Abstract
Background
Runt-related transcription factor 1 (RUNX1) was previously reported to play a dual role in promoting or suppressing tumorigenesis in various malignancies. A public dataset from The Cancer Genome Atlas (TCGA) was used to evaluate the role of RUNX1 in clear cell renal cell carcinoma (ccRCC).
Methods
The Wilcoxon signed-rank test was used to compare the expression of RUNX1 in ccRCC tissues and normal tissues. The Wilcoxon signed-rank test and logistic regression were utilized to investigate the relationship between clinicopathological factors and RUNX1 expression. Additionally, we analysed the differences in prognosis between patients with high and low expression of RUNX1 via the Kaplan–Meier method and Cox regression. Gene set enrichment analysis (GSEA) was performed to explore the mechanisms of RUNX1 in ccRCC.
Results
The expression of RUNX1 in ccRCC tissues was significantly higher than that in normal tissues. High expression of RUNX1 was significantly associated with gender (p = 0.003), clinical stage (p < 0.001), tissue infiltration (p < 0.001), lymph node metastasis (p = 0.037) and histological grade (p < 0.001). Logistic regression analysis showed that high RUNX1 expression was significantly correlated with gender (OR = 1.71 for male vs. female, p = 0.004), histological grade (OR = 11.61 for grade IV vs. I, p < 0.001), clinical stage (OR = 1.55 for stage III/IV vs. I/II, p = 0.014) and tissue infiltration (OR = 1.54 for positive vs. negative, p = 0.018). Kaplan–Meier survival curves revealed that the prognosis of patients with ccRCC with high RUNX1 expression was worse than that of patients with ccRCC with low RUNX1 expression (p < 0.001). Univariate Cox regression analysis showed that high RUNX1 expression was strongly correlated with poor prognosis (HR = 1.60, 95% CI [1.31–1.97], p < 0.001). In addition, high expression of RUNX1 was an independent prognostic factor for poor overall survival (OS), with an HR of 1.50 (95% CI [1.20–1.87], p < 0.001) in multivariate Cox analysis. GSEA showed that the apoptosis, B cell receptor signalling pathway, calcium signalling pathway, chemokine signalling pathway, JAK/STAT signalling pathway, MAPK signalling pathway, p53 signalling pathway, pathways in cancer, T cell receptor signalling pathway, Toll-like receptor signalling pathway, VEGF signalling pathway, and Wnt signalling pathway were significantly enriched in the RUNX1 high-expression phenotype. In conclusion, RUNX1 can be used as a novel prognostic factor and therapeutic target in ccRCC.
Keywords: Clear cell renal cell carcinoma, RUNX1, Prognosis, GSEA, TCGA
Introduction
Renal cell carcinoma (RCC) accounts for nearly 85% of primary renal carcinomas, and in the United States, approximately 63,000 new cases and nearly 14,000 deaths occur each year (Garfield & LaGrange, 2019). The most common pathological type of RCC is clear cell RCC (ccRCC), which accounts for approximately 70–75% of cases (Shuch et al., 2015). However, 30% of patients with ccRCC are diagnosed with advanced cancer (Karakiewicz et al., 2007). The optimal treatment for localized ccRCC is radical resection, but the therapies available for advanced cancer with metastasis are not very effective. Currently, targeted therapy has become a promising strategy. Therefore, the identification of hub genes associated with ccRCC is important for targeted therapy.
Runt-related transcription factor 1 (RUNX1) is widely considered the master regulator of haematopoiesis that mediates endothelial-to-haematopoietic transition (EHT) and the homeostasis of haematopoietic stem and progenitor cells (HSPCs) (Yzaguirre, De Bruijn & Speck, 2017; Yzaguirre et al., 2018; Cheng et al., 2017). The results of increasing studies imply that RUNX1 has contrasting effects of promoting or suppressing tumorigenesis in various malignancies. For example, upregulation of RUNX1 led to the increased expression of SOS1 and phosphorylation of ErbB2/HER2, subsequently promoting the proliferation of gastric cancer cells (Mitsuda et al., 2018). In the ER+ subtype of breast cancer, RUNX1 has been implicated as a tumour suppressor through the stabilization of Axis inhibition protein 1 (AXIN1) expression, but high RUNX1 expression correlates with poor prognosis in triple-negative breast cancers (Mercado-Matos, Matthew-Onabanjo & Shaw, 2017; Chimge et al., 2016). Additionally, loss of RUNX1 resulted in enhanced proliferation, migration, and invasion in lung cancer (Ramsey et al., 2018). Recently, the literature in ccRCC reported the upregulation of RUNX1- RUNX1 partner transcriptional co-repressor 1 (RUNX1-RUNX1T1) gene signatures, the fusion transcript between the RUNX1 gene and the RUNX1T1 locus because of t(8;21)(q22;q22) (Metzeler & Bloomfield, 2017), which was revealed by RNA sequencing (Xiong et al., 2014). However, the relationship between RUNX1 and the prognosis of ccRCC is unknown.
Therefore, we assessed RUNX1 expression in ccRCC and evaluated the correlation between RUNX1 expression and the prognosis of ccRCC using the public dataset from The Cancer Genome Atlas (TCGA). GSEA was performed to explore the mechanisms of RUNX1 in ccRCC.
Materials and Methods
Basic patient information
The mRNA expression data and the corresponding clinical data of ccRCC patients were obtained from the official website of The Cancer Genome Atlas (TCGA). After excluding normal sample data, boxplots were used to analyse the relationship between RUNX1 expression and various clinical variables. Ultimately, we included 537 ccRCC patients with RUNX1 mRNA expression data and clinical data (Table 1).
Table 1. Characteristics of clear cell renal cell carcinoma patients in the TCGA database.
| Clinical characteristics | Total (n = 537) | % | |
|---|---|---|---|
| Age at diagnosis (years) | 61 (26–90) | ||
| Gender | Female | 191 | 35.6 |
| Male | 346 | 64.4 | |
| Histological grade | I | 14 | 2.6 |
| II | 230 | 43.5 | |
| III | 207 | 39.2 | |
| IV | 78 | 14.7 | |
| Stage | I | 269 | 50.3 |
| II | 57 | 10.7 | |
| III | 125 | 23.4 | |
| IV | 83 | 15.6 | |
| Tissue infiltrationa | Negative | 344 | 64.1 |
| Positive | 193 | 35.9 | |
| Lymph node metastasisb | Negative | 240 | 93.3 |
| Positive | 17 | 6.7 | |
| Distant metastasisc | Negative | 426 | 84.3 |
| Positive | 79 | 15.7 |
Notes.
Positive indicates tissue infiltration and negative indicates no tissue infiltration.
Positive indicates lymph node metastasis and negative indicates no lymph node metastasis.
Positive indicates distant metastasis and negative indicates no distant metastasis.
Gene set enrichment analysis (GSEA)
GSEA was utilized to explore the mechanisms of RUNX1 in ccRCC. In this study, the “c2.cp.kegg.v6.2.symbols.gmt” gene sets from the Molecular Signatures Database (MSigDB) were analysed using GSEA 3.0 software. To obtain normalized enrichment scores (NESs), the nominal p-value and false discovery rate (FDR) q-value were determined, the number of gene set permutations for each analysis was set at 1,000, and the phenotype label was the expression level of RUNX1. Gene sets with a nominal p-value of <0.05 and an FDR q-value of <0.25 were considered significantly enriched gene sets.
Statistical analysis
The median value of RUNX1 expression was considered as the cut-off value. The Wilcoxon signed-rank test was used to compare the expression of RUNX1 in ccRCC tissues with that in normal tissues. The Wilcoxon signed-rank test and logistic regression were utilized to investigate the relationship between clinicopathological factors and RUNX1. The correlation between RUNX1 expression and overall survival (OS) was estimated using Kaplan–Meier survival curves. Univariate Cox regression analysis was used to calculate the association of clinicopathological characteristics and RUNX1 expression with OS, and multivariate Cox analysis was carried out for further analysis. All statistical analyses were performed using R 3.5.3 software (R Core Team, 2018).
Results
Patient characteristics
A total of 537 primary tumours with both gene expression and clinical data were downloaded from TCGA ccRCC data in May 2019. In our study cohort, the median age was 63 years (range, 26–90 years). Histological grades I, II, III, and IV accounted for 2.6%, 43.5%, 39.2%, and 14.7% of the cases, respectively. Stages I, II, III and IV accounted for 50.3%, 10.7%, 23.4% and 15.6% of the cases, respectively. A total of 193 of the 537 (35.9%) cases had tissue infiltration. A total of 17 of 257 (6.7%) cases had lymph node metastasis, and 79 of 505 (6.7%) cases had distant metastasis (Table 1).
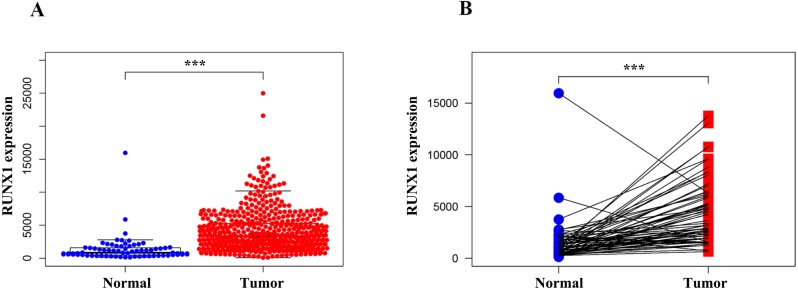
RUNX1 was highly expressed in ccRCC tissues
We compared the expression of RUNX1 in 539 ccRCC tissues and 72 normal tissues using the Wilcoxon signed-rank test. The expression of RUNX1 in ccRCC tissues was significantly higher than that in normal tissues (p < 0.001) (Fig. 1A). In addition, RUNX1 was also obviously overexpressed in the ccRCC tissues relative to its expression in the 72 paired normal tissues (p < 0.001) (Fig. 1B).
Figure 1. Comparison of RUNX1 expression between ccRCC tissues and normal tissues.
The Wilcoxon signed-rank test was used to compare the mRNA expression of RUNX1 in ccRCC tissues and normal tissues obtained from the TCGA database. (A) The expression of RUNX1 in ccRCC tissues (n = 539) was significantly higher than that in normal tissues (n = 72). (B) Compared with 72 paired normal tissues, ccRCC tissues exhibited obvious overexpression of RUNX1. RUNX1, Runt-related transcription factor 1; ccRCC, clear cell renal cell carcinoma; TCGA, The Cancer Genome Atlas ; *, p < 0.05 ; **, p < 0.01; ***, p < 0.001.
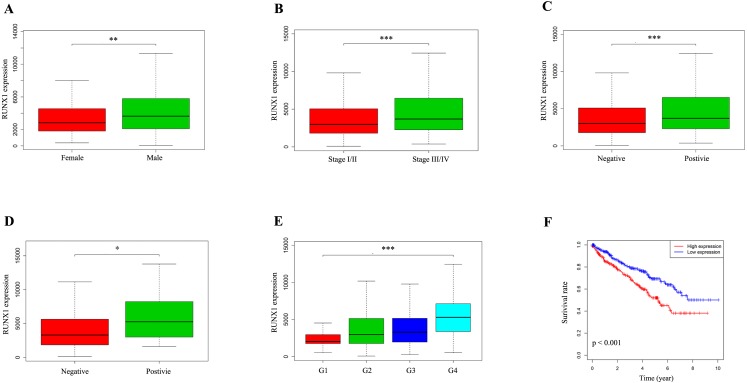
The expression of RUNX1 and its association with clinicopathological variables
We used the Wilcoxon signed-rank test to analyse 537 ccRCC samples from the TCGA database with both RUNX1 expression data and clinical data. The median value of RUNX1 expression was considered as the cut-off value. As shown in Figs. 2A–2E, high expression of RUNX1 was significantly associated with gender (p = 0.003), clinical stage (p < 0.001), tissue infiltration (p < 0.001), lymph node metastasis (p = 0.037) and histological grade (p < 0.001). The logistic regression analysis results showed that high RUNX1 expression was significantly correlated with gender (odds ratio [OR] = 1.71 for male vs. female, p = 0.004), histologic grade (OR = 11.61 for grade IV vs. I, p < 0.001), stage (OR = 1.55 for stage III/IV vs. I/II, p = 0.014) and tissue infiltration (OR = 1.54 for positive vs. negative, p = 0.018) (Table 2).
Figure 2. The expression of RUNX1 and its association with clinicopathologic variables.
The median value of RUNX1 expression was considered as the cut-off value. The Wilcoxon signed-rank test was utilized to investigate the relationship between clinicopathological factors and the expression of RUNX1 in 537 ccRCC tissues. The correlation between RUNX1 expression and overall survival (OS) was estimated using Kaplan–Meier survival curves. (A) Gender, (B) clinical stage, (C) tissue infiltration, (D) lymph node metastasis, (E) histological grade and (F) Kaplan–Meier survival curves showed that the prognosis of patients with ccRCC with high RUNX1 expression was worse than that of patients with ccRCC with low RUNX1 expression. In (C), positive indicates tissue infiltration and negative indicates no tissue infiltration. In (D), positive indicates lymph node metastasis and negative indicates no lymph node metastasis. RUNX1, Runt-related transcription factor 1; ccRCC, clear cell renal cell carcinoma; *, p < 0.05; **, p < 0.01; ***, p < 0.001.
Table 2. Association of RUNX1 expressiona with clinicopathological characteristics (logistic regression analysis).
| Clinical characteristics | Total (N) | Odds ratio for RUNX1 expression | p-value |
|---|---|---|---|
| Age (continuous) | 537 | 0.99 (0.98–1.01) | 0.659 |
| Gender (male vs. female) | 537 | 1.71 (1.19–2.45) | 0.004 |
| Grade (IV vs. I) | 92 | 11.61 (3.22–55.67) | 0.000 |
| Stage (III/IV vs. I/II) | 527 | 1.55 (1.09–2.21) | 0.014 |
| Distant metastasis (positive vs. negative)b | 505 | 1.36 (0.84–2.21) | 0.219 |
| Tissue infiltration (positive vs. negative)c | 537 | 1.54 (1.07–2.19) | 0.018 |
| Lymph node metastasis (positive vs. negative)d | 257 | 1.73 (0.63–5.24) | 0.299 |
Notes.
Categorical dependent variable, greater or less than the median expression level.
Positive indicates distant metastasis and negative indicates no distant metastasis.
Positive indicates tissue infiltration and negative indicates no tissue infiltration.
Positive indicates lymph node metastasis and negative indicates no lymph node metastasis.
Survival outcomes and Cox regression analyses
Kaplan–Meier survival curves revealed that the prognosis of patients with ccRCC with high RUNX1 expression was worse than that of patients with ccRCC with low RUNX1 expression (p < 0.001) (Fig. 2F). The univariate Cox regression analysis results showed that high RUNX1 expression was strongly correlated with poor prognosis (hazard ratio [HR] = 1.60, 95% confidence interval CI [1.31–1.97], p < 0.001; Table 3A). Other clinical variables, such as age, grade, stage, distant metastasis, tissue infiltration and lymph node metastasis, were found to have an impact on OS (all p values <0.05). Moreover, in multivariate analysis, high expression of RUNX1 (HR =1.50, 95% CI [1.20–1.87], p < 0.001), age (HR =1.03, 95% CI [1.01–1.05], p = 0.002) and distant metastasis (HR =2.42, 95% CI [1.14–5.16], p = 0.022) still implied a poor prognosis (Table 3A). These results indicate that the expression of RUNX1 is an independent factor and that increased RUNX1 levels are associated with poor OS.
Table 3. Association with overall survival and clinicopathological characteristics in patients from the TCGA database using Cox regression.
(A) Univariate Cox regression (B) Multivariate Cox regression.
| Clinicopathological variables | Hazard ratio (95% CI) | p-value |
|---|---|---|
| (A) | ||
| Age (continuous) | 1.02 (1.00–1.04) | 0.012 |
| Gender (male vs. female) | 1.01 (0.67–1.54) | 0.951 |
| RUNX1 expression (high vs. low) | 1.60 (1.31–1.97) | 0.000 |
| Grade | 2.24 (1.68–2.99) | 0.000 |
| Stage | 1.86 (1.54–2.25) | 0.000 |
| Distant metastasis (positive vs. negative)a | 4.07 (2.63–6.30) | 0.000 |
| Tissue infiltration (positive vs. negative)b | 3.31 (2.17–5.06) | 0.000 |
| Lymph node metastasis (positive vs. negative)c | 2.93 (1.52–5.67) | 0.001 |
| (B) | ||
| Age (continuous) | 1.03 (1.01–1.05) | 0.002 |
| RUNX1 expression (high vs. low) | 1.50 (1.20–1.87) | 0.000 |
| Distant metastasis (positive vs. negative) | 2.42 (1.14–5.16) | 0.022 |
Notes.
Positive indicates distant metastasis and negative indicates no distant metastasis.
Positive indicates tissue infiltration and negative indicates no tissue infiltration.
Positive indicates lymph node metastasis and negative indicates no lymph node metastasis.
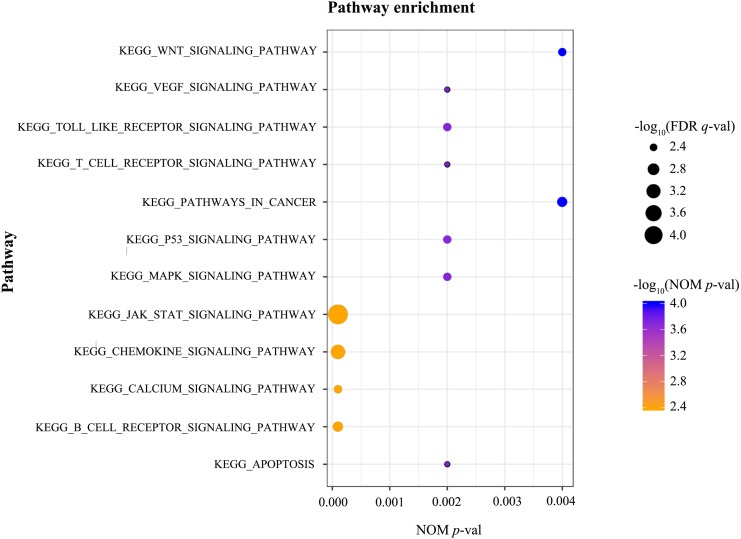
GSEA
GSEA was conducted to identify the differentially activated signalling pathways in the high RUNX1 expression ccRCC data sets. The results shown in Table 4 and Fig. 3 revealed the most significant signalling pathways enriched in the RUNX1 high-expression phenotype.
Table 4. Gene sets enriched in the high-expression phenotype.
| Gene set name | NES | NOM p-val | FDR q-val |
|---|---|---|---|
| KEGG_APOPTOSIS | 1.970 | 0.002 | 0.005 |
| KEGG_B_CELL_RECEPTOR_SIGNALING_PATHWAY | 2.069 | 0.000 | 0.003 |
| KEGG_CALCIUM_SIGNALING_PATHWAY | 2.021 | 0.000 | 0.004 |
| KEGG_CHEMOKINE_SIGNALING_PATHWAY | 2.145 | 0.000 | 0.001 |
| KEGG_JAK_STAT_SIGNALING_PATHWAY | 2.242 | 0.000 | 0.000 |
| KEGG_MAPK_SIGNALING_PATHWAY | 1.997 | 0.002 | 0.004 |
| KEGG_P53_SIGNALING_PATHWAY | 2.022 | 0.002 | 0.004 |
| KEGG_PATHWAYS_IN_CANCER | 2.075 | 0.004 | 0.003 |
| KEGG_T_CELL_RECEPTOR_SIGNALING_PATHWAY | 1.973 | 0.002 | 0.005 |
| KEGG_TOLL_LIKE_RECEPTOR_SIGNALING_PATHWAY | 2.007 | 0.002 | 0.004 |
| KEGG_VEGF_SIGNALING_PATHWAY | 1.966 | 0.002 | 0.005 |
| KEGG_WNT_SIGNALING_PATHWAY | 2.009 | 0.004 | 0.004 |
Notes.
- NES
- normalized enrichment score
- NOM
- nominal;
- FDR
- false discovery rate
Gene sets with NOM p-val <0.05 and FDR q-val <0.25 were considered significant.
Figure 3. GSEA.
GSEA was conducted to identify the differentially activated signalling pathways in the high RUNX1 expression ccRCC data sets. GESA showed that the apoptosis, the B cell receptor signalling pathway, the Calcium signalling pathway, the chemokine signalling pathway, the JAK/STAT signalling pathway, the MAPK signalling pathway, the p53 signalling pathway, pathways in cancer, the T cell receptor signalling pathway, the Toll-like receptor signalling pathway, the VEGF signalling pathway, and the Wnt signalling pathway were significantly enriched in the RUNX1 high-expression phenotype. GSEA, gene set enrichment analysis; RUNX1, Runt-related transcription factor 1; ccRCC, clear cell renal cell carcinoma; NOM p-val, nominal p-value ; FDR q-val, false discovery rate q-value.
Discussion
RUNX1, located on chromosome 21q22.3, consists of 12 exons with two distinct promoters and modulates the transcription of its target genes by affecting the DNA binding capacity (De Braekeleer et al., 2011; Mitsuda et al., 2018; Liu et al., 2019). Researchers have demonstrated differential expression of RUNX1 in several cancers, and deregulation of RUNX1 correlates with tumour progression, which could ultimately lead to its dual role. For example, the expression of RUNX1 in hepatocellular carcinoma tissues is much lower than that in adjacent normal tissues and adjacent cirrhotic tissues (Miyagawa et al., 2006). In addition, RUNX1 is overexpressed in non-small cell lung cancer (NSCLC) and promotes the invasion of NSCLC cells (Wang et al., 2015). RUNX1 was also confirmed to be upregulated in endometrial cancer and related to myometrial invasion (Planaguma et al., 2004). Knockdown of RUNX1 inhibited proliferation and apoptosis induced by Leucine-rich-alpha-2-glycoprotein 1 (LRG1) in colorectal cancer cells (Zhou et al., 2017). RUNX1 has been shown to be androgen-dependent, and loss of RUNX1 may contribute to prostate cancer progression (Takayama et al., 2015). Additionally, RUNX1 suppress the growth of several breast cancer cell lines through the repression of cancer stem cell activity and inhibition of zinc finger E-Box binding protein 1 (ZEB1) expression (Hong et al., 2018). However, the effect of RUNX1 expression on the prognosis of RCC, which is the focus of the current study, remains unclear.
Here, we confirmed that the RUNX1 high-expression phenotype was closely correlated with gender, high histological grade, advanced clinical stage, tissue infiltration and poor prognosis. GSEA was performed to further investigate the biological functions of RUNX1 in ccRCC. GESA is one of the most commonly used methods for pathway analysis in tumours. The results of GESA are based on gene sets rather than a single gene, making these results more reliable and flexible than those obtained using traditional methods (Subramanian et al., 2005). However, the approach of GESA, functional class scoring (FCS), has several limitations. FCS analyses each pathway independently and treats differently significant genes equally, which may overlook the biological significance of genes within these pathways and their complex interactions with each other (Khatri, Sirota & Butte, 2012). Additionally, it is difficult to set the appropriate threshold for determining gene sets for pathways with insufficient annotation information, which may lead to the loss of some less significant but still critical genes, resulting in reduced detection sensitivity. GESA showed that apoptosis, the B cell receptor signalling pathway, the calcium signalling pathway, the chemokine signalling pathway, the JAK/STAT signalling pathway, the MAPK signalling pathway, the p53 signalling pathway, pathways in cancer, the T cell receptor signalling pathway, the Toll like receptor signalling pathway, the VEGF signalling pathway, and the Wnt signalling pathway were significantly enriched in the RUNX1 high-expression phenotype. Some of these pathways have been reported in the literature related to other cancers. The distal P1-Runx1 promoter may be important in the onset or progression of leukaemia via Wnt/beta-catenin signalling (Medina et al., 2016). RUNX1 gene silencing induces p53-promoted core binding factor-beta (CBFB) expression, and upregulated CBFB stabilizes RUNX1 expression in acute myeloid leukaemia cells, resulting in a compensatory RUNX1-p53-CBFB feedback loop (Morita et al., 2017). Moreover, IL-1β induces RUNX1 expression through the MAPK signalling pathway and promotes migration, invasion, and angiogenesis in glioblastoma (Sangpairoj et al., 2017). However, the association of RUNX1 with the ccRCC signalling pathways has not been studied. Our findings suggest that RUNX1 can be used as a novel biomarker for predicting poor prognosis and as a therapeutic target in ccRCC, but the underlying mechanisms need to be further elucidated.
Although the current study elaborated on the role of RUNX1 in ccRCC, it still has some limitations. First, the number of tumour tissues in the TCGA database was significantly higher than the number of normal tissues used as a control. Second, specific details, such as the use of drugs, surgical treatment and surgical details, are lacking, and these factors are important for patient prognosis. Finally, the protein levels and direct mechanisms of RUNX1 in ccRCC could not be clearly assessed from the TCGA database. Therefore, further studies on RUNX1 in ccRCC are needed.
Conclusions
The expression of RUNX1 may be associated with poor survival in ccRCC, and the apoptosis, the B cell receptor signalling pathway, the calcium signalling pathway, the chemokine signalling pathway, the JAK/STAT signalling pathway, the MAPK signalling pathway, the p53 signalling pathway, pathways in cancer, the T cell receptor signalling pathway, the Toll-like receptor signalling pathway, the VEGF signalling pathway, and the Wnt signalling pathway may be significantly correlated with RUNX1 expression in ccRCC. The biological role of RUNX1 in ccRCC should be further assessed in future studies.
Supplemental Information
Acknowledgments
We are grateful for the data provided by the TCGA database for this study.
Funding Statement
This work was supported by the Project of Liaoning Distinguished Professor (Grant No. [2012]145), the Shenyang Plan Project of Science and Technology (Grant No. F17-230-9-08), China Medical University’s 2017 Discipline Promotion Program (Grant No. 3110117040), China Medical University’s 2018 Discipline Promotion Program, and the 2017 National Key R&D Program Key Projects of Precision Medical Research (No. 2017YFC0908000). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Contributor Information
Xiaojun Man, Email: manxj1983@163.com.
Chuize Kong, Email: kongchuize_cmu@sina.cn.
Additional Information and Declarations
Competing Interests
The authors declare there are no competing interests.
Author Contributions
Yang Fu conceived and designed the experiments, performed the experiments, analyzed the data, contributed reagents/materials/analysis tools, prepared figures and/or tables, authored or reviewed drafts of the paper, approved the final draft.
Shanshan Sun conceived and designed the experiments, performed the experiments, analyzed the data, prepared figures and/or tables, authored or reviewed drafts of the paper, approved the final draft.
Xiaojun Man conceived and designed the experiments, authored or reviewed drafts of the paper, approved the final draft.
Chuize Kong conceived and designed the experiments, contributed reagents/materials/analysis tools, authored or reviewed drafts of the paper, approved the final draft.
Data Availability
The following information was supplied regarding data availability:
The raw data are available in the Supplemental File.
References
- Cheng et al. (2017).Cheng Y, Yang H, Sun Y, Zhang H, Yu S, Lu Z, Chen J. RUNX1 promote invasiveness in pancreatic ductal adenocarcinoma through regulating miR-93. Oncotarget. 2017;8:99567–99579. doi: 10.18632/oncotarget.20433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chimge et al. (2016).Chimge NO, Little GH, Baniwal SK, Adisetiyo H, Xie Y, Zhang T, O’Laughlin A, Liu ZY, Ulrich P, Martin A, Mhawech-Fauceglia P, Ellis MJ, Tripathy D, Groshen S, Liang C, Li Z, Schones DE, Frenkel B. RUNX1 prevents oestrogen-mediated AXIN1 suppression and beta-catenin activation in ER-positive breast cancer. Nature Communications. 2016;7:10751–10762. doi: 10.1038/ncomms10751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Braekeleer et al. (2011).De Braekeleer E, Douet-Guilbert N, Morel F, Le Bris MJ, Ferec C, De Braekeleer M. RUNX1 translocations and fusion genes in malignant hemopathies. Future Oncology. 2011;7:77–91. doi: 10.2217/fon.10.158. [DOI] [PubMed] [Google Scholar]
- Garfield & LaGrange (2019).Garfield K, LaGrange CA. Cancer, renal cell. Treasure Island: StatPearls Publishing; 2019. [PubMed] [Google Scholar]
- Hong et al. (2018).Hong D, Fritz AJ, Finstad KH, Fitzgerald MP, Weinheimer A, Viens AL, Ramsey J, Stein JL, Lian JB, Stein GS. Suppression of breast cancer stem cells and tumor growth by the RUNX1 transcription factor. Molecular Cancer Research. 2018;16:1952–1964. doi: 10.1158/1541-7786.MCR-18-0135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karakiewicz et al. (2007).Karakiewicz PI, Briganti A, Chun FK, Trinh QD, Perrotte P, Ficarra V, Cindolo L, De la Taille A, Tostain J, Mulders PF, Salomon L, Zigeuner R, Prayer-Galetti T, Chautard D, Valeri A, Lechevallier E, Descotes JL, Lang H, Mejean A, Patard JJ. Multi-institutional validation of a new renal cancer-specific survival nomogram. Journal of Clinical Oncology. 2007;25:1316–1322. doi: 10.1200/JCO.2006.06.1218. [DOI] [PubMed] [Google Scholar]
- Khatri, Sirota & Butte (2012).Khatri P, Sirota M, Butte AJ. Ten years of pathway analysis: current approaches and outstanding challenges. PLOS Computational Biology. 2012;8:e1002375. doi: 10.1371/journal.pcbi.1002375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu et al. (2019).Liu S, Xing Y, Lu W, Li S, Tian Z, Xing H, Tang K, Xu Y, Rao Q, Wang M, Wang J. RUNX1 inhibits proliferation and induces apoptosis of t(8;21) leukemia cells via KLF4 mediated transactivation of P57. Haematologica. 2019;104(8):1597–1607. doi: 10.3324/haematol.2018.192773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medina et al. (2016).Medina MA, Ugarte GD, Vargas MF, Avila ME, Necunir D, Elorza AA, Gutierrez SE, De Ferrari GV. Alternative RUNX1 promoter regulation by Wnt/beta-Catenin signaling in leukemia cells and human hematopoietic progenitors. Journal of Cellular Physiology. 2016;231:1460–1467. doi: 10.1002/jcp.25258. [DOI] [PubMed] [Google Scholar]
- Mercado-Matos, Matthew-Onabanjo & Shaw (2017).Mercado-Matos J, Matthew-Onabanjo AN, Shaw LM. RUNX1 and breast cancer. Oncotarget. 2017;8:36934–36935. doi: 10.18632/oncotarget.17249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metzeler & Bloomfield (2017).Metzeler KH, Bloomfield CD. Clinical relevance of RUNX1 and CBFB alterations in acute myeloid leukemia and other hematological disorders. Advances in Experimental Medicine and Biology. 2017;962:175–199. doi: 10.1007/978-981-10-3233-2_12. [DOI] [PubMed] [Google Scholar]
- Mitsuda et al. (2018).Mitsuda Y, Morita K, Kashiwazaki G, Taniguchi J, Bando T, Obara M, Hirata M, Kataoka TR, Muto M, Kaneda Y, Nakahata T, Liu PP, Adachi S, Sugiyama H, Kamikubo Y. RUNX1 positively regulates the ErbB2/HER2 signaling pathway through modulating SOS1 expression in gastric cancer cells. Scientific Reports. 2018;8:6423. doi: 10.1038/s41598-018-24969-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyagawa et al. (2006).Miyagawa K, Sakakura C, Nakashima S, Yoshikawa T, Kin S, Nakase Y, Ito K, Yamagishi H, Ida H, Yazumi S, Chiba T, Ito Y, Hagiwara A. Down-regulation of RUNX1, RUNX3 and CBFbeta in hepatocellular carcinomas in an early stage of hepatocarcinogenesis. Anticancer Research. 2006;26:3633–3643. [PubMed] [Google Scholar]
- Morita et al. (2017).Morita K, Noura M, Tokushige C, Maeda S, Kiyose H, Kashiwazaki G, Taniguchi J, Bando T, Yoshida K, Ozaki T, Matsuo H, Ogawa S, Liu PP, Nakahata T, Sugiyama H, Adachi S, Kamikubo Y. Autonomous feedback loop of RUNX1-p53-CBFB in acute myeloid leukemia cells. Scientific Reports. 2017;7:16604. doi: 10.1038/s41598-017-16799-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Planaguma et al. (2004).Planaguma J, Diaz-Fuertes M, Gil-Moreno A, Abal M, Monge M, Garcia A, Baro T, Thomson TM, Xercavins J, Alameda F, Reventos J. A differential gene expression profile reveals overexpression of RUNX1/AML1 in invasive endometrioid carcinoma. Cancer Research. 2004;64:8846–8853. doi: 10.1158/0008-5472.CAN-04-2066. [DOI] [PubMed] [Google Scholar]
- R Core Team (2018).R Core Team . R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2018. [Google Scholar]
- Ramsey et al. (2018).Ramsey J, Butnor K, Peng Z, Leclair T, Van der Velden J, Stein G, Lian J, Kinsey CM. Loss of RUNX1 is associated with aggressive lung adenocarcinomas. Journal of Cellular Physiology. 2018;233:3487–3497. doi: 10.1002/jcp.26201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sangpairoj et al. (2017).Sangpairoj K, Vivithanaporn P, Apisawetakan S, Chongthammakun S, Sobhon P, Chaithirayanon K. RUNX1 regulates migration, invasion, and angiogenesis via p38 mapk pathway in human glioblastoma. Cellular and Molecular Neurobiology. 2017;37:1243–1255. doi: 10.1007/s10571-016-0456-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shuch et al. (2015).Shuch B, Amin A, Armstrong AJ, Eble JN, Ficarra V, Lopez-Beltran A, Martignoni G, Rini BI, Kutikov A. Understanding pathologic variants of renal cell carcinoma: distilling therapeutic opportunities from biologic complexity. European Urology. 2015;67:85–97. doi: 10.1016/j.eururo.2014.04.029. [DOI] [PubMed] [Google Scholar]
- Subramanian et al. (2005).Subramanian A, Tamayo P, Mootha VK, Mukherjee S, Ebert BL, Gillette MA, Paulovich A, Pomeroy SL, Golub TR, Lander ES, Mesirov JP. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proceedings of the National Academy of Sciences of the United States of America. 2005;102:15545–15550. doi: 10.1073/pnas.0506580102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takayama et al. (2015).Takayama K, Suzuki T, Tsutsumi S, Fujimura T, Urano T, Takahashi S, Homma Y, Aburatani H, Inoue S. RUNX1, an androgen- and EZH2-regulated gene, has differential roles in AR-dependent and -independent prostate cancer. Oncotarget. 2015;6:2263–2276. doi: 10.18632/oncotarget.2949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang et al. (2015).Wang X, Zhao Y, Qian H, Huang J, Cui F, Mao Z. The miR-101/RUNX1 feedback regulatory loop modulates chemo-sensitivity and invasion in human lung cancer. International Journal of Clinical and Experimental Medicine. 2015;8:15030–15042. [PMC free article] [PubMed] [Google Scholar]
- Xiong et al. (2014).Xiong Z, Yu H, Ding Y, Feng C, Wei H, Tao S, Huang D, Zheng SL, Sun J, Xu J, Fang Z. RNA sequencing reveals upregulation of RUNX1-RUNX1T1 gene signatures in clear cell renal cell carcinoma. Biomed Research International. 2014;2014:450621–450628. doi: 10.1155/2014/450621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yzaguirre, De Bruijn & Speck (2017).Yzaguirre AD, De Bruijn MF, Speck NA. The role of Runx1 in embryonic blood cell formation. Advances in Experimental Medicine and Biology. 2017;962:47–64. doi: 10.1007/978-981-10-3233-2_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yzaguirre et al. (2018).Yzaguirre AD, Howell ED, Li Y, Liu Z, Speck NA. Runx1 is sufficient for blood cell formation from non-hemogenic endothelial cells in vivo only during early embryogenesis. Development. 2018;145(2):dev158162. doi: 10.1242/dev.158162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou et al. (2017).Zhou Y, Zhang X, Zhang J, Fang J, Ge Z, Li X. LRG1 promotes proliferation and inhibits apoptosis in colorectal cancer cells via RUNX1 activation. PLOS ONE. 2017;12:e175122. doi: 10.1371/journal.pone.0175122. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The following information was supplied regarding data availability:
The raw data are available in the Supplemental File.