Abstract
Study Objectives:
The aim of the current study was to test the hypothesis that there is a temporal correlation between reflux episodes and respiratory events in patients with laryngopharyngeal reflux and obstructive sleep apnea.
Methods:
Adults with clinically diagnosed laryngopharyngeal reflux confirmed by two validated instruments (reflux symptom index ≥ 13 and reflux finding score ≥ 7) and obstructive sleep apnea (OSA) underwent full polysomnography with concomitant and synchronized multichannel intraluminal impedance-pH esophageal monitoring. The apnea-hypopnea and arousal indexes that occurred 15, 30, and 45 minutes before and after each reflux episode were recorded and compared to full-night apnea and hypopnea and arousal index.
Results:
We studied 27 patients (14 males, age 51.7 ± 9.1 years, body mass index 32.4 ± 4.2 kg/m2) with laryngopharyngeal reflux (reflux symptom index 16 ± 2 and reflux finding score 12 ± 3) and OSA (apnea-hypopnea index = 32.3 ± 28.4 events/h). We evaluated 102 reflux episodes. Almost half of the reflux episodes occurred while awake (43.1%) and only five reflux episodes (4.9%) occurred during an obstructive respiratory event. The apnea and hypopnea and arousal indexes 15, 30, and 45 minutes before and after reflux episodes were lower than full-night apnea and hypopnea and arousal indexes, respectively.
Conclusions:
Among patients with well-established laryngopharyngeal reflux and OSA, there is no temporal association between reflux and obstructive respiratory events. Even though the data comprised a small sample size, it seems that a more complex mechanism is involved with these two highly prevalent diseases.
Citation:
Xavier SD, Eckley CA, Duprat AC, de Souza Fontes LH, Navarro-Rodriguez T, Patrocínio J, Tridente D, Lorenzi-Filho G. Temporal association between respiratory events and reflux in patients with obstructive sleep apnea and laryngopharyngeal reflux. J Clin Sleep Med. 2019;15(10):1397–1402.
Keywords: gastroesophageal reflux, laryngopharyngeal reflux, pH impedance, sleep apnea syndrome
BRIEF SUMMARY
Current Knowledge/Study Rationale: Obstructive sleep apnea and laryngopharyngeal reflux frequently coexist but temporal association between them is not well established. The relationship between them is potentially bidirectional.
Study Impact: We performed concomitant evaluation of both reflux and apnea along a continuous period (15, 30, and 45 minutes) by using gold-standard diagnostic methods: polysomnography and multichannel intraluminal impedance-pH esophageal monitoring with no temporal association found between them. Compensatory changes in upper esophageal sphincter and gastroesophageal junction pressures may prevent reflux after an apneic event.
INTRODUCTION
Obstructive sleep apnea (OSA) is a common condition in the general population characterized by repetitive events of partial or complete obstruction of the upper airways during sleep.1 Obesity2 and advanced age3,4 are main risk factors for OSA, and patients with OSA frequently present with multiple comorbidities, such as metabolic syndrome.5 OSA does not only share risk factors with cardiovascular and metabolic diseases, but OSA may trigger or aggravate cardiovascular diseases such as hypertension.3,6–9
Several studies have indicated an association between OSA and laryngopharyngeal reflux (LPR).10–16 OSA and LPR are frequent in the adult population, share several risk factors such as obesity and older age,10,12 and when present may cause morbidity and reduced quality of life.17,18 LPR is more prevalent in patients with OSA than in the general population (60% versus 20%).12,17 In addition, there is evidence that the treatment of OSA improves symptoms of reflux symptoms and vice versa.13,19–22 Because obstructive respiratory events are characterized by futile efforts to breathe against the occluded airways with generation of large negative intrathoracic pressure, it has been long hypothesized that OSA would trigger episodes of LPR. However, the literature is controversial and only a few studies have evaluated studying patients with well-established LPR and OSA with simultaneous recordings of episodes of LPR and respiratory events.11,23–26 Most of these studies use two-channel,24,25 triple sensor,23 or oropharyngeal sensor26 pH testing. Only one study used pH-impedanciometry, which is the gold-standard method for LPR reflux.11
The relationship between LPR and OSA is potentially bidirectional. Pressure gradient changes between the abdomen and thorax reportedly occur during obstructive respiratory events10,12,19 and could lead to an acute episode of LPR or a delayed relaxation of the lower esophageal sphincter (LES), triggering reflux to occur after the obstructive event. Conversely, considering that the inflammatory response to the refluxate at the level of the pharynx can take place after minutes or even hours,10,12 it is possible that LPR episodes could cause a delayed and transient increase in OSA severity.
Thus, the objective of the current study was to investigate the temporal association between reflux and obstructive respiratory events in patients with OSA and LPR by evaluating the frequency of respiratory events before and after reflux episodes.
METHODS
This study was conducted in accordance with the amended Declaration of Helsinki. Following approval by the local Institutional Review Board for research in humans (#311/10), written informed consent was obtained from all patients.
Patients with LPR were enrolled from January 2012 to March 2013 from an outpatient clinic that is a reference location for the study of patients with reflux. Inclusion criteria were age older than 18 years and younger than 70 years; body mass index (BMI) ≤ 40 kg/m2; clinical symptoms and signs of LPR characterized by a reflux symptom index (RSI) > 1327 and a reflux finding score (RFS) > 7,28 corroborated by either an esophagogastroduodenoscopy (erosive esophagitis or Barrett esophagus29) or positive prolonged esophageal pH monitoring. In patients suspected of OSA, the condition is confirmed by a positive Berlin score30 and/or Epworth Sleepiness Scale score higher than 10.31 Exclusion criteria were: current or former smoker, acute or chronic allergic rhinitis, previous surgery or cancer of the head and neck and/or digestive tract, history of alcohol abuse, and chronic use of inhaled steroids and bronchodilators. Patients were instructed to discontinue the use of any drug known to alter gastric secretions 14 days prior to entering the protocol.
Following clinical evaluation, patients underwent simultaneous synchronized standard polysomnography (PSG) (Alice 5 Respironics, Murrysville, Pennsylvania, USA) and multichannel intraluminal impedance-pH esophageal monitoring (MII) (Sandhill Scientific, Highlands Ranch, Colorado, USA). The method involved the input of a timing signal produced by a synchronization signal generator (Sandhill Scientific) to both impedance/pH recordings and PSG. On the morning of the sleep study, all patients underwent esophageal manometry (Sierra Scientific Instruments, Inc., Los Angeles, California, USA). After confirming the position of the upper esophageal sphincter and LES, an impedance/pH catheter was placed with the distal pH sensor positioned 5 cm above the proximal end of the LES high-pressure zone and the upper pH sensor near the crycopharyngeous muscle (larynx/pharynx). Manometric data and impedance/pH recordings were analyzed using Manoview (Sierra Scientific Instruments, Inc.) and Bioview (Sandhill Scientific Inc.) software input.
Sleep stages and respiratory events recorded during PSG were scored by an experienced sleep medicine physician. The sleep stages, arousal events, and respiratory events were all scored using standardized criteria.32,33 The apnea-hypopnea index (AHI) was calculated as the number of apneas and hypopneas per hour during sleep.1 OSA was classified as mild, moderate and severe according to standard criteria (AHI > 5 to 15; AHI >15 to 30, and > 30, respectively).1 Only sleep studies that obtained 4 or more hours of adequate monitoring were included. Patients with an AHI < 5 events/h during PSG or who did not experience at least one episode of reflux during the synchronized study were excluded. Distal pathologic reflux episodes of MII were established following the manufacturer’s guidelines.34 Reflux episodes were characterized as either pure liquid or a mix of liquid and gas, and as acidic, nonacidic, or weakly acidic. Proximal pathologic reflux was defined as episodes reaching the proximal pH sensor with a pH ≤ 5, regardless of its duration.34
The temporal association between obstructive events and episodes of reflux were determined. In order to establish whether the number and severity of respiratory events were associated to the onset of reflux episodes and vice versa, a cutoff period of 15, 30, and 45 minutes before and after each reflux episode was determined and compared to the full night or total AHI. When the extended period of 30 and 45 minutes overlapped another with another reflux episode, the analysis was not performed. Reflux episodes that occurred during rapid eye movement (REM) sleep were excluded from the analysis in order to avoid variations of AHI related to sleep stage.35 Numerical data were expressed as mean ± standard deviation and qualitative data were expressed as absolute and relative frequencies for all patients. The AHI index and arousal index were evaluated before and after reflux episode during different periods and it was compared using the paired t test. All statistical tests were conducted with a 5% significance level.
RESULTS
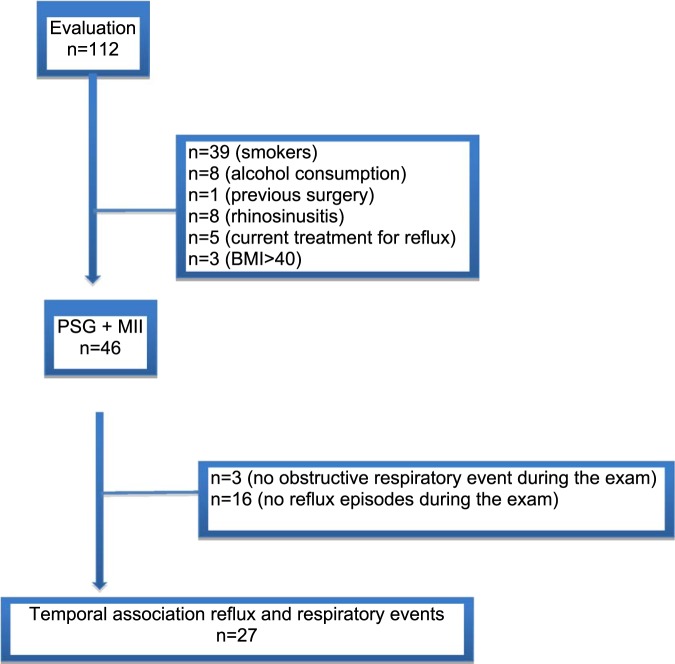
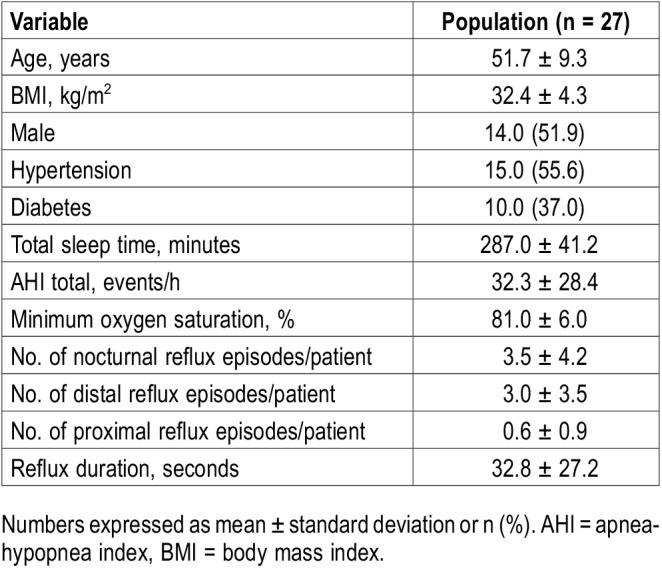
A total of 112 patients with LPR (RSI = 16 ± 2 and RFS = 12 ± 3) and suspected OSA were selected for evaluation. However, 39 were excluded because they were smokers, 8 because they abused alcohol, 1 had undergone esophageal surgery, 8 had acute rhinosinusitis, 5 could not discontinue their reflux treatment, and 5 had a BMI above 40 kg/m2 (Figure 1). Therefore, 46 patients underwent PSG concomitant to MII. In addition, 19 of the 46 patients were excluded because they did not have OSA (n = 3) and 16 because they did not have any proximal or distal reflux episode during the PSG. Therefore, the final analysis consisted of 27 patients. The population studied included a balanced number of males and females who were on average overweight (Table 1).
Figure 1. Flow chart of patient evaluation.
BMI = body mass index, MII = multichannel intraluminal impedance-pH esophageal monitoring, PSG = polysomnography.
Table 1.
Demographic, sleep, and reflux characteristics of the population.
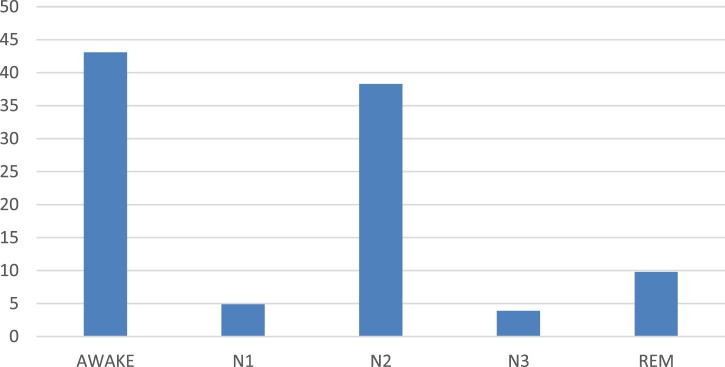
A total of 102 reflux episodes were observed during the sleep studies. Most of the reflux episodes were liquid in composition (80.4%), and the remaining 19.6% were a mix of liquid and gas. Seventy-seven reflux episodes (94.6%) were distal and 15 (5.4%) were proximal. In relation to chemical characteristics of the refluxate, 10.5% were nonacidic, 41.5% were acidic, and 48% were weakly acidic. Almost half of the reflux episodes occurred during awake periods (43.1%), followed by stages N2 (38.3%), R (9.8%), N1 (4.9%), and N3 (3.9%) (Figure 2). Only five reflux episodes (4.9%) occurred during a respiratory obstructive event.
Figure 2. Distribution of laryngopharyngeal reflux events and sleep stages (%).
REM = rapid eye movement.
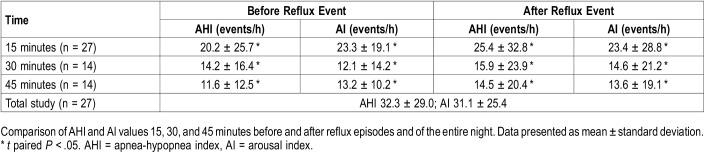
The analysis of the AHI 15 minutes before and after the reflux episode was possible in all 27 patients. The analysis of the AHI 30 and 45 minutes before and after the reflux episode were studied in only 14 patients because of overlap of other reflux episodes. The AHI and arousal index 15, 30, and 45 minutes before and after reflux episodes were lower than the total AHI and arousal index, respectively (Table 2). Total sleep time did not influence the results.
Table 2.
Comparison of AHI and AI values.
DISCUSSION
In the current study, we found no evidence of temporal correlation between reflux episodes and episodes of obstructive events. First, among a carefully selected group of patients with well-established LPR and OSA, 43.1% of the reflux episodes documented during PSG occurred during the awake period. Second, only five reflux episodes (4.9%) occurred during an obstructive respiratory event. Our study findings are consistent with those from Kuribayashi et al,11 who reported that episodes of reflux occurred more often during arousal rather than during apnea. Finally, the number of respiratory events evaluated by the AHI was not higher before the episodes of reflux episodes; nor was arousal index. Conversely, reflux episodes did not increase the subsequent frequency of respiratory events. Suzuki et al25 showed that arousal-related lower esophageal sphincter relaxation may be the main mechanism of reflux in patients with mild to moderate OSA.
Our main hypothesis was that among patients with well-established LPR and OSA, episodes of LPR would occur during obstructive events. We also tested the hypothesis that a sequence of respiratory obstructive events would predispose a reflux episode. The theory that apnea increases intrathoracic pressure gradients and awakenings, which in turn facilitate LES relaxation and reflux,10,11,19,36–41 is not supported by our data. In this case series of patients with well-established LPR and OSA, 43.1% of reflux episodes occurred while awake. It was also surprising that only a small number of the reflux episodes (4.9%) occurred during respiratory events. Finally, we observed no temporal relationship between the frequency of respiratory events and episodes of reflux. The AHI before reflux episodes was not higher than the AHI of the total study. Our second hypothesis was that a reflux episode could increase the frequency of respiratory events after its occurrence reflux due to local inflammation and edema of the upper airway. The laryngopharyngeal inflammation secondary to contact with the refluxate may cause reduction in upper airway patency and alters local reflexive responses.10,12 This hypothesis was also not supported by our data because AHI after reflux episodes was not higher than AHI of total study. This observation, however, does not discount the possibility that the consequences of the refluxate are chronic conditions, contributing to worsening OSA severity.
There is a limited number of studies that evaluated the temporal association between gastroesophageal reflux and OSA that are mostly composed of small series with different methodologies and variable inclusion criteria.11,19,22,38–42 To our knowledge, there is just one study in the literature that studied temporal correlation between LPR and OSA using gold-standard methods for both diseases—pH impedanciometry and PSG.11 This study also did not find a temporal association between laryngopharyngeal reflux and apnea.11
In our study we performed concomitant evaluation of both reflux and apnea during a continuous period (15, 30, and 45 minutes). We also used gold-standard diagnostic methods to diagnose and monitor OSA and episodes of reflux (PSG and MII). The absence of increased episodes of reflux triggered by exaggerated negative intrathoracic pressure during obstructive events may be explained by a concomitant protective effect mechanism. Kuribayashi et al11 showed that end-inspiratory upper esophageal sphincter and gastroesophageal junction pressures progressively increase during OSA, and at the end of OSA events were significantly higher than at the beginning. It was concluded that despite a decrease in esophageal body pressure during OSA events, compensatory changes in upper esophageal sphincter and gastroesophageal junction pressures may prevent reflux.
Our study has some limitations. The fixed cutoff time periods of the current design may not have allowed an accurate analysis of what takes place dynamically in the airway and digestive tract over time. Ideally, longer periods of observation should be established, but this was not possible in the current study because of the overlap in reflux episodes. Another limitation of this study is the relatively small sample size, which did not allow us to study episodes of reflux in REM sleep. Future studies with larger series and rigid design are necessary to better clarify the factors leading to the temporal association found between reflux and respiratory events.
DISCLOSURE STATEMENT
All authors have seen and approved this manuscript. This study was supported by a grant from the São Paulo State Research Aid Foundation (FAPESP#2010/161172-7). Work for this study was performed at Department of Otolaryngology – Santa Casa São Paulo. The authors report no conflicts of interest.
ABBREVATIONS
- AHI
apnea-hypopnea index
- BMI
body mass index
- LPR
laryngopharyngeal reflux
- LES
lower esophageal sphincter
- MII
multichannel intraluminal impedance-pH esophageal monitoring
- OSA
obstructive sleep apnea
- PSG
polysomnography
- RSI
reflux symptom index
- RFS
reflux finding score
REFERENCES
- 1.Berry RB, Budhiraja R, Gottlieb DJ, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8(5):597–619. doi: 10.5664/jcsm.2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Young T, Shahar E, Nieto FJ, et al. Predictors of sleep-disordered breathing in community-dwelling adults: the Sleep Heart Health Study. Arch Intern Med. 2002;162(8):893–900. doi: 10.1001/archinte.162.8.893. [DOI] [PubMed] [Google Scholar]
- 3.Durán J, Esnaola S, Rubio R, Iztueta A. Obstructive sleep apnea-hypopnea and related clinical features in a population-based sample of subjects aged 30 to 70 yr. Am J Respir Crit Care Med. 2001;163(3 Pt 1):685–689. doi: 10.1164/ajrccm.163.3.2005065. [DOI] [PubMed] [Google Scholar]
- 4.Bixler EO, Vgontzas AN, Ten Have T, Tyson K, Kales A. Effects of age on sleep apnea in men. I. Prevalence and severity. Am J Respir Crit Care Med. 1998;157(1):144–148. doi: 10.1164/ajrccm.157.1.9706079. [DOI] [PubMed] [Google Scholar]
- 5.Punjabi NM, Ahmed MM, Polotsky VY, Beamer BA, O’Donnell CP. Sleep-disordered breathing, glucose intolerance, and insulin resistance. Respir Physiol Neurobiol. 2003;136(2-3):167–178. doi: 10.1016/s1569-9048(03)00079-x. [DOI] [PubMed] [Google Scholar]
- 6.Peppard PE, Young T, Palta M, et al. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000;342(19):1378–1384. doi: 10.1056/NEJM200005113421901. [DOI] [PubMed] [Google Scholar]
- 7.Young T, Finn L, Peppard PE, et al. Sleep disordered breathing and mortality: eighteen-year follow up of the Wisconsin sleep cohort. Sleep. 2008;31(8):1071–1078. [PMC free article] [PubMed] [Google Scholar]
- 8.Shah NA, Yaggi HK, Concato J, et al. Obstructive sleep apnea as a risk factor for coronary events or cardiovascular death. Sleep Breath. 2010;14(2):131–136. doi: 10.1007/s11325-009-0298-7. [DOI] [PubMed] [Google Scholar]
- 9.Wang X, Ouyang Y, Wang Z, Zhao G, Liu L, Bi Y. Obstructive sleep apnea and risk of cardiovascular disease and all-cause mortality: a meta-analysis of prospective cohort studies. Int J Cardiol. 2013;169(3):207–214. doi: 10.1016/j.ijcard.2013.08.088. [DOI] [PubMed] [Google Scholar]
- 10.Eskiizmir G, Kezirian E. Is there a vicious cycle between obstructive sleep apnea and laryngopharyngeal reflux disease? Med Hypotheses. 2009;73(5):706–708. doi: 10.1016/j.mehy.2009.04.042. [DOI] [PubMed] [Google Scholar]
- 11.Kuribayashi S, Massey BT, Hafeezullah L, et al. Upper esophageal sphincter and gastroesophageal junction pressure changes act to prevent gastroesophageal and esophagopharyngeal reflux during apneic episodes in patients with obstructive sleep apnea. Chest. 2010;137(4):769–776. doi: 10.1378/chest.09-0913. [DOI] [PubMed] [Google Scholar]
- 12.Karkos P, Leong S, Benton J, Sastry A, Assimakopoulos D, Issing W. Reflux and sleeping disorders: a systematic review. J Laryngol Otol. 2009;123(4):372–374. doi: 10.1017/S0022215109004976. [DOI] [PubMed] [Google Scholar]
- 13.Kim SJ, Kim HY, Jeong JI, Hong SD, Chung SK, Dhong HJ. Changes in the reflux symptom index after multilevel surgery for obstructive sleep apnea. Clin Exp Otorhinolaryngol. 2017;10(3):259–264. doi: 10.21053/ceo.2017.00052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Elhennawi DM, Ahmed MR, Abou-Halawa AS. Correlation of obstructive sleep apnea and laryngopharyngeal reflux: phmetry study. Clin Otolaryngol. 2016;41(6):758–761. doi: 10.1111/coa.12640. [DOI] [PubMed] [Google Scholar]
- 15.Qu Y, Ye JY, Han DM, et al. Esophageal functional changes in obstructive sleep apnea/hypopnea syndrome and their impact on laryngopharyngeal reflux disease. Chin Med J (Engl) 2015;128(16):2162–2167. doi: 10.4103/0366-6999.162506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee JS, Heo SJ, Kim JS, Ahn D, Sohn JH, Kim H. Relationship between the severity of laryngopharyngeal reflux and sleep apnea: using drug-induced sleep endoscopy (DISE) Eur Arch Otorhinolaryngol. 2018;275(1):219–224. doi: 10.1007/s00405-017-4812-4. [DOI] [PubMed] [Google Scholar]
- 17.Veale D, Poussin G, Benes F, Pepin JL, Levy P. Identification of quality of life concerns of patients with obstructive sleep apnea at the time of initiation of continuous positive airway pressure: a discourse analysis. Qual Life Res. 2002;11(4):389–399. doi: 10.1023/a:1015599326110. [DOI] [PubMed] [Google Scholar]
- 18.Carrau RL, Khidr A, Crawley JA, Hillson EM, Davis JK, Pashos CL. The impact of laryngopharyngeal reflux on patient-reported quality of life. Laryngoscope. 2004;114(4):670–674. doi: 10.1097/00005537-200404000-00014. [DOI] [PubMed] [Google Scholar]
- 19.Ing A, Ngu M, Breslin A. Obstructive sleep apnea and gastroesophageal reflux. Am J Med. 2000;108(Suppl 4a):120S–125S. doi: 10.1016/s0002-9343(99)00350-2. [DOI] [PubMed] [Google Scholar]
- 20.Bortolotti M, Gentilini L, Morselli C, Giovannini M. Obstructive sleep apnea is improved by a prolonged treatment of gastro-esophageal reflux with omeprazole. Dig Liver Dis. 2006;38(2):78–81. doi: 10.1016/j.dld.2005.09.018. [DOI] [PubMed] [Google Scholar]
- 21.Kerr P, Shoenut J, Millar T, Buckle P, Kryger M. Nasal CPAP reduces gastroesophageal reflux in obstructive sleep apnea syndrome. Chest. 1992;101(6):1539–1544. doi: 10.1378/chest.101.6.1539. [DOI] [PubMed] [Google Scholar]
- 22.Jecker P, Rassouli S, Selivanova O, Lippold W, Mann WJ. [No correlation between reflux of gastric contents and obstructive sleep apnea] HNO. 2008;56(11):1122–1128. doi: 10.1007/s00106-008-1733-y. [DOI] [PubMed] [Google Scholar]
- 23.Erdem D, Yilmaz YF, Ozcan M, Titiz A, Ozlugedik S, Unal A. Correlation of sleep-disordered breathing and laryngopharyngeal reflux: a two-channel triple-sensor pHmetry catheter study. Eur Arch Otorhinolaryngol. 2018;275(10):2585–2592. doi: 10.1007/s00405-018-5107-0. [DOI] [PubMed] [Google Scholar]
- 24.Eryilmaz A, Erisen L, Demir UL, et al. Management of patients with coexisting obstructive sleep apnea and laryngopharyngeal reflux disease. Eur Arch Otorhinolaryngol. 2012;269(12):2575–2580. doi: 10.1007/s00405-012-2062-z. [DOI] [PubMed] [Google Scholar]
- 25.Suzuki M, Saigusa H, Kurogi R, et al. Arousals in obstructive sleep apnea patients with laryngopharyngeal and gastroesophageal reflux. Sleep Med. 2010;11(4):356–360. doi: 10.1016/j.sleep.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 26.Wang CC, Lien HC, De Virgilio A, et al. Airway pH monitoring in patients with suspected obstructive sleep apnoea using the Dx-pH oropharyngeal probe: preliminary report of a prospective cohort study. Clin Otolaryngol. 2014;39(6):352–358. doi: 10.1111/coa.12297. [DOI] [PubMed] [Google Scholar]
- 27.Belafsky PC, Postma GN, Koufman JA. Validity and reliability of the reflux symptom index (RSI) J Voice. 2002;16(2):274–277. doi: 10.1016/s0892-1997(02)00097-8. [DOI] [PubMed] [Google Scholar]
- 28.Belafsky P, Postma G, Koufman J. The validity and reliability of the reflux finding score (RFS) Laryngoscope. 2001;111(8):1313–1317. doi: 10.1097/00005537-200108000-00001. [DOI] [PubMed] [Google Scholar]
- 29.Lundell L, Dent J, Bennett J, Blum A, Armstrong D, Galmiche J. Endoscopic assessment of esophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999;45(2):172–180. doi: 10.1136/gut.45.2.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999;131(7):485–491. doi: 10.7326/0003-4819-131-7-199910050-00002. [DOI] [PubMed] [Google Scholar]
- 31.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 32.Iber C, Ancoli-Israel S, Chesson AL, Jr, Quan SF, for the American Academy of Sleep Medicine . The AASM Manual for the Scoring of the Sleep and Associated Events: Rules, Terminology and Technical Specifications. 1st ed. Westchester, IL: American Academy of Sleep Medicine; 2007. [Google Scholar]
- 33.Rechtschaffen A, Kales A. A Manual of Standardized Terminology Techniques and Scoring System for Sleep Stages of Human Subjects. Public Health Service Publication No. 204 Washington, DC: US Government Printing Office; 1968. [Google Scholar]
- 34.Lee B, Kim G, Ryu D, et al. Combined dual channel impedance/pH-metry in patients with suspected laryngopharyngeal reflux. J Neurogastroenterol Motil. 2010;16(2):157–165. doi: 10.5056/jnm.2010.16.2.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Eiseman NA, Westover MB, Ellenbogen JM, Bianchi MT. The impact of body posture and sleep stages on sleep apnea severity in adults. J Clin Sleep Med. 2012;8(6):655–666. doi: 10.5664/jcsm.2258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shepherd KL, James AL, Musk AW, Hunter ML, Hillman DR, Eastwood PR. Gastro-esophageal reflux symptoms are related to the presence and severity of obstructive sleep apnea. J Sleep Res. 2011;20(1 Pt 2):241–249. doi: 10.1111/j.1365-2869.2010.00843.x. [DOI] [PubMed] [Google Scholar]
- 37.Kim H, Vorona R, Winn M, Doviak M, Johnson D, Ware J. Symptoms of gastro-esophageal reflux disease and the severity of obstructive sleep apnea syndrome are not related in sleep disorders center patients. Aliment Pharmacol Ther. 2005;21(9):1127–1133. doi: 10.1111/j.1365-2036.2005.02447.x. [DOI] [PubMed] [Google Scholar]
- 38.Graf K, Karaus M, Heinemann S, Körber S, Dorow P, Hampel K. Gastroesophageal reflux in patients with sleep apnea syndrome. Z Gastroenterol. 1995;33(12):689–693. [PubMed] [Google Scholar]
- 39.Penzel T, Becker H, Brandenburg U, Labunski T, Pankow W, Peter J. Arousal in patients with gastro-esophageal reflux and sleep apnea. Eur Respir J. 1999;14(6):1266–1270. doi: 10.1183/09031936.99.14612669. [DOI] [PubMed] [Google Scholar]
- 40.Berg S, Hoffstein V, Gislason T. Acidification of distal esophagus and sleep-related breathing disturbances. Chest. 2004;125(6):2101–2106. doi: 10.1378/chest.125.6.2101. [DOI] [PubMed] [Google Scholar]
- 41.Oztürk O, Oztürk L, Ozdogan A, Oktem F, Pelin Z. Variables affecting the occurrence of gastroesophageal reflux in obstructive sleep apnea patients. Eur Arch Otorhinolaryngol. 2004;261(4):229–232. doi: 10.1007/s00405-003-0658-z. [DOI] [PubMed] [Google Scholar]
- 42.Tardif C, Denis P, Verdure-Poussin A, Hidden F, Pasquis P, Samson-Dollfus D. Gastroesophageal reflux during sleep in obese patients. Neurophysiol Clin. 1988;18(4):323–332. doi: 10.1016/s0987-7053(88)80089-3. [DOI] [PubMed] [Google Scholar]