Abstract
Background. Diabetes mellitus type 1 (DM1) is associated with high risk for cardiovascular disease and early detection of myocardial dysfunction is very important for the prevention of cardiac complications. Although the functionality of right ventricule is important in a lot of disease affecting long time prognosis and progression, in diabetic type 1 patients has not been studied in depth yet. Objectives. To evaluate the right ventricular function by using both conventional echocardiography as well as speckle tracking echocardiography (STE) in young adults with diabetes mellitus type 1. Methods. We included 60 young asymptomatic adults diagnosed with diabetes mellitus type 1 (mean interval from diagnosis 9±6 years) and 90 healthy controls. Conventional and STE Echocardiography was acquired using the GE Vivid S60 equipment. The longitudinal right ventricular strain 6 segments (RV GLS global) and 3 segments (RVFW GLS) of right ventricle (RV GLSbazal, RV GLSmid, RV GLSapex) as well were obtained using the EchoPAC BT13 workstation. Results. No significant intergroup differences in EF were noted. Conventional echocardiographic parameters revealed lower tricuspid annular velocities Et, At and Et/At ratio compared to controls suggesting a diastolic disfunction in diabetes group. RV speckle tracking strain measurements showed no significant difference between the groups. Conclusions. Young adults with type 1 diabetes mellitus and without known heart disease have diastolic right ventricular dysfunction. The subclinical myocardial systolic function is preserved in early stages.
Keywords: Diabetes mellitus, right ventricular dysfunction, speckle tracking, diabetic cardiomiopathy
Introduction
Diabetes Mellitus (DM) is one of the most important cardiovascular risk factor and its incidence has reached epidemiological odds [1,2,3,4,5,6].
In 2017 the International Diabetes Federation has registered a number of 451 million cases and expects, until 2045, the number of diabetes cases will reach 493 million [7,8].
Diabetes may lead to diabetic cardiomiopathy (DCM).
The possibility of DCM as an independent disease was first confirmed in 1972 by Rubler et all, [9,10] through postmortem pathological findings in 4 diabetic patients with HF symptoms.
He defined it as a myocardial dysfunction in patients without hypertension or coronary artery disease (CAD).
DCM is characterized by a long asymptomatic latent period during which is associated with metabolic disturbances and structural abnormalities.
Initially, DCM triggers are LV hypertrophy and remodeling, myocardial fibrosis and diastolic dysfunction which may lead to clinical signs of HF with normal ejection fraction (EF). In later stages, due to the progression of DCM, appear clinical HF and reduced EF [9,10].
Detection of diabetic heart disease in the earliest stages has an important role, because timely changes in lifestyle and even medical interventions may delay the appearance of heart failure.
Previous studies were based on the evaluation of diastolic and systolic left ventricle (LV) function in diabetic patients at the cost of ignoring the right ventricle which has an important role in progression and prognosis of patients with DCM [9,10].
The existing literature contain a few number of studies on the RV cardiomyopathies in patients with type 1 and we can affirm that the RV performance is surely an important issue that should be investigated in this type of patients [11].
The aim of the study was to investigate, by using both conventional and 2D-Speckle Tracking (2D-STE) echocardiography, differences in right ventricular function in diabetic type 1 vs. healthy subjects and correlate with the duration of the disease.
Study Patients, Materials and Methods
Patients
Our study was conducted in the Cardiology Department of Emergency County Hospital Craiova between June 2017-June 2018.
60 patients with type 1 diabetes mellitus were enrolled (40-males, 20-females: with mean age 25±6 years).
The selection criteria were age <40 years, a good image quality that allowed the recording of standard echocardiographic and speckle tracking measurements and the presence of cardiac sinus rhythm.
Exclusion criteria included: presence of moderate-to-severe valvulopathies, signs and symptoms of coronary artery disease and/or significant rhythm disturbances.
We also enrolled 90 healthy subjects (59-males and 31-females: mean age 30±8 years) from our database for normal subjects.
Healthy subjects were selected from hospital employee or relatives, students and/or friends.
The study was performed according to the tenets of the Declaration of Helsinki.
The protocol was approved by the Hospital Ethics Committee.
The informed consent was signed by every subject prior to the study procedures.
Echocardiography
Echocardiography was done with the subject positioned in the left lateral decubitus, using a available ultrasound equipment (Vivid S6, GE Vingmed Ultrasound, with a 3.5 MHz transducer).
All examinations were performed by one physician to minimize interobserver variability.
All parameters were taken according to ASE-American Society of Echocardiography standards and recommendations of the ESC-European Association of Cardiovascular Imaging.
For image acquisition, it were taken 3-cardiac cycles in each incidence with the patient holding his breath.
All images were stored in a special system for echocardiographic analysis named ECHO-PAC, GE version 110.
Assessment of the right ventricle
Conventional measurements of RV
2D echocardiography was used for conventional measurements of:
TAPSE-tricuspid plane systolic excursion calculated by the echocardiograph as the difference between end-diastolic and end-systolic excursion of tricuspid annulus;
RV fractional area change (FAC) another important parameter for evaluation o systolic function was calculated as the difference between diastolic-systolic RV area divided by RV end-diastolic area.
These two measurements were obtained in four chamber view (4-CH).
We used pulsed wave Doppler (PW) for tricuspid inflow.
Peak early diastolic filling velocity (Et) and peak late diastolic filling velocity (At) were measured and ratio (E/A ratio) was also calculated.
2D-Speckle tracking echocardiographic assessment of RV (2D-STE)
For RV speckle tracking analysis we acquired images of the apical 4CH-‘view modified for RV with a 3 cycle-ECG recording. We used a strain software package available for LV to measure the RV longitudinal strain.
We manually traced, in apical 4CH, at the end-systole, the endocardial surface of the septum and free wall view of right ventricle using a speckle-tracking software.
The software automatically generated an epicardial surface tracing of all the markers (“speckles”) in the RV myocardial wall.
Myocardial right ventricle strain results by the change in position of ’’speckles’’.
We obtained the peak systolic longitudinal strain as the average of the peak systolic values of the 6 segments (3 segments of the RV free wall and 3 segments of the interventricular septum).
The RV free wall strain derived from free wall tracking (3 segments only).
Statistical analysis
For the statistical analyses, we used version 17.0 of SPSS software for Windows (SPSS Inc., Chicago, IL).
All the clinical and echocardiographic data were expressed as Mean±SD or absolute number or percentages for categorical variables.
P value under 0.05 was considered significant.
Results
Clinical characteristics
We showed the clinical characteristics of study population is shown in the Table 1.
Table 1.
Study population clinical characteristics
|
Variable |
Diabetic patients (n=60) |
Controls (n=90) |
p value |
|
Gender (female/male) |
20/40 |
31/59 |
<0.05 |
|
Age (years) |
25±6 |
30±8 |
- |
|
Diabetes duration (years) |
9.7±6.3 (2- 27) |
N/A |
- |
|
BMI-Body mass index (kg/m2) |
27±6 |
23±4 |
<0.001 |
|
BSA-Body surface area (m2) |
1.9±0.2 |
1.8±0.2 |
<0.001 |
|
HR (beats/min) |
80±10 |
81±14 |
NS |
|
Systolic BP (mmHg) |
126±14 |
117.2±7.5 |
<0.001 |
|
Diastolic BP (mmHg) |
80± 7.8 |
68±5.4 |
<0.001 |
|
Glycated hemoglobin (%) |
8.1±1.8 |
N/A |
<0.001 |
We observed that mean diabetes duration is 9.7±6 (2-27 years) and mean glycozilated hemoglobin is 8.1±1.8. Patients with DM type 1 have higher systolic BP and diastolic BP, higher BMI and BSA compared control group.
No significant differences between the two groups regarding heart rythm were detected.
In the two groups, the number of male patients was higher than the females and the age was smaller in diabetic study population.
Conventional and tissue Doppler echocardiography
All participants had normal ejection fraction. Conventional echocardiographic parameters revealed lower tricuspid annular velocities Et, At and Et/At ratio compared to controls suggesting a diastolic disfunction in diabetes group. Echocardiographic parameters for evaluation of RV systolic disfunction (TAPSE; FAC; S’t TDI) did not registered any statistical differences. TAPSE was slightly lower in diabetic group.
Standard echocardiographic parameters are summarized in Table 2.
Table 2.
Conventional and Speckle tracking echocardiografic mesurements of RV
|
Variable |
Diabetic patients (n=60) |
Controls (n=90) |
p value |
|
EF(%) |
60.2±7.3 |
58.3±4.3 |
NS |
|
TAPSE (cm) |
19±3.2 |
22.2±3.5 |
NS |
|
FAC (%) |
45.3± 6.3 |
46.4±6.4 |
NS |
|
Et (cm/s) |
13.2 ±2.9 |
15.2±3.7 |
<0.05 |
|
At (cm/s) |
13.45± 4.3 |
10.9±3.5 |
<0.05 |
|
Et deceleration time (ms) |
132.6±4.7 |
132.2±4.4 |
NS |
|
Et/At |
0.9 ±1 |
1.3±1.1 |
<0.05 |
|
S’t (cm/s) |
13.2± 2.2 |
13.4±2.5 |
NS |
|
GLS RV global (%) |
-22 4±0.5 |
-22.9±3.3 |
NS |
|
GLS RV FW (%) |
-26.4± 4.3 |
-27.5± 3.9 |
NS |
|
GLS RV bazal (%) |
-25.5 ±4.9 |
-26.5± 5.5 |
NS |
|
GLS RV mid (%) |
-28.7± 4.6 |
-29.4± 4.8 |
NS |
|
GLS RV apex (%) |
-25.3± 6.03 |
-27.2± 5.5 |
NS |
Speckle tracking echocardiography
The data on the speckle tracking deformation indices of the two study groups are demonstrated in Table 2.
According to our study, the values of the RV basal segment GLS and RV apical segment GLS (GLS RV bazal; GLS RV apex) in diabetic group were slightly lower than controls. However, no significant differences regarding to the speckle tracking RV segmetar longitudinal strain between the two groups was obtained.
We also analyzed RV GLS derived from 6 segments (3 IVS segments of the plus RV free wall 3 segments) and RV free wall strain derived from free wall tracking (3 segments only).
No significant differences between groups.
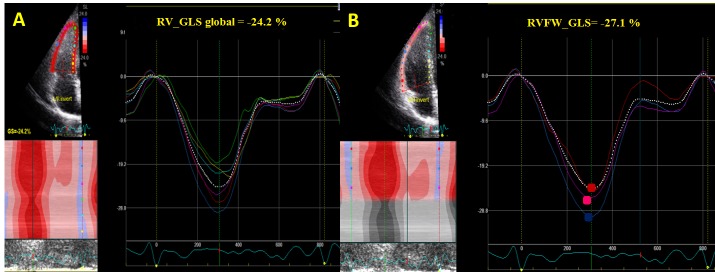
Figure 1.
4-Chamber view (4CH). Strain RV measurements
RV_GLS global : The endocardium was traced and the computer automatically included the strain values of the IVS (basal-red, mid-blue; apex- purple) and RV FW strain (basal-yellow, mid-light blue and apex, green).
RVFW_GLS: We used the same tracking set from RV_GLS-4C. We obtain the average of 3 segments of the free right ventricular wall: max peak longitudinal strain of basal segment (red), mid-wall segment (blue), and apical (purple).
Discussion
Based on conventional PW transtricuspid flow measurements, Et and At-waves velocities were statistical lower in the diabetic type 1 group (P<0.05).
There are contradictory results in literature regarding the Et wave. Our results are in concordance with some studies [12,13] whereas differ from others studies [14].
The present study also found that velocity of the late tricuspid A-wave was lower in the diabetic group control. Most of the studies had found similar results [13,15,16] but others have not reported this difference.
Based on this results, the parameters for RV dyastolic function measured by conventional Doppler were statistical significant in patients with diabetes type 1 compared with healthy subjects.
The results obtained confirms previous few reports found in literature who described RV diastolic dysfunction in patients with type 1 diabetes [17].
In our study we could not demonstrate RV systolic disfunction either by conventional parameters or by speckle tracking.
We are in agreement with the data from literature but in disagreement with others.
In a study by Karamitsos et al., [13] diabetic patients were found to have an impaired RV diastolic with a preserved RV systolic function. Jerdrzejewska et all find right ventricular diastolic and systolic dysfunction at conventional and speckle tracking echocardiographic evaluation [3].
We did not found a correlation between the RV diastolic dysfunction, duration of diabetes mellitus and HbA1c.
The present study is in agreement with some other similar studies [3,18,19].
This results could suggest that controlling diabetes mellitus is more important than its duration [20].
Conclusions
In conclusion, diastolic function may be impaired before the development of myocardial systolic dysfunction in Type1 DM.
If these right ventricular dyastolic abnormalities have an implication in clinical course and prognosis of diabetes mellitus remains to be investigated.
We consider that serial echocardiographic measurements follow up are warranted to evaluate which parameters are the most feasible to evaluate progression from right ventricular subclinical involvement to the right ventricular dysfunction.
List of Abbreviations
DCM=Diabetic Cardiomiopathy
DM1=Type 1 Diabetes Mellitus
FW=Free wall
GLS=Global longitudinal strain
LV=Left Ventricle
RV=Right ventricle
STE=Speckle Tracking Echocardiography
References
- 1.Lee WS, Kim J. Diabetic cardiomyopathy: Where we are and where we are going. Korean J Intern Med. 2017;32(3):404–421. doi: 10.3904/kjim.2016.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Poornima IG, Parikh P, Shannon RP. Diabetic cardiomyopathy: The search for a unifying hypothesis. Circ Res. 2006;98(5):596–605. doi: 10.1161/01.RES.0000207406.94146.c2. [DOI] [PubMed] [Google Scholar]
- 3.Jȩdrzejewska I, Król W, Światowiec A, Wilczewska A, Grzywanowska-Łaniewska I, Dłuzniewski M, Braksator W. Left and right ventricular systolic function impairment in type 1 diabetic young adults assessed by 2D speckle tracking echocardiography. Eur Heart J Cardiovasc Imaging. 2016;17(4):438–446. doi: 10.1093/ehjci/jev164. [DOI] [PubMed] [Google Scholar]
- 4.Tamayo T, Rosenbauer J, Wild SH, Spijkerman AMW, Baan C, Forouhi NG, Herder C, Rathmann W. Diabetes in Europe: An update. Diabetes Res Clin Pract. 2014;103(2):206–217. doi: 10.1016/j.diabres.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 5.Xiao M, O’Neill C. Detection and Management of Diabetes in England: Results from the Health Survey for England. Diabetes Ther. 2017;8(5):1163–1174. doi: 10.1007/s13300-017-0300-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rönnback M, Fagerudd J, Forsblom C, Pettersson-Fernholm K, Reunanen A, Groop PH. Altered age-related blood pressure pattern in type 1 diabetes. Circulation. 2004;110(9):1076–1082. doi: 10.1161/01.CIR.0000139903.29522.8D. [DOI] [PubMed] [Google Scholar]
- 7.Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, Ohlrogge AW, Malanda B. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–281. doi: 10.1016/j.diabres.2018.02.023. [DOI] [PubMed] [Google Scholar]
- 8.Ogurtsova K, da Rocha Fernandes JD, Huang Y, Linnenkamp U, Guariguata L, Cho NH, Cavan D, Shaw JE, Makaroff LE. IDF Diabetes Atlas: Global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract. 2017;128:40–50. doi: 10.1016/j.diabres.2017.03.024. [DOI] [PubMed] [Google Scholar]
- 9.Tarquini R, Lazzeri C, Pala L, Rotella CM, Gensini GF. The diabetic cardiomyopathy. Acta Diabetol. 2011;48(3):173–81. doi: 10.1007/s00592-010-0180-x. [DOI] [PubMed] [Google Scholar]
- 10.Lee MMY, McMurray JJV, Lorenzo-Almorós A, Kristensen SL, Sattar N, Jhund PS, Petrie MC. Diabetic cardiomyopathy. Heart. 2019;105(4):337–345. doi: 10.1136/heartjnl-2016-310342. [DOI] [PubMed] [Google Scholar]
- 11.Konduracka E, Gackowski A, Rostoff P, Galicka-Latala D, Frasik W, Piwowarska W. Diabetesspecific cardiomyopathy in type 1 diabetes mellitus: No evidence for its occurrence in the era of intensive insulin therapy. Eur Heart J. 2007;28(20):2465–2471. doi: 10.1093/eurheartj/ehm361. [DOI] [PubMed] [Google Scholar]
- 12.Ahmed TA, Ahmed YA, Arafa AI, Salah RA. Detection of occult right ventricular dysfunction in young Egyptians with type 1 diabetes mellitus by two-dimensional speckle tracking echocardiography. Indian Heart J. 2018;70(5):665–671. doi: 10.1016/j.ihj.2018.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Song ZZ, Ma J. Early diastolic impairment of diabetic heart: The significance of right ventricle. Int J Cardiol. 2008;126(1):120–121. doi: 10.1016/j.ijcard.2007.01.062. [DOI] [PubMed] [Google Scholar]
- 14.M Abd-El Aziz F, Abdelghaffar S, Hussien EM, Fattouh AM. Evaluation of cardiac functions in children and adolescents with type 1 diabetes. J Cardiovasc Ultrasound. 2017;25(1):12–19. doi: 10.4250/jcu.2017.25.1.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Malik V, Subramaniam A, Kapoor P. Strain and strain rate: An emerging technology in the perioperative period. Ann Card Anaesth. 2016;19(1):112–112. doi: 10.4103/0971-9784.173026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Buckberg G, Hoffman JIE. Right ventricular architecture responsible for mechanical performance: Unifying role of ventricular septum. J Thorac Cardiovasc Surg. 2014;148(6):31663171e4–31663171e4. doi: 10.1016/j.jtcvs.2014.05.044. [DOI] [PubMed] [Google Scholar]
- 17.Tadic M, Pieske-Kraigher E, Cuspidi C, Morris DA, Burkhardt F, Baudisch A, Haßfeld S, Tschöpe C, Pieske B. Right ventricular strain in heart failure: Clinical perspective. Arch Cardiovasc Dis. 2017;110(10):562–571. doi: 10.1016/j.acvd.2017.05.002. [DOI] [PubMed] [Google Scholar]
- 18.Movahed MR, Milne N. Presence of biventricular dysfunction in patients with type II diabetes mellitus. Congest Heart Fail. 2007;13(2):78–80. doi: 10.1111/j.1527-5299.2007.888138.x. [DOI] [PubMed] [Google Scholar]
- 19.Kang Y, Wang S, Huang J, Cai L, Keller BB. Right ventricular dysfunction and remodeling in diabetic cardiomyopathy. Am J Physiol Circ Physiol. 2018;316(1):H113–H122. doi: 10.1152/ajpheart.00440.2018. [DOI] [PubMed] [Google Scholar]
- 20.Hekimsoy V, Kaya EB, Akdogan A, Sahiner L, Evranos B, Canpolat U, Aytemir K, Özer N, Tokgozoglu L. Echocardiographic assessment of regional right ventricular systolic function using two-dimensional strain echocardiography and evaluation of the predictive ability of longitudinal 2D-strain imaging for pulmonary arterial hypertension in systemic sclerosis. Int J Cardiovasc Imaging. 2018;34(6):883–892. doi: 10.1007/s10554-018-1299-z. [DOI] [PubMed] [Google Scholar]