Abstract
Objective:
To examine whether working alliance quality and use of techniques predict improvement in Panic-Specific Reflection Function (PSRF), and misinterpretation of bodily sensations in treatments for panic disorder.
Method:
A sample of 161 patients received either CBT or PFPP (Panic-focused Psychodynamic therapy) within a larger RCT (Milrod et al., 2016). Data were collected on patient-reported working alliance, misinterpretations, PSRF, observer-coded use of techniques, and interviewer-rated panic severity. Random-Intercept Cross-Lagged Panel Models assessed bi-directional associations, disentangling within- and between-patient effects, and accounting for prior change.
Results:
Higher alliance predicted subsequent within-patient improvement in PSRF in PFPP, but worsening in CBT. In both treatments, focus on interpersonal relationships predicted PRSF improvement (with stronger effects in CBT), while focus on thoughts and behaviors predicted worsening in PSRF. In CBT only, early focus on affect and moment-to-moment experience predicted reduced misinterpretation, while high focus on thoughts and cognitions predicted subsequent increase in misinterpretation.
Conclusion:
The quality of the alliance has differential effects on PSRF in distinct treatments. Interpersonal, rather than cognitive or behavioral focus, even when delivered differently within distinct treatments with high adherence, could facilitate improvement in PSRF. Additionally, early focus on affect and moment-to-moment experiences in CBT could reduce misinterpretations.
The importance of identifying the active ingredients (i.e., candidate mechanisms of change) leading to therapeutic improvement in different psychotherapies is well-recognized. However, there is still a relative lack of rigorous empirical work examining the role of such mechanisms, especially in studies with appropriate statistical power (Kazdin, 2007; Kraemer, Wilson, Fairburn, & Agras, 2002). Even when studies have been able to identify specific theory-driven candidate mechanisms of change, researchers rarely examined the role of these mechanisms outside of their own modality (see Gibbons et al., 2009; Barber et al., 2019, for exceptions), despite the important clinical utility of such investigations (Gibbons et al., 2009).
Most psychotherapy researchers agree that the therapeutic relationship and the use of specific therapeutic techniques are the two key features that facilitate therapeutic change (Goldfried & Davila, 2005). However, beyond their association with symptomatic improvement, we still know little about their roles in facilitating therapeutic change. The current study will investigate whether the therapeutic alliance and technique use predict subsequent improvement in two theory-driven candidate mechanisms of change, both of which received preliminary empirical support in the last several decades: (a) Misinterpretation of bodily sensations (Clark, 1986) and (b) Panic-specific Reflective Function (Barber et al., 2019; Rudden et al., 2006; 2009).
Candidate Mechanisms of Change in Treatments for Panic Disorder
Misinterpretation of bodily sensations.
Cognitive-behavioral treatments for panic disorder rely on the premise that panic patients have a tendency to catastrophize and misinterpret bodily sensations as a sign of real danger (e.g., a heart attack, insanity, loss of control). This in turn escalates the severity of panic symptoms, thus further reinforcing the catastrophic cognitions and creating a vicious cycle of anxiety and panic (Clark, 1986). Decrease in misinterpretation of bodily sensations is associated with subsequent reduction in panic symptoms in CBT (Arntz, 2002; Casey et al., 2005; Clark, 1994; 1999; Teachman, Marker, & Clerkin, 2010). Compared to waitlist conditions, patients receiving CBT have showed greater reductions in misinterpretations (Casey, Newcomb, & Oei, 2005; Clark et al., 1999; Smits, Powers, Cho, & Telch, 2004), with some preliminary evidence suggesting greater benefits of change in misinterpretations in CBT compared to other treatments (Arntz, 2002; Clark, 1994; Hoffman et al., 2007; Meuret et al., 2010). Two studies examined the role of misinterpretation of bodily sensation as a mediator of treatment and outcome. While results provided preliminary supporting evidence, the authors in both studies indicated that full temporal precedence could not be established within the study design, and thus, future studies with longitudinal data will be needed (Hoffman et al., 2007; Meuret et al., 2010). Recently, our group found that, in the current sample, early change in misinterpretations predicted subsequent improvement in panic symptoms in both CBT and PFPP (Barber et al., 2019).
Panic-Specific Reflective Function.
Mentalization or in its operationalized term – Reflective Function (RF) – has been identified as a potential mechanism of change in psychotherapy (Bateman & Fonagy, 2012; see Barber et al., 2013 for a review). RF is defined as the capacity to understand and interpret – implicitly and explicitly – one’s own and others’ behaviors as an expression of mental states such as feelings, thoughts, fantasies, beliefs and desires (Fonagy, Gergely, Jurist, & Target, 2002). Rudden, Milrod, and colleagues (2006; 2009) suggested that given that RF is relatively stable over time, it may not change significantly in brief therapies. Thus, they formulated a new construct – Symptom-Specific Reflective Function (SSRF), or in the case of panic-disorder – Panic-Specific Reflective Function (PSRF) (Rudden et al., 2006; 2009). While RF is measured by assessing one’s capacity to reflect on the self and the minds of others [interpersonal relationships], SSRF refers to the ability to reflect on the psychological underpinnings and emotional meaning of symptoms (Rudden et al., 2009). A small pilot study showed that panic patients receiving panic-focused psychodynamic therapy (PFPP) demonstrated improvement in PSRF during treatment, and that this change in PSRF was correlated with symptom relief (Rudden et al., 2006). Another study showed that pre-treatment SSRF levels predicted symptomatic decrease in CBT and IPT for depression (Ekeblad, Falkenström, & Holmqvist, 2016).
In a recent study, our group has shown that increase in PSRF and reduction in misinterpretations predicted subsequent reduction in panic symptoms in both CBT and PFPP (Barber et al., 2019). Thus, identifying specific treatment components which lead or contribute to improvement in these candidate mechanisms could advance our understanding of the trajectories leading to change in these capacities and translate to meaningful clinical recommendations.
Our research questions will be investigated in a sample of panic patients who received either CBT (Craske, Barlow, & Meadows, 2000) or PFPP (Busch, Milrod, Singer, & Aronson, 2012), and Applied Relaxation Therapy (ART; control group) as part of a large-scale, two-site randomized controlled trial for panic disorder (Milrod et al., 2016). Overall, it was found that both PFPP and CBT were effective in panic reduction, with equal efficacy at one site but superiority for CBT at the other (see Milrod et al., 2016 for details). The current study will focus solely on the CBT and PFPP arms due to significantly high rates of drop-outs in the ART arm and high percentage of missing data (see Milrod et al., 2016).
Does Alliance Predict Improvement in Misinterpretation of Bodily Sensations and PSRF?
The working alliance (Bordin, 1979) has been recognized as a trans-theoretical concept and a common factor – a vehicle of change shared by all psychotherapies (Wampold, 2001). The effect of the working alliance on symptom change has been well-documented in both CBT (e.g., Arnow et al., 2013; Castonguay, Constantino, McAleavey, & Goldfried, 2010), and psychodynamic therapies (e.g., Falkenström, Granstrom, & Holqvist, 2014; Zilcha-Mano, Dinger, McCarthy, & Barber, 2014). In the past decade studies investigating the alliance-outcome association have highlighted the importance of disentangling between-patient aspects (i.e. differences between patients’ means of alliance and symptoms), from within-patient fluctuations over time (i.e. changes in individual patients’ deviations from their own mean of alliance and symptoms) (e.g. Falkenström et al., 2014; 2017; Falkenström, Kuria, Othieno, & Kumar, 2018; Zilcha-Mano & Errázuriz, 2017; and see Flückiger, Del Re, Wampold, & Horvath, 2018 for recent meta-analysis). While findings on the alliance-outcome relationship are robust, we still have limited understanding of the ways in which fluctuations in alliance effect patients’ therapeutic trajectories (DeRubeis, Brotman, & Gibbons, 2005), as we know little about the specific capacities patients develop as a result of a strong working alliance.
To the best of our knowledge, only one study directly investigated the relation between alliance and misinterpretation of bodily sensations. Casey, Oei, and Newcomb (2005) found that when controlling for symptomatic change, patients’ (but not therapists’) alliance ratings significantly predicted change in misinterpretations in the first half of CBT for panic disorder, while only therapists’ ratings predicted change in misinterpretations in the second half of therapy. Only one study directly examined the alliance-PSRF relation and found that lower pretreatment PSRF predicted significantly lower therapist- and patient-reported working alliance in both CBT and IPT for depression, but change in alliance over time was not assessed (Ekeblad et al., 2016). Conceptually, the working alliance is presumed to consist the agreement on tasks and goals of therapy, supported by a positive emotional bond (Bordin, 1979). Thus, a strong alliance could potentially facilitate change in the specific mechanisms of target in specific treatments. We hypothesized that higher alliance would predict improvement in misinterpretations in CBT, with no change in PFPP, given that misinterpretations were not the main focus of the latter treatment. Similarly, we hypothesized that in PFPP, higher alliance would predict subsequent increases in PSRF, but not in CBT, since change PSRF is not the focus of cognitive-behavioral treatments.
To ensure that our results are not the by-product of symptomatic change and the alliance-symptom association, and to account for reverse causation (i.e., change in candidate mechanisms predicts change in alliance), we investigated the bi-directional relation between candidate mechanisms and alliance, and accounted for symptomatic change, as well as prior change and reverse causation (see Falkenström et al., 2014; 2017; Zilcha-Mano et al., 2014 for use of similar methodologies).
Which Techniques Predict Change in Misinterpretations of Bodily Sensations and PSRF?
Our second research question focused on investigating whether therapists’ use of interventions would predict subsequent improvement in the predictors or candidate mechanisms studied. Studies on the current RCT sample have previously shown that therapists in this trial were adherent to the specific interventions prescribed by their treatment manuals (Milrod et al., 2016). We focused on the broader categories of therapist behaviors drawn from five subscales of the Multitheoretical List of Interventions – Observer rating scale (MULTI, McCarthy & Barber, 2009). We examined whether therapists’ focus on thoughts, behaviors, affect, experiences in therapy, moment-to-moment experiences, and social and interpersonal relationships predicted subsequent change. These were represented by scores on the MULTI cognitive, behavioral, psychodynamic, process-experiential, and interpersonal subscales, respectively. The MULTI subscales largely reflect what a therapist chooses to talk about in session rather than the way in which he/she implements the treatment modality. Thus, both PFPP and CBT therapists might be coded as using a process-experiential approach – focus on present experience – but this would look very different in the two treatments. The CBT therapist might try to capture the patient’s immediate experience of symptoms in the session, whereas the PFPP therapist may attempt to explore the patient’s feelings as they discuss termination. Examples for each subscale can be found in Table 1.
Table 1.
Examples for use of interventions coded using the Multitheoretical List of Interventions in PFPP and CBT
| MULTI Subscale | Focus of Interventions | PFPP | CBT |
|---|---|---|---|
| Process-experiential | Focusing on moment-to-moment experience, labeling affect, identifying internal conflicts | Tx:”Can we try in here right now to talk about the feelings that are gushing in hopes that being able to talk about them with me will help organizing them in your mind instead of putting it in a can? [exploring moment-to-moment experience] | Tx:”What are you experiencing right now? Are you feeling dizzy? Unreal?” [exploring moment-to-moment experience] |
| Interpersonal | Focusing on present relationships which may relate to patient’s panic; identifying potential changes that could be made in these relationships | Tx: “It’s been tough trying to find the balance of someone who loves you but doesn’t take advantage of you. It’s been hard to share being vulnerable, and yet it sounds like the flip side of being vulnerable, is that then others become overbearing. [identifying recurring relationship patterns] | Pt:[discussing panic symptoms emerging in the context of fear of her elderly parents’ death]: “I don’t understand how I would continue to exist without their love and support” Tx:”I wanna talk about something unpleasant you don’t wanna talk about, which is your parents not being around at some point. The thing that makes it so anxiety-provoking is the belief that you have no comprehension of what would happen if they would die.” [focusing on loss; making connection between interpersonal relationship concern and symptoms; focusing on role of patient’s beliefs] |
| Psychodynamic | Exploring patient’s feelings about therapy; identifying avoided affect; inquiring about past/childhood experiences which may relate to panic symptoms | Tx:”I am a little worried you came in late [to session], you seem like you want to do this, but at the same time you were late. Do you think that therapy has intensified your feelings of dependency? Because there’s something about the nature of therapy that intensifies it?” [exploring feelings about therapy] | Tx:”We wanna think about a plan going forward, how are you gonna maintain some of these gains? Pt:” Oh gosh…I don’t know…” Tx:”If you are having any thoughts about ending treatment and what would that be like those could also go into thought record.” [exploring patient’s feelings about therapy with a focus on cognition] |
| Cognitive | Focusing on perceptions and thoughts that may relate to panic; identifying triggers for panic; exploring the patient’s perspective on his/her panic and offering an alternative perspective | Pt: ” I checked my FB page to see who commented on my post, and then I slept for two hours…I’m putting a lot of pressure on myself. “ Tx: “So after the change in your FB status, you have been feeling anxious? What were you worried was going to happen?” [identifying trigger for panic; exploring patient’s fear of consequences of his/her behavior] |
Tx:” What about some of the thoughts that go through your head when you have a panic attack? What about during the panic attack, do you have any thoughts about the symptoms, like let’s say during heart palpitations do you have any thoughts it’s a heart attack? Fears of fainting?” [making connections between thoughts and symptoms] |
| Behavioral | Focusing on patients’ actions/behaviors as they relate to panic; making suggestions of potential changes patients can make in their behaviors | Tx: “The feelings of dependency are despicable to you so they get channeled into a panicky realm. The tool that should help contain these feelings is an intellectual acceptance of the feelings with a knowledge about their nature. By being so afraid of the feelings, they get larger and so is the fear of exposure…Your coping style is of total avoidance. Once you’re able to articulate the feelings it will help contain them” [identifying coping strategy; facilitating behavioral change; offering an alternative perspective] | Tx: “You don’t have control over changing your boss’s mind, but you do have control over looking for another job, hanging out with friends, spend more time working out.” [exploring alternative behavioral coping strategies; providing practical advice”] |
While no study directly examined whether use of specific techniques predicts change in the candidate mechanisms investigated, preliminary evidence has shown that patients show improvement in misinterpretations when provided with behaviorally focused treatment (i.e., breathing training; Meuret, Rosenfield, Seidel, Bhaskara, & Hofmann, 2010), and cognitive treatment (i.e., cognitive restructuring; Meuret, Hofmann, & Rosenfield, 2010; Meuret et al., 2010). We hypothesized that focusing on the patient’s thoughts and perspectives on panic symptoms (MULTI cognitive subscale) and behaviors and actions (MULTI behavioral subscale) would predict subsequent decrease in misinterpretation of bodily sensations in both CBT and PFPP. Additionally, based on mentalization theory (Bateman & Fonagy, 2012; Fonagy et al., 2002), we predicted that focusing on patients’ affect and moment-to-moment experience (process-experiential MULTI subscale), feelings about therapy, past events related to symptoms and avoided affect (psychodynamic MULTI subscale), and social and interpersonal relationships (interpersonal MULTI subscale) would predict improvement in PSRF in both CBT and PFPP.
Most studies that investigated the role of misinterpretations and PSRF in psychotherapy did not account for temporal precedence and reverse causation, while also disentangling the within-patient effects (i.e., session-by-session changes in patients’ alliance, misinterpretations and PSRF), from the between-patient variation (i.e., patients’ average scores across sessions) (see Teachman et al., 2010; Meuret et al., 2010 for exceptions). Controlling for between-patient variance is especially crucial when examining changes in emotional and cognitive capacities that are generally stable over time. Previous conceptual work has shown that patients have a predisposing (‘trait-like’) tendency to develop a strong alliance (e.g. Zilcha-Mano, 2017), mentalize (e.g. Allen, Fonagy, & Bateman, 2008), and misinterpret bodily sensations (Clark, 1986).
In the current study, we employed novel methodological developments of dynamic cross-lagged panel modeling (e.g. Falkenström et al. 2017; Hamaker, Kuiper, & Grasman, 2015), which allowed us not only to account for prior change and assess the direction of causality by accounting for reverse causation, but also to isolate within-person changes over time from stable between-person differences. Because some authors (e.g. Barber et al., 2008, 2006; McCarthy, Keefe, & Barber, 2016) have found curvilinear relationships between use of techniques and outcome, indicating that moderate use of specific techniques predicted greater subsequent symptomatic relief, we assessed the presence of curvilinear change paths in our sample.
In summary, based on previous studies described above, we hypothesized that: (a) higher levels of alliance will predict: (a1) subsequent increase in PSRF in PFFP (but not CBT); (a2) subsequent reduction in misinterpretations of bodily sensations in CBT (but not PFPP); (b) focus on affect and moment-to-moment experience, feelings about therapy, past events related to symptoms and avoided affect, and social and interpersonal relationships would predict increase in PSRF in both CBT and PFPP; (d) focus on the patient’s thoughts and behaviors would predict subsequent decrease in misinterpretation of bodily sensations in both treatments.
Method
Participants
Patients.
A sample of 201 patients was randomized to three conditions (CBT, PFPP, and Applied Relaxation Therapy) at Weill Cornell Medical College and University of Pennsylvania. This report covers 161 patients assigned to either CBT or PFPP. All patients signed written informed consent. Mean age was 39 (SD = 13.22), with 65% females (n = 105), 74% White (n = 119), 19% Black (n = 31), 5% Asian (n = 8), 1% Native-American (n = 1). Seventeen percent of patients self-identified as Hispanic (n = 28). The inclusion criterion was occurrence of ≥ 1 spontaneous panic attack weekly over a period of the month before entry. Exclusion criteria included active substance dependence (< 6 months’ remission), history of psychosis or bipolar disorder, acute suicidality, and organic mental syndrome. Patients were diagnosed with primary DSM-IV panic disorder with (79%) or without (21%) agoraphobia on the Anxiety Disorders Interview Schedule for DSM-IV Lifetime Version (ADIS-IV; DiNardo, Brown, & Barlow, 1995). Medications were permitted if stable for ≥ 2 months at presentation and were held constant and monitored. The protocol was approved by the institutional review boards in both sites (see Milrod et al., 2016 for details).
Therapists.
Twenty-four therapists (12 female and 12 male) provided one treatment modality only and received training and supervision in that modality prior to and during the trial. Sample included 12 MDs, 11 PhDs, and one PsyD. Therapists had an average of 13 years of post-degree experience (SD = 7.5), with 6 years (SD = 6.3) of experience in time-limited treatment and at least a year’s experience with panic disorder treatment.
Treatments
Cognitive-Behavioral Therapy (CBT; Craske, Barlow, & Meadows, 2000).
The Panic Control Therapy protocol was manualized and modified to fit a 12-week 24-session/45-minute format. Treatment focused on psychoeducation about anxiety and panic, identification and alteration of maladaptive thoughts about panic and anxiety, relaxation training focused on slow diaphragmatic breathing, and interoceptive exposure to bodily sensations designed to mimic sensations experienced in panic. For patients with agoraphobia, in vivo exposure was conducted via homework at Sessions 17-23. Session 24 focused on review and relapse prevention.
Panic-Focused Psychodynamic Psychotherapy (PFPP; Milrod, Busch, Cooper, & Shapiro, 1997).
PFPP protocol included 12-week 24-session/45-minute format. This is a manualized, evidence-based treatment focused on identifying the psychological meanings of the patient’s panic symptoms by uncovering inaccessible feelings and conflicts underlying panic. It consists of three phases: (a) Treatment of acute panic, (b) treatment of panic vulnerability, and (c) termination. PFPP is aimed at increasing patients’ PSRF through identification and expression of anger and guilt surrounding the attacks, exploration of emotional and interpersonal triggers of panic and the underlying emotional and interpersonal conflicts through transference interpretations, and focus on reactions to loss of the therapist at termination.
Measures
Panic Disorder Severity Scale (PDSS; Shear et al., 1997).
Symptomatic outcome was assessed using a 7-item diagnostician-rated scale that provides a diagnosis-based, composite, global rating of Panic Disorder severity. It was administered at baseline, termination, and weeks 1, 5 and 9. Interviewers were MA or PhD diagnosticians who were uninformed as to treatment assignment. Interrater reliability across sites was excellent, ρI =.95, as well as the internal consistency (α = .88) (Milrod et al., 2016).
Reflective Function Interview (Rudden, Milrod, & Target, 2006).
A brief, semi-structured interview assessing RF and PSRF (with questions measuring each of the constructs) was administered in Weeks 1, 5, and 12 (termination). Interview transcripts were coded by three doctoral-level trained coders who were uninformed as to treatment assignment. Interrater reliability was acceptable to excellent as indicated by intraclass correlation coefficients (ICC[2,2] Shrout & Fleiss, 1979) (.72 < ρi < .80).
Brief Bodily Sensations Interpretation Questionnaire (BBSIQ; Clark et al., 1997).
A 7-item self-report measure of catastrophic misinterpretation of panic-related bodily sensations was administered at Weeks 1, 5, and 12 (termination). The BBSIQ has been shown to be internally consistent (α = .86) and reliable over a 3-month period (r = .73). It has demonstrated convergent and discriminant validity and criterion-related validity relative to diagnosis. It was found internally consistent in our study (α =.87).
Working Alliance Inventory-Short Form (WAI-SF; Tracey & Kokotovic, 1989).
The self-report 12-item measure (patient version) was administered at Weeks 1, 3, and 5. Each item was rated on a 7-point Likert-type scale ranging from 1 (never) to 7 (always). Internal consistency in our sample ranged from α = 0.85 to α = 0.88 at the different time points assessed.
Multitheoretical List of Therapeutic Interventions (MULTI; McCarthy & Barber, 2009).
The use of therapeutic techniques was measured using the observer-based rating scale. Five (out of eight) subscales, representing the therapeutic orientations expected to be employed in our trial, were included in the current analyses (behavioral, cognitive, interpersonal, psychodynamic and process-experiential). Each of the MULTI items represents use of a specific technique (e.g., “the therapist explored the client’s dreams, wishes, and desires”), which was rated on a scale ranging from 1 (not at all) to 5 (very) according to how typical a given intervention was to the session. Subscales were created by averaging items belonging to each orientation. Previous studies found the MULTI internally consistent and reliable (e.g. McCarthy & Barber, 2009; McCarthy et al., 2016). MULTI raters (N=25) were advanced Clinical Psychology doctoral students who received at least 20 hours of training. Coders were required to achieve at least acceptable interrater reliability (intraclass correlations >.60) before beginning coding and received ongoing supervision. Therapy sessions were videotaped during the trial for coding purposes. Each therapy session was coded by at least two reliable raters (M=2.58 raters per session) and the mean of raters’ coding was used for analyses. Overall, 830 codings were collected. Intraclass correlations were calculated using lme4 package in R (R Core Team, 2016), and were in the acceptable to good range (.63≤ ρi [2,2]≤.80).
Statistical Analytic Plan
We assessed the time-lagged associations between our independent (alliance and use of techniques) and dependent (PSRF and misinterpretation of bodily sensations) variables using Random-Intercept Cross-Lagged Panel Models (RI-CLPM; Hamaker et al., 2015). The commonly used CLPM only accounts for temporal precedence through inclusion of autoregressive and cross-lagged parameters, thus assuming that each patient’s deviation from the group and individual mean varies across the time points, with no stable trait-like individual differences. This assumption is problematic given the relative stability in psychological constructs over time (Falkenström et al. 2017, Hamaker et al., 2015). Ignoring this distinction will mean that analyses will confound stable individual differences with fluctuations over time.
The RI-CLPM uses within-patient deviation scores for cross-lagged and auto-regressions, while accounting for trait-like stable differences, by estimating between-level variance through the inclusion of a random intercept for both independent and dependent variables. Within-patient deviation scores are unaffected by any variable that is stable over the studied time-period. Thus, any patient variable that is unlikely to change during the study cannot affect results on the within-patient level. Importantly, this includes differences between therapists (e.g. personality characteristics, adherence, competence; Falkenström et al., 2017). In studies of treatment effects, it has long been recognized that ignoring nesting within therapists can increase Type-I error rate substantially due to artificially decreased standard errors (e.g. Crits-Christoph & Mintz, 1991). However, this does not hold for within-patient effects, since they are estimated on level-1 and therapists would be modeled on level-3. In such a scenario, ignoring nesting within therapists affects standard errors on level-2, but not on level-1 (Moerbeek, 2004).
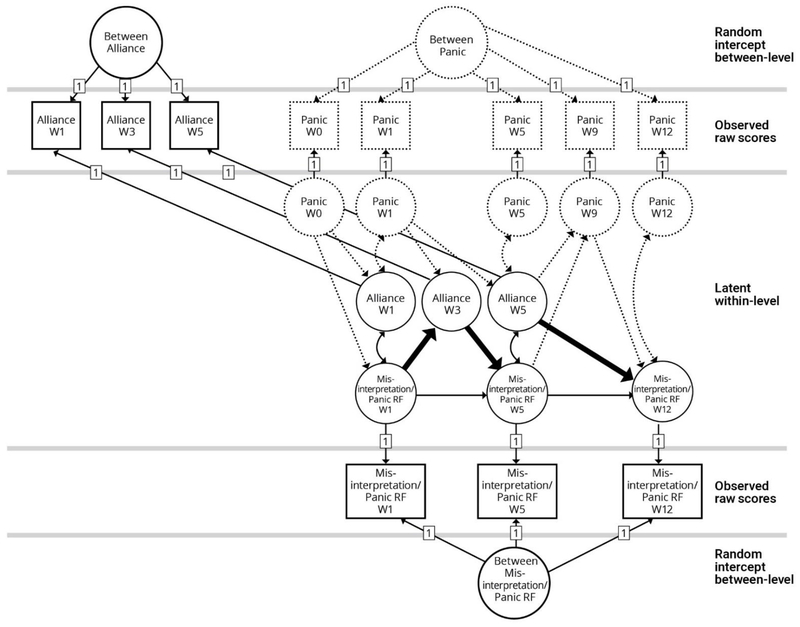
Figure 1 represents the analyses we conducted in order to examine whether higher levels of alliance predict subsequent increase in PSRF and reduction in misinterpretation of bodily sensations. The top and bottom circles (labeled Between Alliance, Between Panic and Between Misinterpretation/Panic RF) represent the random intercepts – the latent between-level variables, which capture the variation among patients in their overall means. The time-specific deviations from each person’s mean, representing within-person fluctuations over time, are estimated by including a latent deviation variable at each time point (represented by circles in Figure 1). In the case of the working alliance, we included the symptomatic measure (PDSS), in order to ensure that the alliance-predictor (i.e. PSRF or misinterpretations) association is not a by-product of symptomatic improvement over time (i.e. patients’ capacities improve as a result of symptomatic relief) (see Figure 1). To insure that our findings are not due to over controlled models, we conducted all analyses in a RI-CLPM model, without controlling for symptom levels across time. Results were equivalent and thus not reported in this manuscript. The main paths which examined our hypotheses are bolded in the figure.
Figure 1.
Random-Intercept Cross-Lagged Panel Model (RI-CLPM) testing hypotheses regarding the alliance-misinterpretation of bodily sensations as well as alliance-PSRF relationships over time. Paths of interest are bolded. The top and bottom circles (“Between”) represent the random intercepts –latent between-level variables. The squares represent observed variables (each assigned with a loading of 1 on the latent between-level variable). The circles represent latent within-level variable for each time-point. Misinterpretation of bodily sensations and panic-specific reflective function were tested in separate models.
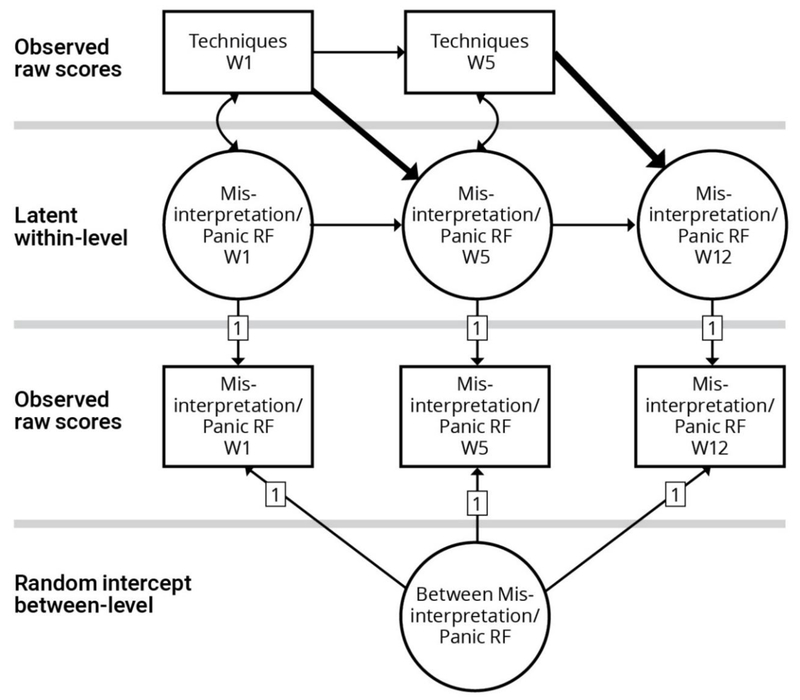
Figure 2 represents the analyses we conducted to investigate whether use of specific techniques (as coded using the MULTI) predict subsequent increase in PSRF and reduction in misinterpretations. Since RI-CLPM requires at least three measurement waves (Hamaker et al., 2015) and use of techniques was only measured at two time points (Week 1 and 5), the techniques variables were estimated using the regular CLPM and scores represent both within- and between- components of variance. As presented in Figure 2, the upper part of the model (i.e. techniques measured by the MULTI) was estimated using CLPM (i.e., path coefficients for the observed, rather than latent variables), and the candidate mechanisms (i.e. PSRF and misinterpretations) were estimated within a RI-CLPM framework. Overall, we assessed whether patients’ within-level fluctuations in alliance and use of techniques (Figures 1 and 2 respectively) predicted subsequent within-level fluctuations in PSRF and misinterpretation of bodily sensations, controlling for prior levels of these variables.
Figure 2.
Random-Intercept, and standard Cross-Lagged Panel Model (RI-CLPM; CLPM) testing the hypotheses regarding the association between use of techniques and PSRF as well as misinterpretation of bodily sensations. The top part of the figure represents CLPM for techniques measured using the MULTI subscales. The bottom part represents RI-CLPM for panic-focused reflective function (PSRF). The bottom circle represent the random intercepts – the latent between-level variable. The squares represent the observed variables (each assigned with a loading of 1 on the latent between-level variable). The circles represent latent within-level variable for each time-point for misinterpretations and PSRF. Misinterpretation of bodily sensations and panic-specific reflective function were tested in separate models
We report the within-level cross-lagged relationships, after controlling for between-level variation and prior change in symptoms (with the exception of techniques as indicated above), since the focus of our study was identifying the relationship between within-patient fluctuations over the course of treatment. RI-CLPM models estimated the cross-lagged associations in PFPP and CBT simultaneously but separately (i.e., two-group models). In a few cases, Heywood cases in the form of negative variance estimates were encountered. Since these were most likely caused by difficulties separating autoregression from between-level variance with only three repeated measures, these were handled by constraining either the variances or the correlation between random effects to zero. These models were also re-run using Bayesian estimation, which does not yield negative variance estimates due to the use of prior distributions that do not contain zero, as a sensitivity analysis. In all cases results were highly similar when Bayesian estimation was used.
Analyses were conducted in Mplus, version 8 (Muthén, & Muthén, 1998-2012). Missing data1 was handled by basing estimates on all available information, using Full Information Maximum Likelihood estimation with robust standard errors. Standardized path coefficients for within-level effects are reported. Reverse causation (i.e., change in candidate mechanisms predict change in alliance or use of techniques) was estimated in all the models and was non-significant unless reported otherwise. Finally, following others’ work (McCarthy et al., 2016) we assessed curvilinear relationships between use of techniques and subsequent change in mechanisms. No significant results emerged, and thus these will not be reported for the purpose of brevity.2
Results
In the primary trial a pattern of non-missing data at random (NMAR) was detected, as patients with worse panic symptoms trajectories were more likely to terminate treatment early Milrod et al., 2016. We tested NMAR in the current sample to examine whether data in the alliance (WAI), misinterpretations (BBSIQ) and panic-focused reflective function (PSRF) was missing at random using TestMCARNormality function in BaylorEdPsych package in R (Beaujean, 2012). Hawkins Test was non-significant (p=.46); thus the NMAR hypothesis was not rejected, thus indicating a random pattern of missingness. Descriptive statistics are presented in Tables 2 and 3. As expected, in both treatments therapists showed low levels (1.4<M<2.2) of use of interventions outside of their theoretical system. PFPP therapists showed low focus on thoughts and actions, and CBT therapists showed low focus on affect, moment-to-moment experience, feelings about therapy, past events related to panic, and social and interpersonal relationships. Fit indices and constraints implemented are included in Appendix A.
Table 2.
Means and Standard Deviations for Measures of Panic Symptoms, Panic-Specific Reflective Function, Misinterpretation of Bodily Sensations, and Working Alliance across Treatment
| PFPP | CBT | ||||
|---|---|---|---|---|---|
| Variable | Time | n | M (SD) | n | M (SD) |
| Panic Symptoms (PDSS) | Baseline | 80 | 14.19(3.46) | 81 | 13.56 (3.83) |
| Week 1 | 70 | 11.73(3.75) | 73 | 12.04 (4.37) | |
| Week 5 | 64 | 9.88 (4.13) | 65 | 9.4 (4.29) | |
| Week 9 | 55 | 8.58 (4.67) | 56 | 7.32 (4.17) | |
| Week 10 | 63 | 7.41 (4.61) | 61 | 5.54 (3.59) | |
| Panic-Specific Reflective Function (PSRF) | Baseline | 74 | 3.38 (1.2) | 70 | 3.62 (1.2) |
| Week 5 | 56 | 4.13 (1.12) | 58 | 3.66 (1.22) | |
| Week 10 | 54 | 4.36 (1.35) | 54 | 3.7 (1.09) | |
| Misinterpretation of Bodily Sensations (BBSIQ) | Baseline | 73 | 1.96 (0.39) | 78 | 1.89 (0.39) |
| Week 5 | 40 | 1.89 (0.4) | 46 | 1.8 (0.4) | |
| Week 10 | 54 | 1.83 (0.4) | 58 | 1.57 (0.29) | |
| Working Alliance (WAI) | Week 1 | 44 | 5.26 (1.22) | 54 | 5.65 (0.92) |
| Week 3 | 40 | 5.41 (1.09) | 54 | 5.77 (0.9) | |
| Week 5 | 39 | 5.49 (1.03) | 43 | 6.01 (0.81) | |
Note. PDSS=Panic Disorder Severity Scale; PSRF= Panic-specific Reflective Function; BBSIQ= Brief Bodily Sensations Interpretation Questionnaire; WAI= Working Alliance Inventory – Client Version
Table 3.
Means and Standard Deviations for Use of Specific Theory-Driven Therapeutic Techniques across Treatment
| PFPP | CBT | |||||
|---|---|---|---|---|---|---|
| MULTI subscale | Time | n | M (SD) | n | M (SD) | |
| Insight-Oriented/Exploratory | Psychodynamic | Week 1 | 55 | 2.85 (0.54) | 74 | 1.46 (0.24) |
| Week 5 | 50 | 2.76 (0.57) | 67 | 1.41 (0.27) | ||
| Process Experiential |
Week 1 | 55 | 2.72 (0.49) | 74 | 1.9 (0.24) | |
| Week 5 | 50 | 2.96 (0.6) | 67 | 2.06 (0.28) | ||
| Interpersonal | Week 1 | 55 | 2.28 (0.39) | 74 | 1.4 (0.22) | |
| Week 5 | 50 | 2.36 (0.77) | 67 | 1.44 (0.38) | ||
| Directive | Behavioral | Week 1 | 55 | 1.84 (0.27) | 74 | 2.8 (0.29) |
| Week 5 | 50 | 1.91 (0.31) | 67 | 2.99 (0.35) | ||
| Cognitive | Week 1 | 55 | 2.11 (0.32) | 74 | 3.00 (0.33) | |
| Week 5 | 50 | 2.2 (0.38) | 67 | 3.25 (0.34) | ||
Note. MULTI= Multitheoretical List of Interventions; PFPP= Panic Focused Psychodynamic Psychotherapy; CBT=Cognitive Behavioral Therapy
Does the Working Alliance Predict Change in Misinterpretations of Bodily Sensations (BBSIQ) and PSRF, beyond Symptomatic Change?
Misinterpretation of bodily sensations (BBSIQ).
We assessed the alliance-misinterpretations association while accounting for within- and between- level variances in panic symptoms (assessed by the PDSS) across time. No significant effects were found for this relationships. While the misinterpretations-symptoms association was not part of our analyses, these paths were included in our model, and thus, we investigated their association in an exploratory post-hoc manner. We found that when controlling for alliance levels, lower panic severity scores at Week 1 predicted a decrease in misinterpretations at Week 5 in both CBT (β = .26, p<.01) and PFPP (β=.30, p<.01). Additionally, lower panic severity at Week 9 predicted a decrease in misinterpretations at termination in both CBT (β = .40, p<.01) and PFPP (β = .37, p=.03).
Panic-specific reflective function (PSRF).
We assessed the alliance-panic RF (PSRF) association while accounting for within- and between- level variances in panic symptoms across time. In CBT, higher alliance levels at Week 5 predicted a significant decrease in PSRF at termination (β = −.40, p=.04). In PFPP, as predicted, higher alliance levels at Week 3 predicted an increase in PSRF at Week 5 (β = .74, p<.01), and higher alliance levels at Week 5 predicted an increase in PSRF at termination (β =.44, p<.01).
Does Use of Specific Techniques predict Change in Misinterpretations of Bodily Sensations (BBSIQ) and PSRF?
Misinterpretation of bodily sensations.
Contrary to our hypothesis, in CBT (but not in PFPP) greater focus on the patient’s thoughts and cognitions (cognitive subscale) at Week 1 predicted an increase in misinterpretation at Week 5 (β = .40, p<.01). However, in CBT, greater focus on the patient’s affect and moment-to-moment experiences (process-experiential MULTI subscale) at Week 1 predicted a decrease in misinterpretations at Week 5 (β = −.27, p=.03).
Panic-specific reflective function.
In CBT (but not in PFPP), focusing on the patient’s experiences in therapy (e.g., whether the patient finds the interventions helpful) and reviewing history of panic symptoms (i.e., past events) at Week 5 (MULTI psychodynamic subscale) predicted PSRF increase at termination (β = .38; p<.01). In both treatments, greater focus on social and interpersonal relationships (MULTI interpersonal subscale) at Week 1 predicted PSRF increase at Week 5 (although findings are at the trend level in PFPP) (CBT; β = .39; p<.01; PFPP; β = .17; p=.09). Similarly, in PFPP (but not CBT), greater focus on interpersonal and social relationships at Week 5 was associated with PSRF increase at termination (β = .26; p = .05).
Additionally, in both treatments, greater focus on the patient’s actions and behaviors (MULTI behavioral subscale; PFPP; β = −.31; p=.04, CBT; β = −.37; p=.02) at Week 1 predicted a decrease in PSRF at Week 5. Focus thoughts and cognitions (MULTI cognitive subscale; CBT; β = −.31; p<.01, PFPP; β = −.33; p=.06) at Week 1 predicted a decrease in PSRF at Week 5 (trend-level in PFPP). In PFPP (but not CBT), greater focus on the patient’s behaviors and actions (β = −.27; p=.04) as well as thoughts and cognitions (β = −.29; p=.03) at Week 5 predicted PSRF decrease at termination.
Discussion
Overall, our results showed that stronger alliance predicted subsequent improvement in panic-specific reflective function (PSRF) in psychodynamic therapy (PFPP), but worsening PSRF in CBT. We did not find significant associations between the quality of the working alliance and subsequent changes in misinterpretation of bodily sensations. However, when controlling for alliance levels, reduction in panic severity predicted subsequent reduction in misinterpretations (but not the other way around). With regard to techniques use as a predictor of change in PSRF and misinterpretations, we found that focus on patients’ interpersonal and social relationships predicted subsequent improvement in both CBT and PFFP (with stronger effects in CBT). In contrast, in both treatments, focus on behaviors and cognitions (i.e. use of behavioral and cognitive techniques) predicted worsening in PSRF (with differences between treatments in time-lagged findings). In CBT, greater focus on patients’ experiences in therapy and review of patient’s history (i.e. psychodynamic multi scale) predicted subsequent increase in PSRF. Additionally, in CBT, early high focus on moment-to-moment experiences and affect (i.e. process-experiential techniques) predicted subsequent reduction in misinterpretation of bodily sensations, while early high use of cognitive techniques predicted increase in misinterpretations.
Does the Working Alliance Predict Change in Misinterpretations of Bodily Sensations (BBSIQ) and PSRF, beyond Symptomatic Change?
Our results suggest that the quality of the therapeutic alliance, as perceived by the patient, has a different impact on the investigated predictors or candidate mechanisms of change in different treatments. When we accounted for prior change and symptomatic improvement across time and between-patient variability, we found that in PFPP improvement in alliance predicted improvement in PSRF, while in CBT improvement in alliance predicted worsening of PSRF. One potential explanation to this finding is that patients who develop a better alliance also trust their therapist and his/her treatment methods more than those who develop low alliance. Thus, when patients report high alliance they may also be more likely to absorb or internalize the therapist’s meaning system rather than alternative ones. Additionally, these patients are more likely to agree with their therapist on the tasks and goals of treatment (i.e., in PFPP – improving PSRF). Thus, it is possible that in PFPP, patients who demonstrate increases in the alliance were more likely to adopt an understanding of their symptoms within a dynamic framework, which is likely to generate higher PSRF scores, while patients receiving CBT adopted a CBT framework and showed improvement on more cognitive (rather than emotional-interpersonal) capacities.
Our findings also show that within-patient symptomatic improvement was predictive of subsequent decreases in within-patient misinterpretations, when accounting for prior change in symptoms and misinterpretations, as well as alliance levels within the model, with no evidence for reverse causation. Previous studies which did not control for between-level variability, have concluded that panic attacks are caused by misinterpretation of bodily sensations, with evidence showing that misinterpretations facilitate catastrophic thoughts, which in turn lead to increased panic symptoms (e.g. Arntz, 2002; Hoffart et al., 2008; Teachman et al., 2010). Meuret and colleagues’ (2010) showed in one of their analyses, that in a cognitive training condition, there was a bidirectional association between reduction in symptom misappraisal (i.e. a measure which included misinterpretations) and panic severity. Notably, Meuret et al.’s (2010) study is the only one which disentangled the between- and within- patient variability. It is possible that the use of this statistical approach enabled us to reveal a pattern that has not been identified in previous studies due to the impact of between-level variability (e.g., therapist effects, setting, or trait-level patient characteristics). Additionally, it is possible that controlling for the levels of alliance in our model significantly affected the direction of this result. From a conceptual perspective, our findings may suggest that when patients feel better and experience less panic, they are better able to verbalize and challenge their cognitive processes or to engage in more adaptive compensatory skills (Barber & DeRubeis, 1989) and thus demonstrate decreases in misinterpretations following symptomatic relief. It is important to note that the association between misinterpretations and symptoms was not included in our initial hypotheses and was not part of the aim of our study, although our model allowed us to test those paths. Thus, the reported finding should be considered exploratory as it was conducted post-hoc.
Does Use of Specific Techniques predict Change in Misinterpretations of Bodily Sensations (BBSIQ) and PSRF?
Our investigation of the effects of therapists’ actions on patient’s outcomes within two distinct treatments allow for greater generalizability and enable us to draw preliminary conclusions regarding the potential effects of use of specific interventions when delivered within a specific treatment package or by therapists who adhere to a specific orientation (psychodynamic or cognitive-behavioral). Specifically, in CBT, when therapists demonstrated greater focus on thoughts and cognitions early in treatment, patients showed an increase in misinterpretations of bodily sensations later on. However, when therapists focused on the patient’s affect and moment-to-moment experiences in session, patients showed a decrease in misinterpretations later in treatment. There are several possible explanations for these results. First, in our sample, when CBT therapists focused on the patient’s moment to moment experience, they often facilitated awareness of bodily sensations (e.g. “what are you feeling in your body right now?” “Does talking about X make you experience shortness of breath?”). Our findings suggest that encouraging the patient to become more aware of the ways in which he/she interprets bodily sensations as they happen in the session may prove to be therapeutic. Our results are in line with other studies which demonstrated the therapeutic benefits of therapists’ responsiveness and flexibility within a given treatment modality (Katz et al., 2019; Owen & Hilsenroth, 2014). For example, Castonguay, Goldfried, Wiser, Rau, and Hayes’ (1996) finding showing that higher levels of patient’s emotional experience in CBT for depression predicted a subsequent decrease in symptoms, suggesting that patients benefit from focus on affect within a CBT framework.
With regard to the negative relationship found between cognitive techniques and misinterpretations, it is possible that focusing on the patients’ cognitions early on was not beneficial. In a recent study, Meuret, Hofmann, and Rosenfield (2010) reported that patients with higher baseline levels of catastrophic cognitions were less likely to benefit from a purely cognitive treatment protocol compared to a breathing training treatment. They concluded that perhaps patients who are highly entrenched in their catastrophic cognitions do not benefit from therapists’ attempts to challenge the logic of these cognitions. Another explanation for our results could be that patients’ reports of increased misinterpretations may indicate that they actually become more aware of their own cognitive processes and are able to report on their cognitive distortions more accurately at mid-treatment.
Our findings suggest that in both treatments, focusing on patients’ interpersonal and social relationships and making connections between these relationships and panic symptoms predict subsequent improvement in patients’ PSRF capacity. It is important to note that there were significant differences in the delivery of an interpersonal focus in the two treatments: In keeping with their orientation, CBT therapists were more likely to identify patients’ behaviors in social and interpersonal relationships as potential triggers of panic and to offer alternative ways of coping with interpersonal conflicts. In contrast, PFPP therapists tended to investigate interpersonal patterns more broadly and to identify connections between the patient’s current symptoms and difficulties in long-lasting attachment relationships. When therapists showed a higher focus on the patients’ thoughts, behaviors, and actions, PSRF decreased, but, at least in CBT, when therapists focused on patients’ experiences in therapy and past events which may relate to panic symptoms (i.e., reviewing history of panic), PSRF capacity was more likely to improve. Conceptually, the capacity to reflect on one’s panic symptoms requires an awareness and understanding of the emotional and interpersonal experiences underlying panic (Busch et al., 2012). Thus, it is possible that when therapists discussed patients’ symptoms in the context of interpersonal experiences, patients were more likely to develop a richer understanding of the developmental origins of their panic, regardless of the treatment they received.
It is important to recognize several limitations of our study. First, we measured alliance using patient self-reports. While self-reports are widely used in most alliance studies, they include risks of biases (Zilcha-Mano, 2017). Additionally, given that we only measured alliance early in treatment, it is important to examine whether our findings will be replicated in other samples with measures of alliance at mid- and late-treatment. Second, our findings were obtained in the context of highly manualized short-term treatment protocols which were provided in a controlled experimental environment. Third, since we measured techniques only at week 1 and 5, we were unable to draw conclusions regarding the effects of techniques use at late phases of treatments. Additionally, we were unable to disentangle the within- from between-patient components for technique use. Thus, it is possible that between-level variability affected our results. Regarding therapist effects, average effects of therapists were included in the random intercepts at the between-patient level, so these are not a threat to our findings. However, it is possible that the effects we have found vary among therapists, in that some processes are more important in some therapists’ work than others. This could be tested by a random coefficient model, in which one or more regression paths are allowed to vary among therapists. Unfortunately, such a complex model was not estimable with our data (Muthén, & Muthén, personal communication, November 30, 2018). Thus, future studies with multiple data points over the course of treatment will be needed in order to investigate this issue. Fourth, while we took precautions when handling missing observations in our sample and confirmed that data was missing at random, our results should be viewed with caution given reported missing data. Fifth, while our coders were unaware of treatment conditions, given their clinical expertise, it is likely they may have guessed the treatment modality used. However, training focused on maintaining an objective and descriptive approach in order to produce data on techniques independent of treatment modality observed. Lastly, it is possible that non-significant findings in our study are due to low statistical power. Future studies might assess whether our results could be replicated in naturalistic settings and across a range of psychotherapies in diverse clinical populations and using more frequent assessments of predictors and alliance.
Conclusions and Clinical Implications
Our findings show that alliance produces differing patterns of changes in putative mechanisms in different treatments. Additionally, we have shown the importance of examining the effects of therapists’ actions on improvement in mechanisms of change. Our results suggest that focus on symptoms in the context of interpersonal relationships could lead to improvements in PSRF in both CBT and PFPP, even as therapists are adherent to their respective treatments. Additionally, early focus on patients’ affect and moment-to-moment experience could facilitate decreases in misinterpretation of bodily sensations. These findings could be translated into preliminary clinical recommendations. Given previous findings suggesting that improvement in misinterpretations and panic-specific reflective function predict subsequent symptomatic change, it may be especially beneficial to focus on patients’ interpersonal relationships throughout treatment to facilitate reflection on symptoms, as well as focus on patients’ affect and moment-to-moment experiences as they emerge in early sessions in order to increase accurate interpretation of panic symptoms. These techniques could facilitate therapeutic change even when conducted within distinct treatment modalities and maintaining adherence. Finally, it is possible that patients who develop a strong therapeutic alliance, may be more likely to show improvement in emotional/interpersonal skills which are targeted by the therapist and treatment provided.
Clinical and Methodological Significance Summary.
The findings show that patients who develop a stronger alliance early in treatment are likely to improve their capacity to reflect on their panic symptoms in brief panic-focused psychodynamic therapy (PFPP), but not in CBT for panic. Our results suggest that focusing on patients’ interpersonal and social relationships (but not on cognitions and behaviors) may be beneficial in facilitating capacity to reflect on symptoms within an interpersonal context (i.e. panic-specific reflective function). Additionally, in CBT, early focus on patients’ affect and moment to moment experiences, rather than high focus on cognitions, is most beneficial in reducing patients’ tendency to misinterpret their symptoms. Findings from our study highlight the importance of examining complex and nuanced longitudinal change processes using statistical models which allow to account for temporal precedence, reverse causation and disentangle within- and between-patient variation over time.
Acknowledgements:
We thank Louis Castonguay, J.Christopher Muran, Denise Hien, Nadia Kuprian, Mary Minges, and Zeynep Sahin for their continued support in this project and their thoughtful comments on earlier versions of the manuscript.
Footnotes
Number of missing observations: PDSS: wk1, n=18; wk5, n=33; wk9, n=50; wk10, n=37; WAI-C: wk1, n=63; wk3, n=67; wk 5, n=79. BBSIQ: wk1, n=11; wk5, n=75; wk10, n=49; PSRF: wk1, n=5; wk5, n=42; wk10, n=50
Analyses were conducted through a series of regression analyses using the lm function in R statistical software. We included the raw scores as well as the quadratic terms for use of techniques (Week 1 or 5) as predictors of the subsequent mechanism change (PSRF or BBSIQ; Week 5 or 12 respectively), while covarying residuals of the first measured time point of the mechanism (i.e. Week 1 or 5) regressed on the second measured time point (i.e. Week 5 or 12 respectively).
References
- Allen JG, Fonagy P, & Bateman AW (2008). Mentalizing in Clinical Practice. Washington, DC: American Psychiatric Publishing. [Google Scholar]
- Arnow BA, Steidtmann D, Blasey C, Manber R, Constantino MJ, Klein DN, … Kocsis JH (2013). The relationship between the therapeutic alliance and treatment outcome in two distinct psychotherapies for chronic depression. Journal of Consulting and Clinical Psychology, 81, 627–638. doi: 10.1037/a0031530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arntz A (2002). Cognitive therapy versus interoceptive exposure as treatment of panic disorder without agoraphobia. Behaviour Research and Therapy, 40, 325–341. doi: 10.1016/S0005-7967(01)00014-6 [DOI] [PubMed] [Google Scholar]
- Barber JP, & DeRubeis RJ (1989). On second thought: Where the action is in cognitive therapy for depression. Cognitive Therapy and Research, 13, 441–457. [Google Scholar]
- Barber JP, Gallop R, Crits-Christoph P, Barrett MS, Klostermann S, McCarthy KS, & Sharpless BA (2008). The role of the alliance and techniques in predicting outcome of supportive expressive dynamic therapy for cocaine dependence. Psychoanalytic Psychology, 25(3), 461–482. doi: 10.1037/0736-9735.25.3.461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barber JP, Gallop R, Crits-Christoph P, Frank A, Thase ME, Weiss RD, & Beth Connolly Gibbons M (2006). The role of therapist adherence, therapist competence, and alliance in predicting outcome of individual drug counseling: Results from the National Institute Drug Abuse Collaborative Cocaine Treatment Study. Psychotherapy Research, 16(02), 229–240. doi: 10.1080/10503300500288951 [DOI] [Google Scholar]
- Barber JP, Milrod B, Gallop R, Rudden MG, Solomonov N, McCarthy KS, & Chambless DL (2019). Mechanisms of change in psychotherapies for panic disorder: Results from the Cornell-Penn Study of psychotherapies for panic disorder. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barber JP, Muran JC, McCarthy KS, Keefe RJ (2013). Research on psychodynamic therapies In Lambert MJ (Ed.). Bergin and Garfield’s handbook of psychotherapy and behavior change (6th ed.) (pp. 443–494). New-York: John Wiley & Sons, Inc. [Google Scholar]
- Bateman AW, & Fonagy P (Eds.). (2012). Handbook of mentalizing in mental health practice. Washington, DC: American Psychiatric Publication. [Google Scholar]
- Beaujean AA (2012). BaylorEdPsych: R package for Baylor University educational psychology quantitative courses R package version 0.5. R foundation for statistical computing; Retrieved from http://CRAN.R-project.org/package=BaylorEdPsych. [Google Scholar]
- Bordin ES (1979). The generalizability of the psychoanalytic concept of the working alliance. Psychotherapy: Theory, Research & Practice, 16, 252–260. [Google Scholar]
- Busch FN, Singer MB, Milrod BL, Aronson AC (2012). Manual of panic focused psychodynamic psychotherapy: Extended range. New York: Taylor and Francis [Google Scholar]
- Casey LM, Oei TP, & Newcombe PA (2005). Looking beyond the negatives: A time period analysis of positive cognitions, negative cognitions, and working alliance in cognitive–behavior therapy for panic disorder. Psychotherapy Research, 15, 55–68. doi: 10.1080/10503300512331327038 [DOI] [Google Scholar]
- Castonguay LG, Constantino MJ, McAleavey AA, & Goldfried MR (2010). The alliance in cognitive-behavioral therapy In Muran JC & Barber JP (Eds.), The therapeutic alliance: An evidence based guide to practice (pp. 150–171). New York: Guilford Press. [Google Scholar]
- Castonguay LG, Goldfried MR, Wiser S, Raue PJ, & Hayes AM (1996). Predicting the effect of cognitive therapy for depression: a study of unique and common factors. Journal of Consulting and Clinical Psychology, 64, 497–504. doi: 10.1037/0022-006X.64.3.497 [DOI] [PubMed] [Google Scholar]
- Clark DM (1986). A cognitive approach to panic. Behaviour Research and Therapy, 24, 461–470. doi: 10.1016/0005-7967(86)90011-2 [DOI] [PubMed] [Google Scholar]
- Clark DM, Salkovskis PM, Hackmann A, Middleton H, Anastasiades P, & Gelder M (1994). A comparison of cognitive therapy, applied relaxation and imipramine in the treatment of panic disorder. The British Journal of Psychiatry, 164, 759–769. doi: 10.1192/bjp.164.6.759 [DOI] [PubMed] [Google Scholar]
- Clark DM, Salkovskis PM, Ost LG, Breitholtz E, Koehler KA, Westling BE,…Gelder M (1997). Misinterpretation of body sensations in panic disorder. Journal of Consulting and Clinical Psychology, 65, 203–213. [DOI] [PubMed] [Google Scholar]
- Clark DM, Salkovskis PM, Hackmann A, Wells A, Ludgate J, & Gelder M (1999). Brief cognitive therapy for panic disorder: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 67, 583–589. doi: 10.1037/0022-006X.67.4.583 [DOI] [PubMed] [Google Scholar]
- Craske MG, Barlow DH, & Meadows EA (2000). Mastery of your anxiety and panic: Therapist guide for anxiety, panic, and agoraphobia. New York, NY: Oxford University Press. [Google Scholar]
- Crits-Christoph P, & Mintz J (1991). Implications of therapist effects for the design and analysis of comparative studies of psychotherapies. Journal of Consulting and Clinical Psychology, 59, 20–26. doi: 10.1037/0022-006X.59.1.20 [DOI] [PubMed] [Google Scholar]
- DeRubeis RJ, Brotman MA, & Gibbons CJ (2005). A conceptual and methodological analysis of the nonspecifics argument. Clinical Psychology: Science and Practice, 12, 174–183. doi: 10.1093/clipsy.bpi022 [DOI] [Google Scholar]
- DiNardo PA, Brown TA, & Barlow DH (1995). Anxiety Disorder Interview Schedule for DSM-IV: Lifetime version (ADIS-IV-L). New York, NY: Graywinds. [Google Scholar]
- Ekeblad A, Falkenström F, & Holmqvist R (2016). Reflective functioning as predictor of working alliance and outcome in the treatment of depression. Journal of Consulting and Clinical psychology, 84, 738–751. doi: 10.1037/ccp0000119 [DOI] [PubMed] [Google Scholar]
- Falkenström F, Finkel S, Sandell R, Rubel JA, & Holmqvist R (2017). Dynamic models of individual change in psychotherapy process research. Journal of Consulting and Clinical Psychology, 85, 537–549. doi: 10.1037/ccp0000203 [DOI] [PubMed] [Google Scholar]
- Falkenström F, Granström F, & Holmqvist R (2014). Working alliance predicts psychotherapy outcome even while controlling for prior symptom improvement. Psychotherapy Research, 24, 146–159. doi: 10.1080/10503307.2013.847985 [DOI] [PubMed] [Google Scholar]
- Falkenström F, Kuria M, Othieno C, & Kumar M (2018). Working alliance predicts symptomatic improvement in public hospital–delivered psychotherapy in Nairobi, Kenya. Journal of Consulting and Clinical Psychology. Advance online publication. doi: 10.1037/ccp0000363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fentz HN, Hoffart A, Jensen MB, Arendt M, O’Toole MS, Rosenberg NK, & Hougaard E (2013). Mechanisms of change in cognitive behaviour therapy for panic disorder: The role of panic self-efficacy and catastrophic misinterpretations. Behaviour Research and Therapy, 51, 579–587. doi: 10.1016/j.brat.2013.06.002 [DOI] [PubMed] [Google Scholar]
- Flückiger C, Del Re AC, Wampold BE, & Horvath AO (2018). The alliance in adult psychotherapy: A meta-analytic synthesis. Psychotherapy, 5(4), 316–340. doi: 10.1037/pst0000172 [DOI] [PubMed] [Google Scholar]
- Fonagy P, Gergely G, Jurist E, & Target M (2002). Affect regulation, mentalization and the development of the Self. New York: Other Press. [Google Scholar]
- Gibbons MB, Crits-Christoph P, Barber JP, Stirman SW, Gallop R, Goldstein LA, … Ring-Kurtz S (2009). Unique and common mechanisms of change across cognitive and dynamic psychotherapies. Journal of Consulting and Clinical Psychology, 77, 801–813. doi: 10.1037/a0016596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldfried MR, & Davila J (2005). The role of relationship and technique in therapeutic change. Psychotherapy: Theory, Research, Practice, Training, 42, 421–430. doi: 10.1037/0033-3204.42.4.421 [DOI] [Google Scholar]
- Gibbons MBC, Crits-Christoph P, Barber JP, Stirman SW, Gallop R, Goldstein LA, & Ring-Kurtz S (2009). Unique and common mechanisms of change across cognitive and dynamic psychotherapies. Journal of Consulting and Clinical Psychology, 77, 801–813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamaker EL, Kuiper RM, & Grasman RP (2015). A critique of the cross-lagged panel model. Psychological Methods, 20, 102–116. doi: 10.1037/a0038889 [DOI] [PubMed] [Google Scholar]
- Hoffart A, Sexton H, Hedley LM, & Martinsen EW (2008). Mechanisms of change in cognitive therapy for panic disorder with agoraphobia. Journal of Behavior Therapy and Experimental Psychiatry, 39, 262–275. doi: 10.1016/j.jbtep.2007.07.006 [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Suvak MK, Barlow DH, Shear MK, Meuret AE, Rosenfield D, … Woods SW (2007). Preliminary evidence for cognitive mediation during cognitive–behavioral therapy of panic disorder. Journal of Consulting and Clinical Psychology, 75, 374–379. doi: 10.1037/0022-006X.75.3.374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz M, Hilsenroth MJ, Gold JR, Moore M, Pitman SR, Levy SR, & Owen J (2019). Adherence, flexibility, and outcome in psychodynamic treatment of depression. Journal of Counseling Psychology, 66(1), 94–103. doi: 10.1037/cou0000299 [DOI] [PubMed] [Google Scholar]
- Kazdin AE (2007). Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology, 3, 1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432 [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, & Agras WS (2002). Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry, 59, 877–883. doi: 10.1001/archpsyc.59.10.877 [DOI] [PubMed] [Google Scholar]
- McCarthy KS, & Barber JP (2009). The multitheoretical list of therapeutic interventions (MULTI): Initial report. Psychotherapy Research, 19, 96–113. doi: 0.1080/10503300802524343 [DOI] [PubMed] [Google Scholar]
- McCarthy KS, Keefe JR, & Barber JP (2016). Goldilocks on the couch: Moderate levels of psychodynamic and process-experiential technique predict outcome in psychodynamic therapy. Psychotherapy Research, 26, 307–317. doi: 10.1080/10503307.2014.973921 [DOI] [PubMed] [Google Scholar]
- Meuret AE, Hofmann SG, & Rosenfield D (2010). Catastrophic appraisal and perceived control as moderators of treatment response in panic disorder. International Journal of Cognitive Therapy, 3, 262–277. doi: 10.1521/ijct.2010.3.3.262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meuret AE, Rosenfield D, Seidel A, Bhaskara L, & Hofmann SG (2010). Respiratory and cognitive mediators of treatment change in panic disorder: evidence for intervention specificity. Journal of Consulting and Clinical Psychology, 78, 691–704. doi: 10.1037/a0019552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milrod B, Busch F, Cooper A, & Shapiro T (1997). Manual of panic-focused psychodynamic psychotherapy. Washington, DC: APA Press. [Google Scholar]
- Milrod B, Chambless DL, Gallop R, Busch FN, Schwalberg M, McCarthy KS, … & Barber JP (2016). Psychotherapies for panic disorder: a tale of two sites. The Journal of Clinical Psychiatry, 77, 927–935. doi: 10.4088/JCP.14m09507 [DOI] [PubMed] [Google Scholar]
- Moerbeek M (2004). The consequence of ignoring a level of nesting in Multilevel Analysis. Multivariate Behavioral Research, 39, 129–149. doi: 10.1207/s15327906mbr3901_5 [DOI] [PubMed] [Google Scholar]
- Muthén LK and Muthén BO (1998-2012). Mplus User’s Guide (7th Ed.). Los Angeles, CA: Muthén & Muthén [Google Scholar]
- Owen J, & Hilsenroth MJ (2014). Treatment adherence: The importance of therapist flexibility in relation to therapy outcomes. Journal of Counseling Psychology, 61(2), 280–288. doi: 10.1037/a0035753 [DOI] [PubMed] [Google Scholar]
- Rudden MG, Milrod B, Meehan KB, Falkenstrom F (2009). Symptom-specific reflective functioning: incorporating psychoanalytic measures into clinical trials. Journal of American Psychoanalytic Association, 57, 1473–1478. doi: 10.1177/00030651090570060804 [DOI] [PubMed] [Google Scholar]
- Rudden M, Milrod B, Target M, Ackerman S, & Graf E (2006). Reflective functioning in panic disorder patients: A pilot study. Journal of the American Psychoanalytic Association, 54, 1339–1343. doi: 10.1177/00030651060540040109 [DOI] [PubMed] [Google Scholar]
- Shear MK, Brown TA, Barlow DH, Money R, Sholomskas DE, Woods SW, … & Papp LA (1997). Multicenter collaborative panic disorder severity scale. American Journal of Psychiatry, 154, 1571–1575. doi: 10.1176/ajp.154.11.1571 [DOI] [PubMed] [Google Scholar]
- Shrout PE, & Fleiss JL (1979). Intraclass correlations: Uses in assessing rater reliability. Psychological Bulletin, 86(2), 420–428. doi: 10.1037/0033-2909.86.2.420 [DOI] [PubMed] [Google Scholar]
- Smits JA, Powers MB, Cho Y, & Telch MJ (2004). Mechanism of change in cognitive-behavioral treatment of panic disorder: evidence for the fear of fear mediational hypothesis. Journal of Consulting and Clinical Psychology, 72, 646–652. doi: 10.1037/0022-006X.72.4.646 [DOI] [PubMed] [Google Scholar]
- Teachman BA, Marker CD, & Clerkin EM (2010). Catastrophic misinterpretations as a predictor of symptom change during treatment for panic disorder. Journal of Consulting and Clinical Psychology, 78, 964–973. doi: 10.1037/a0021067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tracey TJ, & Kokotovic AM (1989). Factor structure of the working alliance inventory. Psychological Assessment: A Journal of Consulting and Clinical psychology, 1, 207–210. doi: 10.1037/1040-3590.1.3.207 [DOI] [Google Scholar]
- Wampold BE (2001). The great psychotherapy debate: Models, methods and findings. Mahwah, NJ: Lawrence Erlbaum. [Google Scholar]
- Zilcha-Mano S, Dinger U, McCarthy KS, & Barber JP (2014). Does alliance predict symptoms throughout treatment, or is it the other way around? Journal of Consulting and Clinical Psychology, 82, 931–935. doi: 10.1037/a0035141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zilcha-Mano S (2017). Is the alliance really therapeutic? Revisiting this question in light of recent methodological advances. American Psychologist, 72, 3–11. doi: 10.1037/a0040435 [DOI] [PubMed] [Google Scholar]