Abstract
Background:
Quadriceps strength and knee extension are believed to be important in the ability to effectively load the knee after anterior cruciate ligament (ACL) reconstruction (ACL-R).
Purpose:
To compare quadriceps strength (QUADS), side-to-side knee extension difference (ExtDiff), and knee energy absorption contribution (EAC) in patients preoperatively, 12 weeks postoperatively, and at return to sport (RTS). A secondary aim was to determine how the factors of QUADS and ExtDiff contributed to the ability to load the knee (knee EAC) at each of the 3 time points.
Study Design:
Case series; Level of evidence, 4.
Methods:
Overall, 41 individuals (mean ± SD age, 15.95 ± 1.63 years) were enrolled in this study. QUADS, ExtDiff, and knee EAC during a double-limb squat were collected preoperatively, 12 weeks postoperatively, and at RTS. Isokinetic QUADS was collected at 60 deg/s, normalized to body mass, and averaged across 5 trials. Knee extension was measured with a goniometer, and ExtDiff was calculated for analyses. Knee EAC was measured during double-limb squat descent and was calculated as a percentage of total energy absorption for the limb. Observations were obtained from both the surgical and nonsurgical limbs at the 3 time points. A mixed regression model with random intercept to compare change over the 3 time points was used, and a model selection was conducted with Akaike information criteria. Significance was set at P < .05.
Results:
Surgical limb QUADS was significantly lower preoperatively (mean ± SD, 1.37 ± 0.49 N·m/kg; P = .0023) and at 12 weeks (1.11 ± 0.38 N·m/kg; P < .0001) than at RTS (1.58 ± 0.47 N·m/kg). Nonsurgical limb QUADS was also significantly lower preoperatively (2.01 ± 0.54 N·m/kg; P < .0256) and at 12 weeks (2.03 ± 0.48 N·m/kg; P < .0233) than at RTS (2.18 ± 0.54 N·m/kg). Knee EAC for the surgical limb was significantly lower at 12 weeks than at RTS (40.98% ± 13.73% vs 47.50% ± 12.04%; P < .0032), and ExtDiff was significantly greater preoperatively than at RTS (–2.68° ± 3.19° vs –0.63° ± 1.43°; P < .0001). Preoperatively, QUADS for both the surgical (P < .0003) and nonsurgical (P = .0023) limbs was a significant predictor of surgical limb knee EAC, explaining 33.99% of the variance. At 12 weeks, surgical limb QUADS was a significant predictor (P < .0051) of surgical limb knee EAC, explaining 18.83% of the variance. At RTS, ExtDiff was a significant predictor (P = .0201) of surgical limb knee EAC, explaining 12.92% of the variance.
Conclusion:
The ability to load the knee after ACL injury changes across the continuum of care and is related to QUADS and ExtDiff. These results provide clinicians with insight into potential contributing factors that may limit knee loading during the rehabilitation process.
Keywords: ACL, continuum of care, energy absorption contribution, double-limb squat, quadriceps strength
Lower extremity joint loading after anterior cruciate ligament (ACL) reconstruction (ACL-R) has been studied across a variety of tasks and time frames.¶ A 62% limb symmetry index of vertical ground-reaction forces has been demonstrated during a sit-to-stand task at 1 month after ACL-R and was found to be predictive of a countermovement jump at 6 months.19 Similarly, deficits in knee energy absorption contribution (EAC) have been demonstrated in the involved limb during a double-limb squat (DLS) when compared with a matched healthy control limb at 3 months after ACL-R.9 Regarding the later phases of rehabilitation, decreased knee extension moments and smaller knee flexion and hip adduction angles are present during single-legged squats in patients who have undergone ACL-R when compared with healthy controls at approximately 7 months postoperatively.1 At return to sport (RTS), adolescent female athletes utilize greater hip EAC (more hip, less knee) than do healthy matched controls during a lateral vertical jump.3 Although these studies highlight lower extremity loading deficits at specific time points following ACL injury, they are limited in their analysis of the clinical factors that may be contributing to the inability to efficiently load the surgical knee following ACL-R.
Previous work examining the ability of the knee to load during a bilateral squatting task after ACL-R suggests underloading of the surgical limb secondary to a variety of factors, including quadriceps strength (QUADS),9,19 increased contribution of the gluteal muscles,9,30 and knee extension loss.19 In a previous study, we found that adolescent athletes exhibited greater hip EAC and lesser knee EAC of the surgical limb during a DLS when compared with a matched limb in the healthy control group at 3 months following ACL-R.9 When QUADS was considered, the reconstructed limb produced significantly less force than the matched healthy limb, and these values were associated with the aforementioned deficits in knee EAC. Similarly, Sigward et al30 found that individuals performing a bilateral squat at 3- and 5-month postoperative ACL-R demonstrate lower peak knee flexion angles and peak knee extension moments, less peak vertical ground reaction force, and greater hip-to-knee extension moment ratios in the surgical limb across time. While strength values were not measured in their study, the deficits in knee extensor moments of the surgical limb hint at the inability to use the quadriceps efficiently. During a sit-to-stand task at 1 month following ACL-R, Labanca et al19 found that participants demonstrated a 38% deficit in loading on the involved limb when compared with the uninvolved limb. These same individuals presented with up to 44% deficits in isometric QUADS of the involved limb, combined with knee extension deficits at 2 months postoperatively. Interestingly, asymmetries in QUADS and loss of knee extension range of motion (ROM) at 2 months were predictive of the ability to perform a symmetrical countermovement jump at 6 months postoperatively.19
Clinically, it is believed that knee extension ROM is an important factor in restoring function following ACL-R. Side-to-side differences in knee extension ROM at 4 weeks are related to restoration of knee extension ROM symmetry at 12 weeks after ACL-R.23 Knee extension loss at 4 weeks following ACL-R has also been demonstrated to be associated with quadriceps muscle atrophy at 4 weeks postsurgery.40 The loss of knee extension potentially limits a patient’s ability to fully load the knee during functional activities, especially during the early stages of rehabilitation. While a combination of the preceding findings denotes deficiencies in optimal surgical knee joint loading after ACL-R, there is limited information in the literature that focuses on the ability of the knee to progressively accept load across the rehabilitation continuum of care.
The primary aim of this study was to compare QUADS, side-to-side knee extension difference (ExtDiff), and knee EAC in patients after ACL-R across the continuum of care: preoperatively, 12 weeks postoperatively, and at RTS. A secondary aim was to determine how the factors of QUADS and knee extension difference contributed to the ability to load the knee (knee EAC) at each of the 3 time points. We hypothesized that QUADS, knee extension difference, and knee EAC in the involved limb would change across the continuum of care, while those same variables would not change in the uninvolved limb. Likewise, we hypothesized that QUADS of the involved limb would be associated with knee EAC at each of the 3 time points.
Methods
Participants
A total of 41 individuals (mean ± SD age, 15.95 ± 1.63 years) who met the inclusion criteria were enrolled into this study prior to their surgical procedure for ACL-R. Participants were tested preoperatively, 12 weeks postoperatively, and at RTS as part of a larger ongoing study examining clinical outcomes across the continuum of care. At each time point, participants were tested for QUADS, knee extension ROM, and knee EAC during a DLS. Table 1 details participant demographics.
TABLE 1.
Demographics of the Study Participants (N = 41)a
| Mean ± SD or % | |
|---|---|
| Age, y | 15.95 ± 1.63 |
| Male sex | 29.3 |
| Height, cm | 168.0 ± 9.3 |
| Weight, kg | 64.6 ± 10.5 |
| Graft type: patellar tendon | 100.0 |
| Mechanism of injury | |
| Direct | 17.1 |
| Indirect | 24.4 |
| Noncontact | 58.5 |
| Surgical limb | |
| Right | 46.3 |
| Left | 53.7 |
| Dominant limb | |
| Right | 97.5 |
| Left | 2.5 |
| Time from injury to surgery, d | 39.8 ± 23.2 |
| IKDC score | |
| Preoperatively | 54.1 ± 15.9 |
| 12 weeks postoperatively | 64.5 ± 8.9 |
| Return to sport | 88.5 ± 14.6 |
aIKDC, International Knee Documentation Committee.
Each participant included in the study received a patellar tendon autograft; the surgical procedure involved careful attention to closure of the harvest site, where the superficial fibers of the patellar tendon were loosely reapproximated with a running 0-Vicryl suture. Participants were considered eligible for this study if they were between the ages of 13 and 25 years and were involved in a level 1 sport (eg, basketball, football, or soccer) or level 2 sport (softball, baseball).5 Eligible participants were enrolled if they injured their ACL for the first time but did not experience any of the following: full-thickness chondral injuries or grade II or III medial, lateral, or posterior collateral ligament injuries. Following enrollment in the study, each participant completed an International Knee Documentation Committee questionnaire and a demographic information sheet that included injury history and sports participation.
All participants gave informed consent for the study, and the rights of each person were protected. If the participant was a minor, parental consent and child assent were attained. The institutional review board of Texas Health Resources approved the research procedures.
Instrumentation
A 10-camera Qualisys Motion Capture System (Qualisys AB) with a capture rate of 120 Hz was used to capture joint motions in all 3 planes during the DLS task. Thirty-three reflective markers were adhered to participants’ skin/clothing with double-sided tape (Figure 1). Marker placement included bilateral posterior superior iliac crest, bilateral superior sacral poles, inferior sacrum, bilateral greater trochanters, bilateral midthigh, bilateral medial and lateral femoral condyles, bilateral midtibia, bilateral medial and lateral malleoli, bilateral first and fifth metatarsal heads, and bilateral calcaneus. Two ATMI force plates capturing at 1200 Hz (Advanced Mechanical Technology) were used during data collection to allow accurate time sequencing during data collection and processing and to capture joint kinetics.
Figure 1.
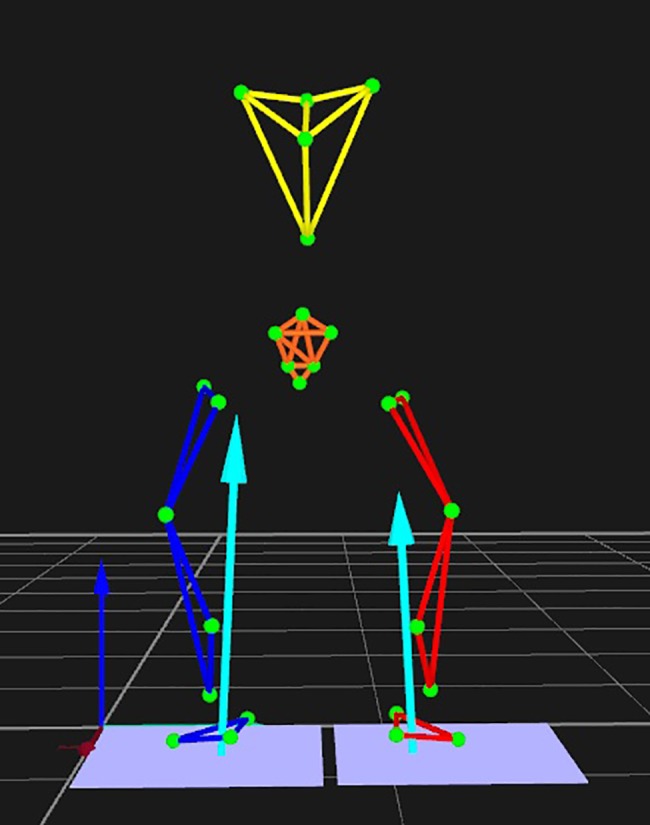
A 3-dimensional motion capture of double limb squat.
Squat Task
Participants were asked to stand with feet shoulder width apart, 1 foot on each force plate, and were instructed to perform a DLS as if they were sitting down onto a chair while keeping their hands raised overhead and their feet flat on the floor (Figure 2). A metronome set at 60 bps was used to ensure consistent pace across testing as participants completed 5 DLSs.
Figure 2.

Participant performing a double limb squat.
Isokinetic Testing
The Biodex Multi-Joint Testing and Rehabilitation System (Biodex Medical Systems) was used for testing extensor peak torque (herein, QUADS). Participants were seated on the Biodex system and secured with padded straps around the thigh, pelvis, and torso to minimize accessory and compensatory movements during testing.7,20 The femoral condyle of the test limb was aligned with the Biodex axis of rotation per the manufacturer’s instructions. Participants performed 5 submaximal knee extension/flexion repetitions to familiarize themselves with the testing motion. To measure QUADS at 60 deg/s, participants performed 5 consecutive concentric contractions.4 All participants began testing on the nonsurgical limb, followed by the surgical limb, and the mean of the 5 trials for each limb was normalized to body weight and used for data analysis.
Knee ROM Measurements
Knee extension ROM measurements were taken at each time point with a goniometer with a bubble level attachment while the participant was in a supine position with both knees in extension.23 The participant was instructed to actively tighten the quadriceps and fully straighten the knee to the best of his or her ability while knee ROM was measured. Both the involved (surgical) and uninvolved (nonsurgical) limbs were measured as described, and the difference between limbs (ExtDiff; surgical – nonsurgical) was used for analyses. Previous work with a goniometer to measure knee ROM demonstrated intraclass correlation coefficient values of 0.98 for intratester reliability and 0.99 for intertester reliability.10,36 Likewise, an earlier study from our institution established good interrater reliability for knee extension in this population.23
Data Analysis and Statistics
Data were exported from the Qualisys system to Visual 3D for data processing. Kinematic and kinetic data were filtered with a Butterworth filter with a cutoff frequency of 12 Hz. The lower extremity joint angles were calculated with an inverse kinematic approach, and the lower extremity internal moment was calculated with an inverse dynamic approach. Energy absorption (EA) of the knee joint was calculated by integrating the negative portion of the scalar power curve (product of net moment and angular velocity; in watts) where joint angular velocity and net joint moment are in opposite directions, indicating eccentric loading during the descent phase of the DLS. This was normalized to the product of height and weight and averaged across the middle 3 trials. EAC of the knee joint was calculated relative to the total limb EA and reported as a percentage: knee EAC = [knee EA / (sum of hip, knee, and ankle EA)] × 100. For purposes of this study, knee joint EAC was included as the variable of interest.
Observations were obtained from the surgical and nonsurgical limbs at the 3 specified time points: preoperative, postoperative 12 weeks, and RTS. Multiple observations obtained from each limb were assumed to be correlated. To account for the correlation between multiple observations within each limb, a 2-level mixed model with random intercept was employed to compare the differences in means between preoperative and RTS, 12 weeks and RTS, and preoperative and 12 weeks. Inclusion of a random effect allows an investigator to model the correlation between multiple observations from the same participant and the degree of heterogeneity in the population of participants.16 The normal distribution assumption for paired data was evaluated, and nonparametric signed rank was used to compare the pre- and postmeasurements when the data varied from normal distribution. Individual-level heterogeneity was evaluated with the Wald test, and the Akaike information criteria for model selection were used. Except where otherwise stated, mean ± SD and 2-sided P values are reported. Alpha level was set at P < .05. All analyses were conducted with SAS (v 9.4; SAS Institute).
Results
A total of 41 patients (12 male, 29 female; age, 15.95 ± 1.63 years) were included in the analysis. Preoperative and 12-week findings were both compared with RTS, while preoperative and 12-week comparisons were also made in the results that follow.
Table 2 highlights the results for each variable at each time point between the surgical and nonsurgical limbs. At RTS, the surgical limb QUADS significantly increased by 15.3% from preoperative (P < .0023) and by 42.3% from 12 weeks postoperative (P < .0001). In contrast, surgical limb QUADS was significantly decreased at 12 weeks compared with preoperative (P < .0001), showing an 18% decrease from before surgery. At RTS, the nonsurgical limb QUADS increased by 8.4% from preoperative and by 7.3% from 12 weeks. Similar to the surgical limb, significant differences were found in the nonsurgical limb QUADS between preoperative and RTS (P < .0256) and between 12 weeks and RTS (P < .0233). No significant nonsurgical limb QUADS differences were seen between preoperative and 12 weeks (P = .9866).
TABLE 2.
Each Study Variable Across the Continuum of Care (N = 41)
| Preoperative | 12-wk | RTS | |
|---|---|---|---|
| ExtDiff, deg | –2.68 ± 3.19b | –1.32 ± 1.89 | –0.63 ± 1.43 |
| QUADS, N·m/kg | |||
| Surgical limb | 1.37 ± 0.49c | 1.11 ± 0.38c | 1.58 ± 0.47 |
| Nonsurgical limb | 2.01 ± 0.54d | 2.03 ± 0.48 | 2.18 ± 0.54d |
| Knee EAC, % total EA | |||
| Surgical limb | 50.54 ± 13.83e | 40.98 ± 13.73e | 47.50 ± 12.04 |
| Nonsurgical limb | 58.52 ± 10.60 | 59.28 ± 13.53 | 55.87 ± 11.95 |
aValues are presented as mean ± SD. EA, energy absorption; EAC, energy absorption contribution; ExtDiff, side-to-side knee extension difference (surgical limb – nonsurgical limb); QUADS, quadriceps strength; RTS, return to sport.
bP < .05, preoperative vs 12-wk and preoperative vs RTS.
cP < .05, preoperative vs 12-wk, 12-wk vs RTS, and preoperative vs RTS.
dP < .05, preoperative vs RTS and 12-wk vs RTS.
eP < .05, preoperative vs 12-wk and 12-wk vs RTS.
Preoperative knee EAC decreased by 6.0% at RTS, whereas the 12-week knee EAC increased by 15.9% at RTS for the surgical limb. No significant surgical limb knee EAC differences were observed between the preoperative and RTS findings (P = .2037); however, 12-week knee EAC was significantly lower than at RTS (P < .0032) and preoperatively (P < .0001). Although a decrease in nonsurgical limb knee EAC at RTS was observed when compared with both preoperative (4.5%) and 12 weeks (5.7%), neither preoperative knee EAC (P = .1830) nor 12-week knee EAC (P = .0833) was significant. Likewise, nonsurgical limb knee EAC was not significantly different between preoperative and 12 weeks (P = .6826).
The ExtDiff at RTS was –0.63° ± 1.43°, which was 76.4% lower (improved) compared with preoperative and 52.3% lower compared with 12 weeks. Although ExtDiff between 12 weeks and RTS was not significant (P = .1955), ExtDiff between preoperative and RTS was found to be highly significant (P < .0001). Similarly, ExtDiff at 12 weeks was significantly improved when compared with preoperative results (P < .0045).
The regression analyses identified preoperative QUADS for both the surgical (P < .0003) and nonsurgical (P = .0023) limbs as a significant predictor of the surgical limb knee EAC preoperatively, explaining 33.99% of the variance (R 2 = 0.3399). At 12 weeks, only the surgical limb QUADS remained a significant predictor (P < .0051) for surgical limb knee EAC, as it explained 18.83% of the variance (R 2 = 0.1883). By RTS, neither the surgical nor the nonsurgical limb QUADS was a significant predictor of knee EAC. Although not significant at the preoperative or 12-week time point, ExtDiff at RTS was found to be a significant predictor (P = .0201) of the surgical limb knee EAC at RTS, explaining 12.92% of the variance (R 2 = 0.1292).
Discussion
Consistent with the original hypotheses, the results of this study demonstrated that QUADS and knee EAC in the surgical limb and knee ExtDiff changed across the continuum of care in participants who had undergone ACL-R. In contrast, in the nonsurgical limb, knee EAC did not change across the continuum of care, while QUADS did demonstrate slight increases over time. Preoperatively, QUADS of the surgical and nonsurgical limbs was predictive of surgical limb loading (knee EAC), explaining >33% of the variance. Interestingly, the 12-week time point appears to be a critical marker for changes in knee EAC and QUADS of the surgical limb following ACL-R, as both demonstrated an 18% decrease in value from the preoperative measurements.
These findings are consistent with previous studies showing loading9,30,31 and QUADS9 deficits at 12 weeks after ACL-R. In our previous study, when participants were tested for QUADS and knee EAC during a DLS at 12 weeks following ACL-R, significant differences were noted, with the surgical limb producing lower strength and loading (knee EAC) values than the matched limb in the healthy control group.9 These loading deficits at the knee were accompanied with an increase in loading at the hip (hip EAC) and also related to QUADS production at the 12-week mark. Similarly, underloading of the surgical limb has been demonstrated in individuals performing DLSs at 3-month postoperative ACL-R, as participants produced less vertical ground-reaction force as compared with the nonsurgical limb and a greater hip-to-knee extensor moment ratio.30
Results from both of these studies9,30 suggest that at 12 weeks following ACL-R, the surgical limb shifts loading demands from the knee to the hip in an effort to perform a functional squat. It is possible that this alteration in loading from the knee to the hip may occur earlier than the 12-week mark; however, at this time, there is limited evidence within the literature. While this would be considered an intralimb compensation, prior studies30,31 have also shown the use of interlimb compensations when functional tasks were performed at 3-month postoperative ACL-R. The current study did not analyze between-limb loading differences at 12 weeks after ACL-R, but a close look at the knee EAC values between the surgical (40.98% ± 13.73%) and nonsurgical (59.28% ± 13.53%) limbs points to interlimb asymmetries.
QUADS deficits have previously been linked to muscle atrophy at 12 weeks,40,7 7 months,33 and approximately 2.5 years17 after ACL-R. Although muscle atrophy was not examined during the current study, the 12-weeks postoperative surgical limb QUADS deficit of 18.0% compared with preoperatively is similar to previously reported discrepancies of 12.0%,41 13.8%,40 and 17.0%12 and could be related to muscle atrophy. The results from these studies may help to explain, in part, the difficulty of these individuals to effectively load the surgical knee at 12 weeks. In the current study, surgical limb QUADS was a significant predictor of knee EAC at this time point and partially (18.83%) explained the variance. Conversely, surgical limb knee EAC and QUADS significantly improved from 12 weeks to RTS by 16.0% and 42.3%, respectively. One might assume that knee loading improvements in the surgical limb at RTS are likely related to the QUADS gains from increased external loads experienced during functional exercises and the structured rehabilitation program8 followed by these individuals.
On the contrary, ExtDiff helped to predict knee EAC at RTS, explaining 12.92% of the variance. In the current study, ExtDiff progressively improved from Pre- to 12 weeks to RTS. As such, it appears that as knee extension becomes more symmetrical, the ability of the knee to accept load improves. The current findings are consistent with earlier data suggesting that patients who achieve symmetrical knee extension ROM following knee surgery have better strength and function.2 Additionally, increased knee extension ROM may improve the passive stability of the knee during the transfer of weight to the surgical limb, thus enabling the individual to more fully load the joint.40
In contrast to surgical limb QUADS, nonsurgical limb QUADS remained consistent and did not demonstrate a significant decline in strength between the preoperative and 12-week time points; however, it did significantly increase at RTS (2.18 ± 0.54 N·m/kg) when compared with both preoperative (2.01 ± 0.54 N·m/kg) and 12 weeks (2.03 ± 0.48 N·m/kg). These results are slightly different from an earlier ACL-R randomized controlled trial by Zolt et al41 that demonstrated a small increase (192.0 ± 59.0 to 202.0 ± 54.0 N·m) in nonsurgical limb isometric QUADS from presurgery to 12 weeks postsurgery, with a subsequent decline (202.0 ± 54.0 to 196.0 ± 58.0 N·m) from 12 to 26 weeks postsurgery. Differing results between the current study and Zolt et al could be attributed to the use of isometric41 versus isokinetic testing as well as variances in age (current, 16.0 ± 1.6 years; Zolt et al, 28.0 ± 10 years) and rehabilitation protocols (eg, timing of introduction of exercises, weightbearing, and joint loading). Either way, these outcomes provide evidence of QUADS changes across the continuum of care and suggest that strength variances are minimal on the nonsurgical limb despite inclusion of focused strengthening throughout the rehabilitation process.
In addition to nonsurgical limb QUADS, the current study examined the ability to load the nonsurgical knee from preoperatively to RTS. Similar to the consistent manner in which nonsurgical limb QUADS presented across the continuum of care, knee EAC on the nonsurgical limb remained stable from preoperatively to 12 weeks to RTS. The lack of QUADS changes and the ability of the nonsurgical limb to effectively load at each time point are in contrast to previously reported findings of bilateral QUADS deficits following knee injuries.13,14,34 While uninvolved (or nonsurgical) limb QUADS has been shown to be diminished at the preoperative ACL-R time point when compared with the matched, dominant limb of healthy controls,13 the current study did not examine strength differences between limbs but rather reported QUADS of the surgical and nonsurgical limbs across the rehabilitation process. Regardless, recent data demonstrate low rates of patients achieving RTS criteria at 6 and 9 months when the surgical limb was matched against the nonsurgical limb.37 As such, comparison of surgical and nonsurgical limb objective data with age-, sex-, and activity-matched controls may provide more valuable insight into the preparedness of an individual to RTS following ACL-R.
The results from the current study demonstrate altered loading patterns during a squat in the surgical limb of adolescent athletes across the continuum of care following ACL-R. These findings may not be transferable to other populations or more dynamic tasks, but they do represent the continuation of the inability to load the surgical knee during a submaximal task such as a squat.31 While the presence of pain could have limited the participant’s ability to perform the given tasks during this study, participants were instructed to stop all testing if they experienced pain and/or discomfort in their knees. In addition, all participants were able to complete testing without complaints of pain.
Another limitation includes the lack of between-limb comparisons across the spectrum of care. While this was not the focus of this particular study, the magnitude of the values of the surgical limb QUADS and knee EAC (Table 2) are considerably lower than those of the nonsurgical limb at each time point. As briefly mentioned earlier, future comparisons with matched limbs of healthy control participants may provide a better standard by which to gauge restoration of loading and strength.
Finally, ExtDiff and QUADS were the variables chosen to help potentially explain variance in the ability to effectively load the surgical knee (knee EAC) across the continuum of care. While these variables did help to explain a portion of the variance seen in knee loading, the explanation most likely involves multiple factors that were not included in the regression model. Earlier data have demonstrated a relationship between the use of an autograft and loss of knee extension after ACL-R,22 which could certainly contribute to deficits in QUADS. Each participant in the current study underwent a patellar tendon autograft, which may have played a role in QUADS values. Likewise, postoperative rehabilitation was not specifically controlled for in this particular study; however, the protocol within our system is standardized such that each participant would have received similar treatment throughout the duration of the rehabilitation process. Future investigations that include potential contributions at the hip and ankle of both the surgical and nonsurgical limbs during a DLS and other dynamic tasks may provide further insight into the efficacy of knee loading following ACL-R.
Conclusion
The ability to effectively load the knee after ACL injury changes across the continuum of care and is related to QUADS and ExtDiff. A substantial decline (18%) in knee EAC and QUADS is evident from preoperative to 12 weeks postoperative in the surgical limb, which highlights the importance of rehabilitation during the early phases of postoperative ACL-R. These results provide clinicians with insight into potential contributing factors that may limit knee loading during the rehabilitation process.
Acknowledgment
The authors thank the Texas Health Sports Medicine staff and research coordinators for their assistance in data collection.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: C.B. has received educational support from Smith & Nephew, Arthrex, and Pylant Medical. S.B.S. has received educational support from Arthrex and Pylant Medical, nonconsulting payments from Arthrex, and hospitality payments from Stryker. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Texas Health Resources Institutional Review Board (No. Pro00005219).
References
- 1. Bell DR, Kulow SM, Stiffler MR, Smith MD. Squatting mechanics in people with and without anterior cruciate ligament reconstruction: the influence of graft type. Am J Sports Med. 2014;42(12):2979–2987. [DOI] [PubMed] [Google Scholar]
- 2. Biggs A, Jenkins WL, Urch SE, Shelbourne KD. Rehabilitation for patients following ACL reconstruction: a knee symmetry model. N Am J Sports Phys Ther. 2009;4(1):2–12. [PMC free article] [PubMed] [Google Scholar]
- 3. Boo ME, Garrison JC, Hannon JP, et al. Energy absorption contribution and strength in female athletes at return to sport after anterior cruciate ligament reconstruction: comparison with healthy controls. Orthop J Sports Med. 2018;6(3):2325967118759522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cvjetkovic DD, Bijeljac S, Palija S, et al. Isokinetic testing in evaluation rehabilition outcome after ACL reconstruction. Med Arch. 2015;69:21–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR. Fate of the ACL-injured patient: a prospective outcome study. Am J Sports Med. 1994;22(5):632–644. [DOI] [PubMed] [Google Scholar]
- 6. Di Stasi S, Hartigan EH, Snyder-Mackler L. Sex-specific gait adaptations prior to and up to 6 months after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2015;45(3):207–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Feiring DC, Ellenbecker TS, Derscheid GL. Test-retest reliability of the Biodex isokinetic dynamometer. J Orthop Sports Phys Ther. 1990;11:298–300. [DOI] [PubMed] [Google Scholar]
- 8. Garrison JC, Bothwell J, Cohen K, Conway JE. Effects of hip strengthening on early outcomes following anterior cruciate ligament reconstruction. Int J Sports Phys Ther. 2014;9(2):157–167. [PMC free article] [PubMed] [Google Scholar]
- 9. Garrison JC, Hannon J, Goto S, Giesler L, Bush C, Bothwell JM. Participants at three months post-operative anterior cruciate ligament reconstruction (ACL-R) demonstrate differences in lower extremity energy absorption contribution and quadriceps strength compared to healthy controls. Knee. 2018;25(5):782–789. [DOI] [PubMed] [Google Scholar]
- 10. Gogia PP, Braatz JH, Rose SJ, Norton BJ. Reliability and validity of goniometric measurements at the knee. Phys Ther. 1987;67(2):192–195. [DOI] [PubMed] [Google Scholar]
- 11. Hall M, Stevermer CA, Gillette JC. Gait analysis post anterior cruciate ligament reconstruction: knee osteoarthritis perspective. Gait Posture. 2012;36(1):56–60. [DOI] [PubMed] [Google Scholar]
- 12. Hallagin C, Garrison JC, Pollard KM, Goto S, Bothwell J, Hannon J. The relationship between pre-operative and 12 week post-operative Y-Balance and quadriceps strength in athletes with an anterior cruciate ligament tear. Int J Sports Phys Ther. 2017;12(6):986–993. [PMC free article] [PubMed] [Google Scholar]
- 13. Hannon J, Wang-Price S, Goto S, Garrison JC, Bothwell JM. Do muscle strength deficits of the uninvolved hip and knee exist in young athletes before anterior cruciate ligament reconstruction? Orthop J Sports Med. 2017;5(1):2325967116683941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hart JM, Pietrosimone B, Hertel J, Ingersoll CD. Quadriceps activation following knee injuries: a systematic review. J Athl Train. 2010;45(1):87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Havens KL, Cohen SC, Pratt KA, Sigward SM. Accelerations from wearable accelerometers reflect knee loading during running after anterior cruciate ligament reconstruction. Clin Biomech (Bristol, Avon). 2018;58:57–61. [DOI] [PubMed] [Google Scholar]
- 16. Hedeker D, Gibbons RD. Longitudinal Data Analysis. Hoboken, NJ: Wiley; 2006. [Google Scholar]
- 17. Kuenze CM, Blemker SS, Hart JM. Quadriceps function relates to muscle size following ACL reconstruction. J Orthop Res. 2016;34(9):1656–1662. [DOI] [PubMed] [Google Scholar]
- 18. Kumar D, Su F, Wu D, et al. Frontal plane knee mechanics and early cartilage degeneration in people with anterior cruciate ligament reconstruction: a longitudinal study. Am J Sports Med. 2018;46(2):378–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Labanca L, Laudani L, Menotti F, et al. Asymmetrical lower extremity loading early after anterior cruciate ligament reconstruction is a significant predictor of asymmetrical loading at the time of return to sport. Am J Phys Med Rehabil. 2016;95(4):248–255. [DOI] [PubMed] [Google Scholar]
- 20. Laudner K, Evans D, Wong R, et al. Relationship between isokinetic knee strength and jump characteristics following anterior cruciate ligament reconstruction. Int J Sports Phys Ther. 2015;10:272–280. [PMC free article] [PubMed] [Google Scholar]
- 21. Lin PE, Sigward SM. Contributors to knee loading deficits during gait in individuals following anterior cruciate ligament reconstruction. Gait Posture. 2018;66:83–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mauro CS, Irrgang JJ, Williams BA, Harner CD. Loss of extension following anterior cruciate ligament reconstruction: analysis of incidence and etiology using IKDC criteria. Arthroscopy. 2008;24(2):146–153. [DOI] [PubMed] [Google Scholar]
- 23. Noll S, Garrison JC, Bothwell J, Conway JE. Knee extension range of motion at 4 weeks is related to knee extension loss at 12 weeks after anterior cruciate ligament reconstruction. Orthop J Sports Med. 2015;3(5):2325967115583632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Pairot de Fontenay B, Argaud S, Blache Y, Monteil K. Asymmetries in joint work during multi-joint movement after anterior cruciate ligament reconstruction: a pilot study. Scand J Med Sci Sports. 2014;24(6):e471–e476. [DOI] [PubMed] [Google Scholar]
- 25. Pollard CD, Stearns KM, Hayes AT, Heiderscheit BC. Altered lower extremity movement variability in female soccer players during side-step cutting after anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(2):460–465. [DOI] [PubMed] [Google Scholar]
- 26. Pratt K, Sigward S. Inertial sensor angular velocities reflect dynamic knee loading during single limb loading in individuals following anterior cruciate ligament reconstruction. Sensors (Basel). 2018;18(10):3460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Renner KE, Franck CT, Miller TK, Queen RM. Limb asymmetry during recovery from anterior cruciate ligament reconstruction. J Orthop Res. 2018;36:1887–1893. [DOI] [PubMed] [Google Scholar]
- 28. Sanford BA, Williams JL, Zucker-Levin A, Mihalko WM. Asymmetric ground reaction forces and knee kinematics during squat after anterior cruciate ligament (ACL) reconstruction. Knee. 2016;23(5):820–825. [DOI] [PubMed] [Google Scholar]
- 29. Schmitt LC, Paterno MV, Ford KR, Myer GD, Hewett TE. Strength asymmetry and landing mechanics at return to sport after anterior cruciate ligament reconstruction. Med Sci Sports Exerc. 2015;47(7):1426–1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sigward SM, Chan M, Lin PE, Almansouri SY, Pratt KA. Compensatory strategies that reduce knee extensor demand during a bilateral squat change from 3 to 5 months following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2018;48(9):713–718. [DOI] [PubMed] [Google Scholar]
- 31. Sigward SM, Lin P, Pratt K. Knee loading asymmetries during gait and running in early rehabilitation following anterior cruciate ligament reconstruction: a longitudinal study. Clin Biomech (Bristol, Avon). 2016;32:249–254. [DOI] [PubMed] [Google Scholar]
- 32. Stearns KM, Pollard CD. Abnormal frontal plane knee mechanics during sidestep cutting in female soccer athletes after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2013;41(4):918–923. [DOI] [PubMed] [Google Scholar]
- 33. Thomas AC, Wojtys EM, Brandon C, Palmieri-Smith RM. Muscle atrophy contributes to quadriceps weakness after anterior cruciate ligament reconstruction. J Sci Med Sport. 2016;19(1):7–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Urbach D, Nebelung W, Weiler H-T, Awiszus F. Bilateral deficit of voluntary quadriceps muscle activation after unilateral ACL tear. Med Sci Sports Exerc. 1999;31(12):1691–1696. [DOI] [PubMed] [Google Scholar]
- 35. Ward SH, Blackburn JT, Padua DA, et al. Quadriceps neuromuscular function and jump-landing sagittal-plane knee biomechanics after anterior cruciate ligament reconstruction. J Athl Train. 2018;53(2):135–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Watkins MA, Riddle DL, Lamb RL, Personius WJ. Reliability of goniometric measurements and visual estimates of knee range of motion obtained in a clinical setting. Phys Ther. 1991;71(2):90–96. [DOI] [PubMed] [Google Scholar]
- 37. Welling W, Benjaminse A, Seil R, Lemmink K, Zaffagnini S, Gokeler A. Low rates of patients meeting return to sport criteria 9 months after anterior cruciate ligament reconstruction: a prospective longitudinal study. Knee Surg Sports Traumatol Arthrosc. 2018;26:3636–3644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Wellsandt E, Gardinier ES, Manal K, Axe MJ, Buchanan TS, Snyder-Mackler L. Decreased knee joint loading associated with early knee osteoarthritis after anterior cruciate ligament injury. Am J Sports Med. 2016;44(1):143–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wellsandt E, Khandha A, Manal K, Axe MJ, Buchanan TS, Snyder-Mackler L. Predictors of knee joint loading after anterior cruciate ligament reconstruction. J Orthop Res. 2017;35(3):651–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Žargi TG, Drobnič M, Vauhnik R, Koder J, Kacin A. Factors predicting quadriceps femoris muscle atrophy during the first 12 weeks following anterior cruciate ligament reconstruction. Knee. 2017;24(2):319–328. [DOI] [PubMed] [Google Scholar]
- 41. Zult T, Gokeler A, van Raay JJ, et al. Cross-education does not accelerate the rehabilitation of neuromuscular functions after ACL reconstruction: a randomized controlled clinical trial. Eur J Appl Physiol. 2018;118:1609–1623. [DOI] [PMC free article] [PubMed] [Google Scholar]


