderator were: reward, managing negative emotions, self-belief, comparison of behavior, and comparison of outcomes.
Preaching to the converted
For the 10 strategies that were mentioned spontaneously, participants often recognized the inherent value of the strategy, but in many cases, they were already using it, so when it was presented participants did not feel it was relevant to them. The system was perceived to be most useful when the messages were not “preaching to the converted”. This applied to strategies that were already in use, as well as information that was already known. For example, the below quotation after the planning and problem-solving strategy was introduced using messages such as “Plan when, where and how you are going to take your medication”:
“I knew how many days I was going away, and I got the tablets appropriately ready to go and took them with me, and every time I’ve gone away on holiday, I’ve done the same.” Male, aged 77
The exception to this seemed to be prompting, eg, “Why not set a reminder on your phone to prompt you to take your medication?” Although many participants already used prompting, which was the most positively received strategy, participants suggested many different self-management targets that may benefit from prompting, eg, taking medication, taking exercise, and reminders to eat regularly; in addition, participants felt that prompts continue to be useful for them, and knowing more about prompts would be useful for others.
“Oh, I’d be grateful. I’d be happy to get [prompting messages], just to remind me.” Male, aged 57
In some cases, there was surprise that others did not implement “common sense” strategies such as problem-solving. This again fed into the differentiation between the participants and who they perceived would need a system like this.
Contrasting opinions toward novel strategies
Whereas those strategies that were spontaneously discussed were generally recognized as valuable (at least to those who had not used them previously), those strategies that were novel to the group either generated greater contrast in opinions or more negative opinions. For messages related to reward, self-belief, and managing negative emotions, the groups were split into people who thought the messages might be useful and those who thought the messages were simplistic or patronizing. For example, the below two quotations related to messages that aimed to increase self-belief, eg, “If you are struggling with your diabetes meds, then don’t worry you will be able to master it in time. You will get on top of it”.
“A bit, you know, what do I need this for, you know what I mean? I’m doing it anyway. It’s not something that I’d appreciate, let’s put it like that.” Male, aged 61
“You will get on top of it, yes one day. They will master it in time, yes I hope so.” Female, aged 68
Messages based on the strategy “comparison of behavior” were reviewed negatively by participants. There was discomfort with the idea of comparing themselves, and the way they were managing their diabetes with others. For example, the quotation below in response to the messages “Your friends and family will be happy that you are taking care of yourself by taking your meds as prescribed” and “Compare yourself to other people who are taking diabetes medication. Are you more or less likely than them to take your meds as prescribed?”:
“The second [message] implies it’s a competitive process, which is ridiculous, and the first one is patronising in the extreme. I think it’s a completely erroneous way to look at it.” Male, aged 61
In contrast, the response given to messages such as “List the benefits of taking your medication as prescribed against the reasons for not wanting to take it” related to comparison of outcomes was more positive. Participants felt the messages could have gone further to highlight the cons of not taking medication through visual images of the consequences of uncontrolled diabetes similar to those used on tobacco packaging in the UK.
“I think quite a lot of people are resistant to taking medication, initially, you know, and they’ve got to be given the pros and the cons of doing it, you know?” Female, aged 72
“ … some pictures, I think that would be helpful as well … for example, if you don’t take the medicine, you might be blind.” Male, aged 56
Beliefs and concerns
Messages based on two beliefs and concerns were shown to participants: i) dealing with side effects and (ii) concerns about health care services and medications (for a description of these, please see Table 1). Both beliefs and concerns were introduced spontaneously by participants before the moderator had introduced them. Dealing with side effects was a commonly understood concern, and many people in the groups had experienced side effects from the medication. The messages addressing it were on the whole well received; however, there was concern about advice to seek help from HCPs as they are already overburdened.
You start thinking, oh is it this, oh is it that? Then you’re on the doctor’s doorstep. It’s hard enough to see a doctor anyway, you know what I mean, but if you start being a nuisance, you might just get totally knocked off the list. Male, aged 61
Concerns about health services and medication (identified from the rapid review14) included messages related to traditional, herbal, or complementary therapies. Participants were not supportive of these approaches in general, or if they were it was as an addition to medicine prescribed by an HCP, rather than an alternative. However, in responding to the example messages participants expressed uncertainty about why they were taking tablets, and if they were truly needed. There was possibly a distinction between knowing that the tablets were good for them and that they should take them, and feeling that they were truly necessary. There was a lack of understanding regarding the necessity of maintaining a preventative medication regime. Some participants spoke of not experiencing any differences whether they took or did not take their medication, and being unconvinced by the evidence that supports metformin (the most commonly prescribed drug for type 2 diabetes).
I’m unsure how effective the medication that we’re all on is, basically … I’m on metformin for medication - and what I picked up was, this is the best we’ve got at the minute. So it isn’t, I don’t think it’s 100 per cent effective. Female, aged 72
Discussion
The usefulness of a digital messaging system to support and encourage diabetes medication self-management was recognized, along with the opportunities provided by using a system such as this. However, through the “us and them” theme, participants largely highlighted the system’s potential usefulness for others rather than themselves. Despite many participants describing occasions when they had not taken their medication, or had altered their dosage, there was a strong distinction drawn by the participants between themselves and those they perceive would need the system. This perceived distinction could reduce the likelihood that these participants would find the idea of a system like this acceptable and go on to adopt such a system. The responsibility for taking diabetes medication as prescribed was seen as the individual’s responsibility, unless prevented by poor health; however, when possible, participants did make use of external support from family, friends or HCPs to support their medication adherence.
Despite this population’s confidence in their own medication management, concerns were raised about why they were taking medication, and if the medication was truly needed. These findings are consistent with previous qualitative studies that have explored reasons for nonadherence. In a recent meta-synthesis, participants viewed diabetes medication as a necessary evil, implying that there was belief in the necessity of the medication; however, participants were also found to engage in active experimentation with the medication regimen to achieve a good fit with their lives.24 This could indicate that for some participants, BCTs that highlight the necessity of taking medication (eg, those that focus on the consequences of poor adherence, or those looking at comparing either taking the medication or not) may not be that acceptable as the necessity is already acknowledged and greater understanding of how experimentation with the medication may have an effect long term (even if short term it does not have an effect on how the person feels) may be more acceptable. Questions were raised by participants about the effectiveness of metformin as a treatment; this is something that could be explored with HCPs in future work.
Previous short message-based interventions have included a limited range of BCTs (as shown by11,12) or have based text messages on existing diabetes education programs.25 It is however recognized that new approaches to medication adherence are needed.4 In using a wide range of previously unexplored BCTs, there were some that prompted discord in the groups due to contrasting opinions, with some participants finding them useful and others patronizing. Comparing this with the BCTs that were spontaneously brought up, it can be concluded that there was greater discord in opinion than if it had been proposed that the intervention would have used the more commonly used BCTs such as “instruction on how to perform a behavior” and “prompts and cues” which were more uniformly accepted. Potentially, the less commonly used BCTs such as “verbal persuasion about capability” may only be effective for a subgroup of people who perceive them to be relevant to themselves. Acceptability, as defined by Sekhon et al, is a combination of perceived relevance, cognitive, and emotional reaction to an intervention. For these participants, perceived relevance seemed to be key, and this relevance guided how participants reacted to the system.17 This suggests that if too many messages that are not perceived as relevant are received, this may be off-putting to people with diabetes and result in a negative reaction toward the system.
Previous research has identified that, in text message interventions, novelty is valued by people with type 2 diabetes.15 Participants in the present research supported this finding as they reported being less interested in strategies and information they had heard before meaning intervention developers should be wary of preaching to the converted. Future technology in this area will need to ensure it is both introduced and tailored in a way that maximizes perceived relevance to the individual and maintains novelty. One approach to this could be for interventions to include BCTs that promote motivation, and self-regulation BCTs that help translate motivation into action at different points in time. It is likely that for those already motivated to take medication as prescribed, additional messages aimed at increasing motivation (eg, “information about emotional consequences” of not taking medication as prescribed) may not promote a change in behavior. By contrast, BCTs that aim to help people self-regulate their behavior in line with their motivation (eg, “habit formation” or “prompts and cues”) may be more effective for motivated participants. In both cases, continued novelty may be important. Brief message systems are ideally suited to providing continued novelty as once the system is set up, it is relatively easy and cheap to change the messages being sent, or tailor the messages being sent in comparison to printed materials. There are numerous apps available to support individuals with their diabetes; however, in many cases, these do not adhere to evidence-based guidelines.26 In focussing on the content of the brief messages, the aim of this study is to explore how they would be perceived received as standalone messages; however, if the content is found to be effective there would be scope to incorporate the messages into a wider evidence-based app, or use internet-based messaging services. In 2017, 42% of those over 65 were found to own a smartphone as opposed to 80% who own any form of mobile phone;27 furthermore, only 36% of those over 65 use the internet on a mobile device as opposed to 70% or more in younger age groups.28 Maintaining flexibility in delivery may allow these messages to reach a wider audience, and not exclude those who do not have, or do not use smartphones.
There seemed to be a desire for further support for aspects of diabetes self-management beyond medication, such as diet and exercise. In a review of brief message interventions targeting diet and physical activity in people with type 2 diabetes, it was found that there was some evidence of a positive effect, but the majority of the studies did not have a theoretical base.29 These findings mirror those found for interventions targeting medication management. This suggests that using recognized BCTs and theories to develop messages would help researchers to understand outcomes, and potentially identify if certain BCTs resulted in more effective messages, across a range of diabetes-related self-management behaviors.
Limitations
The participants were a relatively homogenous group in terms of ethnicity, age, gender, length of time with diabetes, and perceived confidence in their ability to self-manage. During recruitment, we succeeded in recruiting through practices with a range of deprivation scores. When the gender imbalance of respondents became clear, we contacted the recruiting practices to see whether a greater number of men had been invited, but the invites were sent out to approximately equal numbers of each gender. The homogeneity of the sample must be seen as a limitation of these findings, especially as the few exceptions (eg, those with less confidence in their ability to take their medication) who attended provided contrasting opinions on a number of occasions. Although we cannot assume anything about people we did not speak to, this suggests that great effort should be made to recruit a heterogeneous sample in future studies to explore potential similarities and differences across different demographic groups of patients.
For example, in a systematic review of tablet medication adherence in people with type 2 diabetes from Europe, the United States, Australia, and Canada, social and cultural health beliefs were identified as influential either as a barrier or as a facilitator of adherence.30 Furthermore, in a separate systematic review, an association between ethnicity and medication adherence in people with type 2 diabetes who take tablet medication was reported.31 However, there were only three relevant studies identified and the authors of the review concluded that further research is needed to explore why this association may exist.31
South Asian populations are at particular risk from developing type 2 diabetes.32 It is therefore particularly important to understand how ethnicity and social and cultural beliefs may influence adherence in this population. Although the relatively ethnically homogenous sample of this study cannot extend knowledge in this area, the study presented here is part of a wider program of research that includes conducting focus groups in a variety of languages with South Asian populations.33 Future research could consider the findings reported here in conjunction with other studies from the program of research to explore differences and similarities and ensure any intervention developed will be acceptable to groups of different ethnicities.
Implications
For a brief message system to be acceptable to people with type 2 diabetes, it would need to be introduced in a way that promotes personal relevance. Findings related to the “us and them” theme indicate that HCPs should be aware of the potential stigma associated with identifying as someone who does not take their medication, and that this may make people less likely to find a system to support adherence acceptable. The messages sent through the system should address a variety of diabetes management behaviors beyond medication management and to avoid preaching to the converted should maintain novelty to the target population. Brief messages are an ideal way to do this, as they are relatively cheap and easy to tailor, but have a large potential reach.
Future research
Further research should explore how text message systems such as this one are introduced to participants and adopted or abandoned by them. This research could also help to identify if there are certain populations who would be more likely to benefit than others. While it is important to optimize the intervention to be as acceptable as possible to participants, researchers should aim to maintain a balance between ensuring perceived relevance, but also trying novel intervention components that may have an effect despite not initially seeming relevant to the participant. These findings have shown that a wide range of BCTs are perceived to be acceptable; however, participants may experience the messages differently when they receive them “in the wild” as opposed to reading them as part of a focus group. Therefore to optimize the text message library further, research is needed to explore the experienced acceptability of the messages. Targeting a range of self-management behaviors relevant to diabetes through brief messages should be explored further. It is possible this approach may improve perceived relevance amongst those people with type 2 diabetes who do not identify as needing help taking their medication.
Conclusion
A short message system may be an acceptable way to support and encourage people with type 2 diabetes to take their medication as prescribed. Although participants reported high confidence in their own ability to take medication as prescribed, many still missed doses, or changed how they took medication to better fit with their lifestyle. Greater support may be needed around diet and exercise self-management goals for diabetes. The content of the messages, and how the system is introduced to potential users, would need to be tailored to ensure perceived relevance and novelty of the messages received.
Acknowledgment
This publication presents independent research funded by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research programme (RP-PG-1214-20003) and supported by the National Institute for Health Research (NIHR) Oxford Biomedical Research Centre (BRC). DPF is supported by the NIHR Manchester Biomedical Research Centre (IS-BRC-1215-20007). AJF is an NIHR Senior Investigator. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care. The SuMMiT-D research team acknowledges the support of the National Institute for Health Research Clinical Research Network (NIHR CRN). The authors would like to thank both the Thames Valley and South Midlands and the Greater Manchester Clinical Research Networks and the general practices for help with recruitment and Dr Veronika Williams for input into the design of the study.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.World Health Organisation. Global report on diabetes. 2016. ISBN 978 92 4 156525 7 Available from: https://www.who.int/diabetes/publications/grd-2016/en/. Accessed May 1, 2019. [Google Scholar]
- 2.Farmer AJ, Rodgers LR, Lonergan M, et al. Adherence to oral glucose-lowering therapies and associations with 1-year HbA1c: a retrospective cohort analysis in a large primary care database. Diabetes Care. 2016;39(2):258–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cramer JA. A systematic review of adherence with medications for diabetes. Diabetes Care. 2004;27(5):1218–1224. [DOI] [PubMed] [Google Scholar]
- 4.Nieuwlaat R, Wilczynski N, Navarro T, et al. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2014;11:CD000011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Free C, Phillips G, Galli L, et al. The effectiveness of mobile-health technology-based health behavior change or disease management interventions for health care consumers: a systematic review. PLoS Med. 2013;10(1):e1001362. doi: 10.1371/journal.pmed.1001362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Head KJ, Noar SM, Iannarino NT, et al. Efficacy of text messaging-based interventions for health promotion: a meta-analysis. Soc Sci Med. 2013;97:41–48. [DOI] [PubMed] [Google Scholar]
- 7.Horvarth T, Azman H, Kennedy GE, et al. Mobile phone text messaging for promoting adherence to antiretroviral therapy in patients with HIV infection. Cochrane Database Syst Rev. 2012;14(3):CD009756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Farmer AJ, McSharry J, Rowbotham S, et al. Effects of interventions promoting monitoring of medication use ad brief messaging on medication adherence for people with Type 2 diabetes: a systematic review of randomized trials. Diabet Med. 2015;33(5):565–579. [DOI] [PubMed] [Google Scholar]
- 9.National Institute for Health and Care Excellence (NICE). Evidence standards framework for digital health technologies; 2019. Available from: https://www.nice.org.uk/Media/Default/About/what-we-do/our-programmes/evidence-standards-framework/digital-evidence-standards-framework.pdf. Accessed May 1, 2019.
- 10.Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol. 2008;27(3):379–387. [DOI] [PubMed] [Google Scholar]
- 11.Michie S, Richardson M, Johnston M, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95. [DOI] [PubMed] [Google Scholar]
- 12.Dobson R, Whittaker R, Pfaeffli Dale L, et al. The effectiveness of text message-based self-management interventions for poorly-controlled diabetes: a systematic review. Digital Health. 2017;3:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kebede M, Liedtke TP, Möllers T, et al. Characterizing active ingredients of ehealth interventions targeting persons with poorly controlled Type 2 diabetes mellitus using the behavior change techniques taxonomy: scoping review. J Med Internet Res. 2017;19(10):e348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Long H, Bartlett YK, Farmer A, et al. Developing brief message content for interventions delivered via mobile devices to improve medication adherence in people with type 2 diabetes mellitus: a rapid systematic review. J Med Internet Res. 2019;21(1):e10421. doi: 10.2196/10421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nelson LA, Mulvaney SA, Johnson KB, et al. mHealth intervention elements and user characteristics determine utility: a mixed-methods analysis. Diabetes Technol Ther. 2017;19(1):9–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Burner ER, Menchine MD, Kubicek K, et al. Perceptions of successful cues to action and opportunities to augment behavioral triggers in diabetes self-management: qualitative analysis of a mobile intervention for low-income Latinos with diabetes. J Med Internet Res. 2014;16(1):e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sekhon M, Cartwright M, Francis JJ, et al. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Serv Res. 2017;17:88. doi: 10.1186/s12913-017-2031-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dobson R, Carter K, Cutfield R, et al. Diabetes text-message self-management support program (SMS4BG): a pilot study. JMIR Mhealth Uhealth. 2015;3(1):e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dobson R, Whittaker R, Jiang Y, et al. Effectiveness of text message based, diabetes self-management support programme (SMS4BG): two arm, parallel randomised controlled trial. BMJ. 2018;17:361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morgan DL, Kruegar RA. When to use focus groups and why In: Morgan DL, editor. Successful Focus Groups: Advancing the State of the Art. Thousand Oaks: Sage Publications; 1993:3–19. [Google Scholar]
- 21.Krueger RA. Developing Questions for Focus Groups (Vol. 3). Thousand Oaks: SAGE Publications Inc; 1997. [Google Scholar]
- 22.NVivo qualitative data analysis Software. QSR International Pty Ltd. Version 11; 2017. [Google Scholar]
- 23.Ministry of housing Communities and Local Government. English indices of deprivation 2015. Available from: http://imd-by-postcode.opendatacommunities.org/. Accessed May, 2019.
- 24.McSharry J, McGowan L, Farmer AJ, et al. Perceptions and experiences of taking oral medications for the treatment of type 2 diabetes mellitus: a systematic review and meta-synthesis of qualitative studies. Diabet Med. 2016;33(10):1330–1338. [DOI] [PubMed] [Google Scholar]
- 25.Arora S, Peters AL, Burner E, et al. Trial to examine text message-based mHealth in emergency department patients with diabetes (TExT-MED): a randomized controlled trial. Ann Emerg Med. 2014;63(6):745–754. doi: 10.1016/j.annemergmed.2013.10.012 [DOI] [PubMed] [Google Scholar]
- 26.Breland JY, Vivian MS, Yeh M, Yu MSJ. Adherence to evidence-based guidelines among diabetes self-management apps. Transl Behav Med. 2013;3(3):277–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Anderson M, Perrin A. Technology use among seniors; 2017. Available from: https://www.pewinternet.org/2017/05/17/technology-use-among-seniors/. Accessed May 1, 2019.
- 28.Office for National Statistics (ONS). Internet access – households and individuals; 2018. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/householdcharacteristics/homeinternetandsocialmediausage/datasets/internetaccesshouseholdsandindividualsreferencetables. Accessed May 1, 2019.
- 29.Arambepola C, Ricci-Cabello I, Manikavasagam P, et al. The impact of automated brief messages promoting lifestyle changes delivered via mobile devices to people with type 2 diabetes: a systematic literature review and meta-analysis of controlled trials. J Med Internet Res. 2016;18(4):e86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brundisini F, Vanstone M, Hulan D, DeJean D, Giacomini M. Type 2 diabetes patients’ and providers’ differing perspectives on medication nonadherence: a qualitative meta-synthesis. BMC Health Serv Res. 2015;15:516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Peeters B, VanTongelen IV, Boussery K, Mehuys E, Remon JP, Willems S. Factors associated with medication adherence to oral hypoglycaemic agents in different ethnic groups suffering from Type 2 diabetes: systematic literature review and suggestions for further research. Diabet Med. 2011;28:262–275. doi: 10.1111/j.1464-5491.2011.03281.x [DOI] [PubMed] [Google Scholar]
- 32.Gujral UP, Pradeepa R, Beth Weber M, Venkat Narayan KM, Mohan V. Type 2 diabetes in South Asians: similarities and differences with white Caucasian and other populations. Ann NY Acad Sci. 2013;1281(1):51–63. doi: 10.1111/j.1749-6632.2012.06838.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Prinja S. British South Asian narratives of diabetes and views on future research. 2018. Available from: https://www.phc.ox.ac.uk/news/blog/british-south-asian-narratives-of-diabetes-and-views-on-future-researchAccessed May 1, 2019. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- National Institute for Health and Care Excellence (NICE). Evidence standards framework for digital health technologies; 2019. Available from: https://www.nice.org.uk/Media/Default/About/what-we-do/our-programmes/evidence-standards-framework/digital-evidence-standards-framework.pdf. Accessed May 1, 2019.