Abstract
A 10-year-old boy was referred for a circumscribed choroidal hemangioma with underlying exudative detachment of the left eye. To avoid general anesthetics required for laser-based therapy in a child, we began a trial of oral propranolol. The patient’s exudative detachment resolved, with resulting improvement in visual acuity, and remained quiescent for 3 years.
Case Report
A 10-year-old boy with a history of a circumscribed choroidal hemangioma involving the left eye presented at Washington University School of Medicine for progressive vision loss over several weeks. He had received regular eye examinations since 6 years of age for anisometropic amblyopia of the left eye and cup:disk ratio asymmetry. His baseline visual acuity was 20/20 in the right eye and 20/25 in the left eye. Over the prior 5 years his examination showed a stable cup:disk ratio and corneal diameter in both eyes, suggesting no glaucomatous progression.
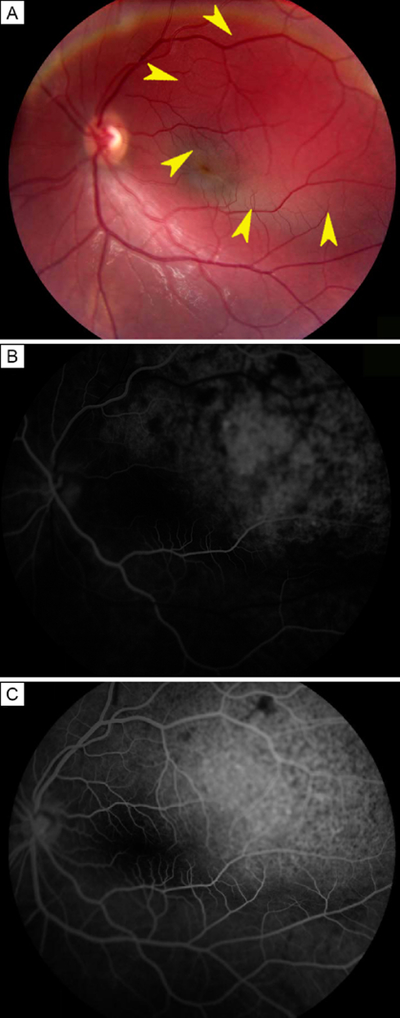
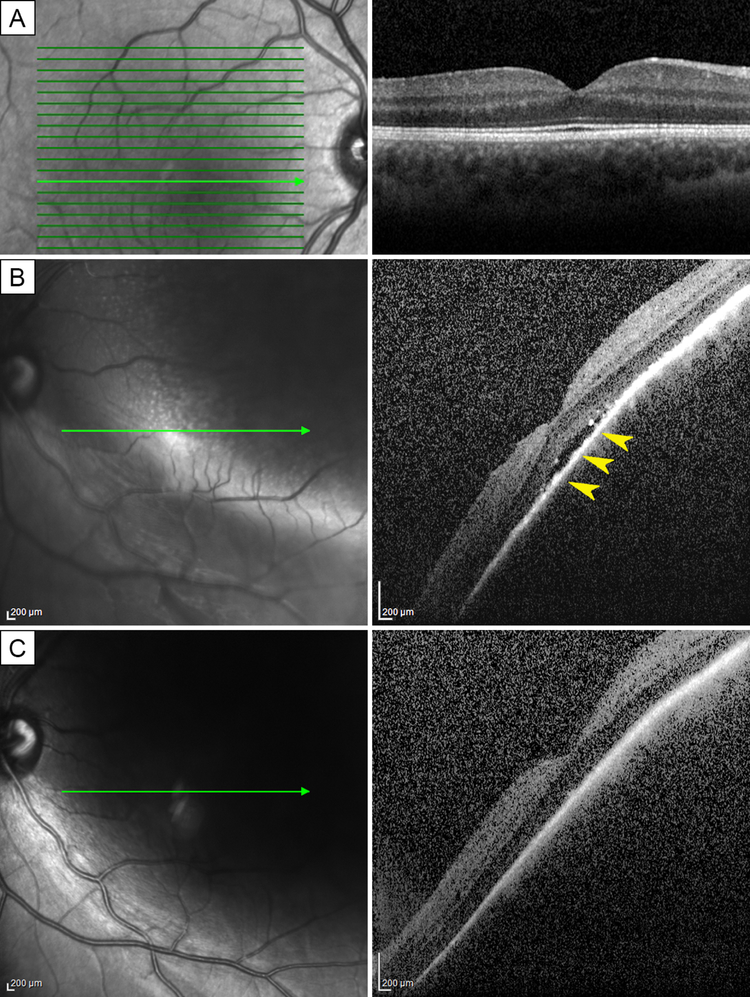
On examination, his visual acuity was 20/50 in the left eye and had remained 20/20 in the right eye. Tonometry was normal in both eyes. Pupillary light responses, ocular motility, confrontational visual fields, and slit-lamp examination were unremarkable. Retinal examination of the left eye revealed a circumscribed choroidal hemangioma with superior exudative detachment involving the macula (Figure 1A). Retinal examination of the right eye was normal. The lesion in the left eye demonstrated diffuse leakage of fluorescein (Figure 1B). Whereas retinal architecture was normal in the right eye (Figure 2A), a subfoveal serous neurosensory detachment was present in the left eye (Figure 2B).
FIG 1.
Choroidal hemangioma in a 10-year-old boy. A, Retinal photograph of the left eye, showing a circumscribed choroidal hemangioma, with exudative retinal detachment superotemporal to and involving the macula (arrowheads). B, Early-phase fluorescein angiogram of the left eye, with coarse hyperfluorescence of the lesion C, Late-phase fluorescein angiogram of the left eye, demonstrating leakage consistent with an exudative detachment.
FIG 2.
Response to therapy with propranolol. A, Optical coherence tomography (OCT) of the right eye showing normal retinal architecture. B, OCT of the left eye prior to therapy showing a pocket of subfoveal fluid (arrowheads). C, OCT 3 months after starting oral propranolol, with resolution of subretinal fluid.
We considered several options for treatment, including treatment with photodynamic therapy (PDT) and thermal laser photocoagulation, which are both standard therapies in adults. However, we elected to begin a trial of oral propranolol to avoid anesthetics required for laser-based therapy in children. Oral propranolol was administered at a dose of 2mg/kg/day for one month. The child experienced no serious adverse side effects, but his parents noted a decrease in his exercise tolerance and a mild increase in his fatigability. His propranolol dose was subsequently tapered down and eventually discontinued over another 4 weeks. Three months after the initiation of therapy, his exudative retinal detachment resolved (Figure 2C) and his visual acuity improved to 20/25. The patient’s choroidal lesions remained quiescent for at least 3 years thereafter without recurrence of subretinal fluid.
Discussion
Circumscribed choroidal hemangiomas are rare, isolated, benign vascular hamartomas. Histologically they are comprised of capillary and cavernous vascular networks.1 Clinically they appear as orange-red, solitary lesions, sometimes associated with serous retinal detachments.2 Although these lesions may be asymptomatic and found incidentally on routine clinical examination, the majority of patients in a large series reported decreased vision.3
Established treatment modalities for symptomatic lesions include thermal laser photocoagulation and PDT, although antivascular endothelial growth factors have also been employed successfully.2–5 However, in pediatric patients, these methods require use of general anesthetic.
Oral propranolol is a first-line therapy to treat infantile capillary hemangiomas. As a nonselective beta-2 blocker, it functions to reduce nitric oxide release and proangiogenic molecules, including hypoxia-inducible factor 1 and vascular endothelial growth factor, ultimately resulting in apoptosis of capillary endothelial cells.1,6 This drug has been used to treat exudative retinal detachments related to circumscribed choroidal hemangiomas in adults with variable success. Sanz-Marco and colleagues1 reported resolution of subretinal fluid and improvement of visual acuity to 20/20 from 20/100 using the same dose of propranolol. However, a study of 5 adults treated with propranolol for long-standing exudative detachments from choroidal hemangiomas found improvement in, but not resolution of, subretinal fluid volume on a maximum of 30 mg propranolol three times daily.5 However, caveats of this study are the inclusion of chronic cases and the use of a low and potentially subtherapeutic dosage of propranolol.
Our patient presented at 10 years of age with a visually significant circumscribed choroidal hemangioma, with secondary exudative retinal detachment. A trial of oral propranolol was appropriate, because alternative treatments would have required use of general anesthetic. Using a weight-based dosage, our patient’s subretinal fluid resolved, and his visual acuity improved to near baseline. Furthermore, his choroidal hemangioma remained stable for at least 3 years.
In the pediatric population, oral propranolol offers a relatively safe potential therapy for exudative retinal detachments related to circumscribed choroidal hemangiomas. As in our patient, this therapy may improve subretinal fluid accumulation and visual acuity in pediatric patients. A trial of oral propranolol may be considered prior to undertaking alternative therapies, such as laser therapy or intravitreal injections, which require general anesthesia.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Sanz-Marco E, Gallego R, Diaz-Llopis M. Oral propranolol for circumscribed choroidal hemangioma. Case Rep Ophthalmol 2011;2:84–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Karimi S, Nourinia R, Mashayekhi A. Circumscribed choroidal hemangioma. J Ophthalmic Vis Res 2015;10:320–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shields CL, Honavar SG, Shields JA, Cater J, Demirci H. Circumscribed choroidal hemangioma: clinical manifestations and factors predictive of visual outcome in 200 consecutive cases. Ophthalmology 2001;108:2237–48. [DOI] [PubMed] [Google Scholar]
- 4.Kwon HJ, Kim M, Lee CS, Lee SC. Treatment of serous macular detachment associated with circumscribed choroidal hemangioma. Am J Ophthalmol 2012;154:137–45.e1. [DOI] [PubMed] [Google Scholar]
- 5.Tanabe H, Sahashi K, Kitano T, Tomita Y, Saito AM, Hirose H. Effects of oral propranolol on circumscribed choroidal hemangioma: a pilot study. JAMA Ophthalmol 2013;131:1617–22. [DOI] [PubMed] [Google Scholar]
- 6.Storch CH, Hoeger PH. Propranolol for infantile haemangiomas: insights into the molecular mechanisms of action. Br J Dermatol 2010;163:269–74. [DOI] [PubMed] [Google Scholar]
- 7.Tanabe H, Sahashi K, Kitano T, Tomita Y, Saito AM, Hirose H. Effects of oral propranolol on a juxtapapillary capillary hemangioma: a single-subject pilot study. Ophthalmic Surg Lasers Imaging Retina 2015;46:380–83. [DOI] [PubMed] [Google Scholar]