Abstract
The purpose of this work was to determine the safety of inhaled hydrogen gas in healthy animals. Female mice were exposed to medical air with or without hydrogen gas (concentration 2.4%) for 72 hours (n = 25 mice/group). Mice underwent a standardized and validated neurobehavioral examination, SmithKline Beecham, Harwell, Imperial College, Royal London Hospital, Phenotype Assessment (SHIRPA) protocol, prior to and following the exposure period. Blood was withdrawn for serologic evaluation and all major organ tissues were evaluated histologically. The average hydrogen concentration within the chamber was 2.27%. Following exposure, there was no significant change in body weight in either group. Similarly, there was no significant change in the total SHIRPA score, although hydrogen-treated mice exhibited significantly lower spontaneous locomotor activity (P < 0.0001) in a subset of the test; all other aspects of the mouse neurologic exam were normal in hydrogen-treated animals. Brain histopathology was also normal in all mice, as was the histology of all other major organs. There were no significant differences in complete blood count, serum chemistry, or arterial blood gases between control and hydrogen-treated mice (P > 0.05 for all). Hydrogen gas did not appear to cause significant adverse effects when administered to healthy mice for 72 hours, with the possible exception of decreased spontaneous locomotor activity. The study was approved by the Institutional Animal Care and Use Committee at Boston Children’s Hospital, USA (approved number 18-01-3536) on January 25, 2018.
Keywords: hydrogen gas, safety, neurobehavioral testing, ischemia-reperfusion injury, neuroprotection, adverse effects
INTRODUCTION
Ischemia reperfusion injury may negatively affect outcomes in a variety of clinical settings, including following myocardial infarction, stroke, and cardiac arrest. One of the mechanisms of ischemia reperfusion injury is the generation of reactive oxygen species, including the hydroxyl radical (•OH). •OH reacts indiscriminately with nucleic acids, lipids and proteins, causing direct cellular injury and stimulating apoptosis. It has been recently shown that molecular dihydrogen (H2) gas selectively reduces •OH,1,2 and modifies several inflammatory pathways.3 There is mounting evidence to support its clinical benefits in treating ischemia reperfusion injury. In rodents, post-ischemic H2 inhalation has been shown to diminish cerebral infarct size and improve neurologic scores in rats following middle cerebral artery occlusion.1 Several rat studies have demonstrated improvement in survival and outcomes in models of cardiac arrest associated with hydrogen administration.4,5,6,7 In swine, inhalation of H2 diminishes cerebral injury volume and improves clinical outcomes in models of simulated perinatal asphyxia8 and cardiopulmonary bypass-related ischemia.9 Similarly, inhaled H2 improves sequelae of ischemia reperfusion injury in animal models of liver10 and lung11 injury.
More recently, inhaled H2 has reached clinical use in Japan. The first study described the 18-hour administration of 2% H2 to 5 patients resuscitated from cardiac arrest and undergoing simultaneous targeted temperature management; 4/5 patients exhibited a normal neurologic examination (cerebral performance category 1) at hospital discharge and no environmental hazards were reported.12 A large, randomized trial of H2 therapy in post-cardiac arrest syndrome is underway.13 Further, inhaled H2 was studied in adults presenting with ST-segment elevation myocardial infarction, randomized to treatment with or without 2% H2 (via face mask) for 24 hours post-reperfusion, with H2-treated patients demonstrating significantly improved ventricular ejection fraction at 6-month follow-up.14 Finally, patients who were randomized to breathing 3% H2 gas for 1 hour twice a day for 7 days following stroke demonstrated improved clinical stroke scores and a diminished volume of injury by brain MRI compared with similarly-treated controls (n = 25 patients/group).15 To our knowledge, no data are available regarding the effects of inhaled H2 in healthy humans.
The purpose of this work was to screen for adverse effects of inhaled hydrogen gas in healthy animals in order to inform a future phase I safety trial in humans.
MATERIALS AND METHODS
Animals
The following protocol was approved by the Institutional Animal Care and Use Committee at Boston Children’s Hospital, USA (approved number 18-01-3536) on January 25, 2018. IGS female mice (n = 50, 10-week-old, CD-1, Charles River Labs, Wilmington, MA, USA) were acclimated to our rodent housing facility in ambient air for 96 hours in a 12-hour alternating light-dark cycle at room temperature with free access to food and water. Animals were then placed into a custom gas-tight chamber (Biospherix, Parish, NY, USA) with a capacity to house five mouse cages (25 mice) (Additional Figure 1 (377KB, tif) ). Within this chamber, mice were exposed to certified medical air with or without hydrogen gas (Praxair, Inc., Danbury, CT, USA) for a 72-hour period (n = 25 per group). The source gas (3.2% hydrogen, 21% oxygen, balance nitrogen) was titrated to maintain a target inhaled gas concentration of approximately 2.4%, and H2 concentration was quantified at the exhaust port of the chamber (Eagle 2, RKI Instruments, Union City, CA, USA). In the control group, medical air was flowed into the chamber at a set flow rate (3 L/min). Mice were housed in litters of five mice each and had free access to food and water during this time. The following endpoints were quantified at the end of the exposure period.
Neurobehavioral assessment
Each mouse underwent a neurologic and behavioral assessment using a well-established neurodevelopmental and behavioral examination (known as SHIRPA, an acronym for SmithKline Beecham, Harwell, Imperial College, Royal London Hospital, Phenotype Assessment)16,17 both before and after the exposure period. All tests were completed by a team member blinded to treatment allocation. This battery of tests includes a scoring system to grade muscular, cerebellar, sensory, neuropsychiatric and autonomic functions (Table 1). Additionally, each mouse was weighed before and after the exposure period.
Table 1.
The SHIRPA scoring system
| Observation | Points |
|---|---|
| Body position | 0 = active; 1 = inactive; 2 = excessive activity |
| Tremor | 0 = present; 1 = absent |
| Palpebral closure | 0 = present; 1 = absent |
| Coat appearance and color | 0 = normal; 1 = abnormal |
| Whiskers | 0 = present; 1 = absent |
| Lacrimation | 0 = present; 1 = absent |
| Defecation | 0 = present; 1 = absent |
| Transfer arousal | 0 = extended freeze; 1 = brief freeze; 2 = immediate movement |
| Locomotor activity | Total # of squares entered in 30 seconds |
| Gait | 0 = fluid movement; 1 = lack of fluidity |
| Tail elevation | 0 = dragging; 1 = horizontal extension; 2 = elevated/straub tail |
| Startle response | 0 = preyer reflex; 1 = absent; 2 = reaction in addition to reflex |
| Touch Escape | 0 = none; 1 = response to touch; 2 = flees prior to touch |
| Positional passivity | 0 = struggles when held by tail; 1 = struggles when scuffed; 2 = struggles when laid supine; 3 = no struggle |
| Skin color | 0 = pale; 1 = pink; 2 = red |
| Trunk curl | 0 = present; 1 = absent |
| Limb grasping | 0 = present; 1 = absent |
| Visual placing | 0 = present; 1 = absent |
| Righting reflex | 0 = present; 1 = absent |
| Pinnal reflex | 0 = present; 1 = absent |
| Contact righting reflex | 0 = present; 1 = absent |
| Corneal reflex | 0 = present; 1 = absent |
| Biting | 0 = present; 1 = absent |
| Vocalization | 0 = present; 1 = absent |
| Morphology | 0 = normal; 1 = abnormal |
| Tail pinch | 0 = response; 1 = no response |
| Pupillary light reflex | 0 = present; 1 = absent |
Note: The SHIRPA scoring system contains three phases: observation in cage, removal of the cage and placement onto an arena, and then provocative testing. SHIRPA: SmithKline Beecham, Harwell, Imperial College, Royal London Hospital, Phenotype Assessment.
Serologic and histologic examinations
After the exposure period and SHIRPA evaluation, mice were anesthetized with 0.5–2% isoflurane (Patterson Veterinary, Greeley, CO, USA) via face mask in oxygen. Pre-sacrifice blood was withdrawn in a subset of animals (n = 5) via terminal left ventricular puncture for evaluation of serologic markers of renal and hepatic injury, coagulopathy, as well as arterial blood gas analysis. In all animals, all major organs were then removed, formalin-fixed, stained by hematoxylin and eosin, and evaluated by light microscopy (Keyence BZ-X710 All-in-One Fluorescence Microscope, Keyence, Itasca, IL, USA) by a pathologist blinded to treatment allocation. In order to examine for any subtle damage (i.e., invisible to light microscopy) to the airways, samples of the mid-trachea were fixed, embedded, sectioned (80 nm-thick), and examined by electron microscopy (Tecnai G2 Spirit BioTWIN Electron Microscope, FEI Company, Hillsboro, OR, USA) by a pathologist blinded to treatment allocation in a subset of animals (n = 5 per group).
Statistical analysis
Body weight was compared prior to and following the exposure period separately for each group by paired t-test. Similarly, the total SHIRPA score and locomotor scores (a subportion of the SHIRPA score) were compared prior to and following exposure by paired t-test. The change in locomotor score was compared between groups using an unpaired t-test after normality was confirmed (D’Agostino & Pearson normality test). All serologic examinations were compared between groups by Mann–Whitney U test. All analyses were performed in GraphPad Prism (Prism version 7.0d, GraphPad Software, La Jolla, CA, USA).
RESULTS
All animals in both groups survived the 72-hour gas exposure. The time-averaged measured hydrogen concentration at the exhaust port was 2.27% (95% confidence interval (CI) 2.26–2.29%) (Additional Figure 2 (435.6KB, tif) ). Gas flow rate in the hydrogen group (6.5 ± 0.3 L/min) was significantly higher than in the control group (3.0 ± 0.0 L/min, P < 0.0001).
Effect of inhaled hydrogen gas on the SHIRPA scoring of healthy mice
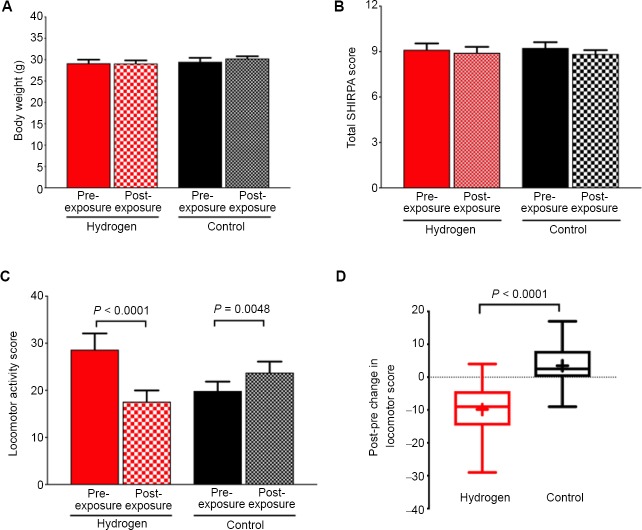
The average pre-exposure body weight was 29.15 ± 0.41 g in the hydrogen group and 29.51 ± 0.46 g in the control group (P = 0.56). There was no significant change in body weight prior to versus following exposure in either the hydrogen or the control group (Figure 1A). There was no significant change in the pre- versus post-exposure SHIRPA score in either hydrogen- or control-exposed animals (Figure 1B). However, a subset of the total SHIRPA score enumerates the number of squares that a mouse contacts within 30 seconds, known as the locomotor activity score. This score was similar between groups pre-exposure (though mathematically higher in the hydrogen-exposed group, P = 0.56), and significantly decreased in hydrogen-exposed mice (P < 0.0001), and significantly increased in control mice (P = 0.0048; Figure 1C); the pre- versus post-exposure change was significant between groups (P < 0.0001, Figure 1D). Following exposure, all animals in both groups exhibited normal skin coloring, activity level, transfer arousal, exhibited signs of neither hyperactivity nor hypoactivity (Additional Table 1).
Figure 1.
Body weight, SHIRPA score, and locomotor activity of mice with hydrogen gas inhaled.
Note: (A) Body weight. (B) Total SHIRPA score. (C) locomotor activity score, a subset of the total SHIRPA score, which enumerates the number of squares that a mouse steps on within 30 seconds. (D) Post-exposure minus preexposure difference in locomotor activity score. Data are means, error is 95% confidence intervals in A–C; and the box represents the interquartile range, the whiskers the range, and the “+” the mean value in D. Data are analyzed by paired t-test or unpaired t-test. SHIRPA: SmithKline Beecham, Harwell, Imperial College, Royal London Hospital, Phenotype Assessment.
| CAGE | 1226645 | 1226645 | 1226645 | 1226645 | 1226645 | 1226646 | 1226646 | 1226646 | 1226646 | 1226646 | 1226647 | 1226647 | 1226647 | 1226647 | 1226647 | 1226648 | 1226648 | 1226648 | 1226648 | 1226648 | 1226649 | 1226649 | 1226649 | 1226649 | 1226649 | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MOUSE | 3 | 4 | 2 | 5 | 1 | 9 | 7 | 6 | 8 | 10 | 15 | 12 | 11 | 14 | 13 | 24 | 22 | 23 | 25 | 21 | 17 | 16 | 20 | 18 | 19 | ||||
| 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | |||||
| TOTAL SCORE | 11 | 9 | 9 | 9 | 9 | 10 | 9 | 8 | 10 | 8 | 10 | 8 | 10 | 10 | 10 | 10 | 7 | 9 | 9 | 10 | 10 | 8 | 9 | 7 | 9 | 0 | 0 | 0 | |
| Viewing Jar | |||||||||||||||||||||||||||||
| 1) Body Position | 0 = active | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||
| 1 = inactive | |||||||||||||||||||||||||||||
| 2 = excessive activity | |||||||||||||||||||||||||||||
| 2) Tremor | 0 = present | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||
| 1 = absent | |||||||||||||||||||||||||||||
| 3) Palpebral Closure | 0 = present | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||
| 1 = absent | |||||||||||||||||||||||||||||
| 4) Coat Appearance | 0 = normal | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||
| & COLOUR | 1 = abnormal | ||||||||||||||||||||||||||||
| 5) Whiskers | 0 = present | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||
| 1 = absent | |||||||||||||||||||||||||||||
| 6) Lacrimation | 0 = present | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||
| 1 = absent | |||||||||||||||||||||||||||||
| 7) Defecation | 0 = present | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | |||
| 1 = absent | |||||||||||||||||||||||||||||
| Arena | |||||||||||||||||||||||||||||
| 1) Transfer Arousal | 0 = extended freeze | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | |||
| 1 = brief freeze | |||||||||||||||||||||||||||||
| 2 = immediate movement | |||||||||||||||||||||||||||||
| 2) Locomotor Activity | total # of squares entered in 30s | 23 | 29 | 28 | 23 | 47 | 22 | 19 | 41 | 39 | 23 | 31 | 25 | 27 | 33 | 48 | 19 | 25 | 22 | 31 | 24 | 18 | 29 | 27 | 39 | 24 | |||
| 3) Gait | 0 = fluid movement | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||
| 1 = lack of fluidity | |||||||||||||||||||||||||||||
| 4) Tail Elevation | 0 = dragging | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||
| 1 = horizontal extension | |||||||||||||||||||||||||||||
| 2 = elevated/straub tail | |||||||||||||||||||||||||||||
| 5) Startle Response | 0 = preyer reflex | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||
| 1 = absent | |||||||||||||||||||||||||||||
| 2 = reaction in addition to reflex | |||||||||||||||||||||||||||||
| 6) Touch Escape | 0 = none | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||
| 1 = response to touch | |||||||||||||||||||||||||||||
| Above the Arena | 2 = flees prior to touch | ||||||||||||||||||||||||||||
| 1) Positional Passivity | 0 = struggles when held by tail | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||
| 1 = struggles when scruffed | |||||||||||||||||||||||||||||
| 2 = struggles when laid supine | |||||||||||||||||||||||||||||
| 3 = no struggle | |||||||||||||||||||||||||||||
| 2) Skin Colour | 0 = pale | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||
| 1 = pink | |||||||||||||||||||||||||||||
| 2 = red | |||||||||||||||||||||||||||||
| 3) Trunk Curl | 0 = present | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||
| 1 = absent | |||||||||||||||||||||||||||||
| 4) Limb Grasping | 0 = present | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||
| 1 = absent | |||||||||||||||||||||||||||||
| 5) Visual Placing | 0 = present | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||
| 1 = absent | |||||||||||||||||||||||||||||
| 6) Righting Reflex | 0 = present | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||
| 1 = absent | |||||||||||||||||||||||||||||
| 7) Pinnal Reflex | 0 = present | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||
| 1 = absent | |||||||||||||||||||||||||||||
| 8) Contact Righting | 0 = present | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||
| Reflex | 1 = absent | ||||||||||||||||||||||||||||
| 9) Corneal Reflex | 0 = present | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||
| 1 = absent | |||||||||||||||||||||||||||||
| 10) Biting | 0 = present | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | |||
| 1 = absent | |||||||||||||||||||||||||||||
| 11) Vocalization | 0 = present | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | |||
| 1 = absent | |||||||||||||||||||||||||||||
| 12) Morphology | 0 = normal | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||
| 1 = abnormal | |||||||||||||||||||||||||||||
| 13) Tail Pinch | 0 = response | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND |
| 1 = no response | |||||||||||||||||||||||||||||
| 14) Pupillary Light | 0 = present | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND |
| Reflex | 1 = absent | ||||||||||||||||||||||||||||
| 1) Weight (g) | 26.7 | 28.9 | 31 | 30.2 | 27.9 | 27.5 | 25.9 | 27.1 | 27.1 | 26.4 | 28.3 | 28.3 | 27.9 | 30.1 | 29.8 | 32.8 | 30.5 | 30.4 | 31.5 | 30.5 | 33.5 | 30.4 | 27.9 | 27.1 | 31.1 |
Effect of inhaled hydrogen gas on the serologic parameters of healthy mice
There were no statistically significant differences between hydrogen-exposed and control mice in markers of liver or renal injury, including alkaline phosphatase, alanine aminotransferase, total bilirubin, blood urea nitrogen and serum creatinine. The white blood cell concentration, hemoglobin concentration, and platelet count were also similar between groups, as was arterial pH, arterial partial pressure of carbon dioxide, and the ratio of arterial oxygen tension to fraction of inspired oxygen (P > 0.05 for all comparisons; Figure 2).
Figure 2.
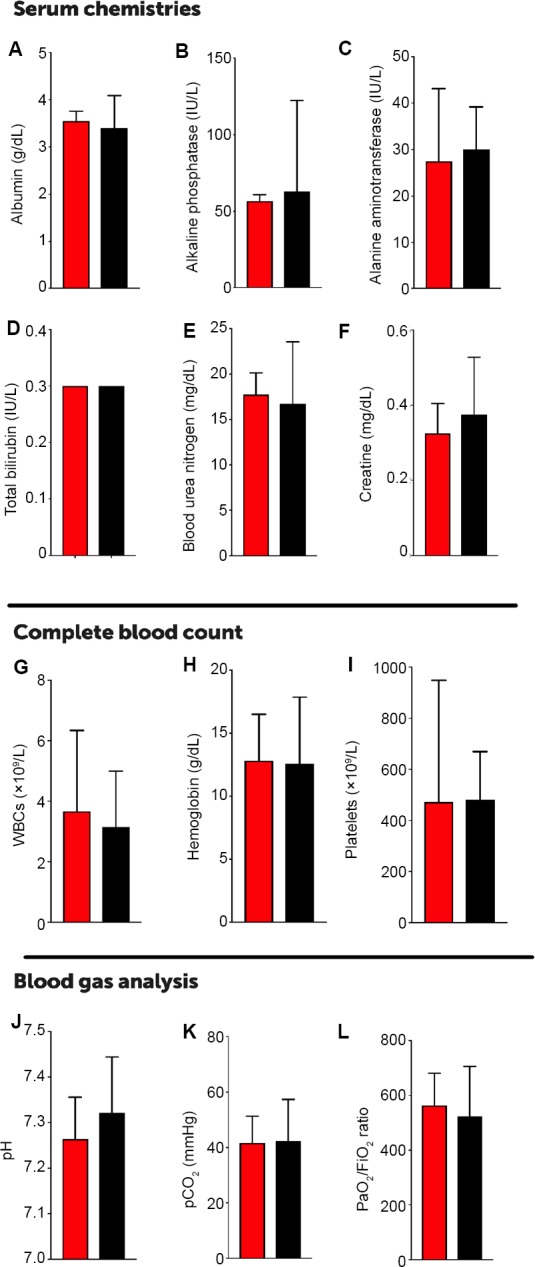
Serologic parameters and complete blood cell count of mice following exposure to gas.
Note: (A–L) Serum albumin (A), alkaline phosphatase (B), alanine aminotransferase (C), total bilirubin (D), blood urea nitrogen (E), serum creatinine (F), white blood cell concentration (WBC; G), hemoglobin concentration (H), platelet count (I), arterial pH (J), arterial partial pressure of carbon dioxide (pCO2; K), or in the ratio of arterial oxygen tension to fraction of inspired oxygen (PaO2/FiO2 ratio; L). In A–L, red represents hydrogen group, and black represents control group. Data are means, error is 95% confidence interval, and analyzed by Mann–Whitney U test.
Effect of inhaled hydrogen gas on the histology of healthy mice
There was no evidence of edema, neutrophilic or lymphocytic infiltration, or microscopic structural injury to the trachea, lungs, heart, brain, spleen, kidney, small intestine, or liver tissue in either group, and all tissues revealed normal cellular and microvascular architecture. No animal in either group exhibited signs of histologic injury by light microscopy (Figure 3). On the whole, there was no evidence of injury to airway epithelial cells by electron microscopy; in two animals exposed to hydrogen gas there was an increase in the prominence of secretory vesicles in respiratory epithelium, though nuclear, mitochondrial and ciliary structures remained intact (Figure 4).
Figure 3.
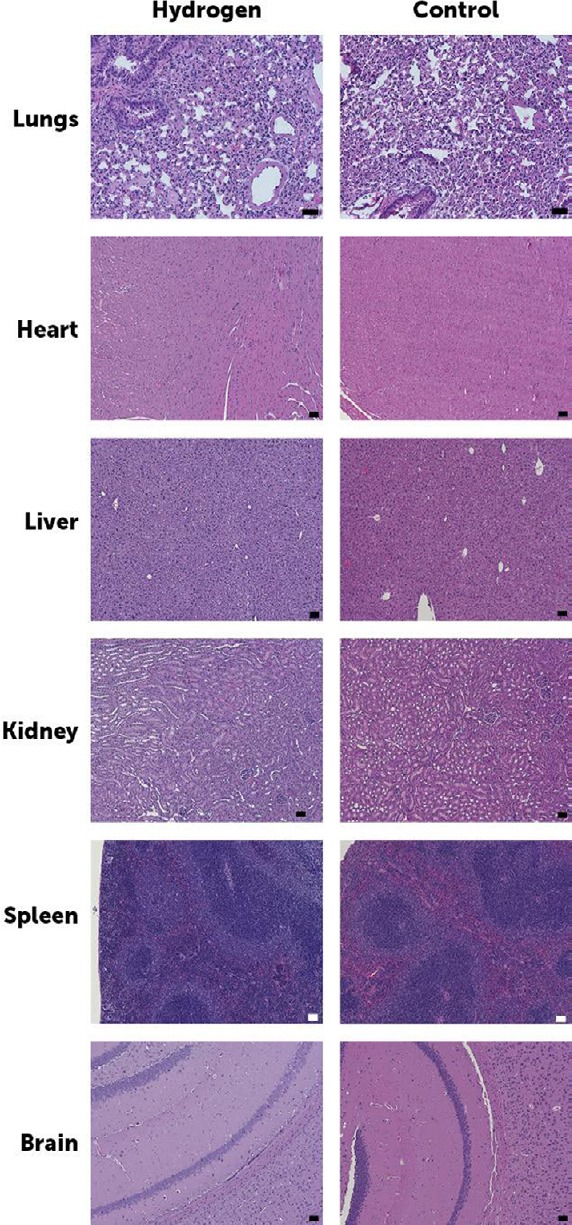
Histology of lungs, heart, liver, kidney, spleen and brain in hydrogenexposed and control animals.
Note: None of the images in either group demonstrates histologic abnormalities. Scale bars: 50 μm.
Figure 4.
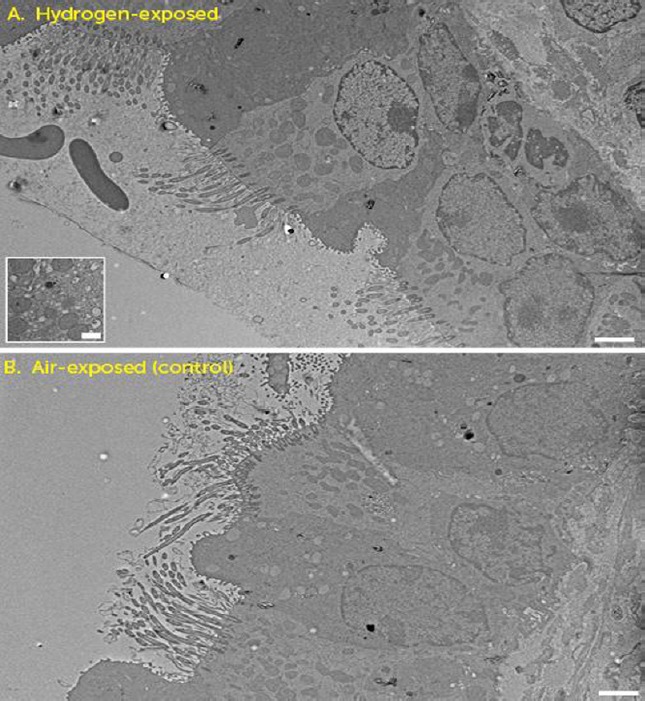
Electron microscopic analysis of the hydrogen- (A) and air-exposed (B) revealed that the micro- and macro-structures of airway epithelial cells were normal.
Note: (A, inset) Two animals exposed to hydrogen gas exhibited a prominence of secretory vesicles in respiratory epithelium, though nuclear, mitochondrial and ciliary structures remained intact. Scale bars: 2 μm.
DISCUSSION
We found that the administration of inhalational ~2% H2 gas for 72 hours is generally benign in healthy rodents, with no evidence for serologic or histologic injury to any major organs or to blood components. Perhaps the most surprising finding was the decrease in locomotor activity as quantified within the so-named subportion of the SHIRPA test, although there was no overall difference in SHIRPA scoring between groups. Notably, all animals exhibited normal skin coloring, activity level, transfer arousal, exhibited signs of neither hyperactivity nor hypoactivity, and had normal weight, making the clinical significance of this finding uncertain. The other potentially important finding was the increased presence of secretory vacuoles in the hydrogen group; this finding lacked any histologic indicators of injury and is most likely due to the increased flow rate of dry gas within the hydrogen relative to the control group.
The primary purpose of this study was to inform which endpoints might be important to examine with rigor as part of a future phase I safety trial in healthy patients. Although no safety animal study has been previously performed per se, several animal and human studies have examined for adverse effects of hydrogen albeit in combination with treatment of an injury (i.e., the equivalent of a combined phase I/IIa trial), with few notable findings. For example, the stroke trial mentioned above describes a battery of testing including hematology and serum chemistries, showing no difference between control- and hydrogen-treated patients over a 14-day period following exposure.15 Because hydrogen is an inhaled gas, it is important to note that at least based on our screening test, hydrogen does not appear to interfere with lung function or to cause significant airway reactions. Although we did not examine for this, it is also theoretically possible that hydrogen may interfere with biological processes that depend on oxyradical formation, such as leukocyte killing or cytokine generation.18 However, it has also been suggested that hydrogen treatment may improve survival in models of septic shock due to other effects, such that this may in fact be beneficial in cases of severe sepsis.18 Finally, because hydrogen has been shown by several groups to ameliorate brain injury, the identification of neurocognitive effects of the drug in healthy patients may be important to inform the results of any future neurocognitive outcomes. Our findings of decreased spontaneous locomotor activity were consistent among animals and are statistically convincing. However, the fact that animals did not appear ill in any way, ate and drank normally, and had normal skin coloring and other reassuring neurologic signs makes this finding difficult to interpret in isolation. A phase I safety trial would be a reasonable place to inquire regarding symptoms and to identify any true motor weaknesses related to hydrogen administration, however unlikely they may be.
Limitations
Our study had several limitations. First, we did not quantify serum or tissue H2 concentrations, instead quantifying the concentration of H2 of inspired gas within the holding chamber. This was primarily due to the challenges of blood sampling in mice, and it has also been demonstrated that serum concentrations of H2 reach a peak of ~10 μM within minutes of inhalation in human and fall rapidly following discontinuation of its administration.19 Second, we studied only female mice, precluding identification of gender-specific effects of the gas. Third, we measured bloodwork in a small subset of animals and were therefore underpowered to detect anything but consistent and large changes in any parameter. Fourth, we tested only a single dose and duration of hydrogen exposure, precluding any conclusions regarding the safety of a higher dose or longer duration of hydrogen administration. Finally, given the high number of endpoints that we measured (27 SHIRPA endpoints and 12 blood tests), we had an 86% likelihood of identifying a statistically significant difference between groups. This may in itself account for the differences we noted in locomotor activity.
Conclusion
Hydrogen gas does not appear to cause significant adverse effects when administered to healthy mice for 72 hours, with the possible exception of decreased spontaneous locomotor activity. Future phase I studies should consider the inclusion of a neurologic screening examination.
Additional files
Additional Figure 1 (377KB, tif) : Custom gas-tight chamber used for this experiment.
Custom gas-tight chamber used for this experiment.
Note: A front door allowed access to animals but was gas-tight when closed. Gas mixtures (air or air-hydrogen) were fed into a small port on the side of the chamber and internal fans were used to ensure air mixture within the chamber. A top vent allowed capture of gas egress, which was directed into a fume hood exhaust. Hydrogen was monitored using a probe placed near this exhaust port.
Additional Figure 1 (435.6KB, tif) : Chamber hydrogen concentration throughout the hydrogen exposure period.
Chamber hydrogen concentration throughout the hydrogen exposure period.
Note: The cage door was opened a single time in order to provide care for animals which resulted in a temporary decrement in hydrogen concentration.
Additional Table 1: Raw data of animal information in both groups.
Acknowledgements
We thank Dana-Farber/Harvard Cancer Center in Boston, MA, USA for the use of the Rodent Histopathology Core, which provided tissue processing and staining. We also thank Maria Ericsson and the Electron Microscopy Facility at Harvard Medical School, USA for processing and imaging electron microscopy images.
Footnotes
Conflicts of interest
No authors disclose any conflicts of interest related to this work.
Financial support
This study was supported by a grant from the American Heart Association, No. 15GRNT25700161 (to JNK), and by philanthropic donations to the Hess Family Cardiac Innovation Fund (to JNK), the Furber Family Innovative Therapies Fund (to JNK) and from Lindsay Bartels. Dana-Farber/Harvard Cancer Center is supported in part by an NCI Cancer Center Support Grant # NIH 5 P30 CA06516.
Institutional review board statement
The study was approved by the Institutional Animal Care and Use Committee at Boston Children’s Hospital, USA (approved number 18-01-3536) on January 25, 2018.
Copyright license agreement
The Copyright License Agreement has been signed by all authors before publication.
Data sharing statement
Datasets analyzed during the current study are available from the corresponding author on reasonable request.
Plagiarism check
Checked twice by iThenticate.
Peer review
Externally peer reviewed.
Funding: This study was supported by a grant from the American Heart Association, No. 15GRNT25700161 (to JNK), and by philanthropic donations to the Hess Family Cardiac Innovation Fund (to JNK), the Furber Family Innovative Therapies Fund (to JNK) and from Lindsay Bartels. Dana-Farber/Harvard Cancer Center is supported in part by an NCI Cancer Center Support Grant # NIH 5 P30 CA06516. Neurobehavioral testing was performed by the Neurodevelopmental Behavior Core, which is supported by 1U54HD090255.
REFERENCES
- 1.Ohsawa I, Ishikawa M, Takahashi K, et al. Hydrogen acts as a therapeutic antioxidant by selectively reducing cytotoxic oxygen radicals. Nat Med. 2007;13:688–694. doi: 10.1038/nm1577. [DOI] [PubMed] [Google Scholar]
- 2.Yu J, Yu Q, Liu Y, Zhang R, Xue L. Hydrogen gas alleviates oxygen toxicity by reducing hydroxyl radical levels in PC12 cells. PLoS One. 2017;12:e0173645. doi: 10.1371/journal.pone.0173645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iuchi K, Imoto A, Kamimura N, et al. Molecular hydrogen regulates gene expression by modifying the free radical chain reaction-dependent generation of oxidized phospholipid mediators. Sci Rep. 2016;6:18971. doi: 10.1038/srep18971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang P, Jia L, Chen B, et al. Hydrogen inhalation is superior to mild hypothermia in improving cardiac function and neurological outcome in an asphyxial cardiac arrest model of rats. Shock. 2016;46:312–318. doi: 10.1097/SHK.0000000000000585. [DOI] [PubMed] [Google Scholar]
- 5.Chen G, Chen B, Dai C, et al. Hydrogen inhalation is superior to mild hypothermia for improving neurological outcome and survival in a cardiac arrest model of spontaneously hypertensive rat. Shock. 2018;50:689–695. doi: 10.1097/SHK.0000000000001092. [DOI] [PubMed] [Google Scholar]
- 6.Hayashida K, Sano M, Kamimura N, et al. Hydrogen inhalation during normoxic resuscitation improves neurological outcome in a rat model of cardiac arrest independently of targeted temperature management. Circulation. 2014;130:2173–2180. doi: 10.1161/CIRCULATIONAHA.114.011848. [DOI] [PubMed] [Google Scholar]
- 7.Huo TT, Zeng Y, Liu XN, et al. Hydrogen-rich saline improves survival and neurological outcome after cardiac arrest and cardiopulmonary resuscitation in rats. Anesth Analg. 2014;119:368–380. doi: 10.1213/ANE.0000000000000303. [DOI] [PubMed] [Google Scholar]
- 8.Nemeth J, Toth-Szuki V, Varga V, Kovacs V, Remzso G, Domoki F. Molecular hydrogen affords neuroprotection in a translational piglet model of hypoxic-ischemic encephalopathy. J Physiol Pharmacol. 2016;67:677–689. [PubMed] [Google Scholar]
- 9.Cole AR, Perry DA, Raza A, et al. Perioperatively inhaled hydrogen gas diminishes neurologic injury following experimental circulatory arrest in swine. JACC Basic Transl Sci. 2019;4:176–187. doi: 10.1016/j.jacbts.2018.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fukuda K, Asoh S, Ishikawa M, Yamamoto Y, Ohsawa I, Ohta S. Inhalation of hydrogen gas suppresses hepatic injury caused by ischemia/reperfusion through reducing oxidative stress. Biochem Biophys Res Commun. 2007;361:670–674. doi: 10.1016/j.bbrc.2007.07.088. [DOI] [PubMed] [Google Scholar]
- 11.Kawamura T, Huang CS, Tochigi N, et al. Inhaled hydrogen gas therapy for prevention of lung transplant-induced ischemia/reperfusion injury in rats. Transplantation. 2010;90:1344–1351. doi: 10.1097/TP.0b013e3181fe1357. [DOI] [PubMed] [Google Scholar]
- 12.Tamura T, Hayashida K, Sano M, et al. Feasibility and safety of hydrogen gas inhalation for post-cardiac arrest syndrome-first-in-human pilot study. Circ J. 2016;80:1870–1873. doi: 10.1253/circj.CJ-16-0127. [DOI] [PubMed] [Google Scholar]
- 13.Tamura T, Hayashida K, Sano M, Onuki S, Suzuki M. Efficacy of inhaled hydrogen on neurological outcome following brain ischemia during post-cardiac arrest care (HYBRID II trial): study protocol for a randomized controlled trial. Trials. 2017;18:488. doi: 10.1186/s13063-017-2246-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Katsumata Y, Sano F, Abe T, et al. The effects of hydrogen gas inhalation on adverse left ventricular remodeling after percutaneous coronary intervention for ST-elevated myocardial infarction-first pilot study in humans. Circ J. 2017;81:940–947. doi: 10.1253/circj.CJ-17-0105. [DOI] [PubMed] [Google Scholar]
- 15.Ono H, Nishijima Y, Ohta S, et al. Hydrogen gas inhalation treatment in acute cerebral infarction: a randomized controlled clinical study on safety and neuroprotection. J Stroke Cerebrovasc Dis. 2017;26:2587–2594. doi: 10.1016/j.jstrokecerebrovasdis.2017.06.012. [DOI] [PubMed] [Google Scholar]
- 16.Rogers DC, Fisher EM, Brown SD, Peters J, Hunter AJ, Martin JE. Behavioral and functional analysis of mouse phenotype: SHIRPA, a proposed protocol for comprehensive phenotype assessment. Mamm Genome. 1997;8:711–713. doi: 10.1007/s003359900551. [DOI] [PubMed] [Google Scholar]
- 17.Rogers DC, Peters J, Martin JE, et al. SHIRPA, a protocol for behavioral assessment: validation for longitudinal study of neurological dysfunction in mice. Neurosci Lett. 2001;306:89–92. doi: 10.1016/s0304-3940(01)01885-7. [DOI] [PubMed] [Google Scholar]
- 18.Yu Y, Yang Y, Bian Y, et al. Hydrogen gas protects against intestinal injury in wild type but not Nrf2 knockout mice with severe sepsis by regulating HO-1 and HMGB1 release. Shock. 2017;48:364–370. doi: 10.1097/SHK.0000000000000856. [DOI] [PubMed] [Google Scholar]
- 19.Ono H, Nishijima Y, Adachi N, et al. A basic study on molecular hydrogen (H2) inhalation in acute cerebral ischemia patients for safety check with physiological parameters and measurement of blood H2 level. Med Gas Res. 2012;2:21. doi: 10.1186/2045-9912-2-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Custom gas-tight chamber used for this experiment.
Note: A front door allowed access to animals but was gas-tight when closed. Gas mixtures (air or air-hydrogen) were fed into a small port on the side of the chamber and internal fans were used to ensure air mixture within the chamber. A top vent allowed capture of gas egress, which was directed into a fume hood exhaust. Hydrogen was monitored using a probe placed near this exhaust port.
Chamber hydrogen concentration throughout the hydrogen exposure period.
Note: The cage door was opened a single time in order to provide care for animals which resulted in a temporary decrement in hydrogen concentration.