Abstract
Introduction: Regarding high prevalence of postpartum pain and side-effects of pharmaceutical analgesics on maternal and neonatal health, the present study aimed to explore the effect of Melissa officinalis on after-pain among mothers hospitalized in Asgariyeh Hospital, Isfahan, 2016.
Methods: In this single-blind clinical trial, 110 women with moderate to severe after-pain were divided into two M.officinalis and mefenamic acid groups by random allocation. Samples in the first group received 250mg of mefenamic acid and the second group received 395mg of M.officinalis oral capsules every 6hours for 24hours following childbirth. The primary outcome (After-pain) was assessed using a numeric 10-point scale before intervention, 1,2 and 3hours after the first intervention and every 6hours to 24hours after delivery for each of second, third and fourth interventions. Data were analyzed, using SPSS by independent t-test, Mann-Whitney and chi-square test.
Results: The demographic and obstetric variables and after-pain severity before the intervention in both groups were homogenous. Pain intensity wasn’t significantly different between the two groups during first and second hours after the first intervention, but there was a significant difference in the third hour, The severity of pain was significantly different between the two groups in different assessments including: an hour after the second, third and fourth intervention (P<0.05). A significant difference was found between mefenamic acid and M.officinalis in pain relief.
Conclusion: M.officinalis can reduce the severity of after-pain, because it eliminates the need for pharmaceutical analgesics and works much better than mefenamic acid.
Keywords: Herbal Medicine, After-Pain, Mefenamic Acid, Melissa Officinalis
Introduction
Immediately after delivery, women may experience a wide range of postpartum problems including: perineal tear and laceration, episiotomy, breast congestion, stretched nipples, hemorrhoid and the cramps as the uterus shrinks back to normal.1 Recurrent shrinkage and contraction of the uterus following childbirth generally cause after-pains which are mostly seen during the second and subsequent childbirths. The main source of postpartum after-pains and discomfort is associated with uterine contractions.2 More than 82% of women experience postpartum pain.3
These pains persist until early postpartum period4 and the severity of these pains is reduced from the third day onwards.2 Such contractions occur in response to oxytocin secreted by the neurohypophysis. Oxytocin is secreted in response to nipple or breast stimulation as well as to auditory stimulation due to the neonate’s cries.5
Endogenous oxytocin released during breastfeeding also stimulates uterine contractions and as a result, there will be an increase in the severity of pain experienced by the mother.6 On the other hand, oral ingestion of oxytocin or methergine also stimulates uterine contractions and thus leads to more painful postpartum problems.7 This after-pain is an obstacle to success in breastfeeding and reduces the mother’s ability for baby care that can spoil an adequate mother-baby relationship.8 Such pain is a stressor for the mother and may have a negative effect on her acceptance of the mother's role, the relationship with the baby and the quality of life of the mother.9 There are different ways to alleviate postpartum pains, including: encouraging the mother to empty her bladder every 2-3 hours, application of a cold- or hot-water bottle and taking chemical drugs.10 However, the use of analgesics is known to be the most effective way to soothe this pain.11 Common painkillers for reducing postpartum pain include: Acetaminophen (500 mg), codeine (60 mg), aspirin (8), mefenamic acid (250 mg)12 which can be taken once every few hours during the first few days after delivery.13
Although analgesics (mefenamic acid and acetaminophen) are very effective in pain alleviation, there are certain known side effects that are associated with their use, including nausea, vomiting, diarrhea, stomachache, gastrointestinal bleeding, dizziness, drowsiness, and finally seizure and a deep coma.14 People from very old times have been using medicinal plants to treat diseases; however, there has been a general decline in the use of medicinal plants with the emergence of chemical drugs.15 Over recent years, medicinal plants have regained some of their past popularity due to their lower cost and lower side-effects and the patients’ adaptation to them.16 World Health Organization (WHO) has reported that the majority of the world population are dependent upon traditional medicine and an increasing intention and interest in traditional medicine is obvious.17 On the other hand, medicinal plants are especially in demand in the developing countries and a plethora of research conducted by WHO in this respect has provided a vigorous scientific basis regarding the application of medicinal plants.18
Traditional medicine recommends basil oil, chamomile, common sage oil, lily and cumin for alleviating after-pains.19 Mellisa officinalis also called common balm, balm mint and lemon balm, is a medicinal plant known as a sedative anti-spasm, antimicrobic plant in traditional medicine. The leaves are used as an herb. This plant is native to South- Eastern Europe, the Mediterranean Basin, Iraq, northern Iran (Talesh and Golestan jungles), and other Iranian provinces like Azerbaijan, Kermanshah, Tehran and Alborz. This plant contains monoterpene, sesquiterpene, and oxygen-containing compounds. The main components of M. Officinalis are citronellal, ocimene and caryophyllene. A hydroalcoholic extract of M. officinalis has sedative and analgesic properties and stimulates and reinforces sleep in animals and also shows antidepressant and anti-anxiety effects.20 Since the old times, M. Officinalis has been widely used to provide asthma relief, to alleviate pain, to promote stomach health and to fight the Alzheimer’s disease. Moreover, as this herb contains α-tocopherol, it can be effective in pain relief, too.21
The public nowadays is getting aware of the complications of chemical drugs and people are turning to herbal medicines.17,22 Several studies have been carried out to explore the analgesic effects of plant extracts in different countries, partly due to the increasing demand for herbal medicine throughout the world.23 The analgesic and anti-spasm effects of M. officinalis,24 combined with the safety of this plant,25 persuaded us, too, to focus on this native plant. There was a scientific study representing the effect of M. officinalis on dysmenorrhea.24 Regarding the high prevalence of postpartum pain,3 previously, the effects of various herbal medicines have been shown to reduce postpartum pain.22 However, there has been no study, to the best of our knowledge, to examine M. officinalis effect on after pain. So the current study innovatively aimed to investigate the effect of M. officinalis on the severity of after-pains among women referring to Asgariyeh, Isfahan City during 2016.
Materials and methods
The current research is a randomized single-blind controlled trial. The community of study included all women who had referred to Asgariyeh hospital in Isfahan to give normal vaginal delivery during 2016. One hundred ten women participated in our study, and the sample size was obtained using the following equation in each group, assuming α=0.05 and β=0.20 based on the same research.26 Considering the probability of falling 20% of sample size, 55 samples were considered in each group: The inclusion criteria were: women with vaginal delivery, giving birth to a healthy singleton baby, mothers capable of breastfeeding, with moderate to severe after-pains. Exclusion criteria were as follows: having forceps delivery or vacuum extraction, using epidural or spinal anesthesia during labor, a history of allergy to herbal medicines, severe complications after delivery such as bleeding and hypertension, suffering from a chronic systemic disease like diabetes, hypertension, and thyroid disease and taking other herbal or pharmaceutical drugs during research to soothe the pain. The sampling was accomplished by convenience sampling method among women who met the inclusion criteria and then, after filling out the participants’ informed consents, random allocation was performed by random number generator in Excel software for two equal number groups. The M. officinalis and mefenamic acid capsules were in the same coat and they were quite similar in color and odor and were placed by the pharmacist within the envelopes encoded 1 (mefenamic acid) and 2 (M. officinalis) which were named as “a” and “b” respectively on the envelopes. Therefore, the researcher and the samples were unaware of the nature of the codes and blindness criterion was accomplished. Analysis was per-protocol and we compared the treatment groups (including just those samples who completed the treatment originally allocated).
Demographic characteristics of the patients under study including the mother’s age, place of residence, body mass index, and the mother’s and her spouse’s education and occupation were collected through a questionnaire. In addition, data concerning the numbers of pregnancies, childbirths, abortions, history of stillbirth, the date of the last delivery, gestational age based on the first day of the last menstrual period, gestational age based on ultrasound of the expectant mothers, wanted or unintended pregnancies, the baby’s gender, favorable gender of the baby, weight and head circumference of the baby and prescription of oxytocin, following childbirth were collected using self-administered questionnaires. Face validity was used to establish scientific validity.
After reading the latest books and scientific articles, a questionnaire was developed based on the research objectives. Then, 10 university professors (7 midwives, 2 gynecologists and 1 pharmacist) studied it and changes were made after collecting their comments. This questionnaire does not require any reliability. The primary outcome was the intensity of after-pain. In order to investigate the pain intensity, a pain scale (the Numerical Rating Scale (NRS)) was used in which 0 represented “no pain”, 1-3 represented mild pain, 4-6 represented moderate pain and 7-10 represented severe pain. This tool has been used in several studies to measure pain and its validity and reliability have been confirmed before.27 In 2011, Hawker et al. tested its reliability by re-test (r=0.94) and its validity was confirmed by correlation with visual analogue with (ICC = 0.95).28
In the present study, M. officinalis capsules were used. To this end, M. officinalis dry leaves were placed on a winnow, ground in an electrical grinder, passed through a 20 power filter and percolated in a percolator with a 1:8 ratio (solvent to alcohol 70 °C ratio) for 72 hours. In the next phase, the resulting extract was removed, its concentration and alcoholic content were determined and it was condensed in a rotary vacuum-drum filter to remove its alcohol. Finally, the resulting liquid was poured on metal trays and dried in autoclave at 40°C. Then, a powder containing M. officinalis extract was obtained. The dried powder was poured into empty shells of 250 mg mefenamic acid capsules and the M. officinalis capsules contained 395 mg pure extract of M. officinalis.25 Actually this is possible by pressing the material through the punch. In the control group, 250 mg capsule of mefenamic acid (made by Alhavi pharmaceutical company with the serial number 0880394) was given to the patients every six hours for the first 24 hours after delivery. In the implementation phase of the study, at first, the severity of postpartum pain was measured, using the pain scale in each patient before each intervention and then, the samples were randomly assigned to either mefenamic acid or M. officinalis treatment groups. Before the intervention, the pain level was first measured and recorded. Then the first capsule was given to the mother and then the intensity of after-pain was assessed 1,2 and 3 hours after providing the capsule during the first 6 hours, as well as every 6 hours for 24 hours following delivery in both groups and the observed data were recorded in the respective checklists. Subsequent capsules were given every 6 hours up to 4 dose. In the treatment group, if a patient, an hour after taking the capsule, expressed that no pain had occurred, mefenamic acid capsule was given for her lack of pain and the sample was excluded from the study.
The current research with a code of ethics IRCT201608023860N25 was registered at the Ethics Committee of Shahid Beheshti University of Medical Sciences and in Iranian Registry of Clinical Trials with registration code IRCT201608023860N25. A written consent was obtained from every participant and they were assured of confidentiality of their information. The collected data were analyzed using SPSS 23.0 and Mann-Whitney, chi-square and independent t-tests. The Kolmogorov–Smirnov test was used to test the normality distribution of data.
Results
One hundred ten participants, in two groups of mefenamic acid and M. officinalis, each with 55 samples, were selected in the present study. The participants’ inclusion and exclusion processes are presented in figure 1.
Figure 1.
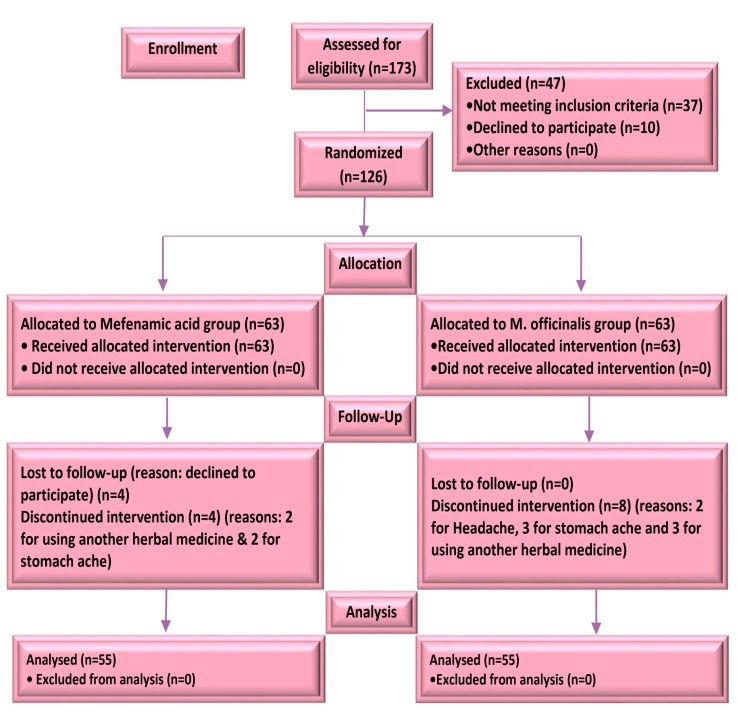
The study flowchart
Both groups were homogenous in terms of demographic and obstetric variables and postpartum pain severity before the intervention (P>0.05): Both groups were similar in terms of an average age of 29.31 (6.450) and an average BMI of 27.565 (35.96) (P>0.05). Regarding education, the largest frequency was high school diploma degree with a frequency of 58.2% in M. officinalis group and 38.2% in mefenamic acid group (P>0.05). In terms of occupation, the maximum frequency was associated with housewives with an average frequency of 91.65% in both groups (P>0.05). For the spouse’s job, the highest frequency was observed for self-employed jobs with an average frequency of 59.65% (P>0.05). As for the number of childbirth, the largest frequency in both groups was one or two childbirths with an average frequency of 88.15% (P>0.05). In our study participants 87.3% had no history of miscarriage (P>0.05). The average age of pregnancy among the subjects of the study was 38.42 (1.445) years (P>0.05). 74.5% of women had a planned and intended pregnancy (P>0.05). According to the neonatal average weight, the highest average birth-weight, 2953.87 (835.19) g, pertained to the M. officinalis group and the largest average head circumference, 35.18 (2.3) cm, was related to the mefenamic acid group (P>0.05). Almost half of the neonates were baby girls and half were baby boys (P>0.05). In terms of favorability of the baby gender, the average favorability of 93.6% was equal in both groups (P>0.05). Further, 47.3% of women in the intervention group and 29.1% in the control group had a history of severe menstrual pain (P>0.05). 71.8% of women of the study had a history of low back pain during pregnancy (P>0.05). 96.1% of women have had oxytocin injection (P>0.05). 91.2% of the subjects had a history of episiotomy (P>0.05).The intensity of pain was not significantly different between the two groups during the first and second hours after the first intervention, but it showed a significant difference in the third hour (P<0.05). However, the severity of pain was significantly different between the two groups an hour after the second intervention (P<0.001).
The severity of pain an hour following the third intervention was significantly different between the two groups (P<0.001). In addition, the severity of pain an hour after the fourth intervention was significantly different between the study groups (P<0.001). Paired t-test and repeated measures analysis of variance showed that the mean scores in both groups decreased, but this decrease was higher in the intervention group(P<0.001) (Table 1). Generally, the average severity of after-pain was lower in the M. officinalis group compared to the mefenamic acid group at all times (figure.2).
Table 1. Severity of pain in different phases of study among the study women .
| Variable |
M. officinalis group
Mean (SD) |
Mefenamic acid group
Mean (SD) |
P-value of t-test |
Size effect (CI * 95%) |
| The first intervention | ||||
| Severity of pain before intervention | 6.4(0.91) | 6.22(1.01) | 0.23 | 0.22 (-0.18 0.62) |
| An hour after intervention | 4.91(1.07) | 5.29(1.27) | 0.09 | 0.38 (-0.02 0.78) |
| Two hours after intervention | 4.44(1.03) | 4.51(1.20) | 0.73 | 0.07 (-0.33 0.47) |
| Three hours after intervention | 3.38(1.06) | 3.94(1.24) | 0.01 | 0.56(0.14 0.96) |
| p-value of repeated measures Anova | <0.001 | <0.001 | ||
| The second intervention | ||||
| Before administration of the second dose | 6.05(0.98) | 5.76(1.06) | 0.13 | 0.29 (-0.11 0.69) |
| After administration of the second dose | 3.55(0.83) | 4.30(0.9) | <0.001 | 0.75 (0.35 1.15) |
| p-value of paired t-test | <0.001 | <0.001 | ||
| The third intervention | ||||
| Before administration of the third dose | 5.76(1.33) | 5.45(1.11) | 0.19 | 0.31 (-0.09 0.71) |
| After administration of the third dose | 3.02(0.99) | 3.95(0.95) | <0.001 | 0.93 (0.53 1.33) |
| p-value of paired t-test | <0.001 | <0.001 | ||
| The fourth intervention | ||||
| Before administration of the fourth dose | 5.34 (087) | 5.13(1.09) | 0.34 | 0.21 (-0.19 0.61) |
| After administration of the fourth dose | 2.54(0.80) | 3.65(0.96) | <0.001 | 1.11 (0.71 1.51) |
| p-value of paired t-test | <0.001 | <0.001 |
*confidence interval
Figure 2.
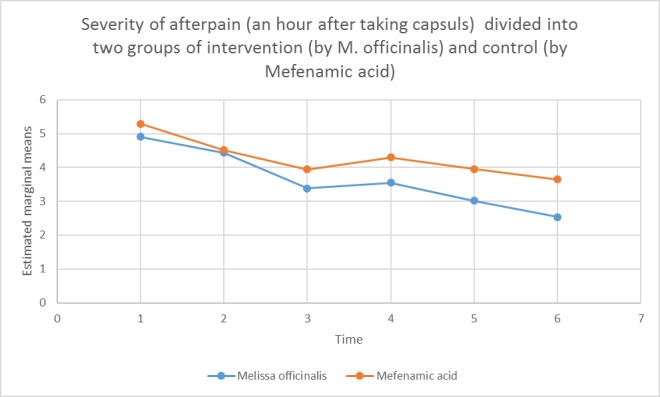
The average severity of pain at all times of study divided into two groups of intervention (by M. officinalis) and control (by Mefenamic acid)
Discussion
Current research assessed the effect of Melissa officinalis on after-pain among women hospitalized at maternity ward, Asgariyeh Hospital in Isfahan during 2016. The results indicated that the average age of the mothers was 28.45 (7.156) in M. Officinalis group and 30.18 (5.745) in the mefenamic acid group (P>0.05). A detailed study stated that older women and those who had higher socioeconomic status expressed less pain than the younger mothers and those with a lower socioeconomic position.29 Several studies have demonstrated that the number of childbirth, duration of labor and breastfeeding are positively correlated with the severity of after-pains.3
However, in the present study, the number of pregnancy, delivery and history of miscarriage were not significantly different between the two groups. Some studies have claimed that episiotomy on the first day after childbirth causes pain in 96.4% of women,30 which can affect the dosage of analgesics and consequently the intensity of after-pain. Nevertheless, our study groups didn’t show significant difference in having or not having an episiotomy (P>0.05).
In a study by Rahjoo et al., titled “investigating the effect of Carum carvi on after-pain”, 81.4% of research subjects had an episiotomy31 which is consistent with the present study. As Jungsten et al., stated in their study, mothers are easily able to distinguish between after-pains and other sources of pain,11 therefore, it should be stressed for the subjects of study that this research is intended to address uterine cramps and the pain from episiotomy stitches is not considered. In the current study, the average after-pain score significantly reduced after administration of M. officinalis capsule compared to before the treatment. This is in line with Ozgoli et al., who assessed the effectiveness of Pimpinella anisum capsule on postpartum pains.26 Furthermore, the present results are consistent with those obtained by Rahjoo et al., who investigated the effect of Carum carvi on postpartum after pains and with the study conducted by Kheiriyat et al., who studied the effect of Anethum graveolens essence and mefenamic acid on postpartum pain.31,32
Birdani et al., also investigated the analgesic and anti-inflammatory effect of M. officinalis extract in the mice. Their results demonstrated that M. officinalis extract in all doses significantly affected the primary (during the first 15 minutes of afterbirth pains) and secondary (15 minutes after commencement of pain) pains33 which was consistent with the results of the current study. Actually, our results indicated that after pains gradually decreased in the M. officinalis group during the first six hours after delivery indicating the beneficial effects of M. officinalis capsule compared to mefenamic acid. Citronellal, Ocimene and Caryophyllene are the main components of M. officinalis.20 In previous studies, the analgesic effect of M. officinalis was related to Rosmarinic acid in the extract of this plant.34 Rosemaric acid is an ester of Caffeic acid, called 3,4-dihydroxyphenyl lactic acid. Rosemaric acid is found in Lamiaceae in the Nepetoidue family and in the subfamily of Boraginaceae in the leaves of the M. officinalis.35
Another possible mechanism may be related to the spasmolytic and antioxidant properties of this plant. Antioxidants prevent the formation of prostaglandin by inhibiting cyclooxygenase and lipoxygenase activity, which prevents the oxidation of unsaturated fatty acids, especially arachidonic acid.36
Naguchi et al., stated that the highest concentration of rosmarinic acid in blood occurs after administering 500 mg of M. officinalis extract and this amount will decrease an hour after its administration25 which is not in agreement with the present study. The reason may be unequal dosage of M. officinalis in the patients. Due to the time of our research, which was in the postpartum period, the mental and physical changes and fatigue caused by delivery affected the mother's response. The researcher tried patiently to relax mothers to control this limitation as much as possible. Also the envelopes of drugs encoded 1 (mefenamic acid) and 2 (M. officinalis) which were named as “a” and “b”; the “a” drug might have been more acceptable to people, and it would have been better if on the envelopes had written the patients code based on the sequence of produced. The strength of this study is that it was the first study to address this issue. Along with the traditional use of this plant in postpartum pain and menstrual pain, this study also provided good clinical evidence. It is suggested that the effect of M. officinalis on pain reduction after cesarean section also be examined.
Conclusion
The results of the current research suggested that Melissa officinalis capsule alleviated postpartum after pains. Therefore, with regard to its negligible complications and favorable effects, M. officinalis is recommended for after-pain relief. It is suggested that future studies consider the effect of M. officinalis on pain relief following cesarean section and Curettage.
Acknowledgments
we would like to appreciate Shahid Beheshti University of Medical Sciences, as well as everyone who participated in this research.
Ethical issues
None to be declared.
Conflict of interest
The authors declare no conflict of interest in this study.
Citation: Naderi Dastjerdi M, Bolbolhaghighi N, Darooneh T, Nasiri M, Moatar F, Esmaeili S, Ozgoli G. Investigating the effect of melissa officinalis on after-pains: a randomized single-blind clinical. J Caring Sci 2019; 8 (3): 129-35. doi:10.15171/jcs.2019.019 .
References
- 1.Can HO, Saruhan A. Evaluation of the effects of ice massage applied to large intestine 4 (hegu) on postpartum pain during the active phase of labor. Iran J Nurs Midwifery Res. 2015;20(1):129–38. (Persian) [PMC free article] [PubMed] [Google Scholar]
- 2.Cunningham F, Leveno K, Bloom S, Spong CY, Dashe J. Williams Obstetrics, 24th ed. New York: Mcgraw-hill; 2014. [Google Scholar]
- 3.Holdcroft A, Snidvongs S, Cason A, Doré CJ, Berkley KJ. Pain and uterine contractions during breast feeding in the immediate post-partum period increase with parity. Pain. 2003;104(3):589–96. doi: 10.1016/S0304-3959(03)00116-7. [DOI] [PubMed] [Google Scholar]
- 4.Declercq E, Cunningham DK, Johnson C, Sakala C. Mothers’ reports of postpartum pain associated with vaginal and cesarean deliveries: results of a national survey. Birth. 2008;35(1):16–24. doi: 10.1111/j.1523-536X.2007.00207.x. [DOI] [PubMed] [Google Scholar]
- 5.Emily G. The symptom experience of postpartum pain after cesarean birth [Disertion] USA, Chicago: University of Illinois Urbana-Champaign; 2013. [Google Scholar]
- 6.Kuritzky L, Samraj GP. Nonsteroidal anti-inflammatory drugs in the treatment of low back pain. J Pain Res. 2012;5(2):579–590. doi: 10.2147/JPR.S6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ebrahimzadeh S Golmakani N, Dadgar S. Evaluation of shapes of uterine contractions with oxytocin in the active phase of labor. The Iranian Journal of Obstetrics, Gynecology and Infertility. 2012;15(25):14–20. (Persian) [Google Scholar]
- 8. Deussen AR, Ashwood P, Martis R. Analgesia for relief of pain due to uterine cramping/involution after birth. Cochrane database of Systematic Reviews 20011; (5): CD004908. doi:10.1002/14651858.cd004908.pub2. [DOI] [PubMed]
- 9.Taleb S, Ozgoli G, Mojab F, Nsiri M, Ahvazi M. Effect of verbascum thapsus cream on intensity of episiotomy pain in primiparous women. The Iranian Journal of Obstetrics, Gynecology and Infertility. 2016;19(7):9–17. (Persian) [Google Scholar]
- 10.Khodam Khodam. R. Tehran: Debaj; 2005. [Google Scholar]
- 11.Jangsten E, Strand R, De Freitas ED, Hellström AL, Johansson A, Bergström S. Women's perceptions of pain and discomfort after childbirth in Angola. Afr J Reprod Health. 2005;9(3):148–58. doi: 10.2307/3583421. [DOI] [PubMed] [Google Scholar]
- 12.Yerby M. Pain in childbearing: key issues in management. 6th ed. London: Elsevier Health Sciences; 2000. [Google Scholar]
- 13.Asgari Nematian M, Mohammadi S. The evaluation of the analgesic effects and acute toxicity of methanol extract of pimpinella anisum. L in male wistar rats. J Babol Univ Med Sci. 2015;17(5):59–65. (Persian) [Google Scholar]
- 14.Martindale S.S.C. the complete drug reference. 36th ed. USA: pharmaceutical Press; 2009. [Google Scholar]
- 15.Aneja KR, Joshi R. Antimicrobial activity of Amomum subulatum and elettaria cardamomum against dental caries causing microorganisms. Ethnobotanical Leaflets. 2009;2009(7):840–49. [Google Scholar]
- 16.Mohamadi J, Motaghi M. Anti-fungal resistance in candida isolated from oral and diaper rash candidiasis in neonates. Bioinformation. 2014;10(11):667–70. doi: 10.6026/97320630010667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Prabuseenivasan S, Jayakumar M, Ignacimuthu S. In vitro antibacterial activity of some plant essential oils. BMC Complement Altern Med. 2006;6(1):39–43. doi: 10.1186/1472-6882-6-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Iwalokun BA, Ogunledun A, Ogbolu DO, Bamiro SB, Jimi-Omojola J. In vitro antimicrobial properties of aqueous garlic extract against multidrug-resistant bacteria and Candida species from Nigeria. J Med Food. 2004;7(3):327–33. doi: 10.1089/jmf.2004.7.327. [DOI] [PubMed] [Google Scholar]
- 19.Tariq SA. Role of ascorbic acid in scavenging free radicals and lead toxicity from biosystems. Molecular biotechnology. 2007;37(1):62–5. doi: 10.1007/s12033-007-0045-x. [DOI] [PubMed] [Google Scholar]
- 20.Chavan SN, More U, Mulgund S, Saxena V, Sontakke AN. Effect of supplementation of vitamin C and E on oxidative stress in osteoporosis. Indian J Clin Biochem. 2007;22(2):101–5. doi: 10.1007/BF02913324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moaveni P, Habibi D, Abbaszadeh B. Effect of drought stress on yield and yield components of four wheat cultivars in shahr-e-gods. I J Agron Plant Breed. 2009;5(1):69–85. [Google Scholar]
- 22.Parsa L, Ozgoli G. A systematic on the medicinal plants used in the treatment of postpartum pain in Iran. The Iranian Journal of Obstetrics, Gynecology and Infertility. 2017;20(5):84–96. (Persian) [Google Scholar]
- 23.Yahya S, Ozgoli G, Mojab F, Alavi Majd H, Shojaee A, Mirhaghjou N. The effect of hypericum perforatum cream on perineal pain after episiotomy in primiparous women. The Iranian Journal of Obstetrics, Gynecology and Infertility. 2015;18(159):1–7. (Persian) [Google Scholar]
- 24.Mirabi P, Alamolhoda SH, Esmaeilzadeh S, Mojab F. Effect of medicinal herbs on primary dysmenorrhoea-a systematic review. Iran J Pharm Res. 2014;13(3):757–67. (Persian) [PMC free article] [PubMed] [Google Scholar]
- 25.Noguchi-Shinohara M, Ono K, Hamaguchi T, Iwasa K, Nagai T, Kobayashi S. et al. Pharmacokinetics, safety and tolerability of melissa officinalis extract which contained rosmarinic acid in healthy individuals: a randomized controlled trial. PloS one. 2015;10(5):e0126422. doi: 10.1371/journal.pone.0126422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ozgoli G, Khodadadie A, Sheikhan Z, Jambarsang S, Mojab F, Taleb S. Comparison of efficacy between herbal capsule of anise and mefenamic acid on after-pain. Journal of Medicinal Plants. 2017;2(62):38–49. (Persian) [Google Scholar]
- 27.Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. Journal of Clinical Nursing. 2005;14(7):798–804. doi: 10.1111/j.1365-2702.2005.01121.x. [DOI] [PubMed] [Google Scholar]
- 28.Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual analog scale for pain (vas pain), numeric rating scale for pain (nrs pain), mcgill pain questionnaire (mpq), short‐form mcgill pain questionnaire (sf‐mpq), chronic pain grade scale (cpgs), short form‐36 bodily pain scale (sf‐36 bps), and measure of intermittent and constant osteoarthritis pain (icoap) Arthritis Care and Research. 2011;63(S11):S240–S52. doi: 10.1002/acr.20543. [DOI] [PubMed] [Google Scholar]
- 29.Tafazoli M, Khadem-Ahmadabadi M, Esmaili H. Comparison the effects of cuminum and mefenamic acid on after pains in multiparous women. The Iranian Journal of Obstetrics, Gynecology and Infertility. 2013;16(75):1–11. (Persian) [Google Scholar]
- 30.Khajvy Shojaei K, Zayeri F. Complications and related factors in epithelial zyatvmy primiparous referred to hospitals in Tehran: a longitudinal study for three months. Journal of Urmia Nursing and Midwifery Faculty. 2009;7(4):217–23. (Persian) [Google Scholar]
- 31. Rahjoo F. A comparison of the effect of Carum carvi L. vs. mefenamic acid on afterpains in multiparous at omidvar hospitals affiliated to larestan University of Medical Sciences in 2012-2013 (Master’s Thesis). Tehran, Iran: Shahid Beheshti University of Medical Sciences; 2013.
- 32.Kheiriyat F, Tadayon Najafabadi M, Mousavi P, Haghighizadeh H, Namjuyan F. Effect of Dill essence and mefenamic acid on postpartum pain. The Iranian Journal of Obstetrics, Gynecology and Infertility. 2016;19(4):8–16. (Persian) [Google Scholar]
- 33.Birdani YO, Cemrk M. Anti-inflammatory and ant nociceptive effects of melissa officials l.in rodents. Revue Med Vet. 2007;185(02):75–81. [Google Scholar]
- 34.Allahverdiyev A, Duran N, Ozguven M, Koltas S. Antiviral activity of the volatile oils of Melissa officinalis L. against Herpes simplex virus type-2. Phytomedicine. 2004;11(7-8):657–61. doi: 10.1016/j.phymed.2003.07.014. [DOI] [PubMed] [Google Scholar]
- 35.Wang H, Provan GJ, Helliwell K. Determination of rosmarinic acid and caffeic acid in aromatic herbs by HPLC. Food Chem. 2004;87(2):307–11. doi: 10.1016/j.foodchem.2003.12.029. [DOI] [Google Scholar]
- 36.Kalvandi R, Alimohammadi S, Pashmakian Z, Rajabi M. The effects of medicinal plants of melissa officinalis and salvia officinalis on primary dysmenorrhea. Avicenna Journal of Clinical Medicine. 2014;21(2):105–11. [Google Scholar]


