Abstract
Introduction: Psoriatic arthritis (PsA) is an inflammatory arthritis, usually involving peripheral joints, associated with cutaneous psoriasis, in the absence of rheumatoid factor and anti-citrullinated protein antibodies. Material and methods: The study included 28 patients diagnosed with psoriatic arthritis according to CASPAR criteria, presenting pain or swelling of the small joints of the hands and wrists, hospitalized in the Department of Rheumatology of the Emergency Clinical County Hospital of Craiova during 2016-2018. Results: In the 28 patients, a total of 840 joints were examined clinically and by ultrasound. From the clinical point of view, out of the total, 32 joints were swollen while 59 joints were tender. Dactylitis was evidenced in 20/280 examined digits upon physical examination. MUS revealed the presence of synovial proliferation in 108/840 sites (12.85%), with grade 1 synovitis in 4 joints (3.7%), grade 2 in 94 joints (87.03%) and grade 3 in 10 joints (9.25%). Out of 280 examined fingers 5.71% presented dactylitis, the third digit being the most commonly targeted. Grade 2 tenosynovitis was found in 40 of the examined tendons, whereas 8 tendons presented with grade 3 tenosynovitis. The most frequently involved were the flexor tendons of the digits (38 out of 40 tendons with inflammatory changes), followed by the extensor carpi ulnaris and flexor carpi radialis tendons. Conclusions: Ultrasound has proven its utility in assessing joint and tendon inflammation to a higher extent that clinically expected. Thus, MUS examination of hand joints may aid the clinician in diagnosing PsA, in evaluating the prognosis and the course of treatment.
Keywords: Psoriatic arthritis, synovitis, tenosynovitis, dactylitis
Introduction
Psoriatic arthritis (PsA) is an inflammatory arthritis, usually involving peripheral joints, associated with cutaneous psoriasis, in the absence of rheumatoid factor and anti-citrullinated protein antibodies.
Classic description of PsA comprises 5 forms: symmetrical polyarthritis, asymmetrical oligoarthritis, distal interphalangeal joint involvement, spondylitis and arthritis mutilans.
In the past years, the spectrum of PsA has extended in order to include extra-articular manifestations such as tenosynovitis, tendinitis, dactylitis and enthesitis, but also nail, eye, intestinal and cardiac involvement [1].
The frequency of distribution of clinical patterns in PsA is variable, mainly because patterns change over time, oligoarticular disease being able evolve to polyarticular involvement.
A tendency to asymmetry has been described due to the fact that all joints of the same digit tend to be affected more frequently rather than the same joints on both sides, in contrast with rheumatoid arthritis [2].
Dactylitis, of particular interest in PsA, is a form of enthesitis described as sausage-like swelling of a digit with a still debated definition, in terms of ultrasound description comprising synovitis, flexor tendon tenosynovitis, subcutaneous tissue edema and even bone edema visualised on magnetic resonance imaging (MRI), more frequently associated with oliagoarticular, erosive arthritis and DIP joint involvement.
In terms of classification, PsA is considered to be part of the spondyloarthropaties group due to the presence of spinal involvement.
Differential diagnosis between PsA and other spondyloarthritis is based on the pattern of peripheral arthritis and the asymmetrical distribution of the axial manifestations including both sacroiliitis and syndesmophytes [3].
In 70-80% of patients, cutaneous lesions appear before joint pain and arthritis, in 20-30% of cases the articular manifestations precede the skin lesions, while approximately 10% of patients experience both skin and joint involvement at the same time [4].
PsA occurs in variable percentages ranging from 10-30% in patients with psoriasis, depending on the studied population [5].
Musculoskeletal ultrasound (MUS) is an inexpensive, non-invasive and accessible diagnostic method in patients with inflammatory pathologies.
Apparently normal joints upon clinical examination may present synovial hypertrophy or power Doppler signal using MUS examination, thus proving the utility of MUS in identifying more affected joints.
Beside the ability to identify structural inflammatory lesions of the bony cortex, joints and periarticular structures such as erosions, synovitis, tenosynovitis, the technique is suitable for a dynamic, multiplanar evaluation of treatment response as well as guidance of therapeutic maneuvers [6].
Material and Methods
The study included 28 patients diagnosed with psoriatic arthritis according to CASPAR criteria, presenting pain or swelling of the small joints of the hands and wrists, hospitalized in the Department of Rheumatology of the Emergency Clinical County Hospital of Craiova during 2016-2018. All patients expressed their informed consent to be a part of this study.
Upon admission detailed disease history was taken and complete clinical examination to assess joint tenderness or swelling was performed. Laboratory tests including erythrocyte sedimentation rate (ESR), C reactive protein (CRP), complete blood count, serum creatinine and liver enzymes were determined in order to evaluate the health state of the patients.
MUS examinations were performed using a MyLab25™Gold US system with a multi-frequency linear array probe of 6-18MHz.
High frequencies >12MHz were used to evaluate hand joints. Grey-scale and power Doppler scans in both longitudinal and transverse planes were used to assess the presence of synovial proliferation, tenosynovitis, erosions and bone proliferations.
A number of 30 joints were examined: wrists, metacarpophalangeal (MCP), proximal interphalangeal (PIP) and distal interphalangeal (DIP) joints.
Flexor and extensor tendons of the hand and wrist were also included in the ultrasound evaluation.
Disease activity was monitored by calculating disease activity in psoriatic arthritis (DAPSA), taking into consideration the swollen and tender joint count, patient pain expressed using the visual analogue scale (VAS), patient global assessment and CRP levels with a value of <5mg/L considered normal.
Results
Twenty eight patients (20 females and 8 males) were enrolled in the study with mean age of 52.5 (±10.68 years).
Two patients had family history of psoriasis and all of them current or past personal history of psoriasis.
The study group included polyarticular disease (60.71%), oligoarticular disease (28.57%), arthritis mutilans (7.16%) and distal interphalangeal joint involvement (3.57%).
Patients were undergoing treatment with methotrexate (78.57%), sulphasalazine (14.28%), combination therapy with methotrexate and sulphasalazine (7.15%), and also steroidal or non-steroidal anti-inflammatory drugs, while 35.71% had a treatment history of leflunomide (Fig.1).
Figure 1.

(A, B) Aspect of psoriatic lesions and onychodystrophy (A), dactylitis and arthritis (B) in patients with PsA
DAPSA was within low range in 8 patients, 10 patients were in the moderate disease activity zone, while the same number of patients (10) had high disease activity score (Fig. 2).
Figure 2.
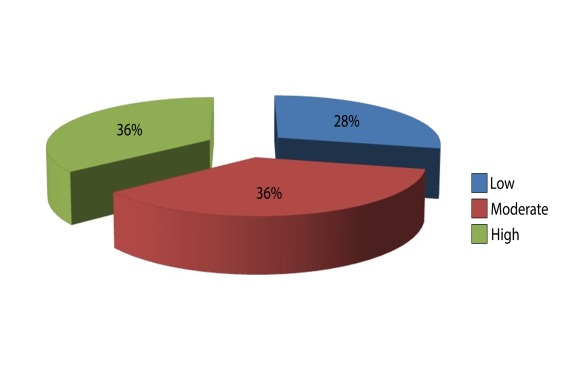
Disease activity score in the study group
In the 28 patients, a total of 840 joints were examined clinically and by ultrasound. From the clinical point of view, out of the total, 32 joints were swollen while 59 joints were tender.
Dactylitis was evidenced in 20/280 examined digits upon physical examination.
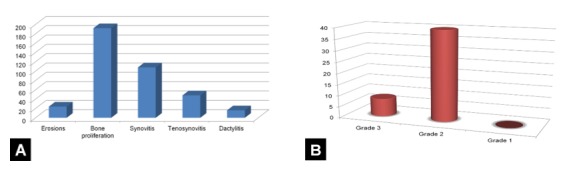
MUS revealed the presence of synovial proliferation in 108/840 sites (12.85%), with grade 1 synovitis in 4 joints (3.7%), grade 2 in 94 joints (87.03%) and grade 3 in 10 joints (9.25%). According to the distribution of involved joints, 40 were MCPs, 26-wrists, 6-PIPs and 16-DIPs, with the second and third MCP being the most frequently affected.
Power Doppler (PD) signal abnormalities were seen in 29/840 joints and in 32.14% of patients (Fig. 3, Fig. 4).
Figure 3.
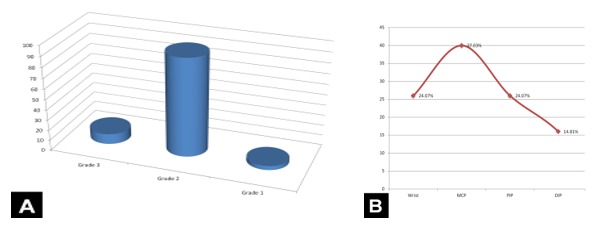
(A, B). Grading (A) and distribution (B) of synovial proliferation
Figure 4.
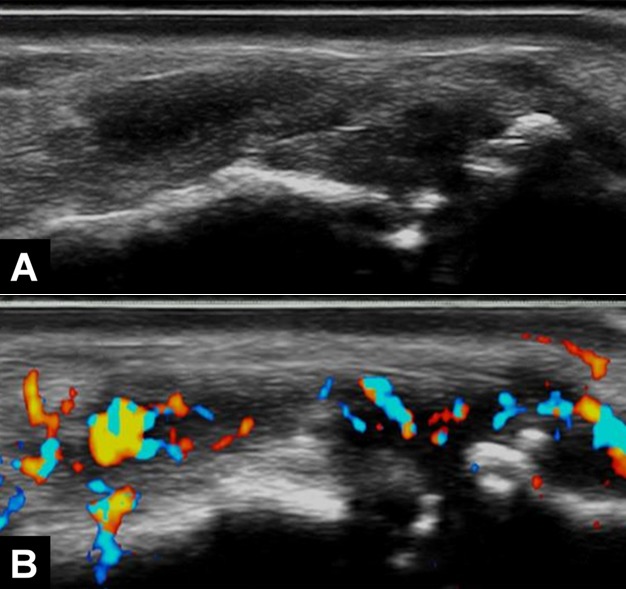
(A, B) Longitudinal scans in grey-scale (A) and power Doppler (B) of the second PIP joint revealing erosions, osteophytes, grade 3 synovial proliferation and power Doppler signal
Out of 280 examined fingers 5.71% presented dactylitis with tenosynovitis of flexor digitorum tendons, synovial proliferation and edema of the subcutaneous cellular tissue, the third digit being the most commonly targeted (Fig.5).
Figure 5.
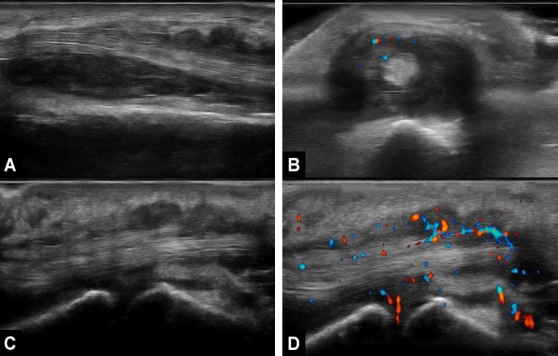
(A-D) Longitudinal (A) and transverse (B) scans of extensor carpi ulnaris tendon revealing grade 3 proliferative tenosynovitis with grade 2 power Doppler signal. Aspect of dactylitis-longitudinal scans in grey-scale (C) and power Doppler (D)
Bone proliferations defined as alterations of the cortical envelope of the bone with “step-up” aspect were encountered in 192 examined joints (22.85%). The presence of erosions interpreted according to the OMERACT definition as a discontinuity of the bone surface visualized in both longitudinal and transverse planes was assessed in 24 bones, mostly in DIP and PIP joints (Fig.6A).
Figure 6.
(A, B) Ultrasound findings in PsA (A) and grading of tenosynovitis of examined sites (B)
The flexor digitorum tendons, both flexor and extensor compartments at the wrist were scanned to evaluate the presence of tenosynovitis as hypoechoic or anechoic thickened tissue with or without fluid in the tendon sheath seen in two perpendicular planes which may present PD signal. The severity of grey-scale tenosynovitis was determined according to synovial thickness from grade 0 to grade 3. Grade 2 tenosynovitis was found in 40 of the examined tendons, whereas 8 tendons presented with grade 3 tenosynovitis. The most frequently involved were the flexor tendons of the digits (38 out of 48 tendons with inflammatory changes), followed by the extensor carpi ulnaris and flexor carpi radialis tendons. PD signal was present in 20.83% of the tendons with structural abnormalities (Fig.6B).
Results and Discussion
Ultrasound (US) evaluation of patients with inflammatory diseases has grown over the past years because of its ability to scan joint structures in dynamic and to provide multi-planar images both in longitudinal and transverse planes of multiple joints.
MUS has demonstrated high potential in identifying inflammation in early stages, signaling groups of patients with poor prognosis and monitoring the effects of conventional or biological disease modifying drugs on disease progression [7].
MUS has proven its efficiency in detecting subclinical inflammation in PsA patients with arthritis involving the joints of the hands. Several studies have shown to be more sensitive than conventional radiography and clinical examination in depicting structural abnormalities in patients with arthritis [8].
US in patients with PsA has been less studied than in patients with rheumatoid arthritis, therefore the available information on the use of MUS in evaluating arthritis is based on the studies performed on patients with rheumatoid arthritis [9].
Our study proved that synovial proliferation is more frequently detected by MUS than clinical examination of the joints, finding consistent with another study conducted by Milosavljevic et al. (2005) on 32 patients with psoriatic arthritis.
The study emphasized on the difficulty in discriminating between arthritis, tenosynovitis and enthesopathy during clinical examination, US providing in this case accurate information on the exact pathology affecting the joints.
The study also stipulated that in early phases of the disease, nor clinical evaluation or conventional radiographs were able to allow a detailed description and location of the inflammatory process. Furthermore, MUS detected more sites with synovial proliferation than clinical examination [10].
A study directed by D’Agostino et al. (2011) determined that most examined sites which had structural abnormalities of joints and tendons also presented PD signal.
In our study, there was a lower incidence of PD on ultrasound, probably due to the fact that all patients were undergoing treatment with disease-modifying drugs and glucocorticoids and/or non-steroidal anti-inflammatory drugs which aid in reducing the inflammation and progression of the disease [11].
Weiner et al. (2008) developed a study based on the sensitivity and specificity of US in detecting bone erosions in comparison with MRI and plain radiographs, proving the higher specificity demonstrated by MUS in evaluating erosions particularly in early stages.
They also stated that more erosions were located at PIP and DIP joints level, findings consistent with our study [12].
Dactylitis from the clinical point of view was more frequent than it was detected by MUS, in contrast with previous statements which demonstrated US high sensitivity in assessing synovitis, consistent with a study conducted by Husic et al. in 2011 [13].
This is probably due to the fact isolated tenosynovitis may be mistaken as dactylitis on physical evaluation, whereas the US definition is more complex taking into consideration tenosynovitis of the flexor digitorum tendons, synovitis of MCP, PIP or DIP joints and subcutaneous tissue edema.
A more recent study directed by Sahbudin et al. in 2018 evaluated the role of ultrasound-defined tenosynovitis and synovitis in prediction of the development of rheumatoid arthritis (RA).
The non-RA group, classified as PsA, showed that the most frequently affected tendons were the flexor digitorum, result consistent with our study.
Furthermore, the presence of synovial proliferation was more commonly encountered in the second and third MCP joints, as in our study [14].
Conclusions
Ultrasound has proven its utility in assessing joint and tendon inflammation to a higher extent that clinically expected. It is a safe, inexpensive, non-invasive method, accessible in the majority of hospitals and clinical practice.
Thus, MUS examination of hand joints may aid the clinician in diagnosing PsA, in evaluating the prognosis and the course of treatment.
However, more extensive studies have to be conducted in order to evaluate the best approach for assessing involvement of joints and tendons in PsA patients.
Conflict of interests
The authors declare that they have no conflict of interests.
References
- 1.Torre Alonso JC, Rodriguez Perez A, Arribas Castrillo JM, Ballina Garcia J, Riestra Noriega JL, Lopez Larrea C. Psoriatic arthritis (PA): a clinical, immunological and radiological study of 180 patients. British Journal of Rheumatology. 1991;30(4):245–250. doi: 10.1093/rheumatology/30.4.245. [DOI] [PubMed] [Google Scholar]
- 2.Hugh NJ, Balachrishnan C, Jones SM. Progression of peripheral joint disease in psoriatic arthritis: a 5-yr prospective study. Rheumatology (Oxford) 2003;42(6):778–783. doi: 10.1093/rheumatology/keg217. [DOI] [PubMed] [Google Scholar]
- 3.Gladman DD. Clinical aspects of the spondyloarthropathies. Am J Med Sci. 1998;316(4):234–238. doi: 10.1097/00000441-199810000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Yamamoto T. Angiogenic and inflammatory properties of psoriatic arthritis. ISRN Dermatol. 2013;2013:630620–630620. doi: 10.1155/2013/630620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prasad PV, Bikku B, Kaviarasan PK, Senthilnathan A. A clinical study of psoriatic arthropathy. Indian J Dermatol Venereol Leprol. 2007;73(3):166–170. doi: 10.4103/0378-6323.32739. [DOI] [PubMed] [Google Scholar]
- 6.Her M, Kavanaugh A. A review of disease activity measures for psoriatic arthritis: what is the best approach. Expert Rev Clin Immunol. 2014;10(9):1241–1254. doi: 10.1586/1744666X.2014.943663. [DOI] [PubMed] [Google Scholar]
- 7.Devauchelle-Pensec V, Saraux A, Alapetite S, Colin D, Le Goff P. Diagnostic value of radiographs of the hands and feet in early rheumatoid arthritis. Joint Bone Spine: Revue du Rhumatisme. 2002;69(5):434–441. doi: 10.1016/s1297-319x(02)00427-x. [DOI] [PubMed] [Google Scholar]
- 8.Kane D, Stafford L, Bresnihan B, FitzGerald O. A prospective, clinical and radiological study of early psoriatic arthritis: an early synovitis clinic experience. Rheumatology (Oxford) 2003;42(12):1460–1468. doi: 10.1093/rheumatology/keg384. [DOI] [PubMed] [Google Scholar]
- 9.Solivetti FM, Andreoli GM, Bacaro D. Ultrasound and psoriatic arthritis-Review of the literature and general considerations. J Ultrasound. 2007;10(2):63–67. doi: 10.1016/j.jus.2007.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Milosavljevic J, Lindqvist U, Elvin A. Ultrasound and power doppler evaluation of the hand and wrist in patients with psoriatic arthritis. Acta Radiologica. 2005;46(4):374–385. doi: 10.1080/02841850510021256. [DOI] [PubMed] [Google Scholar]
- 11.De Simone C, Caldarola G, D'Agostino M, Carbone A, Guerriero C, Bonomo L, Amerio P, Magarelli N. Usefulness of Ultrasound Imaging in Detecting Psoriatic Arthritis of Fingers and Toes in Patients with Psoriasis. Clin Dev Immunol. 2011;2011:390726–390726. doi: 10.1155/2011/390726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weiner SM, Jurenz S, Uhl M, Warnatz K, Peter HH, Walker UA. Ultrasonography in the assessment of peripheral joint involvement in psoriatic arthritis. Clin Rheumatology. 2008;27(8):983–989. doi: 10.1007/s10067-008-0835-y. [DOI] [PubMed] [Google Scholar]
- 13.Husic R, Gretler J, Felber A, Graninger WB, Duftner C, Hermann J, Dejaco C. Disparity between ultrasound and clinical findings in psoriatic arthritis. Ann Rheum Dis. 2014;73(8):1529–1536. doi: 10.1136/annrheumdis-2012-203073. [DOI] [PubMed] [Google Scholar]
- 14.Sahbudin I, Pickup L, Nightingale P, Allen G, Cader Z, Singh R, de Pablo P, Buckley CD, Raza K, Filer A. The role of ultrasound-defined tenosynovitis and synovitis in the prediction of rheumatoid arthritis development. Rheumatology (Oxford) 2018;57(7):1243–1252. doi: 10.1093/rheumatology/key025. [DOI] [PMC free article] [PubMed] [Google Scholar]


