Abstract
Introduction: This study aimed to determine the effect of warm footbath before bedtime on the quality of sleep on patients with acute Coronary Syndrome in Cardiac Care Unit.
Methods: This study was conducted on 120 patients admitted to CCU at Mazandaran Heart Center and randomly divided into two groups of intervention and control. In the intervention group, warm footbath was performed after the second night in hospital before bed time by 41 C water for 20 minutes for three consecutive nights; in contrast, the control group did not receive anything of this sort. The next day, St Mary's Hospital Sleep Questionnaire was completed to evaluate sleep quality. Then, the obtained data were analyzed using SPSS software and Friedman, Wilcoxon exact statistical tests.
Results: The quality of sleep in the first night of hospitalization was different from the third night after the intervention in both groups and the improvement process of sleep quality was observed in both groups. Most patients had moderate impairments (23-36), which had not changed during the intervention. In intervention groups, 8 patients had severe sleep disorders (greater than 37), which declined to 1 after three nights of intervention. While, in the control group this number fell from 10 patients with severe sleep disorders to 5. Warm footbath had a great positive impact on patients suffering from severe sleep disorders (P<0.05).
Conclusion: Although warm footbath did not improve the quality of sleep in all patients, it reduced the number of patients who had severe sleep disturbances.
Keywords: Cardiac Care Unit, Heat, Sleep Disorder, Sleep Quality, Warm Footbath
Introduction
The cardiovascular diseases (CVD) are the most common cause of death in the world, and the number of their victims is still on the rise worldwide.1,2 17.3 million People die annually due to cardiovascular diseases and it is estimated that this number will rise up to 23.6 million by 2030. The prevalence of CVD in Asia, the Middle Eastern countries and Iran is rising, too. 3.6 million people are hospitalized each year in Iran among whom a significant percentage suffer from cardiovascular problems and are hospitalized in the intensive care units.3,4 Sleep disorder is common among patients with cardiovascular diseases.5,6 The causes of sleep disorders in cardiac care unit can be related to internal factors such as pain, discomfort, drugs, anxiety, stress, aging, and external factors such unfamiliar environment, ambient noise, bright light, continuous nursing care, drugs ( such as, sedatives and inotropes) which may alter the daily sleep rhythm.7-9 Sleep is a basic human psychological need which is a regular mode that can be easily reversible, playing an important role in human health and wellbeing.10,11 The poor quality of sleep causes various physiological effects, including changes in the immune function, increased sensitivity to pain, decreased vital capacity, forced expiratory volume reduction, metabolic changes in endocrine, increased secretion of norepinephrine and epinephrine, increased sympathetic activity and decreased parasympathetic activity. These factors can lead to increased heart rate and blood pressure, increased heart work, intensified ischemia and infarction.9,12 Medication is commonly used to treat sleep disorders in the intensive care unit. The impact of pharmacologic therapy is faster, but the speed comes at the price of more side effects; however, the non-pharmacologic therapies have delayed, but longer-lasting, effects along with fewer side effects.13,14
Sleep-wake rhythm is synchronized with the rhythm of body temperature. Also, the human body temperature rises by activities during the day, the core temperature reaches its peak at about 16 to 20 pm; after the peak, the core body temperature decreases through thermal transfer from core to the skin of distal extremities such as fingers and toes.15,16 Heating of the skin of distal extremities stimulates the peroptic center of the anterior hypothalamus.17
The more the heat (or the temperature difference between the proximal (e g., stomach) and distal (fingers and toes) organs (called distal- proximal gradient) the better the sleep onset and depth.
The heat transfer from the center to the environment is done through vasodilation. The transfer of heat from the center to environment impairs by age and impaired vascular changes.15,18,19 Cardiovascular diseases and hospitalization in cardiac care units create stress and anxiety.20 This stress stimulates the sympathetic nervous system activity, vasoconstriction, decreased skin temperature of distal and the central extremities,21 thereby reducing sleep quality and delaying the sleep onset. There are several ways to warm the lower extremities including localized heating with warmer or warm footbath. Warm footbath is one of the known methods for creating patient comfort. This method was used so many years ago for pain relief and relaxation for palliative care patients.22 Warm footbath is a common nursing method that not only preserves the integrity of the skin, but also affects the body and the mind and the heart rate.23 Warm footbath at 38 to 42 C for 30 minutes can reduce the heart rate, blood pressure and vascular resistance, it can also increase the blood flow to the legs.24 Warm footbath can increase peripheral blood flow and may facilitate sleep onset and improve sleep quality.19,25 So, this study aimed to examine the effect of warm footbath before bedtime on the quality of sleep in patients with Acute Coronary Syndrome in Cardiac Care Unit.
Materials and methods
This randomized controlled clinical trial was performed to determine the effect of warm footbath before bedtime on the quality of sleep among 60 patients hospitalized in CCU of Fatemeh Zahra Hospital of Sari (North of Iran).
120 participants were divided into two groups, using the table of random numbers according to the date of arrival, 24 hours after they were admitted to CCU. The inclusion criteria included full awareness of the patient, minimum age of 18 years,26 having no mental disorder,27 EF more than 40%,28 having stable vital signs,29 having no chronic sleep disorder and not a long-term sleep-inducing pills treatment.30 Exclusion criteria included fatigue or patient withdrawal, discharge from the CCU, the patient's hemodynamic changes, vascular diseases, skin diseases, having a wound or dressing in the area below the knee, and receiving narcotic drugs less than 4 hours before the intervention.30 In order to prevent disorder in the treatment of patients who receive sleep-inducing drugs according to the routine schedule of the unit, random sampling method was used in intervention and control groups. In order to adjust the confounding factors of the environment, the research was performed in the same unit. Before starting the study, the aim of the study was explained to the patients and a written consent was taken from them. Then, the demographic characteristics were recorded using a demographic questionnaire, including age, sex, educational level, occupation, medical history, history of sleep disorder, sleep-inducing drug history, history of injection drug affecting arteries. St Mary's Hospital Sleep Questionnaire was used in most of the studies in order to assess the quality of sleep in the hospital31-33 and its validity and reliability were verified, for example its reliability was 0.94 in Elise et al.,34 0.91 in Abouhasani35 and 0.91 in Oshvandi studies.27 The St Mary's Hospital Sleep Questionnaire (SMHSQ) was used to measure sleep quality. This 14-item questionnaire was designed to assess sleep quality in patients admitted to the hospital the night before and has the ability to be repeated.36,37 In the present study, considering the validity and reliability of the questionnaire used by Heydary Gorgji et al., the validity and reliability were calculated as 92% and 80%, respectively.38
There is no single method for scoring this questionnaire and scoring was done based on research objectives and design experts.39 In this study, scoring was done based on goals and expert opinions. The scores could vary from 10 to 50. Score 10 would imply no sleep disorder, 11 to 22 would indicate mild sleep disorder, 23 to 36 moderate sleep disorder, and 37 to 50 severe sleep disorder. No intervention was done on the first night of hospitalization; in the morning after hospitalization, the sleep quality was measured and recorded, using the SMHSQ questionnaire as the basic sleep quality of the samples. At the second night, the intervention group received warm footbath for 20 minutes at a temperature of 41 degrees below the knee. The foot skin temperature was measured using infrared thermometers UTNI T UT912 Made in Taiwan before and 20 minutes after the intervention. This thermometer is capable of measuring body and surface temperature from a distance of 5-10 cm.
The core temperature was measured using Beaver laser tympanic thermometer FT55 model made in Germany before, during and 20 minutes after the intervention. The laser thermometers are capable of measuring the tympanic temperature with a margin of 0.2 error. It has been shown in many studies that tympanic temperature is closely related to the core temperature.39 For warm footbath, a special plastic container was used that could contain the leg below the knee to the toes and soles of the feet. The intervention was performed in the intervention group in three consecutive nights and the next morning SMHSQ questionnaire was completed. For the control group, sleep quality questionnaire was recorded without any intervention. Warm footbath time and temperature were 50 minutes before bedtime and at 41 C based on a study.15 During the intervention, the patient's vital signs were controlled every five minutes and the patient was under cardiac monitoring to discontinue the intervention if there were any problems.
After data collection, data analysis was done using software SPSS version 13 (IBM, Armonk, NY, USA). For demographic data, descriptive statistics such as mean (standard) deviation and relative frequency distribution table were used; for the comparison of the sleep quality, the Friedman test was used to compare the sleep quality during the hospitalization nights; then a paired comparison was performed for the quality of sleep at hospitalized night using the Wilcoxon test; and finally, the frequency of sleep quality scores were compared using Fisher's exact test. Fischer's exact test was used to compare the dispersion of sleep quality between the two groups. P˂0.05 was considered as significant level in this study.
Results
The results showed that there were no significant differences in terms of age. In the intervention group the mean and standard deviation were 62.06, 8.49 and in the control group the mean and standard deviation were 61.45 and 7.50, respectively. T-test showed no statistically significant difference between the two groups (P=0.67, t=0.421, df=118). In terms of gender, there was 51.7% females in the control group and 38.3% females in the intervention group while the rest were males. The Chi-square test showed no significant difference in terms of gender (P=0.142). The mean EF was 45.28. In both groups, the mean sleep quality decreased during hospitalization, so that the worst sleep quality was at their first night and the best sleep quality was at the third night after the intervention. The quality of sleep during the hospitalization nights were significantly different in the control group and the intervention group with Friedman test (Table 1).
Table 1. Comparison quality of sleep during the hospitalization nights in the control and intervention group with friedman test .
| Group Time | Intervention Mean-rank | Control Mean-rank |
| First night of hospitalization | 2.65 | 2.56 |
| First night after intervention | 2.45 | 2.63 |
| Second night after intervention | 2.48 | 2.53 |
| Third night after intervention | 2.42 | 2.29 |
| Statistical Test | 14.50 | 15.83 |
| Significant Level | P=0.002 | P=0.001 |
In the intervention group, the sleep quality at the first hospitalization night was different from the first and third nights after the intervention; in the Control group, the first night with the third night, and also first and second nights after the intervention were different from the third night after the intervention (Table 2).
Table 2. Comparison mean of sleep quality during the hospitalization nights in the control and intervention groups .
| Time of intervention | Significant difference | |
| Intervention group | Control group | |
| First night of hospitalization via first night after intervention | P=0.01 | P=0.31 |
| First night after intervention via second night after intervention | P=0.31 | P=0.08 |
| Second night after intervention via third night after intervention | P=0.15 | P=0.15 |
| First night after intervention via third night after intervention | P=0.564 | P=0.56 |
| First night of hospitalization via third night after intervention | P=0.008 | P=0.008 |
Fisher's exact test indicated no difference in terms of the frequency of sleep quality in the two groups, so that no patient had a score less than 10 during the nights of hospitalization (no sleep disorder). 8 cases had a score between 11 and 22 (mild sleep disorder) on the first night of hospitalization in the control group and their score was almost unchanged during hospitalization. eight cases had a score between 37 to 50 (severe sleep disturbances) on the first night of hospitalization in the control group, but this score was reduced to zero after the first night of intervention and did not increase during the intervention, whereas in the control group 10 cases had a score of 37 to 50 on the first night of hospitalization in the control group, which increased to 12 cases and eventually decreased to 5 cases after the intervention (Figure 1).
Figure 1.
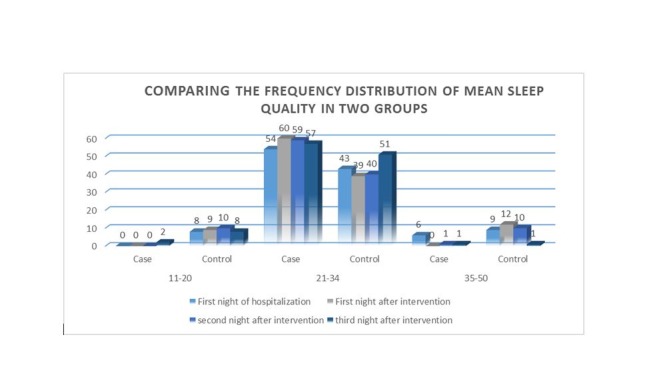
Comparing the frequency distribution of mean sleep quality in two groups
Most patients had sleep quality score of 23-36 (moderate sleep disorder) which had no changes in both groups after the intervention in the first night (Table 3).
Table 3. Comparison the frequency of rating sleep quality in hospitalization nights in the control and intervention group .
| Score time | First night of hospitalization | First night after intervention | Second night after intervention | Third night after intervention | ||||
| Intervention | Control | Intervention | Control | Intervention | Control | Intervention | Control | |
| 11 to 22 (mild sleep disorder) |
8 | 0 | 9 | 0 | 10 | 0 | 8 | 2 |
| 23to36 (moderate sleep disorder) |
42 | 52 | 39 | 60 | 39 | 59 | 47 | 57 |
| 37 to 50 (severe sleep disturbances) |
10 | 8 | 12 | 0 | 11 | 1 | 5 | 1 |
| Fisher's exact test | 0.007 | 0.001 | 0.001 | 0.036 | ||||
The frequency of sleep quality scores showed that the patients in the intervention group with severe sleep disorders had a greater reduction compared to the control group; but the number of patients with moderate sleep disorder had no specific changes. Therefore, it can be concluded that warm footbath cannot improve sleep quality in all patients.
Discussion
Average sleep quality based on SMHSQ showed that most patients in both groups had moderate sleep disorders during the nights of intervention. Several studies have shown that hospitalization can reduce sleep quality. The studies investigating the impact of blindfolds on sleep quality in patients at CCU have revealed that 63% of patients,31 or 74% of hospitalized patients had sleep disorders.14 The higher incidence of sleep disorders in this study as compared to the above studies could be due to a different hospital unit or questionnaires, that is those studies used a Pittsburgh questionnaire, while SMHSQ was used in this study. Pittsburgh questionnaire sleep quality index can measure sleep quality in the previous month while SMHSQ measures the quality of sleep in the hospital. The study of Heydari Gorji on the effect of massage with Valarin oil on the sleep quality of patients in CCU showed that during the intervention and hospitalization sleep quality based on SMHSQ was in the range of moderate sleep disorder in both intervention and control groups.38
In the study of Oshvandi27 patients had moderate sleep disorders based on SMHSQ, which was consistent with our results. The reasons of the decline in sleep quality scores in both groups included getting used to the conditions of hospitalization, the symptoms of disease improving, and having pain and sleep medication reduced based on the hospital routine. According to the findings, warm footbath cannot improve the quality of sleep in all patients; however, this method reduced the number of patients who had severe sleep disorders. The findings of the present study are consistent with two separate studies of Liao using polysomnography as a tool for sleep quality measurement (the most accurate method of measuring the quality of sleep).15,19
Our results are not consistent with those of Hiroyuki on the impact of Leg Thermal Therapy on sleep quality of patients with congestive heart failure.40 Nor are they also not consistent with the results of the studies of Silva (fibromyalgia patients at 36 C)41 and Lai Min Fan (liver cirrhosis patients at 38 to 45 C for 7 nights).16 In those studies, warm footbath improved the quality of sleep, but in the present study it worked only in a small percentage of patients who had severe sleep disorders. Reviewing the above studies, we found that the environment and the duration of warm footbath and sleep quality measuring tools were varied. Several factors can affect the quality of sleep, including the environment, disease, pain, medicine, nursing cares, noise, light and circadian rhythm disorder which are varied in different hospitals, so they can have different effects on sleep. Patients admitted to CCU are known to suffer from some degree of stress, because of the seriousness of their disease, in fact, as the studies would verify it, these patients actually have the highest amount of stress. And anxiety can increase the sympathetic activity and narrowing of the arteries and can reduce heat transfer from the center to the environment. Although warm footbath stimulates the synthesis of nitric oxide, dilates blood vessels, reduces vascular resistance, increases blood flow and enhances the heat transfer to the environment, increases distal- proximal gradient18,42 and thereby improves sleep quality in other studies, it still failed to improve the quality of sleep in all patients in this study. Another limitation of this study was training the nurses about the physiological effects of warm foot bath, the precise methods of doing foot bath, measuring the water temperature, the time needed for the foot bath, because the incorrect implementation of intervention method can lead to the fatigue of the patient, or may cause organ burns.
Conclusion
Warm footbath had more positive effects only on patients who had severe sleep disorders; however, it did not seem to be equally effective on patients with average sleep disorders. Although the increased temperature of the skin is required at the starting point of a good sleep, sleep quality is influenced by several factors. For further research, it seems relevant and prudent to investigate the effect of warm foot bath on physiological parameters and anxiety of patients admitted to CCU.
Acknowledgments
The present study is a result of a graduate thesis at the Mazandaran University of Medical Sciences and was recorded by the code of IRCT201412141315N9 and it was approved by ethics Committee of Mazandaran University of Sciences by the code of IR.MAZUMS.REC.94-1454. We here bye appreciate the cooperation of the Research Deputy, hospital staff, and patients who helped us during the project are highly appreciated.
Ethical issues
None to be declared.
Conflict of interest
The authors declare no conflict of interest in this study.
Citation: Talebi Ghadicolaei H, Heydary Gorji MA, Bagheri B, Yazdani Charati J, Hadinejad Z. The effect of warm footbath on the quality of sleep on patients with acute coronary syndrome in cardiac care unit. J Caring Sci 2019; 8 (3): 137-42. doi:10.15171/jcs.2019.020.
References
- 1.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ. et al. Heart disease and stroke statistics--2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Writing Group Members, Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD. et al. Executive summary: heart disease and stroke statistics—2012 update a report from the American Heart Association. Circulation. 2012;125(1):188–197. doi: 10.1161/CIR.0b013e3182456d46. [DOI] [PubMed] [Google Scholar]
- 3.Naghavi M, Abolhassani F, Pourmalek F, Lakeh MM, Jafari N, Vaseghi S. et al. The burden of disease and injury in Iran 2003. Population Health Metrics. 2009;7(1):9. doi: 10.1186/1478-7954-7-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Taghipour B, Nia HS, Soleimani MA, Afshar MH, Far SS. Comparison of the clinical symptoms of myocardial infarction in the middle-aged and elderly. Journal of Kermanshah University of Medical Sciences. 2014;18(5):281–89. (Persian) [Google Scholar]
- 5.Cho MY, Min ES, Hur MH, Lee MS. Effects of aromatherapy on the anxiety, vital signs, and sleep quality of percutaneous coronary intervention patients in intensive care units. Evidence-Based Complementary and Alternative Medicine. 2013;2013:381. doi: 10.1155/2013/381381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mashayekhi F, Pilevarzadeh M, Amiri M, Rafiei H. The effect of eye mask on sleep quality in patients of coronary care unit o efeito da mascara de olhos na qualidade de sono em pacientes em uma unidade coronariana. Sleep Science. 2013;6(3):108–11. [Google Scholar]
- 7.Eliassen KM, Hopstock LA. Sleep promotion in the intensive care unit—A survey of nurses’ interventions. Intensive and Critical Care Nursing. 2011;27(3):138–42. doi: 10.1016/j.iccn.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 8.Schiza SE, Simantirakis E, Bouloukaki I, Mermigkis C, Arfanakis D, Chrysostomakis S. et al. Sleep patterns in patients with acute coronary syndromes. Sleep Medicine. 2010;11(2):149–153. doi: 10.1016/j.sleep.2009.07.016. [DOI] [PubMed] [Google Scholar]
- 9.Kamdar BB, Needham DM, Collop NA. Sleep Deprivation in Critical Illness Its Role in Physical and Psychological Recovery. Journal of Intensive Care Medicine. 2012;27(2):97–111. doi: 10.1177/0885066610394322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arasteh M, Yousefi F, Sharifi Z. Investigation of sleep quality and its influencing factors in patients admitted to the gynecology and general surgery of beat hospital in sanandaj. Medical Journal of Mashhad University of Medical Sciences. 2014;57(6):762–9. (Persian) [Google Scholar]
- 11.Amagai Y, Ishikawa S, Gotoh T, Kayaba K, Nakamura Y, Kajii E. Sleep duration and incidence of cardiovascular events in a Japanese population: the Jichi Medical School cohort study. Journal of Epidemiology. 2010;20(2):106–10. doi: 10.2188/jea.JE20090053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fontana CJ, Pittiglio LI. Sleep deprivation among critical care patients. Crit Care Nurs Q. 2010;33(1):75–81. doi: 10.1097/CNQ.0b013e3181c8e030. [DOI] [PubMed] [Google Scholar]
- 13.Richardson A, Allsop M, Coghill E, Turnock C. Earplugs and eye masks: do they improve critical care patients’ sleep? Nursing in Critical Care. 2007;12(6):278–286. doi: 10.1111/j.1478-5153.2007.00243.x. [DOI] [PubMed] [Google Scholar]
- 14.Zerahati F, Saif Rabiee M, Araqhchian M, Sabori T. Evaluate sleep quality and use of Sleeping medication in adults admitted to Internal department hospital ekbatan Hamedan. J Med Sci Health Serv Hamedan. 2009;16(4):31–6. (Persian) [Google Scholar]
- 15.Liao WC, Wang L, Kuo CP, Lo C, Chiu MJ, Ting H. Effect of a warm footbath before bedtime on body temperature and sleep in older adults with good and poor sleep: An experimental crossover trial. Int J Nurs Stud. 2013;50(12):1607–16. doi: 10.1016/j.ijnurstu.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 16.Li MF. Effect of foot bath and massage on insomnia in patients with liver cirrhosis and investigation of nursing satisfaction. Journal of Acupuncture and Tuina Science. 2014;12(2):105–8. [Google Scholar]
- 17.Mallick HN, Kumar VM. Basal forebrain thermore gulatory mechanism modulates auto-regulated sleep. Front Neurol. 2012;3:102. doi: 10.3389/fneur.2012.00102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liao WC, Landis CA, Lentz MJ, Chiu MJ. Effect of foot bathing on distal-proximal skin temperature gradient in elders. Int J Nurs Stud. 2005;42(7):717–722. doi: 10.1016/j.ijnurstu.2004.11.011. [DOI] [PubMed] [Google Scholar]
- 19.Liao WC, Chiu MJ, Landis CA. A warm footbath before bedtime and sleep in older Taiwanese with sleep disturbance. Research in Nursing & Health. 2008;31(5):514–28. doi: 10.1002/nur.20283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tavakolizadeh J, Kianmehr M, Basiri Moghadam M, Pahlavan M. Effect of Guided Visualization on Anxiety of Patients with Acute Coronary Syndrome Admitted to the Cardiac Intensive Care Unit. The Horizon of Medical Sciences. 2015;21(3):147–53. doi: 10.18869/acadpub.hms.21.3.147. [DOI] [Google Scholar]
- 21.Vinkers CH, Penning R, Hellhammer J, Verster JC, Klaessens JH, Olivier B. et al. The effect of stress on core and peripheral body temperature in humans. Stress. 2013;16(5):520–30. doi: 10.3109/102538902013.807243. [DOI] [PubMed] [Google Scholar]
- 22.Yamamoto K, Aso Y, Nagata S, Kasugai K, Maeda S. Autonomic, neuro-immunological and psychological responses to wrapped warm footbaths—a pilot study. Complementary Therapies in Clinical Practice. 2008;14(3):195–203. doi: 10.1016/j.ctcp.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 23.Saeki Y. The effect of foot-bath with or without the essential oil of lavender on the autonomic nervous system: a randomized trial. Complementary Therapies in Medicine. 2000;8(1):2–7. doi: 10.1016/S0965-2299(00)90703-9. [DOI] [PubMed] [Google Scholar]
- 24.XU FH, Uebaba K. Temperature dependent circulatory changes by footbath-changes of systemic, cerebral and peripheral circulation. The Journal of The Japanese Society of Balneology, Climatology and Physical Medicine. 2003;66(4):214–226. [Google Scholar]
- 25.Raymann RJ, Van Someren EJ. Diminished capability to recognize the optimal temperature for sleep initiation may contribute to poor sleep in elderly people. Sleep. 2008;31(9):1301–9. doi: 10.5665/sleep/31.9.1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zeighami R, Mohamadihariry F, Jalilolghadr S. Investigating the Effect of “Citrus Aurantium” Aroma on Sleep Quality of Patients Hospitalized in the Coronary Care Unit (CCU) Complementary Medicine Journal of faculty of Nursing & Midwifery. 2014;4(1):720–33. (Persian) [Google Scholar]
- 27.Oshvandi K, ABDI S, Karampourian A, Moghimbaghi A, HOMAYOUNFAR S. The effect of foot massage on quality of sleep in ischemic heart disease patients hospitalized in CCU. Iran J Crit Care Nurs. 2014;7(2):66–73. (Persian) [Google Scholar]
- 28.Nesami MB, Gorji MA, Rezaie S, Pouresmail Z, Chorati JY. The effect of acupressure on the quality of sleep in patients with acute coronary syndrome in Cardiac Care Unit. Iran J Crit Care Nurs. 2014;7(1):7–14. (Persian) [Google Scholar]
- 29.Zolfaghari M, Farokhnezhad Afshar P, Asadi Noghabi AA, Ajri Khameslou M. Modification of environmental factors on quality of sleep among patients admitted to CCU. Hayat. 2013;18(4):61–8. (Persian) [Google Scholar]
- 30.Pacheco LD, Saade GR, Hankins GD. Mechanical ventilation during pregnancy: sedation, analgesia, and paralysis. Clinical Obstetrics and Gynecology. 2014;57(4):844–50. doi: 10.1097/GRF.0000000000000064. [DOI] [PubMed] [Google Scholar]
- 31.Nesami MB, Gorji MA, Rezaie S, Pouresmail Z, Chorati JY. The effect of acupressure on the quality of sleep in patients with acute coronary syndrome in Cardiac Care Unit. Iran J Crit Care Nurs. 2014;7(1):7–14. (Persian) [Google Scholar]
- 32.McGregor C, Srisurapanont M, Jittiwutikarn J, Laobhripatr S, Wongtan T, White JM. The nature, time course and severity of methamphetamine withdrawal. Addiction. 2005;100(9):1320–29. doi: 10.1111/j.1360-0443.2005.01160.x. [DOI] [PubMed] [Google Scholar]
- 33.Janssens JP, Metzger M, Sforza E. Impact of volume targeting on efficacy of bi-level non-invasive ventilation and sleep in obesity-hypoventilation. Respiratory Medicine. 2009;103(2):165–72. doi: 10.1016/j.rmed.2008.03.013. [DOI] [PubMed] [Google Scholar]
- 34.Ellis BW, Johns MW, Lancaster R, Raptopoulos P, Angelopoulos N, Priest RG. The St. Mary's Hospital sleep questionnaire: a study of reliability. Sleep. 1981;4(1):93–7. doi: 10.1093/sleep/4.1.93. [DOI] [PubMed] [Google Scholar]
- 35. Abolhasani, S., Effect of sensory stimulation on sleep deprivation symptoms and cardiac index in patients admitted to coronary care unit selected hospitals of Isfahan University of Medical Sciences. [Master's Thesis] Isfahan: Isfahan University of Medical Sciences; 2003.
- 36.Ziegler G, Ploch M, Miettinen-Baumann A, Collet W. Efficacy and tolerability of valerian extract LI 156 compared with oxazepam in the treatment of non-organic insomnia--a randomized, double-blind, comparative clinical study. Eur J Med Res. 2002;7(11):480–86. [PubMed] [Google Scholar]
- 37.Shahid A, Wilkinson K, Marcu S, Shapiro CM. STOP, THAT and One Hundred Other Sleep Scales, Chapter 31: FACES (Fatigue, Anergy, Consciousness, Energy, and Sleepiness) Springer Science+ Business Media. 2012;200:155–56. [Google Scholar]
- 38.Bagheri-Nesami M, Gorji MA, Rezaie S, Pouresmail Z, Cherati JY. Effect of acupressure with valerian oil 2.5 on the quality and quantity of sleep in patients with acute coronary syndrome in a cardiac intensive care unit. J Tradit Complement Med. 2015;5(4):241–47. doi: 10.1016/j.jtcme.2014.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hu Q, Zhu W, Zhu Y, Zheng L, Hughson RL. Acute effects of warm footbath on arterial stiffness in healthy young and older women. Eur J Appl Physiol. 2012;112(4):1261–8. doi: 10.1007/s00421-011-2066-1. [DOI] [PubMed] [Google Scholar]
- 40.Hu Q, Zhu W, Zhu Y, Zheng L, Hughson RL. Acute effects of warm footbath on arterial stiffness in healthy young and older women. Eur J Appl Physiol. 2012;112(4):1261–8. doi: 10.1007/s00421-011-2066-1. [DOI] [PubMed] [Google Scholar]
- 41.Sawatari H, Shinohara M, Ando SI, Nishizaka M, Hashiguchi N, Rahmawati A. et al. Leg Thermal therapy improved sleep structure in patients with congestive heart disease. Transactions of Japanese Society for Medical and Biological Engineering. 2013;51(Supplement):R–235. doi: 10.11239/jsmbe.51.R-235. [DOI] [Google Scholar]
- 42.Silva A, Queiroz SS, Andersen ML, Mônico-Neto M, Campos RM, Roizenblatt S. et al. Passive body heating improves sleep patterns in female patients with fibromyalgia. Clinics. 2013;68(2):135–40. doi: 10.6061/CLINICS/2013(02)OA03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kuwahata S, Miyata M, Fujita S, Kubozono T, Shinsato T, Ikeda Y. et al. Improvement of autonomic nervous activity by Waon therapy in patients with chronic heart failure. Journal of Cardiology. 2011;57(1):100–6. doi: 10.1016/j.jjcc.2010.08.005. [DOI] [PubMed] [Google Scholar]


